The Effects of Early Bispectral Index to Predict Poor Neurological Function in Cardiac Arrest Patients: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Index and Reference Tests
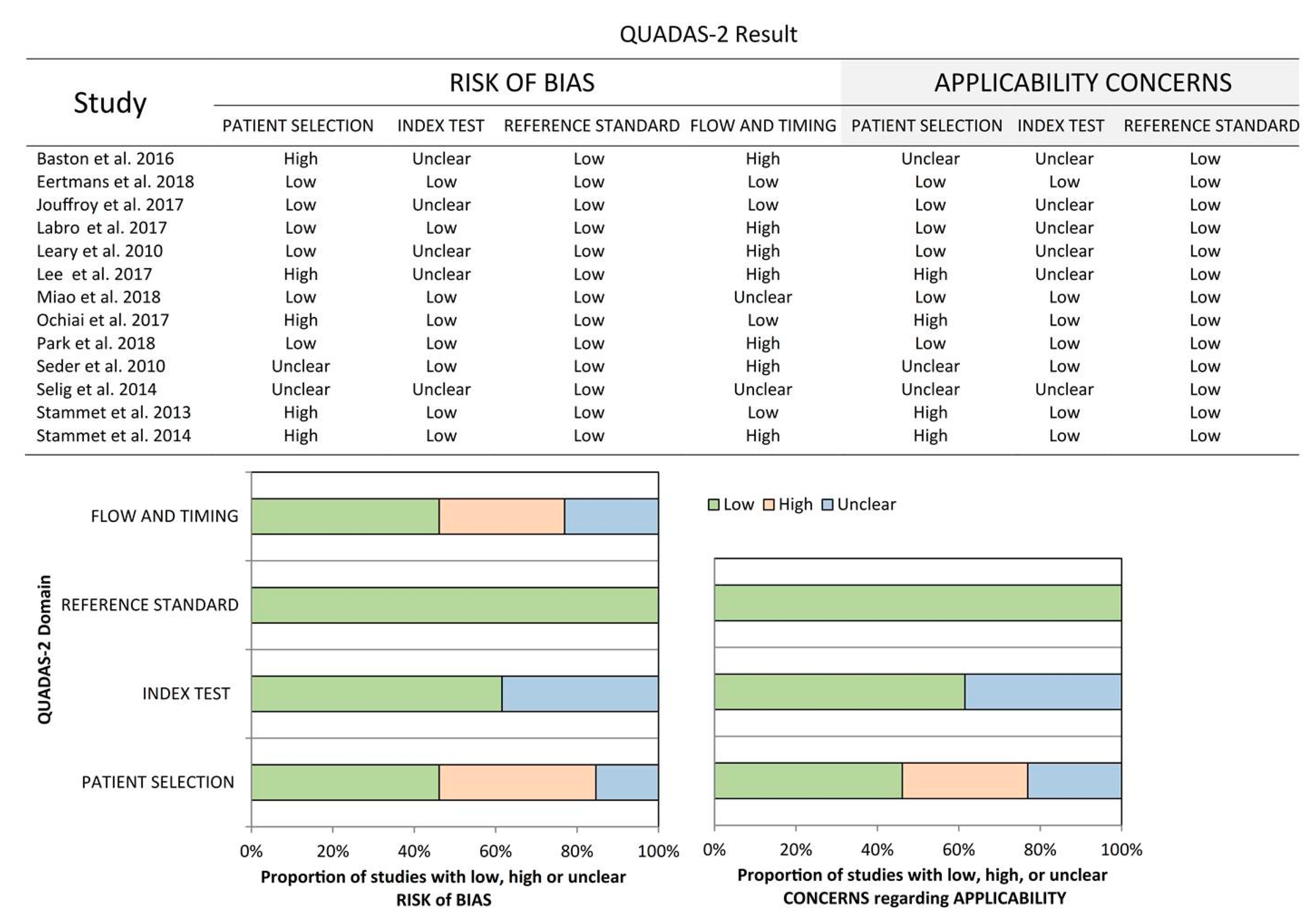
2.5. Risk of Bias in Individual Studies
2.6. Data Extraction
2.7. Statistical Analysis
3. Results
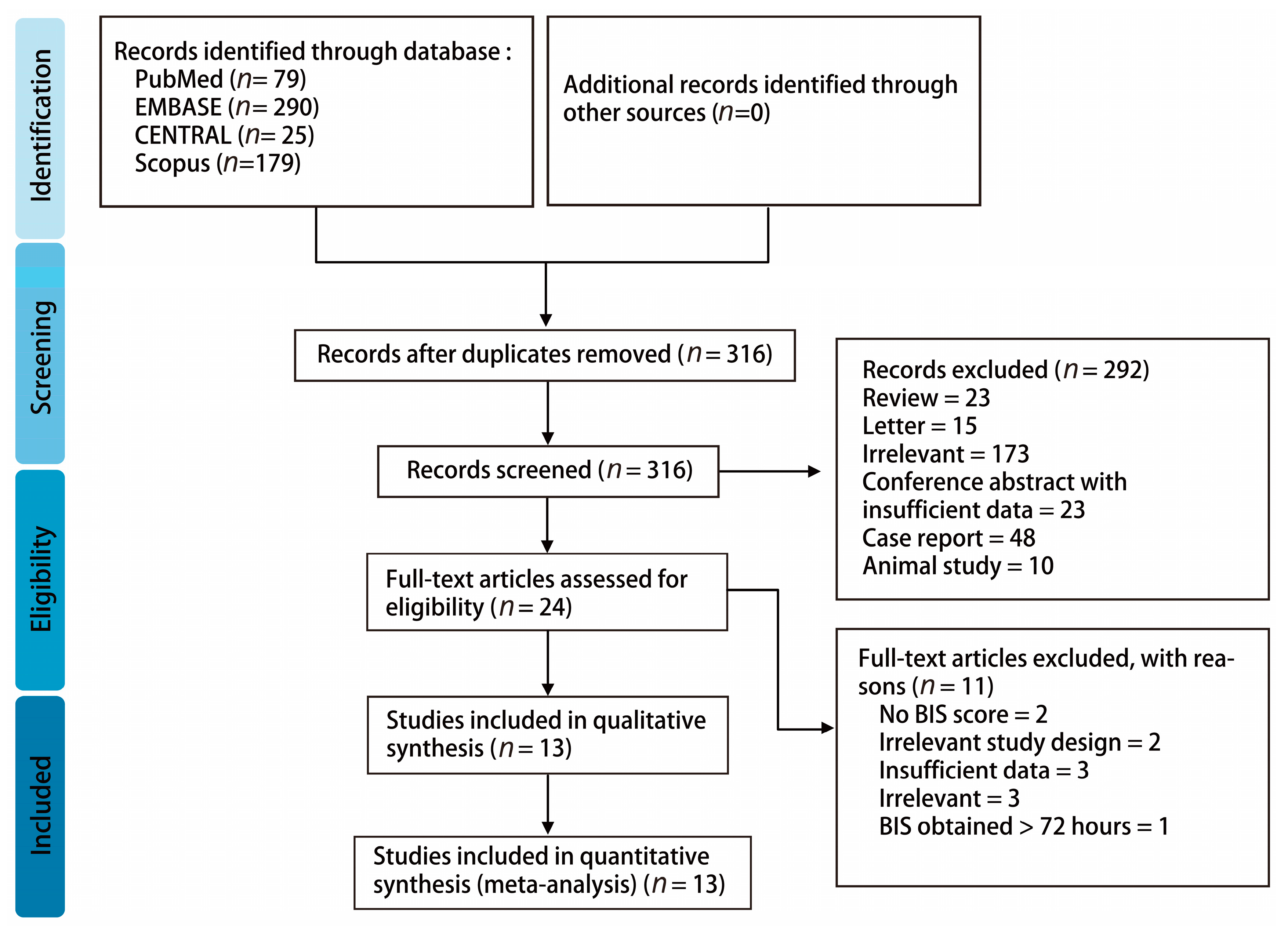
3.1. Study Identification and Selection
3.2. Study Characteristics
3.3. Overall Meta-Analysis of BIS for the Prediction of Poor Neurological Outcomes
3.3.1. Descriptive Data for the Included Studies
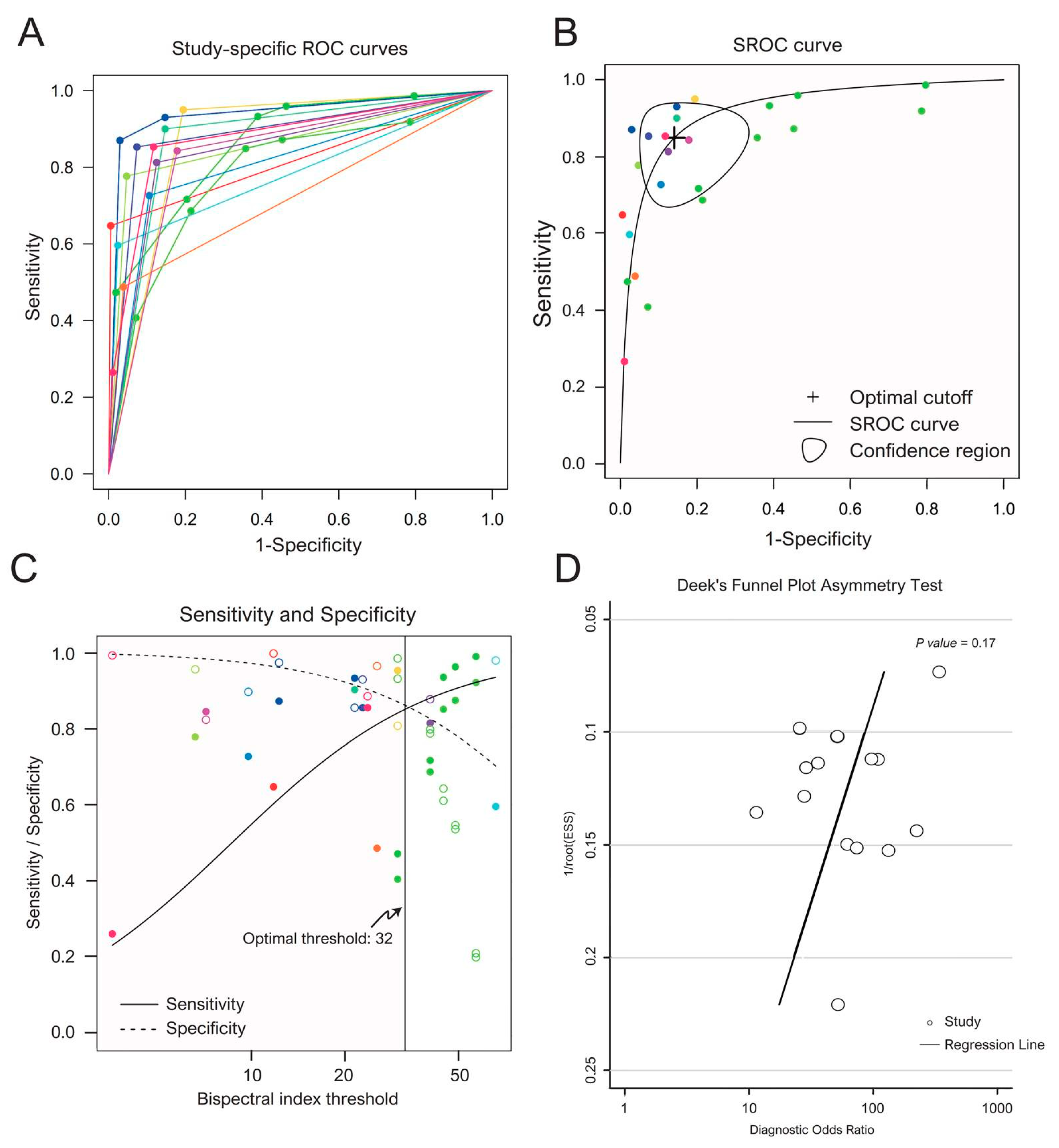
3.3.2. Pooled Sensitivity, Specificity and Optimal Threshold
3.4. Exploration of the Potential Sources of Heterogeneity
3.5. Publication Bias
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AHA | American Heart Association |
| AUC | Area under the curve |
| BIS | Bispectral index |
| CA | Cardiac arrest |
| CENTRAL | Cochrane Central Register of Controlled Trials |
| CPC | Cerebral Performance Category |
| CI | Confidence interval |
| EEG | Electroencephalography |
| EMS | Emergency medical services |
| ERC | European Resuscitation Council |
| ESICM | European Society of Intensive Care Medicine |
| GCS | Glasgow Coma Scale |
| ILCOR | International Liaison Committee on Resuscitation |
| NMBA | Neuromuscular blocking agents |
| OHCA | Out-of-hospital cardiac arrest |
| PRISMA-DTA | Preferred Reporting Items for a Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies |
| QUADAS-2 | Quality Assessment of Diagnostic Accuracy Studies-2 |
| REML | Restricted maximum likelihood |
| ROSC | Return of spontaneous circulation |
| SROC | Summary receiver operating characteristic |
| TTM | Targeted temperature management |
References
- Eckstein, M.; Stratton, S.J.; Chan, L.S. Cardiac Arrest Resuscitation Evaluation in Los Angeles: CARE-LA. Ann. Emerg. Med. 2005, 45, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Lombardi, G.; Gallagher, J.; Gennis, P. Outcome of out-of-hospital cardiac arrest in New York City. The Pre-Hospital Arrest Survival Evaluation (PHASE) Study. JAMA 1994, 271, 678–683. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart disease and stroke statistics—2018 update: A report from the American heart association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef] [PubMed]
- Roger, V.L.; Go, A.S.; Lloyd-Jones, D.M.; Benjamin, E.J.; Berry, J.D.; Borden, W.B.; Bravata, D.M.; Dai, S.; Ford, E.S.; Fox, C.S.; et al. Heart disease and stroke statistics—2012 update: A report from the American heart association. Circulation 2012, 125, e2–e220. [Google Scholar]
- Elmer, J.; Torres, C.; Aufderheide, T.P.; Austin, M.A.; Callaway, C.W.; Golan, E.; Herren, H.; Jasti, J.; Kudenchuk, P.J.; Scales, D.C.; et al. Association of early withdrawal of life-sustaining therapy for perceived neurological prognosis with mortality after cardiac arrest. Resuscitation 2016, 102, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart disease and stroke statistics—2019 update: A report from the American heart association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef]
- Wu, M.Y.; Yiang, G.T.; Liao, W.T.; Tsai, A.P.; Cheng, Y.L.; Cheng, P.W.; Li, C.Y.; Li, C.J. Current mechanistic concepts in ischemia and reperfusion injury. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2018, 46, 1650–1667. [Google Scholar] [CrossRef]
- Sandroni, C.; Nolan, J.P. Neuroprognostication after cardiac arrest in Europe: New timings and standards. Resuscitation 2015, 90, A4–A5. [Google Scholar] [CrossRef]
- Nolan, J.P.; Soar, J.; Cariou, A.; Cronberg, T.; Moulaert, V.R.; Deakin, C.D.; Bottiger, B.W.; Friberg, H.; Sunde, K.; Sandroni, C.; et al. European resuscitation council and European society of intensive care medicine 2015 guidelines for post-resuscitation care. Intensive Care Med. 2015, 41, 2039–2056. [Google Scholar] [CrossRef]
- Health Quality Ontario. Bispectral index monitor: An evidence-based analysis. Ont. Health Technol. Assess. Ser. 2004, 4, 1–70. [Google Scholar]
- Donaldson, M.; Goodchild, J.H. Use of bispectral index system (BIS) to monitor enteral conscious (moderate) sedation during general dental procedures. J. Can. Dent. Assoc. 2009, 75, 709. [Google Scholar] [PubMed]
- PRISMA-DTA Group; McInnes, M.D.F.; Moher, D.; Thombs, B.D.; McGrath, T.A.; Bossuyt, P.M.; Clifford, T.; Cohen, J.F.; Deeks, J.J.; Gatsonis, C.; et al. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: The PRISMA-DTA statement. JAMA 2018, 319, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Edgren, E.; Hedstrand, U.; Kelsey, S.; Sutton-Tyrrell, K.; Safar, P. Assessment of neurological prognosis in comatose survivors of cardiac arrest. BRCT I Study Group. Lancet 1994, 343, 1055–1059. [Google Scholar] [CrossRef]
- Perkins, G.D.; Jacobs, I.G.; Nadkarni, V.M.; Berg, R.A.; Bhanji, F.; Biarent, D.; Bossaert, L.L.; Brett, S.J.; Chamberlain, D.; de Caen, A.R.; et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: Update of the UTSTEIN resuscitation registry templates for out-of-hospital cardiac arrest: A statement for healthcare professionals from a task force of the international liaison committee on resuscitation (American heart association, European resuscitation council, Australian and New Zealand council on resuscitation, heart and stroke foundation of Canada, InterAmerican heart foundation, resuscitation council of Southern Africa, resuscitation council of Asia); and the American heart association emergency cardiovascular care committee and the council on cardiopulmonary, critical care, perioperative and resuscitation. Circulation 2015, 132, 1286–1300. [Google Scholar]
- Steinhauser, S.; Schumacher, M.; Rucker, G. Modelling multiple thresholds in meta-analysis of diagnostic test accuracy studies. BMC Med. Res. Methodol. 2016, 16, 97. [Google Scholar] [CrossRef]
- Reitsma, J.B.; Glas, A.S.; Rutjes, A.W.; Scholten, R.J.; Bossuyt, P.M.; Zwinderman, A.H. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J. Clin. Epidemiol. 2005, 58, 982–990. [Google Scholar] [CrossRef]
- Riley, R.D.; Ahmed, I.; Ensor, J.; Takwoingi, Y.; Kirkham, A.; Morris, R.K.; Noordzij, J.P.; Deeks, J.J. Meta-analysis of test accuracy studies: An exploratory method for investigating the impact of missing thresholds. Syst. Rev. 2015, 4, 12. [Google Scholar] [CrossRef]
- Macaskill, P.; Gatsonis, C.; Deeks, J.J.; Harbord, R.M.; Takwoingi, Y. Chapter 10: Analysing and presenting results. In Cochrane Handbook for Systematic Reviews of Diagnostic Test Accuracy, version 1.0.; Deeks, J.J., Bossuyt, P.M., Gatsonis, C., Eds.; The Cochrane Collaboration: London, UK, 2010; Available online: http://srdta.cochrane.org/ (accessed on 25 October 2019).
- Khot, S.; Tirschwell, D.L. Long-term neurological complications after hypoxic-ischemic encephalopathy. Semin. Neurol. 2006, 26, 422–431. [Google Scholar] [CrossRef]
- Deeks, J.J.; Macaskill, P.; Irwig, L. The performance of tests of publication bias and other sample size effects in systematic reviews of diagnostic test accuracy was assessed. J. Clin. Epidemiol. 2005, 58, 882–893. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria. Available online: https://www.R-project.org/ (accessed on 25 October 2019).
- Gerta Rucker, S.S.; Kolampally, S.; Schwarzer, G. Diagmeta: Meta-Analysis of Diagnostic Accuracy Studies with Several Cutpoints. R package version 0.3–1. 2019. Available online: https://CRAN.R-project.org/ package=diagmeta (accessed on 25 October 2019).
- Doebler, P. Meta-Analysis of Diagnostic Accuracy. Available online: https://CRAN.R-project.org/ package=mada (accessed on 25 October 2019).
- Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- Jouffroy, R.; Lamhaut, L.; Guyard, A.; Philippe, P.; An, K.; Spaulding, C.; Baud, F.; Carli, P.; Vivien, B. Early detection of brain death using the Bispectral Index (BIS) in patients treated by extracorporeal cardiopulmonary resuscitation (E-CPR) for refractory cardiac arrest. Resuscitation 2017, 120, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Seder, D.B.; Fraser, G.L.; Robbins, T.; Libby, L.; Riker, R.R. The bispectral index and suppression ratio are very early predictors of neurological outcome during therapeutic hypothermia after cardiac arrest. Intensive Care Med. 2010, 36, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Oh, J.H.; Choi, S.P.; Wee, J.H. Neurologic outcome after out-of-hospital cardiac arrest could be predicted with the help of bispectral-index during early targeted temperature management. Scand. J. Trauma Resusc. Emerg. Med. 2018, 26, 59. [Google Scholar] [CrossRef] [PubMed]
- Eertmans, W.; Genbrugge, C.; Vander Laenen, M.; Boer, W.; Mesotten, D.; Dens, J.; Jans, F.; De Deyne, C. The prognostic value of bispectral index and suppression ratio monitoring after out-of-hospital cardiac arrest: A prospective observational study. Ann. Intensive Care 2018, 8, 34. [Google Scholar] [CrossRef] [PubMed]
- Miao, W.; Sun, Q.; Wang, H.; Li, H. The maximum value of bispectral index predicts outcome in hypoxic-ischemic encephalopathy after resuscitation, better than minimum or mean value. Brain Inj. 2018, 32, 1135–1141. [Google Scholar] [CrossRef]
- Leary, M.; Fried, D.A.; Gaieski, D.F.; Merchant, R.M.; Fuchs, B.D.; Kolansky, D.M.; Edelson, D.P.; Abella, B.S. Neurologic prognostication and bispectral index monitoring after resuscitation from cardiac arrest. Resuscitation 2010, 81, 1133–1137. [Google Scholar] [CrossRef]
- Labro, G.; Belon, F.; Luu, V.P.; Chenet, J.; Besch, G.; Puyraveau, M.; Piton, G.; Capellier, G. Evaluation of the prognostic value of the bispectral index (BIS) and suppression ratio (RS) among patients admitted to the ICU for cardiac arrest. Ann. Intensive Care 2017, 7, 2. [Google Scholar]
- Rial Baston, V.; Lopez De Sa, E.; Meras, P.; Irazusta, F.J.; Rosillo, S.; Monedero, M.C.; Armada, E.; Gonzalez, O.; Ponz, I.; Iniesta, A.M.; et al. Bispectral index: An early predictor of neurological outcomes in cardiac arrest survivors. Eur. Heart J. 2016, 37, 972. [Google Scholar]
- Stammet, P.; Collignon, O.; Werer, C.; Sertznig, C.; Devaux, Y. Bispectral index to predict neurological outcome early after cardiac arrest. Resuscitation 2014, 85, 1674–1680. [Google Scholar] [CrossRef]
- Stammet, P.; Wagner, D.R.; Gilson, G.; Devaux, Y. Modeling serum level of s100β and bispectral index to predict outcome after cardiac arrest. J. Am. Coll. Cardiol. 2013, 62, 851–858. [Google Scholar] [CrossRef]
- Lee, S.B.; Wee, J.H.; Choi, S.P.; Park, J.H. Bispectral index in early target temperature management could be a good predictor of unfavourable neurological outcome after cardiac arrest. Circulation 2017, 136, A12405. [Google Scholar]
- Ochiai, K.; Shiraishi, A.; Otomo, Y.; Koido, Y.; Kanemura, T.; Honma, M. Increasing or fluctuating bispectral index values during post-resuscitation targeted temperature management can predict clinical seizures after rewarming. Resuscitation 2017, 114, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Selig, C.; Riegger, C.; Dirks, B.; Pawlik, M.; Seyfried, T.; Klingler, W. Bispectral index (BIS) and suppression ratio (SR) as an early predictor of unfavourable neurological outcome after cardiac arrest. Resuscitation 2014, 85, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Sandroni, C.; Cariou, A.; Cavallaro, F.; Cronberg, T.; Friberg, H.; Hoedemaekers, C.; Horn, J.; Nolan, J.P.; Rossetti, A.O.; Soar, J. Prognostication in comatose survivors of cardiac arrest: An advisory statement from the European resuscitation council and the European society of intensive care medicine. Intensive Care Med. 2014, 40, 1816–1831. [Google Scholar] [CrossRef] [PubMed]
- Wijdicks, E.F.; Young, G.B. Myoclonus status in comatose patients after cardiac arrest. Lancet 1994, 343, 1642–1643. [Google Scholar] [CrossRef]
- Jorgensen, E.O.; Holm, S. The natural course of neurological recovery following cardiopulmonary resuscitation. Resuscitation 1998, 36, 111–122. [Google Scholar] [CrossRef]
- Callaway, C.W.; Donnino, M.W.; Fink, E.L.; Geocadin, R.G.; Golan, E.; Kern, K.B.; Leary, M.; Meurer, W.J.; Peberdy, M.A.; Thompson, T.M.; et al. Part 8: Post-cardiac arrest care: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015, 132, S465–S482. [Google Scholar] [CrossRef]
- Yee, T.; Gronner, A.; Knight, R.T. CT findings of hypoxic basal ganglia damage. South Med. J. 1994, 87, 624–626. [Google Scholar] [CrossRef]
- Pfeifer, R.; Borner, A.; Krack, A.; Sigusch, H.H.; Surber, R.; Figulla, H.R. Outcome after cardiac arrest: Predictive values and limitations of the neuroproteins neuron-specific enolase and protein S-100 and the Glasgow Coma Scale. Resuscitation 2005, 65, 49–55. [Google Scholar] [CrossRef]

| Study | Country | Design | Population | Therapeutic Hypothermia | BIS Initiation | Age † | Male (%) | Outcome | Timing | Threshold | N | TP | FP | FN | TN |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jouffroy et al., 2017 [25] | France | Prospective cohort | Refractory OHCA | 32–34 °C during the first 12–24 h | During TTM in the first 12–24 h | 52.0(13.0) | 30(65.2) | CPC 5 | Day 28 | 30 | 46 | 28 | 3 | 1 | 14 |
| Selig et al., 2014 [37] | Germany | Not mentioned | OHCA, IHCA | Mild hypothermia was induced for 12–24 h in 47.5% of the patients with ROSC | On average 37.0 min after the initiation of CPR | 69 (21–91) ‡ | 58(73.4) | CPC 3–5 | Day 3, 7 and 1 month | 40 | 26 | 6 | 2 | 1 | 17 |
| Seder et al., 2010 [26] | USA | Prospective cohort | Patients with HIE within 12 h of ROSC after CA | Targeted bladder temperature of 33 °C for 18–24 h | After the first dose of NMBA (median 84 (45–166) minutes after TH) | 62(48–72) § | 54(65.0) | CPC 3–5 | At hospital discharge | 22 | 83 | 43 | 2 | 7 | 31 |
| Park et al., 2018 [27] | South Korea | Prospective cohort | OHCA | Core temperature of 32–34 °C for 24 h, followed by an increase of 0.25 °C/hour to 36.5 °C | Average time from ROSC to the first significant BIS value = 2.3 ± 1.0 h | 55.6(16.8) | 49(75.4) | CPC 3–5 | 6 months | 10.5 | 65 | 43 | 0 | 6 | 16 |
| CPC 3–5 Φ | 6 months | 20.5 | 65 | 46 Φ | 2 Φ | 3 Φ | 14 Φ | ||||||||
| Eertmans et al., 2018 [28] | Belgium | Prospective cohort | OHCA | TTM at 33 °C for 24 h followed by rewarming for 12 h (0.3 °C/hour) | Continuous monitoring for 36 h during hypothermia and rewarming phase | Good outcome: 67.0(13.0) Poor outcome: 61.0(13.0) | Good outcome: 31(81.6) Poor outcome: 31(79.5) | CPC 3–5 | Day 180 | 25 | 77 | 19 | 1 | 20 | 37 |
| Miao et al., 2018 [29] | China | Prospective cohort | Patients resuscitated from CA | Not mentioned | On admission to the ICU, continuous monitoring for 12 h | 65.0 (20.0) | 27(60.0) | CPC 5* | Day 60 | 71.5 | 45 | 15 * | 0 * | 10 * | 20 * |
| Lee et al., 2017 [35] | South Korea | Retrospective cohort | CA | TTM | As soon as TTM started in CA patients | Not mentioned | Not mentioned | CPC 3–5 | 6 months | 20.5 | 50 | 31 | 2 | 3 | 14 |
| Leary et al., 2010 – A [30] | USA | Prospective cohort | Patients who achieved ROSC after resuscitation from OHCA and IHCA | Temperature of 32–34 °C for 24 h | Immediately after resuscitation | 55.0(16.0) | 36(58.1) | CPC 3–5 Φ | At hospital discharge | 30 | 62 | 17 Φ | 1 Φ | 25 Φ | 19 Φ |
| CPC 3–5 Φ | At hospital discharge | 40 | 62 | 29 Φ | 4 Φ | 13 Φ | 16 Φ | ||||||||
| CPC 3–5 Φ | At hospital discharge | 45 | 62 | 36 Φ | 7 Φ | 6 Φ | 13 Φ | ||||||||
| CPC 3–5 Φ | At hospital discharge | 50 | 62 | 37 Φ | 9 Φ | 5 Φ | 11 Φ | ||||||||
| CPC 3–5 Φ | At hospital discharge | 60 | 62 | 39 Φ | 16 Φ | 3 Φ | 4 Φ | ||||||||
| Leary et al., 2010 – B [30] | USA | Prospective cohort | Patients who achieved ROSC after resuscitation from OHCA and IHCA | Temperature of 32–34 °C for 24 h | Immediately after resuscitation | 55.0(16.0) | 36(58.1) | CPC 5 * | At hospital discharge | 30 | 62 | 17 * | 0 * | 19 * | 26 * |
| CPC 5 * | At hospital discharge | 40 | 62 | 26 * | 5 * | 10 * | 21 * | ||||||||
| CPC 5 * | At hospital discharge | 45 | 62 | 34 * | 10 * | 2 * | 16 * | ||||||||
| CPC 5 * | At hospital discharge | 50 | 62 | 35 * | 12 * | 1 * | 14 * | ||||||||
| CPC 5 * | At hospital discharge | 60 | 62 | 36 * | 21 * | 0 * | 5 * | ||||||||
| Labro et al., 2017 [31] | France | Prospective cohort | Patients admitted to the ICU for CA | Not mentioned | Mean duration from ROSC to BIS measurement = 5.7 ± 3.0 h | 57.6(16.8) | 61(70.9) | CPC 3–5 | 3 months | 5 | 86 | 43 | 1 | 12 | 30 |
| Ochiai et al., 2017 [36] | Japan | Retrospective cohort | Consecutive adult patients with OHCA or IHCA | The target temperature (33 or 34 °C), the period of maintaining this temperature (24 or 48 h), and rewarming times (12–48 h) varied depending on the era of patient treatment. | Recorded at intervals not exceeding 2 h between the time of target temperature achievement and completion of rewarming | Patients without clinical seizure: 59(47–68) § Patients with clinical seizure: 55(43–68) § | Patients without clinical seizure: 51(70.8) Patients with clinical seizure: 23(74.2) | CPC 3–5 | Day 30 | 68 | 103 | 38 | 5 | 14 | 46 |
| Baston et al., 2016 [32] | Spain | Prospective cohort | Successfully resuscitated patients who were unconscious at arrival | TH for 24 h | Started after TH, continuously monitor for 48 h | 73.8 | 140(75.2) | CPC 3–5 | At hospital discharge | 10 | 185 | 61 | 0 | 33 | 91 |
| Stammet et al., 2014 [33] | Luxembourg | Prospective cohort | All successfully resuscitated adult CA patients | Induced hypothermia at 33 °C for 24 h | Started after hypothermia and throughout the 24 h period | Good outcome: 57(21–81) ‡ Poor outcome: 67(24–83) ‡ | Good outcome: 42(91%) Poor outcome: 36(72%) | CPC 3–5 | 6 months | 23 | 96 | 43 | 5 | 7 | 41 |
| CPC 3–5 | 6 months | 2.4 | 96 | 13 | 0 | 37 | 46 | ||||||||
| Stammet et al., 2013 [34] | Luxembourg | Prospective cohort | CA patients admitted to the general ICU of the hospital | Patients were treated with hypothermia at 33 °C for 24 h after successful resuscitation | After admission to the ICU, monitor for 48 h | Good outcome: 61(29–82) ‡ Poor outcome: 69(38–83) ‡ | Good outcome: 34(82.9) Poor outcome: 23(67.6) | CPC 3–5 | 6 months | 5.5 | 75 | 29 | 7 | 5 | 34 |
| Covariate | Sensitivity (95% CI) | p Value † | Specificity (95% CI) | p Value ‡ | p Value § |
|---|---|---|---|---|---|
| CA type | 0.84 | ||||
| OHCA | 78.5% (58.1–90.6%) | <0.01 | 91.4% (72.7–97.7%) | <0.01 | |
| Mixed | 81.2% (72.5–87.6%) | <0.01 | 87.2% (78.5–92.8%) | <0.01 | |
| Outcome | 0.65 | ||||
| CPC 3–5 | 79.3% (70.5–86.0%) | <0.01 | 89.2% (81.5–93.9%) | <0.01 | |
| CPC 5 | 84.7% (66.3–94.0%) | <0.01 | 82.6% (58.7–94.1%) | <0.01 | |
| Timing | 0.37 | ||||
| < 30 days | 83.0% (72.4–90.1%) | <0.01 | 83.7% (71.2–91.5%) | <0.01 | |
| > 30 days | 77.9% (66.0–86.4%) | <0.01 | 91.6% (83.1–96.0%) | <0.01 | |
| TTM | 0.26 | ||||
| Yes | 82.2% (74.0–88.2%) | <0.01 | 86.1% (77.3–91.9%) | <0.01 | |
| No | 69.8% (43.7–87.3%) | 0.13 | 96.7% (82.4–99.5%) | <0.01 | |
| Sedation | 0.37 | ||||
| Yes | 80.7% (70.9–87.8%) | <0.01 | 86.2% (76.3–92.4%) | <0.01 | |
| No | 81.1% (66.8–90.1%) | <0.01 | 92.8% (81.2–97.5%) | <0.01 | |
| NMBA | 0.43 | ||||
| Yes | 82.1% (74.0–88.1%) | <0.01 | 86.2% (77.3–91.9%) | <0.01 | |
| No | 74.1% (52.5–88.1%) | 0.03 | 94.0% (80.0–98.4%) | <0.01 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, C.-Y.; Chen, C.-S.; Chien, Y.-J.; Lin, P.-C.; Wu, M.-Y. The Effects of Early Bispectral Index to Predict Poor Neurological Function in Cardiac Arrest Patients: A Systematic Review and Meta-Analysis. Diagnostics 2020, 10, 271. https://doi.org/10.3390/diagnostics10050271
Chang C-Y, Chen C-S, Chien Y-J, Lin P-C, Wu M-Y. The Effects of Early Bispectral Index to Predict Poor Neurological Function in Cardiac Arrest Patients: A Systematic Review and Meta-Analysis. Diagnostics. 2020; 10(5):271. https://doi.org/10.3390/diagnostics10050271
Chicago/Turabian StyleChang, Chun-Yu, Chien-Sheng Chen, Yung-Jiun Chien, Po-Chen Lin, and Meng-Yu Wu. 2020. "The Effects of Early Bispectral Index to Predict Poor Neurological Function in Cardiac Arrest Patients: A Systematic Review and Meta-Analysis" Diagnostics 10, no. 5: 271. https://doi.org/10.3390/diagnostics10050271
APA StyleChang, C.-Y., Chen, C.-S., Chien, Y.-J., Lin, P.-C., & Wu, M.-Y. (2020). The Effects of Early Bispectral Index to Predict Poor Neurological Function in Cardiac Arrest Patients: A Systematic Review and Meta-Analysis. Diagnostics, 10(5), 271. https://doi.org/10.3390/diagnostics10050271






