Effect of Scanning Resolution on the Prediction of Trabecular Bone Microarchitectures Using Dental Cone Beam Computed Tomography
Abstract
1. Introduction
2. Materials and Methods
2.1. Specimen Preparation
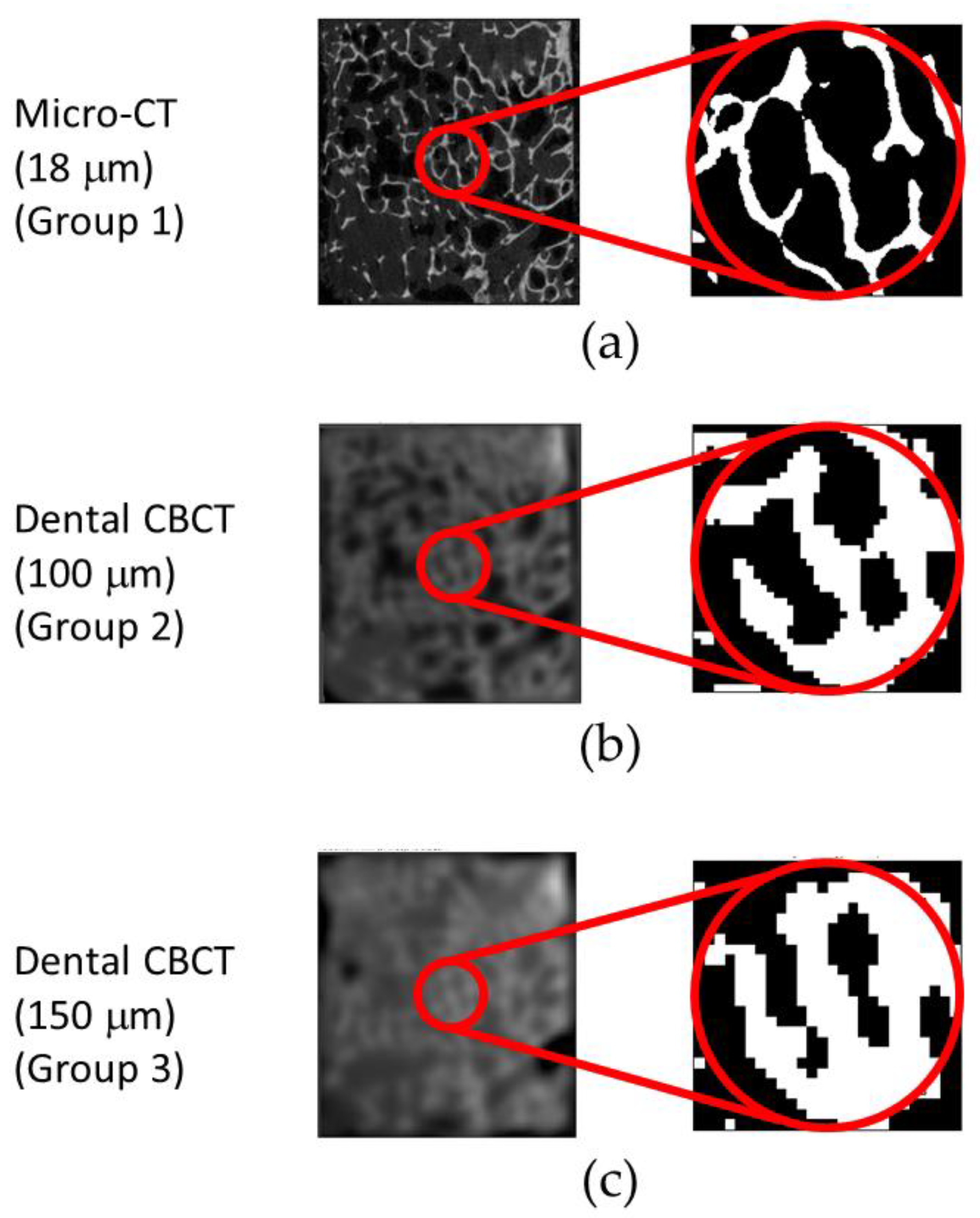
2.2. Micro-CT and Dental CBCT Scanning and Trabecular Bone Microarchitectural Measurement
2.3. Statistical Analysis
3. Results
3.1. Trabecular Bone Microarchitectures Measured with Micro-CT and Dental CBCT
3.2. Relation between the Trabecular Bone Microstructures from Micro-CT and Dental CBCT
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Guillaume, B. Dental implants: A review. Morphologie 2016, 100, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Pye, A.; Lockhart, D.; Dawson, M.; Murray, C.; Smith, A. A review of dental implants and infection. J. Hosp. Infect. 2009, 72, 104–110. [Google Scholar] [CrossRef] [PubMed]
- De Groot, R.; Oomens, M.; Forouzanfar, T.; Schulten, E. Bone augmentation followed by implant surgery in the edentulous mandible: A systematic review. J. Oral Rehabil. 2018, 45, 334–343. [Google Scholar] [CrossRef] [PubMed]
- Ko, Y.C.; Huang, H.L.; Shen, Y.W.; Cai, J.Y.; Fuh, L.J.; Hsu, J.T. Variations in crestal cortical bone thickness at dental implant sites in different regions of the jawbone. Clin. Implant Dent. Relat. Res. 2017, 19, 440–446. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Albrektsson, T.; Wennerberg, A. Bone Quality and Quantity and Dental Implant Failure: A Systematic Review and Meta-analysis. Int. J. Prosthodont. 2017, 30, 219–237. [Google Scholar] [CrossRef]
- Porter, J.A.; Von Fraunhofer, J.A. Success or failure of dental implants? A literature review with treatment considerations. Gen. Dent. 2005, 53, 423–432. [Google Scholar]
- Bouxsein, M.L.; Boyd, S.K.; Christiansen, B.A.; Guldberg, R.E.; Jepsen, K.J.; Müller, R. Guidelines for assessment of bone microstructure in rodents using micro–computed tomography. J. Bone Miner. Res. 2010, 25, 1468–1486. [Google Scholar] [CrossRef]
- Donnelly, E. Methods for assessing bone quality: A review. Clin. Orthop. Relat. Res. 2011, 469, 2128–2138. [Google Scholar] [CrossRef]
- Schambach, S.J.; Bag, S.; Schilling, L.; Groden, C.; Brockmann, M.A. Application of micro-CT in small animal imaging. Methods 2010, 50, 2–13. [Google Scholar] [CrossRef]
- Holdsworth, D.W.; Thornton, M.M. Micro-CT in small animal and specimen imaging. Trends Biotechnol. 2002, 20, S34–S39. [Google Scholar] [CrossRef]
- Fuh, L.; Huang, H.; Chen, C.; Fu, K.; Shen, Y.; Tu, M.; Shen, W.; Hsu, J. Variations in bone density at dental implant sites in different regions of the jawbone. J. Oral Rehabil. 2010, 37, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Norton, M.R.; Gamble, C. Bone classification: An objective scale of bone density using the computerized tomography scan. Clin. Oral Implant. Res. 2001, 12, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Parsa, A.; Ibrahim, N.; Hassan, B.; Stelt, P.; Wismeijer, D. Bone quality evaluation at dental implant site using multislice CT, micro-CT, and cone beam CT. Clin. Oral Implant. Res. 2015, 26, e1–e7. [Google Scholar] [CrossRef]
- Aranyarachkul, P.; Caruso, J.; Gantes, B.; Schulz, E.; Riggs, M.; Dus, I.; Yamada, J.M.; Crigger, M. Bone density assessments of dental implant sites: 2. Quantitative cone-beam computerized tomography. Int. J. Oral Maxillofac. Implant. 2005, 20, 416–424. [Google Scholar]
- Lee, S.; Gantes, B.; Riggs, M.; Crigger, M. Bone density assessments of dental implant sites: 3. Bone quality evaluation during osteotomy and implant placement. Int. J. Oral Maxillofac. Implant. 2007, 22, 208–212. [Google Scholar]
- González-García, R.; Monje, F. The reliability of cone-beam computed tomography to assess bone density at dental implant recipient sites: A histomorphometric analysis by micro-CT. Clin. Oral Implant. Res. 2013, 24, 871–879. [Google Scholar] [CrossRef]
- Alamri, H.M.; Sadrameli, M.; Alshalhoob, M.; Alshehri, M. Applications of CBCT in dental practice: A review of the literature. Gen. Dent. 2012, 60, 390–400. [Google Scholar]
- Benavides, E.; Rios, H.F.; Ganz, S.D.; An, C.-H.; Resnik, R.; Reardon, G.T.; Feldman, S.J.; Mah, J.K.; Hatcher, D.; Kim, M.-J. Use of cone beam computed tomography in implant dentistry: The International Congress of Oral Implantologists consensus report. Implant Dent. 2012, 21, 78–86. [Google Scholar] [CrossRef]
- Benic, G.I.; Elmasry, M.; Hämmerle, C.H. Novel digital imaging techniques to assess the outcome in oral rehabilitation with dental implants: A narrative review. Clin. Oral Implant. Res. 2015, 26, 86–96. [Google Scholar] [CrossRef]
- Dawood, A.; Brown, J.; Sauret-Jackson, V.; Purkayastha, S. Optimization of cone beam CT exposure for pre-surgical evaluation of the implant site. Dentomaxillofac. Radiol. 2012, 41, 70–74. [Google Scholar] [CrossRef]
- He, R.-T.; Tu, M.-G.; Huang, H.-L.; Tsai, M.-T.; Wu, J.; Hsu, J.-T. Improving the prediction of the trabecular bone microarchitectural parameters using dental cone-beam computed tomography. BMC Med. Imaging 2019, 19, 10. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, N.; Parsa, A.; Hassan, B.; Stelt, P.; Aartman, I.H.; Wismeijer, D. Accuracy of trabecular bone microstructural measurement at planned dental implant sites using cone-beam CT datasets. Clin. Oral Implant. Res. 2014, 25, 941–945. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-E.; Yi, W.-J.; Heo, M.-S.; Lee, S.-S.; Choi, S.-C.; Huh, K.-H. Three-dimensional evaluation of human jaw bone microarchitecture: Correlation between the microarchitectural parameters of cone beam computed tomography and micro-computer tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2015, 120, 762–770. [Google Scholar] [CrossRef]
- Naitoh, M.; Aimiya, H.; Hirukawa, A.; Ariji, E. Morphometric analysis of mandibular trabecular bone using cone beam computed tomography: An in vitro study. Int. J. Oral Maxillofac. Implant. 2010, 25, 1093–1098. [Google Scholar]
- Panmekiate, S.; Ngonphloy, N.; Charoenkarn, T.; Faruangsaeng, T.; Pauwels, R. Comparison of mandibular bone microarchitecture between micro-CT and CBCT images. Dentomaxillofac. Radiol. 2015, 44, 20140322. [Google Scholar] [CrossRef]
- Pauwels, R.; Faruangsaeng, T.; Charoenkarn, T.; Ngonphloy, N.; Panmekiate, S. Effect of exposure parameters and voxel size on bone structure analysis in CBCT. Dentomaxillofac. Radiol. 2015, 44, 20150078. [Google Scholar] [CrossRef]
- Ho, J.-T.; Wu, J.; Huang, H.-L.; Chen, M.Y.; Fuh, L.-J.; Hsu, J.-T. Trabecular bone structural parameters evaluated using dental cone-beam computed tomography: Cellular synthetic bones. Biomed. Eng. Online 2013, 12, 115. [Google Scholar] [CrossRef]
- Kang, S.-R.; Bok, S.-C.; Choi, S.-C.; Lee, S.-S.; Heo, M.-S.; Huh, K.-H.; Kim, T.-I.; Yi, W.-J. The relationship between dental implant stability and trabecular bone structure using cone-beam computed tomography. J. Periodontal Implant Sci. 2016, 46, 116–127. [Google Scholar] [CrossRef]
- Nicolielo, L.; Van Dessel, J.; Jacobs, R.; Soares, M.; Collaert, B. Relationship Between Trabecular Bone Architecture and Early Dental Implant Failure in the Posterior Region of the Mandible. Clin. Oral Implant. Res. 2020, 31, 153–161. [Google Scholar] [CrossRef]
- Kulah, K.; Gulsahi, A.; Kamburoğlu, K.; Geneci, F.; Ocak, M.; Celik, H.; Ozen, T. Evaluation of Maxillary Trabecular Microstructure as an Indicator of Implant Stability by Using 2 Cone Beam Computed Tomography Systems and Micro-Computed Tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 127, 247–256. [Google Scholar] [CrossRef]
- Van Dessel, J.; Huang, Y.; Depypere, M.; Rubira-Bullen, I.; Maes, F.; Jacobs, R. A comparative evaluation of cone beam CT and micro-CT on trabecular bone structures in the human mandible. Dentomaxillofac. Radiol. 2013, 42, 20130145. [Google Scholar] [CrossRef] [PubMed]
| Group Number | Scanning Method | Resolution | Machine | Scanning Voltage | Scanning Current | Scanning Time |
|---|---|---|---|---|---|---|
| 1 | Micro-CT | 18 μm | Skyscan 1076 | 80 kV | 313 μA | 450 ms |
| 2 | Dental CBCT | 100 μm | Asahi AZ 3000 | 85 kV | 6 mA | 17 s |
| 3 | Dental CBCT | 150 μm | Asahi AZ 3000 | 85 kV | 6 mA | 17 s |
| Scanning Method | Group | Trabecular Bone Microstructure Parameter | |||
|---|---|---|---|---|---|
| BV/TV (%) | Tb.Th (mm) | Tb.N (mm−1) | Tb.Sp (mm) | ||
| Mean ± S.D. * | Mean ± S.D. * | Mean ± S.D. * | Mean ± S.D. * | ||
| Micro-CT | 1 | 24.900 ± 7.031 a | 0.200 ± 0.021 a | 1.184 ± 0.367 a | 0.717 ± 0.215 a |
| Dental CBCT | 2 | 44.100 ± 12.554 b | 0.648 ± 0.075 b | 0.672 ± 0.155 b | 0.855 ± 0.215 b |
| Dental CBCT | 3 | 49.957 ± 8.100 b | 0.719 ± 0.077 b | 0.699 ± 0.117 b | 0.810 ± 0.172 b |
| Comparison | Trabecular Bone Microarchitecture | ||||
|---|---|---|---|---|---|
| BV/TV | Tb.Th | Tb.N | Tb.Sp | ||
| Group 1 vs. Group 2 | r | 0.840 | 0.294 | 0.739 | 0.820 |
| p | <0.001 | 0.129 | <0.001 | <0.001 | |
| Group 1 vs. Group 3 | r | 0.758 | 0.215 | 0.367 | 0.724 |
| p | <0.001 | 0.271 | 0.055 | <0.001 | |
| Group 2 vs. Group 3 | r | 0.876 | 0.350 | 0.625 | 0.736 |
| p | <0.001 | 0.068 | <0.001 | <0.001 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, M.-T.; He, R.-T.; Huang, H.-L.; Tu, M.-G.; Hsu, J.-T. Effect of Scanning Resolution on the Prediction of Trabecular Bone Microarchitectures Using Dental Cone Beam Computed Tomography. Diagnostics 2020, 10, 368. https://doi.org/10.3390/diagnostics10060368
Tsai M-T, He R-T, Huang H-L, Tu M-G, Hsu J-T. Effect of Scanning Resolution on the Prediction of Trabecular Bone Microarchitectures Using Dental Cone Beam Computed Tomography. Diagnostics. 2020; 10(6):368. https://doi.org/10.3390/diagnostics10060368
Chicago/Turabian StyleTsai, Ming-Tzu, Rong-Ting He, Heng-Li Huang, Ming-Gene Tu, and Jui-Ting Hsu. 2020. "Effect of Scanning Resolution on the Prediction of Trabecular Bone Microarchitectures Using Dental Cone Beam Computed Tomography" Diagnostics 10, no. 6: 368. https://doi.org/10.3390/diagnostics10060368
APA StyleTsai, M.-T., He, R.-T., Huang, H.-L., Tu, M.-G., & Hsu, J.-T. (2020). Effect of Scanning Resolution on the Prediction of Trabecular Bone Microarchitectures Using Dental Cone Beam Computed Tomography. Diagnostics, 10(6), 368. https://doi.org/10.3390/diagnostics10060368





