Establishment of CTPA Local Diagnostic Reference Levels with Noise Magnitude as a Quality Indicator in a Tertiary Care Hospital
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. CT Parameters
2.3. Risk Assessments
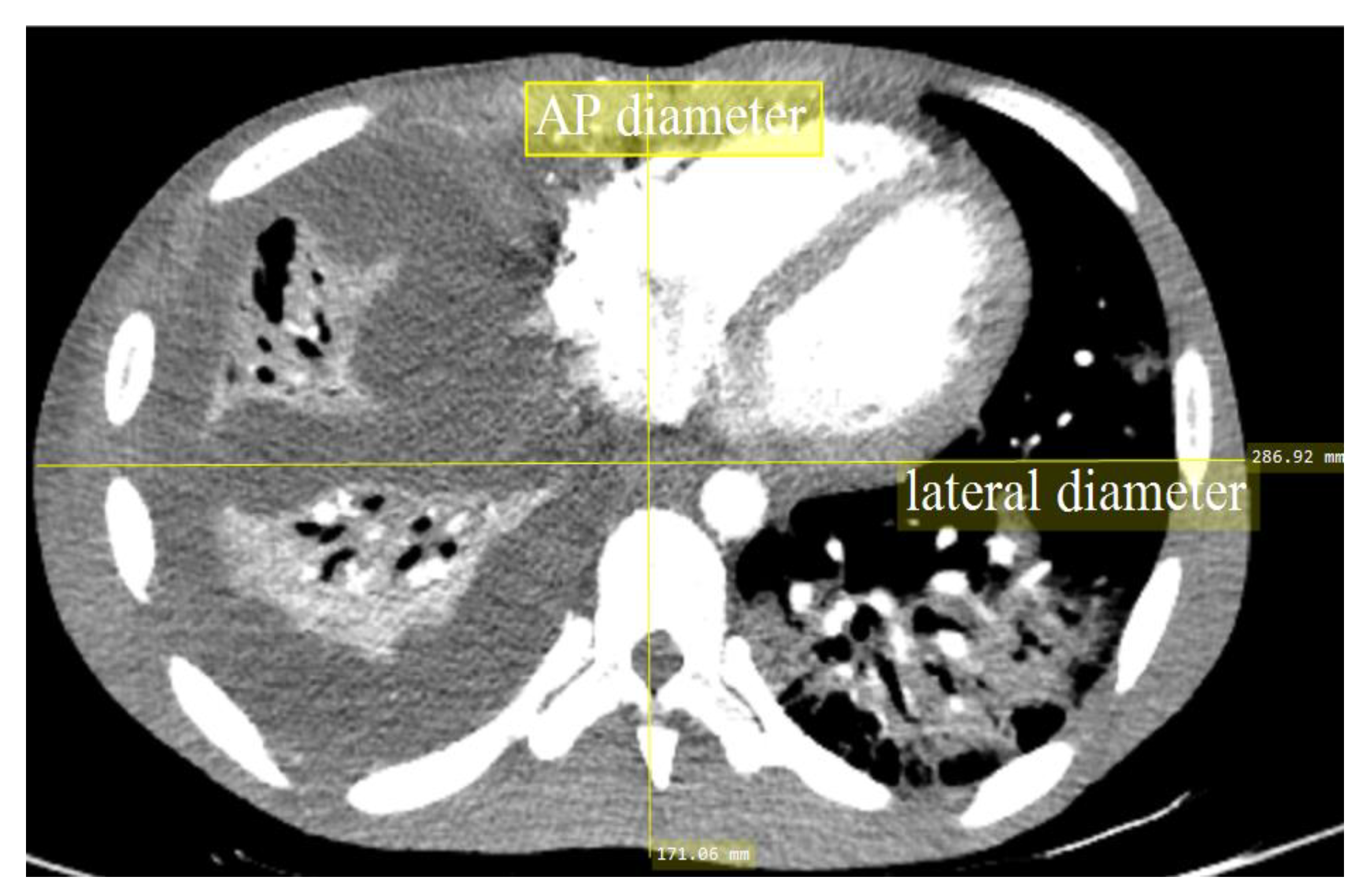
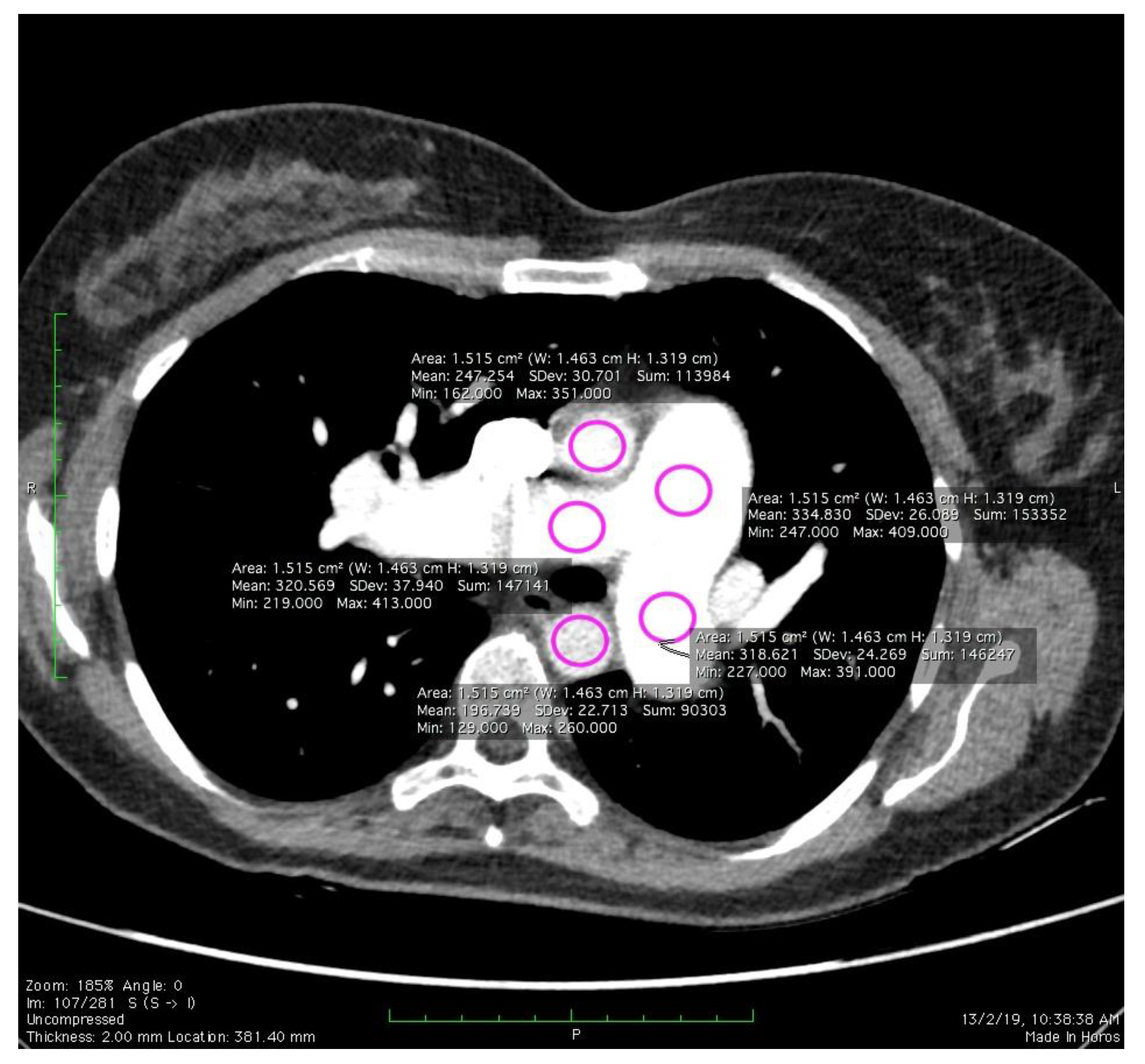
2.4. Image Quality Evaluation
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Brenner, D.J.; Hall, E.J. Cancer Risks from CT Scans: Now We Have Data, What Next? Radiology 2012, 265, 330–331. [Google Scholar] [CrossRef] [PubMed]
- Sabarudin, A.; Siong, T.W.; Chin, A.W.; Hoong, N.K.; Karim, M.K.A. A comparison study of radiation effective dose in ECG-Gated Coronary CT Angiography and calcium scoring examinations performed with a dual-source CT scanner. Sci. Rep. 2019, 9, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Karim, M.K.A.; Hashim, S.; Bradley, D.A.; Bahruddin, N.A.; Ang, W.C.; Salehhon, N. Assessment of knowledge and awareness among radiology personnel regarding current computed tomography technology and radiation dose. J. Phys. Conf. Ser. 2016, 694, 012031. [Google Scholar] [CrossRef]
- Harun, H.H.; Karim, M.K.A.; Abbas, Z.; Sabarudin, A.; Muniandy, S.C.; Razak, H.R.A.; Ng, K.H. The influence of iterative reconstruction level on image quality and radiation dose in CT pulmonary angiography examinations. Radiat. Phys. Chem. 2020, 108989. [Google Scholar] [CrossRef]
- Kalender, W.A. Dose in X-ray computed tomography. Phys. Med. Biol. 2014, 59, R129–R150. [Google Scholar] [CrossRef]
- Sorantin, E.; Weissensteiner, S.; Hasenburger, G.; Riccabona, M. CT in children-dose protection and general considerations when planning a CT in a child. Eur. J. Radiol. 2013, 82, 1043–1049. [Google Scholar] [CrossRef]
- Karim, M.K.A.; Rahim, N.A.; Matsubara, K.; Hashim, S.; Mhareb, M.H.A.; Musa, Y. The effectiveness of bismuth breast shielding with protocol optimization in CT Thorax examination. J. X-ray Sci. Technol. 2019, 27, 139–147. [Google Scholar] [CrossRef]
- Ang, W.C.; Hashim, S.; Khalis, M.; Karim, A.; Ashiqin, N.; Salehhon, N. Adaptive iterative dose reduction (AIDR) 3D in low dose CT abdomen-pelvic: Effects on image quality and radiation exposure. J. Phys. Conf. Ser. 2017, 851, 12006. [Google Scholar] [CrossRef]
- Gay, F.; Pavia, Y.; Pierrat, N.; Lasalle, S.; Neuenschwander, S.; Brisse, H.J. Dose reduction with adaptive statistical iterative reconstruction for paediatric CT: Phantom study and clinical experience on chest and abdomen CT. Eur. Radiol. 2014, 24, 102–111. [Google Scholar] [CrossRef]
- Christianson, O.; Winslow, J.; Frush, D.P.; Samei, E. Automated technique to measure noise in clinical CT examinations. Am. J. Roentgenol. 2015, 205, W93–W99. [Google Scholar] [CrossRef]
- Papadakis, A.E.; Damilakis, J. Automatic Tube Current Modulation and Tube Voltage Selection in Pediatric Computed Tomography: A Phantom Study on Radiation Dose and Image Quality. Investig. Radiol. 2019, 54, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Dane, B.; Patel, H.; O’Donnell, T.; Girvin, F.; Brusca-Augello, G.; Alpert, J.B.; Niu, B.; Attia, M.; Babb, J.; Ko, J.P. Image Quality on Dual-energy CTPA Virtual Monoenergetic Images: Quantitative and Qualitative Assessment. Acad. Radiol. 2018, 25, 1075–1086. [Google Scholar] [CrossRef] [PubMed]
- Viry, A.; Aberle, C.; Racine, D.; Knebel, J.F.; Schindera, S.T.; Schmidt, S.; Becce, F.; Verdun, F.R. Effects of various generations of iterative CT reconstruction algorithms on low-contrast detectability as a function of the effective abdominal diameter: A quantitative task-based phantom study. Phys. Medica 2018, 48, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Abadi, E.; Sanders, J.; Samei, E. Patient-specific quantification of image quality: An automated technique for measuring the distribution of organ Hounsfield units in clinical chest CT images. Med. Phys. 2017, 44, 4736–4746. [Google Scholar] [CrossRef] [PubMed]
- Sookpeng, S.; Martin, C.J.; Gentle, D.J. Comparison of different phantom designs for CT scanner automatic tube current modulation system tests. J. Radiol. Prot. 2013, 33, 735–761. [Google Scholar] [CrossRef] [PubMed]
- Harun, H.H.; Karim, M.K.A.; Muhammad, N.A.; Razak, H.R.A.; Sabarudin, A.; Muniandy, S.C. Effect of Iterative Reconstruction Algorithm Associated with Low Contrast Detectability Performance from CT Pulmonary Angiography Examinations. J. Phys. Conf. Ser. 2020, 1505, 012029. [Google Scholar] [CrossRef]
- Vañó, E.; Miller, D.L.; Martin, C.J.; Rehani, M.M.; Kang, K.; Rosenstein, M.; Ortiz-López, P.; Mattsson, S.; Padovani, R.; Rogers, A. ICRP Publication 135: Diagnostic Reference Levels in Medical Imaging. Ann. ICRP 2017, 46, 1–144. [Google Scholar] [CrossRef]
- Karim, M.K.A.; Hashim, S.; Bradley, D.A.; Bakar, K.A.; Haron, M.R.; Kayun, Z. Radiation doses from computed tomography practice in Johor Bahru, Malaysia. Radiat. Phys. Chem. 2016, 121, 69–74. [Google Scholar] [CrossRef]
- Vassileva, J.; Rehani, M.; Kostova-Lefterova, D.; Al-Naemi, H.M.; Al Suwaidi, J.S.; Arandjic, D.; Bashier, E.H.O.; Renha, S.K.; El-Nachef, L.; Aguilar, J.G.; et al. A study to establish international diagnostic reference levels for paediatric computed tomography. Radiat. Prot. Dosim. 2015, 165, 70–80. [Google Scholar] [CrossRef]
- Ria, F.; Davis, J.T.; Solomon, J.B.; Wilson, J.M.; Smith, T.B.; Frush, D.P.; Samei, E. Expanding the concept of diagnostic reference levels to noise and dose reference levels in CT. Am. J. Roentgenol. 2019, 213, 889–894. [Google Scholar] [CrossRef]
- Rehani, M.M. Limitations of diagnostic reference level (DRL) and introduction of acceptable quality dose (AQD). Br. J. Radiol. 2015, 88, 11–13. [Google Scholar] [CrossRef] [PubMed]
- Mahesh, M. NCRP Report Number 160: Its significance to medical imaging. J. Am. Coll. Radiol. 2009, 6, 890–892. [Google Scholar] [CrossRef] [PubMed]
- Kanal, K.M.; Butler, P.F.; Sengupta, D.; Bhargavan-Chatfield, M.; Coombs, L.P.; Morin, R.L. U.S. diagnostic reference levels and achievable doses for 10 adult CT examinations. Radiology 2017, 284, 120–133. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, J.C.L.; Mathias, H.; Negus, I.S.; Manghat, N.E.; Hamilton, M.C.K. Intravenous contrast medium administration at 128 multidetector row CT pulmonary angiography: Bolus tracking versus test bolus and the implications for diagnostic quality and effective dose. Clin. Radiol. 2012, 67, 1053–1060. [Google Scholar] [CrossRef] [PubMed]
- Matsubara, K.; Koshida, H.; Sakuta, K.; Takata, T.; Horii, J.; Iida, H.; Koshida, K.; Ichikawa, K.; Matsui, O. Radiation dose and physical image quality in 128-section dual-source computed tomographic coronary angiography: A phantom study. J. Appl. Clin. Med. Phys. 2012, 13, 252–261. [Google Scholar] [CrossRef]
- Qurashi, A.A.; Rainford, L.A.; Foley, S.J. Establishmentof diagnostic reference levels for CT trunk examinations in thewestern region of Saudi Arabia. Radiat. Prot. Dosim. 2015, 167, 569–575. [Google Scholar] [CrossRef]
- Visscher, K.; Jonkergouw, P.; Pieters, B.; Harbers, M.; Zöllner, J.; Geleijns, K.; Schimmel, K.; Van Swol, C.; Zweers, D.; Poot, L.; et al. NCS Report 21: Diagnostische Referentieniveaus in Nederland; Netherland Commission on Radiation Dosimetry: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Foley, S.J.; McEntee, M.F.; Rainford, L.A. Establishment of CT diagnostic reference levels in Ireland. Br. J. Radiol. 2012, 85, 1390–1397. [Google Scholar] [CrossRef]
- Shrimpton, P.C.; Hillier, M.C.; Meeson, S.; Golding, S.J. Doses from Computed Tomography (CT) Examinations in the UK—2011 Review about Public Health England; Public Health England: London, UK, 2014; ISBN 9780859517591.
- Aroua, A.; Samara, E.-T.; Bochud, F.O.; Meuli, R.; Verdun, F.R. Exposure of the Swiss population to computed tomography. BMC Med. Imaging 2013, 13, 22. [Google Scholar] [CrossRef]
- Kalender, W.A.; Buchenau, S.; Deak, P.; Kellermeier, M.; Langner, O.; van Straten, M.; Vollmar, S.; Wilharm, S. Technical approaches to the optimisation of CT. Phys. Medica 2008, 24, 71–79. [Google Scholar] [CrossRef]
- Blum, A.; Gervaise, A.; Teixeira, P. Iterative reconstruction: Why, how and when? Diagn. Interv. Imaging 2015, 96, 421–422. [Google Scholar] [CrossRef][Green Version]
- Sookpeng, S.; Martin, C.J.; Gentle, D.J. Investigation of the influence of image reconstruction filter and scan parameters on operation of automatic tube current modulation systems for different CT scanners. Radiat. Prot. Dosim. 2015, 163, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Karim, M.K.A.; Sabarudin, A.; Muhammad, N.A.; Ng, K.H. A comparative study of radiation doses between phantom and patients via CT angiography of the intra-/extra-cranial, pulmonary, and abdominal/pelvic arteries. Radiol. Phys. Technol. 2019, 12, 374–381. [Google Scholar] [CrossRef] [PubMed]
- Seeram, E.; Davidson, R.; Bushong, S.; Swan, H. Optimizing the exposure indicator as a dose management strategy in computed radiography. Radiol. Technol. 2016, 87, 380–391. [Google Scholar] [PubMed]
- Sabel, B.O.; Buric, K.; Karara, N.; Thierfelder, K.M.; Dinkel, J.; Sommer, W.H.; Meinel, F.G. High-pitch CT pulmonary angiography in third generation dual-source CT: Image quality in an unselected patient population. PLoS ONE 2016, 11, e0146949. [Google Scholar] [CrossRef]
- McLaughlin, P.D.; Liang, T.; Homiedan, M.; Louis, L.J.; O’Connell, T.W.; Krzymyk, K.; Nicolaou, S.; Mayo, J.R. High pitch, low voltage dual source CT pulmonary angiography: Assessment of image quality and diagnostic acceptability with hybrid iterative reconstruction. Emerg. Radiol. 2015, 22, 117–123. [Google Scholar] [CrossRef]
- Lu, G.M.; Luo, S.; Meinel, F.G.; McQuiston, A.D.; Zhou, C.S.; Kong, X.; Zhao, Y.E.; Zheng, L.; Schoepf, U.J.; Zhang, L.J. High-pitch computed tomography pulmonary angiography with iterative reconstruction at 80 kVp and 20 mL contrast agent volume. Eur. Radiol. 2014, 24, 3260–3268. [Google Scholar] [CrossRef]

| Baseline Characteristic | 100 kV Group (n = 74) | 120 kV Group (n = 53) | ||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| No. of examination (n) | 34 | 40 | 21 | 32 |
| AP body length (cm) * | 19.79 ± 2.61 | 20.81 ± 2.52 | 23.38 ± 3.58 | 23.36 ± 2.47 |
| Age * | 49.36 ± 17.84 | 48.00 ± 20.29 | 48.19 ± 15.97 | 53.58 ± 18.12 |
| Scanning Parameter | Values |
|---|---|
| Tube Voltage (kV) | 100 and 120 kV |
| Tube Current (mAs) * | 186.64 ± 81.84 |
| Scan Range (mm) * | 277.44 ± 88.03 |
| Pitch Factor | 0.798 |
| Beam Collimation (mm) | 0.625 × 64 |
| Slice Thickness (mm) | 1 |
| Reconstruction Interval (mm) | 0.5 |
| Rotation Time (s) | 0.50 |
| Tube Potential (kV)/Group | 100 | 120 | ||||
|---|---|---|---|---|---|---|
| P1 | P2 | P3 | P1 | P2 | P3 | |
| No. of examinations (n) | 29 | 38 | 7 | 3 | 26 | 24 |
| CTDIvol (mGy) * | 5.63 ± 2.11 | 7.20 ± 2.17 | 11.60 ± 5.71 | 9.27 ± 3.35 | 15.44 ± 6.81 | 20.44 ± 5.43 |
| DLP (mGy.cm) * | 227.71 ± 85.79 | 270.17 ± 91.48 | 465.20 ± 261.09 | 373.09 ± 104.37 | 577.71 ± 219.51 | 799.84 ± 255.25 |
| Effective Dose (mSv) * | 4.34 ± 1.95 | 5.43 ± 2.01 | 8.88 ± 3.68 | 7.47 ± 2.50 | 11.75 ± 5.04 | 15.47± 4.84 |
| Tube Potential (kVp)/Group | 100 | 120 | |||||
|---|---|---|---|---|---|---|---|
| P1 | P2 | P3 | P1 | P2 | P3 | ||
| No. of examinations (n) | 29 | 38 | 7 | 3 | 26 | 24 | |
| Noise Magnitude (HU) | Range | 14.90–33.80 | 17.03–43.44 | 18.28–33.25 | 21.46–29.81 | 17.17–34.46 | 14.90–35.36 |
| Median | 24.10 | 24.67 | 23.97 | 22.27 | 22.16 | 24.11 | |
| Mean | 23.85 | 25.91 | 24.46 | 24.51 | 23.58 | 23.96 | |
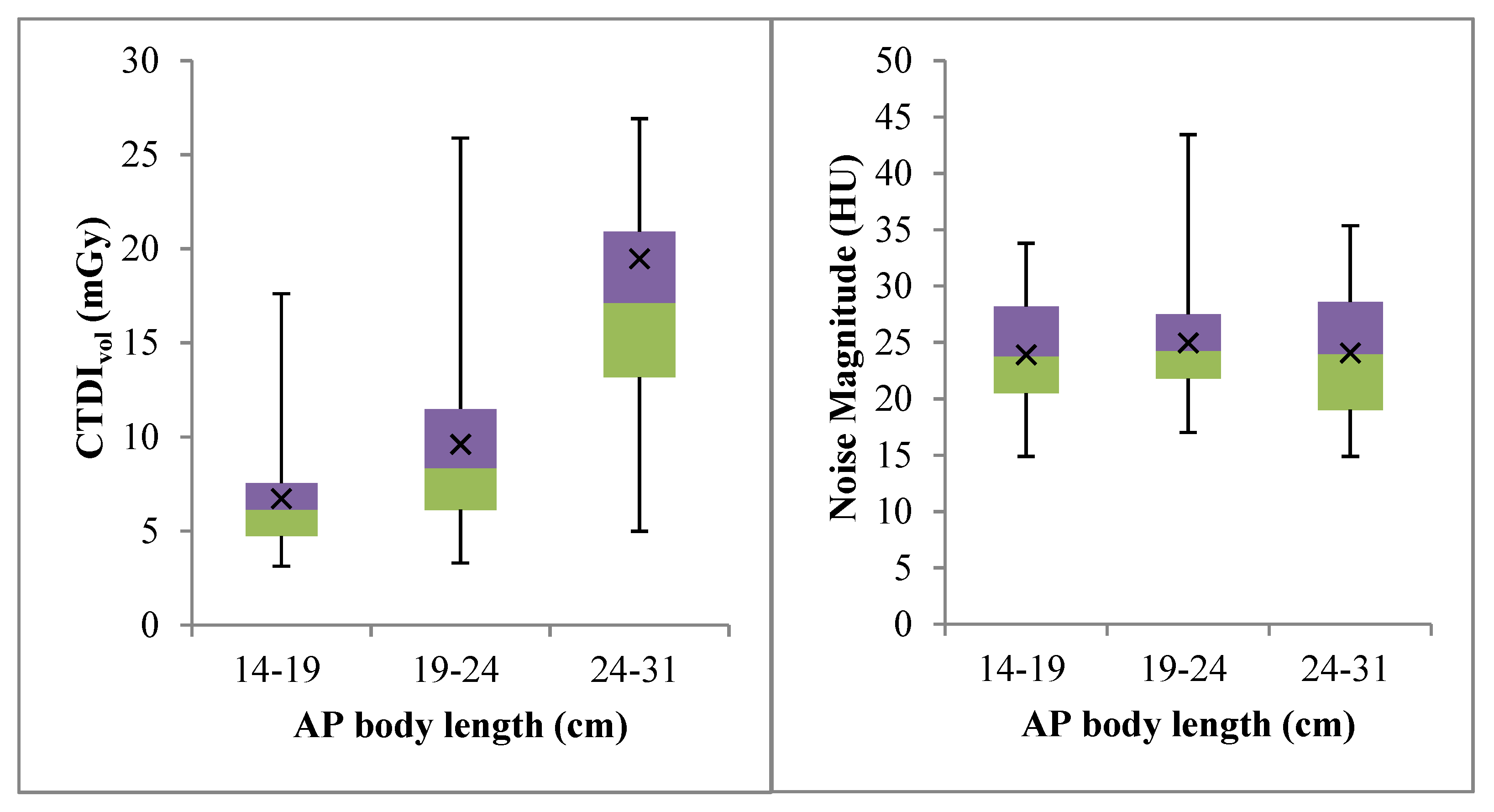
| AP Body Length (cm) * | 14–19 | 19–24 | 24–31 | p-Value |
|---|---|---|---|---|
| Dose Reference Level (mGy) | 6.13 | 8.35 | 21.40 | <0.001 |
| Dose Reference Range (mGy) | 4.73–7.55 | 6.13–11.50 | 13.70–25.20 | n.a. |
| Noise Reference Level (HU) | 23.78 | 24.26 | 23.97 | 0.703 |
| Noise Reference Range (HU) | 20.49–28.18 | 21.80–27.50 | 19.02–28.60 | n.a. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Harun, H.H.; Abdul Karim, M.K.; Abd Rahman, M.A.; Abdul Razak, H.R.; Che Isa, I.N.; Harun, F. Establishment of CTPA Local Diagnostic Reference Levels with Noise Magnitude as a Quality Indicator in a Tertiary Care Hospital. Diagnostics 2020, 10, 680. https://doi.org/10.3390/diagnostics10090680
Harun HH, Abdul Karim MK, Abd Rahman MA, Abdul Razak HR, Che Isa IN, Harun F. Establishment of CTPA Local Diagnostic Reference Levels with Noise Magnitude as a Quality Indicator in a Tertiary Care Hospital. Diagnostics. 2020; 10(9):680. https://doi.org/10.3390/diagnostics10090680
Chicago/Turabian StyleHarun, Hanif Haspi, Muhammad Khalis Abdul Karim, Mohd Amiruddin Abd Rahman, Hairil Rashmizal Abdul Razak, Iza Nurzawani Che Isa, and Faeezah Harun. 2020. "Establishment of CTPA Local Diagnostic Reference Levels with Noise Magnitude as a Quality Indicator in a Tertiary Care Hospital" Diagnostics 10, no. 9: 680. https://doi.org/10.3390/diagnostics10090680
APA StyleHarun, H. H., Abdul Karim, M. K., Abd Rahman, M. A., Abdul Razak, H. R., Che Isa, I. N., & Harun, F. (2020). Establishment of CTPA Local Diagnostic Reference Levels with Noise Magnitude as a Quality Indicator in a Tertiary Care Hospital. Diagnostics, 10(9), 680. https://doi.org/10.3390/diagnostics10090680







