Evaluation of Mandibular Fixation Techniques Using Monocortical Plates After Mandibular Setback Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
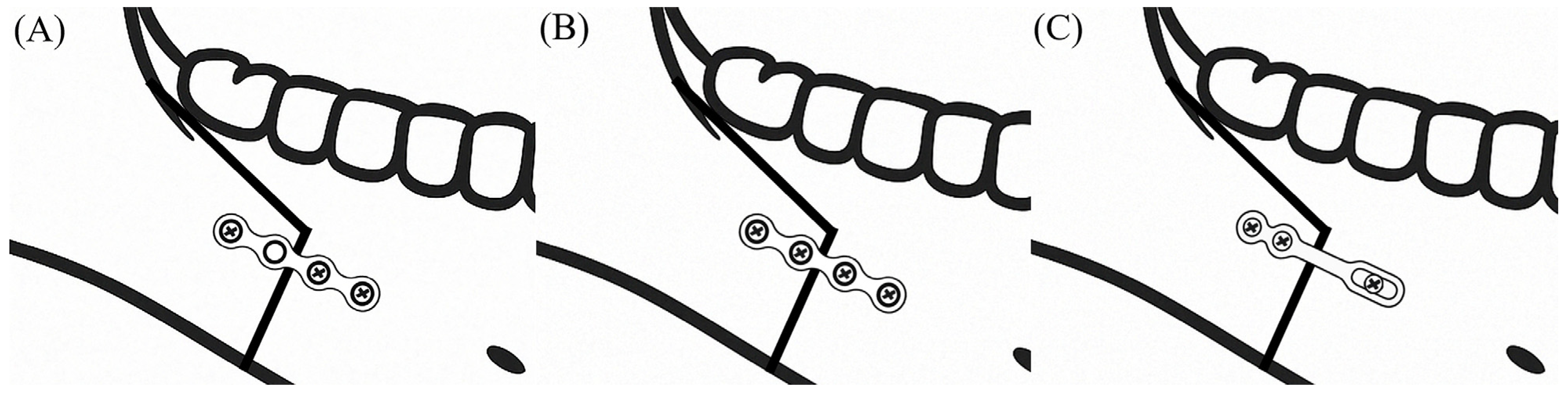
2.2. Preoperative Planning and Surgical Procedure
2.3. Data Acquisition
2.4. Measuring the Movements of the Proximal Segment and Relapse
2.5. Statistical Analysis
3. Results
3.1. Postoperative Rotational Movement of the Proximal Segment
3.2. Relapses of the Distal Segment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chung, I.H.; Yoo, C.K.; Lee, E.K.; Ihm, J.A.; Park, C.J.; Lim, J.S.; Hwang, K.G. Postoperative stability after sagittal split ramus osteotomies for a mandibular setback with monocortical plate fixation or bicortical screw fixation. J. Oral Maxillofac. Surg. 2008, 66, 446–452. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.I.; Cho, B.H.; Jung, Y.H.; Son, W.S.; Park, S.B. Cone-beam computerized tomography evaluation of condylar changes and stability following two-jaw surgery: Le Fort I osteotomy and mandibular setback surgery with rigid fixation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2011, 111, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Stoelinga, P.J.; Borstlap, W.A. The fixation of sagittal split osteotomies with miniplates: The versatility of a technique. J. Oral Maxillofac. Surg. 2003, 61, 1471–1476. [Google Scholar] [CrossRef] [PubMed]
- Proffit, W.R.; Phillips, C.; Dann, C.T.; Turvey, T.A. Stability after surgical-orthodontic correction of skeletal Class III malocclusion. I. Mandibular setback. Int. J. Adult Orthodon. Orthognath. Surg. 1991, 6, 7–18. [Google Scholar]
- Ureturk, E.U.; Apaydin, A. Does fixation method affects temporomandibular joints after mandibular advancement? J. Craniomaxillofac. Surg. 2018, 46, 923–931. [Google Scholar] [CrossRef]
- Ueki, K.; Hashiba, Y.; Marukawa, K.; Alam, S.; Nakagawa, K.; Yamamoto, E. Skeletal stability after mandibular setback surgery: Bicortical fixation using a 2.0-mm locking plate system versus monocortical fixation using a nonlocking plate system. J. Oral Maxillofac. Surg. 2008, 66, 900–904. [Google Scholar] [CrossRef]
- Kabasawa, Y.; Sato, M.; Kikuchi, T.; Sato, Y.; Takahashi, Y.; Higuchi, Y.; Omura, K. Analysis and comparison of clinical results of bilateral sagittal split ramus osteotomy performed with the use of monocortical locking plate fixation or bicortical screw fixation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 116, e333–e341. [Google Scholar] [CrossRef]
- Ueki, K.; Okabe, K.; Marukawa, K.; Mukozawa, A.; Moroi, A.; Miyazaki, M.; Sotobori, M.; Ishihara, Y.; Yoshizawa, K.; Ooi, K. Skeletal stability after mandibular setback surgery: Comparison between the hybrid technique for fixation and the conventional plate fixation using an absorbable plate and screws. J. Craniomaxillofac. Surg. 2014, 42, 351–355. [Google Scholar] [CrossRef]
- Ueki, K.; Moroi, A.; Yoshizawa, K.; Hotta, A.; Tsutsui, T.; Fukaya, K.; Hiraide, R.; Takayama, A.; Tsunoda, T.; Saito, Y. Comparison of skeletal stability after sagittal split ramus osteotomy among mono-cortical plate fixation, bi-cortical plate fixation, and hybrid fixation using absorbable plates and screws. J. Craniomaxillofac. Surg. 2017, 45, 178–182. [Google Scholar] [CrossRef]
- Larson, B.E.; Lee, N.K.; Jang, M.J.; Jo, D.W.; Yun, P.Y.; Kim, Y.K. Comparative evaluation of the sliding plate technique for fixation of a sagittal split ramus osteotomy: Finite element analysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 123, e148–e152. [Google Scholar] [CrossRef]
- Choi, B.J.; Choi, Y.H.; Lee, B.S.; Kwon, Y.D.; Choo, Y.J.; Ohe, J.Y. A CBCT study on positional change in mandibular condyle according to metallic anchorage methods in skeletal class III patients after orthognatic surgery. J. Craniomaxillofac. Surg. 2014, 42, 1617–1622. [Google Scholar] [CrossRef] [PubMed]
- Ghang, M.H.; Kim, H.M.; You, J.Y.; Kim, B.H.; Choi, J.P.; Kim, S.H.; Choung, P.H. Three-dimensional mandibular change after sagittal split ramus osteotomy with a semirigid sliding plate system for fixation of a mandibular setback surgery. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Ku, J.K.; Choi, S.K.; Lee, J.G.; Yu, H.C.; Kim, S.Y.; Kim, Y.K.; Shin, Y.; Lee, N.K. Analysis of Sagittal Position Changes of the Condyle After Mandibular Setback Surgery Across the Four Different Types of Plating Systems. J. Craniofac. Surg. 2021, 32, 2441–2445. [Google Scholar] [CrossRef] [PubMed]
- Roh, Y.C.; Shin, S.H.; Kim, S.S.; Sandor, G.K.; Kim, Y.D. Skeletal stability and condylar position related to fixation method following mandibular setback with bilateral sagittal split ramus osteotomy. J. Craniomaxillofac. Surg. 2014, 42, 1958–1963. [Google Scholar] [CrossRef]
- Baek, R.M.; Lee, S.W. A new condyle repositionable plate for sagittal split ramus osteotomy. J. Craniofac. Surg. 2010, 21, 489–490. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Ellis, E. Stability of bicortical screw versus plate fixation after mandibular setback with the bilateral sagittal split osteotomy: A systematic review and meta-analysis. Int. J. Oral Maxillofac. Surg. 2016, 45, 1–7. [Google Scholar] [CrossRef]
- Lee, J.Y.; Kim, Y.K.; Yun, P.Y.; Lee, N.K.; Kim, J.W.; Choi, J.H. Evaluation of stability after orthognathic surgery with minimal orthodontic preparation: Comparison according to 3 types of fixation. J. Craniofac. Surg. 2014, 25, 911–915. [Google Scholar] [CrossRef]
- Kim, S.S.; Kwak, K.H.; Ko, C.C.; Park, S.B.; Son, W.S.; Kim, Y.I. Comparison of postoperative changes in the distal and proximal segments between conventional and sliding mini-plate fixation following mandibular setback. Korean J. Orthod. 2016, 46, 372–378. [Google Scholar] [CrossRef]
- Lee, H.G.; Agpoon, K.J.; Besana, A.N.; Lim, H.K.; Jang, H.S.; Lee, E.S. Mandibular stability using sliding or conventional four-hole plates for fixation after bilateral sagittal split ramus osteotomy for mandibular setback. Br. J. Oral Maxillofac. Surg. 2017, 55, 378–382. [Google Scholar] [CrossRef]
- Jung, J.; Kim, J.H.; Lee, J.W.; Ohe, J.Y.; Choi, B.J. Three-dimensional volumetric analysis of condylar head and glenoid cavity after mandibular advancement. J. Craniomaxillofac. Surg. 2018, 46, 1470–1475. [Google Scholar] [CrossRef]
- Stella, J.P.; Astrand, P.; Epker, B.N. Patterns and etiology of relapse after correction of Class III open bite via subcondylar ramus osteotomy. Int. J. Adult Orthod. Orthognath. Surg. 1986, 1, 91–99. [Google Scholar]
- Reyneke, J.P.; Ferretti, C. Intraoperative diagnosis of condylar sag after bilateral sagittal split ramus osteotomy. Br. J. Oral Maxillofac. Surg. 2002, 40, 285–292. [Google Scholar] [CrossRef] [PubMed]
- An, S.B.; Park, S.B.; Kim, Y.I.; Son, W.S. Effect of post-orthognathic surgery condylar axis changes on condylar morphology as determined by 3-dimensional surface reconstruction. Angle Orthod. 2014, 84, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Park, S.B.; Yang, Y.M.; Kim, Y.I.; Cho, B.H.; Jung, Y.H.; Hwang, D.S. Effect of bimaxillary surgery on adaptive condylar head remodeling: Metric analysis and image interpretation using cone-beam computed tomography volume superimposition. J. Oral Maxillofac. Surg. 2012, 70, 1951–1959. [Google Scholar] [CrossRef]
- Ha, M.H.; Kim, Y.I.; Park, S.B.; Kim, S.S.; Son, W.S. Cone-beam computed tomographic evaluation of the condylar remodeling occurring after mandibular set-back by bilateral sagittal split ramus osteotomy and rigid fixation. Korean J. Orthod. 2013, 43, 263–270. [Google Scholar] [CrossRef]
- Zupnik, J.T.; Ioshida, M.; Yatabe, M.; Ruellas, A.C.O.; Gomes, L.R.; Aronovich, S.; Benavides, E.; Edwards, S.P.; Paniagua, B.; Cevidanes, L.H.S. Three-dimensional analysis of condylar changes in surgical correction for open bite patients with skeletal class II and class III malocclusions. Int. J. Oral Maxillofac. Surg. 2019, 48, 739–745. [Google Scholar] [CrossRef]
- Kim, H.M.; Baek, S.H.; Kim, T.Y.; Choi, J.Y. Evaluation of three-dimensional position change of the condylar head after orthognathic surgery using computer-aided design/computer-aided manufacturing-made condyle positioning jig. J. Craniofac. Surg. 2014, 25, 2002–2007. [Google Scholar] [CrossRef]
- Li, J.; Ryu, S.Y.; Park, H.J.; Kook, M.S.; Jung, S.; Han, J.J.; Oh, H.K. Changes in condylar position after BSSRO with and Without Le Fort I osteotomy via surgery-first approach in mandibular prognathism with facial asymmetry. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2017, 123, 661–669. [Google Scholar] [CrossRef]
- Wang, T.; Han, J.J.; Oh, H.K.; Park, H.J.; Jung, S.; Kook, M.S. Comparison of Orthodontics-First and Surgery-First Approach in Positional Changes of the Condyle After Mandibular Setback Surgery Using Three-Dimensional Analysis. J. Oral Maxillofac. Surg. 2016, 74, 2487–2496. [Google Scholar] [CrossRef]
- Choi, B.J.; Kim, B.S.; Lim, J.M.; Jung, J.; Lee, J.W.; Ohe, J.Y. Positional change in mandibular condyle in facial asymmetric patients after orthognathic surgery: Cone-beam computed tomography study. Maxillofac. Plast. Reconstr. Surg. 2018, 40, 13. [Google Scholar] [CrossRef]
- Park, J.B.; Jin, I.G.; Han, J.J.; Hwang, S.J. Postoperative relapse after mandibular setback surgery with perioperative counterclockwise rotation of the mandibular proximal segment. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 121, 609–617. [Google Scholar] [CrossRef] [PubMed]
- Fujioka, M.; Fujii, T.; Hirano, A. Comparative study of mandibular stability after sagittal split osteotomies: Biocortical versus monocortical osteosynthesis. Cleft Palate Craniofac. J. 2000, 37, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Ellis, E., III; Esmail, N. Malocclusions resulting from loss of fixation after sagittal split ramus osteotomies. J. Oral Maxillofac. Surg. 2009, 67, 2528–2533. [Google Scholar] [CrossRef] [PubMed]


| Variable | Group 1 | Group 2 | Group 3 | p-Value |
|---|---|---|---|---|
| Subject (male/female) | 25 (12/13) | 40 (22/18) | 28 (17/11) | 0.653 |
| Age (years) | 24.5 ± 7.0 | 22.7 ± 4.9 | 22.9 ± 4.8 | 0.431 |
| Amount of mandibular setback (mm) | 4.8 | 5.6 | 5.6 | 0.095 |
| Group 1 | Group 2 | Group 3 | p-Value | |
|---|---|---|---|---|
| Yaw movement (°) | ||||
| T2–T1 | 1.66 (±4.17) a | 1.75 (±3.38) a | 1.53 (±3.30) a | 0.939 |
| T3–T2 | −0.11 (±2.65) a | −0.37 (±2.90) a | 0.69 (±3.11) a | 0.105 |
| T3–T1 | 1.55 (±4.08) a | 1.38 (±3.28) a | 2.22 (±3.77) a | 0.404 |
| Roll movement (°) | ||||
| T2–T1 | 2.24 (±5.01) a | 0.99 (±1.75) a | 0.80 (±2.49) a | 0.039 * |
| T3–T2 | −0.17 (±2.10) a | 0.32 (±1.40) a | −0.02 (±2.25) a | 0.316 |
| T3–T1 | 2.06 (±4.60) a | 1.31 (±1.86) a | 0.78 (±2.72) a | 0.099 |
| Pitch movement (°) | ||||
| T2–T1 | 2.74 (±1.76) a | 1.74 (±1.98) b | 1.89 (±2.38) ab | 0.021 * |
| T3–T2 | 0.12 (±1.28) a | 0.12 (±1.18) a | 0.19 (±1.47) a | 0.947 |
| T3–T1 | 2.86 (±1.78) a | 1.86 (±1.87) b | 2.07 (±2.78) ab | 0.035 * |
| Group 1 | Group 2 | Group 3 | p-Value | |
|---|---|---|---|---|
| Horizontal relapse (mm) | ||||
| T2–T1 | 0.98 (±1.56) a | 1.61 (±1.84) ab | 1.99 (±1.87) b | 0.015 * |
| T3–T2 | −0.01 (±1.07) a | 0.40 (±0.92) a | 0.04 (±0.99) a | 0.034 * |
| T3–T1 | 0.97 (±2.10) a | 2.01 (±1.94) b | 2.03 (±2.10) b | 0.009 * |
| Vertical relapse (mm) | ||||
| T2–T1 | 0.12 (±1.55) a | 1.05 (±1.55) a | 1.03 (±1.69) a | 0.051 |
| T3–T2 | −0.09 (±0.97) a | −0.04 (±0.87) a | 0.26 (±0.94) a | 0.304 |
| T3–T1 | 0.03 (±1.62) a | 1.01 (±1.50) b | 1.29 (±1.61) b | 0.011 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-W.; Jeong, B.-J.; Jung, J. Evaluation of Mandibular Fixation Techniques Using Monocortical Plates After Mandibular Setback Surgery. Life 2025, 15, 845. https://doi.org/10.3390/life15060845
Lee S-W, Jeong B-J, Jung J. Evaluation of Mandibular Fixation Techniques Using Monocortical Plates After Mandibular Setback Surgery. Life. 2025; 15(6):845. https://doi.org/10.3390/life15060845
Chicago/Turabian StyleLee, Seung-Woo, Bong-Jin Jeong, and Junho Jung. 2025. "Evaluation of Mandibular Fixation Techniques Using Monocortical Plates After Mandibular Setback Surgery" Life 15, no. 6: 845. https://doi.org/10.3390/life15060845
APA StyleLee, S.-W., Jeong, B.-J., & Jung, J. (2025). Evaluation of Mandibular Fixation Techniques Using Monocortical Plates After Mandibular Setback Surgery. Life, 15(6), 845. https://doi.org/10.3390/life15060845





