Does Proprioceptive Neuromuscular Facilitation-Based Hamstring Stretching Influence Deep Cervical Flexor Muscle Endurance?
Abstract
1. Introduction
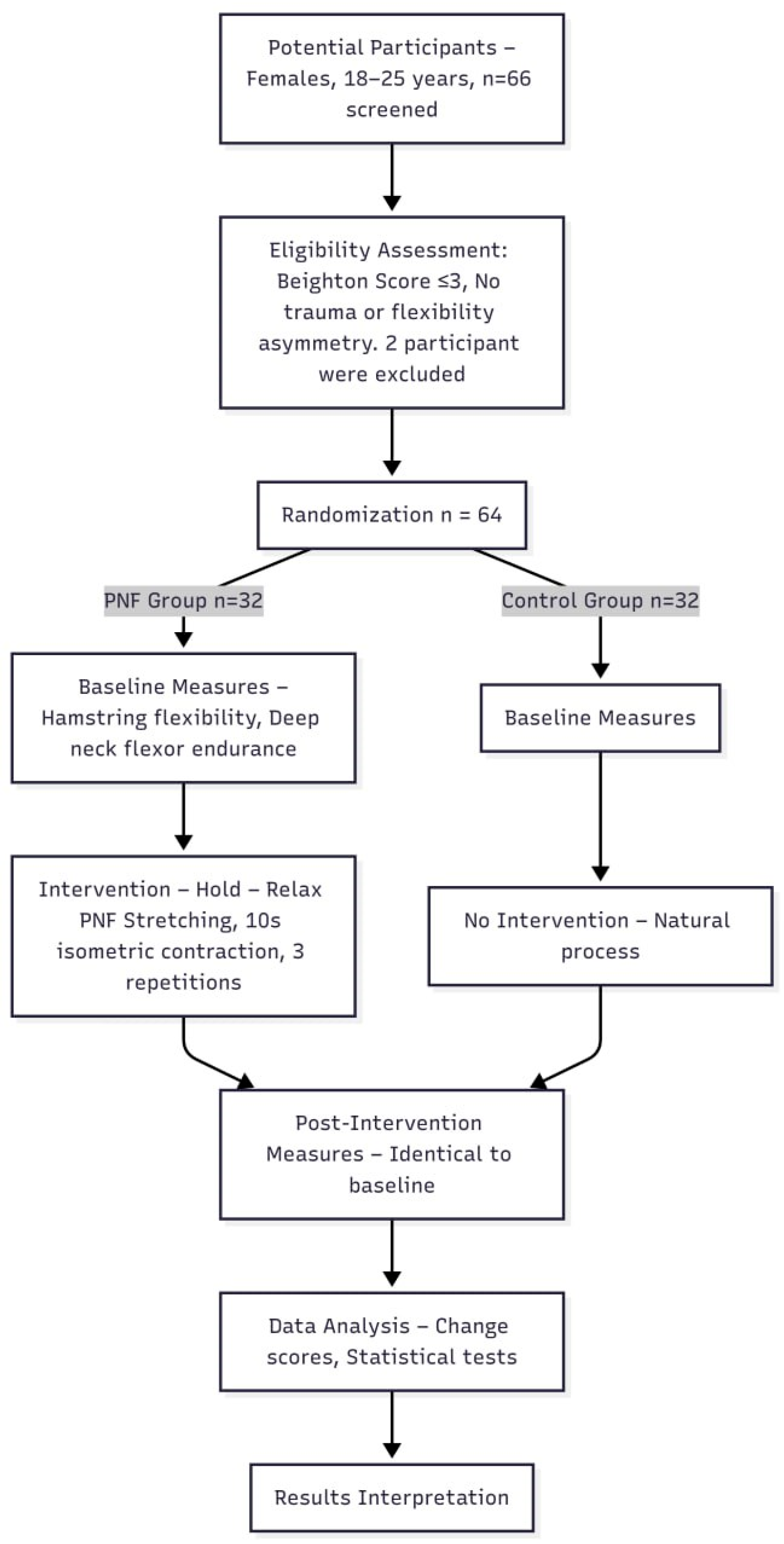
2. Methods and Methods
2.1. Study Design and Ethical Considerations
2.2. Population and Participant Selection
- −
- Standing forward flexion with knees extended and palms touching the floor (1 point).
- −
- Passive hyperextension of the fifth metacarpophalangeal joint beyond 90° (1 point per side, maximum 2 points).
- −
- Elbow hyperextension beyond 10° (1 point per side, maximum 2 points).
- −
- Passive opposition of the thumb to the volar aspect of the forearm (1 point per side, maximum 2 points).
- −
- Knee hyperextension beyond 10° (1 point per side, maximum 2 points).
2.3. Variables and Data Collection
2.4. Assessment Methods
2.5. Intervention Protocol
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dhiman, N.R.; Das, B.; Mohanty, C.; Singh, O.; Gyanpuri, V.; Raj, D. Myofascial release versus other soft tissue release techniques along superficial back line structures for improving flexibility in asymptomatic adults: A systematic review with meta-analysis. J. Bodyw. Mov. Ther. 2021, 28, 450–457. [Google Scholar] [CrossRef] [PubMed]
- Behnampour, M.; Barati, A.H.; Jafari, B.; Bahramian, M. The Effect of Immediate Self-Myofascial Release and Static Stretching of the Gastrocnemius Muscle and Plantar Fascia in the Superficial Back Line on Range of Motion and chronic Neck Pain: A Randomized Clinical Trial. J. Maz. Univ. Med. Sci. 2024, 34, 27–39. [Google Scholar]
- Dischiavi, S.L.; Wright, A.A.; Hegedus, E.J.; Bleakley, C.M. Biotensegrity and myofascial chains: A global approach to an integrated kinetic chain. Med. Hypotheses. 2018, 110, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Woźniacka, R.; Oleksy, Ł.; Jankowicz-Szymańska, A.; Mika, A.; Kielnar, R.; Stolarczyk, A. The association between symmetrical or asymmetrical high-arched feet and muscle fatigue in young women. Symmetry 2022, 14, 52. [Google Scholar] [CrossRef]
- Jung, M.; Kim, N.; Lee, Y. Immediate effect of hip hinge exercise stretching on flexibility of lower limb, pelvic tilting angle, proprioception and dynamic balance in individual with hamstring tightness. Phys. Ther. Rehabil. Sci. 2022, 11, 259–268. [Google Scholar] [CrossRef]
- Ozyurek, S.; Aktar, B.; Kosova, A.; Aydin, E.; Turedi, R.; Pekyavas, N.O. Effect of hamstring flexibility on cervical range of motion and deep neck flexor endurance in healthy young adults: A study to explore myofascial tensegrity network. J. Bodyw. Mov. Ther. 2024, 40, 662–668. [Google Scholar] [CrossRef]
- Ragia, M.K.; Safaa, M.S.; Saleh, P.D.; Marwa, S. Immediate effect of neurodynamic tensioner versus proprioceptive neuromuscular facilitation stretch on subjects with short hamstring syndrome. Med. J. Cairo Univ. 2021, 89, 627–634. [Google Scholar] [CrossRef]
- Bokaee, F.; Dehghan Manshadi, F. Performance of Longus Colli Muscle in Women with and without Forward Head Posture. Muscles Ligaments Tendons J. 2021, 11, 193–200. [Google Scholar] [CrossRef]
- Sikka, I.; Chawla, C.; Seth, S.; Alghadir, A.H.; Khan, M. Effects of Deep Cervical Flexor Training on Forward Head Posture, Neck Pain, and Functional Status in Adolescents Using Computer Regularly. Biomed. Res. Int. 2020, 2020, 8327565. [Google Scholar] [CrossRef]
- Jeong, E.-D.; Kim, C.-Y.; Kim, N.-H.; Kim, H.-D. Immediate effects of static and proprioceptive neuromuscular facilitation stretching of hamstring muscles on straight leg raise, craniovertebral angle, and cervical spine range of motion in neck pain patients with hamstring tightness: A prospective randomized controlled trial. J. Back Musculoskelet. Rehabil. 2022, 35, 429–438. [Google Scholar]
- Araujo, F.X.D.; Ferreira, G.E.; Scholl Schell, M.; Castro, M.P.D.; Ribeiro, D.C.; Silva, M.F. Measurement properties of the craniocervical flexion test: A systematic review. Phys. Ther. 2020, 100, 1094–1117. [Google Scholar] [CrossRef] [PubMed]
- Siracusa, R.; Paola, R.D.; Cuzzocrea, S.; Impellizzeri, D. Fibromyalgia: Pathogenesis, Mechanisms, Diagnosis and Treatment Options Update. Int. J. Mol. Sci. 2021, 22, 3891. [Google Scholar] [CrossRef]
- Faro, M.; Sàez-Francás, N.; Castro-Marrero, J.; Aliste, L.; Fernández De Sevilla, T.; Alegre, J. Gender Differences in Chronic Fatigue Syndrome. Reumatol. Clín. 2016, 12, 72–77. [Google Scholar] [CrossRef]
- Glenmark, B.; Nilsson, M.; Gao, H.; Gustafsson, J.-Å.; Dahlman-Wright, K.; Westerblad, H. Difference in skeletal muscle function in males vs. females: Role of estrogen receptor-β. Am. J. Physiol. Endocrinol. Metab. 2004, 287, E1125–E1131. [Google Scholar] [CrossRef] [PubMed]
- Haizlip, K.M.; Harrison, B.C.; Leinwand, L.A. Sex-based differences in skeletal muscle kinetics and fiber-type composition. Physiology 2015, 30, 30–39. [Google Scholar] [CrossRef] [PubMed]
- Malek, S.; Reinhold, E.J.; Pearce, G.S. The Beighton Score as a measure of generalised joint hypermobility. Rheumatol. Int. 2021, 41, 1707–1716. [Google Scholar] [CrossRef]
- Boyle, K.L.; Witt, P.; Riegger-Krugh, C. Intrarater and interrater reliability of the Beighton and Horan Joint Mobility Index. J. Athl. Train. 2003, 38, 281. [Google Scholar]
- Hyong, I.H.; Kang, J.H. The immediate effects of passive hamstring stretching exercises on the cervical spine range of motion and balance. J. Phys. Ther. Sci. 2013, 25, 113–116. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Tsiringakis, G.; Dimitriadis, Z.; Triantafylloy, E.; Mclean, S. Motor control training of deep neck flexors with pressure biofeedback improves pain and disability in patients with neck pain: A systematic review and meta-analysis. Musculoskelet. Sci. Pract. 2020, 50, 102220. [Google Scholar] [CrossRef]
- Kang, D.Y. Deep cervical flexor training with a pressure biofeedback unit is an effective method for maintaining neck mobility and muscular endurance in college students with forward head posture. J. Phys. Ther. Sci. 2015, 27, 3207–3210. [Google Scholar] [CrossRef] [PubMed]
- Lempke, L.; Wilkinson, R.; Murray, C.; Stanek, J. The effectiveness of PNF versus static stretching on increasing hip-flexion range of motion. J. Sport Rehabil. 2018, 27, 289–294. [Google Scholar] [CrossRef]
- Kuilart, K.E.; Woollam, M.; Barling, E.; Lucas, N. The active knee extension test and Slump test in subjects with perceived hamstring tightness. Int. J. Osteopath. Med. 2005, 8, 89–97. [Google Scholar] [CrossRef]
- Sadler, S.G.; Spink, M.J.; Ho, A.; De Jonge, X.J.; Chuter, V.H. Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: A systematic review of prospective cohort studies. BMC Musculoskelet. Disord. 2017, 18, 179. [Google Scholar] [CrossRef]
- Feland, J.B.; Myrer, J.; Merrill, R. Acute changes in hamstring flexibility: PNF versus static stretch in senior athletes. Phys. Ther. Sport. 2001, 2, 186–193. [Google Scholar] [CrossRef]
- Grieve, R.; Goodwin, F.; Alfaki, M.; Bourton, A.-J.; Jeffries, C.; Scott, H. The immediate effect of bilateral self myofascial release on the plantar surface of the feet on hamstring and lumbar spine flexibility: A pilot randomised controlled trial. J. Bodyw. Mov. Ther. 2015, 19, 544–552. [Google Scholar] [CrossRef]
- Ajimsha, M.; Shenoy, P.D.; Gampawar, N. Role of fascial connectivity in musculoskeletal dysfunctions: A narrative review. J. Bodyw. Mov. Ther. 2020, 24, 423–431. [Google Scholar] [CrossRef]
- Anggiat, L. The Effects of Proprioceptive Neuromuscular Facilitation and Mckenzie Method in Non-Specific Low Back Pain Among University Population. Ph.D. Thesis, KPJ Healthcare University College, Nilai, Malaysia, 2018. [Google Scholar]
- Naroz, H.; Fayaz, N.; Abdelmegeed, S.F.; Al Hamaky, D. Correlation between the Degree of Forward Head Posture and Hamstring Muscles Tightness in Non-Specific Neck Pain. Egypt. J. Hosp. Med. 2024, 94, 932–939. [Google Scholar]
- Krause, F.; Wilke, J.; Vogt, L.; Banzer, W. Intermuscular force transmission along myofascial chains: A systematic review. J. Anat. 2016, 228, 910–918. [Google Scholar] [CrossRef]
- Riaz, S.; Javed, A.; Liaqat, R.; Mohsin, F.; Hashim, A. Effects of Sub-Occipital Muscle Inhibition with and Without Hold Relax Agonist Contraction of Hamstrings on Pain, Disability and Craniovertebral Angle in Neck Pain Patients with Hamstring Tightness. J. Heal. Rehab. Res. 2024, 4, 984–989. [Google Scholar]
- Joshi, D.G.; Balthillaya, G.; Prabhu, A. Effect of remote myofascial release on hamstring flexibility in asymptomatic individuals–A randomized clinical trial. J. Bodyw. Mov. Ther. 2018, 22, 832–837. [Google Scholar] [CrossRef] [PubMed]
- Jeong, E.-D.; Kim, C.-Y.; Kim, S.-M.; Lee, S.-J.; Kim, H.-D. Short-term effects of the suboccipital muscle inhibition technique and cranio-cervical flexion exercise on hamstring flexibility, cranio-vertebral angle, and range of motion of the cervical spine in subjects with neck pain: A randomized controlled trial. J. Back Musculoskelet. Rehabil. 2018, 31, 1025–1034. [Google Scholar] [CrossRef] [PubMed]
- Fousekis, K.; Eid, K.; Tafa, E.; Gkrilias, P.; Mylonas, K.; Angelopoulos, P.; Koumoundourou, D.; Billis, V.; Tsepis, E. Can the application of the Ergon® IASTM treatment on remote parts of the superficial back myofascial line be equally effective with the local application for the improvement of the hamstrings’ flexibility? A randomized control study. J. Phys. Ther. Sci. 2019, 31, 508–511. [Google Scholar] [CrossRef] [PubMed]

| Groups | ||||
|---|---|---|---|---|
| Control (n = 32) | PNF (n = 32) | Test Statistic/ p (Between Groups) | Effect Size | |
| Age | 21 (21–22) | 22 (21–23) | U = 363.5/p = 0.038 ‡ | Cohen’s d = 0.537 |
| Sex, female | 32 (100.00%) | 32 (100.00%) | N/A | N/A |
| Height, m | 1.64 ± 0.07 | 1.65 ± 0.05 | t = −0.385/p = 0.702 † | Cohen’s d = 0.096 |
| Weight, kg | 59 (51.5–66) | 62.5 (57–72) | U = 399/p = 0.129 ‡ | Cohen’s d = 0.350 |
| Body mass index, kg/m2 | 22.30 ± 2.95 | 23.78 ± 4.53 | t = −1.547/p = 0.128 † | Cohen’s d = 0.387 |
| Beighton Hypermobility Score | ||||
| Score 0 | 20 (62.50%) | 24 (75.00%) | Exact = 3.698/p = 0.328 ¶ | Cramer’s V = 0.246 |
| Score 1 | 6 (18.75%) | 2 (6.25%) | ||
| Score 2 | 5 (15.63%) | 3 (9.38%) | ||
| Score 3 | 1 (3.13%) | 3 (9.38%) | ||
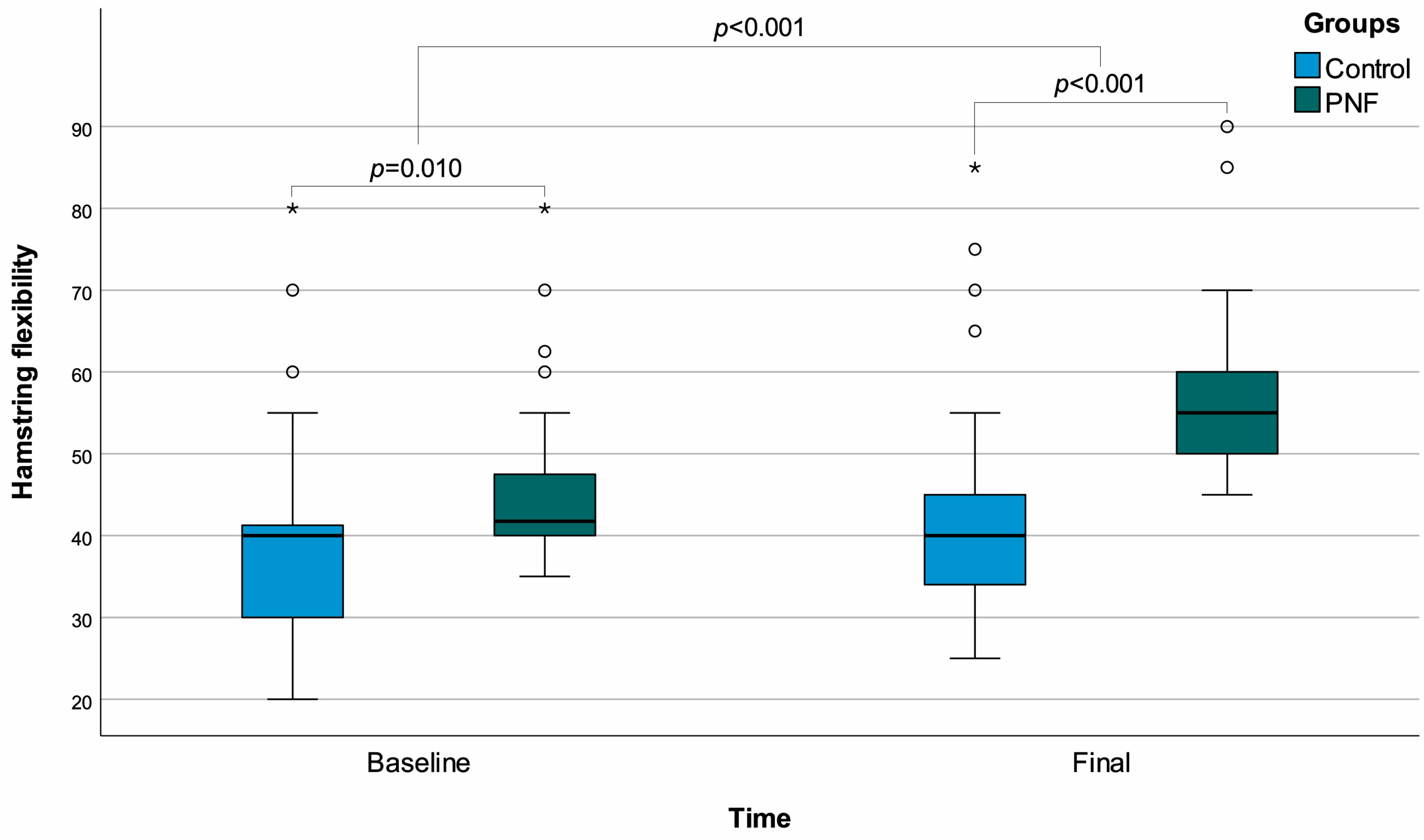
| Hamstring flexibility | ||||
| Baseline | 40 (30–41.25) | 41.75 (40–47.5) | U = 322.5/p = 0.010 ‡ | Cohen’s d = 0.397 |
| Final | 40 (34–45) | 55 (50–60) | U = 173/p < 0.001 ‡ | Cohen’s d = 1.097 |
| Test statistic p (within groups) | z = −3.905 p < 0.001 § | z = −5.068 p < 0.001 § | ||
| Effect size | Cohen’s d = 1.061 | Cohen’s d = 3.458 | ||
| Change (a) | 2.5 (0–5) | 10 (10–14.5) | U = 9/p < 0.001 ‡ | Cohen’s d = 3.310 |
| Deep neck flexor endurance | ||||
| Baseline | 15.5 (8.5–21) | 17.5 (7.5–42) | U = 443/p = 0.353 ‡ | Cohen’s d = 0.448 |
| Final | 17 (11.5–25.5) | 24 (13–50) | U = 384/p = 0.085 ‡ | Cohen’s d = 0.592 |
| Test statistic p (within groups) | z = −4.478 p < 0.001 § | z = −4.292 p < 0.001 § | ||
| Effect size | Cohen’s d = 1.352 | Cohen’s d = 0.940 | ||
| Change (a) | 2 (1–4) | 3.5 (0.5–6.5) | U = 426/p = 0.244 ‡ | Cohen’s d = 0.546 |
| All Individuals (n = 64) | Control Group (n = 32) | PNF Group (n = 32) | ||||
|---|---|---|---|---|---|---|
| r | p | r | p | r | p | |
| Age | −0.045 | 0.724 | −0.206 | 0.259 | −0.036 | 0.844 |
| Height, m | 0.089 | 0.484 | −0.148 | 0.419 | 0.234 | 0.196 |
| Weight, kg | 0.093 | 0.465 | 0.128 | 0.486 | 0.064 | 0.729 |
| Body mass index, kg/m2 | 0.054 | 0.669 | 0.211 | 0.247 | −0.066 | 0.721 |
| Beighton Hypermobility Score | −0.115 | 0.365 | −0.031 | 0.868 | −0.156 | 0.392 |
| Hamstring flexibility, baseline | −0.072 | 0.571 | −0.077 | 0.677 | −0.176 | 0.335 |
| Hamstring flexibility, final | −0.023 | 0.857 | −0.145 | 0.427 | −0.157 | 0.391 |
| Hamstring flexibility, change | 0.054 | 0.670 | −0.301 | 0.094 | −0.061 | 0.742 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kosova, A.; Pala, O.O. Does Proprioceptive Neuromuscular Facilitation-Based Hamstring Stretching Influence Deep Cervical Flexor Muscle Endurance? Life 2025, 15, 1019. https://doi.org/10.3390/life15071019
Kosova A, Pala OO. Does Proprioceptive Neuromuscular Facilitation-Based Hamstring Stretching Influence Deep Cervical Flexor Muscle Endurance? Life. 2025; 15(7):1019. https://doi.org/10.3390/life15071019
Chicago/Turabian StyleKosova, Altay, and Omer Osman Pala. 2025. "Does Proprioceptive Neuromuscular Facilitation-Based Hamstring Stretching Influence Deep Cervical Flexor Muscle Endurance?" Life 15, no. 7: 1019. https://doi.org/10.3390/life15071019
APA StyleKosova, A., & Pala, O. O. (2025). Does Proprioceptive Neuromuscular Facilitation-Based Hamstring Stretching Influence Deep Cervical Flexor Muscle Endurance? Life, 15(7), 1019. https://doi.org/10.3390/life15071019







