Exploring Disorders of Gut–Brain Interaction in Schoolchildren and Adolescents with Autism
Abstract
:1. Introduction
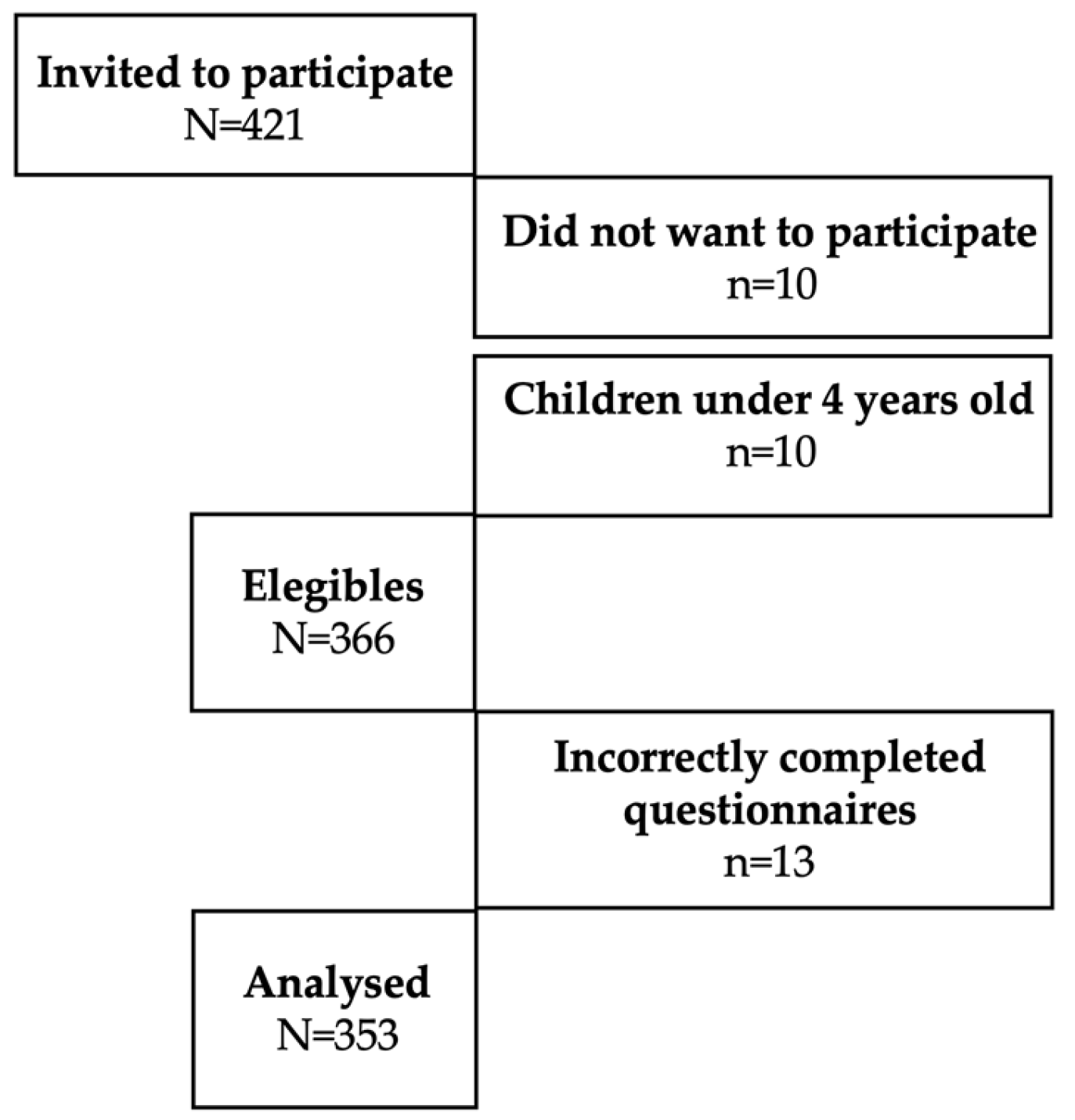
2. Materials and Methods
3. Results
3.1. Prevalence
3.2. Possible Associations
3.3. Validation and Internal Consistency of the QPGS IV in Spanish for ASD
3.4. Main Digestive Symptoms Identified
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| DGBIs | Disorders of Gut–Brain Interaction |
| ASD | Autism Spectrum Disorder |
| SA | South America |
| CA | Central America |
| OR | Odds ratio |
| BMI | Body Mass Index |
| FC | Functional constipation |
| QPGS IV | Questionnaire for Pediatric Gastrointestinal Symptoms Rome IV |
| FINDERS | Functional International Digestive Epidemiological Research Survey |
| DSM-V | Diagnostic Statistical Manual of Mental Disorders |
| LASPGHAN | Latin America Society of Paediatric Gastroenterology, Hepatology, and Nutrition |
| FD | Functional dyspepsia |
| FAP | Functional abdominal pain |
References
- Kasarello, K.; Cudnoch-Jedrzejewska, A.; Czarzasta, K. Communication of gut microbiota and brain via immune and neuroendocrine signaling. Front. Microbiol. 2023, 14, 1118529. [Google Scholar] [CrossRef] [PubMed]
- Velasco-Benítez, C.A.; Collazos-Saa, L.I.; García-Perdomo, H.A. A systematic review and meta-analysis in schoolchildren and adolescents with functional gastrointestinal disorders according to Rome IV criteria. Arq. Gastroenterol. 2022, 59, 304–313. [Google Scholar] [CrossRef]
- Drossman, D.A. Functional gastrointestinal disorders: History, pathophysiology, clinical features and Rome IV. Gastroenterology 2016, 150, 1262–1279. [Google Scholar] [CrossRef]
- Dargenio, V.N.; Dargenio, C.; Castellaneta, S.; De Giacomo, A.; Laguardia, M.; Schettini, F.; Francavilla, R.; Cristofori, F. Intestinal barrier dysfunction and microbiota-gut-brain axis: Possible implications in the pathogenesis and treatment of autism spectrum disorder. Nutrients 2023, 15, 1620. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2014. [Google Scholar]
- Lasheras, I.; Real-López, M.; Santabárbara, J. Prevalence of gastrointestinal symptoms in autism spectrum disorder: A meta-analysis. An. Pediatr. 2023, 99, 102–110. [Google Scholar] [CrossRef]
- Morton, J.T.; Jin, D.-M.; Mills, R.H.; Shao, Y.; Rahman, G.; McDonald, D.; Zhu, Q.; Balaban, M.; Jiang, Y.; Cantrell, K.; et al. Multi-level analysis of the gut-brain axis shows autism spectrum disorder-associated molecular and microbial profiles. Nat. Neurosci. 2023, 26, 1208–1217. [Google Scholar] [CrossRef]
- Velasco-Benítez, C.A.; Ortíz-Rivera, C.J.; Sánchez-Pérez, M.P.; Játiva-Mariño, E.; Villamarín-Betancourt, E.A.; Saps, M. Utilidad de los cuestionarios de Roma IV en español para identificar desórdenes gastrointestinales funcionales en pediatría. Grupo de trabajo de la Sociedad Latinoamericana de Gastroenterología, Hepatología y Nutrición Pediátrica (SLAGHNP). Acta Gastroenterol. Latinoam. 2019, 49, 259–296. [Google Scholar]
- Saps, M.; Nichols-Vinueza, D.X.; Mintjens, S.; Pusatcioglu, C.K.; Velasco-Benítez, C.A. Construct validity of the pediatric Rome III criteria. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 577–581. [Google Scholar] [CrossRef]
- Zimmet, P.; Alberti, K.G.M.; Kaufman, F.; Tajima, N.; Silink, M.; Arslanian, S.; Wong, G.; Bennet, P.; Shaw, J.; Caprio, S.; et al. The metabolic syndrome in children and adolescents—An IDF consensus report. Pediatr. Diabetes 2007, 8, 299–306. [Google Scholar] [CrossRef]
- Vargas, M.E.; Souki, A.; Ruiz, G.; García, D.; Mengual, E.; Gonzalez, C.C.; Chavez, M.; Gonzalez, M. Percentiles de circunferencia de cintura en niños y adolescentes del municipio de Maracaibo del Estado Zulia, Venezuela. An. Venez. 2011, 24, 13–20. [Google Scholar]
- Collins, L.M. Research Design and Methods; Elsevier Inc.: Pennsylvania, PA, USA, 2007; pp. 419–429. [Google Scholar]
- Barbosa, E.Y. A neurodidactic model for teaching elementary EFL students in a college context. Engl. Lang. Teach. 2021, 14, 42. [Google Scholar] [CrossRef]
- Baaleman, D.F.; Velasco-Benítez, C.A.; Méndez-Guzmán, L.M.; Benninga, M.A.; Saps, M. Can we rely on the Rome IV questionnaire to diagnose children with functional gastrointestinal disorders? J. Neurogastroenterol. Motil. 2021, 27, 626–631. [Google Scholar] [CrossRef]
- Velasco-Benítez, C. Trastornos Digestivos Funcionales En Pediatría, 1st ed.; Grupo Distribuna: Bogota, Colombia, 2022; pp. 4–5. [Google Scholar]
- Robin, S.G.; Keller, C.; Zwiener, R.; Hyman, P.E.; Nurko, S.; Saps, M.; Di Lorenzo, C.; Shulman, R.J.; Hyams, J.S.; Palsson, O.; et al. Prevalence of pediatric functional gastrointestinal disorders utilizing the Rome IV criteria. J. Pediatr. 2018, 195, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Selimović, A.; Mekić, N.; Terzić, S.; Ćosićkić, A.; Zulić, E.; Mehmedović, M. Functional gastrointestinal disorders in children: A single centre experience. Med. Glas. 2024, 21, 112–117. [Google Scholar] [CrossRef]
- Cenni, S.; Pensabene, L.; Dolce, P.; Campanozzi, A.; Salvatore, S.; Pujia, R.; Serra, M.R.; Scarpato, E.; Miele, E.; Staiano, A.; et al. Prevalence of functional gastrointestinal disorders in Italian children living in different regions: Analysis of the difference and the role of diet. Dig. Liver Dis. 2023, 55, 1640–1646. [Google Scholar] [CrossRef]
- Aydın, Ö.G.; Baykara, H.B.; Akın, K.; Kahveci, S.; Şeker, G.; Güler, Y.; Öztürk, Y. Evaluation of functional gastrointestinal disorders in children aged 4–10 years with autism spectrum disorder. Turk. J. Pediatr. 2024, 66, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Saurman, V.; Margolis, K.G.; Luna, R.A. Autism spectrum disorder as a brain-gut-microbiome axis disorder. Dig. Dis. Sci. 2020, 65, 818–828. [Google Scholar] [CrossRef] [PubMed]
- Rego, R.M.P.; Machado, N.C.; Carvalho, M.A.; Graffunder, J.S.; Ortolan, E.V.P.; Lourenção, P.L.T.A. Transcutaneous posterior tibial nerve stimulation in children and adolescents with functional constipation: A protocol for an interventional study. Medicine 2019, 98, e17755. [Google Scholar] [CrossRef]
- Yu, Z.T.; Song, J.M.; Qiao, L.; Wang, Y.; Chen, Y.; Wang, E.H.; Zhang, S.C. A randomized, double-blind, controlled trial of percutaneous tibial nerve stimulation with pelvic floor exercises in the treatment of childhood constipation. Am. J. Gastroenterol. 2023, 118, 553–560. [Google Scholar] [CrossRef]
- Di Lorenzo, C.; Nurko, S.; Hyams, J.S.; Rodriguez-Araujo, G.; Almansa, C.; Shakhnovich, V.; Saps, M.; Simon, M. Randomized controlled trial of linaclotide in children aged 6-17 years with functional constipation. J. Pediatr. Gastroenterol. Nutr. 2024, 78, 1059–1068. [Google Scholar] [CrossRef]
- Di Lorenzo, C.; Robert, J.; Rodriguez-Araujo, G.; Shakhnovich, V.; Xie, W.; Nurko, S.; Saps, M. Safety and efficacy of linaclotide in children aged 2–5 years with functional constipation: Phase 2, randomized study. J. Pediatr. Gastroenterol. Nutr. 2024, 79, 510–518. [Google Scholar] [CrossRef]
- Di Lorenzo, C.; Khlevner, J.; Rodriguez-Araujo, G.; Xie, W.; Huh, S.Y.; Ando, M.; Hyams, J.S.; Nurko, S.; Benninga, M.A.; Simon, M.; et al. Efficacy and safety of linaclotide in treating functional constipation in paediatric patients: A randomised, double-blind, placebo-controlled, multicentre, phase 3 trial. Lancet Gastroenterol. Hepatol. 2024, 9, 238–250. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.N.; Zhang, K.; Xiong, Y.Y.; Liu, S. The relationship between functional constipation and overweight/obesity in children: A systematic review and meta-analysis. Pediatr. Res. 2023, 94, 1878–1886. [Google Scholar] [CrossRef] [PubMed]
- Koppen, I.J.N.; Velasco-Benítez, C.A.; Benninga, M.A.; Di Lorenzo, C.; Saps, M. Is there an association between functional constipation and excessive bodyweight in children? J. Pediatr. 2016, 171, 178–182.e1. [Google Scholar] [CrossRef]
- Hill, P.; Muir, J.G.; Gibson, P.R. Controversies and Recent Developments of the Low-FODMAP Diet. Gastroenterol. Hepatol. 2017, 13, 36–45. [Google Scholar]
- Hakime, N.; Walton, J.; Roberts, K.M.; Nahikian-Nelms, M.; Witwer, A.N. The Effect of the Low FODMAP Diet on Gastrointestinal Symptoms, Behavioral Problems and Nutrient Intake in Children with Autism Spectrum Disorder: A Randomized Controlled Pilot Trial. J. Autism Dev. Disord. 2021, 51, 2800–2811. [Google Scholar]
- Saad, K.; Shabaan, I.; Hassan, A.E.M.M.; Ezzat, M.; Abouzed, M.A.; Hamed, Y.; Fahmy, M.; Gad, E.F. Gluten-Free, Casein-Free Diet for Children with Autism Spectrum Disorder: A Case-Controlled Study. J. Pharm. Biallied Sci. 2024, 16, S905–S908. [Google Scholar] [CrossRef]
- Bourne, L.; Mandy, W.; Bryant-Waugh, R. Avoidant/restrictive food intake disorder and severe food selectivity in children and young people with autism: A scoping review. Dev. Med. Child. Neurol. 2022, 64, 691–700. [Google Scholar] [CrossRef]
- Raju, S.; Hepsibah, P.E.V.; Niharika, M.K. Quality of life in parents of children with Autism spectrum disorder: Emphasizing challenges in the Indian context. Int. J. Dev. Disabil. 2023, 69, 371–378. [Google Scholar] [CrossRef]
- Musetti, A.; Manari, T.; Dioni, B.; Raffin, C.; Bravo, G.; Mariani, R.; Esposito, G.; Dimitriou, D.; Plazzi, G.; Franceschini, C.; et al. Parental Quality of Life and Involvement in Intervention for Children or Adolescents with Autism Spectrum Disorders: A Systematic Review. J. Pers. Med. 2021, 11, 894. [Google Scholar] [CrossRef]
- Rodakis, J. An n=1 case report of a child with autism improving on antibiotics and a father’s quest to understand what it may mean. Microb. Ecol. Health Dis. 2015, 26, 26382. [Google Scholar] [CrossRef] [PubMed]
- Iglesias-Vázquez, L.; Van Ginkel Riba, G.; Arija, V.; Canals, J. Composition of gut microbiota in children with autism spectrum disorder: A systematic review and meta-analysis. Nutrients 2020, 12, 792. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.; Zhang, Q.; Sun, J.; Li, Q.; Li, D.; Zhu, M.; Fu, X.; Zhao, L.; Wang, M.; Lou, X.; et al. A comparison between children and adolescents with autism spectrum disorders and healthy controls in biomedical factors, trace elements, and microbiota biomarkers: A meta-analysis. Front. Psychiatry 2024, 14, 1318637. [Google Scholar] [CrossRef] [PubMed]
- Ma, B.; Liang, J.; Dai, M.; Wang, J.; Luo, J.; Zhang, Z.; Jing, J. Altered Gut Microbiota in Chinese Children With Autism Spectrum Disorders. Front. Cell Infect. Microbiol. 2019, 9, 40. [Google Scholar] [CrossRef]
- Wang, L.; Christophersen, C.T.; Sorich, M.J.; Gerber, J.P.; Angley, M.T.; Conlon, M.A. Low relative abundances of the mucolytic bacterium Akkermansia muciniphila and Bifidobacterium spp. in feces of children with autism. Appl. Environ. Microbiol. 2011, 77, 6718–6721. [Google Scholar] [CrossRef]
- Strati, F.; Cavalieri, D.; Albanese, D.; De Felice, C.; Donati, C.; Hayek, J.; Jousson, O.; Leoncini, S.; Renzi, D.; Calabrò, A.; et al. New evidences on the altered gut microbiota in autism spectrum disorders. Microbiome 2017, 5, 24. [Google Scholar] [CrossRef]
- Argou-Cardozo, I.; Zeidán-Chuliá, F. Clostridium Bacteria and Autism Spectrum Conditions: A Systematic Review and Hypothetical Contribution of Environmental Glyphosate Levels. Med. Sci. 2018, 6, 29. [Google Scholar] [CrossRef]
- Zang, P. Influence of Foods and Nutrition on the Gut Microbiome and Implications for Intestinal Health. Int. J. Mol. Sci. 2022, 23, 9588. [Google Scholar]
- Berding, K.; Donovan, S.M. Diet Can Impact Microbiota Composition in Children With Autism Spectrum Disorder. Front. Neurosci. 2018, 12, 515. [Google Scholar] [CrossRef]
- Sanctuary, M.R.; Kain, J.N.; Chen, S.Y.; Kalanetra, K.; Lemay, D.G.; Rose, D.R.; Yang, H.T.; Tancredi, D.J.; German, J.B.; Slupsky, C.M.; et al. Pilot study of probiotic/colostrum supplementation on gut function in children with autism and gastrointestinal symptoms. PLoS ONE 2019, 14, e0210064. [Google Scholar] [CrossRef]
- Patusco, R.; Ziegler, J. Role of probiotics in managing gastrointestinal dysfunction in children with autism spectrum disorder: An update for practitioners. Adv. Nutr. 2018, 9, 637–650. [Google Scholar] [CrossRef] [PubMed]
- Dossaji, Z.; Khattak, A.; Tun, K.M.; Hsu, M.; Batra, K.; Hong, A.S. Efficacy of fecal microbiota transplant on behavioral and gastrointestinal symptoms in pediatric autism: A systematic review. Microorganisms 2023, 11, 806. [Google Scholar] [CrossRef]
- Yu, Y.; Wang, W.; Zhang, F. The next generation fecal microbiota transplantation: To transplant bacteria or virome. Adv. Sci. 2023, 10, e2301097. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, S.; Li, Y.; Joneja, S.; Hsu, S. Experiences of racism and racial disparities in health care among children and youth with autism and their caregivers: A systematic review. Disabil. Rehabil. 2025, 47, 1061–1080. [Google Scholar] [CrossRef] [PubMed]
- Lai, K.Y.C.; Leung, P.W.L.; Hung, S.F.; Shea, C.K.S.; Mo, F.; Che, K.K.I.; Tse, C.Y.; Lau, F.L.F.; Ma, S.L.; Wu, J.C.Y.; et al. Gastrointestinal problems in Chinese children with autism spectrum disorder. Neuropsychiatr. Dis. Treat. 2020, 16, 1807–1815. [Google Scholar] [CrossRef]
- Gan, H.; Su, Y.; Zhang, L.; Huang, G.; Lai, C.; Lv, Y.; Li, Y. Questionnaire-based analysis of autism spectrum disorders and gastrointestinal symptoms in children and adolescents: A systematic review and meta-analysis. Front. Pediatr. 2023, 11, 1120728. [Google Scholar] [CrossRef]
- Restrepo, B.; Angkustsiri, K.; Taylor, S.L.; Rogers, S.J.; Cabral, J.; Heath, B.; Hechtman, A.; Solomon, M.; Ashwood, P.; Amaral, D.G.; et al. Developmental-behavioral profiles in children with autism spectrum disorder and co-occurring gastrointestinal symptoms. Autism Res. 2020, 13, 1778–1789. [Google Scholar] [CrossRef]
- Holingue, C.; Poku, O.; Pfeiffer, D.; Murray, S.; Fallin, M.D. Gastrointestinal concerns in children with autism spectrum disorder: A qualitative study of family experiences. Autism 2022, 26, 1698–1711. [Google Scholar] [CrossRef]
- Holingue, C.; Kalb, L.G.; Musci, R.; Lukens, C.; Lee, L.-C.; Kaczaniuk, J.; Landrum, M.; Buie, T.; Fallin, M.D. Characteristics of the autism spectrum disorder gastrointestinal and related behaviors inventory in children. Autism Res. 2022, 15, 1142–1155. [Google Scholar] [CrossRef]
- Bandini, L.G.; Curtin, C.; Phillips, S.; Anderson, S.E.; Maslin, M.; Must, A. Changes in food selectivity in children with autism spectrum disorder. J. Autism Dev. Disord. 2017, 47, 439–446. [Google Scholar] [CrossRef]
| All (N = 353) | 4–10 Years Old (n = 242) | 11–18 Years Old (n = 111) | |
|---|---|---|---|
| Sociodemographic variables | |||
| Age (years) | |||
| Mean SD | 9.0 ± 3.7 | 6.8 ± 1.8 | 13.7 ± 2.4 |
| Range | 4–18 | 4–10 | 11–18 |
| Age groups (years) n (%) | |||
| Schoolchildren (8–12) | 290 (82.2) | 242 (100.0) | 48 (43.2) |
| Adolescents (13–18) | 63 (17.8) | 0 (0.0) | 63 (56.8) |
| Sex n (%) | |||
| Female | 75 (21.3) | 47 (19.4) | 28 (25.2) |
| Male | 278 (78.8) | 195 (80.6) | 83 (74.8) |
| Race n (%) | |||
| White | 198 (56.1) | 132 (54.5) | 66 (59.5) |
| Mixed race | 144 (40.8) | 100 (41.3) | 44 (39.6) |
| Afro-descendant | 7 (2.0) | 7 (2.9) | 0 (0.0) |
| Indigenous | 4 (1.1) | 3 (1.2) | 1 (0.9) |
| Country n (%) | |||
| South America | 148 (41.9) | 102 (42.1) | 46 (41.4) |
| Argentina | 82 (23.2) | 61 (25.2) | 21 (18.9) |
| Colombia | 66 (18.7) | 41 (16.9) | 25 (22.5) |
| Central America | 205 (58.1) | 140 (57.9) | 65 (58.6) |
| Costa Rica | 52 (14.7) | 33 (13.6) | 19 (17.1) |
| El Salvador | 47 (13.3) | 39 (16.1) | 8 (7.2) |
| Mexico | 50 (14.2) | 30 (12.4) | 20 (18.0) |
| Panama | 56 (15.9) | 38 (15.7) | 18 (16.2) |
| Type of school n (%) | |||
| Public | 48 (13.6) | 31 (12.8) | 17 (15.3) |
| Private | 280 (79.3) | 192 (79.3) | 88 (79.3) |
| Does not attend school | 25 (7.1) | 19 (7.9) | 6 (5.4) |
| All (N = 353) | 4–10 Years Old (n = 242) | 11–18 Years Old (n = 111) | p | |
|---|---|---|---|---|
| Clinical variables n (%) | ||||
| Caesarean section | ||||
| No | 150 (42.5) | 98 (40.5) | 52 (46.9) | 0.158 |
| Yes | 203 (57.5) | 144 (59.5) | 59 (53.1) | |
| Prematurity | ||||
| No | 292 (82.7) | 202 (83.5) | 90 (81.1) | 0.341 |
| Yes | 61 (17.3) | 40 (16.5) | 21 (18.9) | |
| Level of autism according to DSM-5 | ||||
| I | ||||
| No | 99 (28.1) | 67 (27.7) | 32 (28.8) | 0.552 |
| Yes | 81 (22.9) | 55 (22.7) | 26 (23.4) | |
| II | ||||
| No | 110 (31.2) | 74 (30.6) | 36 (32.4) | 0.494 |
| Yes | 70 (19.8) | 48 (19.8) | 22 (19.8) | |
| III | ||||
| No | 151 (42.8) | 103 (42.6) | 48 (43.2) | 0.466 |
| Yes | 29 (8.2) | 19 (7.9) | 10 (9.0) | |
| Not classified yet or do not know at the time of the study | ||||
| No | 180 (51.0) | 122 (50.4) | 58 (52.2) | 0.418 |
| Yes | 173 (49.0) | 120 (49.6) | 53 (47.8) | |
| Comorbidity | ||||
| No | 268 (75.9) | 188 (77.7) | 80 (72.1) | 0.156 |
| Yes | 85 (24.1) | 54 (22.3) | 31 (27.9) | |
| Altered nutritional status | ||||
| No | 198 (56.1) | 134 (55.4) | 64 (57.7) | 0.388 |
| Yes | 155 (43.9) | 108 (44.6) | 38 (42.3) | |
| Family variables n (%) | ||||
| Only child | ||||
| No | 238 (67.4) | 158 (65.3) | 80 (72.1) | 0.127 |
| Yes | 115 (32.6) | 84 (34.7) | 31 (27.9) | |
| Firstborn | ||||
| No | 160 (45.3) | 113 (46.7) | 47 (42.3) | 0.259 |
| Yes | 193 (54.7) | 129 (53.3) | 64 (57.7) | |
| Separated/divorced parents | ||||
| No | 261 (73.9) | 193 (79.8) | 68 (61.3) | 0.000 |
| Yes | 92 (26.1) | 49 (20.2) | 43 (38.7) | |
| DGBIs intra-family | ||||
| No | 339 (96.0) | 232 (95.9) | 107 (96.4) | 0.536 |
| Yes | 14 (4.0) | 10 (4.1) | 4 (3.6) | |
| Autism in the family | ||||
| No | 335 (94.9) | 230 (95.0) | 105 (94.6) | 0.521 |
| Yes | 18 (5.1) | 12 (5.0) | 6 (5.4) | |
| All (N = 353) | 4–10 Years Old (n = 242) | 11–18 Years Old (n = 111) | |
|---|---|---|---|
| DGBIs n (%) | |||
| No | 145 (41.1) | 99 (40.9) | 46 (41.4) |
| Yes | 208 (58.9) | 143 (59.1) | 65 (58.6) |
| Associated with nausea and vomiting | 10 (2.9) | 6 (2.4) | 4 (3.6) |
| Functional vomiting | 6 (1.7) | 2 (0.8) | 4 (3.6) |
| Cyclic vomiting | 1 (0.3) | 1 (0.4) | 0 (0.0) |
| Rumination | 2 (0.6) | 2 (0.8) | 0 (0.0) |
| Aerophagia | 1 (0.3) | 1 (0.4) | 0 (0.0) |
| Associated with abdominal pain | 100 (28.3) | 69 (28.5) | 31 (27.9) |
| Functional dyspepsia | 77 (21.8) | 55 (22.7) | 22 (19.8) |
| Postprandial | 74 (21.0) | 53 (21.9) | 21 (18.9) |
| Epigastric | 2 (0.6) | 1 (0.4) | 1 (0.9) |
| Irritable bowel syndrome | 5 (1.4) | 5 (2.1) | 0 (0.0) |
| IBS with diarrhoea | 1 (0.3) | 1 (0.4) | 0 (0.0) |
| IBS with constipation | 4 (1.1) | 4 (1.7) | 0 (0.0) |
| Abdominal migraine | 2 (0.6) | 1 (0.4) | 1 (0.9) |
| Functional abdominal pain not otherwise specified | 16 (4.5) | 8 (3.3) | 8 (7.2) |
| Associated with defecation | 98 (27.8) | 68 (28.1) | 30 (27.0) |
| Functional constipation | 96 (27.2) | 67 (27.7) | 29 (26.1) |
| Non-retentive faecal incontinence | 2 (0.6) | 1 (0.4) | 1 (0.9) |
| DGBIs | OR | 95% CI | p | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| 145 (41.1) | 208 (58.9) | ||||
| Sociodemographic variables | |||||
| Age groups | |||||
| Schoolchildren | 120 (82.8) | 170 (81.7) | 1.00 | 0.8040 | |
| Adolescents | 25 (17.2) | 38 (18.3) | 1.07 | 0.59–1.95 | |
| Sex | |||||
| Female | 31 (21.4) | 44 (21.2) | 1.00 | 0.9594 | |
| Male | 114 (78.6) | 164 (78.8) | 1.01 | 0.58–1.75 | |
| Race | |||||
| White | |||||
| No | 64 (44.1) | 91 (43.8) | 1.00 | 0.9424 | |
| Yes | 81 (55.9) | 117 (56.2) | 1.01 | 0.64–1.59 | |
| Mixed race | |||||
| No | 91 (62.8) | 118 (56.7) | 1.00 | 0.2569 | |
| Yes | 54 (37.2) | 90 (43.3) | 1.28 | 0.81–2.03 | |
| Afro-descendant | |||||
| No | 138 (95.2) | 208 (100.0) | n/a | ||
| Yes | 7 (4.8) | 0 (0.0) | |||
| Indigenous | |||||
| No | 142 (97.9) | 207 (99.5) | 1.00 | 0.1655 | |
| Yes | 3 (2.1) | 1 (0.5) | 0.22 | 0.004–2.89 | |
| Type of school | |||||
| Public | |||||
| No | 122 (84.1) | 183 (88.0) | 1.00 | 0.3001 | |
| Yes | 23 (15.9) | 25 (12.0) | 0.72 | 0.37–1.40 | |
| Private | |||||
| No | 34 (23.5) | 39 (18.7) | 1.00 | 0.2836 | |
| Yes | 111 (76.5) | 169 (81.3) | 1.32 | 0.76–2.30 | |
| Does not attend school | |||||
| No | 134 (94.4) | 194 (93.3) | 1.00 | 0.7579 | |
| Yes | 11 (5.6) | 14 (6.7) | 0.87 | 0.35–2.21 | |
| Country | |||||
| South America | |||||
| No | 70 (48.3) | 135 (64.9) | 1.00 | 0.0018 | |
| Yes | 75 (51.7) | 73 (35.1) | 0.50 | 0.31–0.79 | |
| Argentina | |||||
| No | 110 (75.9) | 161 (77.4) | 1.00 | 0.7358 | |
| Yes | 35 (24.1) | 47 (22.6) | 0.91 | 0.54–1.56 | |
| Colombia | |||||
| No | 105 (72.4) | 182 (87.5) | 1.00 | 0.0003 | |
| Yes | 40 (27.6) | 26 (12.5) | 0.37 | 0.20–0.67 | |
| Central America | |||||
| No | 75 (51.7) | 73 (35.1) | 1.00 | 0.0018 | |
| Yes | 70 (48.3) | 135 (64.9) | 1.98 | 1.25–3.12 | |
| Panama | |||||
| No | 126 (86.9) | 171 (82.2) | 1.00 | 0.2359 | |
| Yes | 19 (13.1) | 37 (17.8) | 1.43 | 0.76–2.77 | |
| El Salvador | |||||
| No | 123 (84.3) | 183 (88.0) | 1.00 | 0.3909 | |
| Yes | 22 (15.2) | 25 (12.0) | 0.76 | 0.39–1.49 | |
| Costa Rica | |||||
| No | 130 (89.7) | 171 (82.2) | 1.00 | 0.0522 | |
| Yes | 15 (10.3) | 37 (17.8) | 1.87 | 0.95–3.83 | |
| Mexico | |||||
| No | 131 (90.3) | 172 (82.7) | 1.00 | 0.0425 | |
| Yes | 14 (9.7) | 36 (17.3) | 1.95 | 0.98–4.09 | |
| Clinical variables | |||||
| Caesarean section | |||||
| No | 58 (40.0) | 92 (44.2) | 1.00 | 0.4289 | |
| Yes | 87 (60.0) | 116 (55.8) | 0.84 | 0.53–1.32 | |
| Prematurity | |||||
| No | 118 (81.4) | 174 (83.7) | 1.00 | 0.5782 | |
| Yes | 27 (18.6) | 34 (16.4) | 0.85 | 0.47–1.55 | |
| Level of autism according to DSM-5 | |||||
| I | |||||
| No | 37 (56.9) | 62 (53.9) | 1.00 | 0.6966 | |
| Yes | 28 (43.1) | 53 (46.1) | 1.12 | 0.58–2.18 | |
| II | |||||
| No | 39 (60.0) | 71 (61.7) | 1.00 | 0.8182 | |
| Yes | 26 (40.0) | 44 (38.3) | 0.92 | 0.47–1.82 | |
| III | |||||
| No | 54 (83.1) | 97 (84.4) | 1.00 | 0.8237 | |
| Yes | 11 (16.9) | 18 (15.6) | 0.91 | 0.37–2.30 | |
| Not classified yet or do not know at the time of the study | |||||
| No | 65 (44.8) | 115 (55.3) | 1.00 | 0.0531 | |
| Yes | 80 (55.2) | 93 (44.7) | 0.65 | 0.41–1.02 | |
| Comorbidity | |||||
| No | 112 (77.2) | 156 (75.0) | 1.00 | 0.6280 | |
| Yes | 33 (22.8) | 52 (25.0) | 1.13 | 0.66–1.93 | |
| Altered nutritional status | |||||
| No | 84 (57.9) | 114 (54.8) | 1.00 | 0.5607 | |
| Yes | 61 (42.1) | 94 (45.2) | 1.13 | 0.72–1.78 | |
| Family variables | |||||
| Only child | |||||
| No | 97 (66.9) | 141 (67.8) | 1.00 | 0.8604 | |
| Yes | 48 (33.1) | 67 (32.2) | 0.96 | 0.59–1.55 | |
| Firstborn | |||||
| No | 67 (46.2) | 93 (44.7) | 1.00 | 0.7813 | |
| Yes | 78 (53.8) | 115 (55.3) | 1.06 | 0.67–1.66 | |
| Separated/divorced parents | |||||
| No | 110 (75.9) | 151 (72.6) | 1.00 | 0.4916 | |
| Yes | 35 (24.1) | 57 (27.4) | 1.18 | 0.70–1.99 | |
| DGBIs intra-family | |||||
| No | 142 (97.9) | 197 (94.7) | 1.00 | 0.1273 | |
| Yes | 3 (2.1) | 11 (5.3) | 2.64 | 0.67–14.98 | |
| Autism in the family | |||||
| No | 138 (95.2) | 197 (94.7) | 1.00 | 0.8464 | |
| Yes | 7 (4.8) | 11 (5.3) | 1.10 | 0.37–3.43 | |
| Alpha De Cronbach | Interpretation | |
|---|---|---|
| Total questionnaire | 0.7818 | High |
| Section A | 0.7331 | High |
| Section B | 0.4706 | Moderate |
| Section C | 0.6535 | High |
| Section D | 0.6110 | High |
| Section E | 0.6367 | High |
| Symptom | n (%) |
|---|---|
| Flatus | 178 (50.4) |
| Painful stool | 126 (35.7) |
| Large stools | 108 (30.6) |
| History of large faecal mass in rectum | 94 (26.6) |
| Hard stools | 84 (23.8) |
| Belching | 84 (23.8) |
| Stool retention | 78 (22.1) |
| Soiling | 73 (20.7) |
| Abdominal pain around and below belly button | 68 (19.3) |
| Early satiation | 66 (18.7) |
| Abdominal pain above belly button | 53 (15.0) |
| Abdominal distension | 48 (13.6) |
| Watery stools | 28 (7.9) |
| Swallowing air | 26 (7.4) |
| Nausea | 25 (7.1) |
| Heartburn | 16 (4.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Velasco-Benítez, C.A.; Rojas-Cerón, C.A.; Ortiz-Rivera, C.J.; Velasco-Suárez, D.A.; Juvinao-Quintero, M.C.; Zubiri, C.E.; Fernández, J.M.; Bigliardi, R.; Zosi, A.; Chanis Águila, R.A.; et al. Exploring Disorders of Gut–Brain Interaction in Schoolchildren and Adolescents with Autism. Life 2025, 15, 912. https://doi.org/10.3390/life15060912
Velasco-Benítez CA, Rojas-Cerón CA, Ortiz-Rivera CJ, Velasco-Suárez DA, Juvinao-Quintero MC, Zubiri CE, Fernández JM, Bigliardi R, Zosi A, Chanis Águila RA, et al. Exploring Disorders of Gut–Brain Interaction in Schoolchildren and Adolescents with Autism. Life. 2025; 15(6):912. https://doi.org/10.3390/life15060912
Chicago/Turabian StyleVelasco-Benítez, Carlos Alberto, Christian Andrés Rojas-Cerón, Claudia Jimena Ortiz-Rivera, Daniela Alejandra Velasco-Suárez, María Carolina Juvinao-Quintero, Cecilia Elena Zubiri, Julián Martín Fernández, Román Bigliardi, Anabella Zosi, Ricardo A. Chanis Águila, and et al. 2025. "Exploring Disorders of Gut–Brain Interaction in Schoolchildren and Adolescents with Autism" Life 15, no. 6: 912. https://doi.org/10.3390/life15060912
APA StyleVelasco-Benítez, C. A., Rojas-Cerón, C. A., Ortiz-Rivera, C. J., Velasco-Suárez, D. A., Juvinao-Quintero, M. C., Zubiri, C. E., Fernández, J. M., Bigliardi, R., Zosi, A., Chanis Águila, R. A., Guzmán Acevedo, C., Reynoso Zarzosa, F. A., & Zablah Cordova, R. A. (2025). Exploring Disorders of Gut–Brain Interaction in Schoolchildren and Adolescents with Autism. Life, 15(6), 912. https://doi.org/10.3390/life15060912







