High-Flow Nasal Cannula in Weaning Patients from Mechanical Ventilation in Head and Neck Surgery: Retrospective Study
Abstract
1. Introduction
2. Methods
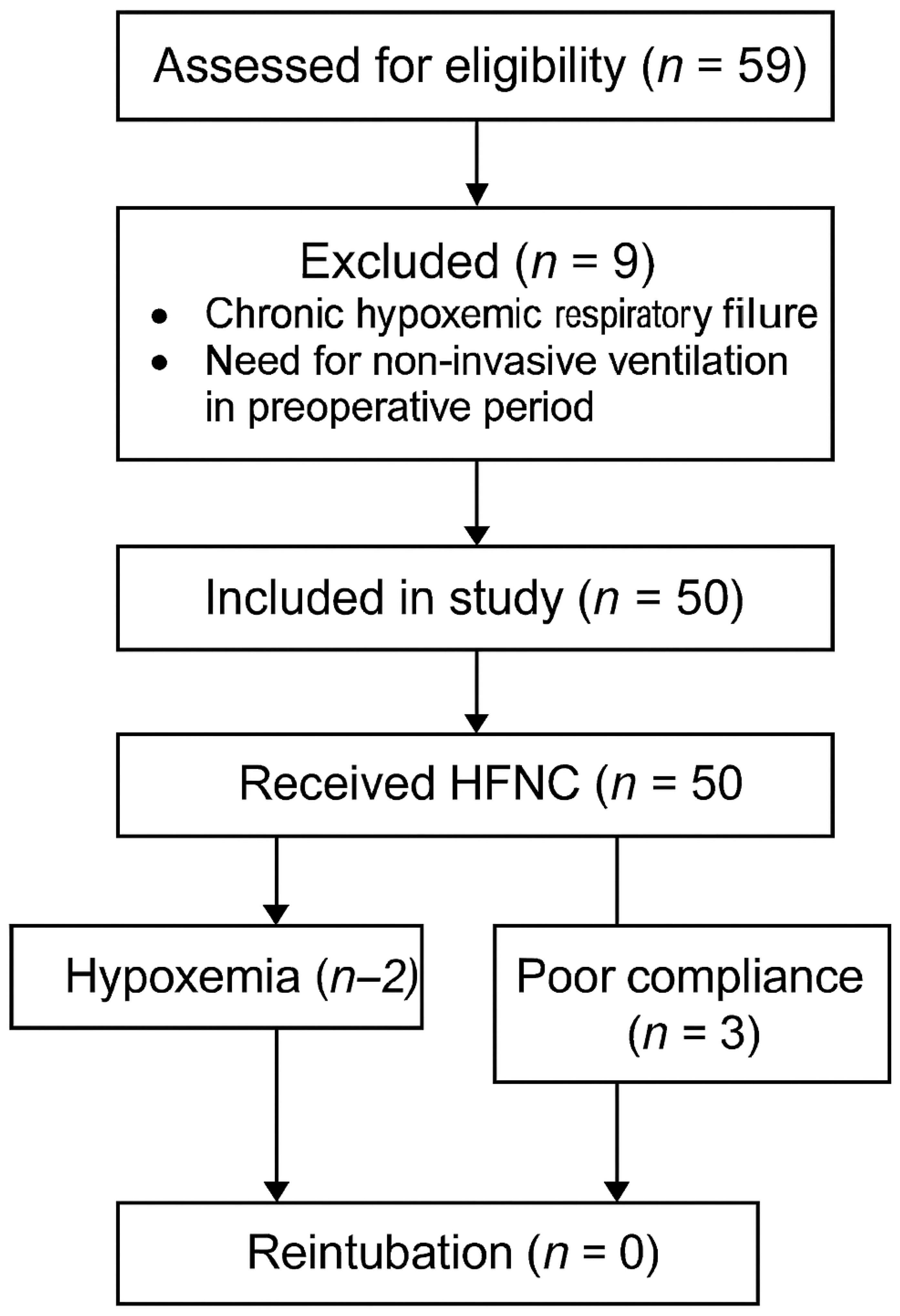
- Patients extubated after head and neck cancer ablation with concomitant free flap reconstruction surgery and admitted to the ICU.
- Application of HFNC.
- Adults over 18 years of age who were able to provide consent.
- Exclusion criteria included the following:
- Chronic hypoxiemic disease.
- Need of non-invasive ventilation during the preoperative period.
3. Statistical Analysis
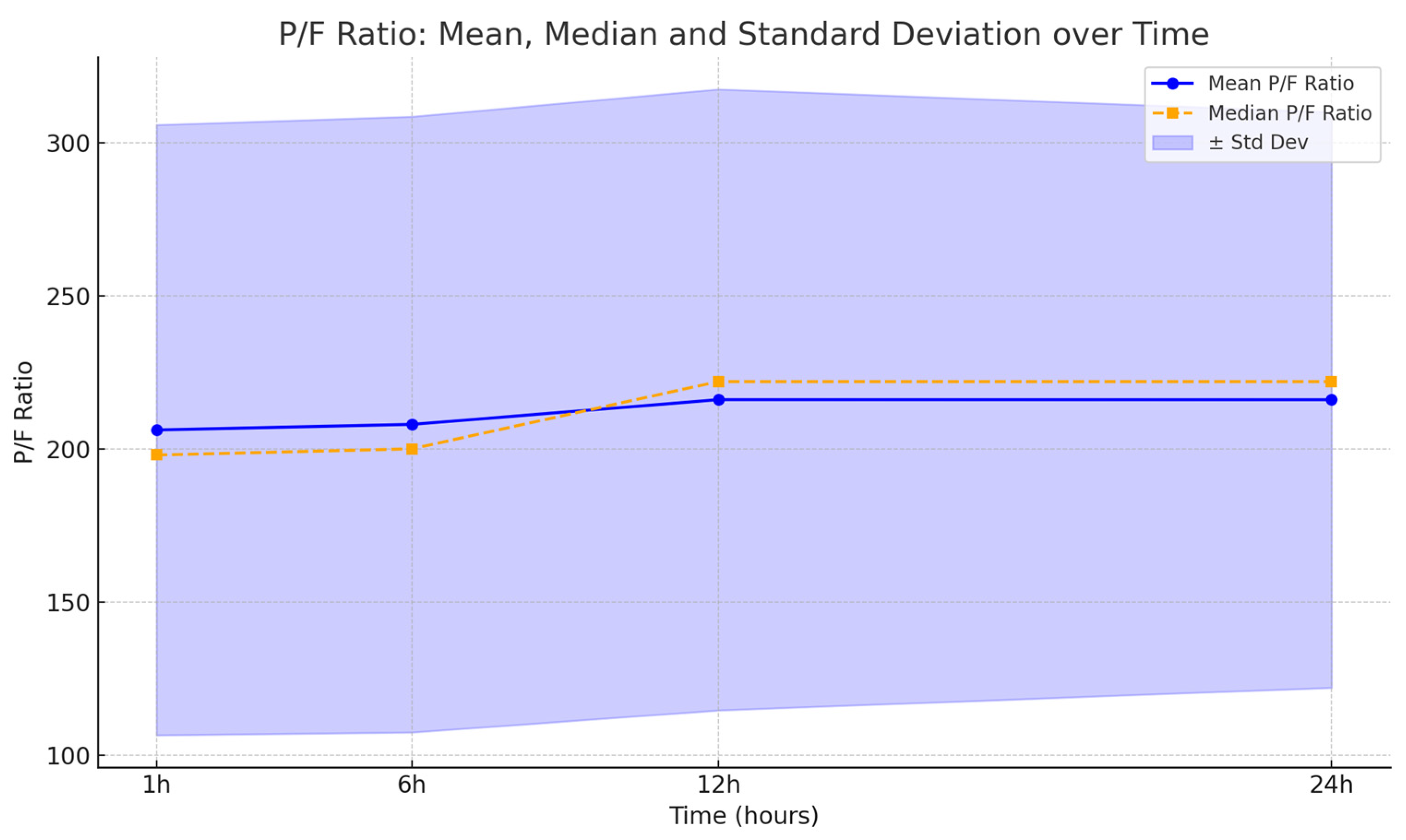
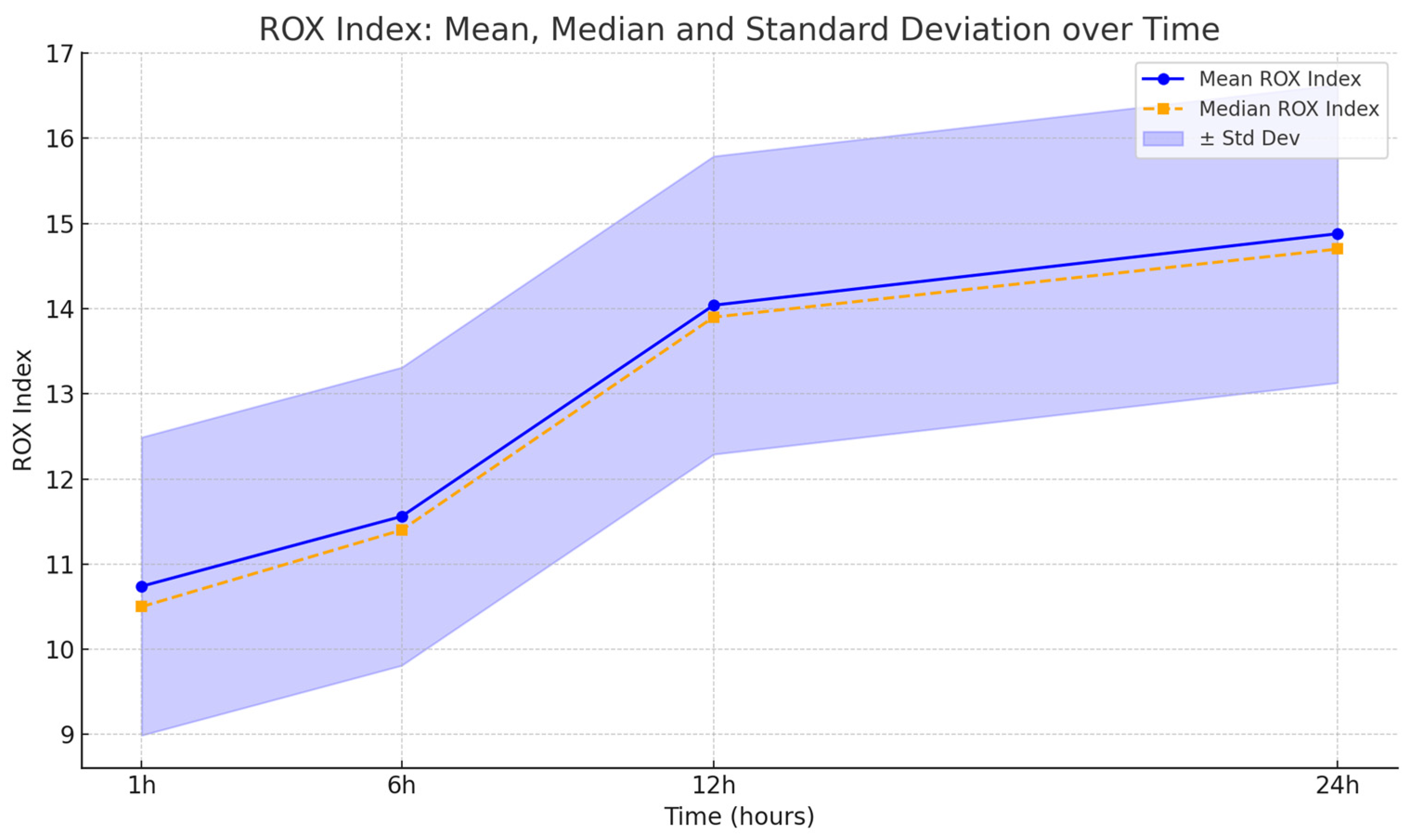
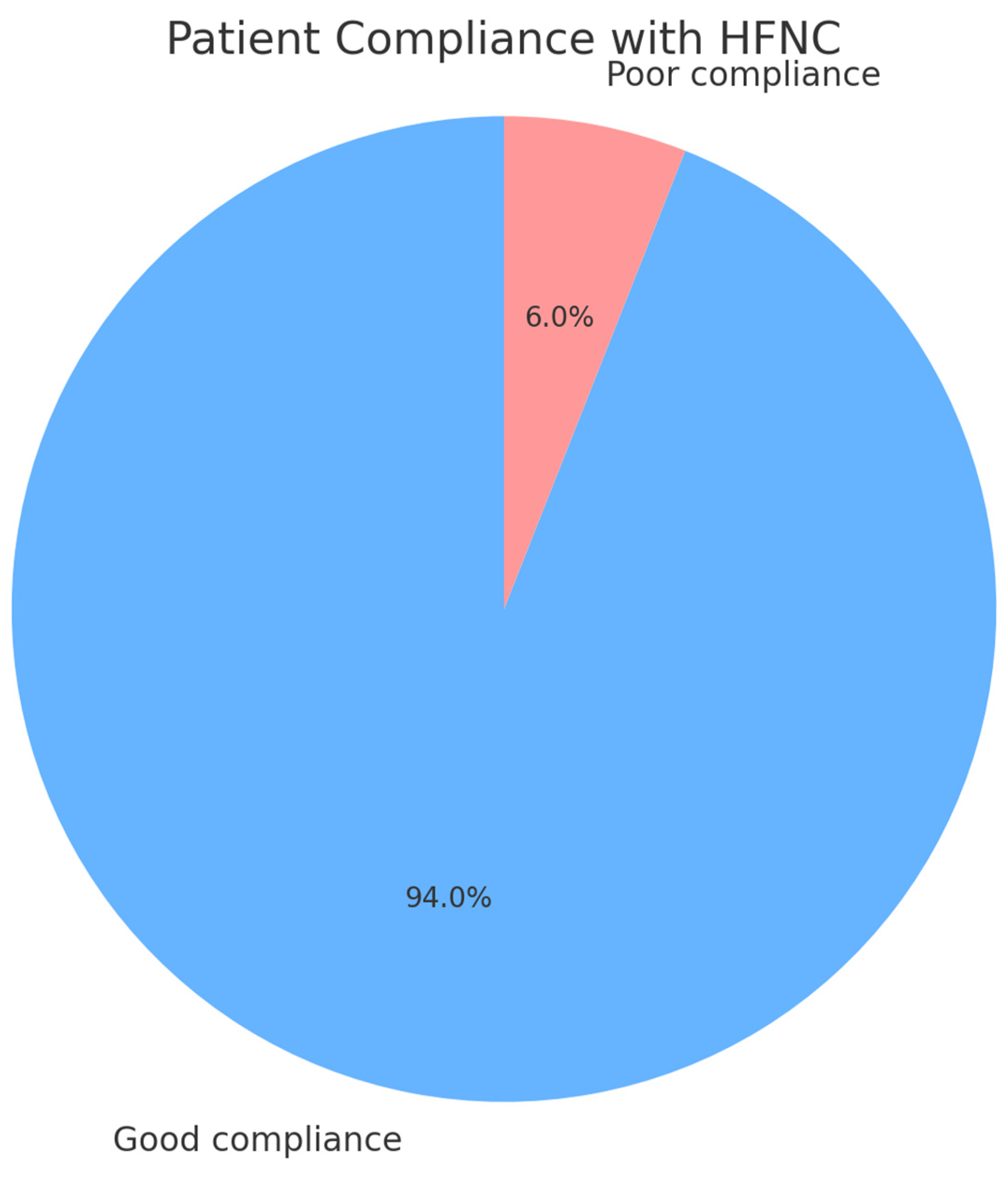
4. Results
5. Discussion
6. Conclusions
7. Limitation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AHRF | Acute Hypoxemic Respiratory Failure |
| AR | Absolute Risk |
| BMI | Body Mass Index |
| COT | Conventional Oxygen Therapy |
| ERAS | Enhanced Recovery After Surgery |
| FiO2 | Fraction of Inspired Oxygen |
| HFNC | High-Flow Nasal Cannula |
| ICU | Intensive Care Unit |
| length of stay | Length of Stay |
| MV | Mechanical Ventilation |
| NIV | Non-Invasive Ventilation |
| NPPV | Non-Invasive Positive Pressure Ventilation |
| OR | Operating Room |
| PACU | Post-Anesthesia Care Unit |
| PaO2 | Arterial Partial Pressure of Oxygen |
| PEEP | Positive End-Expiratory Pressure |
| P/F ratio | Ratio of PaO2 to FiO2 |
| PPC | Postoperative Pulmonary Complication |
| PSV | Pressure Support Ventilation |
| RCT | Randomized Controlled Trial |
| RR | Respiratory Rate |
| ROX Index | SpO2/FiO2 to Respiratory Rate Index |
| SpO2 | Peripheral Oxygen Saturation |
References
- Bizuneh, Y.B.; Zeleke, M.E.; Gebru, A.M.; Teshome, D.F.; Mekonnen, F.A.; Angaw, D.A.; Getahun, A.B. Global prevalence of postoperative hypoxemia among adult and pediatric surgical patients: A systematic review and meta-analysis. BMC Anesthesiol. 2025, 25, 284. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pensier, J.; Guerrero, M.A.; Berger-Estilita, J.; Borgstedt, L.; Zaher, A.M.; Jaber, S.; De Jong, A. Perioperative ventilation support, what clinicians and searchers must know. Anaesth. Crit. Care Pain Med. 2025, 44, 101554. [Google Scholar] [CrossRef] [PubMed]
- Xuan, L.; Ma, J.; Tao, J.; Zhu, L.; Lin, S.; Chen, S.; Pan, S.; Zhu, D.; Yi, L.; Zheng, Y. Comparative study of high-flow nasal catheter device and non-invasive positive pressure ventilation for sequential treatment in sepsis patients after weaning from mechanical ventilation in intensive care unit. Ann. Palliat. Med. 2021, 10, 6270–6278. [Google Scholar] [CrossRef] [PubMed]
- Frat, J.P.; Coudroy, R.; Marjanovic, N.; Thille, A.W. High-flow nasal oxygen therapy and noninvasive ventilation in the management of acute hypoxemic respiratory failure. Ann. Transl. Med. 2017, 5, 297. [Google Scholar] [CrossRef]
- Yang, X.; Cheng, J.; Wang, Z.; Dong, M.; Xu, Z.; Yu, H.; Liang, G. High-flow nasal cannula oxygen therapy versus noninvasive ventilation for elderly COPD patients after extubation: Randomized controlled trial protocol. BMC Pulm. Med. 2024, 24, 539. [Google Scholar] [CrossRef] [PubMed]
- Mamiya, H.; Ichinohe, T.; Kaneko, Y. Negative pressure pulmonary edema after oral and maxillofacial surgery. Anesth. Prog. 2009, 56, 49–52. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fitzmaurice, C.; Akinyemiju, T.F.; Al Lami, F.H.; Alam, T.; Alizadeh-Navaei, R.; Allen, C.; Alsharif, U.; Alvis-Guzman, N.; Amini, E.; Anderson, B.O.; et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2016: A systematic analysis for the global burden of disease study. JAMA Oncol. 2018, 4, 1553–1568. [Google Scholar] [CrossRef]
- Kinzinger, M.R.; Bewley, A.F. Perioperative care of head and neck free flap patients. Curr. Opin. Otolaryngol. Head. Neck Surg. 2017, 25, 405–410. [Google Scholar] [CrossRef]
- Coyle, M.J.; Main, B.; Hughes, C.; Craven, R.; Alexander, R.; Porter, G.; Thomas, S. Enhanced Recovery After Surgery (ERAS) for head and neck oncology patients. Clin. Otolaryngol. 2016, 41, 118–126. [Google Scholar] [CrossRef]
- Vetrugno, L.; Deana, C.; Colaianni-Alfonso, N.; Tritapepe, F.; Fierro, C.; Maggiore, S.M. Noninvasive respiratory support in the perioperative setting: A narrative review. Front. Med. 2024, 11, 1364475. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, R.; Liu, L.; Wei, K.; Zheng, X.; Zeng, J.; Chen, Q. Effect of noninvasive respiratory support after extubation on postoperative pulmonary complications in obese patients: A systematic review and network meta-analysis. J. Clin. Anesth. 2023, 91, 111280. [Google Scholar] [CrossRef] [PubMed]
- Arora, G.; Arshad, Z.; Prakash, R.; Sharma, M.; Singh, G.P.; Kohli, M. High-Flow Nasal Cannula as an Alternate Weaning Strategy: A Randomized Controlled Trial. Cureus 2023, 15, e36511. [Google Scholar] [CrossRef] [PubMed]
- ARDS Definition of Task Force; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome. JAMA 2012, 307, 2526–2533. [Google Scholar] [CrossRef]
- Croke, L. Preventing Postoperative Pulmonary Complications. AORN J. 2022, 116, P7–P10. [Google Scholar] [CrossRef] [PubMed]
- Pfeifer, K.; Smetana, G.W. Preoperative evaluation. In Murray and Nadel’s Textbook of Respiratory Medicine, 6th ed.; Elsevier Saunders: Philadelphia, PA, USA, 2015; pp. 472–479. [Google Scholar]
- Yoder, M.A. Perioperative Pulmonary Management. Medscape. Updated 16 January 2021. Available online: https://emedicine.medscape.com/article/284983 (accessed on 26 September 2022).
- Andualem, A.A.; Yesuf, K.A. Incidence and associated factors of postoperative hypoxemia among adult elective surgical patients at Dessie Comprehensive Specialized Hospital: An observational study. Ann. Med. Surg. 2022, 78, 103747. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Melesse, D.Y.; Denu, Z.A.; Kassahun, H.G.; Agegnehu, A.F. The incidence of early post-operative hypoxemia and its contributing factors among patients underwent operation under anesthesia at University of Gondar comprehensive and specialized referral hospital, Gondar, North West Ethiopia, 2018. A prospective observational study. Int. J. Surg. Open 2020, 22, 38–46. [Google Scholar] [CrossRef]
- Wolde, G.; Awol, M.; Obsa, M.; Wesene, N.; Gemechu, A.; Tadesse, E. Magnitude and associated factors of immediate postoperative hypoxemia among elective surgical procedures at Tikur Anbessa Specialized hospital, Addis Ababa, Ethiopia. J. Anesth. Clin. Res. 2018, 9, 2. [Google Scholar] [CrossRef]
- Tang, S.; Zhang, L.; Han, W.; Xue, Y.; Tian, Y.; Zhang, X.; Huang, Y. Incidence of Hypoxemia in a Post-anaesthesia Care Unit and Relevant Risk Factors: A Retrospective Study of 14604 Patients with General Anaesthesia. Res. Sq. Platf. 2019, 1–20. [Google Scholar]
- Ishikawa, M.; Sakamoto, A. Postoperative desaturation and bradypnea after general anesthesia in non-ICU patients: A retrospective evaluation. J. Clin. Monit. Comput. 2020, 34, 81–87. [Google Scholar] [CrossRef]
- Oczkowski, S.; Ergan, B.; Bos, L.; Chatwin, M.; Ferrer, M.; Gregoretti, C.; Heunks, L.; Frat, J.-P.; Longhini, F.; Nava, S.; et al. ERS clinical practice guidelines: High-flow nasal cannula in acute respiratory failure. Eur. Respir. J. 2022, 59, 2101574. [Google Scholar] [CrossRef]
- Deana, C.; Vecchiato, M.; Bellocchio, F.; Tullio, A.; Martino, A.; Ziccarelli, A.; Patruno, V.; Pascolo, M.; Bassi, F.; Pontoni, M.; et al. High flow nasal oxygen vs. conventional oxygen therapy over respiratory oxygenation index after esophagectomy: An observational study. J. Thorac. Dis. 2024, 16, 997–1008. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Munroe, E.S.; Prevalska, I.; Hyer, M.; Meurer, W.J.; Mosier, J.M.; Tidswell, M.A.; Prescott, H.C.; Wei, L.; Wang, H.; Fung, C.M. High-Flow Nasal Cannula Versus Noninvasive Ventilation as Initial Treatment in Acute Hypoxia: A Propensity Score-Matched Study. Crit. Care Explor. 2024, 6, e1092. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wang, Q.; Peng, Y.; Xu, S.; Lin, L.; Chen, L.; Lin, Y. The efficacy of high-flow nasal cannula (HFNC) versus non-invasive ventilation (NIV) in patients at high risk of extubation failure: A systematic review and meta-analysis. Eur. J. Med. Res. 2023, 28, 120. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Futier, E.; Paugam-Burtz, C.; Godet, T.; Khoy-Ear, L.; Rozencwajg, S.; Delay, J.M.; Verzilli, D.; Dupuis, J.; Chanques, G.; Bazin, J.E.; et al. Effect of early postextubation high-flow nasal cannula vs conventional oxygen therapy on hypoxaemia in patients after major abdominal surgery: A French multicentre randomised controlled trial (OPERA). Intensive Care Med. 2016, 42, 1888–1898. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, D.; Granton, D.; Wang, D.X.; Burns, K.E.; Helviz, Y.; Einav, S.; Trivedi, V.; Mauri, T.; Ricard, J.D.; Mancebo, J.; et al. High flow nasal cannula in the immediate postoperative period: A systematic review and meta-analysis. CHEST 2020, 158, 1934–1946. [Google Scholar] [CrossRef]
- Twose, P.; Thomas, C.; Morgan, M.; Broad, M.A. Comparison of high-flow oxygen therapy with standard oxygen therapy for prevention of postoperative pulmonary complications after major head and neck surgery involving insertion of a tracheostomy: A feasibility study. Br. J. Oral. Maxillofac. Surg. 2019, 57, 1014–1018. [Google Scholar] [CrossRef] [PubMed]
- 29. Liu, C.; Lin, Q.; Li, D. High-flow nasal cannula therapy versus conventional oxygen therapy for adult patients after cardiac surgery: A systemic review and meta-analysis. Heart Lung 2024, 66, 47–55. [Google Scholar] [CrossRef] [PubMed]
| ASA | III |
|---|---|
| Gender | 60% Male |
| 40% Female | |
| Length of Surgery | 677.5 min (DS 72.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pota, V.; Coppolino, F.; Giaccari, L.G.; Barbarisi, M.; Fiore, M.; Santagata, M.; Passavanti, M.B.; Pace, M.C.; Rugge, L.; Tartaro, G.; et al. High-Flow Nasal Cannula in Weaning Patients from Mechanical Ventilation in Head and Neck Surgery: Retrospective Study. Life 2025, 15, 1264. https://doi.org/10.3390/life15081264
Pota V, Coppolino F, Giaccari LG, Barbarisi M, Fiore M, Santagata M, Passavanti MB, Pace MC, Rugge L, Tartaro G, et al. High-Flow Nasal Cannula in Weaning Patients from Mechanical Ventilation in Head and Neck Surgery: Retrospective Study. Life. 2025; 15(8):1264. https://doi.org/10.3390/life15081264
Chicago/Turabian StylePota, Vincenzo, Francesco Coppolino, Luca Gregorio Giaccari, Manlio Barbarisi, Marco Fiore, Mario Santagata, Maria Beatrice Passavanti, Maria Caterina Pace, Luigi Rugge, Gianpaolo Tartaro, and et al. 2025. "High-Flow Nasal Cannula in Weaning Patients from Mechanical Ventilation in Head and Neck Surgery: Retrospective Study" Life 15, no. 8: 1264. https://doi.org/10.3390/life15081264
APA StylePota, V., Coppolino, F., Giaccari, L. G., Barbarisi, M., Fiore, M., Santagata, M., Passavanti, M. B., Pace, M. C., Rugge, L., Tartaro, G., Sansone, P., & Aurilio, C. (2025). High-Flow Nasal Cannula in Weaning Patients from Mechanical Ventilation in Head and Neck Surgery: Retrospective Study. Life, 15(8), 1264. https://doi.org/10.3390/life15081264













