Stakeholders’ Perspectives for the Development of a Point-of-Care Diagnostics Curriculum in Rural Primary Clinics in South Africa—Nominal Group Technique
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.1.1. Study Participants
2.1.2. Sampling Strategy
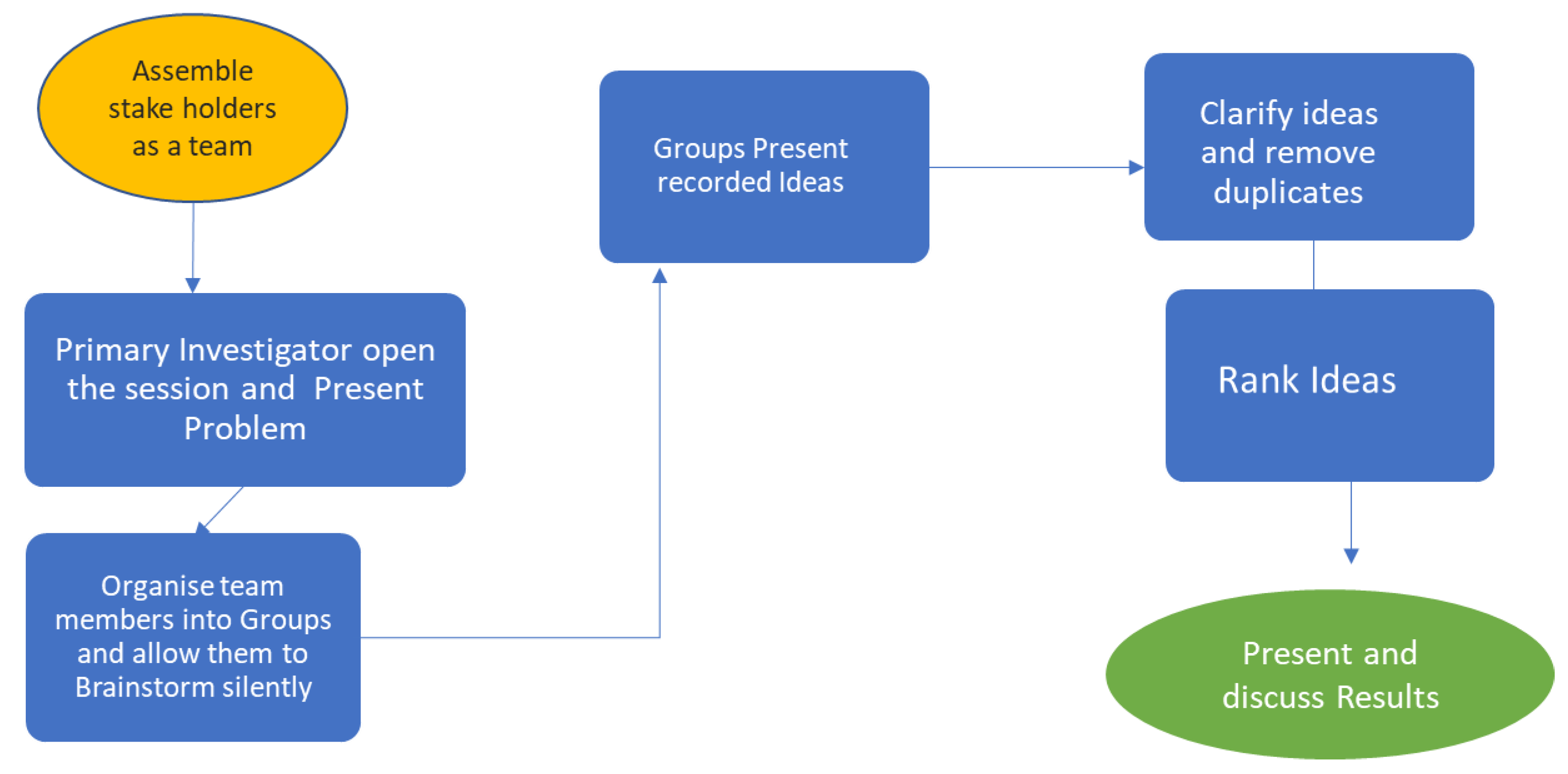
2.1.3. NGT Process
2.1.4. Silent Brainstorming
2.1.5. Group Discussion
2.1.6. Group Presentations and Clarification
2.1.7. Ranking of Ideas
2.1.8. Data Management
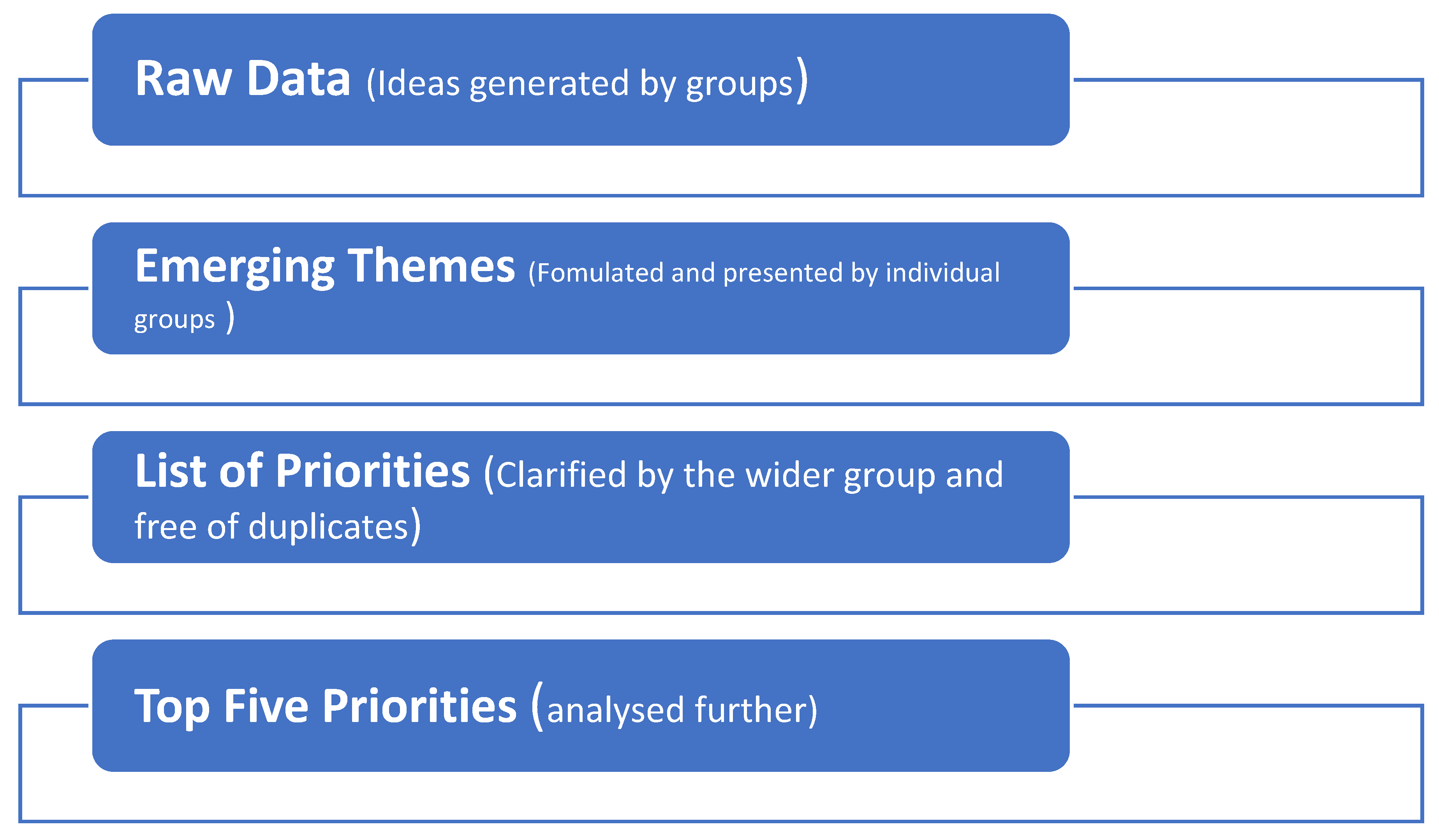
2.2. Data Analysis
2.2.1. Raw Data Analysis
2.2.2. Quantitative Data Analysis
2.2.3. Qualitative Data Analysis
3. Results
3.1. Characteristics of Study Participants
3.2. Nominal Group Ranking
3.3. Thematic Analysis of Top Five Priorities
3.3.1. Absence of POC Testing Curriculum for Nurses
3.3.2. Absence of Training of Staff on HIV Testing and Counselling as Lay Counsellors Are Being Phased Out
3.3.3. Absence of Continuous Professional Development
3.3.4. HPRS Tracking and Registering Patients before Testing: Correct Record Keeping
3.3.5. Lack of Staff Involvement in POC Management Programs
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
References
- Pai, N.P.; Vadnais, C.; Denkinger, C.; Engel, N.; Pai, M. Point-of-care testing for infectious diseases: Diversity, complexity and barriers in low-and middle-income countries. Plos Med. 2012, 9, e1001306. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.K.; Rutstein, S.E.; Powers, K.A.; Fidler, S.; Miller, W.C.; Eron, J.J., Jr.; Cohen, M.S. The detection and management of early HIV infection: A clinical and public health emergency. J. Acquir. Immune Defic. Syndr. (1999) 2013, 63, S187. [Google Scholar] [CrossRef] [PubMed]
- Jaya, Z.; Drain, P.K.; Mashamba-Thompson, T.P. Evaluating quality management systems for HIV rapid testing services in primary healthcare clinics in rural KwaZulu-Natal, South Africa. PLoS ONE 2017, 12, e0183044. [Google Scholar] [CrossRef] [PubMed]
- Mashamba-Thompson, T.; Jama, N.; Sartorius, B.; Drain, P.; Thompson, R. Implementation of point-of-care diagnostics in rural primary healthcare clinics in South Africa: Perspectives of key stakeholders. Diagnostics 2017, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Mashauri, F.; Siza, J.; Temu, M.; Mngara, J.; Kishamawe, C.; Changalucha, J. Assessment of quality assurance in HIV testing in health facilities in Lake Victoria zone, Tanzania. Tanzan. J. Health Res. 2007, 9, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.H.; Makumbi, F.; Serwadda, D.; Lutalo, T.; Nalugoda, F.; Opendi, P.; Kigozi, G.; Reynolds, S.J.; Sewankambo, N.K.; Wawer, M.J. Limitations of rapid HIV-1 tests during screening for trials in Uganda: Diagnostic test accuracy study. Bmj (Clin. Res. Ed.) 2007, 335, 188. [Google Scholar] [CrossRef] [PubMed]
- Munyewende, P.O.; Rispel, L.C. Using diaries to explore the work experiences of primary health care nursing managers in two South African provinces. Glob. Health Action 2014, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Nyambo, R.; Hizza, E.; Ntangeki, D. Increasing Accountability for the Reliability of Rapid HIV Test Results: Observations from Seven Facilities in Rungwe District Council, Tanzania. Available online: https://www.usaidassist.org/sites/default/files/assist_tanzania_rtqi_technical_report_mar2018_a4.pdf (accessed on 9 January 2020).
- FIND. Hiv Rapid Test Quality Improvement Initiative. 2016. Available online: https://www.finddx.org/wp-content/uploads/2016/12/RQTII_project.pdf (accessed on 9 January 2020).
- Delbecq, A.L.; Van de Ven, A.H. A group process model for problem identification and program planning. J. Appl. Behav. Sci. 1971, 7, 466–492. [Google Scholar] [CrossRef]
- Harvey, N.; Holmes, C.A. Nominal group technique: An effective method for obtaining group consensus. Int. J. Nurs. Pract. 2012, 18, 188–194. [Google Scholar] [CrossRef] [PubMed]
- McMillan, S.S.; Kelly, F.; Sav, A.; Kendall, E.; King, M.A.; Whitty, J.A.; Wheeler, A.J. Using the Nominal Group Technique: How to analyse across multiple groups. Health Serv. Outcomes Res. Methodol. 2014, 14, 92–108. [Google Scholar] [CrossRef]
- Mashamba-Thompson, T.; Sartorius, B.; Drain, P. Operational assessment of point-of-care diagnostics in rural primary healthcare clinics of KwaZulu-Natal, South Africa: A cross-sectional survey. BMC Health Serv. Res. 2018, 18, 380. [Google Scholar] [CrossRef] [PubMed]
- Gonzales, C.K.; Leroy, G. Eliciting user requirements using appreciative inquiry. Empir. Softw. Eng. 2011, 16, 733–772. [Google Scholar] [CrossRef]
- Delbecq, A.L.; Van de Ven, A.H.; Gustafson, D.H. Group Techniques for Program Planning: A Guide to Nominal Group and Delphi Processes; Oxford University Press: New York, NY, USA, 1976; p. 338. [Google Scholar]
- Poling, R. THE NOMINAL GROUP TECHNIQUE. Available online: https://www.uaex.edu/support-units/program-staff-development/docs/NGTProcess%2012.pdf (accessed on 9 January 2020).
- Dening, K.H.; Jones, L.; Sampson, E.L. Preferences for end-of-life care: A nominal group study of people with dementia and their family carers. Palliat. Med. 2013, 27, 409–417. [Google Scholar] [CrossRef] [PubMed]
- Hiligsmann, M.; van Durme, C.; Geusens, P.; Dellaert, B.G.; Dirksen, C.D.; van der Weijden, T.; Reginster, J.-Y.; Boonen, A. Nominal group technique to select attributes for discrete choice experiments: An example for drug treatment choice in osteoporosis. Patient Prefer. Adherence 2013, 7, 133. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, T.; Hewlett, S.; Richards, P.; Morris, M.; Calnan, M. Utilizing qualitative data from nominal groups: Exploring the influences on treatment outcome prioritization with rheumatoid arthritis patients. J. Health Psychol. 2012, 17, 132–142. [Google Scholar] [CrossRef] [PubMed]
- Johnson, L.F.; Dorrington, R.E.; Moolla, H. Progress towards the 2020 targets for HIV diagnosis and antiretroviral treatment in South Africa. S. Afr. J. Hiv Med. 2017, 18. [Google Scholar] [CrossRef] [PubMed]
- UNAIDS. UNAIDS DATA 2017. 2017. Available online: https://www.unaids.org/en/resources/documents/2017/2017_data_book (accessed on 9 January 2020).
- Gaede, B.; Versteeg, M. The state of the right to health in rural South Africa. South Afr. health Rev. 2011, 1, 99–106. [Google Scholar]
- Engel, N.; Ganesh, G.; Patil, M.; Yellappa, V.; Pai, N.P.; Vadnais, C.; Pai, M. Barriers to point-of-care testing in India: Results from qualitative research across different settings, users and major diseases. PLoS ONE 2015, 10, e0135112. [Google Scholar] [CrossRef] [PubMed]
- Gopal, T. In-Depth: The Problem of Stopping or not Starting HIV Treatment. Available online: https://www.google.com.hk/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&ved=2ahUKEwidp8iSx_XmAhX6wosBHZ_CCP4QFjAAegQIBRAB&url=https%3A%2F%2Fwww.spotlightnsp.co.za%2F2019%2F03%2F06%2Fin-depth-the-problem-of-stopping-or-not-starting-hiv-treatment%2F&usg=AOvVaw3HFvVqkZ9Nv-qvh7zqK5M0 (accessed on 9 January 2020).
- Sink, D.S. Using the nominal group technique effectively. Natl. Product. Rev. 1983, 2, 173–184. [Google Scholar] [CrossRef]
| District/Institution | Occupation | POC Diagnostics Involvement |
|---|---|---|
| Umgungundlovu | Professional Nurse | Testing and HIV Program co-Ordinator |
| Harry Gwala | Professional Nurse | Full patient consultations, including HIV testing |
| Uthukela | Professional Nurse | Full patient consultations, including HIV testing |
| Umzinyathi | TB Professional Nurse | TB and HIV testing |
| Ilembe | HIV/AIDS lay councillor | HIV Testing |
| Ethekwini | TB assistant | Previous HIV lay counsellor |
| University of KZN | Academic Leader | Medical Scientist, Public Health Professor with expertise on implementation research for POC diagnostics |
| University of KZN | Postdoctoral Fellow | Researcher in implementation and supply chain management of POC diagnostic tests |
| Item | Summing by Votes Scores | Total% | ||||
|---|---|---|---|---|---|---|
| 5 | 4 | 3 | 2 | 1 | 100 | |
| No POC Testing Curriculum for nurses | 7 | 2 | 0 | 1 | 0 | 90 |
| No training of staff on HIV testing and counselling as lay counsellors are being phased out. | 7 | 0 | 2 | 1 | 0 | 86 |
| Continuous Professional Development | 6 | 1 | 3 | 0 | 0 | 84 |
| HPIC Tracking and registering patients before testing: Correct Record Keeping | 6 | 2 | 0 | 1 | 1 | 82 |
| Staff involvement in POC Management program | 5 | 2 | 2 | 0 | 1 | 80 |
| Pressure on lay councillors due to staff shortage and having to meet targets | 4 | 3 | 1 | 1 | 1 | 76 |
| Supply Chain Management for POC diagnostics testing | 4 | 3 | 1 | 1 | 1 | 76 |
| Confidentiality-Stigma | 4 | 2 | 2 | 1 | 1 | 74 |
| Research Study Process control: Better informed participants to ensure adherence to study timelines | 2 | 1 | 5 | 1 | 1 | 64 |
| Client Attitude to testing | 2 | 1 | 5 | 1 | 1 | 64 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chamane, N.; Kuupiel, D.; Mashamba-Thompson, T.P. Stakeholders’ Perspectives for the Development of a Point-of-Care Diagnostics Curriculum in Rural Primary Clinics in South Africa—Nominal Group Technique. Diagnostics 2020, 10, 195. https://doi.org/10.3390/diagnostics10040195
Chamane N, Kuupiel D, Mashamba-Thompson TP. Stakeholders’ Perspectives for the Development of a Point-of-Care Diagnostics Curriculum in Rural Primary Clinics in South Africa—Nominal Group Technique. Diagnostics. 2020; 10(4):195. https://doi.org/10.3390/diagnostics10040195
Chicago/Turabian StyleChamane, Nkosinothando, Desmond Kuupiel, and Tivani Phosa Mashamba-Thompson. 2020. "Stakeholders’ Perspectives for the Development of a Point-of-Care Diagnostics Curriculum in Rural Primary Clinics in South Africa—Nominal Group Technique" Diagnostics 10, no. 4: 195. https://doi.org/10.3390/diagnostics10040195
APA StyleChamane, N., Kuupiel, D., & Mashamba-Thompson, T. P. (2020). Stakeholders’ Perspectives for the Development of a Point-of-Care Diagnostics Curriculum in Rural Primary Clinics in South Africa—Nominal Group Technique. Diagnostics, 10(4), 195. https://doi.org/10.3390/diagnostics10040195






