Triple Pulmonary Coinfection with SARS-CoV-2, Nocardia cyriacigeorgica, and Aspergillus fumigatus Causing Necrotizing Pneumonia in an Immunomodulated Rheumatoid Arthritis Patient: Diagnostic and Therapeutic Insights
Abstract
1. Introduction
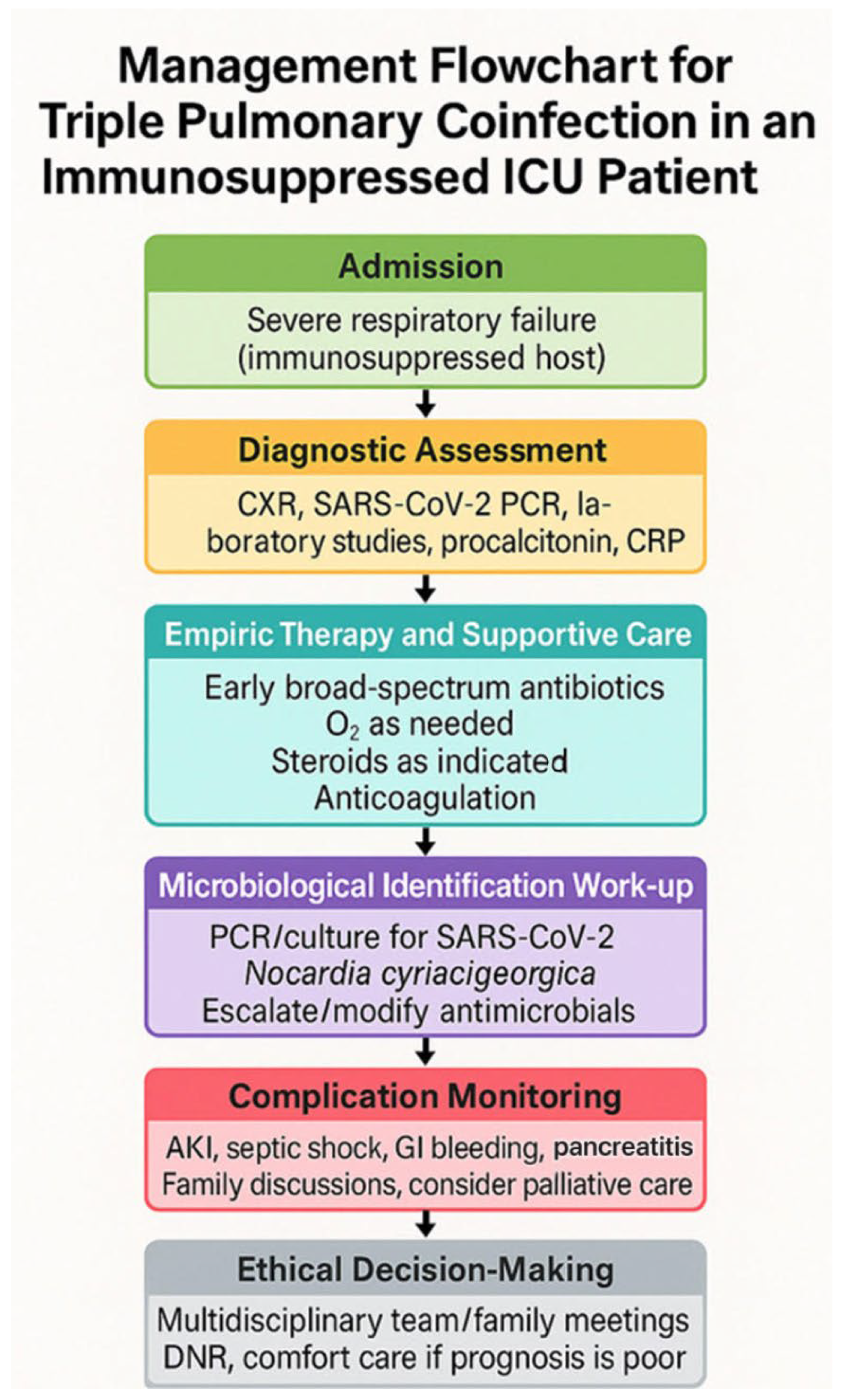
2. Case Presentation
2.1. Patient History and Initial Assessment
2.2. ICU Management, Diagnostic Work-Up, and Course
- Nocardia cyriacigeorgica in sputum cultures (19 December 2023; 20 December 2023) and BAL (20 December 2023), confirmed by MALDI-TOF and susceptibility testing.
- Aspergillus fumigatus from BAL, with a positive galactomannan antigen (0.60, elevated), and positive fungal culture.
- COVID-19 PCR and antigen tests remained positive until 21 December 2023.
- Blood cultures remained negative throughout admission.
- Multiplex PCR panels for tuberculosis, Pneumocystis jirovecii, CMV, and HSV were negative.
- No Clostridium difficile or other major pathogens were identified in stool testing.
2.3. Complications, Supportive Care, and Ethical Considerations
- Septic shock (24–25 December 2023): This required the escalation of vasopressor support (norepinephrine and vasopressin). The family declined further escalation (second-line vasopressors).
- Acute kidney injury with anuria and severe hyperkalemia (up to 6.9 mmol/L): The family declined hemodialysis.
- Metabolic acidosis and persistent normocytic anemia: This required multiple packed red blood cell transfusions (19 December 2023; 24 December 2023; 25 December 2023; 28 December 2023).
- Profound hypothermia (25–27 December 2023).
- Gastrointestinal bleeding: Coffee-ground and subsequently dark red gastric aspirates were found on 27 December 2023, likely secondary to a stress-related ulcer.
- Acute pancreatitis: This was diagnosed by markedly elevated amylase (5664 U/L) and lipase (>2000 U/L) on 29 December 2023; abdominal ultrasound showed pancreatic edema and peripheral fluid accumulation.
- Transient bilateral pupil dilation without light reflex (25–27 December 2023): Neurological imaging was deferred due to the family’s preference for palliative care and avoidance of high-risk transport.
- Pressure ulcers and skin breakdown: These were managed by ICU nursing staff with standard wound care protocols.
- Ventilator management: Progressive hypoxemia required adjustments in ventilator settings, with increasing FiO2 and inspiratory pressure, but oxygenation continued to deteriorate.
2.4. Clinical Timeline and Key Data
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ye, J.; Li, Y.; Hao, J.; Song, M.; Guo, Y.; Gao, W.; Zheng, C.; Huang, Y.; Feng, Z.; Zhang, L. Rare occurrence of pulmonary coinfection involving Aspergillus fumigatus and Nocardia cyriacigeorgica in immunocompetent patients based on NGS: A case report and literature review. Medicine 2023, 102, e36692. [Google Scholar] [CrossRef]
- Wang, L.; Liu, Y.; Li, H. Co-infection of Nocardia and Aspergillus fumigatus in an immunosuppressed patient. Medicine 2024, 103, e37073. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Salmanton-García, J.; Sprute, R.; Stemler, J.; Bartoletti, M.; Dupont, D.; Valerio, M.; Garcia-Vidal, C.; Falces-Romero, I.; Machado, M.; de La Villa, S.; et al. COVID-19–Associated Pulmonary Aspergillosis, March–August 2020. Emerg. Infect. Dis. 2021, 27, 1077–1086. [Google Scholar] [CrossRef] [PubMed]
- Feldman, C.; Anderson, R. The role of co-infections and secondary infections in patients with COVID-19. Pneumonia 2021, 13, 5. [Google Scholar] [CrossRef]
- Strangfeld, A.; Schäfer, M.; Gianfrancesco, M.A.; Lawson-Tovey, S.; Liew, J.W.; Ljung, L.; Mateus, E.F.; Richez, C.; Santos, M.J.; Schmajuk, G.; et al. Factors associated with COVID-19-related death in people with rheumatic diseases: Results from the COVID-19 Global Rheumatology Alliance. Ann. Rheum. Dis. 2021, 80, 930–942. [Google Scholar] [CrossRef]
- Kandi, V.; Kollipara, R.; Manne, M.; Puvvada, S.; Koganti, M.V.; Taduri, S.R.; Imran, M.; Bharadwaj, S.; Balla, S.; Reddy, V.B.; et al. Nocardia infections in humans: A review. Braz. J. Microbiol. 2016, 47, 31–40. [Google Scholar] [CrossRef]
- Figueroa-Parra, G.; Gilbert, E.L.; Valenzuela-Almada, M.O.; Vallejo, S.; Neville, M.R.; Patel, N.J.; Cook, C.; Fu, X.; Hagi, R.; McDermott, G.C.; et al. Risk of severe COVID-19 outcomes associated with rheumatoid arthritis and phenotypic subgroups: A retrospective, comparative, multicentre cohort study. Lancet Rheumatol. 2022, 4, e765–e774. [Google Scholar] [CrossRef]
- Lansbury, L.; Lim, B.; Baskaran, V.; Lim, W.S. Co-infections in people with COVID-19: A systematic review and meta-analysis. J. Infect. 2020, 81, 266–275. [Google Scholar] [CrossRef]
- Brown-Elliott, B.A.; Brown, J.M.; Conville, P.S.; Wallace, R.J., Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin. Microbiol. Rev. 2006, 19, 259–282. [Google Scholar] [CrossRef]
- Yagi, K.; Ishii, M.; Namkoong, H.; Asami, T.; Fujiwara, H.; Nishimura, T.; Saito, F.; Kimizuka, Y.; Asakura, T.; Suzuki, S.; et al. Pulmonary nocardiosis caused by Nocardia cyriacigeorgica in patients with Mycobacterium avium complex lung disease: Two case reports. BMC Infect. Dis. 2014, 14, 684. [Google Scholar] [CrossRef]
- Wilson, J.W. Nocardiosis: Updates and clinical overview. In Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 2012; Volume 87, pp. 403–407. [Google Scholar] [CrossRef]
- Beaman, B.L.; Beaman, L. Nocardia species: Host-parasite relationships. Clin. Microbiol. Rev. 1994, 7, 213–264. [Google Scholar] [CrossRef] [PubMed]
- Woods, C.R. Nocardia cyriacigeorgica: An emerging cause of nocardiosis. Infect. Dis. Clin. Pract. 2021, 29, 73–79. [Google Scholar] [CrossRef]
- Bartoletti, M.; Pascale, R.; Cricca, M.; Maccaro, A.; Bussini, L.; Fornaro, G.; Tonetti, T.; Pizzilli, G.; Francalanci, E.; Giuntoli, L.; et al. Epidemiology of invasive pulmonary aspergillosis among COVID-19 intubated patients: A prospective study. Clin. Infect. Dis. 2021, 73, e3606–e3614. [Google Scholar] [CrossRef] [PubMed]
- Koehler, P.; Bassetti, M.; Chakrabarti, A.; Chen, S.C.; Colombo, A.L.; Hoenigl, M.; Klimko, N.; Lass-Flörl, C.; Oladele, R.O.; Vinh, D.C.; et al. Defining and managing COVID-19-associated pulmonary aspergillosis: The 2020 ECMM/ISHAM consensus criteria. Lancet Infect. Dis. 2021, 21, e149–e162. [Google Scholar] [CrossRef]
- Segrelles-Calvo, G.; Araújo, G.R.; Llopis-Pastor, E.; Carrillo, J.; Hernández-Hernández, M.; Rey, L.; Rodríguez Melean, N.; Escribano, I.; Antón, E.; Zamarro, C.; et al. Prevalence of opportunistic invasive aspergillosis in COVID-19 patients with severe pneumonia. Mycoses 2021, 64, 144–151. [Google Scholar] [CrossRef]
- Donnelly, J.P.; Chen, S.C.; Kauffman, C.A.; Steinbach, W.J.; Baddley, J.W.; Verweij, P.E.; Clancy, C.J.; Wingard, J.R.; Lockhart, S.R.; Groll, A.H.; et al. Revision and Update of the Consensus Definitions of Invasive Fungal Disease from the EORTC/MSGERC. Clin. Infect. Dis. 2020, 71, 1367–1376. [Google Scholar] [CrossRef]
- van de Veerdonk, F.L.; Kolwijck, E.; Lestrade, P.P.; Hodiamont, C.J.; Rijnders, B.J.; Van Paassen, J.; Haas, P.-J.; Oliveira dos Santos, C.; Kampinga, G.A.; Bergmans, D.C.; et al. Influenza-associated aspergillosis in critically ill patients. Am. J. Respir. Crit. Care Med. 2017, 196, 524–527. [Google Scholar] [CrossRef]
- Bassetti, M.; Azoulay, E.; Kullberg, B.-J.; Ruhnke, M.; Shoham, S.; Vazquez, J.; Giacobbe, D.R.; Calandra, T. EORTC/MSGERC definitions and management of invasive fungal diseases in critically ill patients. Intensive Care Med. 2019, 45, 512–525. [Google Scholar]
- McGonagle, D.; Sharif, K.; O’Regan, A.; Bridgewood, C. The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun. Rev. 2020, 19, 102537. [Google Scholar] [CrossRef]
- Truog, R.D.; Campbell, M.L.; Curtis, J.R.; Haas, C.E.; Luce, J.M.; Rubenfeld, G.D.; Rushton, C.H.; Kaufman, D.C. Recommendations for end-of-life care in the intensive care unit: A consensus statement. Crit. Care Med. 2008, 36, 953–963. [Google Scholar] [CrossRef]
- Kon, A.A.; Davidson, J.E.; Morrison, W.; Danis, M.; White, D.B.; American College of Critical Care Medicine; American Thoracic Society. Shared decision-making in ICUs: An American College of Critical Care Medicine and American Thoracic Society Policy Statement. Crit. Care Med. 2016, 44, 188–201. [Google Scholar] [CrossRef]
- Musuuza, J.S.; Watson, L.; Parmasad, V.; Putman-Buehler, N.; Christensen, L.; Safdar, N. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0251170. [Google Scholar] [CrossRef]
- Gianfrancesco, M.A.; Hyrich, K.L.; Al-Adely, S.; Carmona, L.; Danila, M.I.; Gossec, L.; Izadi, Z.; Jacobsohn, L.; Katz, P.; Lawson-Tovey, S.; et al. Characteristics associated with hospitalisation for COVID-19 in people with rheumatic disease. Ann. Rheum. Dis. 2020, 79, 859–866. [Google Scholar] [CrossRef]
| Date | Event/Findings | Labs/Imaging | Microbiology | Intervention |
|---|---|---|---|---|
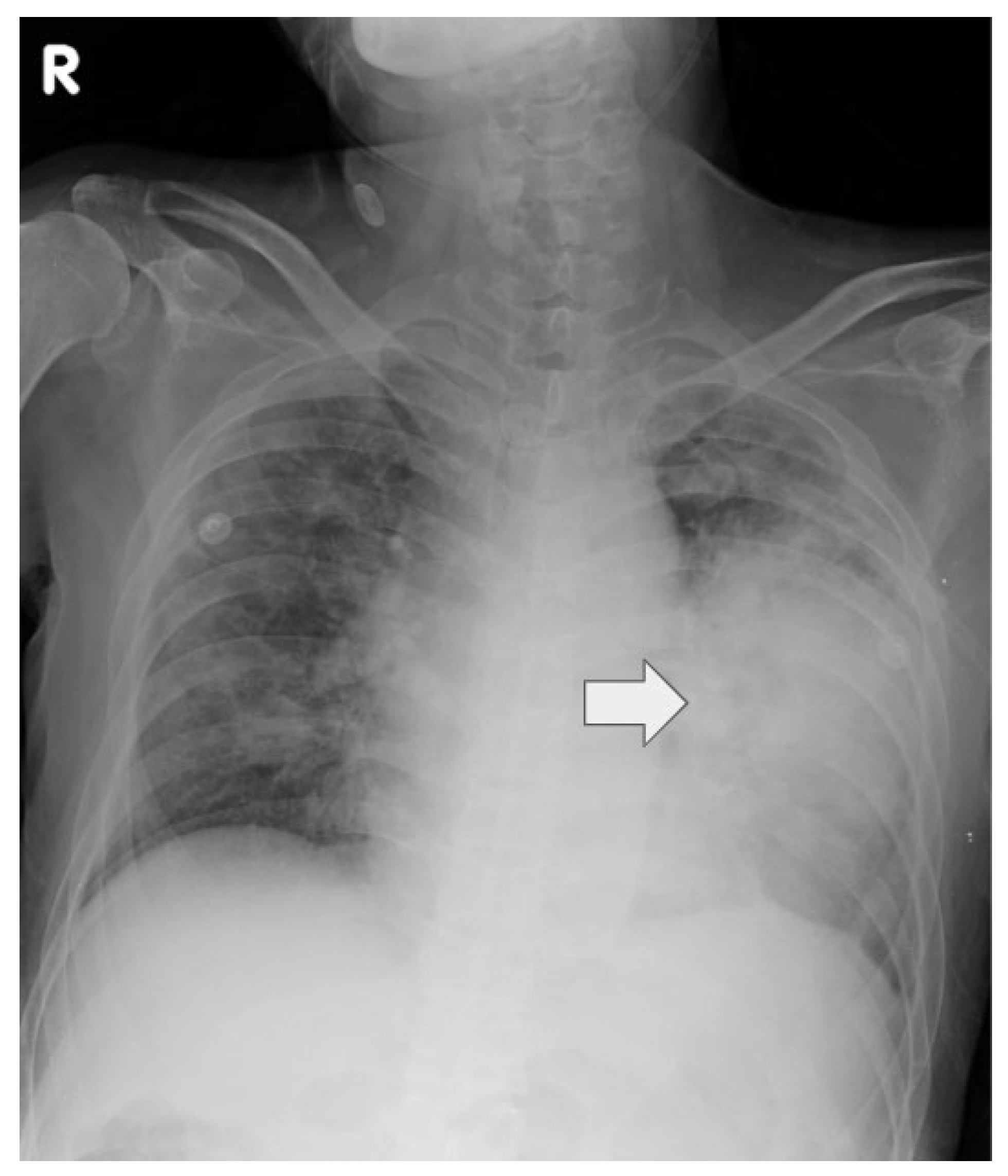
| 12/16 | Admission, intubation | CXR: bilateral pneumonia | — | Empiric abx, ICU admit |
| 12/18 | COVID PCR+, consult | CT: necrosis | Sputum: Nocardia cyriacigeorgica | Remdesivir, steroids |
| 12/19 | COVID PCR+, culture | — | Sputum: Nocardia cyriacigeorgica | TMP-SMX, Linezolid |
| 12/20 | BAL performed | — | BAL: Aspergillus fumigatus | Voriconazole |
| 12/24 | Septic shock | Labs: AKI, shock | — | Vasopressors |
| 12/27 | GI bleeding | — | — | PRBC transfusion |
| 12/29 | Acute pancreatitis | Abd Sono: edema | — | Supportive |
| 12/31 | Multi-organ failure | — | — | Comfort care, expired |
| Date | WBC (×103/µL) | Hb (g/dL) | Cr (mg/dL) | CRP (mg/dL) | K+ (mmol/L) | pH | Comment |
|---|---|---|---|---|---|---|---|
| 12/16 | 21.6 | 9.6 | 1.4 | 33.1 | 4.2 | 7.26 | ICU admission |
| 12/18 | 18.5 | 9.2 | 1.1 | 28.7 | 4.5 | 7.32 | Post-intubation |
| 12/19 | 17.3 | 8.7 | 1.2 | 24.0 | 4.7 | 7.33 | PRBC 2U, Remdesivir |
| 12/24 | 15.1 | 8.2 | 2.0 | 22.0 | 5.3 | 7.25 | Septic shock onset |
| 12/25 | 14.5 | 7.9 | 2.4 | 21.0 | 5.5 | 7.22 | PRBC 1U, shock |
| 12/28 | 12.8 | 7.8 | 3.5 | 18.4 | 5.8 | 7.18 | Anuria, PRBC 2U |
| 12/29 | 13.0 | 7.8 | 3.4 | 17.9 | 5.9 | 7.21 | Acute pancreatitis |
| 12/30 | 12.5 | 7.6 | 3.4 | 16.0 | 6.3 | 7.16 | Hyperkalemia |
| 12/31 | 11.8 | 7.2 | 3.4 | 15.7 | 6.9 | 7.10 | Pre-mortem |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, W.-H.; Hu, T.-Y.; Kuo, L.-K. Triple Pulmonary Coinfection with SARS-CoV-2, Nocardia cyriacigeorgica, and Aspergillus fumigatus Causing Necrotizing Pneumonia in an Immunomodulated Rheumatoid Arthritis Patient: Diagnostic and Therapeutic Insights. Life 2025, 15, 1336. https://doi.org/10.3390/life15091336
Chang W-H, Hu T-Y, Kuo L-K. Triple Pulmonary Coinfection with SARS-CoV-2, Nocardia cyriacigeorgica, and Aspergillus fumigatus Causing Necrotizing Pneumonia in an Immunomodulated Rheumatoid Arthritis Patient: Diagnostic and Therapeutic Insights. Life. 2025; 15(9):1336. https://doi.org/10.3390/life15091336
Chicago/Turabian StyleChang, Wei-Hung, Ting-Yu Hu, and Li-Kuo Kuo. 2025. "Triple Pulmonary Coinfection with SARS-CoV-2, Nocardia cyriacigeorgica, and Aspergillus fumigatus Causing Necrotizing Pneumonia in an Immunomodulated Rheumatoid Arthritis Patient: Diagnostic and Therapeutic Insights" Life 15, no. 9: 1336. https://doi.org/10.3390/life15091336
APA StyleChang, W.-H., Hu, T.-Y., & Kuo, L.-K. (2025). Triple Pulmonary Coinfection with SARS-CoV-2, Nocardia cyriacigeorgica, and Aspergillus fumigatus Causing Necrotizing Pneumonia in an Immunomodulated Rheumatoid Arthritis Patient: Diagnostic and Therapeutic Insights. Life, 15(9), 1336. https://doi.org/10.3390/life15091336






