In Vivo Endoscopic Optical Coherence Tomography of the Healthy Human Oral Mucosa: Qualitative and Quantitative Image Analysis
Abstract
1. Introduction
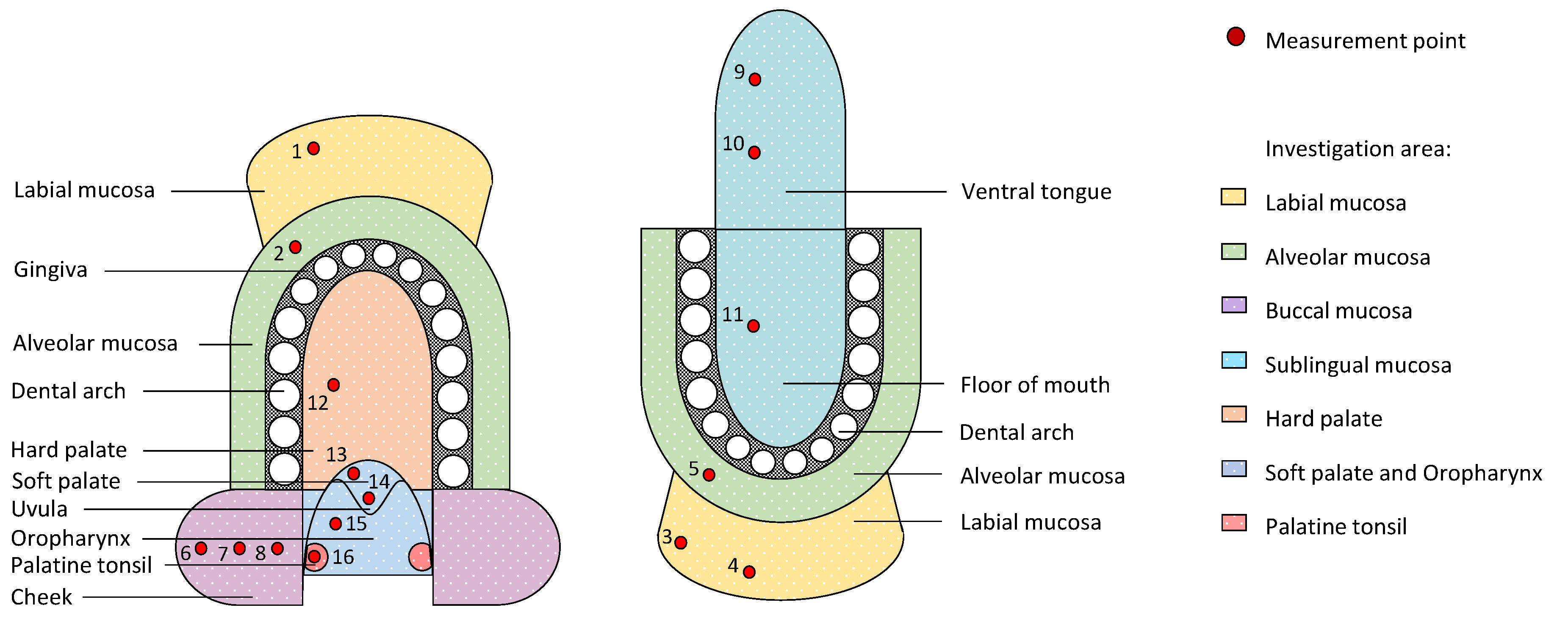
2. Materials and Methods
2.1. Study Population
2.2. Endoscopic OCT System
2.3. Measurement Protocol
2.4. OCT Image Analysis
2.5. Statistical Analysis
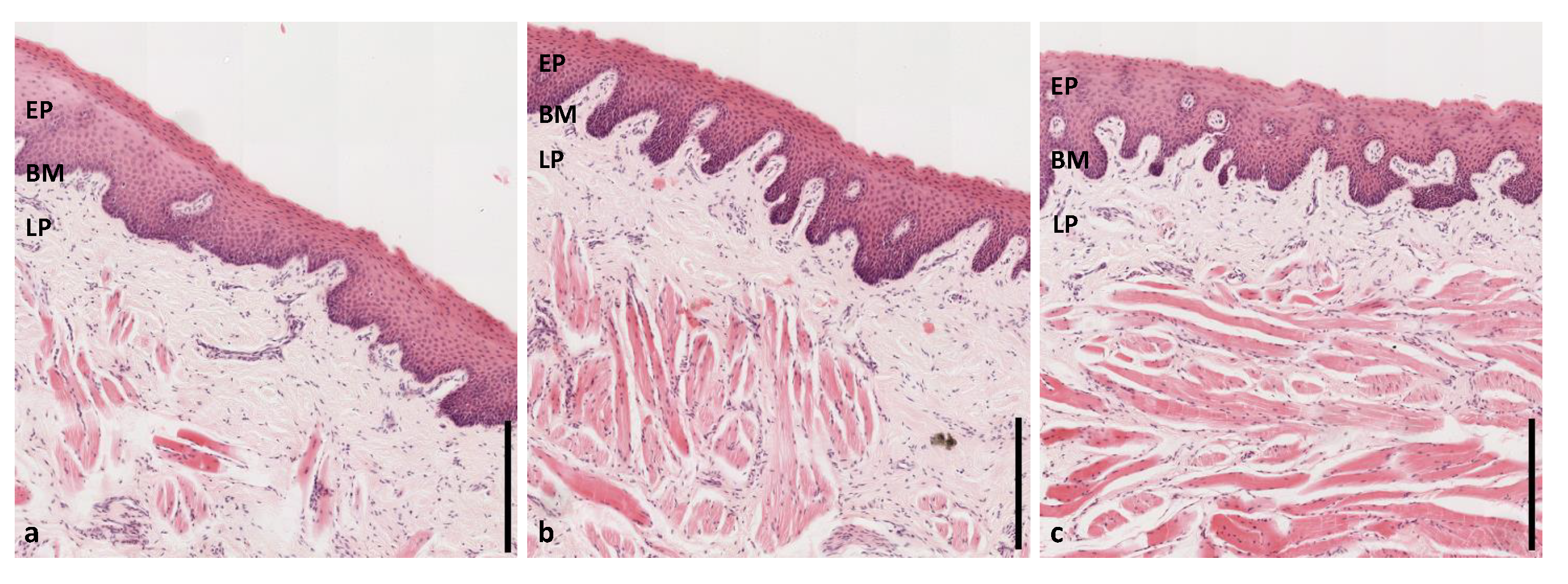
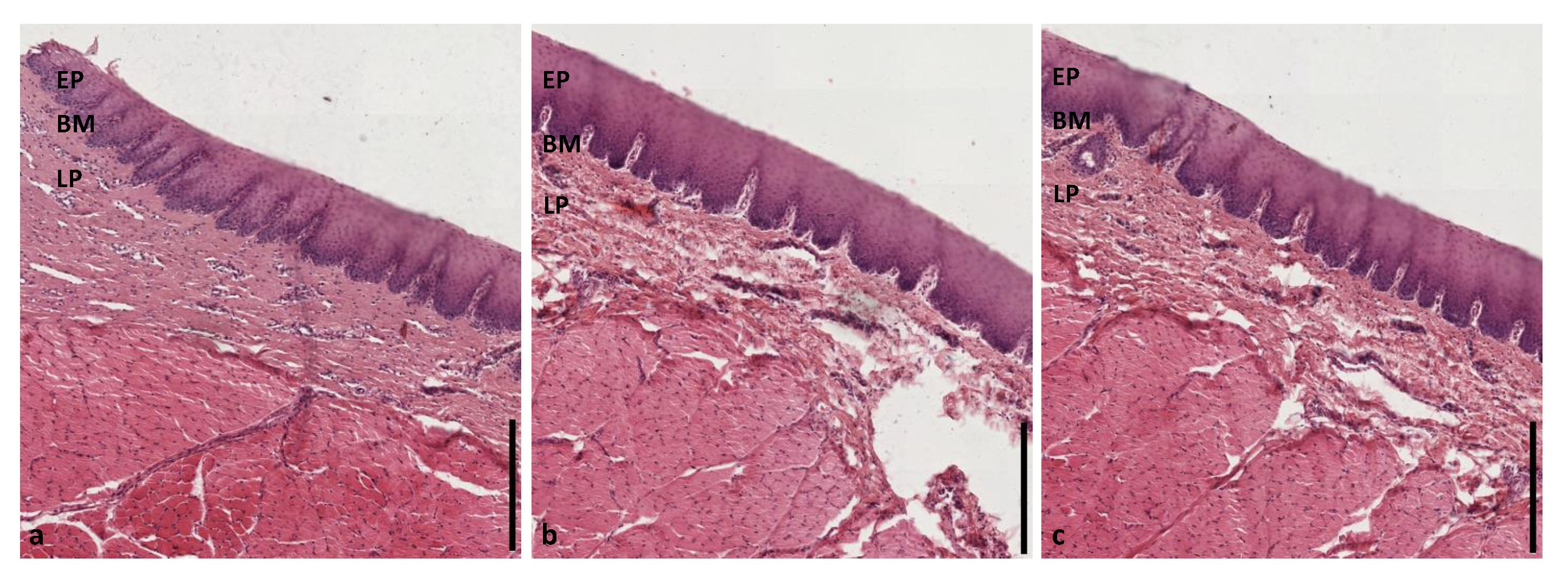
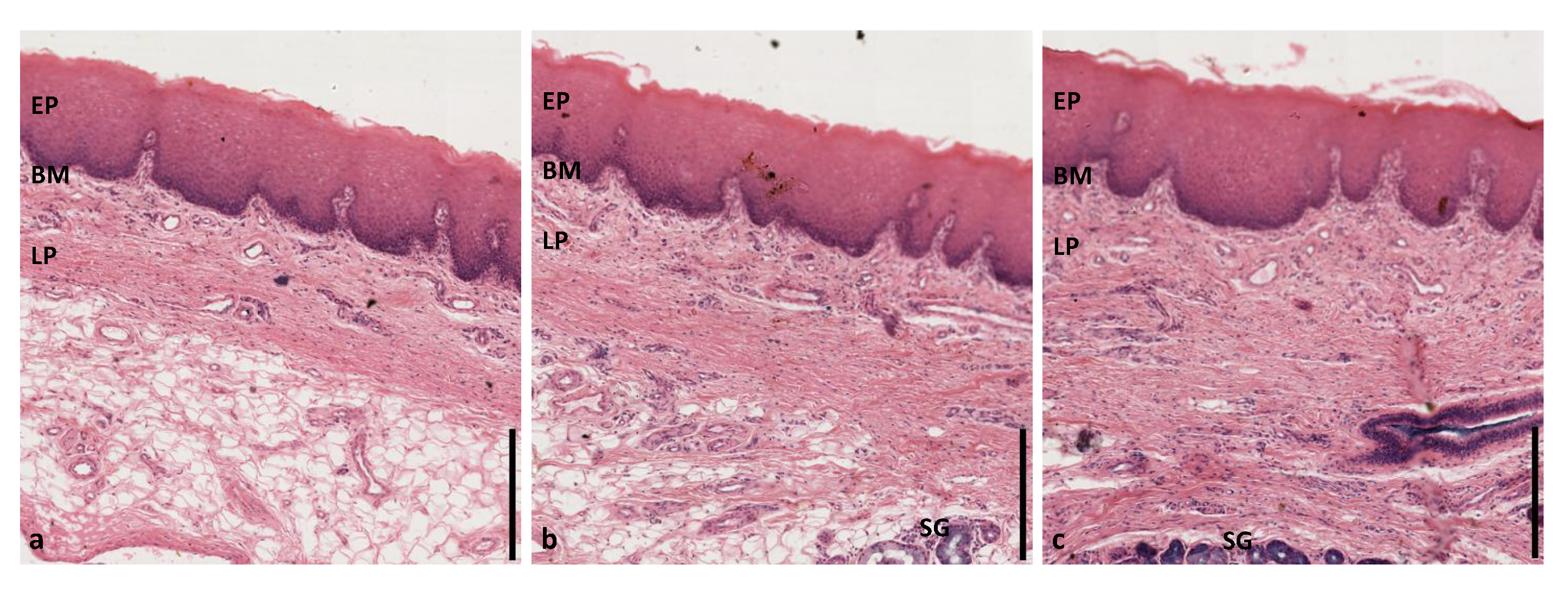
2.6. Histological Analysis
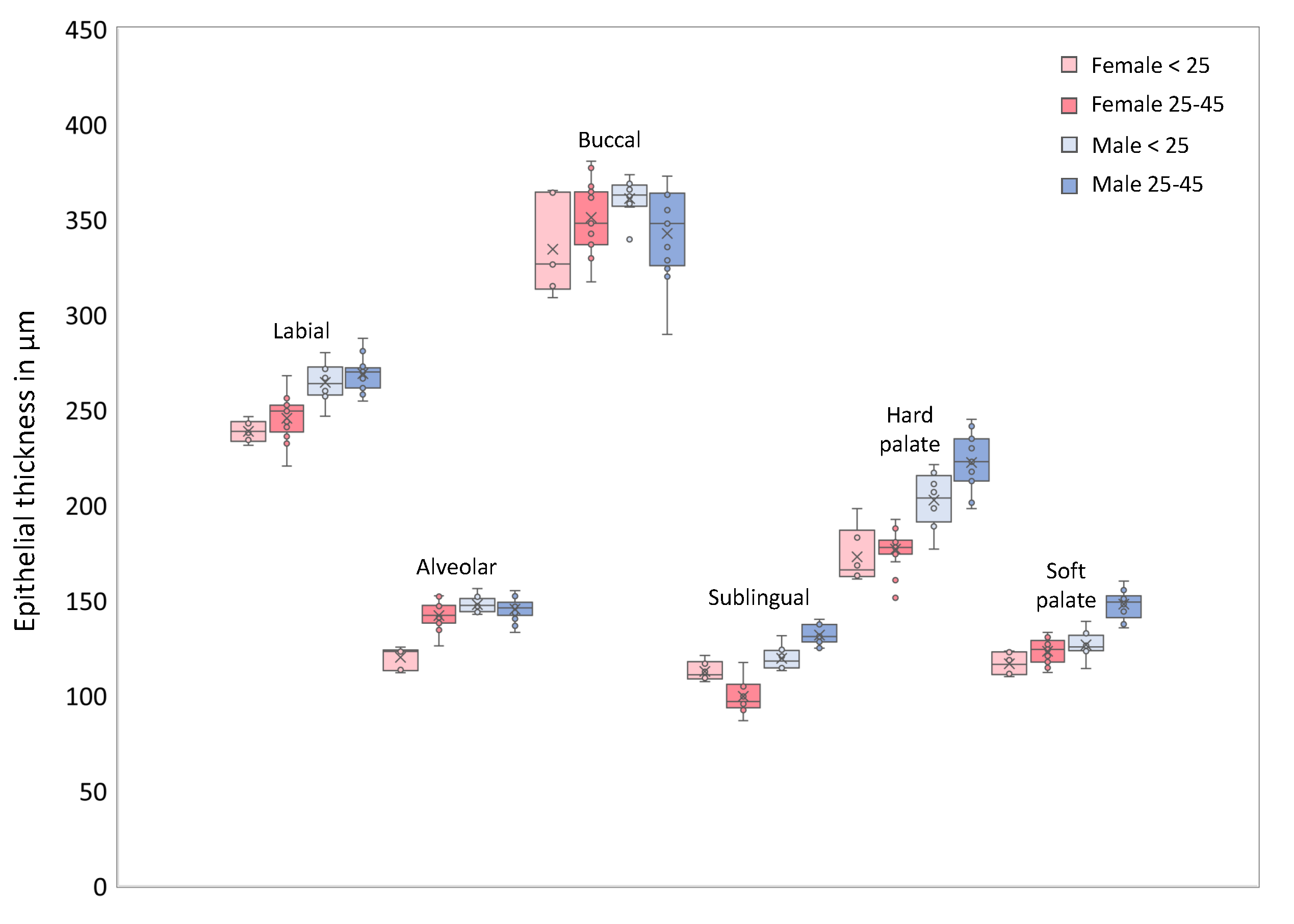
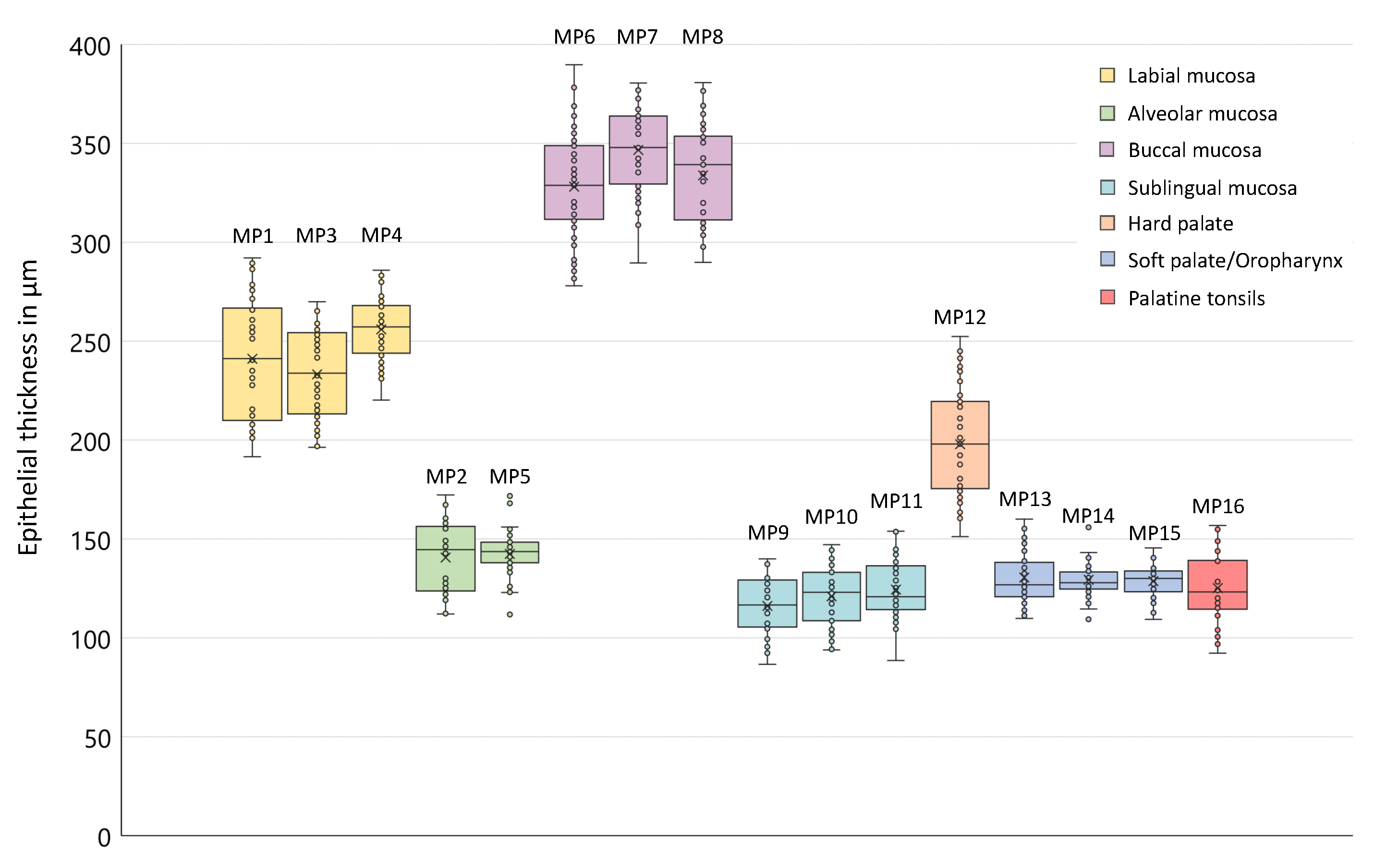
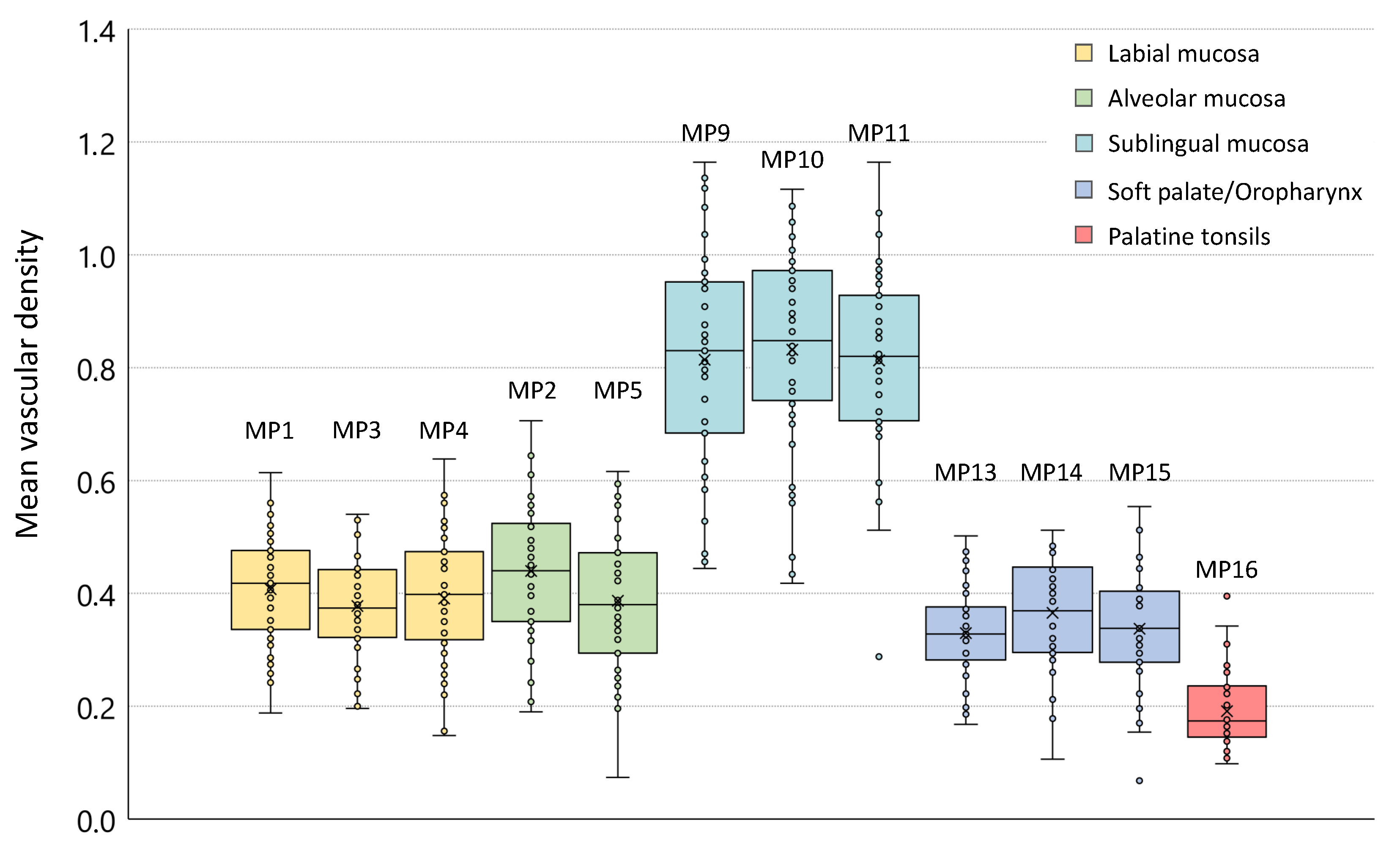
3. Results
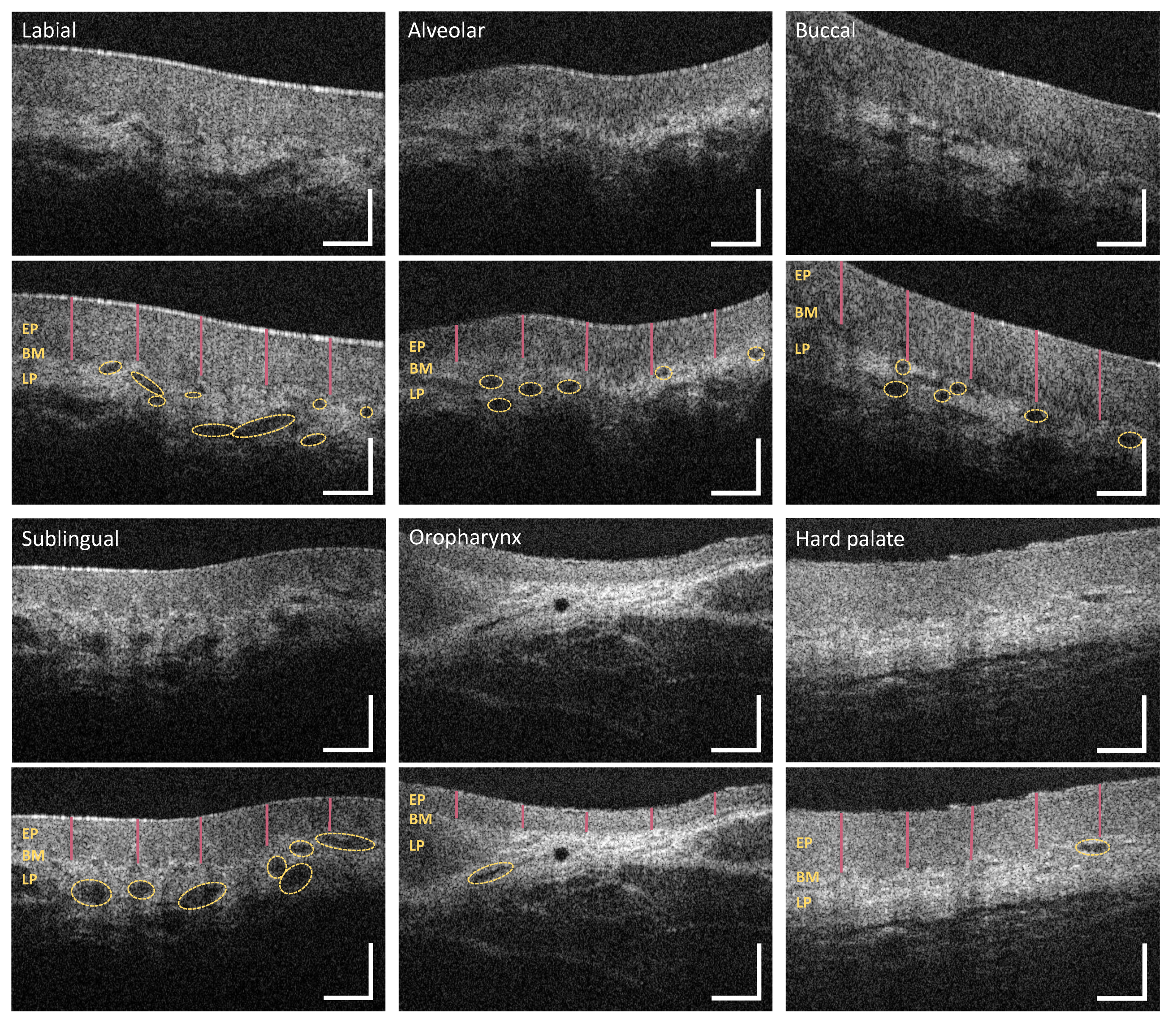
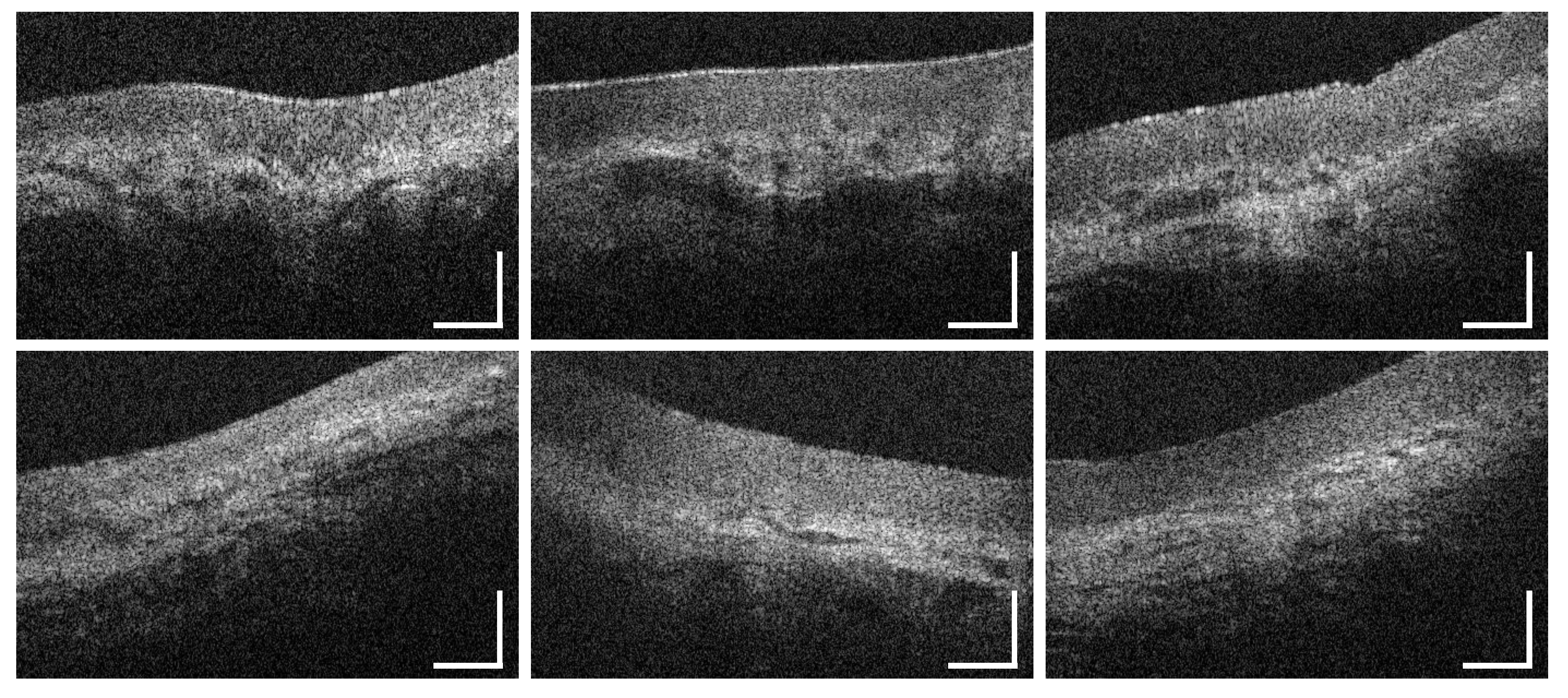
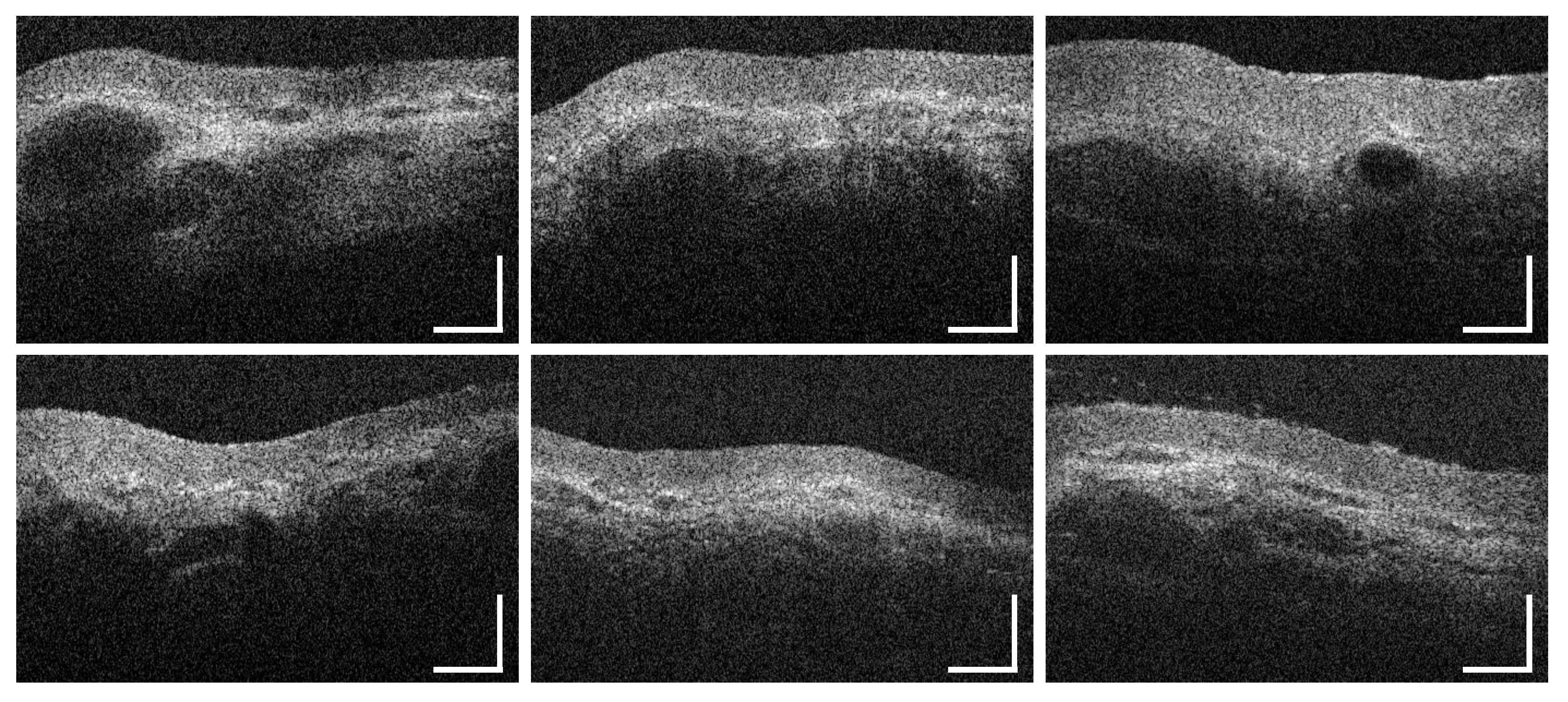
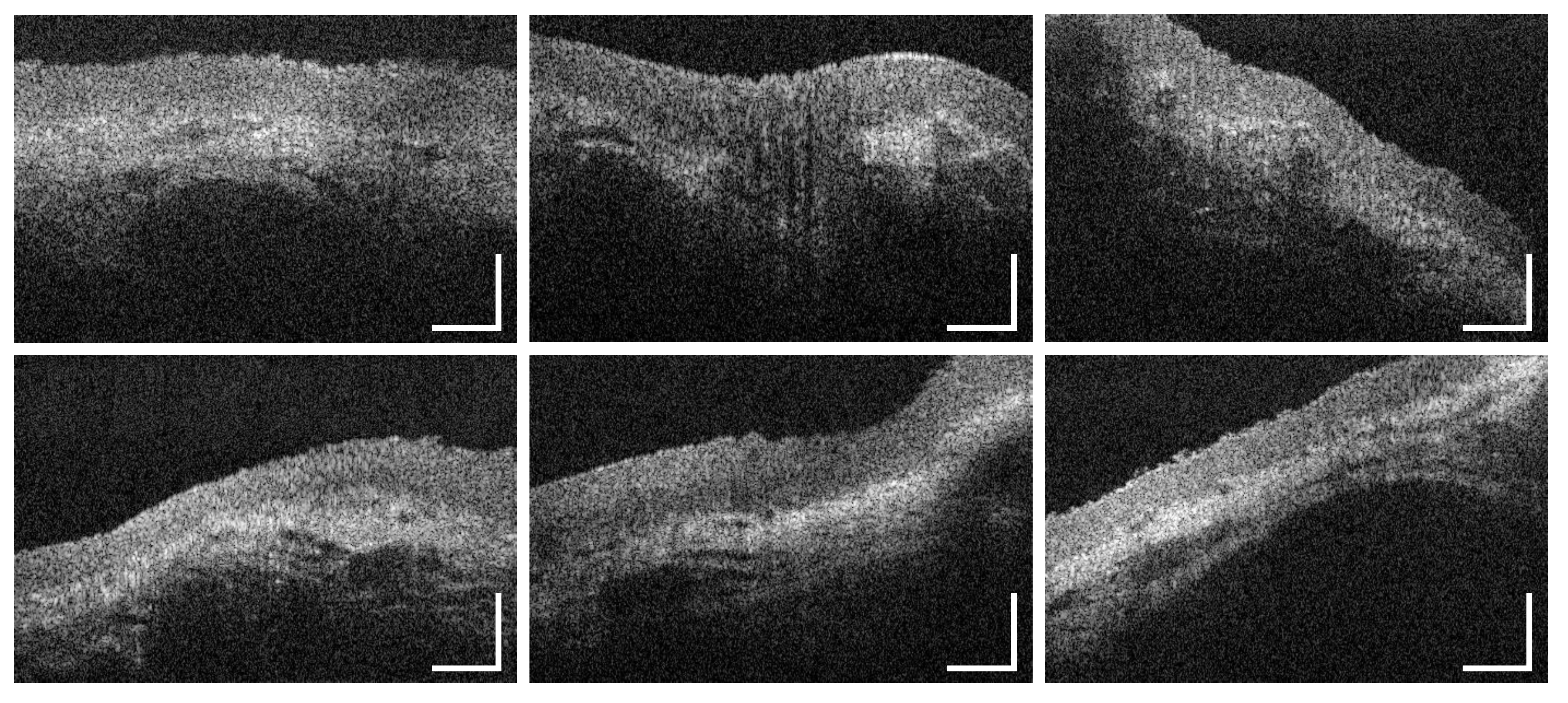
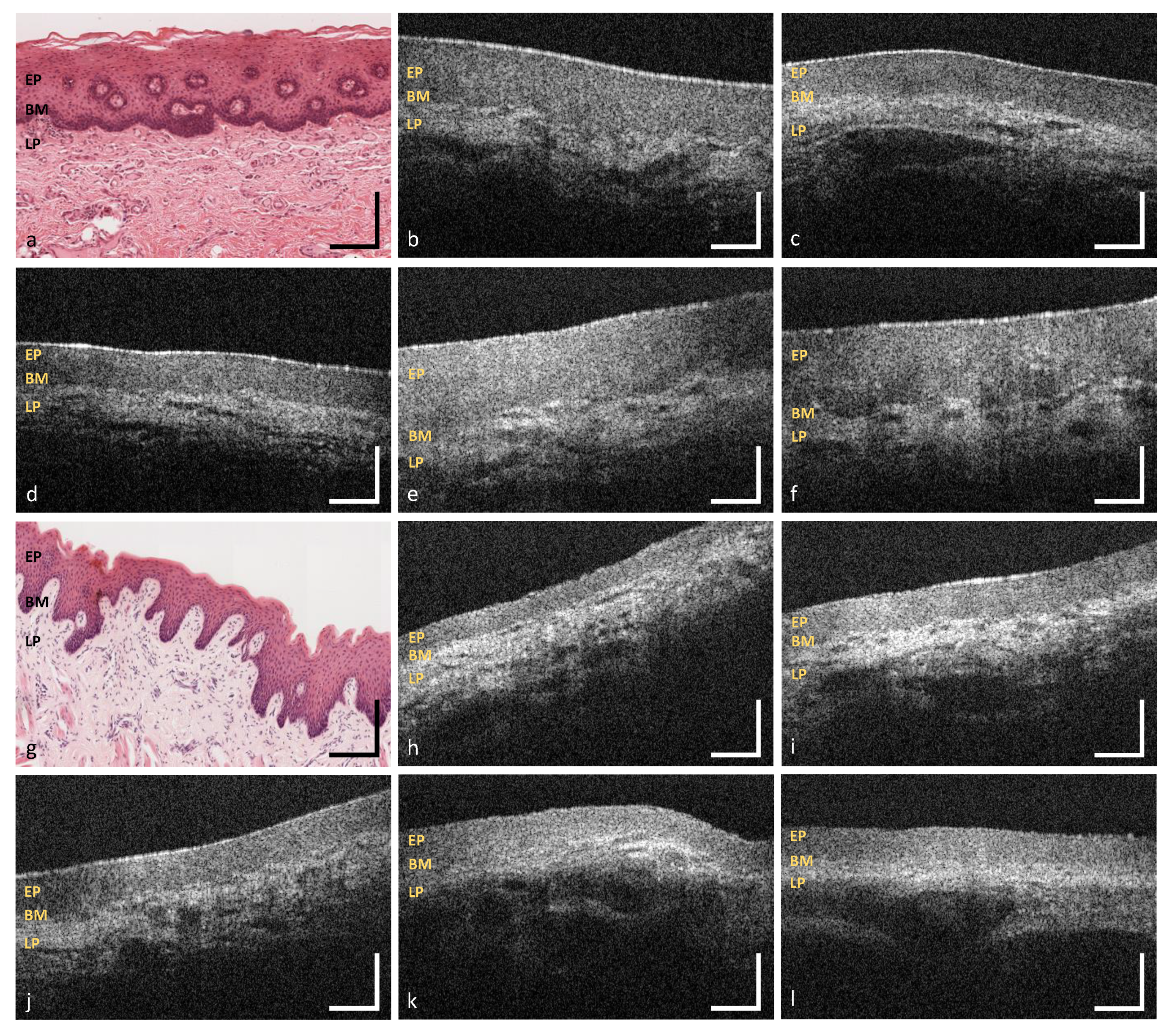
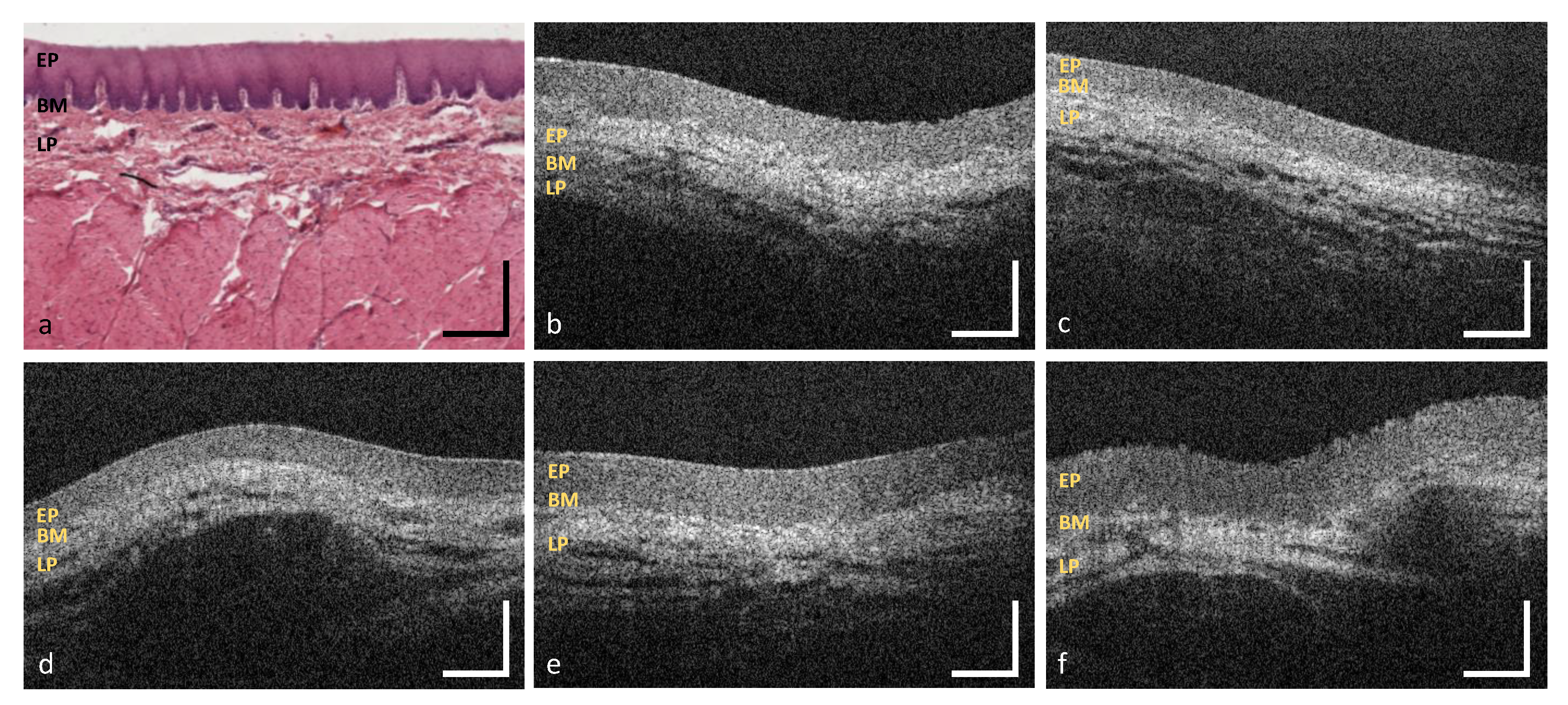
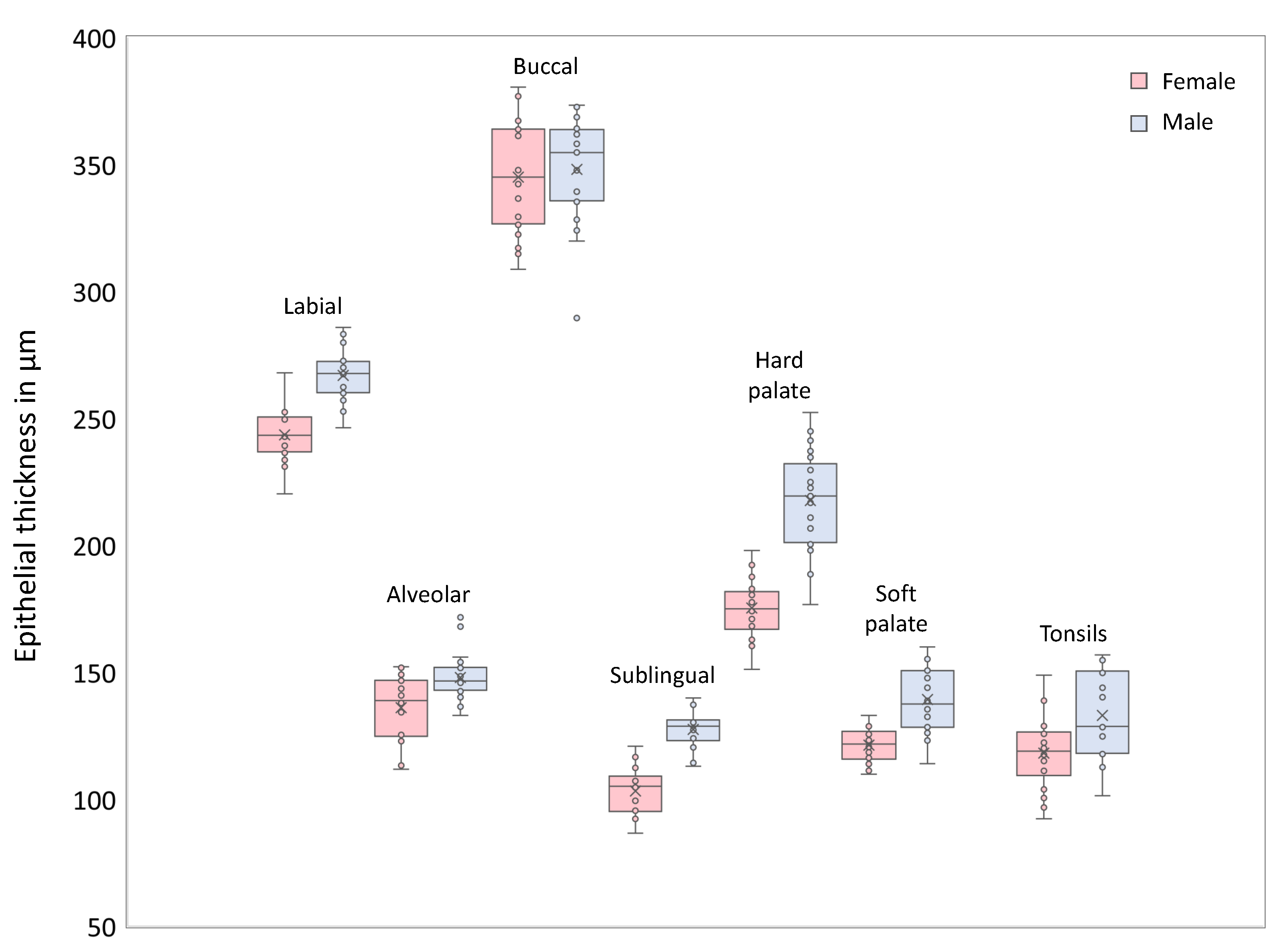
3.1. Labial and Alveolar Mucosa
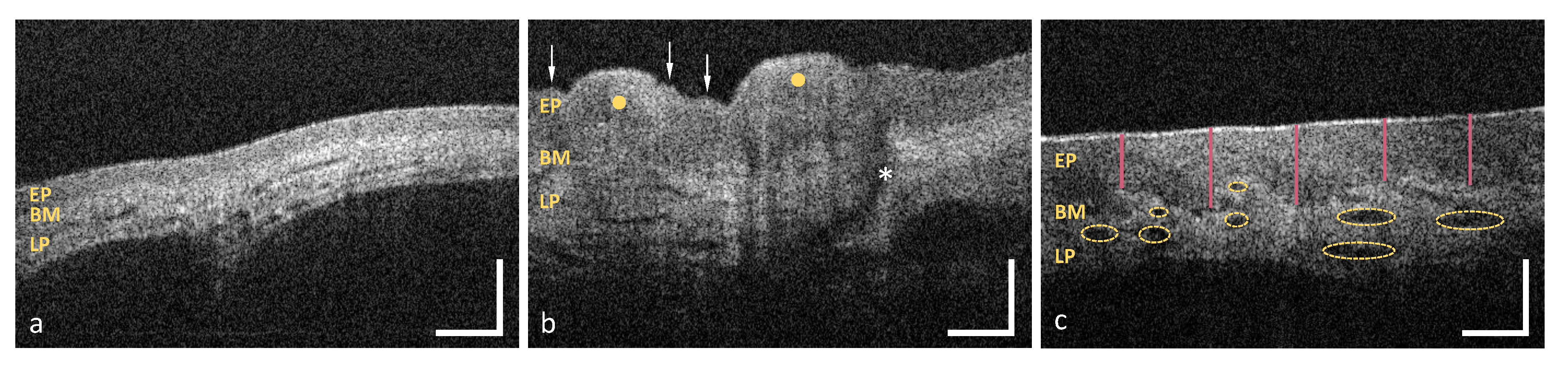
3.2. Buccal Mucosa
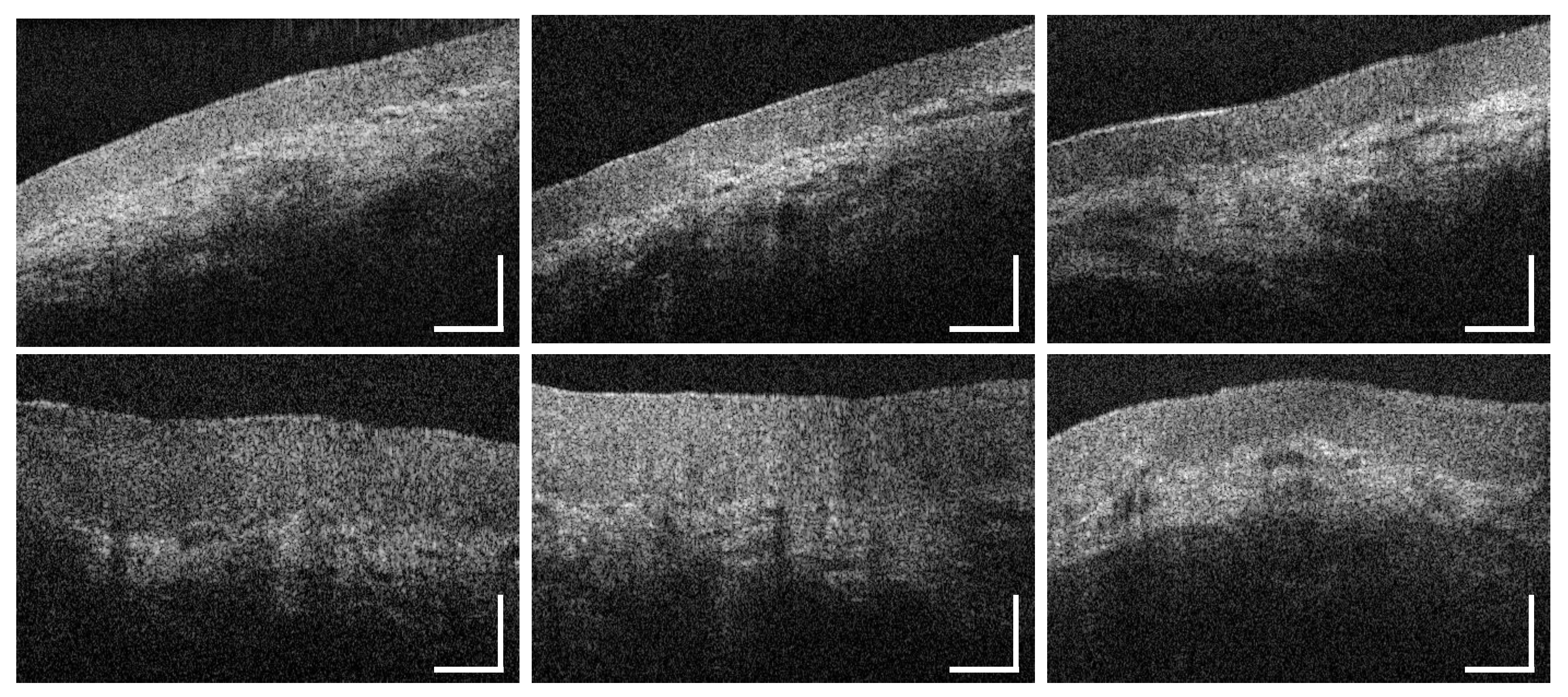
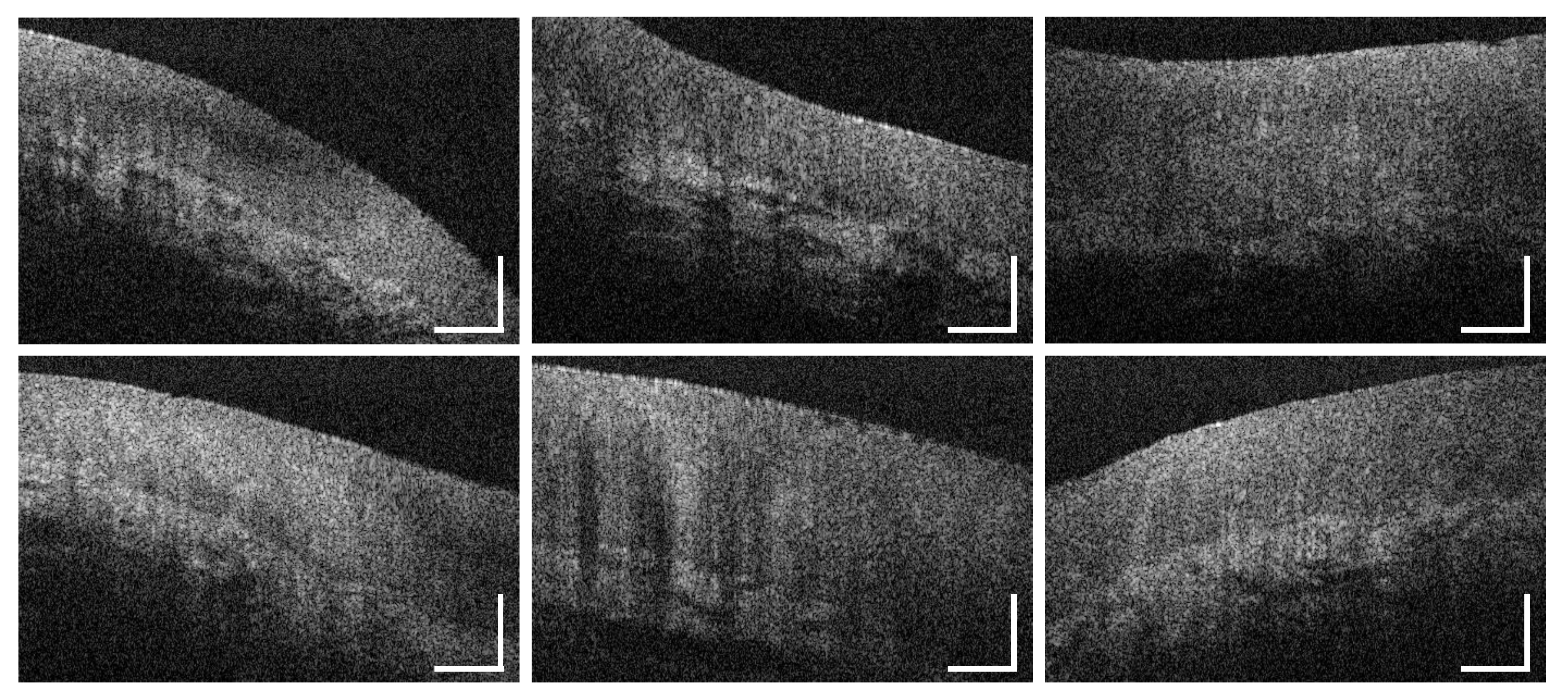
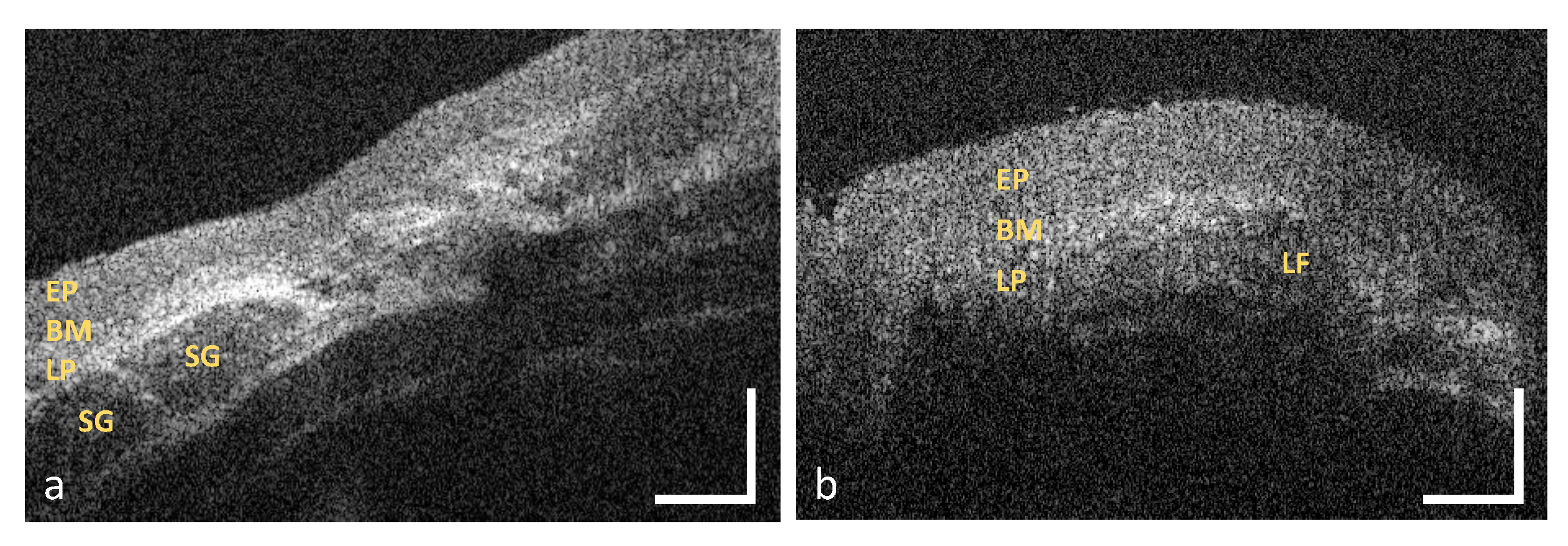
3.3. Sublingual Mucosa
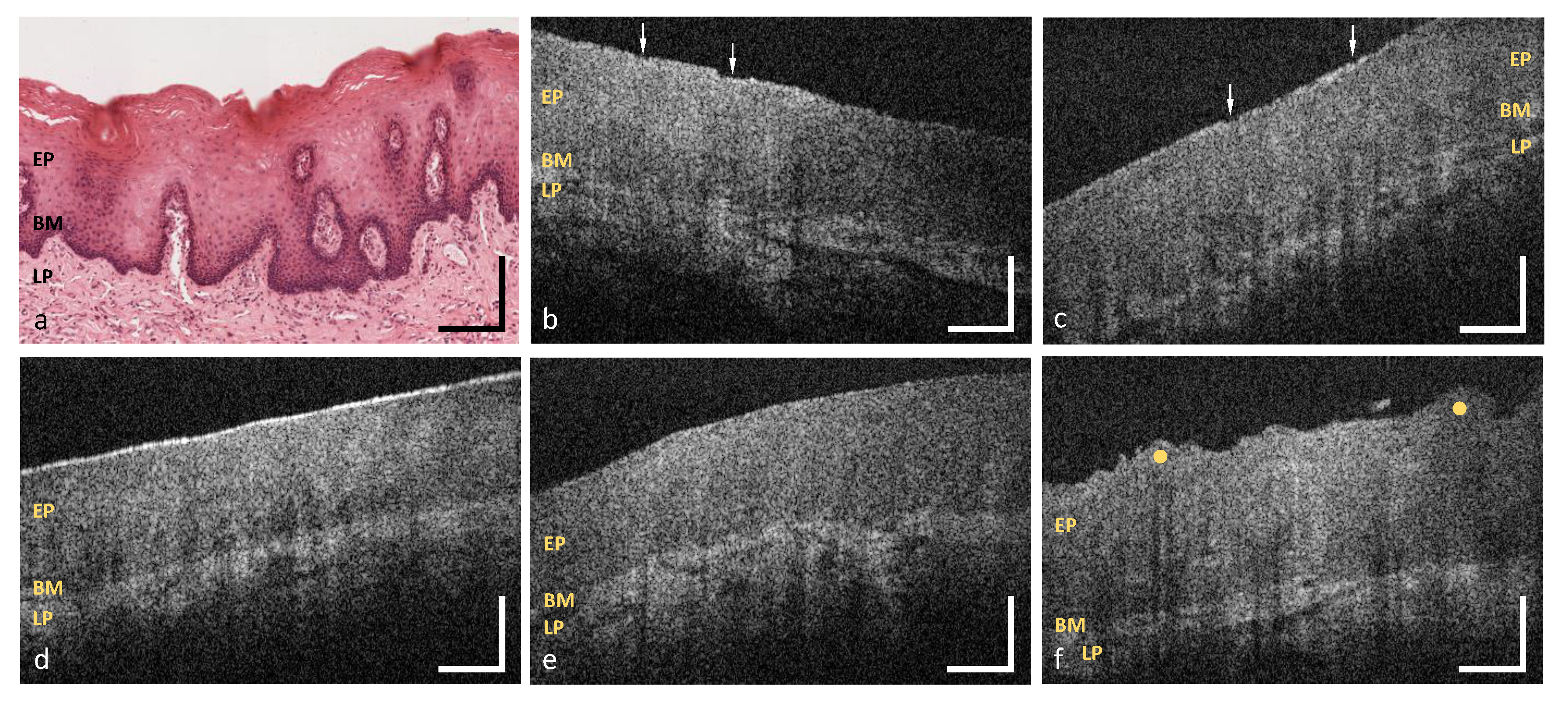
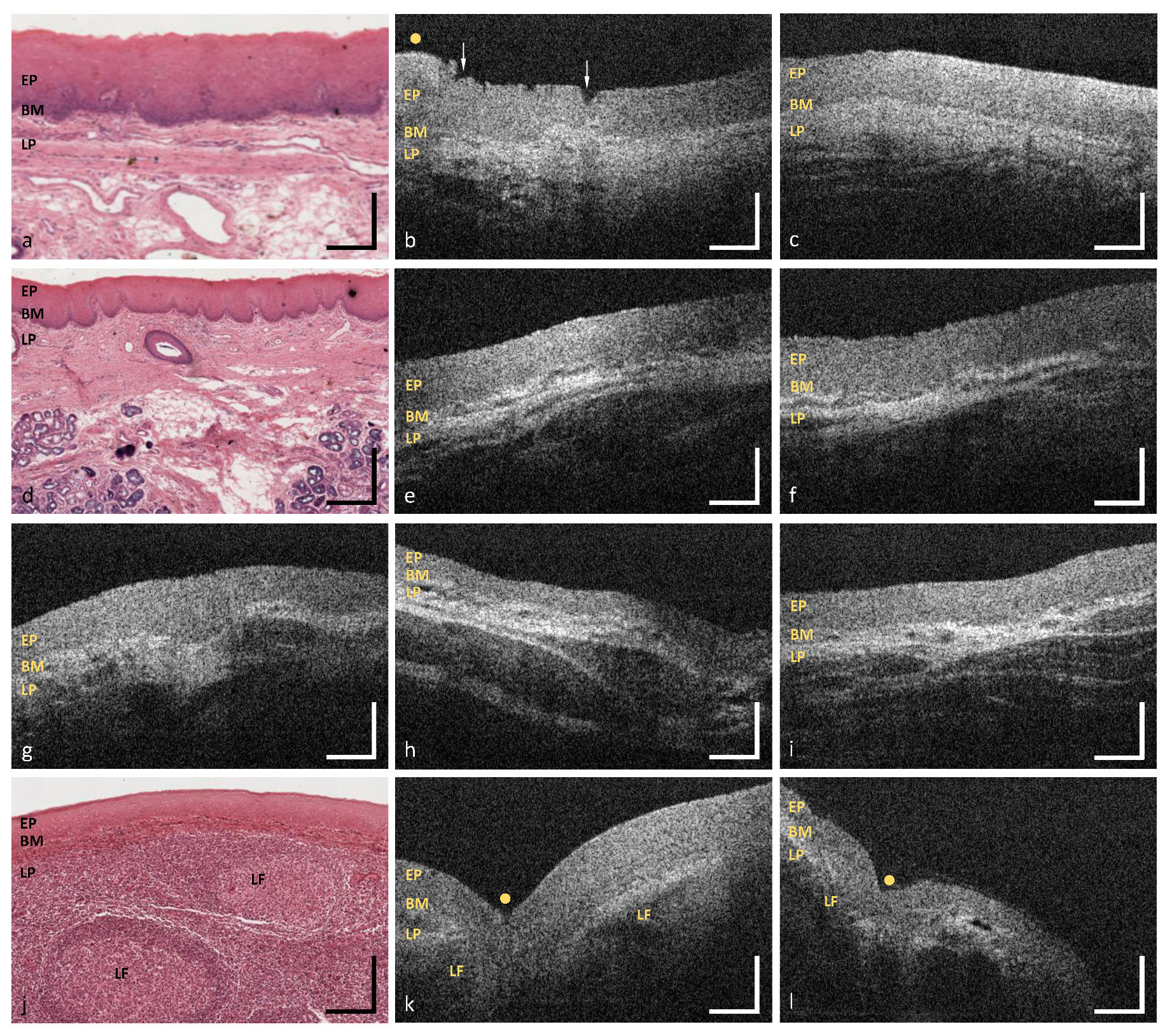
3.4. Hard Palate
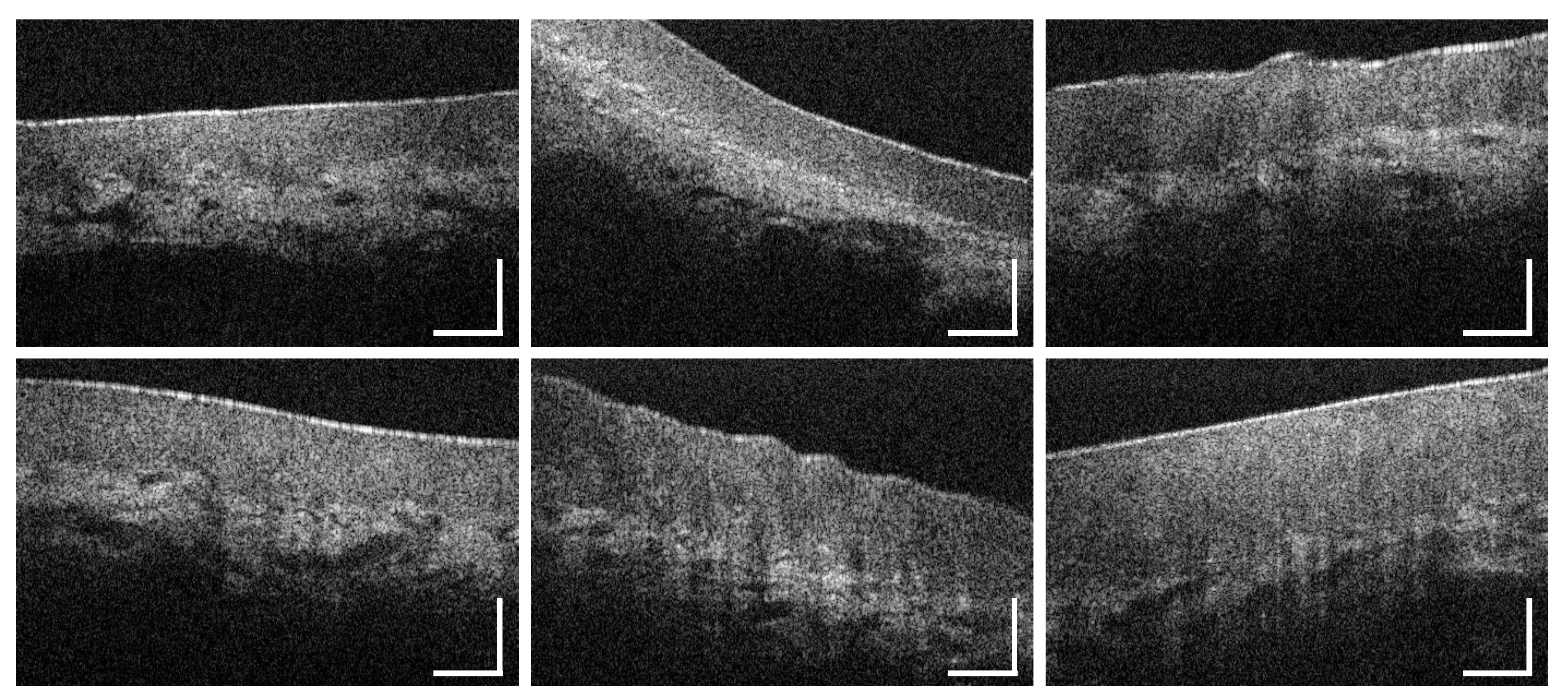
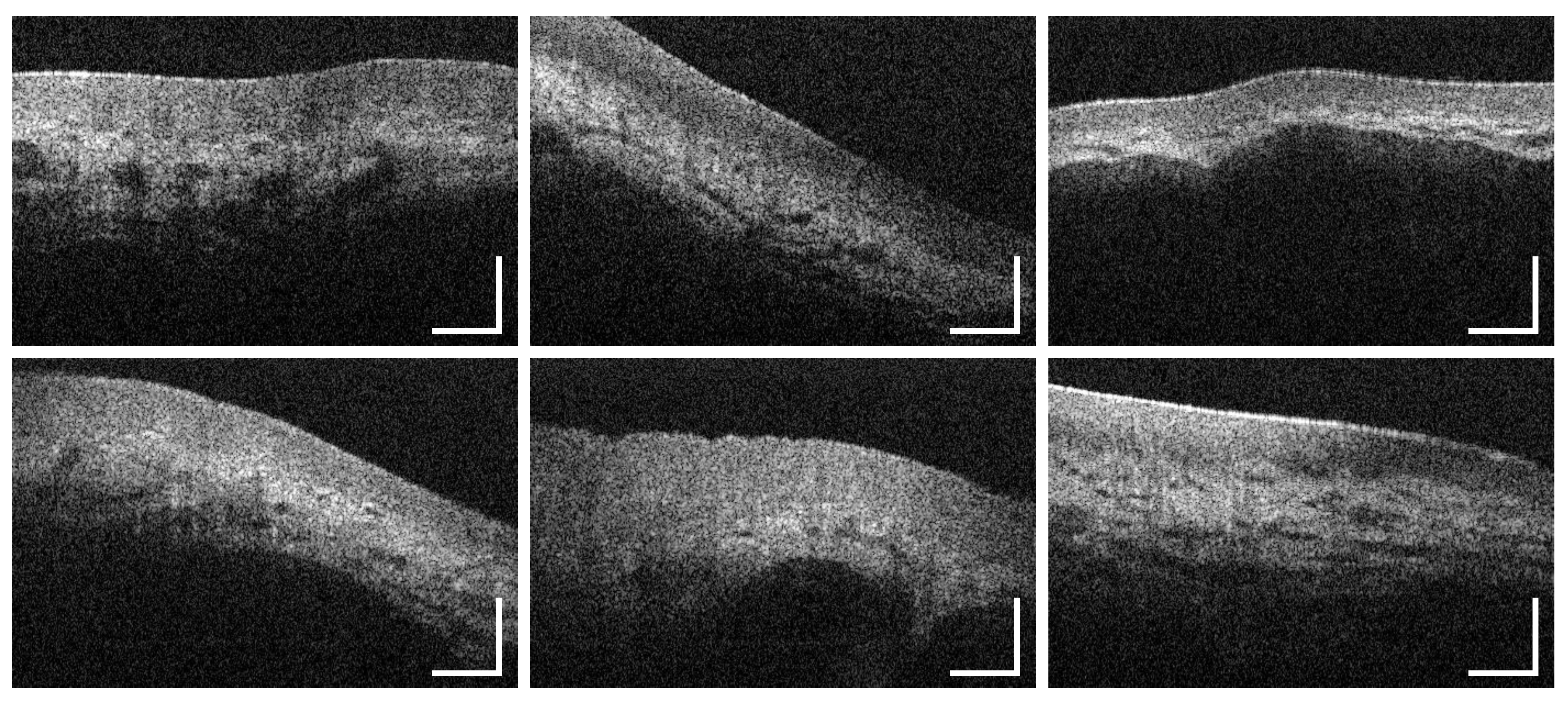
3.5. Soft Palate and Oropharynx
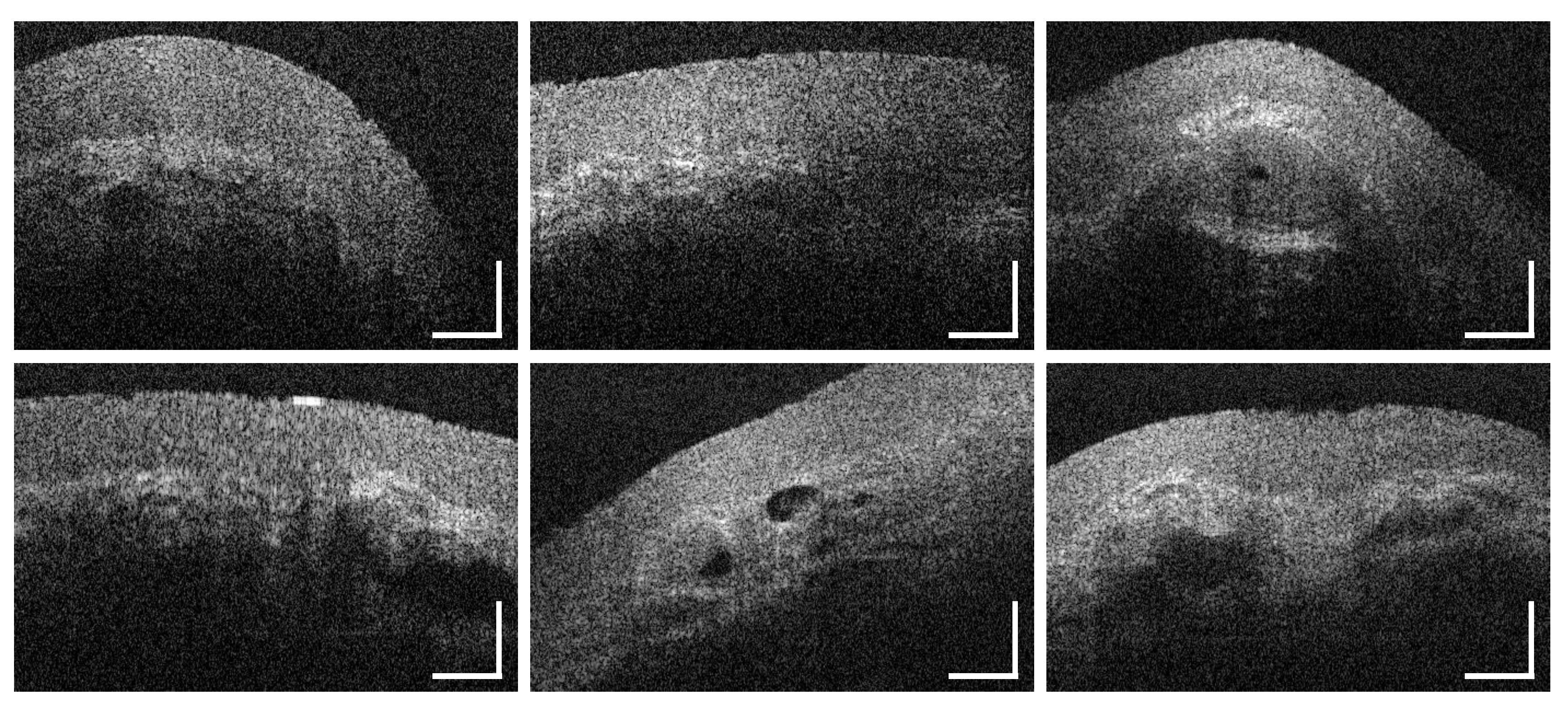
3.6. Palatine Tonsils
4. Discussion
5. Summary and Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A

| Measurement Point/Region | Sex Distribution | Age Group | Total | |||
|---|---|---|---|---|---|---|
| Male | Female | < 25 | 25–45 | > 45 | ||
| MP 1 | ||||||
| MP 2 | ||||||
| MP 3 | ||||||
| MP 4 | ||||||
| MP 5 | ||||||
| MP 6 | ||||||
| MP 7 | ||||||
| MP 8 | ||||||
| MP 9 | ||||||
| MP 10 | ||||||
| MP 11 | ||||||
| MP 12 | ||||||
| MP 13 | ||||||
| MP 14 | ||||||
| MP 15 | ||||||
| MP 16 | ||||||
| Labial mucosa | ||||||
| Alveolar mucosa | ||||||
| Buccal mucosa | ||||||
| Sublingual mucosa | ||||||
| Hard palate | ||||||
| Soft palate and oropharynx | ||||||
| Palatine tonsils | ||||||
| Measurement Point/Region | Vascularization |
|---|---|
| MP1 | |
| MP2 | |
| MP3 | |
| MP4 | |
| MP5 | |
| MP9 | |
| MP10 | |
| MP11 | |
| MP13 | |
| MP14 | |
| MP15 | |
| MP16 | |
| Labial mucosa | |
| Alveolar mucosa | |
| Sublingual mucosa | |
| Soft palate and oropharynx | |
| Palatine tonsils |
| Participant Number | Age Group | Sex | Measurement Point | Success Rate (%) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 3 | 4 | 2 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | ||||
| 1 | (1) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 2 | (1) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 3 | (1) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 4 | (1) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 5 | (1) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | x | 93.8 |
| 6 | (1) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 87.5 |
| 7 | (1) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 87.5 |
| 8 | (1) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 0 | 81.3 |
| 9 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 10 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 11 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 12 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 13 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 14 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 15 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 16 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | x | 93.8 |
| 17 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | x | 93.8 |
| 18 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 87.5 |
| 19 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 87.5 |
| 20 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 87.5 |
| 21 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 0 | 81.3 |
| 22 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 0 | 0 | 75.0 |
| 23 | (2) | m | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 0 | 0 | 75.0 |
| 24 | (3) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 25 | (3) | m | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 26 | (1) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 27 | (1) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 28 | (1) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 29 | (1) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | x | 93.8 |
| 30 | (1) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 0 | 81.3 |
| 31 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 32 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 33 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 34 | (1) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 35 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 36 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 37 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 38 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 39 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 40 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 41 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 42 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| 43 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | x | 93.8 |
| 44 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 87.5 |
| 45 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 87.5 |
| 46 | (2) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | 0 | 0 | 0 | 100 |
| 47 | (3) | f | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | 100 |
| Investigation area | Labial mucosa | Alveolar mucosa | Buccal mucosa | Sublingual mucosa | Hard palate | Soft palate/oropharynx | Palatine tonsil | ||||||||||||
| Success rate % | 100 | 100 | 100 | 100 | 100 | 95.7 | 85.1 | 61.7 | 72.3 | ||||||||||












References
- World Health Organization (WHO). Cancer Today—Data Visualization Tools for Exploring the Global Cancer Burden in 2018; World Health Organization (WHO): Geneva, Switzerland, 2019. [Google Scholar]
- Montero, P.H.; Patel, S.G. Cancer of the Oral Cavity. Surg. Oncol. Clin. N. Am. 2015, 24, 491–508. [Google Scholar] [CrossRef] [PubMed]
- Rivera, C.; Venegas, B. Histological and molecular aspects of oral squamous cell carcinoma. Oncol. Lett. 2014, 8, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Robert Koch-Institut; die Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V. Krebs in Deutschland für 2015/2016; Technical report; 2020; Available online: https://www.krebsdaten.de/Krebs/DE/Content/Publikationen/Krebs_in_Deutschland/krebs_in_deutschland_inhalt.html (accessed on 15 October 2020).
- Shield, K.D.; Ferlay, J.; Jemal, A.; Sankaranarayanan, R.; Chaturvedi, A.K.; Bray, F.; Soerjomataram, I. The global incidence of lip, oral cavity, and pharyngeal cancers by subsite in 2012. CA Cancer J. Clin. 2017, 67, 51–64. [Google Scholar] [CrossRef] [PubMed]
- de Martel, C.; Georges, D.; Bray, F.; Ferlay, J.; Clifford, G.M. Global burden of cancer attributable to infections in 2018: A worldwide incidence analysis. Lancet Glob. Health 2020, 8, e180–e190. [Google Scholar] [CrossRef]
- Deutsche Krebsgesellschaft; Deutsche Krebshilfe; AWMF. Konsultationsfassung S3-Leitlinie Diagnostik und Therapie des Mundhöhlenkarzinoms; Leitlinienprogramm Onkologie: Berlin, Germany, 2019; Volume 3.01, pp. 26–37. Available online: https://www.leitlinienprogramm-onkologie.de/fileadmin/user_upload/Downloads/Leitlinien/Mundhoehlenkarzinom/Version_3/LL_Mundhoehlenkarzinom_Langversion_Konsultationsfassung_3.01.pdf (accessed on 15 October 2020).
- Rivera, C. Essentials of oral cancer. Int. J. Clin. Exp. Pathol. 2015, 8, 11884–11894. [Google Scholar] [CrossRef]
- Avon, S.L.; Klieb, H.B. Oral soft-tissue biopsy: An overview. J. Can. Dent. Assoc. 2012, 78, 1–9. [Google Scholar]
- Kumaraswamy, K.L.; Vidhya, M.; Rao, P.K.; Mukanda, A. Oral biopsy: Oral pathologist’s perspective. J. Cancer Res. Ther. 2012, 8, 192–198. [Google Scholar] [CrossRef]
- Herranz González-Botas, J.; Varela Vázquez, P.; Vázquez Barro, C. Second primary tumours in head and neck cancer. Curr. Oncol. Rep. 2016, 67, 123–129. [Google Scholar] [CrossRef]
- Bhatia, N.; Lalla, Y.; Vu, A.N.; Farah, C.S. Advances in optical adjunctive aids for visualisation and detection of oral malignant and potentially malignant lesions. Int. J. Dent. 2013, 2013. [Google Scholar] [CrossRef]
- Huang, D.; Swanson, E.A.; Lin, C.P.L.; Schuman, J.S.; Stinson, W.G.; Chang, W.; Hee, M.R.; Flotte, T.; Gregory, K.; Puliafito, C.A.; et al. Optical coherence tomography (OCT). Science 1991, 254, 1178–1181. [Google Scholar] [CrossRef]
- Wilder-Smith, P.; Holtzman, J.; Epstein, J.; Le, A. Optical diagnostics in the oral cavity: An overview. Oral Dis. 2010, 16, 717–728. [Google Scholar] [CrossRef] [PubMed]
- Gora, M.J.; Suter, M.J.; Tearney, G.J.; Li, X. Endoscopic optical coherence tomography: Technologies and clinical applications [Invited]. Biomed. Opt. Express 2017, 8, 2405–2444. [Google Scholar] [CrossRef] [PubMed]
- Higgins, L.M.; Pierce, M.C. Design and characterization of a handheld multimodal imaging device for the assessment of oral epithelial lesions. J. Biomed. Opt. 2014, 19, 086004. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gentile, E.; Maio, C.; Romano, A.; Laino, L.; Lucchese, A. The potential role of in vivo optical coherence tomography for evaluating oral soft tissue: A systematic review. J. Oral Pathol. Med. 2017, 46, 864–876. [Google Scholar] [CrossRef] [PubMed]
- Matheny, E.S.; Hanna, N.M.; Jung, W.G.; Chen, Z.; Wilder-Smith, P.; Mina-Araghi, R.; Brenner, M. Optical coherence tomography of malignancy in hamster cheek pouches. J. Biomed. Opt. 2004, 9, 978. [Google Scholar] [CrossRef]
- Wilder-Smith, P.; Lee, K.; Guo, S.; Zhang, J.; Osann, K.; Chen, Z.; Messadi, D. In vivo diagnosis of oral daysplasia and malignancy using optical coherence tomography: Preliminary studies in 50 Patients. Lasers Surg. Med. 2009, 41, 353–357. [Google Scholar] [CrossRef]
- Hamdoon, Z.; Jerjes, W.; Upile, T.; McKenzie, G.; Jay, A.; Hopper, C. Optical coherence tomography in the assessment of suspicious oral lesions: An immediate ex vivo study. Photodiagnosis Photodyn. Ther. 2013, 10, 17–27. [Google Scholar] [CrossRef]
- Volgger, V.; Stepp, H.; Ihrler, S.; Kraft, M.; Leunig, A.; Patel, P.M.; Susarla, M.; Jackson, K.; Betz, C.S. Evaluation of optical coherence tomography to discriminate lesions of the upper aerodigestive tract. Head Neck 2012, 35, 1558–1566. [Google Scholar] [CrossRef]
- Tsai, M.T.; Lee, C.K.; Lee, H.C.; Wang, Y.M.; Yang, C.C.; Chiang, C.P. Effective indicators for oral cancer diagnosis based on optical coherence tomography. Opt. Infobase Conf. Pap. 2008, 16, 15847–15862. [Google Scholar] [CrossRef]
- Tsai, M.T.; Lee, C.K.; Lee, H.C.; Chen, H.M.; Chiang, C.P.; Wang, Y.M.; Yang, C.C. Differentiating oral lesions in different carcinogenesis stages with optical coherence tomography. J. Biomed. Opt. 2009, 14, 044028. [Google Scholar] [CrossRef]
- Lee, C.K.; Chi, T.T.; Wu, C.T.; Tsai, M.T.; Chiang, C.P.; Yang, C.C.C.C. Diagnosis of oral precancer with optical coherence tomography. Biomed. Opt. Express 2012, 3, 1632. [Google Scholar] [CrossRef] [PubMed]
- Prestin, S.; Rothschild, S.I.; Betz, C.S.; Kraft, M. Measurement of epithelial thickness within the oral cavity using optical coherence tomography. Head Neck 2012, 34, 1777–1781. [Google Scholar] [CrossRef] [PubMed]
- Ridgeway, J.M.; Armstrong, W.B.; Guo, S.; Mahmood, U.; Su, J.; Jackson, R.P.; Shibuya, T.; Crumley, R.L.; Gu, M.; Chen, Z.; et al. In vivo optical coherence tomography of the human oral cavity and oropharynx. Arch. Otolaryngol.—Head Neck Surg. 2006, 132, 1074–1081. [Google Scholar] [CrossRef] [PubMed]
- Di Stasio, D.; Lauritano, D.; Iquebal, H.; Romano, A.; Gentile, E.; Lucchese, A. Measurement of oral epithelial thickness by optical coherence tomography. Diagnostics 2019, 9, 90. [Google Scholar] [CrossRef] [PubMed]
- Pande, P.; Shrestha, S.; Park, J.; Serafino, M.J.; Gimenez-Conti, I.; Brandon, J.; Cheng, Y.S.; Applegate, B.E.; Jo, J.A. Automated classification of optical coherence tomography images for the diagnosis of oral malignancy in the hamster cheek pouch. J. Biomed. Opt. 2014, 19, 086022. [Google Scholar] [CrossRef][Green Version]
- Goldan, R.N.; Lee, A.; Cahill, L.C.; Liu, K.Y.; MacAulay, C.E.; Poh, C.F.; Lane, P.M. Automated Segmentation of Oral Mucosa from Wide-Field OCT Images (Conference Presentation). In Advanced Biomedical and Clinical Diagnostic and Surgical Guidance Systems XIV; International Society for Optics and Photonics: Bellingham, WA, USA, 2016; p. 25. [Google Scholar] [CrossRef]
- Wei, W.; Choi, W.J.; Wank, R.K. Microvascular imaging and monitoring of human oral cavity lesions in vivo by swept-source OCT based angiography. Lasers Med Sci. 2018, 33, 123–134. [Google Scholar] [CrossRef]
- de Boer, J.F.; Hitzenberger, C.K.; Yasuno, Y. Polarization sensitive optical coherence tomography—A review [Invited]. Biomed. Opt. Express 2017, 8, 1838–1873. [Google Scholar] [CrossRef]
- Walther, J.; Golde, J.; Kirsten, L.; Tetschke, F.; Hempel, F.; Rosenauer, T.; Hannig, C.; Koch, E. In vivo imaging of human oral hard and soft tissues by polarization-sensitive optical coherence tomography. J. Biomed. Opt. 2017, 22, 1–17. [Google Scholar] [CrossRef]
- Walther, J.; Li, Q.; Villiger, M.; Farah, C.S.; Koch, E.; Karnowski, K.; Sampson, D.D. Depth-resolved birefringence imaging of collagen fiber organization in the human oral mucosa in vivo. Biomed. Opt. Express 2019, 10, 1942. [Google Scholar] [CrossRef] [PubMed]
- Burger, M.; Brönstrup, A.; Pietrzik, K. Derivation of tolerable upper alcohol intake levels in Germany: A systematic review of risks and benefits of moderate alcohol consumption. Prev. Med. 2004, 39, 111–127. [Google Scholar] [CrossRef]
- Hashibe, M.; Brennan, P.; Benhamou, S.; Castellsague, X.; Chen, C.; Curado, M.P.; Maso, L.D.; Daudt, A.W.; Fabianova, E.; Wünsch-Filho, V.; et al. Alcohol drinking in never users of tobacco, cigarette smoking in never drinkers, and the risk of head and neck cancer: Pooled analysis in the international head and neck cancer epidemiology consortium. J. Natl. Cancer Inst. 2007, 99, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Walther, J.; Schnabel, C.; Tetschke, F.; Rosenauer, T.; Golde, J.; Ebert, N.; Baumann, M.; Hannig, C.; Koch, E. In vivo imaging in the oral cavity by endoscopic optical coherence tomography. J. Biomed. Opt. 2018, 23, 071207. [Google Scholar] [CrossRef]
- Walther, J.; Krüger, A.; Cuevas, M.; Koch, E. Effects of axial, transverse, and oblique sample motion in FD OCT in systems with global or rolling shutter line detector. J. Opt. Soc. Am. 2008, 25, 2791. [Google Scholar] [CrossRef]
- Abràmoff, M.D.; Magalhães, P.J.; Ram, S.J. Image processing with imageJ. Biophotonics Int. 2004, 11, 36–41. [Google Scholar] [CrossRef]
- Curl, C.L.; Bellair, C.J.; Harris, T.; Allman, B.E.; Harris, P.J.; Stewart, A.G.; Roberts, A.; Nugent, K.A.; Delbridge, L.M. Refractive index measurement in viable cells using quantitative phase-amplitude microscopy and confocal microscopy. Cytom. Part A 2005, 65, 88–92. [Google Scholar] [CrossRef]
- Tsai, M.T.; Chen, Y.; Lee, C.Y.; Huang, B.H.; Trung, N.H.; Lee, Y.J.; Wang, Y.L. Noninvasive structural and microvascular anatomy of oral mucosae using handheld optical coherence tomography. Biomed. Opt. Express 2017, 8, 5001–5012. [Google Scholar] [CrossRef]
- Maslennikova, A.V.; Sirotkina, M.A.; Moiseev, A.A.; Finagina, E.S.; Ksenofontov, S.Y.; Gelikonov, G.V.; Matveev, L.A.; Kiseleva, E.B.; Zaitsev, V.Y.; Zagaynova, E.V.; et al. In-vivo longitudinal imaging of microvascular changes in irradiated oral mucosa of radiotherapy cancer patients using optical coherence tomography. Sci. Rep. 2017, 7, 16505. [Google Scholar] [CrossRef] [PubMed]
- Grulkowski, I.; Nowak, J.K.; Karnowski, K.; Zebryk, P.; Puszczewicz, M.; Walkowiak, J.; Wojtkowski, M. Quantitative assessment of oral mucosa and labial minor salivary glands in patients with Sjögren’s syndrome using swept source OCT. Biomed. Opt. Express 2014, 5, 259–274. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pahlevaninezhad, H.; Lee, A.M.; Rosin, M.; Sun, I.; Zhang, L.; Hakimi, M.; MacAulay, C.; Lane, P.M. Optical coherence tomography and autofluorescence imaging of human tonsil. PLoS ONE 2014, 9, e115889. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Institute of Anatomy, Faculty of Medicine, Technische Universitaet Dresden. Virtual Database—Histological Cross Sections of the Healthy Human Oral Mucosa; Institute of Anatomy, Faculty of Medicine, Technische Universitaet Dresden: Dresden, Germany, 2020. [Google Scholar]
- Otis, L.L.; Piao, D.; Gibson, C.W.; Zhu, Q. Quantifying labial blood flow using optical Doppler tomography. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2004, 98, 189–194. [Google Scholar] [CrossRef]
- Squier, C.; Brogden, K.A. Human Oral Mucosa—Development, Structure & Function; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2011. [Google Scholar] [CrossRef]
- Kessler, A.T.; Bhatt, A.A. Review of the Major and Minor Salivary Glands, Part 1: Anatomy, Infectious, and Inflammatory Processes. J. Clin. Imaging Sci. 2018, 8, 47. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Kwon, Y.H.; Park, J.B.; Herr, Y.; Shin, S.I.; Heo, S.J.; Chung, J.H. Epithelial Thickness of the Palatal Mucosa: A Histomorphometric Study in Koreans. Anat. Rec. 2010, 293, 1966–1970. [Google Scholar] [CrossRef] [PubMed]
- Harada, K. The histopathological study of human palatine tonsils—Especially age changes. Nihon Jibiinkoka Gakkai Kaiho 1989, 92, 1049–1064. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pai, S.I.; Westra, W.H. Molecular Pathology of Head and Neck Cancer: Implications for Diagnosis, Prognosis, and Treatment. Annu. Rev. Pathol. 2009, 4, 49–70. [Google Scholar] [CrossRef]
- Landay, M.A.; Schroeder, H.E. Quantitative electron microscopic analysis of the stratified epithelium of normal human buccal mucosa. Cell Tissue Res. 1977, 177, 383–405. [Google Scholar] [CrossRef]
- Singhal, P.; Singh, N.N.; Sreedhar, G.; Banerjee, S.; Batra, M.; Garg, A. Evaluation of histomorphometric changes in tissue architecture in relation to alteration in fixation protocol—An invitro study. J. Clin. Diagn. Res. 2016, 10, ZC28–ZC32. [Google Scholar] [CrossRef]
- Hand, A.R.; Pathmanathan, D.; Field, R.B. Morphological features of the minor salivary glands. Arch. Oral Biol. 1999, 44, S3–S10. [Google Scholar] [CrossRef]

| Criterion | Evaluation |
|---|---|
| Surface integrity | intact/with alterations |
| Surface profile | even/uneven |
| Epithelial homogeneity | homogeneous/inhomogeneous |
| Epithelial thickness | mean value of 25 measurements () |
| Basement membrane | intact/unsharp/not assessable |
| Tissue vascularization | low (<0.10)/moderate (0.10–0.30)/high (>0.30) |
| Additional components | Description of regional features within the lamina propria |
| Study Population | OCT Cross Sections | ||
|---|---|---|---|
| Nb. of volunteers | 47 | Investigation area | Nb. of images |
| Male | 25 (53.2%) | ||
| Female | 22 (46.8%) | Labial mucosa | 705 |
| Mean age (years) | 29.36 | Alveolar mucosa | 470 |
| <25 years | 14 (29.8%) | Buccal mucosa | 705 |
| 25–45 years | 30 (63.8%) | Sublingual mucosa | 705 |
| >45 years | 3 (6.4%) | Hard palate | 235 |
| Oral symptoms/lesions | 0 | Soft palate & oropharynx | 570 |
| Alcohol intake > TL 1 | 0 | Palatine tonsils | 170 |
| Never drinking | 19 (40.4%) | ||
| Tobacco consumption > TL 1 | 0 | Total | 3,560 |
| Never smoking | 20 (42.6%) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Albrecht, M.; Schnabel, C.; Mueller, J.; Golde, J.; Koch, E.; Walther, J. In Vivo Endoscopic Optical Coherence Tomography of the Healthy Human Oral Mucosa: Qualitative and Quantitative Image Analysis. Diagnostics 2020, 10, 827. https://doi.org/10.3390/diagnostics10100827
Albrecht M, Schnabel C, Mueller J, Golde J, Koch E, Walther J. In Vivo Endoscopic Optical Coherence Tomography of the Healthy Human Oral Mucosa: Qualitative and Quantitative Image Analysis. Diagnostics. 2020; 10(10):827. https://doi.org/10.3390/diagnostics10100827
Chicago/Turabian StyleAlbrecht, Marius, Christian Schnabel, Juliane Mueller, Jonas Golde, Edmund Koch, and Julia Walther. 2020. "In Vivo Endoscopic Optical Coherence Tomography of the Healthy Human Oral Mucosa: Qualitative and Quantitative Image Analysis" Diagnostics 10, no. 10: 827. https://doi.org/10.3390/diagnostics10100827
APA StyleAlbrecht, M., Schnabel, C., Mueller, J., Golde, J., Koch, E., & Walther, J. (2020). In Vivo Endoscopic Optical Coherence Tomography of the Healthy Human Oral Mucosa: Qualitative and Quantitative Image Analysis. Diagnostics, 10(10), 827. https://doi.org/10.3390/diagnostics10100827





