High-Grade Appendiceal Goblet Cell Adenocarcinoma—A Literature Review Starting from a Rare Case
Abstract
1. Introduction
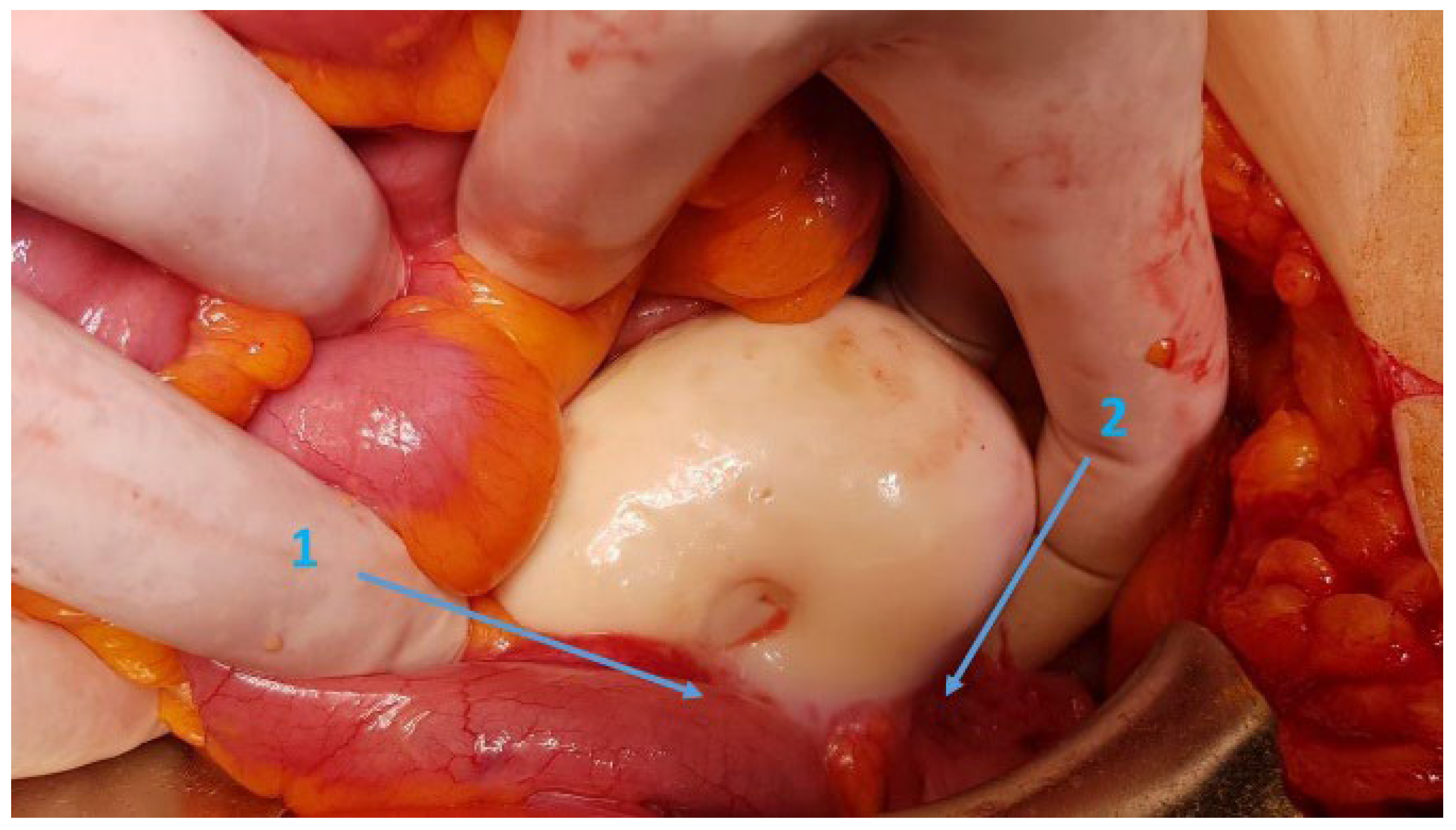
2. Case Presentation
3. Literature Review
| No | Authors | Year | Title | Number of Cases |
|---|---|---|---|---|
| 1 | Clift et al. [8] | 2018 | Goblet cell carcinoid of the appendix—diagnostic challenges and treatment updates: a case report and review of the literature. | 21 Tang ABC TNM |
| 2 | Rossi et al. [12] | 2022 | Goblet Cell Adenocarcinoma of the Appendix: A Systematic Review and Incidence and Survival of 1225 Cases From an English Cancer Registry. | 1225 Tang TNM |
| 3 | Reid Y et al. [13] | 2022 | Appendiceal Goblet Cell Adenocarcinoma: A Historically Informed Reading of 6 Cases. | 6 TNM retrospective |
| 4 | Taggart et al. [14] | 2024 | Goblet Cell Carcinoid of the Appendix: Six Case Reports. | 6 TNM |
| 5 | Lamarca et al. [15] | 2018 | Adenocarcinoma Ex-Goblet Cell: A Retrospective Experience. | 23 Tang B, C |
| 6 | Nonaka et al. [16] | 2015 | Goblet cell appendiceal tumors—management dilemmas and long-term outcomes. | 48 Tang ABC |
| 7 | Falk et al. [17] | 2023 | Clinicopathological spectrums and prognosis of primary appendiceal adenocarcinoma, goblet cell adenocarcinoma, and low-grade appendiceal mucinous neoplasms. | 40 G1, G2, G3 |
| 8 | Ibrahim et al. [18] | 2020 | Clinicopathological analysis of appendiceal goblet cell adenocarcinoma with peritoneal metastasis: World Health Organization grade predicts survival following cytoreductive surgery with intraperitoneal chemotherapy. | 63 G1, 2, 3 Tang ABC |
| 9 | Gilmore et al. [19] | 2020 | Molecular Characterization of Appendiceal Goblet Cell Carcinoid. | 53 NGS TP53-24.0% ARID1A-15.4% SMAD4-9.4% KRAS-7.5% MSI, MMR-0% PDL1-2% |
| 10 | Olsen et al. [20] | 2016 | Adenocarcinoma ex-goblet cell carcinoid (appendiceal-type crypt cell adenocarcinoma) is a morphologically distinct entity with highly aggressive behavior and frequent association with peritoneal/intra-abdominal dissemination: an analysis of 77 cases. | 77 High grade AexGCC |
| 11 | Tsang et al. [21] | 2018 | A study of appendiceal crypt cell adenocarcinoma (so-called goblet cell carcinoid and its related adenocarcinoma). | 105 TNM Low grade, high grade |
| 12 | Yozu et al. [22] | 2015 | Goblet cell carcinoid tumor, mixed goblet cell carcinoid-adenocarcinoma, and adenocarcinoma of the appendix: comparison of clinicopathologic features and prognosis. | 74 TNM |
| 13 | Zakka et al. [23] | 2016 | Appendiceal Goblet Cell Carcinoids: Management Considerations from a Reference Peritoneal Tumour Service Centre and ENETS Centre of Excellence. | 74 TNM AJCC Tang |
| 14 | Webb et al. [24] | 2018 | Histologic and Outcome Study Supports Reclassifying Appendiceal Goblet Cell Carcinoids as Goblet Cell Adenocarcinomas, and Grading and Staging Similarly to Colonic Adenocarcinomas. | 126 Low grade High grade TNM AJCC |
| 15 | Wang et al. [25] | 2021 | Is adjuvant chemotherapy beneficial for stage II–III goblet cell carcinoid/goblet cell adenocarcinoma of the appendix? | 619 AJCC |
| 16 | Jedrzkiewicz et al. [26] | 2018 | Endoscopic diagnosis of a goblet cell carcinoid tumour of the appendix. | 1 TNM |
| 17 | Chen et al. [27] | 2020 | Outcomes in Peritoneal Carcinomatosis from Appendiceal Goblet Cell Carcinoma Treated with Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy (CRS/HIPEC). | 27 TNM AJCC |
| 18 | Arai et al. [28] | 2018 | Adenocarcinoma Ex-goblet Cell Carcinoid of the Appendix: a Case Report and Overview of the Disease. | 1 Grade B |
| 19 | Taniguchi et al. [29] | 2020 | Impact of Referral Center Pathology Review on Diagnosis and Management of Patients With Appendiceal Neoplasms. | 24 NS |
| 20 | Kowalsky et al. [30] | 2015 | Goblet cell carcinoids: characteristics of a Danish cohort of 83 patients. | 83 TNM, Tang |
| 21 | Zambrano et al. [31] | 2018 | Goblet cell carcinoid of the appendix—diagnostic challenges and treatment. | 1 TNM, Tang |
| 22 | Madsen et al. [32] | 2021 | Appendiceal tumors with glandular and neuroendocrine features exhibiting peritoneal metastases—Critical evaluation of outcome following cytoreductive surgery with perioperative chemotherapy. | 47 TNM, Tang |
| 23 | Radomski et al. [33] | 2021 | Lymph node positivity and association with long-term survival for different histologies of appendiceal cancer. | 4435 TNM |
| 24 | Das et al. [34] | 2019 | Treatment patterns and outcomes in goblet cell carcinoid tumors of the appendix. | 2552 AJCC, G |
| 25 | Barrak et al. [35] | 2025 | Impact of genetic mutations on prognosis and chemotherapy efficacy in advanced appendiceal carcinoma: insights from the nationwide Japanese comprehensive genomic profiling test database. | 39 Gene panel testing |
| 26 | Shyu et al. [36] | 2021 | Chemotherapy in the treatment of different histological types of appendiceal cancers: a SEER based study. | 1087 TNM AJCC |
| 27 | Palmer et al. [37] | 2018 | Outcomes of Surgical and Chemotherapeutic Treatments of Goblet Cell Carcinoid Tumors of the Appendix. | 86/88 TNM, Tang |
| 28 | Höfler et al. [38] | 2018 | Effects of Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) in the Treatment of Goblet Cell Carcinoma: A Prospective Cohort Study. | 48 TNM |
3.1. Diagnosis Challenges
3.2. Tratment Patterns (Table 2)
3.2.1. Surgical Treatment
| No | Authors | Year | Title | Case Number | Grade | Stage | Surgery | Oncology | Type | Survival |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Lamarca.et al. [15] | 2019 | Adenocarcinoma Ex-Goblet Cell: a Retrospective Experience. | 23 | A-0 B-14 C-9 | IV-17 | RHC-8 RHC+HIPEC-5 | PC-17 | FOLFOX/FOLFIRI | NR NR mOS 32.9mo |
| 2 | Nonaka et al. [16] | 2015 | Appendiceal Goblet cell tumors (GCTs) are clinically more aggressive, and have a worse outcome than midgut neuroendocrine tumors (mNETs). | 48 (44a) | I/II-27 III-15 IV-6 | A-44 pRHC-41 CRS-24 | AC-9 PC-5 | FOLFOX/CAPOX/FOLFIRI | 1yOS-92% 3yOS-62.5% 5yOS-42% | |
| 3 | Ibrahim et al. [18] | 2020 | Clinicopathological analysis of appendiceal goblet cell adenocarcinoma with peritoneal metastasis: World Health Organization grade predicts survival following cytoreductive surgery with intraperitoneal chemotherapy. | 63 (48 GCA) | A-4 B-25 C-34 | I–III-5 IV-58 | RHC+HIPEC-55 | AC-51 | FOLFOX 4 FOLFIRI | G1/2mOS-98mo G3mOS-33mo |
| 4 | Wang et al. [25] | 2021 | Is adjuvant chemotherapy beneficial for stage II–III goblet cell carcinoid/goblet cell adenocarcinoma of the appendix? | 619 | H-360 L-259 | II-512 III-107 | RHC-603 TC-16 | AC-99 No-496 NA-21 | 5yOS-85, 5/82.7/42.8% II-5yOS-100%/90.9% III-77.1 | |
| 5 | Das et al. [34] | 2019 | Treatment patterns and outcomes in goblet cell carcinoid tumors of the appendix. | 2552 | L-449 H-144 NA-830 | I-279 II-811 III-152 IV-181 | A-639 RHC-1288 | AC-409 | 5yOS-77.8% 10yOS- 58.7% | |
| 6 | Zakka et al. [23] | 2016 | Appendiceal Goblet Cell Carcinoids: Management Considerations from a Reference Peritoneal Tumour Service Centre and ENETS Centre of Excellence. Neuroendocrinology. | 74 | A-33 B-31 C-5 NA-5 | I-2 II-29 III-12 IV-28 | A-9 A+RHC-24 A+RHC+HIPEC-10 A+RHC+HIPEC+CRS-15 MS-15 PS-10 | AC-18 PC-24 | FOLFOX/FOLFIRI | I-5yOS-100% II-5yOS-87% III-5yOS-40% IV-5yOS-18% |
| 7 | Chen et al. [27] | 2020 | Outcomes in Peritoneal Carcinomatosis from Appendiceal Goblet Cell Carcinoma Treated with Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy (CRS/HIPEC) | 27 | G1-17 G3-3 | A-11 RHC-10 CRS/HIPEC-20 | NAC-7 AC-17 | FOLFOX BEVACIZUMAB (2) | 1yOS-100% 3yOS-40% 5yOS-40% | |
| 8 | Höfler et al. [38] | 2018 | Effects of Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) in the Treatment of Goblet Cell Carcinoma: A Prospective Cohort Study. | 48 | LD-6 PS-8 EID-7 | RHC-6 pHIPEC+CRS-8 HIPEC+CRS-27 PS-7 | AC-16 PC-19 SC-2 | FOLFOX/CAPOX | LD-5yOS- 100% PS-5yOS-63% EID-5yOS- 57% | |
| 9 | Madsen et al. [32] | 2021 | Appendiceal tumors with glandular and neuroendocrine features exhibiting peritoneal metastases—Critical evaluation of outcome following cytoreductive surgery with perioperative chemotherapy. | 47 | A-6 B-25 C-13 | CRS-47 CRS+ICT-32 | NAT-32 AC-21 | mOS-48.5mo 5yOS-34.88% 10yOS-8.72% | ||
| 10 | Kowalsky et al. [30] | 2015 | Goblet cell carcinoids: characteristics of a Danish cohort of 83 patients. | 83 | A-34 B-40 C-9 | I-12 II-35 III-3 IV-27 | A-4 A+RHC-53 A+RHC+BSO-16 A+BSO-10 CRS+HIPEC-4 | AC-24 | SCLC r-11 CRC r-3 NET r-1 OC r-1 | mOS-83mo 1yOS-90% 3yOS-58% 5yOS-38% |
| 11 | Palmer et al. [37] | 2018 | Outcomes of Surgical and Chemotherapeutic Treatments of Goblet Cell Carcinoid Tumors of the Appendix. Oncol. | 86 | A-48 B-21 C-10 | I–III-67 IV-19 | A-40 RHC-51 MOR+HIPEC-9 | AC-9 | 5FU-5 FOLFOX-4 | 5yOS-68% |
| 12 | Adsay et al. [39] | 2016 | Curative Surgical Resection as a Component of Multimodality Therapy for Peritoneal Metastases from Goblet Cell Carcinoids. | 43 | A-4 B-22 C-7 | CRS+HIPEC-43 | NAT-32 AC-20 | - | mOS-22mo 3yOS-39% 5yOS-9% | |
| 13 | Clift et al. [8] | 2018 | Goblet cell carcinomas of the appendix: rare but aggressive neoplasms with challenging management. | 21 | A-8 B-10 C-3 | I-1 II-10 III-5 IV-5 | A-12 RHC-6+8 A+BSO-2 RHC+BSO-1 HIPEC-1 | AC-6 | 1yOS-79.4% 3yOS-60% 5yOS-60% |
3.2.2. Systemic Chemotherapy
3.2.3. Overall Survival
3.3. Critical Appraisal
- This is an extremely rare pathological entity, and much of the literature consists of case reports or small case series originating from North America, Europe, or Asia. However, these sources are not uniform in terms of nomenclature. AGCA remains a rare neoplasm globally, with the best-documented incidence data coming from North American databases.The lack of standardized reporting and variable diagnostic criteria across regions contribute to an epidemiological gap that warrants multinational registry collaboration (Table S2) and uniform adoption of WHO and Tang/Yozu classifications.
- Most retrospective studies have been conducted on large cohorts, predominantly from North American populations, based on SEER and NCDB databases. These studies often include cases reported prior to 2019—before goblet cell tumors (GCTs) were reclassified as goblet cell adenocarcinomas (GCAs). Consequently, nomenclature changes were not reflected in earlier publications.
- Therefore, even in studies published after 2019, the term “GCC” is still frequently used. Although “GCC” (goblet cell carcinoid) had long been the preferred term in the literature, its inclusion of “carcinoid” has caused confusion with well-differentiated neuroendocrine tumors (NETs), potentially leading to misdiagnosis and inappropriate treatments. Despite Yozu’s 2018 [22] recommendation for reclassification to GCA, and the WHO’s formal adoption of this nomenclature in 2019, inconsistency persists. Thus, we observe a significant source of confusion in referring to the same pathological entity by different names. At present, approximately 20 studies have adopted the 2019 WHO classification using the term GCA in case reports, small series, and larger cohorts.
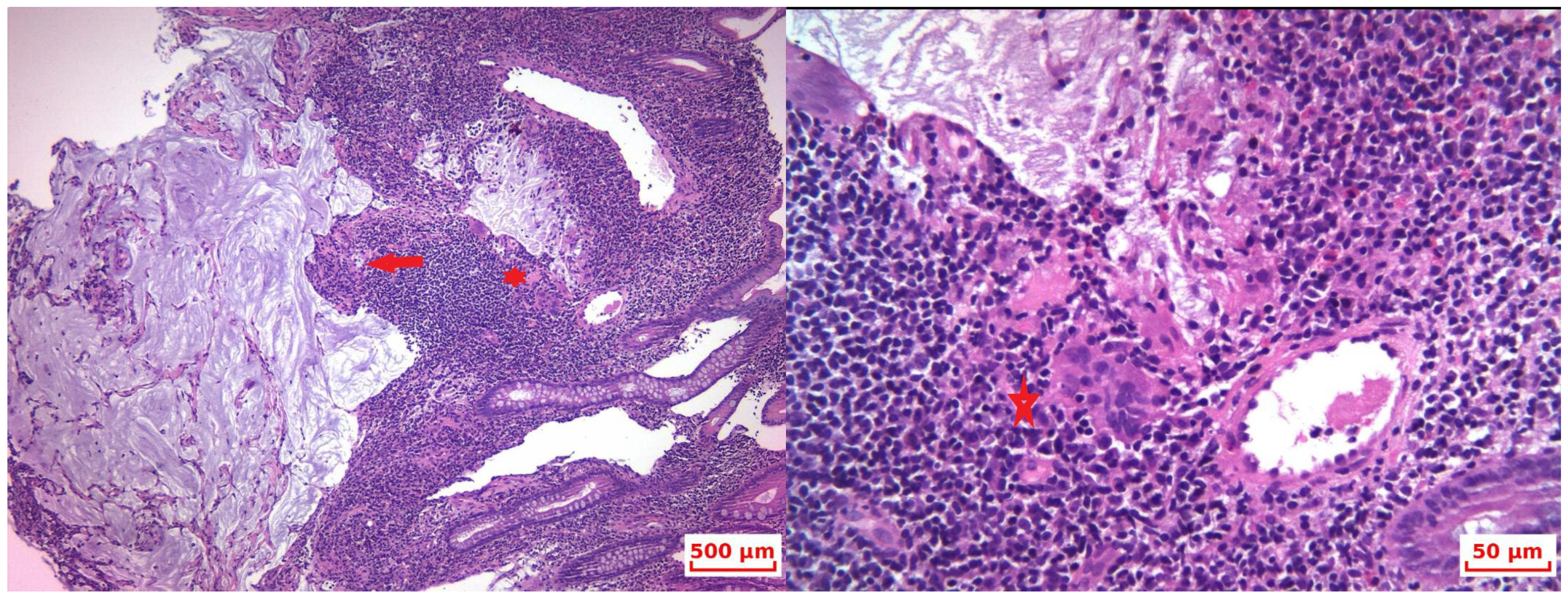
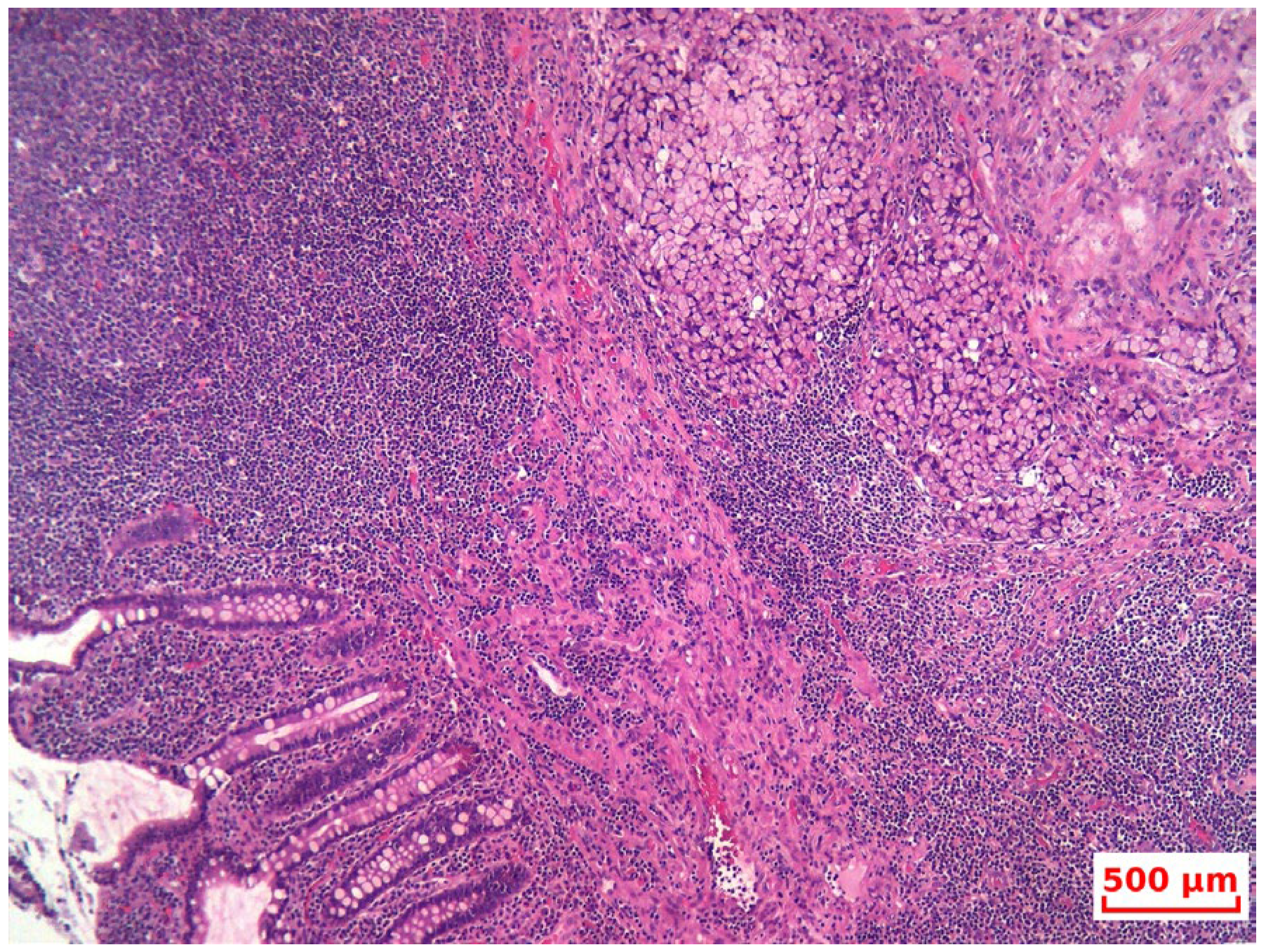
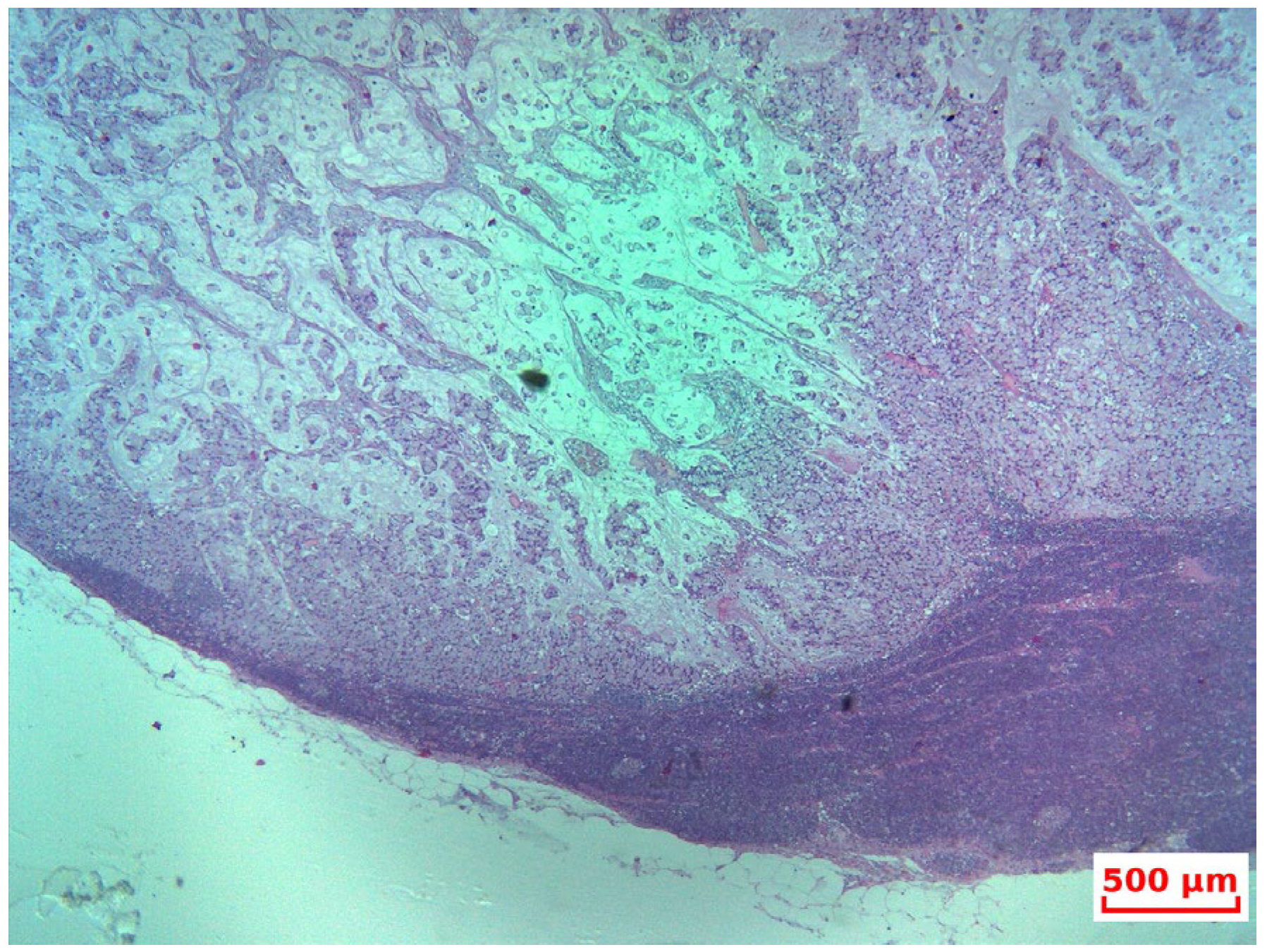
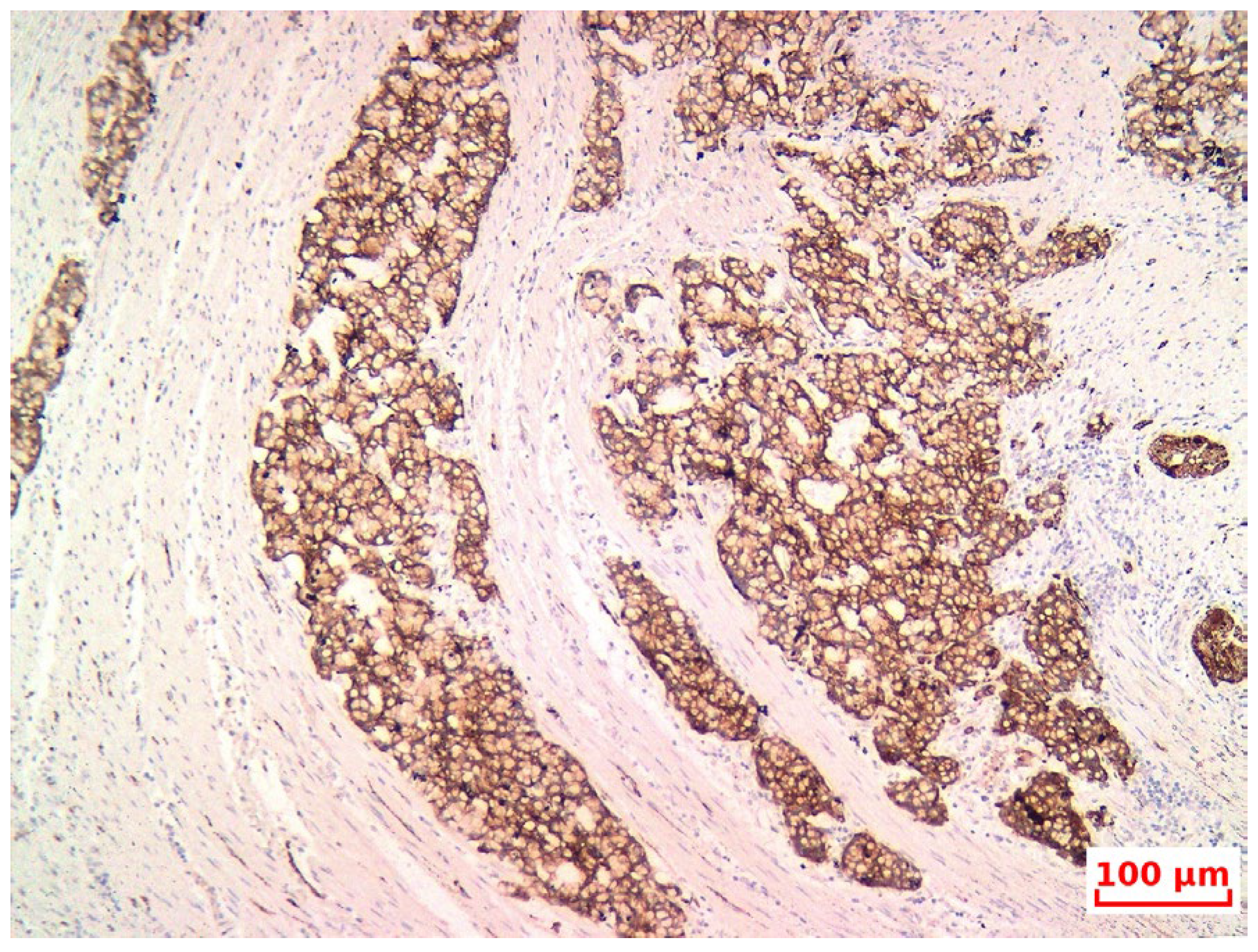
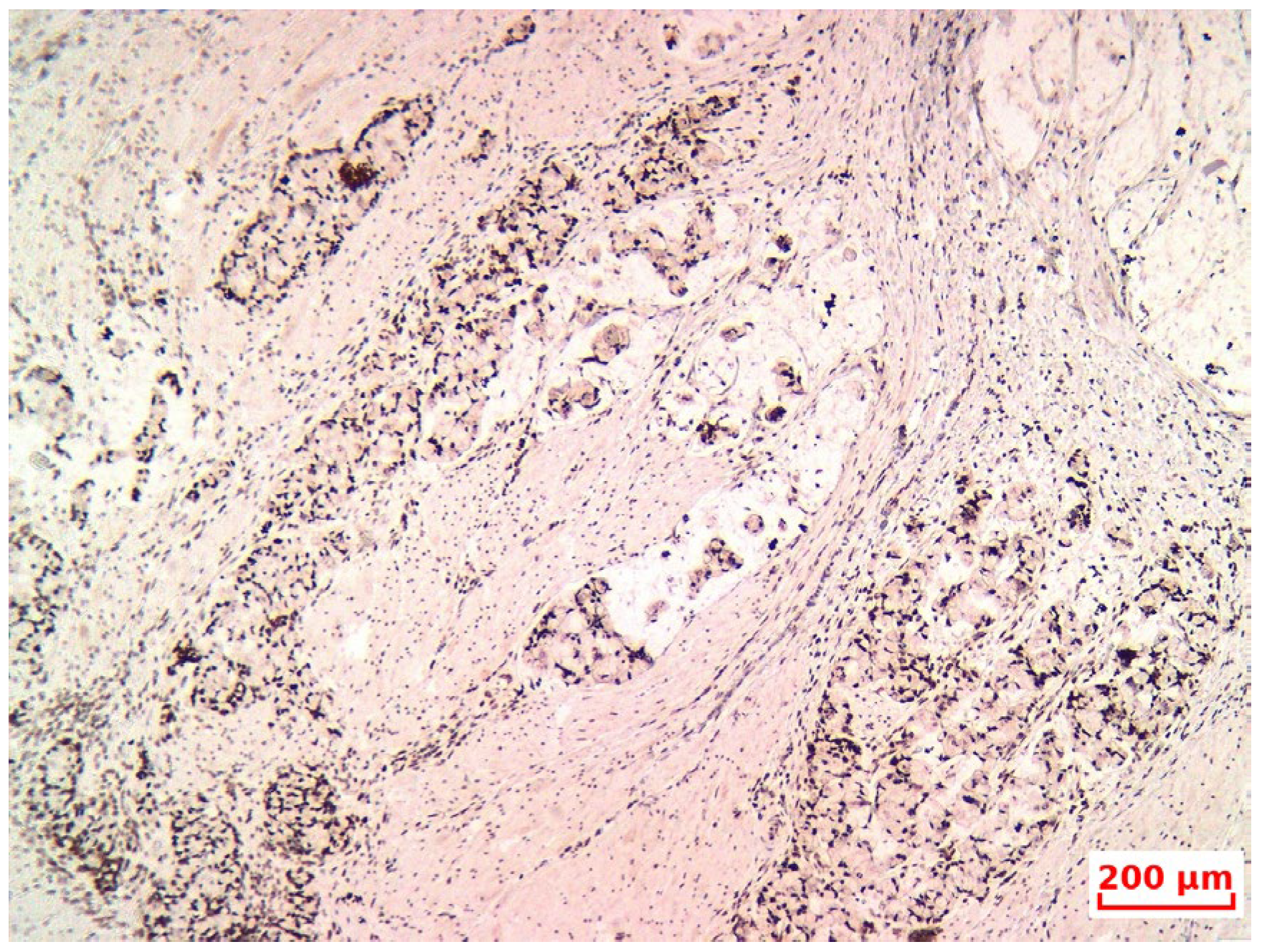
- The diagnosis of GCA was confirmed based on its characteristic histopathological features, and the non-endocrine component was verified through immunohistochemistry (IHC), although this may erroneously lead pathologists toward a NET diagnosis. Therefore, subspecialty pathology review of appendiceal neoplasms at referral centers is warranted, as emphasized by Jedrkiewicz [25].
- In most articles, the Tang classification—a histological grading system that more accurately reflects tumor biology and behavior—is used alongside the TNM classification—a universal anatomical staging framework critical for treatment planning and prognostication. The integration of both systems in diagnosing GCA offers a clearer understanding of tumor aggressiveness, the need for adjuvant treatment, and the surgical extent required. Additionally, consistent use and reporting of TNM staging is recommended to standardize cancer registry data across institutions.
- In an effort to further characterize this entity, molecular studies have also been conducted. Two major studies concluded that GCA presents a mutational profile distinctly different from both appendiceal adenocarcinomas and neuroendocrine tumors. Molecular classification was described in two large retrospective series based on analysis of resected appendiceal carcinoma specimens, aimed at identifying prognostic and predictive mutations to support potential targeted therapies [35,40].
- The lack of randomized controlled trials has led to conflicting data regarding the survival benefits of various surgical approaches. While some authors advocate for standard right hemicolectomy (RHC), others, such as Lamarca [23], report no survival advantage. In contrast, Tsang considers RHC to be the standard therapy, while Rossi supports it as a preventive strategy against recurrence. Several authors emphasize the importance of addressing peritoneal disease through cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC), noting the marked peritoneal tropism of GCA. CRS and HIPEC are strongly supported for patients with peritoneal involvement by authors such as Madsen and Tsang, whereas others, including Radomski, suggest that patients with Tang C tumors do not benefit significantly from aggressive surgical approaches.
- There is also no consensus regarding systemic chemotherapy. Some authors advocate for diagnostic laparoscopy followed by neoadjuvant chemotherapy [32]. Most adopt gastrointestinal regimens (e.g., FOLFOX or FOLFIRI) [15,16], although others have applied chemotherapy protocols typically used for ovarian, pulmonary, or neuroendocrine tumors [30]. The benefit of adjuvant chemotherapy in stage III disease is supported by Zakka, yet other studies [23,32] fail to confirm this, possibly due to small sample sizes or cohort heterogeneity. In selected cases, targeted therapies have been proposed when actionable molecular markers or receptors are identified [27].
- Overall survival (OS) rates remain highly variable, even when applying the same Tang classification system. This variation is attributed to differences in cohort composition and limited patient numbers. For example, Clift et al. [8] reported median OS for Tang A, B, and C tumors of 73.1 months, with 1-year OS rates of 85.7%, 85.7%, and 51.4%, respectively—lower than figures reported by Olsen. While some studies support the prognostic value of Tang grading, with OS rates of 118, 83, and 20 months for classes A, B, and C, respectively (p = 0.0002) [30], others, such as Shyu, found no statistically significant difference in OS among the Tang subtypes [36].
- This scarcity of high-level evidence complicates the establishment of standardized treatment protocols and hinders the ability to perform evidence-based comparisons of surgical techniques, chemotherapy regimens, or emerging targeted therapies. Consequently, clinical decisions are often extrapolated from guidelines for colorectal adenocarcinoma or neuroendocrine tumors, which may not fully capture the distinct biological behavior of GCA. Addressing this knowledge gap through multicenter registries and collaborative prospective trials is essential to improve outcomes and develop consensus-based treatment strategies.
- Nevertheless, several treatment recommendations can be made:
3.4. Guideline Discrepancies in the Management of Appendiceal Goblet Cell Adenocarcinoma (AGCA)
- The NCCN Guidelines tend to align AGCA with appendiceal or colorectal adenocarcinomas, advocating for aggressive surgical management strategies, such as right hemicolectomy for localized disease, and systemic chemotherapy regimens similar to those used in colorectal cancer. This approach reflects the high-grade behavior and aggressive clinical course typically observed in AGCA.
- In contrast, the ENETS Guidelines, which primarily address neuroendocrine neoplasms, frequently classify AGCA under the broader category of mixed neuroendocrine-nonneuroendocrine neoplasms (MiNENs). ENETS emphasizes a multidisciplinary approach that includes aspects of neuroendocrine tumor management, such as consideration of somatostatin analogs, proliferation indices, and personalized systemic therapy regimens tailored to the tumor’s neuroendocrine component.
4. Discussions
- Diagnostic pitfalls: Goblet cell adenocarcinoma (GCA) often presents with overlapping histological features of both adenocarcinoma and neuroendocrine tumors, which can lead to misclassification as typical carcinoid or mixed adenoneuroendocrinecarcinoma (MANEC). The diagnosis requires awareness of the dual phenotype, with both glandular (mucin-secreting) and neuroendocrine features, best demonstrated by morphology and immunohistochemistry (e.g., synaptophysin/chromogranin A positivity with Ki-67 > 20% in high-grade cases).
- Differentiation from MANEC and typical carcinoids: According to the 2019 WHO classification, GCAs are considered distinct from MANECs, as they represent a unique histologic and molecular entity. Unlike classical NET G1/G2 carcinoids, GCAs tend to be more aggressive, display infiltrative growth, and have a higher proliferative index.
- Imaging and tumor markers for surveillance: We have also added comments on surveillance strategies. While CT and MRI remain the primary modalities for post-treatment follow-up, especially in high-grade or disseminated disease, tumor markers such as CEA, CA19-9, and occasionally chromogranin A may be useful for monitoring, although no marker is specific. Their utility is often case-dependent and guided by initial expression levels.
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| GCA | Goblet Cell Adenocarcinoma |
| AGCA | Appendiceal Goblet Cell Adenocarcinoma |
| GCC | goblet cell carcinoid |
| GCT | goblet cell tumor |
| MiNEN | mixed neuroendocrine-nonneuroendocrine neoplasm |
| MANEC | mixed adenoneuroendocrine carcinoma |
| FOLFOX | fluorouracil, leucovorin calcium (folinic acid)and oxaliplatin |
| FOLFIRI | fluorouracil, leucovorin calcium (folinic acid) and irinotecan |
| WHO | World Health Organization |
| AJCC | American Joint Committee on Cancer |
| CRS | Cytoreductive Surgery |
| HIPEC | hyperthermic intraperitoneal chemotherapy |
| NET | Neuroendocrine Tumor |
| mNET | midgut Neuroendocrine tumors |
| CEA | Carcinoembryonic antigen |
| COPD | chronic obstructive pulmonary disease |
| FEV | Forced Expiratory Volume |
| IT | inspiratory time |
| CT | computed Tomography |
| HP | histopathology |
| IHC | Immunohistochemistry |
| OS | overall survival |
| CSS | cancer specific survival |
| PFS | progression free survival |
| NCDB | National Cancer Database |
| ICD-O | International Classification of Diseases for Oncology |
| SEER | Surveillance, Epidemiology, and End Results |
| AC | appendiceal carcinoma |
| a- | appendix |
| A- | appendectomy |
| NR | not reach |
| RHC | right hemicolectomy |
| MS | metastasectomy |
| PS | palleative surgery |
| AC | adjuvant chemotherapy |
| PC | palleative chemotherapy |
| SC | Supportive care |
| ICT | intraperitoneal chemotherapy |
| BSO | bilateral salpingo-oophorectomy |
| SCLC r | Small-cell-lung-cancer regimen |
| CRC r | Colorectal cancer regimen |
| NET r | Neuroendocrine Tumor regimen |
| OC r | ovarian cancer regimen |
| MOR | multiorgan resection |
| LD | localized disease, |
| PS | peritoneal spread |
| EID | extensive intraperitoneal disease |
| PCI | peritoneal carcinomatosis index |
| ENETS | European Neuroendocrine Tumor Society |
| ASCRS | American Society of Colon and Rectal Surgeons |
| NANETS | North American Neuroendocrine Tumor Society |
| NCCN | National Comprehensive Cancer Network |
| ESMO | European Society for Medical Oncology |
References
- Misdraji, J.; Carr, N.J.; Pai, P.K. Appendiceal goblet cell adenocarcinoma. In WHO Classification of Tumours. Digestive System Tumors, 5th ed.; Lokuhetty, D., White, V.A., Watanabe, R., Cree, I.A., Eds.; IARC Press: Lyon, France, 2019; pp. 149–151. [Google Scholar]
- Goede, A.C.; Caplin, M.E.; Winslet, M.C. Carcinoid tumour of the appendix. Br. J. Surg. 2003, 90, 1317–1322. [Google Scholar] [CrossRef] [PubMed]
- Stancu, M.; Wu, T.-T.; Wallace, C.; Houlihan, P.S.; Hamilton, S.R.; Rashid, A. Genetic alterations in goblet cell carcinoids of the vermiform appendix and comparison with gastrointestinal carcinoid tumors. Mod. Pathol. 2003, 16, 1189–1198. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Long, H.; Wang, W.; Liu, H.; Tang, Y.; Zhang, X. Clinicopathological features and immunoexpression profiles of goblet cell carcinoid and typical carcinoid of the appendix. Pathol. Oncol. Res. 2011, 17, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Van Eeden, S.; Offerhaus, G.J.; Hart, A.A.; Boerrigter, L.; Nederlof, P.M.; Porter, E.; van Velthuysen, M.L. Goblet cell carcinoid of the appendix: A specific type of carcinoma. Histopathology 2007, 51, 763–773. [Google Scholar] [CrossRef] [PubMed]
- Yan, T.D.; Brun, E.A.; Sugarbaker, P.H. Discordant Histology of Primary Appendiceal Adenocarcinoid Neoplasms with Peritoneal Dissemination. Ann. Surg. Oncol. 2008, 15, 1440–1446. [Google Scholar] [CrossRef]
- Pape, U.F.; Perren, A.; Niederle, B.; Gross, D.; Gress, T.; Costa, F.; Arnold, R.; Denecke, T.; Plöckinger, U.; Salazar, R.; et al. Barcelona Consensus Conference participants. ENETS Consensus Guidelines for the management of patients with neuroendocrine neoplasms from the jejuno-ileum and the appendix, including goblet cell carcinomas. Neuroendocrinology 2012, 95, 135–156. [Google Scholar] [CrossRef] [PubMed]
- Clift, A.K.; Frilling, A. Neuroendocrine, goblet cell and mixed adeno-neuroendocrine tumours of the appendix: Updates, clinical applications, and the future. Expert Rev. Gastroenterol. Hepatol. 2017, 11, 237–247. [Google Scholar] [CrossRef]
- Turaga, K.K.; Pappas, S.G.; Gamblin, T. Importance of histologic subtype in the staging of appendiceal tumors. Ann. Surg. Oncol. 2012, 19, 1379–1385. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.; Rashid, A.; Xing, Y.; Chiang, Y.J.; Chagpar, R.B.; Fournier, K.F.; Chang, G.J.; You, Y.N.; Feig, B.W.; Cormier, J.N. Varying malignant potential of appendiceal neuroendocrine tumors: Importance of histologic subtype. J. Surg. Oncol. 2013, 107, 136–143. [Google Scholar] [CrossRef] [PubMed]
- McCusker, M.E.; Coté, T.R.; Clegg, L.X.; Sobin, L.H. Primary malignant neoplasms of the appendix: A population-based study from the surveillance, epidemiology, and end-results program, 1973–1998. Cancer 2002, 94, 3307–3312. [Google Scholar] [CrossRef] [PubMed]
- Rossi, R.E.; Luong, T.V.; Caplin, M.E.; Thirlwell, C.; Meyer, T.; Garcia-Hernandez, J.; Baneke, A.; Conte, D.; Toumpanakis, C. Goblet cell appendiceal tumors—Management dilemmas and long-term outcomes. Surg. Oncol. 2015, 24, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Reid, M.D.; Basturk, O.; Shaib, W.L.; Xue, Y.; Balci, S.; Choi, H.J.; Akkas, G.; Memis, B.; Robinson, B.S.; El-Rayes, B.F.; et al. Adenocarcinoma ex-goblet cell carcinoid (appendiceal-type crypt cell adenocarcinoma) is a morphologically distinct entity with highly aggressive behavior and frequent association with peritoneal/intra-abdominal dissemination: An analysis of 77 cases. Mod.Pathol. 2016, 29, 1243–1253. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Taggart, M.W.; Abraham, S.C.; Overman, M.J.; Mansfield, P.F.; Rashid, A. Goblet cell carcinoid tumor, mixed goblet cell carcinoid-adenocarcinoma, and adenocarcinoma of the appendix: Comparison of clinicopathologic features and prognosis. Arch. Pathol. Lab. Med. 2015, 139, 782–790. [Google Scholar] [CrossRef] [PubMed]
- Lamarca, A.; Nonaka, D.; Lopez Escola, C.; Hubner, R.A.; O’Dwyer, S.; Chakrabarty, B.; Fulford, P.; Valle, J.W. Appendiceal Goblet Cell Carcinoids: Management Considerations from a Reference Peritoneal Tumour Service Centre and ENETS Centre of Excellence. Neuroendocrinology 2016, 103, 500–517. [Google Scholar] [CrossRef] [PubMed]
- Nonaka, D.; Papaxoinis, G.; Lamarca, A.; Fulford, P.; Valle, J.; Chakrabarty, B. A study of appendiceal crypt cell adenocarcinoma (so-called goblet cell carcinoid and its related adenocarcinoma). Hum. Pathol. 2018, 72, 18–27. [Google Scholar] [CrossRef] [PubMed]
- Falk, V.; Ballantyne, M.; Zepeda-Gómez, S.; Kohansal-Vajargah, A. Endoscopic diagnosis of a goblet cell carcinoid tumour of the appendix. BMJ Case Rep. 2018, 2018, bcr2017223298. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ibrahim, U.; Valecha, G.; Garcia, G.; Saqib, A.; Wrzolek, M.; Dhar, M. Adenocarcinoma Ex-goblet Cell Carcinoid of the Appendix: A Case Report and Overview of the Disease. J. Gastrointest. Cancer 2018, 49, 497–500. [Google Scholar] [CrossRef] [PubMed]
- Gilmore, G.; Jensen, K.; Saligram, S.; Sachdev, T.P.; Arekapudi, S.R. Goblet cell carcinoid of the appendix–diagnostic challenges and treatment updates: A case report and review of the literature. J. Med. Case Rep. 2018, 12, 275. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Olsen, I.H.; Holt, N.; Langer, S.W.; Hasselby, J.P.; Grønbæk, H.; Hillingsø, J.; Mahmoud, M.; Ladekarl, M.; Iversen, L.H.; Kjær, A.; et al. Goblet cell carcinoids: Characteristics of a Danish cohort of 83 patients. PLoS ONE 2015, 10, e0117627. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tsang, E.S.; McConnell, Y.J.; Schaeffer, D.F.; Lee, L.; Yin, Y.; Zerhouni, S.; Schaff, K.; Speers, C.; Kennecke, H.F. Outcomes of Surgical and Chemotherapeutic Treatments of Goblet Cell Carcinoid Tumors of the Appendix. Ann. Surg. Oncol. 2018, 25, 2391–2399. [Google Scholar] [CrossRef] [PubMed]
- Yozu, M.; Johncilla, M.E.; Srivastava, A.; Ryan, D.P.; Cusack, J.C.; Doyle, L.; Setia, N.; Yang, M.; Lauwers, G.Y.; Odze, R.D.; et al. Histologic and Outcome Study Supports Reclassifying Appendiceal Goblet Cell Carcinoids as Goblet Cell Adenocarcinomas, and Grading and Staging Similarly to Colonic Adenocarcinomas. Am. J. Surg. Pathol. 2018, 42, 898–910. [Google Scholar] [CrossRef] [PubMed]
- Zakka, K.; Williamson, S.; Jiang, R.; Reid, M.D.; Alese, O.B.; Shaib, W.L.; Wu, C.; Behera, M.; El-Rayes, B.F.; Akce, M. Is adjuvant chemotherapy beneficial for stage II-III goblet cell carcinoid/goblet cell adenocarcinoma of the appendix? Surg. Oncol. 2021, 36, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Webb, C.; Chang, Y.H.; Pockaj, B.A.; Gray, R.J.; Stucky, C.C.; Wasif, N. Lymph node positivity and association with long-term survival for different histologies of appendiceal cancer. J. Surg. Oncol. 2021, 124, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.; Li, Q.; Chen, W. Chemotherapy in the treatment of different histological types of appendiceal cancers: A SEER based study. BMC Cancer 2021, 21, 778. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jedrzkiewicz, J.; Tateishi, Y.; Kirsch, R.; Conner, J.; Bischof, D.; McCart, A.; Riddell, R.; Pollett, A.; Taylor, E.L.; Govindarajan, A. Impact of Referral Center Pathology Review on Diagnosis and Management of Patients With Appendiceal Neoplasms. Arch. Pathol. Lab. Med. 2020, 144, 764–768. [Google Scholar] [CrossRef] [PubMed]
- Chen, I.; Liu, X.; Kovar-Peltz, S.; Conrad, S.J.; Chen, H.H.; Liao, X. Clinicopathological spectrums and prognosis of primary appendiceal adenocarcinoma, goblet cell adenocarcinoma, and low-grade appendiceal mucinous neoplasms. Pathology 2023, 55, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Arai, H.; Baca, Y.; Battaglin, F.; Kawanishi, N.; Wang, J.; Soni, S.; Zhang, W.; Millstein, J.; Johnston, C.; Goldberg, R.M.; et al. Molecular Characterization of Appendiceal Goblet Cell Carcinoid. Mol. Cancer Ther. 2020, 19, 2634–2640. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Taniguchi, S.H.; Takahashi, M.; Chiu, S.W.; Komine, K.; Wakayama, S.; Numakura, R.; Yoshida, Y.; Kasahara, Y.; Ouchi, K.; Imai, H.; et al. Impact of genetic mutations on prognosis and chemotherapy efficacy in advanced appendiceal carcinoma: Insights from the nationwide Japanese comprehensive genomic profiling test database. Int. J. Clin. Oncol. 2025, 30, 914–925. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kowalsky, S.J.; Nassour, I.; AlMasri, S.; Paniccia, A.; Zureikat, A.H.; Choudry, H.A.; Pingpank, J.F. Omission of Right Hemicolectomy May be Safe for Some Appendiceal Goblet Cell Adenocarcinomas: A Survival Analysis of the National Cancer Database. Ann. Surg. Oncol. 2021, 28, 8916–8925. [Google Scholar] [CrossRef] [PubMed]
- Zambrano-Vera, K.; Sardi, A.; Munoz-Zuluaga, C.; Studeman, K.; Nieroda, C.; Sittig, M.; King, M.C.; Sipok, A.; Gushchin, V. Outcomes in Peritoneal Carcinomatosis from Appendiceal Goblet Cell Carcinoma Treated with Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy (CRS/HIPEC). Ann. Surg. Oncol. 2020, 27, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Madsen, A.H.; Ladekarl, M.; Villadsen, G.E.; Grønbæk, H.; Sørensen, M.M.; Stribolt, K.; Verwaal, V.J.; Iversen, L.H. Effects of Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy (HIPEC) in the Treatment of Goblet Cell Carcinoma: A Prospective Cohort Study. Ann. Surg. Oncol. 2018, 25, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Radomski, M.; Pai, R.K.; Shuai, Y.; Ramalingam, L.; Jones, H.; Holtzman, M.P.; Ahrendt, S.A.; Pingpank, J.F.; Zeh, H.J.; Bartlett, D.L.; et al. Curative Surgical Resection as a Component of Multimodality Therapy for Peritoneal Metastases from Goblet Cell Carcinoids. Ann. Surg. Oncol. 2016, 23, 4338–4343. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Shi, C.; Du, L.; Idrees, K.; Berlin, J. Adenocarcinoma Ex-Goblet Cell: A Retrospective Experience. J. Gastrointest. Cancer 2019, 50, 709–715. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Barrak, D.; Desale, S.; Yoon, J.J.; Dugan, M.M.; Kodavanti, P.P.; Sampah, M.E.; Sugarbaker, P.H. Appendiceal tumors with glandular and neuroendocrine features exhibiting peritoneal metastases—Critical evaluation of outcome following cytoreductive surgery with perioperative chemotherapy. Eur. J. Surg. Oncol. 2021, 47, 1278–1285. [Google Scholar] [CrossRef] [PubMed]
- Shyu, S.; Choudry, H.; Hall, L.; Pingpank, J.; Holtzman, M.; Bartlett, D.; Pai, R.K. Clinicopathological analysis of appendiceal goblet cell adenocarcinoma with peritoneal metastasis: World Health Organization grade predicts survival following cytoreductive surgery with intraperitoneal chemotherapy. Histopathology 2020, 77, 798–809. [Google Scholar] [CrossRef] [PubMed]
- Palmer, K.; Weerasuriya, S.; Chandrakumaran, K.; Rous, B.; White, B.E.; Paisey, S.; Srirajaskanthan, R.; Ramage, J.K. Goblet Cell Adenocarcinoma of the Appendix: A Systematic Review and Incidence and Survival of 1225 Cases From an English Cancer Registry. Front. Oncol. 2022, 12, 915028. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Höfler, H.; Klöppel, G.; Heitz Ph, U. Combined Production of Mucus, Amines and Peptides by Goblet-Cell Carcinoids of the Appendix and Ileum. Pathol. Res. Pract. 1984, 178, 555–561. [Google Scholar] [CrossRef]
- Adsay, N.V.; Klimstra, D.S. Surgical Pathology of the GI Tract, Liver, Biliary Tract, and Pancreas; Elsevier: Philadelphia, PA, USA, 2015; pp. 803–820. [Google Scholar]
- Tang, L.H.; Shia, J.; Soslow, R.A.; Dhall, D.; Wong, W.D.; O’Reilly, E.; Qin, J.; Paty, P.; Weiser, M.R.; Guillem, J.; et al. Pathologic Classification and Clinical Behavior of the Spectrum of Goblet Cell Carcinoid Tumors of the Appendix. Am. J. Surg. Pathol. 2008, 32, 1429–1443. [Google Scholar] [CrossRef]
- Riddell, R.; Petras, R.; Williams, G.; Sobin, L.H. Endocrine cell tumors. In Tumors of the Intestines; Armed Forces Institute of Pathology: Washington, DC, USA, 2003; Volume 32, pp. 304–309. [Google Scholar]
- Arnold, C.A.; Graham, R.P.; Jain, D.; Kakar, S.; Lam-Himlin, D.M.; Naini, B.V.; Wu, T.T.; Yeh, M.M.; Torbenson, M.S. Knowledge gaps in the appendix: A multi-institutional study from seven academic centers. Mod. Pathol. 2019, 32, 988–996. [Google Scholar] [CrossRef] [PubMed]
- Shenoy, S. Goblet cell carcinoids of the appendix: Tumor biology, mutations and management strategies. World J. Gastrointest. Surg. 2016, 8, 660–669. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gagné, F.; Fortin, P.; Dufour, V.; Delage, C. Tumeurs de l’appendiceassociant des caractèreshistologiques de carcinoïde et d’adénocarcinome [Tumors of the appendix associating histologic features of carcinoid and adenocarcinoma]. Ann. Anat. Pathol. 1969, 14, 393–406. (In French) [Google Scholar] [PubMed]
- Subbuswamy, S.G.; Gibbs, N.M.; Ross, C.F.; Morson, B.C. Goblet cell carcinoid of the appendix. Cancer 1974, 34, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Warkel, R.L.; Cooper, P.H.; Helwig, E.B. Adenocarcinoid, a mucin-producing carcinoid tumor of the appendix: A study of 39 cases. Cancer 1978, 42, 2781–2793. [Google Scholar] [CrossRef] [PubMed]
- Carr, N.J.; Sobin, L.H. Adenocarcinoma of the appendix. In World Health Organization Classification of Tumours of the Digestive System; Bosman, F.T., Carneiro, F., Hruban, R.H., Theise, N.D., Eds.; IARC Press: Lyon, France, 2010; Volume 3, pp. 120–125. [Google Scholar]
- Wen, K.W.; Hale, G.; Shafizadeh, N.; Hosseini, M.; Huang, A.; Kakar, S. Appendiceal goblet cell carcinoid: Common errors in staging and clinical interpretation with a proposal for an improved terminology. Hum. Pathol. 2017, 65, 187–193. [Google Scholar] [CrossRef]
- Jesinghaus, M.; Konukiewitz, B.; Foersch, S.; Stenzinger, A.; Steiger, K.; Muckenhuber, A.; Groß, C.; Mollenhauer, M.; Roth, W.; Detlefsen, S.; et al. Appendiceal goblet cell carcinoids and adenocarcinomas ex-goblet cell carcinoid are genetically distinct from primary colorectal-type adenocarcinoma of the appendix. Mod. Pathol. 2018, 31, 829–839. [Google Scholar] [CrossRef] [PubMed]
- Hanna, N.; Hanna, A.N.; Hanna, D.N. AJCC Cancer Staging System Version 9: Appendiceal Adenocarcinoma. Ann. Surg. Oncol. 2024, 31, 2177–2180. [Google Scholar] [CrossRef]
- Azuma, T.; Sato, Y.; Chiba, H.; Haga, J. Appendiceal goblet cell adenocarcinoma newly classified by WHO 5th edition: A case report (a secondary publication). Surg. Case Rep. 2024, 10, 168. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Toshima, T.; Inada, R.; Sakamoto, S.; Takeda, E.; Yoshioka, T.; Kumon, K.; Mimura, N.; Takata, N.; Tabuchi, M.; Oishi, K.; et al. Goblet cell carcinoid of the appendix: Six case reports. World J. Clin. Cases 2024, 12, 5217–5224. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, S.C.; Gaertner, W.; Stewart, D.; Davids, J.; Alavi, K.; Paquette, I.M.; Steele, S.R.; Feingold, D.L. The American Society of Colon and Rectal Surgeons, Clinical Practice Guidelines for the Management of Appendiceal Neoplasms. Dis. Colon Rectum 2019, 62, 1425–1438. [Google Scholar] [CrossRef]
- Boudreaux, J.P.; Klimstra, D.S.; Hassan, M.M.; Woltering, E.A.; Jensen, R.T.; Goldsmith, S.J.; Nutting, C.; Bushnell, D.L.; Caplin, M.E.; Yao, J.C.; et al. The NANETS consensus guideline for the diagnosis and management of neuroendocrine tumors: Well-differentiated neuroendocrine tumors of the Jejunum, Ileum, Appendix, and Cecum. Pancreas 2010, 39, 753–766. [Google Scholar] [CrossRef]
- Japanese Society for Cancer of the Colon and Rectum. Japanese Classification of Colorectal, Appendiceal, and Anal Carcinoma: The 3d English Edition [Secondary Publication]. J. Anus Rectum Colon 2019, 3, 175–195. [Google Scholar] [CrossRef] [PubMed]
- Benson, A.B.; Venook, A.P.; Adam, M.; Chang, G.; Chen, Y.J.; Ciombor, K.K.; Cohen, S.A.; Cooper, H.S.; Deming, D.; Garrido-Laguna, I.; et al. Colon Cancer, Version 3.2024, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2024, 22, e240029. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.-H.; Yonemura, Y.; Hsieh, M.-C.; Mizumoto, A.; Wakama, S.; Lu, C.-Y. Cytoreductive Surgery and Hyperthermic Intraperitoneal Chemotherapy for Appendiceal Goblet Cell Carcinomas with Peritoneal Carcinomatosis: Results From a Single Specialized Center. Cancer Manag. Res. 2017, 9, 513–523. [Google Scholar] [CrossRef] [PubMed]
- Gaillard, M.; Van Eyken, P.; Verswijvel, G.; Van der Speeten, K. Appendiceal Goblet Cell Carcinoma: Role of Cytoreductive Surgery (CRS) and Hyperthermic Intraperitoneal Chemotherapy (HIPEC). Indian J. Surg. Oncol. 2023, 14 (Suppl. S1), 240–249. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- AlMasri, S.; Nassour, I.; Kowalsky, S.J.; Hrebinko, K.; Singhi, A.D.; Lee, K.K.; Choudry, H.A.; Bartlett, D.; Zureikat, A.; Paniccia, A. The Role of Adjuvant Chemotherapy in Non-Metastatic Goblet Cell Carcinoid of the Appendix: An 11-Year Experience From the National Cancer Database. Ann. Surg. Oncol. 2021, 28, 3873–3881. [Google Scholar] [CrossRef]
- Fields, A.C.; Lu, P.; Enzinger, A.; Goldberg, J.; Irani, J.; Bleday, R.; Nash, G.; Melnitchouk, N. Treatment Patterns and Outcomes in Goblet Cell Carcinoid Tumors of the Appendix. J. Surg. Oncol. 2019, 120, 1096–1101. [Google Scholar] [CrossRef]
- Strach, M.C.; Chakrabarty, B.; Nagaraju, R.T.; Mullamitha, S.; Braun, M.; O’Dwyer, S.T.; Aziz, O.; Barriuso, J. Defining a role for systemic chemotherapy in local and advanced appendix adenocarcinoma. ESMO Open 2023, 8, 101619. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gheorghe, M.; Birla, R.D.; Evsei-Seceleanu, A.; Bitina, L.; Mates, I.N.; Predescu, D.V. High-Grade Appendiceal Goblet Cell Adenocarcinoma—A Literature Review Starting from a Rare Case. Life 2025, 15, 1047. https://doi.org/10.3390/life15071047
Gheorghe M, Birla RD, Evsei-Seceleanu A, Bitina L, Mates IN, Predescu DV. High-Grade Appendiceal Goblet Cell Adenocarcinoma—A Literature Review Starting from a Rare Case. Life. 2025; 15(7):1047. https://doi.org/10.3390/life15071047
Chicago/Turabian StyleGheorghe, Mircea, Rodica Daniela Birla, Anca Evsei-Seceleanu, Luiza Bitina, Ioan Nicolae Mates, and Dragos Valentin Predescu. 2025. "High-Grade Appendiceal Goblet Cell Adenocarcinoma—A Literature Review Starting from a Rare Case" Life 15, no. 7: 1047. https://doi.org/10.3390/life15071047
APA StyleGheorghe, M., Birla, R. D., Evsei-Seceleanu, A., Bitina, L., Mates, I. N., & Predescu, D. V. (2025). High-Grade Appendiceal Goblet Cell Adenocarcinoma—A Literature Review Starting from a Rare Case. Life, 15(7), 1047. https://doi.org/10.3390/life15071047








