Improving Access to Diagnostics for Schistosomiasis Case Management in Oyo State, Nigeria: Barriers and Opportunities
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Study Setting
2.3. Study Sample
2.4. Data Collection
2.5. Data Entry and Analysis
3. Results
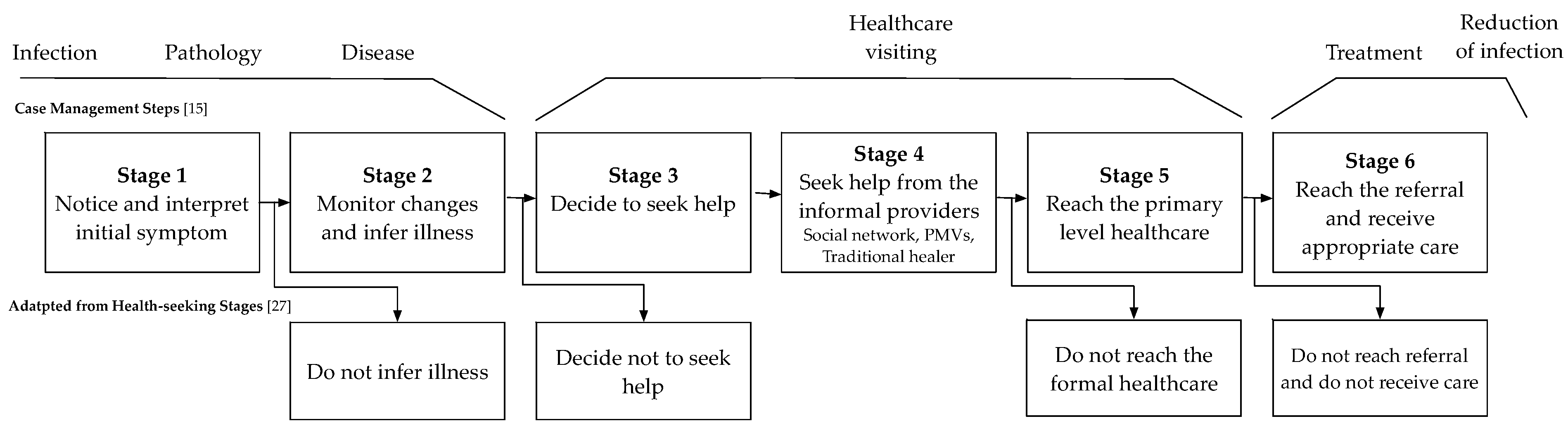
3.1. Health-Seeking Stages Identified in the Case Management
3.1.1. Stage 1: Notice and Interpret the Initial Symptoms
“I told her mum to keep her eyes on him, and she later saw him urinate and sighted blood in his urine, …”.—Parent of a child who had schistosomiasis from Rural LGA
“I said it’s like a cultural thing, once you have haematuria, that normalises you as a true son of the soil…”—Public Health Researcher
“You know that dogs have blood in their urine. In the Southwest of Nigeria, it is called Atosi Aja. This is why they believe that it is not a medical condition and they prefer treating it traditionally”—PHC Coordinator (Rural LGA)
“Some people are aware of schistosomiasis, but most people believe that the spiritual forces have cursed the victim”—Community mobilizer (Urban LGA)
3.1.2. Stage 2: Monitor Changes and Infer Illness
“after five days…, okay you want to see if his condition will be better before deciding to take him to the hospital.”—Parent of a child who had schistosomiasis (Rural LGA)
“We gave him paracetamol and yet there was no difference, he was sweating, and we took him outside to take fresh air…”—Parent of a child who had schistosomiasis (Rural LGA)
3.1.3. Stage 3: Decide to Seek Help
“Where I (people community) will go next is dependent on that. For instance, if I speak to a friend who is a pastor and he asks me to come to his church for healing prayers, then I would go to the church. If someone says that they had once experienced such and they saw a Community Health Extension Workers (CHEW), I would follow suit.”—Doctor PHC (Urban LGA)
“…it is possible that it is a sexually transmitted disease…So it is possible that people may contract the disease but may be too shy or lack the courage to tell someone because of losing their dignity and privacy.”—Guardian of child who had schistosomiasis (Urban LGA)
3.1.4. Stage 4: Seek Help from the Social Network and Informal Healthcare Providers
Stage 4.1. Seeking Help from Social Network
“He said it just found out he urinated blood …. so when he mentioned it was where his apprentice told him there is someone that treated him when he contracted the same disease…”—Traditional healer (Urban LGA)
“…he confided in someone that he had contracted the disease and I got to know through that person though I was warned not to ask him or pretend as if I am not aware…”—Guardian of a child who had schistosomiasis (Urban LGA)
“he has never heard of it (schistosomiasis), he only knows about reddish urine…”—Guardian of a child who had schistosomiasis 2 (Urban LGA)
Stage 4.2. Seeking Help through Traditional Medicine
“they probably just tell them “oh it is spiritual problem” “Oh, it’s not normal, it’s something spiritual...”—Public Health Researcher
“It depends on customs and traditions. It also depends on the condition because they may think that the disease is as a result of witchcraft and wizardry...”—PHC Coordinator (Rural LGA)
Stage 4.3. Seeking Over-the-Counter Medications from PMVs or Drug Vendors
“I usually bought drugs from drug vendors that hawks…”—Mother with a treated child with schistosomiasis (Rural LGA)
“They want immediate solutions, so they first buy herbs or patronize the PMVs.”—Community Mobilizer/CHO (Rural LGA)
“Because of ignorance, the people go to them because they are at every nook and cranny”—MOH/PHC Coordinator (Urban LGA)
“They mostly do trial and error just in a bid to make money regardless of lacking knowledge…”—NTD Officer (Urban LGA)
3.1.5. Stage 5: Reach the Primary Level Healthcare
“The PHC is a bit far away from their places but they still come around because of the relationship we have with them.”—CHEW (Rural LGA)
“Based on the relationship we have with them; they can easily tell us without feeling embarrassed or shy…. They know me, and I have been with them for a long time.”—Community mobilizer (Rural LGA)
“The attitude needs to be improved so that we can be more receptive to these people”—MOH/PHC Coordinator (Urban LGA)
“We make sure things are friendly and simplified in order to make sure they are not scared…”—NTD Officer (Urban LGA)
Stage 5.1. Consultation
“When the patients are brought to the clinic, we ask about the complaints, we find out if the child bathes near wells and rivers and they say yes....”—Community mobilizer (Rural LGA)
“In Ibadan (city), for instance, there is a location called Dandaaru. It is around University College Hospital. People live around that community and their children go there to bath. In the process, they get infected with schistosomiasis.”—Public health researcher
“if a patient comes with a case of blood in their urine and if the health worker does not have adequate knowledge to say that it is similar to schistosomiasis, there is no way the patient can take a step further to investigate… There may be misdiagnosis and some cases may be entirely missed. Some may have the disease and assume that it is a sexually transmitted infections…Training of the health workers to build their skills to detect schistosomiasis is very important.”—MOH/PHC Coordinator (Urban LGA)
“I’m not sure maybe 5 or 9 of them had a microscopic (haematuria) and not the haematuria… it wasn’t like they came with symptoms.”—Public health researcher
Stage 5.2. Diagnosis
“You must carry out urinalysis with at least simple microscopy. It is very important to know what you are dealing with and to rule out certain thing…”—MOH/PHC (Urban LGA)
“Diagnosis is very important because, without it, no treatment can be made.”—PHC Coordinator (Rural LGA)
“Now a patient comes to the laboratory and the physician has requested a urinalysis, for a urine analysis and a urine microscopy”—Lab scientist (Urban LGA)
“There is no machine (microscope). We do have labs, but we are limited to some tests to be carried out at the LGA level.”—NTD Officer (Rural LGA)
“But at times, when we don’t have equipment, we call our boss and ask to either to refer the patient or if he is on his way down, if he is, he would bring the equipment needed from Moniya by his bike…”—CHEW (Rural LGA)
“there is currently no power supply. We have an old generator and there is no money…”—Lab scientist (Urban LGA)
“… Then manpower should be on ground. Scientists, more scientists should be on ground so that the work won’t be too much on individuals…”—Lab scientist at PHC (Urban LGA)
“She is a laboratory technician, not a full scientist. She is just a technician…”When asked about the lab personnel at the PHC– Head of PHC (Urban LGA)
“the skill of their laboratory technician is not good enough to pick that, then you might miss even if there are 100 cases in that community…”—Public Health Researcher
“our people are still poor, if test is expensive they will say they will come back…. She told me she didn’t have enough money on her for the test that she had only five hundred naira…”—Guardian of child who had schistosomiasis II (Urban LGA)
Stage 5.3. Symptom-Based Diagnosis and Treatment
“We combine the signs and symptoms with the patient history of the patient… We treated them clinically as we did not have any laboratory to confirm it.”—Community Mobilizer (Rural LGA)
“Even on clinical level, such a diagnosis can be missed…So, when you have this patient and you do not use your initiative to conclude that you have to conduct urinalysis with microscopy on this patient, it is possible to miss the diagnosis…”—MOH/PHC Coordinator (Urban LGA)
Stage 5.4. Treatment and Follow-Up
“After everything, my boss told me they got drugs and that it was schistosomiasis. However, I did not see the laboratory results.”—CHEW (Rural LGA)
“If you ask the patient to go home without giving them anything, they will not come back to you. This is why you have to reassure and give them something without the case being confirmed”—PHC Coordinator (Rural LGA)
“after that they will tell them to take their drugs properly, they will also tell them to do check-up either the following or after two days…”—Guardian of a child who had schistosomiasis II (Urban LGA)
3.1.6. Stage 6: Reach the Referral and Receive Appropriate Care
“Even transportation is a cause for concern. They want immediate attention and asking them to go to another hospital is like adding salt to their journey…”—Community mobilizer/CHO (Rural LGA)
“Even if free drugs are available at the hospital, they have to think of the transport fare from their house to the hospital.”—PHC Coordinator (Rural LGA)
“We have heard of cases of people with phobias for health center that close their eyes when they walk pass by the facility”—NTD officer (Urban LGA)
“I said fear and shyness, fear that they will be admitted (to hospital) and may not be allowed to come go back home…”—Guardian of child who had schistosomiasis (Urban LGA)
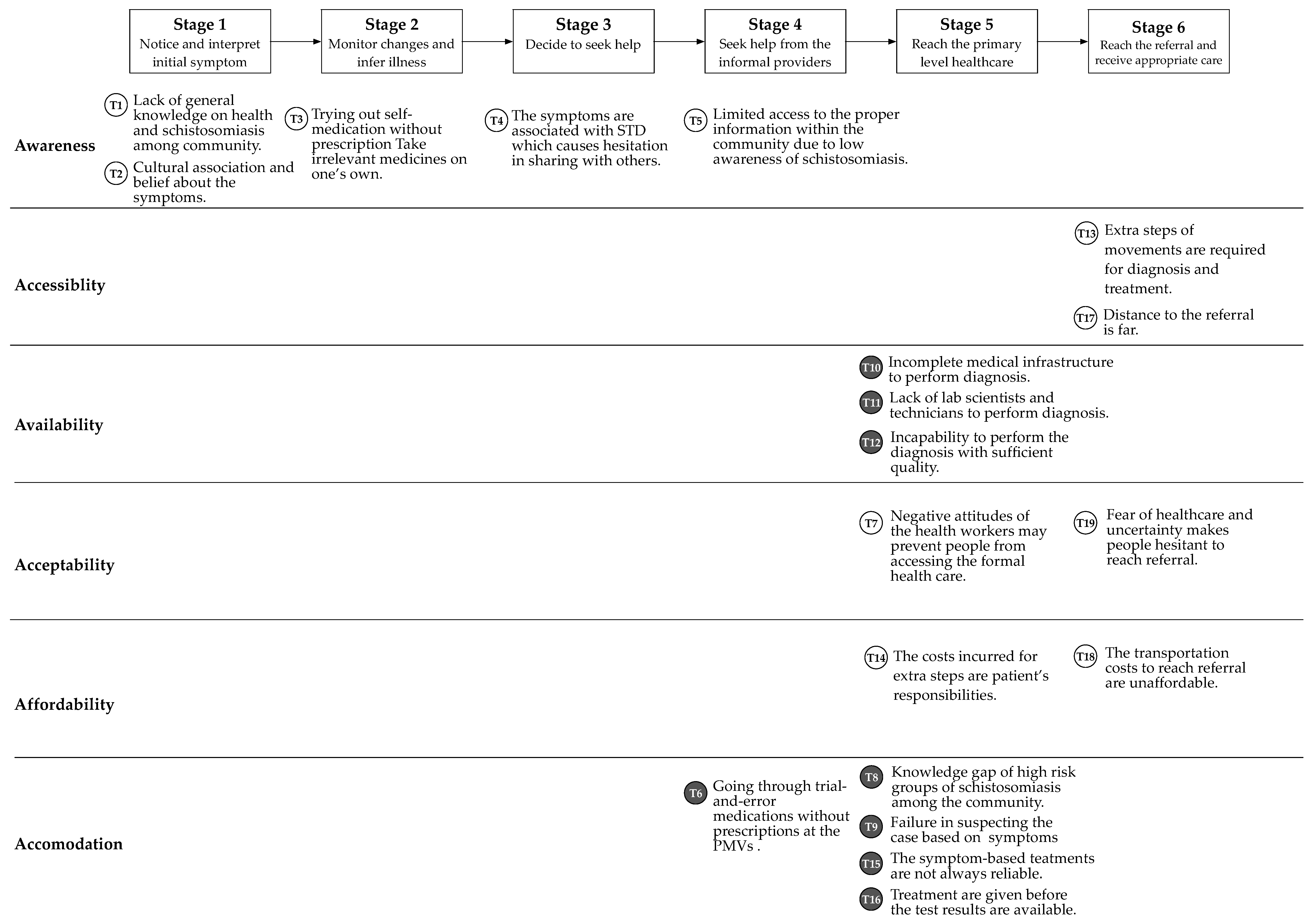
3.2. Barriers to the Case Management and Diagnosis
4. Discussion
4.1. Main Findings
4.2. Opportunities
4.2.1. Community Sensitization Program for Awareness Creation
4.2.2. A Study to Identify Prevalence of Schistosomiasis Among other High-Risk Groups
4.2.3. Enhancing the Existing Diagnostics Capacity
4.2.4. Implementation of Point-of-Care Diagnostics Solution
4.2.5. Community-Based Screening for Treatment and Monitoring
4.2.6. Capability Strengthening of the Health Workers
4.3. Limitations of the Study
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| 6A Dimension | Barriers Identified | HC Seeker | HC Provider |
|---|---|---|---|
| Awareness | T1: Lack of general knowledge on health and schistosomiasis among community (Stage 1) | ✓ 1 | |
| T2: Cultural association and belief about the symptoms (Stage 1) | ✓ | ||
| T3: Trying out self-medication without prescription Take irrelevant medicines on one’s own (Stage 2) | ✓ | ||
| T4: The symptoms are associated with STD which causes hesitation in sharing with others (Stage 3) | ✓ | ||
| T5: Limited access to the right information within the community due to low awareness of schistosomiasis (Stage 4) | ✓ | ||
| Accessibility | T13: Extra steps of movements are required for diagnosis and treatment. | ✓ | |
| T17: Distance to the referral is far (Stage 6) | ✓ | ||
| Availability | T10: Incomplete medical infrastructure to perform diagnosis (Stage 5) | ✓ | |
| T11: Lack of lab scientists and technicians to perform diagnosis (Stage 5) | ✓ | ||
| T12: Incapability to perform the diagnosis with sufficient quality (Stage 5) | ✓ | ||
| Acceptability | T7: Negative attitudes of the health workers may prevent people from accessing the formal health care (Stage 4) | ✓ | |
| T19: Fear of healthcare and uncertainty makes people hesitant to reach referral (Stage 5) | ✓ | ||
| Affordability | T14: The costs incurred for extra steps are patient’s responsibilities. | ✓ | |
| T18: The transportation costs to reach referral are unaffordable (Stage 6) | ✓ | ||
| Adequacy/Accommodation | T6: Going through trial-and-error medications without prescriptions at the PMVs (Stage 4) | ✓ | |
| T8: Knowledge gap of high risk groups of schistosomiasis among the community (Stage 5) | ✓ | ||
| T9: Failure in suspecting the case based on symptoms (Stage 5) | ✓ | ||
| T15: The symptom-based treatments are not always available (Stage 5) | ✓ | ||
| T18: Treatment are given before the test results are available. (Stage 5) | ✓ |
References
- Savioli, L.; Engels, D.; Roungou, J.B.; Fenwick, A.; Endo, H. Schistosomiasis control. Lancet 2004, 20, 363–658. [Google Scholar] [CrossRef]
- Ezeh, C.O.; Onyekwelu, K.C.; Akinwale, O.P.; Shan, L.; Wei, H. Urinary schistosomiasis in Nigeria: A 50 year review of prevalence, distribution and disease burden. Parasite 2019, 26, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- King, C.H. Parasites and poverty: The case of schistosomiasis. Acta Trop. 2010, 113, 95–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adenowo, A.F.; Oyinloye, B.E.; Ogunyinka, B.I.; Kappo, A.P. Impact of human schistosomiasis in sub-Saharan Africa. Braz. J. Infect. Dis. 2015, 19, 196–205. [Google Scholar] [CrossRef] [Green Version]
- Federal Ministry of Health. Report on Epidemiological Mapping of Schistosomiasis and Soil Transmitted Helminthiasis in 19 States and the FCT, Nigeria. 2015. Available online: www.health.gov.ng/doc/SchistoSTH.pdf (accessed on 1 April 2020).
- Mafe, M.A.; Von Stamm, T.; Utzinger, J.; N’goran, E.K. Control of urinary schistosomiasis: An investigation into the effective use of questionnaires to identify high-risk communities and individuals in Niger State, Nigeria. Trop. Med. Int. Health 2000, 5, 53–63. [Google Scholar] [CrossRef]
- Evans, D.S.; King, J.D.; Eigege, A.; Umaru, J.; Adamani, W.; Alphonsus, K.; Sambo, Y.; Miri, E.S.; Goshit, D.; Ogah, G.; et al. Assessing the WHO 50% prevalence threshold in school-aged children as indication for treatment of urogenital schistosomiasis in adults in central Nigeria. Am. J. Trop. Med. Hyg. 2013, 88, 441–445. [Google Scholar] [CrossRef] [Green Version]
- Mafe, M.A.; Appelt, B.; Adewale, B.; Idowu, E.T.; Akinwale, O.P.; Adeneye, A.K.; Manafa, O.U.; Sulyman, M.A.; Akande, O.D.; Omotola, B.D. Effectiveness of different approaches to mass delivery of praziquantel among school-aged children in rural communities in Nigeria. Acta Trop. 2005, 93, 181–190. [Google Scholar] [CrossRef]
- Bruun, B.; Aagaard-Hansen, J. The Social Context of Schistosomiasis and Its Control; World Health Organisation: Geneva, Switzerland, 2008; pp. 118–119.
- Hopkins, D.R.; Eigege, A.; Miri, E.S.; Gontor, I.; Ogah, G.; Umaru, J.; Gwomkudu, C.C.; Mathai, W.; Jinadu, M.Y.; Amadiegwu, S.; et al. Lymphatic filariasis elimination and schistosomiasis control in combination with onchocerciasis control in Nigeria. Am. J. Trop. Med. Hyg. 2002, 67, 266–272. [Google Scholar] [CrossRef] [Green Version]
- Richards, F.O., Jr.; Eigege, A.; Miri, E.S.; Jinadu, M.Y.; Hopkins, D.R. Integration of mass drug administration programmes in Nigeria: The challenge of schistosomiasis. Bull. World Health Organ. 2006, 84, 673–676. [Google Scholar] [CrossRef]
- N’Goran, E.K.; Utzinger, J.; N’guessan, A.N.; Müller, I.; Zamblé, K.; Lohourignon, K.L.; Traoré, M.; Sosthène, B.A.; Lengeler, C.; Tanner, M. Reinfection with Schistosoma haematobium following school-based chemotherapy with praziquantel in four highly endemic villages in Côte d’Ivoire. Trop. Med. Int. Health 2001, 6, 817–825. [Google Scholar] [CrossRef] [Green Version]
- Utzinger, J.; Raso, G.; Brooker, S.; De Savigny, D.; Tanner, M.; Ørnbjerg, N.; Singer, B.H.; N’goran, E.K. Schistosomiasis and neglected tropical diseases: Towards integrated and sustainable control and a word of caution. Parasitology 2009, 136, 1859–1874. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chiamah, O.C.; Ubachukwu, P.O.; Anorue, C.O.; Ebi, S. Urinary schistosomiasis in Ebonyi State, Nigeria from 2006 to 2017. J. Vector Borne Dis. 2019, 56, 87–91. [Google Scholar] [CrossRef] [PubMed]
- van der Werf, M. Schistosomiasis Morbidity and Management of Cases in Africa. Ph.D. Thesis, Erasmus University Rotterdam, Rotterdam, The Netherlands, 21 May 2003. [Google Scholar]
- World Health Organisation. The Control of Schistosomiasis; Technical Report Series; No. 728; World Health Organisation: Geneva, Switzerland, 1993. [Google Scholar]
- Utzinger, J.; Becker, S.L.; Van Lieshout, L.; Van Dam, G.J.; Knopp, S. New diagnostic tools in schistosomiasis. Clin. Microbiol. Infect. 2015, 21, 529–542. [Google Scholar] [CrossRef] [Green Version]
- Ajibola, O.; Gulumbe, B.H.; Eze, A.A.; Obishakin, E. Tools for detection of schistosomiasis in resource limited settings. Med. Sci. 2018, 6, 39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Urdea, M.; Penny, L.A.; Olmsted, S.S.; Giovanni, M.Y.; Kaspar, P.; Shepherd, A.; Wilson, P.; Dahl, C.A.; Buchsbaum, S.; Moeller, G.; et al. Requirements for high impact diagnostics in the developing world. Nature 2006, 444, 73–79. [Google Scholar] [CrossRef] [PubMed]
- De Vlas, S.J.; Danso-Appiah, A.; Van Der Werf, M.J.; Bosompem, K.M.; Habbema, J.D.F. Quantitative evaluation of integrated schistosomiasis control: The example of passive case finding in Ghana. Trop. Med. Int. Health 2004, 9, A16–A21. [Google Scholar] [CrossRef] [PubMed]
- van der Werf, M.J.; de Vlas, S.J.; Landouré, A.; Bosompem, K.M.; Habbema, J.D.F. Measuring schistosomiasis case management of the health services in Ghana and Mali. Trop. Med. Int. Health 2004, 9, 149–157. [Google Scholar] [CrossRef] [Green Version]
- Oyekale, A.S. Assessment of primary health care facilities’ service readiness in Nigeria. BMC Health Serv. Res. 2017, 17, 172. [Google Scholar] [CrossRef] [Green Version]
- Ehiri, J.E.; Oyo-Ita, A.E.; Anyanwu, E.C.; Meremikwu, M.M.; Ikpeme, M.B. Quality of child health services in primary health care facilities in south-east Nigeria. Child Care Health Dev. 2005, 31, 181–191. [Google Scholar] [CrossRef]
- Dawaki, S.; Al-Mekhlafi, H.M.; Ithoi, I.; Ibrahim, J.; Abdulsalam, A.M.; Ahmed, A.; Sady, H.; Nasr, N.A.; Atroosh, W.M. The menace of schistosomiasis in Nigeria: Knowledge, attitude, and practices regarding schistosomiasis among rural communities in Kano State. PLoS ONE 2015, 10, e0143667. [Google Scholar] [CrossRef]
- Tidi, S.K.; Jummai, A.T. Urinary schistosomiasis: Health seeking behaviour among residents of Kiri in Shelleng Local Government Area of Adamawa state. J. Environ. Toxicol. Publ. Health 2015, 1, 30–35. [Google Scholar]
- National Bureau of Statistics. 2017, Demographic Statistics Bulletin; National Bureau of Statistics: Abuja, Nigeria, 2018; p. 8.
- Kohler, R.E.; Gopal, S.; Miller, A.R.; Lee, C.N.; Reeve, B.B.; Weiner, B.J.; Wheeler, S.B. A framework for improving early detection of breast cancer in sub-Saharan Africa: A qualitative study of help-seeking behaviors among Malawian women. Patient Educ. Couns. 2017, 100, 167–173. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oladepo, O.; Salami, K.K.; Adeoye, B.W.; Oshiname, F.; Ofi, B.; Oladepo, M.; Ogunbemi, O.; Lawal, A.; Brieger, W.R.; Bloom, G.; et al. Malaria Treatment and Policy in Three Regions in Nigeria: The Role of Patent Medicine Vendors; Future Health Systems, 2007; pp. 1–29. [Google Scholar]
- Bloom, G.; Standing, H.; Lucas, H.; Bhuiya, A.; Oladepo, O.; Peters, D.H. Making health markets work better for poor people: The case of informal providers. Health Policy Plan. 2011, 26 (Suppl. 1), i45–i52. [Google Scholar] [CrossRef] [PubMed]
- Saurman, E. Improving access: Modifying Penchansky and Thomas’s theory of access. J. Health Serv. Res. Policy 2016, 21, 36–39. [Google Scholar] [CrossRef]
- Penchansky, R.; Thomas, J.W. The concept of access: Definition and relationship to consumer satisfaction. Med. Care 1981, 19, 127–140. [Google Scholar] [CrossRef]
- Iwamoto, R.; Santos, A.L.R.; Chavannes, N.; Reis, R.; Diehl, J.C. Considerations for an Access-Centered Design of the Fever Thermometer in Low-Resource Settings: A Literature Review. JMIR Hum. Factors 2017, 4, e3. [Google Scholar] [CrossRef]
| Stakeholder Categories | Respondents | LGA | |
|---|---|---|---|
| 1 | Community members who have experience with schistosomiasis | 6 Parents/Guardians of people who were treated for schistosomiasis | Ibadan North, Akinyele |
| 2 | Stakeholders within community that can impact on the patient decision to access care | 1 Traditional healer 1 Community leader 1 Patent Medicine Vendor (PMV) | 1 Ibadan North |
| 3 | Stakeholders in the formal health care | 2 Community Health worker 2 Community mobilizers 1 Doctor 5 Lab personnel | Ibadan North, Akinyele |
| 4 | Stakeholders within Local and State Government | 1 Medical Officer of Health/PHC Coordinator 2 Disease Surveillance Notification Officers (DSNO) 1 PHC Coordinator 2 LGA NTD Officer 1 State NTD Officer | Ibadan North, Akinyele |
| 5 | Stakeholders in academia | 3 Researchers | University of Ibadan |
| Dimensions | Component | Theme |
|---|---|---|
| Awareness | Communication and information | General health literacy Knowledge about symptoms, care and prevention |
| Accessibility | Location | Distribution of, and distance to, health care providers |
| Availability | Supply and demand | Incomplete medical infrastructure Lack of equipment Lack of health care professionals Lack of training for health care professionals |
| Acceptability | Consumer perception | Cultural belief and influence from the community |
| Affordability | Financial and incidental costs | Cost of treatment Cost of transport to health care provider |
| Adequacy (Accommodation) | Organisation | Mismatch between available information and awareness, knowledge, and education needs Lack of relevant and complete diagnostic information |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van, G.-Y.; Onasanya, A.; van Engelen, J.; Oladepo, O.; Diehl, J.C. Improving Access to Diagnostics for Schistosomiasis Case Management in Oyo State, Nigeria: Barriers and Opportunities. Diagnostics 2020, 10, 328. https://doi.org/10.3390/diagnostics10050328
Van G-Y, Onasanya A, van Engelen J, Oladepo O, Diehl JC. Improving Access to Diagnostics for Schistosomiasis Case Management in Oyo State, Nigeria: Barriers and Opportunities. Diagnostics. 2020; 10(5):328. https://doi.org/10.3390/diagnostics10050328
Chicago/Turabian StyleVan, G-Young, Adeola Onasanya, Jo van Engelen, Oladimeji Oladepo, and Jan Carel Diehl. 2020. "Improving Access to Diagnostics for Schistosomiasis Case Management in Oyo State, Nigeria: Barriers and Opportunities" Diagnostics 10, no. 5: 328. https://doi.org/10.3390/diagnostics10050328
APA StyleVan, G.-Y., Onasanya, A., van Engelen, J., Oladepo, O., & Diehl, J. C. (2020). Improving Access to Diagnostics for Schistosomiasis Case Management in Oyo State, Nigeria: Barriers and Opportunities. Diagnostics, 10(5), 328. https://doi.org/10.3390/diagnostics10050328