RNA-Based Multiplexing Assay for Routine Testing of Fusion and Splicing Variants in Cytological Samples of NSCLC Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient and Cell Line Samples
2.2. nCounter Elements Assay for ALK, ROS1, RET Gene Fusions and MET Alterations
2.3. DNA Purification and NGS
2.4. RT-PCR for ALK and MET
2.5. FISH and IHC
3. Results
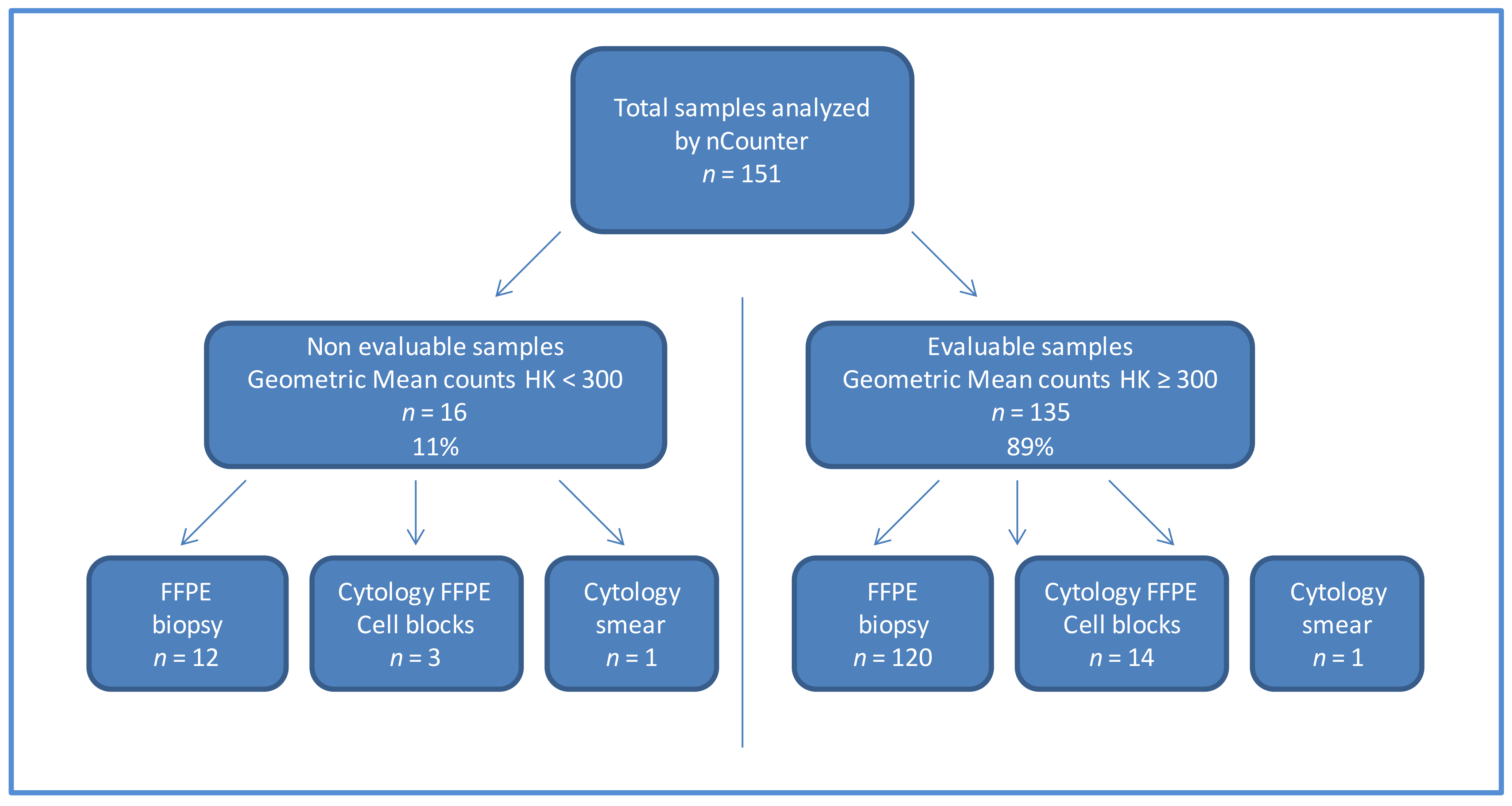
3.1. Sample Characterization
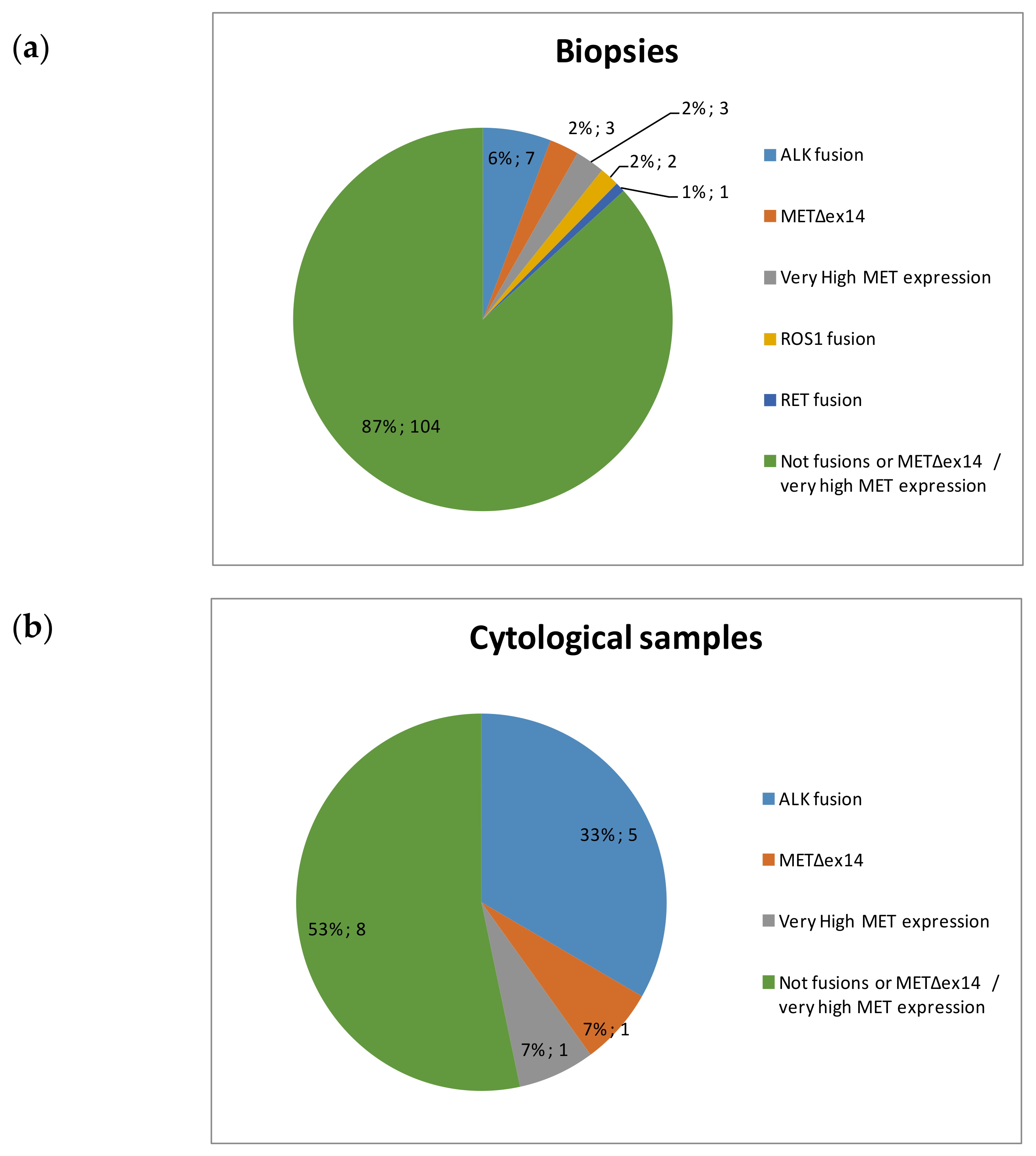
3.2. nCounter Results of Cytological Samples and Biopsies
3.3. Response to TKIs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosell, R.; Moran, T.; Queralt, C.; Porta, R.; Cardenal, F.; Camps, C.; Majem, M.; Lopez-Vivanco, G.; Isla, D.; Provencio, M.; et al. Screening for epidermal growth factor receptor mutations in lung cancer. N. Engl. J. Med. 2009, 361, 958–967. [Google Scholar] [CrossRef]
- Ramalingam, S.S.; Vansteenkiste, J.; Planchard, D.; Cho, B.C.; Gray, J.E.; Ohe, Y.; Zhou, C.; Reungwetwattana, T.; Cheng, Y.; Chewaskulyong, B.; et al. Overall Survival with Osimertinib in Untreated, EGFR-Mutated Advanced NSCLC. N. Engl. J. Med. 2020, 382, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Wolf, J.; Seto, T.; Han, J.Y.; Reguart, N.; Garon, E.B.; Groen, H.J.M.; Tan, D.S.W.; Hida, T.; de Jonge, M.; Orlov, S.V.; et al. Capmatinib in MET Exon 14-Mutated or MET-Amplified Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2020, 383, 944–957. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.; Camidge, D.R.; Shaw, A.T.; Gadgeel, S.; Ahn, J.S.; Kim, D.W.; Ou, S.I.; Perol, M.; Dziadziuszko, R.; Rosell, R.; et al. Alectinib versus Crizotinib in Untreated ALK-Positive Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2017, 377, 829–838. [Google Scholar] [CrossRef] [PubMed]
- Shaw, A.T.; Riely, G.J.; Bang, Y.J.; Kim, D.W.; Camidge, D.R.; Solomon, B.J.; Varella-Garcia, M.; Iafrate, A.J.; Shapiro, G.I.; Usari, T.; et al. Crizotinib in ROS1-rearranged advanced non-small-cell lung cancer (NSCLC): Updated results, including overall survival, from PROFILE 1001. Ann. Oncol. 2019, 30, 1121–1126. [Google Scholar] [CrossRef]
- Lira, M.E.; Choi, Y.L.; Lim, S.M.; Deng, S.; Huang, D.; Ozeck, M.; Han, J.; Jeong, J.Y.; Shim, H.S.; Cho, B.C.; et al. A single-tube multiplexed assay for detecting ALK, ROS1, and RET fusions in lung cancer. J. Mol. Diagn. 2014, 16, 229–243. [Google Scholar] [CrossRef]
- Karlsson, A.; Cirenajwis, H.; Ericson-Lindquist, K.; Brunnstrom, H.; Reutersward, C.; Jonsson, M.; Ortiz-Villalon, C.; Hussein, A.; Bergman, B.; Vikstrom, A.; et al. A combined gene expression tool for parallel histological prediction and gene fusion detection in non-small cell lung cancer. Sci. Rep. 2019, 9, 5207. [Google Scholar] [CrossRef]
- Ali, G.; Bruno, R.; Savino, M.; Giannini, R.; Pelliccioni, S.; Menghi, M.; Boldrini, L.; Proietti, A.; Chella, A.; Ribechini, A.; et al. Analysis of Fusion Genes by NanoString System: A Role in Lung Cytology? Arch. Pathol. Lab. Med. 2018, 142, 480–489. [Google Scholar] [CrossRef]
- Reguart, N.; Teixido, C.; Gimenez-Capitan, A.; Pare, L.; Galvan, P.; Viteri, S.; Rodriguez, S.; Peg, V.; Aldeguer, E.; Vinolas, N.; et al. Identification of ALK, ROS1, and RET Fusions by a Multiplexed mRNA-Based Assay in Formalin-Fixed, Paraffin-Embedded Samples from Advanced Non-Small-Cell Lung Cancer Patients. Clin. Chem. 2017, 63, 751–760. [Google Scholar] [CrossRef]
- Marin, E.; Teixido, C.; Carmona-Rocha, E.; Reyes, R.; Arcocha, A.; Vinolas, N.; Rodriguez-Mues, M.; Cabrera, C.; Sanchez, M.; Vollmer, I.; et al. Usefulness of Two Independent DNA and RNA Tissue-Based Multiplex Assays for the Routine Care of Advanced NSCLC Patients. Cancers 2020, 12, 1124. [Google Scholar] [CrossRef]
- Aguado, C.; Teixido, C.; Román, R.; Reyes, R.; Giménez-Capitán, A.; Marin, E.; Cabrera, C.; Viñolas, N.; Castillo, S.; Muñ1oz, S.; et al. RNA-based testing for multiplex detection of clinically relevant MET alterations in advanced non-small cell lung cancer. Mol. Oncol. 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- Villatoro, S.; Mayo-de-Las-Casas, C.; Jordana-Ariza, N.; Viteri-Ramirez, S.; Garzon-Ibanez, M.; Moya-Horno, I.; Garcia-Pelaez, B.; Gonzalez-Cao, M.; Malapelle, U.; Balada-Bel, A.; et al. Prospective detection of mutations in cerebrospinal fluid, pleural effusion, and ascites of advanced cancer patients to guide treatment decisions. Mol. Oncol. 2019, 13, 2633–2645. [Google Scholar] [CrossRef] [PubMed]
- Volckmar, A.L.; Leichsenring, J.; Kirchner, M.; Christopoulos, P.; Neumann, O.; Budczies, J.; Morais de Oliveira, C.M.; Rempel, E.; Buchhalter, I.; Brandt, R.; et al. Combined targeted DNA and RNA sequencing of advanced NSCLC in routine molecular diagnostics: Analysis of the first 3000 Heidelberg cases. Int. J. Cancer 2019, 145, 649–661. [Google Scholar] [CrossRef]
- Li, J.; Li, X.; Wang, W.; Shao, Y.; Zhang, Y.; Song, Z. Gene Alterations in Paired Supernatants and Precipitates from Malignant Pleural Effusions of Non-Squamous Non-Small Cell Lung Cancer. Transl. Oncol. 2020, 13, 100784. [Google Scholar] [CrossRef]
- Pisapia, P.; Malapelle, U.; Roma, G.; Saddar, S.; Zheng, Q.; Pepe, F.; Bruzzese, D.; Vigliar, E.; Bellevicine, C.; Luthra, R.; et al. Consistency and reproducibility of next-generation sequencing in cytopathology: A second worldwide ring trial study on improved cytological molecular reference specimens. Cancer Cytopathol. 2019, 127, 285–296. [Google Scholar] [CrossRef]
- Velizheva, N.P.; Rechsteiner, M.P.; Wong, C.E.; Zhong, Q.; Rossle, M.; Bode, B.; Moch, H.; Soltermann, A.; Wild, P.J.; Tischler, V. Cytology smears as excellent starting material for next-generation sequencing-based molecular testing of patients with adenocarcinoma of the lung. Cancer Cytopathol. 2017, 125, 30–40. [Google Scholar] [CrossRef] [PubMed]
- Lindeman, N.I.; Cagle, P.T.; Aisner, D.L.; Arcila, M.E.; Beasley, M.B.; Bernicker, E.H.; Colasacco, C.; Dacic, S.; Hirsch, F.R.; Kerr, K.; et al. Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment with Targeted Tyrosine Kinase Inhibitors: Guideline from the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology. J. Thorac. Oncol. 2018, 13, 323–358. [Google Scholar] [PubMed]
- Song, W.; Platteel, I.; Suurmeijer, A.J.H.; van Kempen, L.C. Diagnostic yield of NanoString nCounter FusionPlex profiling in soft tissue tumors. Genes Chromosomes Cancer 2020, 59, 318–324. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.T.E.; Goytain, A.; Tucker, T.; Karsan, A.; Lee, C.H.; Nielsen, T.O.; Ng, T.L. Development and Evaluation of a Pan-Sarcoma Fusion Gene Detection Assay Using the NanoString nCounter Platform. J. Mol. Diagn. 2018, 20, 63–77. [Google Scholar] [CrossRef]
- Ryall, S.; Arnoldo, A.; Krishnatry, R.; Mistry, M.; Khor, K.; Sheth, J.; Ling, C.; Leung, S.; Zapotocky, M.; Guerreiro Stucklin, A.; et al. Multiplex Detection of Pediatric Low-Grade Glioma Signature Fusion Transcripts and Duplications Using the NanoString nCounter System. J. Neuropathol. Exp. Neurol. 2017, 76, 562–570. [Google Scholar] [CrossRef]
- Evangelista, A.F.; Zanon, M.F.; Carloni, A.C.; de Paula, F.E.; Morini, M.A.; Ferreira-Neto, M.; Soares, I.C.; Miziara, J.E.; de Marchi, P.; Scapulatempo-Neto, C.; et al. Detection of ALK fusion transcripts in FFPE lung cancer samples by NanoString technology. BMC Pulm. Med. 2017, 17, 86. [Google Scholar] [CrossRef] [PubMed]
- Schrock, A.B.; Frampton, G.M.; Suh, J.; Chalmers, Z.R.; Rosenzweig, M.; Erlich, R.L.; Halmos, B.; Goldman, J.; Forde, P.; Leuenberger, K.; et al. Characterization of 298 Patients with Lung Cancer Harboring MET Exon 14 Skipping Alterations. J. Thorac. Oncol. 2016, 11, 1493–1502. [Google Scholar] [CrossRef] [PubMed]
- Sacher, A.G.; Dahlberg, S.E.; Heng, J.; Mach, S.; Janne, P.A.; Oxnard, G.R. Association between Younger Age and Targetable Genomic Alterations and Prognosis in Non-Small-Cell Lung Cancer. JAMA Oncol. 2016, 2, 313–320. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, S.; Petrella, F.; Buscarino, V.; De Maria, F.; Raimondi, S.; Barberis, M.; Fumagalli, C.; Spitaleri, G.; Rampinelli, C.; De Marinis, F.; et al. CT Radiogenomic Characterization of EGFR, K-RAS, and ALK Mutations in Non-Small Cell Lung Cancer. Eur. Radiol. 2016, 26, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Liang, H.; Lin, J.; Cai, X.; Pan, Z.; Liu, J.; Xie, X.; Li, C.; Cheng, B.; Zhao, Y.; et al. The incidence of lymph node metastasis in patients with different oncogenic driver mutations among T1 non-small-cell lung cancer. Lung Cancer 2019, 134, 218–224. [Google Scholar] [CrossRef]


| Probes | Number |
|---|---|
| Gene Fusions Probes (ALK, ROS1, RET, NTRK1) | 29 pairs |
| Imbalance Probes (ALK, ROS1, RET, NTRK1) | 32 pairs |
| Housekeeping Genes Probes (ACTB, GAPDH, PSMC4, MRPL19) | 3 pairs |
| MET Gene Probes (METΔex14, MET wild type) | 2 pairs |
| Characteristics | Cytological Samples (n = 15) | Biopsies (n = 120) |
|---|---|---|
| Histological type | ||
| Adenocarcinoma | 15 | 96 |
| Squamous cell carcinoma | 0 | 10 |
| Other | 0 | 13 |
| Unknown | 0 | 1 |
| UICC stage | ||
| I-IIIA | 0 | 13 |
| IIIB-IV | 12 | 84 |
| Unknown | 3 | 23 |
| Collection time | ||
| Basal | 10 | 73 |
| Progression | 3 | 11 |
| Unknown | 2 | 36 |
| Case Number | Sample Type | Procedure | Organ | % of Tumor Cell | Histology | RNA ng/µL | GeoMean Housekeeping |
|---|---|---|---|---|---|---|---|
| 1 | Cytologic smear | nd | nd | 60 | ADK | 5.2 | 1027 |
| 2 | Cell Block | FNA | Lymph node | 80 | ADK | 40 | 3043 |
| 3 | Cell Block | FNA | Suprarrenal | 85 | ADK | 13.4 | 3250 |
| 4 | Cell Block | FNA | Lung | 75 | ADK | 1.65 | 399 |
| 5 | Cell Block | nd | nd | 40 | ADK | 22.6 | 4282 |
| 6 | Cell Block | FNA | nd | 90 | ADK | 49.3 | 10,358 |
| 7 | Cell Block | FNA | Lung | 50 | ADK | 1.8 | 311 |
| 8 | Cell Block | FNA | ND | 70 | ADK | 16.2 | 3575 |
| 9 | Cell Block | nd | Lung | 50 | ADK | 1.8 | 323 |
| 10 | Cell Block | FNA | Lymph node | 80 | ADK | 3.05 | 1650 |
| 11 | Cell Block | FNA | Lung | 50 | ADK | nd | 5838 |
| 12 | Cell Block | FNA | Lymph node | 40 | ADK | 6 | 343 |
| 13 | Cell Block | FNA | Lymph node | 40 | ADK | 10.1 | 1232.98 |
| 14 | Cell Block | FNA | Lung | 60 | ADK | 3.99 | 516.98 |
| 15 | Cell Block | FNA | Lymph node | 90 | ADK | 3.04 | 1738.58 |
| Case Number | nCounter Result | FISH Genes/Result | IHC Genes/Result | RT-PCR Genes/Result | Other Results NGS Genes/Result |
|---|---|---|---|---|---|
| 1 | Wt | na | na | na | ERBB2/Amplification copies = 11 |
| 2 | Wt | na | na | na | ERBB2/Amplification copies = 9 |
| 3 | Wt | ALK/No fusión; ROS1/No fusión; MET/No amplification | ALK/Neg; MET/Neg | METΔex14/nd | nd |
| 4 | ALK fusión (5′/3′, v1) | ALK/n v | ALK/95% 3+ | METΔex14/nd; ALK v1, v2, v3/detected v1 | nd |
| 5 | Wt | na | ALK/Neg; MET/Neg | METΔex14/nd | nd |
| 6 | Wt | na | na | METΔex14/nd | EGFR/Amplification copies = 11 |
| 7 | Very high MET expression | MET/Amplification r > 5 | MET/80% 3+ | METΔex14/nd | MET Amplification copies = 25.1 |
| 8 | Wt | na | na | na | EGFR/Amplification copies = 7 |
| 9 | ALK fusión (5′/3′, v1) | na | na | na | na |
| 10 | ALK fusión (5′/3′, v3) | ALK/Fusión 58% | na | METΔex14/nd | nd |
| 11 | METΔex14 | na | na | METΔex14/detected | METΔex14 |
| 12 | Wt | na | na | METΔex14/nd | CDK4/Amplification; TP53/p.R248W |
| 13 | Wt | na | na | na | ERBB2 p.S335P; TP53 p.V157F |
| 14 | ALK fusión (5′/3′, v1) | na | ALK/Pos | na | na |
| 15 | ALK fusión (5′/3′, nd) | na | ALK/Pos | na | na |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aguado, C.; Giménez-Capitán, A.; Román, R.; Rodríguez, S.; Jordana-Ariza, N.; Aguilar, A.; Cabrera-Gálvez, C.; Rivas-Corredor, C.; Lianes, P.; Viteri, S.; et al. RNA-Based Multiplexing Assay for Routine Testing of Fusion and Splicing Variants in Cytological Samples of NSCLC Patients. Diagnostics 2021, 11, 15. https://doi.org/10.3390/diagnostics11010015
Aguado C, Giménez-Capitán A, Román R, Rodríguez S, Jordana-Ariza N, Aguilar A, Cabrera-Gálvez C, Rivas-Corredor C, Lianes P, Viteri S, et al. RNA-Based Multiplexing Assay for Routine Testing of Fusion and Splicing Variants in Cytological Samples of NSCLC Patients. Diagnostics. 2021; 11(1):15. https://doi.org/10.3390/diagnostics11010015
Chicago/Turabian StyleAguado, Cristina, Ana Giménez-Capitán, Ruth Román, Sonia Rodríguez, Núria Jordana-Ariza, Andrés Aguilar, Carlos Cabrera-Gálvez, Carlos Rivas-Corredor, Pilar Lianes, Santiago Viteri, and et al. 2021. "RNA-Based Multiplexing Assay for Routine Testing of Fusion and Splicing Variants in Cytological Samples of NSCLC Patients" Diagnostics 11, no. 1: 15. https://doi.org/10.3390/diagnostics11010015
APA StyleAguado, C., Giménez-Capitán, A., Román, R., Rodríguez, S., Jordana-Ariza, N., Aguilar, A., Cabrera-Gálvez, C., Rivas-Corredor, C., Lianes, P., Viteri, S., Moya, I., & Molina-Vila, M. A. (2021). RNA-Based Multiplexing Assay for Routine Testing of Fusion and Splicing Variants in Cytological Samples of NSCLC Patients. Diagnostics, 11(1), 15. https://doi.org/10.3390/diagnostics11010015







