Tumor Multifocality is a Significant Risk Factor of Urinary Bladder Recurrence after Nephroureterectomy in Patients with Upper Tract Urothelial Carcinoma: A Single-Institutional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Description of Enrolled Subjects
2.2. Statistical Analysis
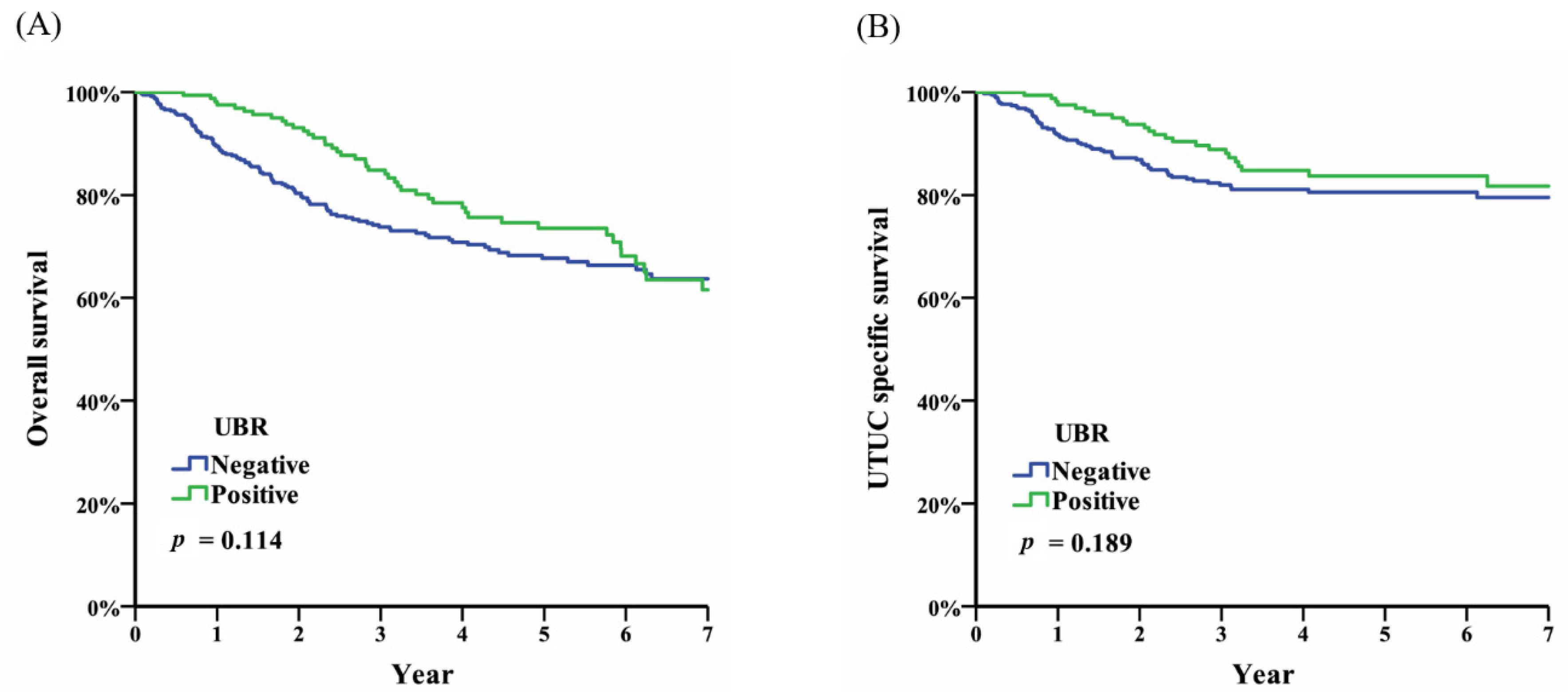
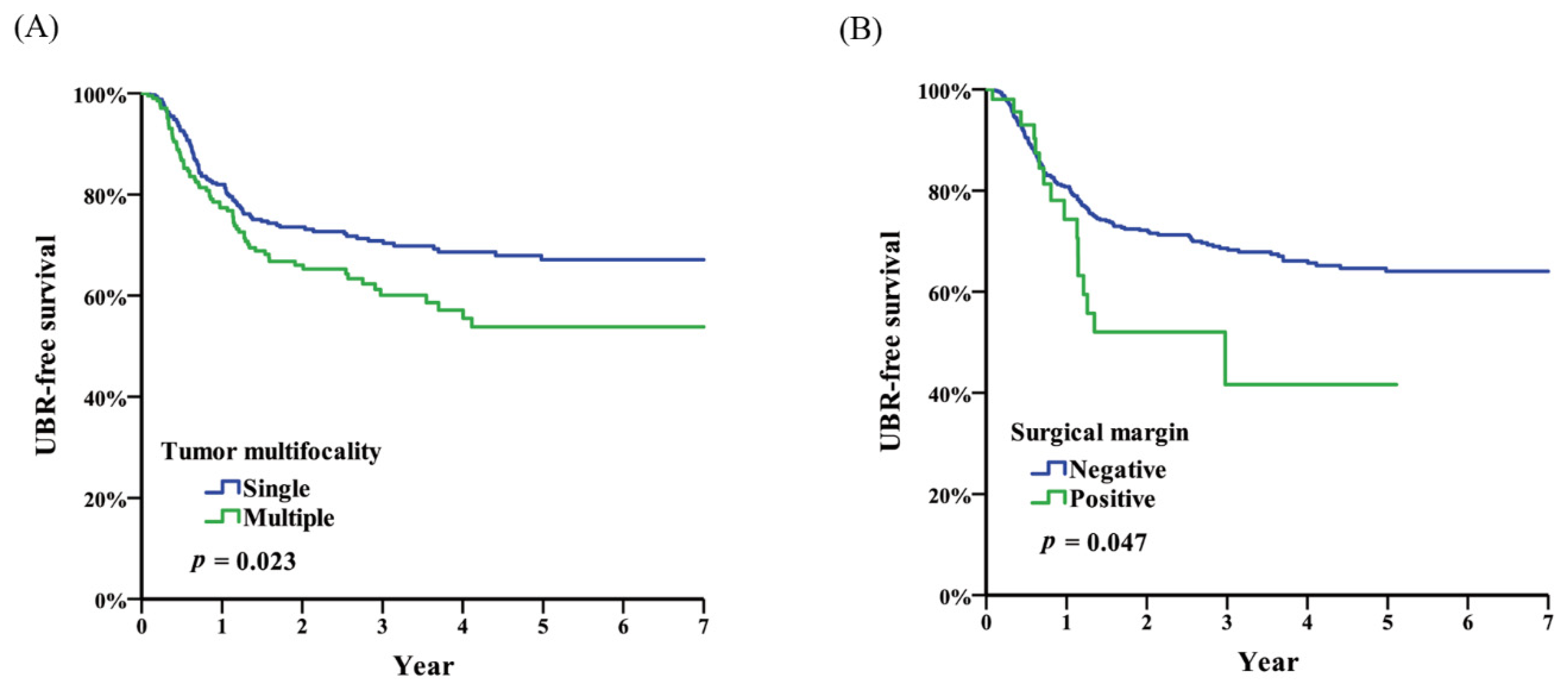
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Landis, S.H.; Murray, T.; Bolden, S.; Wingo, P.A. Cancer statistics, 1998. CA Cancer J. Clin. 1998, 48, 6–29. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.H.; Chen, K.K.; Yen, C.C.; Wang, W.S.; Chang, Y.H.; Huang, W.J.; Fan, F.S.; Chiou, T.J.; Liu, J.H.; Chen, P.M. Unusually high incidence of upper urinary tract urothelial carcinoma in taiwan. Urology 2002, 59, 681–687. [Google Scholar] [CrossRef]
- Ozsahin, M.; Zouhair, A.; Villa, S.; Storme, G.; Chauvet, B.; Taussky, D.; Gouders, D.; Ries, G.; Bontemps, P.; Coucke, P.A.; et al. Prognostic factors in urothelial renal pelvis and ureter tumours: A multicentre rare cancer network study. Eur. J. Cancer 1999, 35, 738–743. [Google Scholar] [CrossRef]
- Li, C.C.; Chang, T.H.; Wu, W.J.; Ke, H.L.; Huang, S.P.; Tsai, P.C.; Chang, S.J.; Shen, J.T.; Chou, Y.H.; Huang, C.H. Significant predictive factors for prognosis of primary upper urinary tract cancer after radical nephroureterectomy in taiwanese patients. Eur. Urol. 2008, 54, 1127–1134. [Google Scholar] [CrossRef] [PubMed]
- Elalouf, V.; Xylinas, E.; Klap, J.; Pignot, G.; Delongchamps, N.B.; Saighi, D.; Peyromaure, M.; Flam, T.; Zerbib, M. Bladder recurrence after radical nephroureterectomy: Predictors and impact on oncological outcomes. Int. J. Urol.: Off. J. Jpn. Urol. Assoc. 2013, 20, 1078–1083. [Google Scholar] [CrossRef] [PubMed]
- Xylinas, E.; Colin, P.; Audenet, F.; Phe, V.; Cormier, L.; Cussenot, O.; Houlgatte, A.; Karsenty, G.; Bruyere, F.; Polguer, T.; et al. Intravesical recurrence after radical nephroureterectomy for upper tract urothelial carcinomas: Predictors and impact on subsequent oncological outcomes from a national multicenter study. World J. Urol. 2013, 31, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; You, D.; Jeong, I.G.; Hong, J.H.; Ahn, H.; Kim, C.S. Muscle-invasive bladder cancer developing after nephroureterectomy for upper urinary tract urothelial carcinoma. Urol. Oncol. 2013, 31, 1643–1649. [Google Scholar] [CrossRef] [PubMed]
- Fang, D.; Xiong, G.Y.; Li, X.S.; Chen, X.P.; Zhang, L.; Yao, L.; He, Z.S.; Zhou, L.Q. Pattern and risk factors of intravesical recurrence after nephroureterectomy for upper tract urothelial carcinoma: A large chinese center experience. J. Formos. Med Assoc. 2014, 113, 820–827. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hartmann, A.; Rosner, U.; Schlake, G.; Dietmaier, W.; Zaak, D.; Hofstaedter, F.; Knuechel, R. Clonality and genetic divergence in multifocal low-grade superficial urothelial carcinoma as determined by chromosome 9 and p53 deletion analysis. Lab. Investig. J. Tech. Methods Pathol. 2000, 80, 709–718. [Google Scholar] [CrossRef] [PubMed]
- Ito, A.; Shintaku, I.; Satoh, M.; Ioritani, N.; Tochigi, T.; Numata, I.; Namima, T.; Kambe, K.; Kyan, A.; Ueno, S.; et al. Intravesical seeding of upper urinary tract urothelial carcinoma cells during nephroureterectomy: An exploratory analysis from the thpmg trial. Jpn. J. Clin. Oncol. 2013, 43, 1139–1144. [Google Scholar] [CrossRef] [PubMed]
- Seisen, T.; Granger, B.; Colin, P.; Leon, P.; Utard, G.; Renard-Penna, R.; Comperat, E.; Mozer, P.; Cussenot, O.; Shariat, S.F.; et al. A systematic review and meta-analysis of clinicopathologic factors linked to intravesical recurrence after radical nephroureterectomy to treat upper tract urothelial carcinoma. Eur. Urol. 2015, 67, 1122–1133. [Google Scholar] [CrossRef] [PubMed]
- Hirano, D.; Okada, Y.; Nagane, Y.; Satoh, K.; Mochida, J.; Yamanaka, Y.; Hirakata, H.; Yamaguchi, K.; Kawata, N.; Takahashi, S.; et al. Intravesical recurrence after surgical management of urothelial carcinoma of the upper urinary tract. Urol. Int. 2012, 89, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, N.; Kikuchi, E.; Kanao, K.; Matsumoto, K.; Shirotake, S.; Kobayashi, H.; Miyazaki, Y.; Ide, H.; Obata, J.; Hoshino, K.; et al. The predictive value of positive urine cytology for outcomes following radical nephroureterectomy in patients with primary upper tract urothelial carcinoma: A multi-institutional study. Urol. Oncol. 2014, 32, 48.e19–48.e26. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Lu, J.; Hong, K.; Huang, Y.; Ma, L. Independent prognostic factors for initial intravesical recurrence after laparoscopic nephroureterectomy for upper urinary tract urothelial carcinoma. Urol. Oncol. 2014, 32, 146–152. [Google Scholar] [CrossRef] [PubMed]
- Krabbe, L.M.; Westerman, M.E.; Bagrodia, A.; Gayed, B.A.; Khalil, D.; Kapur, P.; Shariat, S.F.; Raj, G.V.; Sagalowsky, A.I.; Cadeddu, J.A.; et al. Surgical management of the distal ureter during radical nephroureterectomy is an independent predictor of oncological outcomes: Results of a current series and a review of the literature. Urol. Oncol. 2014, 32, 54.e19–54.e26. [Google Scholar] [CrossRef] [PubMed]
- Zou, L.; Zhang, L.; Zhang, H.; Jiang, H.; Ding, Q. Comparison of post-operative intravesical recurrence and oncological outcomes after open versus laparoscopic nephroureterectomy for upper urinary tract urothelial carcinoma. World J. Urol. 2014, 32, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Shigeta, K.; Kikuchi, E.; Hagiwara, M.; Ando, T.; Mizuno, R.; Abe, T.; Mikami, S.; Miyajima, A.; Nakagawa, K.; Oya, M. The conditional survival with time of intravesical recurrence of upper tract urothelial carcinoma. J. Urol. 2017, 198, 1278–1285. [Google Scholar] [CrossRef] [PubMed]
- Xylinas, E.; Rink, M.; Cha, E.K.; Clozel, T.; Lee, R.K.; Fajkovic, H.; Comploj, E.; Novara, G.; Margulis, V.; Raman, J.D.; et al. Impact of distal ureter management on oncologic outcomes following radical nephroureterectomy for upper tract urothelial carcinoma. Eur. Urol. 2014, 65, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Fang, D.; Li, X.S.; Xiong, G.Y.; Yao, L.; He, Z.S.; Zhou, L.Q. Prophylactic intravesical chemotherapy to prevent bladder tumors after nephroureterectomy for primary upper urinary tract urothelial carcinomas: A systematic review and meta-analysis. Urol. Int. 2013, 91, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Yoo, S.H.; Jeong, C.W.; Kwak, C.; Kim, H.H.; Choo, M.S.; Ku, J.H. Intravesical chemotherapy after radical nephroureterectomy for primary upper tract urothelial carcinoma: A systematic review and network meta-analysis. J. Clin. Med. 2019, 8, 1059. [Google Scholar] [CrossRef] [PubMed]
| Variables | N | % | Variables | N | % |
|---|---|---|---|---|---|
| Gender | Tumor location | ||||
| Male | 237 | (43.1%) | calyx | 129 | (23.5%) |
| Female | 313 | (56.9%) | renal pelvis | 338 | (61.5%) |
| Age | proximal ureter | 167 | (30.4%) | ||
| ≤65 | 220 | (40.0%) | middle ureter | 109 | (19.8%) |
| >65 | 330 | (60.0%) | distal ureter | 120 | (21.8%) |
| Performance status (ECOG) | Tumor multifocality | ||||
| 0 | 57 | (10.4%) | Single | 338 | (61.5%) |
| 1 | 384 | (69.8%) | Multiple | 212 | (38.5%) |
| 2 | 101 | (18.4%) | Surgical margin | ||
| 3 | 6 | (1.1%) | Negative | 497 | (90.4%) |
| 4 | 2 | (0.4%) | Positive | 53 | (9.6%) |
| Body mass index (BMI) | Pathological TNM stage | ||||
| <18.5 | 25 | (4.5%) | T1 N0 M0 | 259 | (47.1%) |
| 18.5–24 | 260 | (47.3%) | T2 N0 M0 | 78 | (14.2%) |
| 24–27 | 170 | (30.9%) | T3 N0 M0 | 145 | (26.4%) |
| ≥27 | 95 | (17.3%) | T4 N0 M0 | 12 | (2.2%) |
| Smoking status | Tany N1 M0 | 18 | (3.3%) | ||
| Never | 391 | (71.1%) | Tany N2/3 M0 | 16 | (2.9%) |
| Current | 76 | (13.8%) | Tany Nany M1 | 22 | (4.0%) |
| Former | 83 | (15.1%) | Tumor grade | ||
| Preoperative renal function (mg/dL) | G1 | 16 | (2.9%) | ||
| ≤1.4 | 310 | (56.4%) | G2 | 182 | (33.1%) |
| >1.4 | 240 | (43.6%) | G3 | 352 | (64.0%) |
| History of uremia | Concomitant CIS | ||||
| Negative | 478 | (86.9%) | Negative | 469 | (85.3%) |
| Positive | 72 | (13.1%) | Positive | 81 | (14.7%) |
| Renal transplantation (−) | 65 | (90.3%) | Lymphovascular invasion | ||
| Renal transplantation (+) | 7 | (9.7%) | Negative | 430 | (78.2%) |
| Side | Positive | 120 | (21.8%) | ||
| Right | 244 | (44.4%) | Recurrence | ||
| Left | 306 | (55.6%) | Local | ||
| Surgical modality | Negative | 506 | (92.0%) | ||
| Open | 116 | (21.1%) | Positive | 44 | (8.0%) |
| Laparoscopy | 417 | (75.8%) | UB | ||
| Retroperitoneoscopy | 17 | (3.1%) | Negative | 386 | (70.2%) |
| Positive | 164 | (29.8%) | |||
| Contralateral | |||||
| Negative | 520 | (94.5%) | |||
| Positive | 30 | (5.5%) |
| Univariate | Multivariate | |||||
| Hazard Ratio | (95%CI) | p | Hazard Ratio | (95%CI) | p | |
| Gender | ||||||
| Female | 1.00 | (Reference) | ||||
| Male | 1.22 | (0.90–1.66)1.66) | 0.203 | |||
| Age | ||||||
| ≤65 | 1.00 | (Reference) | ||||
| >65 | 0.99 | (0.72–1.35)1.35) | 0.941 | |||
| Performance status (ECOG) | ||||||
| 0 | 1.00 | (Reference) | ||||
| 1 | 1.53 | (0.88–2.65)2.65) | 0.134 | |||
| 2 | 1.17 | (0.61–2.26)2.26) | 0.639 | |||
| 3 | - | |||||
| 4 | - | |||||
| BMI | ||||||
| <18.5 | 1.00 | (Reference) | ||||
| 18.5–24 | 1.25 | (0.54–2.88)2.88) | 0.595 | |||
| 24–27 | 1.60 | (0.69–3.69)3.69) | 0.272 | |||
| ≥27 | 0.86 | (0.35–2.12)2.12) | 0.737 | |||
| Smoking status | ||||||
| Never | 1.00 | (Reference) | ||||
| Current | 1.20 | (0.78–1.83)1.83) | 0.408 | |||
| Former | 1.10 | (0.66–1.83)1.83) | 0.708 | |||
| Preoperative renal function (mg/dl) | ||||||
| ≤1.4 | 1.00 | (Reference) | ||||
| >1.4 | 1.25 | (0.92–1.70)1.70) | 0.157 | |||
| History of uremia | ||||||
| Negative | 1.00 | (Reference) | ||||
| Positive | 1.46 | (0.97–2.20)2.20) | 0.073 | |||
| Surgical modality | ||||||
| Open | 1.00 | (Reference) | ||||
| Laparoscopy | 1.00 | (0.68–1.46)1.46) | 0.987 | |||
| Retroperitoneoscopy | 1.17 | (0.49–2.80)2.80) | 0.722 | |||
| Tumor location | ||||||
| Without distal ureter tumor | 1.00 | (Reference) | ||||
| With distal ureter tumor | 1.37 | (0.97–1.95)1.95) | 0.078 | |||
| Tumor multifocality | ||||||
| Single | 1.00 | (Reference) | 1.00 | (Reference) | ||
| Multiple | 1.43 | (1.05–1.95) | 0.024 * | 1.40 | (1.02–1.91) | 0.037 * |
| Surgical margin | ||||||
| Negative | 1.00 | (Reference) | 1.00 | (Reference) | ||
| Positive | 1.68 | (1.00–2.83) | 0.049 * | 1.55 | (0.92–2.62) | 0.101 |
| Pathological TNM stage | ||||||
| T1 N0 M0 | 1.00 | (Reference) | ||||
| T2 N0 M0 | 0.98 | (0.63–1.52)1.52) | 0.938 | |||
| T3 N0 M0 | 0.88 | (0.61–1.27)1.27) | 0.498 | |||
| T4 N0 M0 | 0.78 | (0.11–5.60)5.60) | 0.803 | |||
| Tany N1 M0 | 0.76 | (0.28–2.06)2.06) | 0.586 | |||
| Tany N2/3 M0 | - | |||||
| Tany Nany M1 | 0.22 | (0.03–1.57) | 0.131 | |||
| Tumor grade | ||||||
| G1 | 1.00 | (Reference) | ||||
| G2 | 0.80 | (0.37–1.75)1.75) | 0.585 | |||
| G3 | 0.68 | (0.31–1.46)1.46) | 0.317 | |||
| Concomitant CIS | ||||||
| Negative | 1.00 | (Reference) | ||||
| Positive | 1.33 | (0.89–1.98)1.98) | 0.169 | |||
| Lymphovascular invasion | ||||||
| Negative | 1.00 | (Reference) | ||||
| Positive | 1.12 | (0.76–1.65)1.65) | 0.566 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.-S.; Li, J.-R.; Wang, S.-S.; Yang, C.-K.; Cheng, C.-L.; Yang, C.-R.; Ou, Y.-C.; Ho, H.-C.; Lin, C.-Y.; Hung, S.-C.; et al. Tumor Multifocality is a Significant Risk Factor of Urinary Bladder Recurrence after Nephroureterectomy in Patients with Upper Tract Urothelial Carcinoma: A Single-Institutional Study. Diagnostics 2020, 10, 201. https://doi.org/10.3390/diagnostics10040201
Chen C-S, Li J-R, Wang S-S, Yang C-K, Cheng C-L, Yang C-R, Ou Y-C, Ho H-C, Lin C-Y, Hung S-C, et al. Tumor Multifocality is a Significant Risk Factor of Urinary Bladder Recurrence after Nephroureterectomy in Patients with Upper Tract Urothelial Carcinoma: A Single-Institutional Study. Diagnostics. 2020; 10(4):201. https://doi.org/10.3390/diagnostics10040201
Chicago/Turabian StyleChen, Chuan-Shu, Jian-Ri Li, Shian-Shiang Wang, Cheng-Kuang Yang, Chen-Li Cheng, Chi-Rei Yang, Yen-Chuan Ou, Hao-Chung Ho, Chia-Yen Lin, Sheng-Chun Hung, and et al. 2020. "Tumor Multifocality is a Significant Risk Factor of Urinary Bladder Recurrence after Nephroureterectomy in Patients with Upper Tract Urothelial Carcinoma: A Single-Institutional Study" Diagnostics 10, no. 4: 201. https://doi.org/10.3390/diagnostics10040201
APA StyleChen, C.-S., Li, J.-R., Wang, S.-S., Yang, C.-K., Cheng, C.-L., Yang, C.-R., Ou, Y.-C., Ho, H.-C., Lin, C.-Y., Hung, S.-C., Chen, C.-C., Wang, S.-C., Chiu, K.-Y., & Yang, S.-F. (2020). Tumor Multifocality is a Significant Risk Factor of Urinary Bladder Recurrence after Nephroureterectomy in Patients with Upper Tract Urothelial Carcinoma: A Single-Institutional Study. Diagnostics, 10(4), 201. https://doi.org/10.3390/diagnostics10040201






