Innovative Strategies in the Diagnosis and Treatment of Liver Cirrhosis and Associated Syndromes
Abstract
1. Introduction
2. Methodology
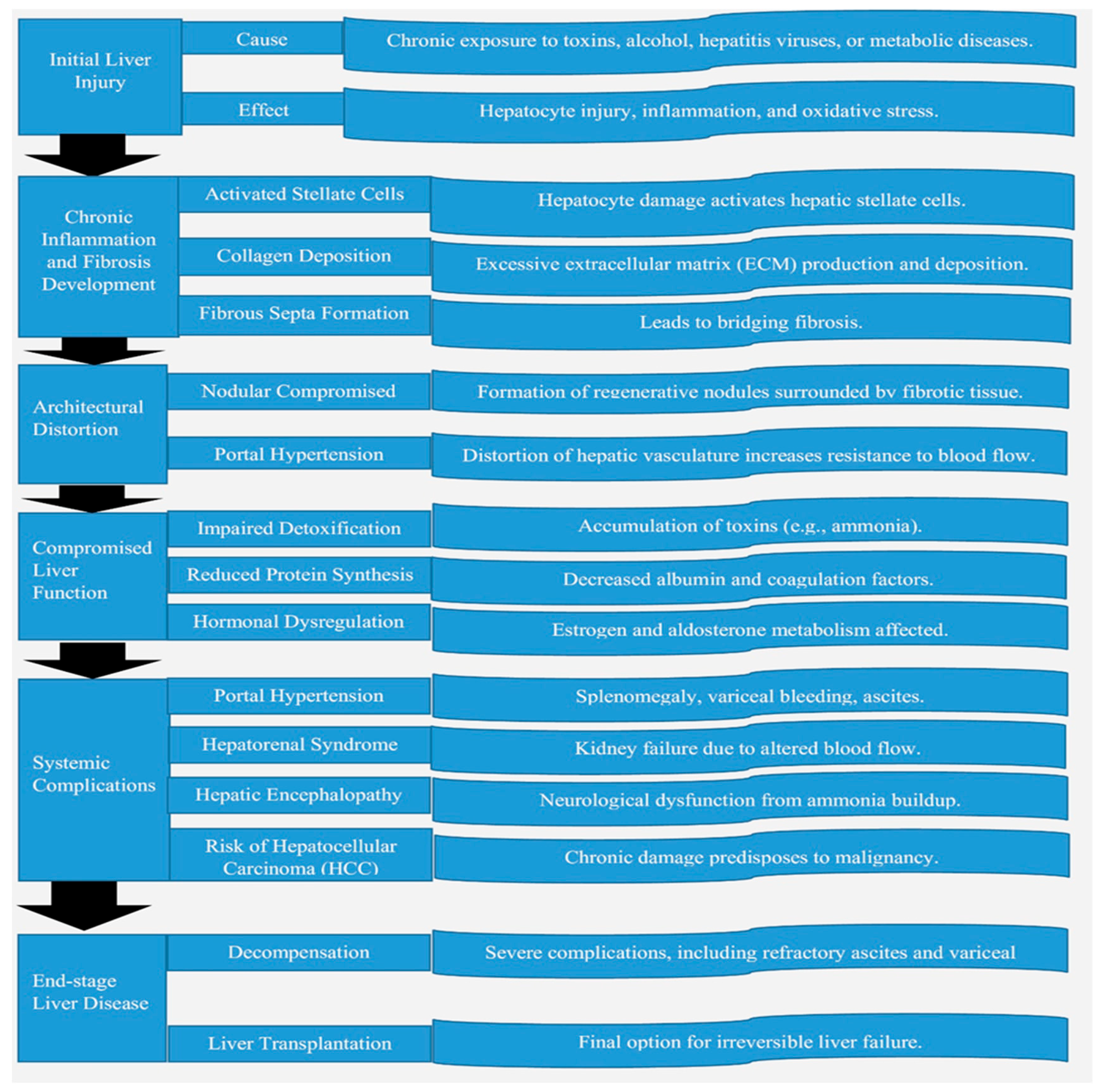
3. Pathophysiology of Liver Cirrhosis
3.1. Mechanisms Leading to Liver Cirrhosis
3.2. Common Etiologies of Liver Cirrhosis
3.2.1. Viral Hepatitis
3.2.2. Alcoholic Liver Disease (ALD)
3.2.3. Genetic Disorders
4. Advances in Diagnosis of Liver Cirrhosis
4.1. Non-Invasive Diagnostic Tools
4.2. Imaging Techniques
4.3. Molecular and Genomic Approaches
5. Innovative Treatment Modalities for Liver Cirrhosis
5.1. Pharmacological Therapies
5.2. Endoscopic Interventions
5.3. Transplantation Advances
5.4. Regenerative Medicines
6. Managing Associated Syndromes of Liver Cirrhosis
6.1. Portal Hypertension
6.2. Ascites
6.3. Hepatic Encephalopathy
6.4. Hepatorenal Syndrome
7. Role of Prognostic Scoring in Liver Cirrhosis
7.1. Scoring Systems and Integration of New Biomarkers
7.2. Integration of New Biomarkers into Prognostic Models
8. Future Directions in Liver Cirrhosis Management
8.1. Role of AI and Machine Learning in Early Diagnosis
Applications in Liver Cirrhosis Diagnosis
8.2. Precision Medicine Approaches
Key Developments in Precision Medicine
8.3. Emerging Therapies Under Clinical Trials: Therapies Targeting Fibrosis
9. Challenges in Implementing Innovative Strategies for Liver Cirrhosis
9.1. Costs of Advanced Diagnostics and Therapies
9.2. Limitations of Current Diagnostic and Therapeutic Approaches
9.2.1. Diagnostic Limitations
9.2.2. Therapeutic Limitations
9.3. Addressing Disparities in Global Healthcare
Global Disparities
10. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Pellicoro, A.; Ramachandran, P.; Iredale, J.P.; Fallowfield, J.A. Liver fibrosis and repair: Immune regulation of wound healing in a solid organ. Nat. Rev. Immunol. 2014, 14, 181–194. [Google Scholar] [CrossRef]
- Asrani, S.K.; Devarbhavi, H.; Eaton, J.; Kamath, P.S. Burden of liver diseases in the world. J. Hepatol. 2019, 70, 151–171. [Google Scholar] [CrossRef] [PubMed]
- Mokdad, A.A.; Lopez, A.D.; Shahraz, S.; Lozano, R.; Mokdad, A.H.; Stanaway, J.; Murray, C.J.; Naghavi, M. Liver cirrhosis mortality in 187 countries between 1980 and 2010: A systematic analysis. BMC Med. 2014, 12, 145. [Google Scholar] [CrossRef] [PubMed]
- Abd El-Kader, S.M.; El-Den Ashmawy, E.M. Non-alcoholic fatty liver disease: The diagnosis and management. World J. Hepatol. 2015, 7, 846–858. [Google Scholar] [CrossRef] [PubMed]
- Arroyo, V.; Moreau, R.; Kamath, P.S.; Jalan, R.; Ginès, P.; Nevens, F.; Fernández, J.; To, U.; García-Tsao, G.; Schnabl, B. Acute-on-chronic liver failure in cirrhosis. Nat. Rev. Dis. Primers 2016, 2, 16041. [Google Scholar] [CrossRef]
- Devarbhavi, H.; Asrani, S.K.; Arab, J.P.; Nartey, Y.A.; Pose, E.; Kamath, P.S. Global burden of liver disease: 2023 update. J. Hepatol. 2023, 79, 516–537. [Google Scholar] [CrossRef]
- Xiao, S.; Xie, W.; Zhang, Y.; Lei, L.; Pan, Y. Changing epidemiology of cirrhosis from 2010 to 2019: Results from the Global Burden Disease study 2019. Ann. Med. 2023, 55, 2252326. [Google Scholar] [CrossRef]
- Mitra, S.; De, A.; Chowdhury, A. Epidemiology of non-alcoholic and alcoholic fatty liver diseases. Transl. Gastroenterol. Hepatol. 2020, 5, 16. [Google Scholar] [CrossRef]
- Pinzani, M. Pathophysiology of Liver Fibrosis. Dig. Dis. 2015, 33, 492–497. [Google Scholar] [CrossRef]
- Forbes, S.J.; Newsome, P.N. Liver regeneration—Mechanisms and models to clinical application. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 473–485. [Google Scholar] [CrossRef]
- Kisseleva, T.; Brenner, D. Molecular and cellular mechanisms of liver fibrosis and its regression. Nat. Rev. Gastroenterol. Hepatol. 2021, 18, 151–166. [Google Scholar] [CrossRef] [PubMed]
- Elpek, G.Ö. Cellular and molecular mechanisms in the pathogenesis of liver fibrosis: An update. World J. Gastroenterol. 2014, 20, 7260–7276. [Google Scholar] [CrossRef] [PubMed]
- Cao, L.; Quan, X.B.; Zeng, W.J.; Yang, X.O.; Wang, M.J. Mechanism of Hepatocyte Apoptosis. J. Cell Death 2016, 9, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Tsuchida, T.; Friedman, S.L. Mechanisms of hepatic stellate cell activation. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 397–411. [Google Scholar] [CrossRef]
- Čoma, M.; Fröhlichová, L.; Urban, L.; Zajíček, R.; Urban, T.; Szabo, P.; Novák, Š.; Fetissov, V.; Dvořánková, B.; Smetana, K., Jr.; et al. Molecular Changes Underlying Hypertrophic Scarring Following Burns Involve Specific Deregulations at All Wound Healing Stages (Inflammation, Proliferation and Maturation). Int. J. Mol. Sci. 2021, 22, 897. [Google Scholar] [CrossRef]
- Okazaki, I.; Noro, T.; Tsutsui, N.; Yamanouchi, E.; Kuroda, H.; Nakano, M.; Yokomori, H.; Inagaki, Y. Fibrogenesis and Carcinogenesis in Nonalcoholic Steatohepatitis (NASH): Involvement of Matrix Metalloproteinases (MMPs) and Tissue Inhibitors of Metalloproteinase (TIMPs). Cancers 2014, 6, 1220–1255. [Google Scholar] [CrossRef]
- Lee, M.J. A review of liver fibrosis and cirrhosis regression. J. Pathol. Transl. Med. 2023, 57, 189–195. [Google Scholar] [CrossRef]
- Zhou, W.C.; Zhang, Q.B.; Qiao, L. Pathogenesis of liver cirrhosis. World J. Gastroenterol. 2014, 20, 7312–7324. [Google Scholar] [CrossRef]
- Petruzziello, A. Epidemiology of Hepatitis B Virus (HBV) and Hepatitis C Virus (HCV) Related Hepatocellular Carcinoma. Open Virol. J. 2018, 12, 26–32. [Google Scholar] [CrossRef]
- Lamontagne, R.J.; Bagga, S.; Bouchard, M.J. Hepatitis B virus molecular biology and pathogenesis. Hepatoma Res. 2016, 2, 163–186. [Google Scholar] [CrossRef]
- Moretti, R.; Giuffrè, M.; Merli, N.; Caruso, P.; Di Bella, S.; Tiribelli, C.; Crocè, L.S. Hepatitis C Virus-Related Central and Peripheral Nervous System Disorders. Brain Sci. 2021, 11, 1569. [Google Scholar] [CrossRef] [PubMed]
- Ginès, P.; Krag, A.; Abraldes, J.G.; Solà, E.; Fabrellas, N.; Kamath, P.S. Liver cirrhosis. Lancet 2021, 398, 1359–1376. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Zhang, T.; Kusumanchi, P.; Han, S.; Yang, Z.; Liangpunsakul, S. Alcohol Metabolizing Enzymes, Microsomal Ethanol Oxidizing System, Cytochrome P450 2E1, Catalase, and Aldehyde Dehydrogenase in Alcohol-Associated Liver Disease. Biomedicines 2020, 8, 50. [Google Scholar] [CrossRef] [PubMed]
- Galicia-Moreno, M.; Gutiérrez-Reyes, G. The role of oxidative stress in the development of alcoholic liver disease. Rev. Gastroenterol. Mex. 2014, 79, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Slevin, E.; Baiocchi, L.; Wu, N.; Ekser, B.; Sato, K.; Lin, E.; Ceci, L.; Chen, L.; Lorenzo, S.R.; Xu, W.; et al. Kupffer Cells: Inflammation Pathways and Cell-Cell Interactions in Alcohol-Associated Liver Disease. Am. J. Pathol. 2020, 190, 2185–2193. [Google Scholar] [CrossRef]
- Tacke, F.; Weiskirchen, R. Non-alcoholic fatty liver disease (NAFLD)/non-alcoholic steatohepatitis (NASH)-related liver fibrosis: Mechanisms, treatment and prevention. Ann. Transl. Med. 2021, 9, 729. [Google Scholar] [CrossRef]
- Ziolkowska, S.; Binienda, A.; Jabłkowski, M.; Szemraj, J.; Czarny, P. The Interplay between Insulin Resistance, Inflammation, Oxidative Stress, Base Excision Repair and Metabolic Syndrome in Nonalcoholic Fatty Liver Disease. Int. J. Mol. Sci. 2021, 22, 11128. [Google Scholar] [CrossRef]
- Beretta-Piccoli, B.T.; Mieli-Vergani, G.; Vergani, D. Autoimmune hepatitis. In The Rose and Mackay Textbook of Autoimmune Diseases; Academic Press: Cambridge, MA, USA, 2024; pp. 869–904. [Google Scholar]
- Czaja, A.J. Examining pathogenic concepts of autoimmune hepatitis for cues to future investigations and interventions. World J. Gastroenterol. 2019, 25, 6579–6606. [Google Scholar] [CrossRef]
- Wu, K.J.; Qian, Q.F.; Zhou, J.R.; Sun, D.L.; Duan, Y.F.; Zhu, X.; Sartorius, K.; Lu, Y.J. Regulatory T cells (Tregs) in liver fibrosis. Cell Death Discov. 2023, 9, 53. [Google Scholar] [CrossRef]
- Li, Y.N.; Ma, H.; Zhou, L.; Zhang, J.; Guo, L.P.; Li, S.Q.; Qian, Y.Q.; Wang, B.M. Autoimmune Hepatitis-related Cirrhosis: Clinical Features and Effectiveness of Immunosuppressive Treatment in Chinese Patients. Chin. Med. J. 2016, 129, 2434–2440. [Google Scholar] [CrossRef]
- Jansen, P.L.; Ghallab, A.; Vartak, N.; Reif, R.; Schaap, F.G.; Hampe, J.; Hengstler, J.G. The ascending pathophysiology of cholestatic liver disease. Hepatology 2017, 65, 722–738. [Google Scholar] [CrossRef] [PubMed]
- Ozaslan, E.; Efe, C.; Gokbulut Ozaslan, N. The diagnosis of antimitochondrial antibody-negative primary biliary cholangitis. Clin. Res. Hepatol. Gastroenterol. 2016, 40, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Gulamhusein, A.F.; Eaton, J.E.; Tabibian, J.H.; Atkinson, E.J.; Juran, B.D.; Lazaridis, K.N. Duration of Inflammatory Bowel Disease Is Associated with Increased Risk of Cholangiocarcinoma in Patients with Primary Sclerosing Cholangitis and IBD. Am. J. Gastroenterol. 2016, 111, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Hollerer, I.; Bachmann, A.; Muckenthaler, M.U. Pathophysiological consequences and benefits of HFE mutations: 20 years of research. Haematologica 2017, 102, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Teschke, R.; Eickhoff, A. Wilson Disease: Copper-Mediated Cuproptosis, Iron-Related Ferroptosis, and Clinical Highlights, with Comprehensive and Critical Analysis Update. Int. J. Mol. Sci. 2024, 25, 4753. [Google Scholar] [CrossRef]
- Hosseini, M.J.; Shaki, F.; Ghazi-Khansari, M.; Pourahmad, J. Toxicity of copper on isolated liver mitochondria: Impairment at complexes I, II, and IV leads to increased ROS production. Cell Biochem. Biophys. 2014, 70, 367–381. [Google Scholar] [CrossRef]
- Karatas, E.; Bouchecareilh, M. Alpha 1-Antitrypsin Deficiency: A Disorder of Proteostasis-Mediated Protein Folding and Trafficking Pathways. Int. J. Mol. Sci. 2020, 21, 1493. [Google Scholar] [CrossRef]
- Seitz, H.K.; Bataller, R.; Cortez-Pinto, H.; Gao, B.; Gual, A.; Lackner, C.; Mathurin, P.; Mueller, S.; Szabo, G.; Tsukamoto, H. Alcoholic liver disease. Nat. Rev. Dis. Primers 2018, 4, 16. [Google Scholar] [CrossRef]
- Romanelli, R.G.; Stasi, C. Recent Advancements in Diagnosis and Therapy of Liver Cirrhosis. Curr. Drug Targets 2016, 17, 1804–1817. [Google Scholar] [CrossRef]
- Lurie, Y.; Webb, M.; Cytter-Kuint, R.; Shteingart, S.; Lederkremer, G.Z. Non-invasive diagnosis of liver fibrosis and cirrhosis. World J. Gastroenterol. 2015, 21, 11567–11583. [Google Scholar] [CrossRef]
- Heyens, L.J.M.; Busschots, D.; Koek, G.H.; Robaeys, G.; Francque, S. Liver Fibrosis in Non-alcoholic Fatty Liver Disease: From Liver Biopsy to Non-invasive Biomarkers in Diagnosis and Treatment. Front. Med. 2021, 8, 615978. [Google Scholar] [CrossRef] [PubMed]
- Neuberger, J.; Cain, O. The Need for Alternatives to Liver Biopsies: Non-Invasive Analytics and Diagnostics. Hepat. Med. 2021, 13, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Maheshwari, S.; Gu, C.N.; Caserta, M.P.; Kezer, C.A.; Shah, V.H.; Torbenson, M.S.; Menias, C.O.; Fidler, J.L.; Venkatesh, S.K. Imaging of Alcohol-Associated Liver Disease. AJR Am. J. Roentgenol. 2024, 222, e2329917. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.H.; Chu, C.Y.; Chen, H.L.; Lin, I.T.; Wu, C.H.; Lee, Y.K.; Hu, P.J.; Bair, M.J. Subgroup analysis of the predictive ability of aspartate aminotransferase to platelet ratio index (APRI) and fibrosis-4 (FIB-4) for assessing hepatic fibrosis among patients with chronic hepatitis C. J. Microbiol. Immunol. Infect. 2020, 53, 542–549. [Google Scholar] [CrossRef]
- Huang, D.; Lin, T.; Wang, S.; Cheng, L.; Xie, L.; Lu, Y.; Chen, M.; Zhu, L.; Shi, J. The liver fibrosis index is superior to the APRI and FIB-4 for predicting liver fibrosis in chronic hepatitis B patients in China. BMC Infect. Dis. 2019, 19, 878. [Google Scholar] [CrossRef]
- Wazir, H.; Abid, M.; Essani, B.; Saeed, H.; Ahmad Khan, M.; Nasrullah, F.; Qadeer, U.; Khalid, A.; Varrassi, G.; Muzammil, M.A.; et al. Diagnosis and Treatment of Liver Disease: Current Trends and Future Directions. Cureus 2023, 15, e49920. [Google Scholar] [CrossRef]
- Battaglia, V.; Cervelli, R. Liver investigations: Updating on US technique and contrast-enhanced ultrasound (CEUS). Eur. J. Radiol. 2017, 96, 65–73. [Google Scholar] [CrossRef]
- Oliveira, A.G.; Fiorotto, R. Novel approaches to liver disease diagnosis and modeling. Transl. Gastroenterol. Hepatol. 2021, 6, 19. [Google Scholar] [CrossRef]
- Rauff, B.; Alzahrani, B.; Chudhary, S.A.; Nasir, B.; Mahmood, S.; Bhinder, M.A.; Faheem, M.; Amar, A. PNPLA3 and TM6SF2 genetic variants and hepatic fibrosis and cirrhosis in Pakistani chronic hepatitis C patients: A genetic association study. BMC Gastroenterol. 2022, 22, 401. [Google Scholar] [CrossRef]
- Ferro, A.; Saccu, G.; Mattivi, S.; Gaido, A.; Herrera Sanchez, M.B.; Haque, S.; Silengo, L.; Altruda, F.; Durazzo, M.; Fagoonee, S. Extracellular Vesicles as Delivery Vehicles for Non-Coding RNAs: Potential Biomarkers for Chronic Liver Diseases. Biomolecules 2024, 14, 277. [Google Scholar] [CrossRef]
- Drag, M.H.; Kilpeläinen, T.O. Cell-free DNA and RNA-measurement and applications in clinical diagnostics with focus on metabolic disorders. Physiol. Genomics 2021, 53, 33–46. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Hu, Q.; Ying, Y.; Lu, C.; Li, W.; Huang, C.; Xu, W.; Li, Q.; Qi, X.; Zhang, X.; et al. Using Next-generation Sequencing to Identify Novel Exosomal miRNAs as Biomarkers for Significant Hepatic Fibrosis. Discov. Med. 2021, 31, 147–159. [Google Scholar] [PubMed]
- Rashid, S.; Sun, Y.; Ali Khan Saddozai, U.; Hayyat, S.; Munir, M.U.; Akbar, M.U.; Khawar, M.B.; Ren, Z.; Ji, X.; Ihsan Ullah Khan, M. Circulating tumor DNA and its role in detection, prognosis and therapeutics of hepatocellular carcinoma. Chin. J. Cancer Res. 2024, 36, 195–214. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, M.; Trépo, E.; Degré, D.; Gustot, T.; Verset, L.; Demetter, P.; Devière, J.; Adler, M.; Moreno, C. Transient elastography using Fibroscan is the most reliable noninvasive method for the diagnosis of advanced fibrosis and cirrhosis in alcoholic liver disease. Eur. J. Gastroenterol. Hepatol. 2015, 27, 1074–1079. [Google Scholar] [CrossRef] [PubMed]
- Srinivasa Babu, A.; Wells, M.L.; Teytelboym, O.M.; Mackey, J.E.; Miller, F.H.; Yeh, B.M.; Ehman, R.L.; Venkatesh, S.K. Elastography in Chronic Liver Disease: Modalities, Techniques, Limitations, and Future Directions. Radiographics 2016, 36, 1987–2006. [Google Scholar] [CrossRef]
- Anstee, Q.M.; Castera, L.; Loomba, R. Impact of non-invasive biomarkers on hepatology practice: Past, present and future. J. Hepatol. 2022, 76, 1362–1378. [Google Scholar] [CrossRef]
- Chartampilas, E.; Rafailidis, V.; Georgopoulou, V.; Kalarakis, G.; Hatzidakis, A.; Prassopoulos, P. Current Imaging Diagnosis of Hepatocellular Carcinoma. Cancers 2022, 14, 3997. [Google Scholar] [CrossRef]
- Freitas, P.S.; Janicas, C.; Veiga, J.; Matos, A.P.; Herédia, V.; Ramalho, M. Imaging evaluation of the liver in oncology patients: A comparison of techniques. World J. Hepatol. 2021, 13, 1936–1955. [Google Scholar] [CrossRef]
- Yeom, S.K.; Lee, C.H.; Cha, S.H.; Park, C.M. Prediction of liver cirrhosis, using diagnostic imaging tools. World J. Hepatol. 2015, 7, 2069–2079. [Google Scholar] [CrossRef]
- Peruhova, M.; Banova-Chakarova, S.; Miteva, D.G.; Velikova, T. Genetic screening of liver cancer: State of the art. World J. Hepatol. 2024, 16, 716–730. [Google Scholar] [CrossRef]
- Thakral, S.; Ghoshal, K. miR-122 is a unique molecule with great potential in diagnosis, prognosis of liver disease, and therapy both as miRNA mimic and antimir. Curr. Gene Ther. 2015, 15, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Martinou, E.; Pericleous, M.; Stefanova, I.; Kaur, V.; Angelidi, A.M. Diagnostic Modalities of Non-Alcoholic Fatty Liver Disease: From Biochemical Biomarkers to Multi-Omics Non-Invasive Approaches. Diagnostics 2022, 12, 407. [Google Scholar] [CrossRef] [PubMed]
- Heimbach, J.K.; Kulik, L.M.; Finn, R.S.; Sirlin, C.B.; Abecassis, M.M.; Roberts, L.R.; Zhu, A.X.; Murad, M.H.; Marrero, J.A. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 2018, 67, 358–380. [Google Scholar] [CrossRef]
- Weiskirchen, R. Hepatoprotective and Anti-fibrotic Agents: It’s Time to Take the Next Step. Front. Pharmacol. 2016, 6, 303. [Google Scholar] [CrossRef] [PubMed]
- Tan, Z.; Sun, H.; Xue, T.; Gan, C.; Liu, H.; Xie, Y.; Yao, Y.; Ye, T. Liver Fibrosis: Therapeutic Targets and Advances in Drug Therapy. Front. Cell Dev. Biol. 2021, 9, 730176. [Google Scholar] [CrossRef]
- Shan, L.; Wang, F.; Zhai, D.; Meng, X.; Liu, J.; Lv, X. New Drugs for Hepatic Fibrosis. Front. Pharmacol. 2022, 13, 874408. [Google Scholar] [CrossRef]
- Puente, A.; Fortea, J.I.; Cabezas, J.; Arias Loste, M.T.; Iruzubieta, P.; Llerena, S.; Huelin, P.; Fábrega, E.; Crespo, J. LOXL2—A New Target in Antifibrogenic Therapy? Int. J. Mol. Sci. 2019, 20, 1634. [Google Scholar] [CrossRef]
- Huang, D.Q.; Terrault, N.A.; Tacke, F.; Gluud, L.L.; Arrese, M.; Bugianesi, E.; Loomba, R. Global epidemiology of cirrhosis—Aetiology, trends and predictions. Nat. Rev. Gastroenterol. Hepatol. 2023, 20, 388–398. [Google Scholar] [CrossRef]
- Usuda, D.; Kaneoka, Y.; Ono, R.; Kato, M.; Sugawara, Y.; Shimizu, R.; Inami, T.; Nakajima, E.; Tsuge, S.; Sakurai, R.; et al. Current perspectives of viral hepatitis. World J. Gastroenterol. 2024, 30, 2402–2417. [Google Scholar] [CrossRef]
- Konings, L.A.M.; Miguelañez-Matute, L.; Boeren, A.M.P.; van de Luitgaarden, I.A.T.; Dirksmeier, F.; de Knegt, R.J.; Tushuizen, M.E.; Grobbee, D.E.; Holleboom, A.G.; Cabezas, M.C. Pharmacological treatment options for metabolic dysfunction-associated steatotic liver disease in patients with type 2 diabetes mellitus: A systematic review. Eur. J. Clin. Investig. 2025, 55, e70003. [Google Scholar] [CrossRef]
- Lesmana, C.R.A.; Raharjo, M.; Gani, R.A. Managing liver cirrhotic complications: Overview of esophageal and gastric varices. Clin. Mol. Hepatol. 2020, 26, 444–460. [Google Scholar] [CrossRef] [PubMed]
- Fazal, M.O.; Akram, H.; Chughtai, A.Z.; Yaqoob, M.Y.; Musharaf, M.U. Comparison of betablockers and endoscopic variceal band ligation (EVBL) for secondary prevention of variceal bleed in cirrhotics. Prof. Med. J. 2022, 29, 1499–1505. [Google Scholar]
- Putra, I.G.; Hakim, A.R.; Soebroto, H.; Sembiring, Y.E.; Limanto, D.H.; Rizki, M. Clinical outcomes of splenorenal shunts in esophageal varices patients: A literature review. J. Indones. Vasc. Access 2024, 4, 1–4. [Google Scholar] [CrossRef]
- Sousa Da Silva, R.X.; Weber, A.; Dutkowski, P.; Clavien, P.A. Machine perfusion in liver transplantation. Hepatology 2022, 76, 1531–1549. [Google Scholar] [CrossRef] [PubMed]
- Hackl, C.; Schmidt, K.M.; Süsal, C.; Döhler, B.; Zidek, M.; Schlitt, H.J. Split liver transplantation: Current developments. World J. Gastroenterol. 2018, 24, 5312–5321. [Google Scholar] [CrossRef]
- Brown RSJr Fisher, R.A.; Subramanian, R.M.; Griesemer, A.; Fernandes, M.; Thatcher, W.H.; Stiede, K.; Curtis, M. Artificial Liver Support Systems in Acute Liver Failure and Acute-on-Chronic Liver Failure: Systematic Review and Meta-Analysis. Crit. Care Explor. 2025, 7, e1199. [Google Scholar] [CrossRef]
- Legallais, C.; Kim, D.; Mihaila, S.M.; Mihajlovic, M.; Figliuzzi, M.; Bonandrini, B.; Salerno, S.; Yousef Yengej, F.A.; Rookmaaker, M.B.; Sanchez Romero, N.; et al. Bioengineering Organs for Blood Detoxification. Adv. Healthc. Mater. 2018, 7, e1800430. [Google Scholar] [CrossRef]
- Wang, W.L.; Lian, H.; Liang, Y.; Ye, Y.; Tam, P.K.H.; Chen, Y. Molecular Mechanisms of Fibrosis in Cholestatic Liver Diseases and Regenerative Medicine-Based Therapies. Cells 2024, 13, 1997. [Google Scholar] [CrossRef]
- Nazarie Ignat, S.R.; Gharbia, S.; Hermenean, A.; Dinescu, S.; Costache, M. Regenerative Potential of Mesenchymal Stem Cells’ (MSCs) Secretome for Liver Fibrosis Therapies. Int. J. Mol. Sci. 2021, 22, 13292. [Google Scholar] [CrossRef]
- Shi, M.; Li, Y.Y.; Xu, R.N.; Meng, F.P.; Yu, S.J.; Fu, J.L.; Hu, J.H.; Li, J.X.; Wang, L.F.; Jin, L.; et al. Mesenchymal stem cell therapy in decompensated liver cirrhosis: A long-term follow-up analysis of the randomized controlled clinical trial. Hepatol. Int. 2021, 15, 1431–1441. [Google Scholar] [CrossRef]
- Shi, W.; Zhang, Z.; Wang, X. The Prospect of Hepatic Decellularized Extracellular Matrix as a Bioink for Liver 3D Bioprinting. Biomolecules 2024, 14, 1019. [Google Scholar] [CrossRef]
- Böttcher, K.; Pinzani, M. Pathophysiology of liver fibrosis and the methodological barriers to the development of anti-fibrogenic agents. Adv. Drug Deliv. Rev. 2017, 121, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Aryan, M.; Qian, S.; Cabrera, R.; Liu, X. A Focused Review on Recent Advances in the Diagnosis and Treatment of Viral Hepatitis. Gastroenterol. Res. 2021, 14, 139–156. [Google Scholar] [CrossRef]
- Beyaz Coşkun, A.; Sağdiçoğlu Celep, A.G. Therapeutic modulation methods of gut microbiota and gut-liver axis. Crit. Rev. Food Sci. Nutr. 2022, 62, 6505–6515. [Google Scholar] [CrossRef]
- Hwang, J.H.; Shergill, A.K.; Acosta, R.D.; Chandrasekhara, V.; Chathadi, K.V.; Decker, G.A.; Early, D.S.; Evans, J.A.; Fanelli, R.D.; Fisher, D.A.; et al. The role of endoscopy in the management of variceal hemorrhage. Gastrointest. Endosc. 2014, 80, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Onofrio, F.Q.; Pereira-Lima, J.C.; Valença, F.M.; Azeredo-da-Silva, A.L.F.; Tetelbom Stein, A. Efficacy of endoscopic treatments for acute esophageal variceal bleeding in cirrhotic patients: Systematic review and meta-analysis. Endosc. Int. Open 2019, 7, E1503–E1514. [Google Scholar] [CrossRef]
- Khalil, A.; Quaglia, A.; Gélat, P.; Saffari, N.; Rashidi, H.; Davidson, B. New Developments and Challenges in Liver Transplantation. J. Clin. Med. 2023, 12, 5586. [Google Scholar] [CrossRef]
- He, Y.T.; Qi, Y.N.; Zhang, B.Q.; Li, J.B.; Bao, J. Bioartificial liver support systems for acute liver failure: A systematic review and meta-analysis of the clinical and preclinical literature. World J. Gastroenterol. 2019, 25, 3634–3648. [Google Scholar] [CrossRef] [PubMed]
- He, C.; Yang, Y.; Zheng, K.; Chen, Y.; Liu, S.; Li, Y.; Han, Q.; Zhao, R.C.; Wang, L.; Zhang, F. Mesenchymal stem cell-based treatment in autoimmune liver diseases: Underlying roles, advantages and challenges. Ther. Adv. Chronic Dis. 2021, 12, 2040622321993442. [Google Scholar] [CrossRef]
- Ali, S.; Haque, N.; Azhar, Z.; Saeinasab, M.; Sefat, F. Regenerative Medicine of Liver: Promises, Advances and Challenges. Biomimetics 2021, 6, 62. [Google Scholar] [CrossRef]
- Zabaleta, N.; Unzu, C.; Weber, N.D.; Gonzalez-Aseguinolaza, G. Gene therapy for liver diseases—Progress and challenges. Nat. Rev. Gastroenterol. Hepatol. 2023, 20, 288–305. [Google Scholar] [CrossRef] [PubMed]
- Nishida, N. Advancements in Artificial Intelligence-Enhanced Imaging Diagnostics for the Management of Liver Disease-Applications and Challenges in Personalized Care. Bioengineering 2024, 11, 1243. [Google Scholar] [CrossRef]
- Gonzalez-Rodriguez, A.; MValverde, A. RNA interference as a therapeutic strategy for the treatment of liver diseases. Curr. Pharm. Des. 2015, 21, 4574–4586. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Li, Y.; Liang, Q.; Liu, J.; Liu, Y. Combination therapy based on targeted nano drug co-delivery systems for liver fibrosis treatment: A review. J. Drug Target. 2022, 30, 577–588. [Google Scholar] [CrossRef] [PubMed]
- Premkumar, M.; Anand, A.C. Overview of Complications in Cirrhosis. J. Clin. Exp. Hepatol. 2022, 12, 1150–1174. [Google Scholar] [CrossRef]
- Vilstrup, H.; Amodio, P.; Bajaj, J.; Cordoba, J.; Ferenci, P.; Mullen, K.D.; Weissenborn, K.; Wong, P. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology 2014, 60, 715–735. [Google Scholar] [CrossRef]
- Celsa, C.; Veneziano, M.; Di Giorgio, F.M.; Cannova, S.; Lombardo, A.; Errigo, E.; Landro, G.; Simone, F.; Sinagra, E.; Calvaruso, V. Non-Invasive Diagnostic Tests for Portal Hypertension in Patients with HBV- and HCV-Related Cirrhosis: A Comprehensive Review. Medicina 2024, 60, 690. [Google Scholar] [CrossRef]
- Baliss, M.; Patel, D.; Madi, M.Y.; Bazarbashi, A.N. EUS-Guided Vascular Interventions. J. Clin. Med. 2023, 12, 2165. [Google Scholar] [CrossRef]
- Pereira, K.; Carrion, A.F.; Salsamendi, J.; Doshi, M.; Baker, R.; Kably, I. Endovascular Management of Refractory Hepatic Encephalopathy Complication of Transjugular Intrahepatic Portosystemic Shunt (TIPS): Comprehensive Review and Clinical Practice Algorithm. Cardiovasc. Interv. Radiol. 2016, 39, 170–182. [Google Scholar] [CrossRef]
- Edelson, J.; Basso, J.E.; Rockey, D.C. Updated strategies in the management of acute variceal haemorrhage. Curr. Opin. Gastroenterol. 2021, 37, 167–172. [Google Scholar] [CrossRef]
- Bajaj, R.; Huang, X.; Kilic, Y.; Ramasamy, A.; Jain, A.; Ozkor, M.; Tufaro, V.; Safi, H.; Erdogan, E.; Serruys, P.W.; et al. Advanced deep learning methodology for accurate, real-time segmentation of high-resolution intravascular ultrasound images. Int. J. Cardiol. 2021, 339, 185–191. [Google Scholar] [CrossRef] [PubMed]
- Aithal, G.P.; Palaniyappan, N.; China, L.; Härmälä, S.; Macken, L.; Ryan, J.M.; Wilkes, E.A.; Moore, K.; Leithead, J.A.; Hayes, P.C.; et al. Guidelines on the management of ascites in cirrhosis. Gut 2021, 70, 9–29. [Google Scholar] [CrossRef] [PubMed]
- Lenz, K.; Buder, R.; Kapun, L.; Voglmayr, M. Treatment and management of ascites and hepatorenal syndrome: An update. Ther. Adv. Gastroenterol. 2015, 8, 83–100. [Google Scholar] [CrossRef]
- Szczepanska-Sadowska, E.; Zera, T.; Sosnowski, P.; Cudnoch-Jedrzejewska, A.; Puszko, A.; Misicka, A. Vasopressin and Related Peptides; Potential Value in Diagnosis, Prognosis and Treatment of Clinical Disorders. Curr. Drug Metab. 2017, 18, 306–345. [Google Scholar] [CrossRef]
- Fukui, H.; Kawaratani, H.; Kaji, K.; Takaya, H.; Yoshiji, H. Management of refractory cirrhotic ascites: Challenges and solutions. Hepat. Med. 2018, 10, 55–71. [Google Scholar] [CrossRef]
- Jayakumar, A.R.; Norenberg, M.D. Hyperammonemia in Hepatic Encephalopathy. J. Clin. Exp. Hepatol. 2018, 8, 272–280. [Google Scholar] [CrossRef] [PubMed]
- Sanchez-Delgado, J.; Miquel, M. Papel de la rifaximina en el tratamiento de la encefalopatía hepática [Role of rifaximin in the treatment of hepatic encephalopathy]. Gastroenterol. Hepatol. 2016, 39, 282–292. [Google Scholar] [CrossRef]
- Won, S.M.; Oh, K.K.; Gupta, H.; Ganesan, R.; Sharma, S.P.; Jeong, J.J.; Yoon, S.J.; Jeong, M.K.; Min, B.H.; Hyun, J.Y.; et al. The Link between Gut Microbiota and Hepatic Encephalopathy. Int. J. Mol. Sci. 2022, 23, 8999. [Google Scholar] [CrossRef]
- Gambello, M.J.; Li, H. Current strategies for the treatment of inborn errors of metabolism. J. Genet. Genomics 2018, 45, 61–70. [Google Scholar] [CrossRef]
- Ginès, P.; Solà, E.; Angeli, P.; Wong, F.; Nadim, M.K.; Kamath, P.S. Hepatorenal syndrome. Nat. Rev. Dis. Primers 2018, 4, 23. [Google Scholar] [CrossRef]
- Belcher, J.M.; Parada, X.V.; Simonetto, D.A.; Juncos, L.A.; Karakala, N.; Wadei, H.M.; Sharma, P.; Regner, K.R.; Nadim, M.K.; Garcia-Tsao, G.; et al. Terlipressin and the Treatment of Hepatorenal Syndrome: How the CONFIRM Trial Moves the Story Forward. Am. J. Kidney Dis. 2022, 79, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Kitchlu, A.; Adhikari, N.; Burns, K.E.; Friedrich, J.O.; Garg, A.X.; Klein, D.; Richardson, R.M.; Wald, R. Outcomes of sustained low efficiency dialysis versus continuous renal replacement therapy in critically ill adults with acute kidney injury: A cohort study. BMC Nephrol. 2015, 16, 127. [Google Scholar] [CrossRef] [PubMed]
- McPhail, M.J.; Shawcross, D.L.; Abeles, R.D.; Chang, A.; Patel, V.; Lee, G.H.; Abdulla, M.; Sizer, E.; Willars, C.; Auzinger, G.; et al. Increased Survival for Patients with Cirrhosis and Organ Failure in Liver Intensive Care and Validation of the Chronic Liver Failure-Sequential Organ Failure Scoring System. Clin. Gastroenterol. Hepatol. 2015, 13, 1353–1360.e8. [Google Scholar] [CrossRef] [PubMed]
- Wong, V.W.; Adams, L.A.; de Lédinghen, V.; Wong, G.L.; Sookoian, S. Noninvasive biomarkers in NAFLD and NASH—Current progress and future promise. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 461–478. [Google Scholar] [CrossRef]
- Singal, A.K.; Kamath, P.S. Model for End-stage Liver Disease. J. Clin. Exp. Hepatol. 2013, 3, 50–60. [Google Scholar] [CrossRef] [PubMed]
- El-Khateeb, E.; Darwich, A.S.; Achour, B.; Athwal, V.; Rostami-Hodjegan, A. Review article: Time to revisit Child-Pugh score as the basis for predicting drug clearance in hepatic impairment. Aliment. Pharmacol. Ther. 2021, 54, 388–401. [Google Scholar] [CrossRef]
- Liu, Y.; Ran, L.; Zhang, H.; Ren, H.; Jiang, X.; Liao, P.; Ou, M. Comparison of Child-Pugh, MELD, MELD-Na, and ALBI Scores in Predicting In-Hospital Mortality in Patients with HCC. Int. J. Clin. Med. 2023, 14, 148–162. [Google Scholar] [CrossRef]
- Mai, R.Y.; Lu, T.L.; Lu, R.J.; Zeng, C.; Lian, F.; Li, L.Q.; Wu, G.B.; Ye, J.Z. C-Reactive Protein-Albumin Ratio (CAR): A More Promising Inflammation-Based Prognostic Marker for Patients Undergoing Curative Hepatectomy for Hepatocellular Carcinoma. J. Inflamm. Res. 2024, 17, 919–931. [Google Scholar] [CrossRef]
- Azam, A.; Klisic, A.; Mercantepe, F.; Faseeh, H.; Mercantepe, T.; Rafaqat, S. Role of Coagulation Factors in Hepatocellular Carcinoma: A Literature Review. Life 2024, 15, 34. [Google Scholar] [CrossRef]
- Kubota, N.; Fujiwara, N.; Hoshida, Y. Clinical and Molecular Prediction of Hepatocellular Carcinoma Risk. J. Clin. Med. 2020, 9, 3843. [Google Scholar] [CrossRef]
- Jampoka, K.; Muangpaisarn, P.; Khongnomnan, K.; Treeprasertsuk, S.; Tangkijvanich, P.; Payungporn, S. Serum miR-29a and miR-122 as Potential Biomarkers for Non-Alcoholic Fatty Liver Disease (NAFLD). Microrna 2018, 7, 215–222. [Google Scholar] [CrossRef]
- Jaurigue, M.M.; Cappell, M.S. Therapy for alcoholic liver disease. World J. Gastroenterol. 2014, 20, 2143–2158. [Google Scholar] [CrossRef] [PubMed]
- Ho, D.; Quake, S.R.; McCabe, E.R.B.; Chng, W.J.; Chow, E.K.; Ding, X.; Gelb, B.D.; Ginsburg, G.S.; Hassenstab, J.; Ho, C.M.; et al. Enabling Technologies for Personalized and Precision Medicine. Trends Biotechnol. 2020, 38, 497–518. [Google Scholar] [CrossRef]
- Ahn, J.C.; Connell, A.; Simonetto, D.A.; Hughes, C.; Shah, V.H. Application of Artificial Intelligence for the Diagnosis and Treatment of Liver Diseases. Hepatology 2021, 73, 2546–2563. [Google Scholar] [CrossRef]
- Oyeniyi, J.; Oluwaseyi, P. Emerging trends in AI-powered medical imaging: Enhancing diagnostic accuracy and treatment decisions. Int. J. Enhanc. Res. Sci. Technol. Eng. 2024, 13, 2319–7463. [Google Scholar]
- Dana, J.; Venkatasamy, A.; Saviano, A.; Lupberger, J.; Hoshida, Y.; Vilgrain, V.; Nahon, P.; Reinhold, C.; Gallix, B.; Baumert, T.F. Conventional and artificial intelligence-based imaging for biomarker discovery in chronic liver disease. Hepatol. Int. 2022, 16, 509–522. [Google Scholar] [CrossRef] [PubMed]
- Schneider, C.V.; Li, T.; Zhang, D.; Mezina, A.I.; Rattan, P.; Huang, H.; Creasy, K.T.; Scorletti, E.; Zandvakili, I.; Vujkovic, M.; et al. Large-scale identification of undiagnosed hepatic steatosis using natural language processing. EClinicalMedicine 2023, 62, 102149. [Google Scholar] [CrossRef]
- Lin, B.; Ma, Y.; Wu, S. Multi-Omics and Artificial Intelligence-Guided Data Integration in Chronic Liver Disease: Prospects and Challenges for Precision Medicine. OMICS 2022, 26, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.; Wallace, D.F.; Powell, E.E.; Rahman, T.; Clark, P.J.; Subramaniam, V.N. Gene Variants Implicated in Steatotic Liver Disease: Opportunities for Diagnostics and Therapeutics. Biomedicines 2023, 11, 2809. [Google Scholar] [CrossRef]
- Hu, Y.; Peng, L.; Zhuo, X.; Yang, C.; Zhang, Y. Hedgehog Signaling Pathway in Fibrosis and Targeted Therapies. Biomolecules 2024, 14, 1485. [Google Scholar] [CrossRef]
- De Mattia, E.; Cecchin, E.; Guardascione, M.; Foltran, L.; Di Raimo, T.; Angelini, F.; D’Andrea, M.; Toffoli, G. Pharmacogenetics of the systemic treatment in advanced hepatocellular carcinoma. World J. Gastroenterol. 2019, 25, 3870–3896. [Google Scholar] [CrossRef] [PubMed]
- Sotoudeheian, M. Galectin-3 and Severity of Liver Fibrosis in Metabolic Dysfunction-Associated Fatty Liver Disease. Protein Pept. Lett. 2024, 31, 290–304. [Google Scholar] [CrossRef] [PubMed]
- Schilter, H.; Findlay, A.D.; Perryman, L.; Yow, T.T.; Moses, J.; Zahoor, A.; Turner, C.I.; Deodhar, M.; Foot, J.S.; Zhou, W.; et al. The lysyl oxidase like 2/3 enzymatic inhibitor, PXS-5153A, reduces crosslinks and ameliorates fibrosis. J. Cell Mol. Med. 2019, 23, 1759–1770. [Google Scholar] [CrossRef] [PubMed]
- Ocker, M.; Mayr, C.; Kiesslich, T.; Stintzing, S.; Neureiter, D. Immunmodulatory Treatment Strategies of Hepatocellular Carcinoma: From Checkpoint Inhibitors Now to an Integrated Approach in the Future. Cancers 2021, 13, 1558. [Google Scholar] [CrossRef]
- Yao, L.; Hu, X.; Dai, K.; Yuan, M.; Liu, P.; Zhang, Q.; Jiang, Y. Mesenchymal stromal cells: Promising treatment for liver cirrhosis. Stem Cell Res. Ther. 2022, 13, 308. [Google Scholar] [CrossRef]
| Ref. | Category | Technique | Description | Advantages | Limitations |
|---|---|---|---|---|---|
| [55] | Non-Invasive Diagnostic Tools | FibroScan (Transient Elastography) | Measures liver stiffness non-invasively to assess fibrosis. | Quick, painless, portable, and widely used. | Limited accuracy in patients with obesity or significant ascites. |
| [56] | Shear Wave Elastography | Advanced ultrasound-based technology to measure liver stiffness. | High resolution and accuracy. | Operator dependency and higher cost. | |
| [57] | Serum Biomarkers (e.g., APRI, FIB-4) | Blood tests calculating scores based on liver enzymes and platelet counts. | Non-invasive, inexpensive, and widely available. | Limited specificity and sensitivity in early-stage cirrhosis. | |
| [58] | Imaging Techniques | Ultrasound | Common imaging for liver assessment and detection of nodular patterns. | Widely accessible and cost-effective. | Limited in detecting mild fibrosis. |
| [59] | Advanced MRI (e.g., MRE, DWI-MRI) | Magnetic resonance elastography (MRE) and diffusion-weighted imaging (DWI) for detailed fibrosis mapping. | Superior sensitivity and specificity for detecting fibrosis and inflammation. | High cost and limited availability. | |
| [60] | CT Imaging | Provides detailed liver architecture and identifies complications like varices. | Effective for detecting advanced cirrhosis and complications. | Involves radiation exposure; limited use in early-stage diagnosis. | |
| [61] | Molecular and Genomic Approaches | Genetic Markers | Identification of mutations and genetic predisposition for liver diseases. | Enables personalized risk assessment and targeted therapies. | Requires advanced laboratory facilities and high costs. |
| [62] | Molecular Diagnostics (e.g., miRNA) | Detection of specific biomarkers, such as microRNAs, linked to fibrosis and inflammation. | High accuracy in early-stage diagnosis and progression monitoring. | Requires specialized expertise and equipment. | |
| [63] | Multiomics Approaches | Integration of genomics, proteomics, and metabolomics for comprehensive liver disease profiling. | Holistic understanding of disease pathways and potential therapeutic targets. | Complexity, high cost, and limited widespread application. |
| Ref. | Category | Treatment Modality | Description | Advantages | Challenges/Concerns |
|---|---|---|---|---|---|
| [83] | Pharmacological Therapies | Antifibrotic Agents | Drugs targeting fibrogenesis pathways to reduce liver scarring (e.g., simtuzumab, losartan). | Slows or reverses fibrosis progression. | Limited effectiveness in late-stage illness, possible side effects, lack of licensed medications, continuing clinical trials, and regulatory ambiguity. |
| [84] | Targeted Therapies | Antivirals for hepatitis (e.g., tenofovir, entecavir), immunotherapies for autoimmune etiologies. | Treats underlying causes of liver disease. | Contraindications in certain comorbidities, unpleasant effects, high costs, little clinical evidence, ethical problems in long-term usage, and pending regulatory clearance. | |
| [85] | Gut Microbiota Modulation | Probiotics or fecal microbiota transplantation (FMT) to restore gut–liver axis health. | Improves inflammation and reduces endotoxemia. | Variable patient response, danger of infection, ethical problems with FMT, lack of standardization, and insufficient regulatory advice. | |
| [86] | Endoscopic Interventions | Variceal Banding | Bands placed on esophageal varices to prevent bleeding. | Minimally invasive and effective for variceal bleeding prevention. | Requires competent staff; danger of ulceration and rebleeding; may require several sessions; contraindicated in active infections or recalcitrant individuals. |
| [87] | Sclerotherapy | Injection of sclerosants into varices to control bleeding. | Immediate bleeding control. | High risk of complications (e.g., ulceration, perforation), contraindicated in severe coagulopathy, may induce recurrence, and less recommended than banding owing to side effects. | |
| [88] | Transplantation Advances | Innovations in Liver Transplantation | Use of marginal donors, split-liver transplantation, and robotic surgery. | Expands donor pool and improves surgical precision. | Living donation raises ethical difficulties because of its high cost, danger of rejection, long-term immunosuppressive effects, and restricted availability in resource-poor regions. |
| [89] | Artificial Liver Support Systems | Bioartificial livers and extracorporeal liver support systems (e.g., MARS). | Provides temporary support for acute liver failure. | High costs, limited availability, lack of long-term effectiveness, contraindications in multi-organ failure, and no permanent cure. | |
| [90] | Regenerative Medicine | Stem Cell Therapy | Use of mesenchymal stem cells to regenerate damaged liver tissue. | Potential to repair liver damage and delay transplantation. | Lack of large-scale clinical studies, regulatory limits, potential immunological responses, ethical problems, and uncertainty about long-term safety and efficacy. |
| [91] | Tissue Engineering | Creation of bioengineered liver tissue for transplantation. | Addresses organ shortage crisis. | Mostly preclinical, ethical and regulatory difficulties, high expenses, technological complexity, and lack of functional long-term results in people. | |
| [92] | Gene Therapy | Modifying genes to prevent or treat liver fibrosis and cirrhosis. | Potential for curative treatment of genetic liver diseases. | High cost, safety issues (e.g., immunological responses, off-target effects), ethical difficulties, little clinical evidence, and complicated regulatory approval. | |
| [93] | Emerging Approaches | AI-Guided Personalized Therapies | AI-driven algorithms to design individualized treatment plans. | Enhances treatment precision and efficiency. | Data privacy problems, reliance on high-quality data, possible bias in algorithms, legal barriers, and inadequate long-term clinical validation. |
| [94] | RNA-Based Therapies | Use of RNA interference (RNAi) to silence fibrotic genes (e.g., siRNA drugs). | Targets fibrosis at molecular level. | Limited clinical evidence, possible off-target effects, immunological responses, high costs, and regulatory issues. | |
| [95] | Nano-Drug Delivery Systems | Nanoparticles for targeted delivery of antifibrotic drugs. | Reduces off-target effects and enhances drug efficacy. | Limited clinical evidence, possible toxicity of nanoparticles, high cost, regulatory barriers, and scalability issues. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sah, A.K.; Afzal, M.; Elshaikh, R.H.; Abbas, A.M.; Shalabi, M.G.; Prabhakar, P.K.; Babker, A.M.A.; Khalimova, F.T.; Sabrievna, V.A.; Choudhary, R.K. Innovative Strategies in the Diagnosis and Treatment of Liver Cirrhosis and Associated Syndromes. Life 2025, 15, 779. https://doi.org/10.3390/life15050779
Sah AK, Afzal M, Elshaikh RH, Abbas AM, Shalabi MG, Prabhakar PK, Babker AMA, Khalimova FT, Sabrievna VA, Choudhary RK. Innovative Strategies in the Diagnosis and Treatment of Liver Cirrhosis and Associated Syndromes. Life. 2025; 15(5):779. https://doi.org/10.3390/life15050779
Chicago/Turabian StyleSah, Ashok Kumar, Mohd Afzal, Rabab H. Elshaikh, Anass M. Abbas, Manar G. Shalabi, Pranav Kumar Prabhakar, Asaad M. A. Babker, Fariza Tursunbaevna Khalimova, Velilyaeva Aliya Sabrievna, and Ranjay Kumar Choudhary. 2025. "Innovative Strategies in the Diagnosis and Treatment of Liver Cirrhosis and Associated Syndromes" Life 15, no. 5: 779. https://doi.org/10.3390/life15050779
APA StyleSah, A. K., Afzal, M., Elshaikh, R. H., Abbas, A. M., Shalabi, M. G., Prabhakar, P. K., Babker, A. M. A., Khalimova, F. T., Sabrievna, V. A., & Choudhary, R. K. (2025). Innovative Strategies in the Diagnosis and Treatment of Liver Cirrhosis and Associated Syndromes. Life, 15(5), 779. https://doi.org/10.3390/life15050779









