Ultrasound Assessment of the Abdominal Wall Muscles in Women with and without Primary Dysmenorrhea: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Considerations
2.3. Participants
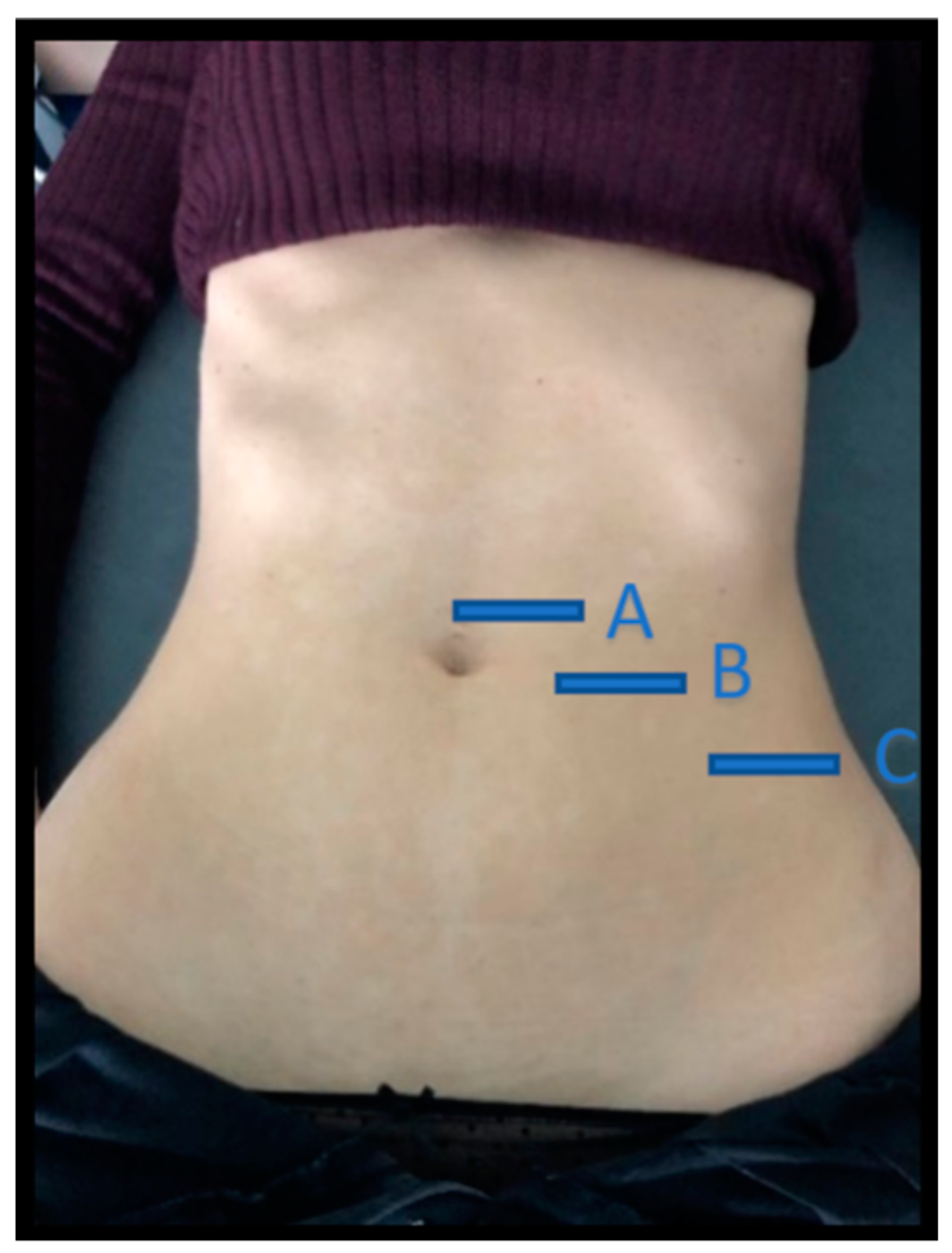
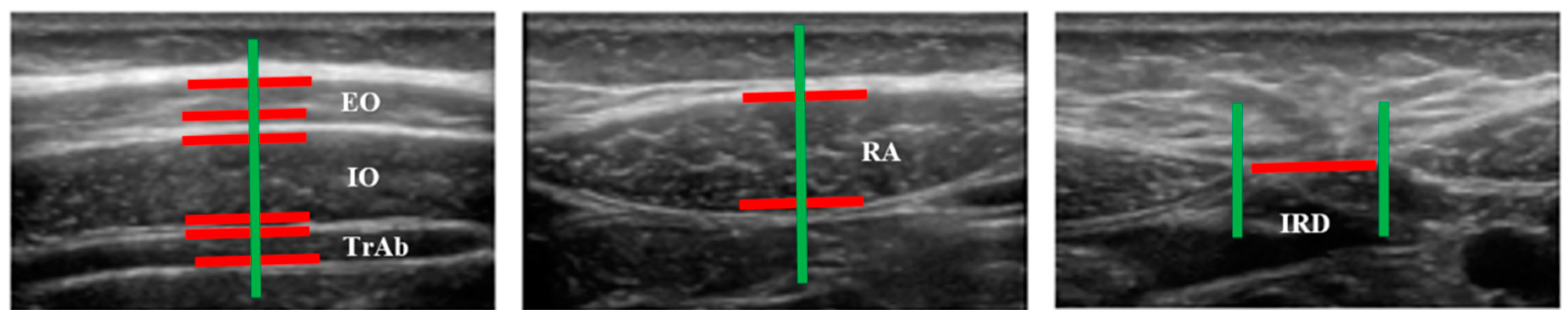
2.4. Outcome Measurements
2.5. Statistical Analysis
3. Results
4. Discussion
Limitations and Future Lines
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Westling, A.M.; Tu, F.F.; Griffith, J.W.; Hellman, K.M. The association of dysmenorrhea with noncyclic pelvic pain accounting for psychological factors. Am. J. Obstet. Gynecol. 2013, 209, 422.e1–422.e10. [Google Scholar] [CrossRef] [PubMed]
- Vincent, K. Pelvic pain in women: Clinical and scientific aspects. Curr. Opin. Support. Palliat. Care 2011, 5, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Ju, H.; Jones, M.; Mishra, G. The prevalence and risk factors of dysmenorrhea. Epidemiol. Rev. 2014, 36, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Polat, A.; Celik, H.; Gurates, B.; Kaya, D.; Nalbant, M.; Kavak, E.; Hanay, F. Prevalence of primary dysmenorrhea in young adult female university students. Arch. Gynecol. Obstet. 2009, 279, 527–532. [Google Scholar] [CrossRef]
- Dawood, M.Y. Primary dysmenorrhea: Advances in pathogenesis and management. Obstet. Gynecol. 2006, 108, 428–441. [Google Scholar] [CrossRef]
- Chan, W.; Dawood, M.; Fuchs, F. Prostaglandins in primary dysmenorrhea: Comparison of prophylactic and nonprophylactic treatment with ibuprofen and use of oral contraceptives. Am. J. Med. 1981, 70, 535–541. [Google Scholar] [CrossRef]
- Bernardi, M.; Lazzeri, L.; Perelli, F.; Reis, F.M.; Petraglia, F. Dysmenorrhea and related disorders. F1000Research 2017, 6, 1645. [Google Scholar] [CrossRef]
- Coxon, L.; Horne, A.W.; Vincent, K. Pathophysiology of endometriosis-associated pain: A review of pelvic and central nervous system mechanisms. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 51, 53–67. [Google Scholar] [CrossRef]
- La Rosa, V.L.; De Franciscis, P.; Barra, F.; Schiattarella, A.; Torok, P.; Shah, M.; Karaman, E.; Marques Cerentini, T.; Di Guardo, F.; Gullo, G.; et al. Quality of life in women with endometriosis: A narrative overview. Minerva Med. 2019. [Google Scholar] [CrossRef]
- Patel, V.; Tanksale, V.; Sahasrabhojanee, M.; Gupte, S.; Nevrekar, P. The burden and determinants of dysmenorrhoea: A population-based survey of 2262 women in Goa, India. BJOG Int. J. Obstet. Gynaecol. 2006, 113, 453–463. [Google Scholar] [CrossRef]
- Oladosu, F.; Tu, F.; Farhan, S.; Garrison, E.F.; Steiner, N.D.; Roth, G.E.; Hellman, K.M. Abdominal skeletal muscle activity precedes spontaneous menstrual cramping pain in primary dysmenorrhea. Am. J. Obstet. Gynecol. 2018, 219, 91.e1–91.e7. [Google Scholar] [CrossRef] [PubMed]
- KiM, M.; BaeK, I.H.; Goo, B.O. The relationship between pelvic alignment and dysmenorrhea. J. Phys. Ther. Sci. 2016, 28, 757–760. [Google Scholar] [CrossRef] [PubMed]
- Holtzman, D.; Petrocco-Napuli, K.; Burke, J.R. Prospective case series on the effects of lumbosacral manipulation on dysmenorrhea. J. Manip. Physiol. Ther. 2008, 31, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Blakey, H.; Chisholm, C.; Dear, F.; Harris, B.; Hartwell, R.; Daley, A.J.; Jolly, K. Is exercise associated with primary dysmenorrhoea in young women? BJOG Int. J. Obstet. Gynaecol. 2010, 117, 222–224. [Google Scholar] [CrossRef] [PubMed]
- Molins-Cubero, S.; Rodríguez-Blanco, C.; Oliva-Pascual-Vaca, Á.; Heredia-Rizo, A.M.; Boscá-Gandía, J.J.; Ricard, F. Changes in pain perception after pelvis manipulation in women with primary dysmenorrhea: A randomized controlled trial. Pain Med. 2014, 15, 1455–1463. [Google Scholar] [CrossRef] [PubMed]
- Proctor, M.; Hing, W.; Johnson, T.; Murphy, P. Spinal manipulation for primary and secondary dysmenorrhoea. In Cochrane Database of Systematic Reviews; John Wiley & Sons: Hoboken, NJ, USA, 2001. [Google Scholar]
- Hides, J.A.; Miokovic, T.; Belavý, D.L.; Stanton, W.R.; Richardson, C.A. Ultrasound Imaging Assessment of Abdominal Muscle Function During Drawing-in of the Abdominal Wall: An Intrarater Reliability Study. J. Orthop. Sport. Phys. Ther. 2007, 37, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Teyhen, D.S.; Gill, N.W.; Whittaker, J.L.; Henry, S.M.; Hides, J.A.; Hodges, P. Rehabilitative ultrasound imaging of the abdominal muscles. J. Orthop. Sports Phys. Ther. 2007, 37, 450–466. [Google Scholar] [CrossRef]
- Whittaker, J.L.; Stokes, M. Ultrasound Imaging and Muscle Function. J. Orthop. Sport. Phys. Ther. 2011, 41, 572–580. [Google Scholar] [CrossRef]
- Morales, C.R.; Polo, J.A.; Sanz, D.R.; López, D.L.; González, S.V.; Buría, J.L.A.; Lobo, C.C. Ultrasonography features of abdominal perimuscular connective tissue in elite and amateur basketball players: An observational study. Rev. Assoc. Med. Bras. 2018, 64, 936–941. [Google Scholar] [CrossRef]
- Abuín-Porras, V.; de la Cueva-Reguera, M.; Benavides-Morales, P.; Ávila-Pérez, R.; de la Cruz-Torres, B.; Pareja-Galeano, H.; Blanco-Morales, M.; Romero-Morales, C. Comparison of the Abdominal Wall Muscle Thickness in Female Rugby Players Versus Non-Athletic Women: A Cross-Sectional Study. Medicina 2019, 56, 8. [Google Scholar]
- Koppenhaver, S.L.; Hebert, J.J.; Fritz, J.M.; Parent, E.C.; Teyhen, D.S.; Magel, J.S. Reliability of Rehabilitative Ultrasound Imaging of the Transversus Abdominis and Lumbar Multifidus Muscles. Arch. Phys. Med. Rehabil. 2009, 90, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [CrossRef] [PubMed]
- Whittaker, J.L.; Warner, M.B.; Stokes, M. Comparison of the Sonographic Features of the Abdominal Wall Muscles and Connective Tissues in Individuals With and Without Lumbopelvic Pain. J. Orthop. Sport. Phys. Ther. 2013, 43, 11–19. [Google Scholar] [CrossRef]
- Kim, M.; Baek, I.; Goo, B. The effect of lumbar-pelvic alignment and abdominal muscle thickness on primary dysmenorrhea. J. Phys. Ther. Sci. 2016, 28, 2988–2990. [Google Scholar] [CrossRef]
- Payne, L.A.; Seidman, L.C.; Sim, M.S.; Rapkin, A.J.; Naliboff, B.D.; Zeltzer, L.K. Experimental evaluation of central pain processes in young women with primary dysmenorrhea. Pain 2019, 160, 1421–1430. [Google Scholar] [CrossRef]
- Caruso, S.; Cianci, S.; Vitale, S.G.; Fava, V.; Cutello, S.; Cianci, A. Sexual function and quality of life of women adopting the levonorgestrel-releasing intrauterine system (LNG-IUS 13.5 mg) after abortion for unintended pregnancy. Eur. J. Contracept. Reprod. Health Care 2018, 23, 24–31. [Google Scholar] [CrossRef]
- Sansone, A.; De Rosa, N.; Giampaolino, P.; Guida, M.; Lagana, A.S.; Di Carlo, C. Effects of etonogestrel implant on quality of life, sexual function, and pelvic pain in women suffering from endometriosis: Results from a multicenter, prospective, observational study. Arch. Gynecol. Obstet. 2018, 298, 731–736. [Google Scholar] [CrossRef]
- Lim, C.; Park, Y.; Bae, Y. The effect of the kinesio taping and spiral taping on menstrual pain and premenstrual syndrome. J. Phys. Ther. Sci. 2013, 25, 761–764. [Google Scholar] [CrossRef]
- Whittaker, J.L. Ultrasound imaging of the lateral abdominal wall muscles in individuals with lumbopelvic pain and signs of concurrent hypocapnia. Man. Ther. 2008, 13, 404–410. [Google Scholar] [CrossRef]
- Schrepf, A.; Williams, D.A.; Gallop, R.; Naliboff, B.D.; Basu, N.; Kaplan, C.; Harper, D.E.; Richard Landis, J.; Quentin Clemens, J.; Strachan, E.; et al. Sensory sensitivity and symptom severity represent unique dimensions of chronic pain: A MAPP Research Network study. Pain 2018, 159, 2002–2011. [Google Scholar] [CrossRef] [PubMed]
- Stuge, B.; Morkved, S.; Dahl, H.H.; Vollestad, N. Abdominal and pelvic floor muscle function in women with and without long lasting pelvic girdle pain. Man. Ther. 2006, 11, 287–296. [Google Scholar] [CrossRef] [PubMed]
- Gildea, J.; Hides, J.; Hodges, P.W. Morphology of the abdominal muscles in ballet dancers with and without low back pain: A magnetic resonance imaging study. J. Sci. Med. Sport 2014, 17, 452–456. [Google Scholar] [CrossRef] [PubMed]
| Data | DP (n = 19) | Controls (n = 20) | p-Value |
|---|---|---|---|
| Age, years | 20 ± 4 † | 22.50 ± 7 † | 0.647 †† |
| Height, m | 1.64 ± 0.09 † | 1.68 ± 0.055 * | 0.134 †† |
| Weight, kg | 56.00 ± 23 † | 60.55 ± 7.29 * | 0.322 †† |
| BMI (kg/m2) | 21.61 ± 3.26 * | 21.47 ± 3.67 * | 0.881 * |
| Measures | PD (n = 19) | Controls (n = 20) | p-Value |
|---|---|---|---|
| Distance (cm) IRD | 0.96 ± 0.48 (0.29–2.28) * | 1.26 ± 0.59 (0.54–2.58) * | 0.098 ** |
| Thickness (cm) | |||
| Right TrAb | 0.32 ± 0.74 (0.21–0.50) * | 0.34 ± 0.10 (0.18 –0.61) * | 0.428 ** |
| Right IO | 0.72 ± 0.14 (0.41–0.97) * | 0.71 ± 0.17 (0.41–1.09) * | 0.903 ** |
| Right OE | 0.48 ± 0.09 (0.29–0.60) * | 0.49 ± 0.11 (0.33–0.70) * | 0.557 ** |
| Left TrAb | 0.30 ± 0.06 (0.18–0.43) * | 0.32 ± 0.09 (0.20–0.57) * | 0.413 ** |
| Left IO | 0.72 ± 0.14 (0.46–0.94) * | 0.72 ± 0.17 (0.44–1.12) * | 0.939 ** |
| Left EO | 0.53 ± 0.79 (0.40–0.69) * | 0.52 ± 0.12 (0.34–0.81) * | 0.930 ** |
| Right RA | 1.02 ± 0.16 (0.67–1.22) * | 1.08 ± 0.21 (0.76–1.52) * | 0.341 ** |
| Left RA | 1.06 ± 0.13 (0.77–1.30) * | 1.07 ± 0.22 (0.78–1.54) * | 0.873 ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romero-Morales, C.; de la Cueva-Reguera, M.; Miñambres-Vallejo, B.; Ruiz-Ruiz, B.; Calvo-Lobo, C.; Casado-Hernández, I.; López-López, D.; Abuín-Porras, V. Ultrasound Assessment of the Abdominal Wall Muscles in Women with and without Primary Dysmenorrhea: A Cross-Sectional Study. Diagnostics 2020, 10, 166. https://doi.org/10.3390/diagnostics10030166
Romero-Morales C, de la Cueva-Reguera M, Miñambres-Vallejo B, Ruiz-Ruiz B, Calvo-Lobo C, Casado-Hernández I, López-López D, Abuín-Porras V. Ultrasound Assessment of the Abdominal Wall Muscles in Women with and without Primary Dysmenorrhea: A Cross-Sectional Study. Diagnostics. 2020; 10(3):166. https://doi.org/10.3390/diagnostics10030166
Chicago/Turabian StyleRomero-Morales, Carlos, Mónica de la Cueva-Reguera, Beatriz Miñambres-Vallejo, Beatriz Ruiz-Ruiz, César Calvo-Lobo, Israel Casado-Hernández, Daniel López-López, and Vanesa Abuín-Porras. 2020. "Ultrasound Assessment of the Abdominal Wall Muscles in Women with and without Primary Dysmenorrhea: A Cross-Sectional Study" Diagnostics 10, no. 3: 166. https://doi.org/10.3390/diagnostics10030166
APA StyleRomero-Morales, C., de la Cueva-Reguera, M., Miñambres-Vallejo, B., Ruiz-Ruiz, B., Calvo-Lobo, C., Casado-Hernández, I., López-López, D., & Abuín-Porras, V. (2020). Ultrasound Assessment of the Abdominal Wall Muscles in Women with and without Primary Dysmenorrhea: A Cross-Sectional Study. Diagnostics, 10(3), 166. https://doi.org/10.3390/diagnostics10030166









