Red Blood Cell Distribution Width (RDW) Predicts COVID-19 Severity: A Prospective, Observational Study from the Cincinnati SARS-CoV-2 Emergency Department Cohort
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Partient Characteristics and Outcomes
3.2. Red Blood Cell Indices and RDW
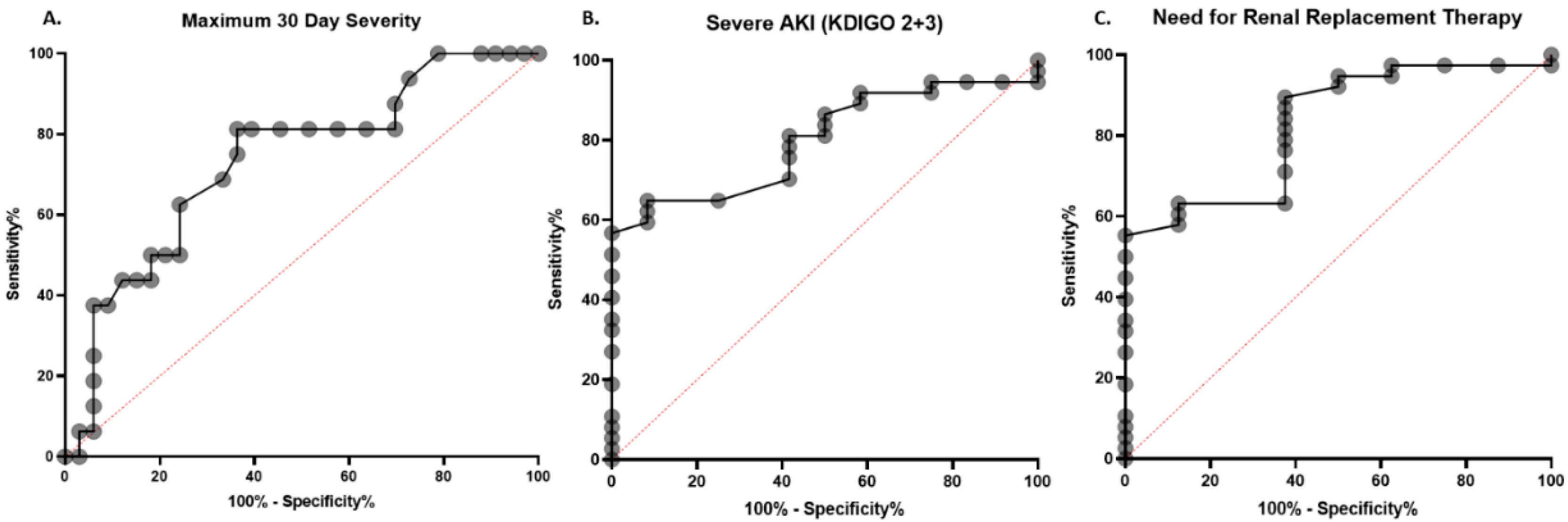
3.3. Diagnostic Performance of RDW
3.4. RDW as Predictor of Disease Severity and Severe AKI
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cowling, B.J.; Leung, G.M. Epidemiological research priorities for public health control of the ongoing global novel coronavirus (2019-nCoV) outbreak. EuroSurveillance 2020, 25. [Google Scholar] [CrossRef] [PubMed]
- Abate, S.M.; Ali, S.A.; Mantfardo, B.; Basu, B. Rate of Intensive Care Unit admission and outcomes among patients with coronavirus: A systematic review and Meta-analysis. PLoS ONE 2020, 15, e0235653. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Sanchis-Gomar, F.; Henry, B.M. Coronavirus disease 2019 (COVID-19): The portrait of a perfect storm. Ann. Transl. Med. 2020, 8, 497. [Google Scholar] [CrossRef] [PubMed]
- Wurmb, T.; Scholtes, K.; Kolibay, F.; Schorscher, N.; Ertl, G.; Ernestus, R.-I.; Vogel, U.; Franke, A.; Kowalzik, B. Hospital preparedness for mass critical care during SARS-CoV-2 pandemic. Crit. Care 2020, 24, 386. [Google Scholar] [CrossRef]
- Lippi, G.; Mattiuzzi, C.; Cervellin, G. Learning more and spending less with neglected laboratory parameters: The paradigmatic case of red blood cell distribution width. Acta Biomed 2016, 87, 323–328. [Google Scholar]
- Zhang, L.; Yu, C.-H.; Guo, K.-P.; Huang, C.-Z.; Mo, L.-Y. Prognostic role of red blood cell distribution width in patients with sepsis: A systematic review and meta-analysis. BMC Immunol. 2020, 21, 40. [Google Scholar] [CrossRef] [PubMed]
- Otero, T.M.N.; Yeh, D.D.; Bajwa, E.K.; Azocar, R.J.; Tsai, A.L.; Belcher, D.M.; Quraishi, S.A. Elevated Red Cell Distribution Width Is Associated with Decreased Ventilator-Free Days in Critically Ill Patients. J. Intensive Care Med. 2018, 33, 241–247. [Google Scholar] [CrossRef]
- Cheruiyot, I.; Henry, B.; Lippi, G.; Kipkorir, V.; Ngure, B.; Munguti, J.; Misiani, M. Acute Kidney Injury is Associated with Worse Prognosis In COVID-19 Patients: A Systematic Review and Meta-analysis. Acta Biol. Med. 2020, 91. [Google Scholar] [CrossRef]
- Hedley, B.D.; Kenney, M.; Chin-Yee, I.; Brown, W. Initial performance evaluation of the UniCel® DxH 800 Coulter® cellular analysis system. Int. J. Lab. Hematol. 2011, 33, 45–56. [Google Scholar] [CrossRef]
- Kdigo, A.K.I. Working Group KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2012, 2, 1–138. [Google Scholar]
- Wynants, L.; Van Calster, B.; Collins, G.S.; Riley, R.D.; Heinze, G.; Schuit, E.; Bonten, M.M.J.; Damen, J.A.A.; Debray, T.P.A.; De Vos, M.; et al. Prediction models for diagnosis and prognosis of covid-19 infection: Systematic review and critical appraisal. BMJ 2020, 369, m1328. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; de Oliveira, M.H.S.; Benoit, S.; Plebani, M.; Lippi, G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): A meta-analysis. Clin. Chem. Lab. Med. 2020, 58, 1021–1028. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.V.; Semba, R.D.; Ferrucci, L.; Newman, A.B.; Fried, L.P.; Wallace, R.B.; Bandinelli, S.; Phillips, C.S.; Yu, B.; Connelly, S.; et al. Red cell distribution width and mortality in older adults: A meta-analysis. J. Gerontol. A Biol. Sci. Med. Sci. 2010, 65, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Luo, R.; Hu, J.; Jiang, L.; Zhang, M. Prognostic Value of Red Blood Cell Distribution Width in Non-Cardiovascular Critically or Acutely Patients: A Systematic Review. PLoS ONE 2016, 11, e0167000. [Google Scholar] [CrossRef]
- Hu, Z.-D.; Lippi, G.; Montagnana, M. Diagnostic and prognostic value of red blood cell distribution width in sepsis: A narrative review. Clin. Biochem. 2020, 77, 1–6. [Google Scholar] [CrossRef]
- Lee, J.H.; Chung, H.J.; Kim, K.; Jo, Y.H.; Rhee, J.E.; Kim, Y.J.; Kang, K.W. Red cell distribution width as a prognostic marker in patients with community-acquired pneumonia. Am. J. Emerg. Med. 2013, 31, 72–79. [Google Scholar] [CrossRef]
- Yu, X.-S.; Chen, Z.-Q.; Hu, Y.-F.; Chen, J.-X.; Xu, W.-W.; Shu, J.; Pan, J.-Y. Red blood cell distribution width is associated with mortality risk in patients with acute respiratory distress syndrome based on the Berlin definition: A propensity score matched cohort study. Heart Lung 2020. [Google Scholar] [CrossRef]
- Wang, C.; Deng, R.; Gou, L.; Fu, Z.; Zhang, X.; Shao, F.; Wang, G.; Fu, W.; Xiao, J.; Ding, X.; et al. Preliminary study to identify severe from moderate cases of COVID-19 using combined hematology parameters. Ann. Transl. Med. 2020, 8, 593. [Google Scholar] [CrossRef]
- Thomas, T.; Stefanoni, D.; Dzieciatkowska, M.; Issaian, A.; Nemkov, T.; Hill, R.C.; Francis, R.O.; Hudson, K.E.; Buehler, P.W.; Zimring, J.C.; et al. Evidence for structural protein damage and membrane lipid remodeling in red blood cells from COVID-19 patients. medRxiv 2020. [Google Scholar] [CrossRef]
- Prieto-Pérez, L.; Fortes, J.; Soto, C.; Vidal-González, Á.; Alonso-Riaño, M.; Lafarga, M.; Cortti, M.J.; Lazaro-Garcia, A.; Pérez-Tanoira, R.; Trascasa, Á.; et al. Histiocytic hyperplasia with hemophagocytosis and acute alveolar damage in COVID-19 infection. Mod. Pathol. 2020, 1–8. [Google Scholar] [CrossRef]
- Lazarian, G.; Quinquenel, A.; Bellal, M.; Siavellis, J.; Jacquy, C.; Re, D.; Merabet, F.; Mekinian, A.; Braun, T.; Damaj, G.; et al. Autoimmune haemolytic anaemia associated with COVID-19 infection. Br. J. Haematol. 2020, 190, 29–31. [Google Scholar] [CrossRef] [PubMed]
- Angileri, F.; Légaré, S.; Gammazza, A.M.; de Macario, E.C.; Macario, A.J.L.; Cappello, F. Is molecular mimicry the culprit in the autoimmune haemolytic anaemia affecting patients with COVID-19? Br. J. Haematol. 2020, 190, e92–e93. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Sanchis-Gomar, F.; Henry, B.M. COVID-19: Unravelling the clinical progression of nature’s virtually perfect biological weapon. Ann. Transl. Med. 2020, 8, 693. [Google Scholar] [CrossRef] [PubMed]
- Martinelli, N.; Montagnana, M.; Pizzolo, F.; Friso, S.; Salvagno, G.L.; Forni, G.L.; Gianesin, B.; Morandi, M.; Lunardi, C.; Lippi, G.; et al. A relative ADAMTS13 deficiency supports the presence of a secondary microangiopathy in COVID 19. Thromb. Res. 2020, 193, 170–172. [Google Scholar] [CrossRef] [PubMed]
- Salvagno, G.L.; Sanchis-Gomar, F.; Picanza, A.; Lippi, G. Red blood cell distribution width: A simple parameter with multiple clinical applications. Crit. Rev. Clin. Lab. Sci. 2015, 52, 86–105. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Henry, B.; Hoehn, J.; Benoit, S.; Benoit, J. Validation of the Corona-Score for rapid identification of SARS-CoV-2 infections in patients seeking emergency department care in the United States. Clin. Chem. Lab. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Favaloro, E.J.; Lippi, G. Recommendations for Minimal Laboratory Testing Panels in Patients with COVID-19: Potential for Prognostic Monitoring. Semin. Thromb. Hemost. 2020, 46, 379–382. [Google Scholar] [CrossRef]
| Variable | Maximum 30-Day Severity | |||
|---|---|---|---|---|
| Mild (n = 16) | Moderate (n = 17) | Severe (n = 16) | p-Value | |
| Male: n (%) | 11 (68.8%) | 8 (44.4%) | 10 (62.5%) | 0.425 |
| Age (years): median (IQR) | 44 (32–50) | 59 (39–68) | 66 (53–71) | 0.002 |
| Body Mass Index: median (IQR) | 28 (25–33) | 26 (25–36) | 29 (25–32) | 0.886 |
| Race/Ethnicity: n (%) | ||||
| Asian | 0 (0%) | 1 (5.9%) | 0 (0%) | 0.093 |
| Black | 4 (25.0%) | 10 (58.8%) | 7 (41.2%) | |
| Hispanic | 9 (56.2%) | 3 (17.6%) | 5 (31.3%) | |
| White | 1 (6.3%) | 3 (17.6%) | 4 (25.0%) | |
| Multiracial/Other | 2 (12.5%) | 0 (0%) | 0 (0%) | |
| Comorbidities: n (%) | ||||
| Coronary Artery Disease | 0 (0%) | 4 (23.5%) | 3 (18.8%) | 0.128 |
| Heart Failure | 0 (0%) | 4 (23.5%) | 5 (31.3%) | 0.059 |
| Hypertension | 3 (18.8%) | 11 (64.7%) | 11 (68.8%) | 0.007 |
| Hyperlipidemia | 2 (12.5%) | 5 (29.4%) | 5 (31.3%) | 0.395 |
| Diabetes | 3 (18.8%) | 12 (70.6%) | 5 (31.3%) | 0.007 |
| Chronic Obstructive Pulmonary Disease | 0 (0%) | 2 (11.8%) | 6 (37.5%) | 0.013 |
| Chronic Kidney Disease | 0 (0%) | 3 (17.6%) | 3 (18.8%) | 0.191 |
| Chronic Liver Disease | 1 (0%) | 2 (11.8%) | 4 (25.0%) | 0.296 |
| Cerebrovascular Disease | 0 (0%) | 3 (17.6%) | 4 (25.0%) | 0.115 |
| Cancer | 0 (0%) | 1 (5.9%) | 3 (18.8%) | 0.148 |
| Obesity | 5 (31.3%) | 8 (44.4%) | 5 (31.3%) | 0.551 |
| Current Smoker | 4 (25.0%) | 4 (23.5%) | 5 (31.3%) | 0.869 |
| Former Smoker | 1 (6.3%) | 3 (17.6%) | 4 (25.0%) | 0.351 |
| Labs at ED * Presentation: Median (IQR) | ||||
| White Blood Cell Count (×103/mm3) | 5.7 (4.6–8.2) | 7.0 (5.7–9.8) | 6.8 (5.2–9.6) | 0.442 |
| Neutrophil Count (×103/mm3) | 3.8 (2.8–6.2) | 4.8 (4.0–8.0) | 5.2 (3.9–8.8) | 0.034 |
| Lymphocyte Count (×103/mm3) | 0.8 (0.5–1.6) | 1.0 (0.8–1.4) | 0.8 (0.6–1.2) | 0.332 |
| Platelet Count (×103/mm3) | 193.0 (164.8–238.0) | 208.0 (155.0–275.3) | 211.5 (152.5–346.8) | 0.710 |
| C-Reactive Protein (mg/dL) | 1.5 (0.7–7.5) | 8.6 (2.8–15.8) | 4.8 (2.7–12.2) | 0.108 |
| Ferritin (ug/L) | 352.0 (122.0–1088.0) | 251.0 (101.5–995.5) | 1032.0 (232.5–1475.0) | 0.1198 |
| Days from symptom onset to ED presentation: median (IQR) | 6 (3–7) | 7 (5–10) | 5 (1–10) | 0.551 |
| Variable | ED Disposition Severity | Maximum Severity within 30 Days of Presentation | ||||||
|---|---|---|---|---|---|---|---|---|
| Mild (n = 16) | Moderate (n = 27) | Severe (n = 6) | p-Value | Mild (n = 16) | Moderate (n = 17) | Severe (n = 16) | p-Value | |
| Hematocrit (%) | 43.9 (40.4–45.4) | 37.5 (34.3–41.4) | 35.1 (24.7–42.0) | <0.001 | 43.9 (40.4–45.4) | 38.5 (34.8–41.3) | 37.1 (31.9–42.1) | 0.002 |
| Hemoglobin (g/dL) | 14.8 (14.0–15.4) | 12.6 (11.2–13.7) | 11.1 (8.4–13.9) | <0.001 | 14.1 (13.7–15.2) | 12.3 (11.3–13.4) | 12.5 (10.1–14.0) | 0.017 |
| Mean corpuscular volume (MCV) (fL) | 86.4 (82.9–89.1) | 85.9 (81.1–88.3) | 86.7 (81.5–94.4) | 0.639 | 86.4 (82.9–89.1) | 85.8 (81.8–87.6) | 86.0 (81.1–90.5) | 0.685 |
| Mean corpuscular hemoglobin (MCH) (pg/cell) | 29.7 (28.7–30.6) | 27.7 (26.5–30.1) | 29.4 (27.1–31.1) | 0.236 | 29.7 (28.7–30.6) | 27.3 (26.7–29.9) | 29.3 (26.7–31.1) | 0.244 |
| Mean corpuscular hemoglobin concentration (MCHC) (g/DL) | 34.4 (33.3–34.7) | 32.8 (31.4–34.0) | 33.3 (31.4–34.6) | 0.049 | 34.4 (33.3–34.7) | 32.3 (31.6–33.9) | 33.5 (32.1–34.3) | 0.035 |
| Red Blood Cell Distribution Width (RDW-CV) (%) | 13.5 (13.1–13.9) | 14.8 (13.9–16.7) | 17.7 (14.9–19.48) | <0.001 | 13.5 (13.1–13.8) | 14.8 (13.8–16.7) | 16.0 (14.6–18.7) | 0.001 |
| Severe COVID-19 | ||||
| Variable | Estimate | Std Error | OR (95% CI) | p-Value |
| Age | 0.109 | 0.042 | 1.12 (1.03–1.21) | 0.010 |
| Sex (Male) | 1.856 | 0.974 | 6.40 (0.95–43.12) | 0.057 |
| Race (Hispanic) | 2.485 | 1.311 | 12 (0.92–156.66) | 0.058 |
| Race (White) | −0.106 | 1.143 | 0.90 (0.1–8.45) | 0.926 |
| Elevated RDW | 2.220 | 1.114 | 9.20 (1.04–81.74) | 0.046 |
| Severe AKI (KDIGO) | ||||
| Variable | Estimate | Std Error | OR (95% CI) | p-Value |
| BMI | −0.134 | 0.066 | 0.87 (0.7–0.99) | 0.043 |
| Elevated RDW | 2.774 | 1.133 | 16.03 (1.74–147.6) | 0.014 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Henry, B.M.; Benoit, J.L.; Benoit, S.; Pulvino, C.; Berger, B.A.; Olivera, M.H.S.d.; Crutchfield, C.A.; Lippi, G. Red Blood Cell Distribution Width (RDW) Predicts COVID-19 Severity: A Prospective, Observational Study from the Cincinnati SARS-CoV-2 Emergency Department Cohort. Diagnostics 2020, 10, 618. https://doi.org/10.3390/diagnostics10090618
Henry BM, Benoit JL, Benoit S, Pulvino C, Berger BA, Olivera MHSd, Crutchfield CA, Lippi G. Red Blood Cell Distribution Width (RDW) Predicts COVID-19 Severity: A Prospective, Observational Study from the Cincinnati SARS-CoV-2 Emergency Department Cohort. Diagnostics. 2020; 10(9):618. https://doi.org/10.3390/diagnostics10090618
Chicago/Turabian StyleHenry, Brandon Michael, Justin Lee Benoit, Stefanie Benoit, Christina Pulvino, Brandon A. Berger, Maria Helena Santos de Olivera, Christopher A. Crutchfield, and Giuseppe Lippi. 2020. "Red Blood Cell Distribution Width (RDW) Predicts COVID-19 Severity: A Prospective, Observational Study from the Cincinnati SARS-CoV-2 Emergency Department Cohort" Diagnostics 10, no. 9: 618. https://doi.org/10.3390/diagnostics10090618
APA StyleHenry, B. M., Benoit, J. L., Benoit, S., Pulvino, C., Berger, B. A., Olivera, M. H. S. d., Crutchfield, C. A., & Lippi, G. (2020). Red Blood Cell Distribution Width (RDW) Predicts COVID-19 Severity: A Prospective, Observational Study from the Cincinnati SARS-CoV-2 Emergency Department Cohort. Diagnostics, 10(9), 618. https://doi.org/10.3390/diagnostics10090618







