Interest of Lung Ultrasound in the Management of Acute Heart Failure in Post-Emergency Service
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Population
2.3. Heart Failure Treatment and Protocol
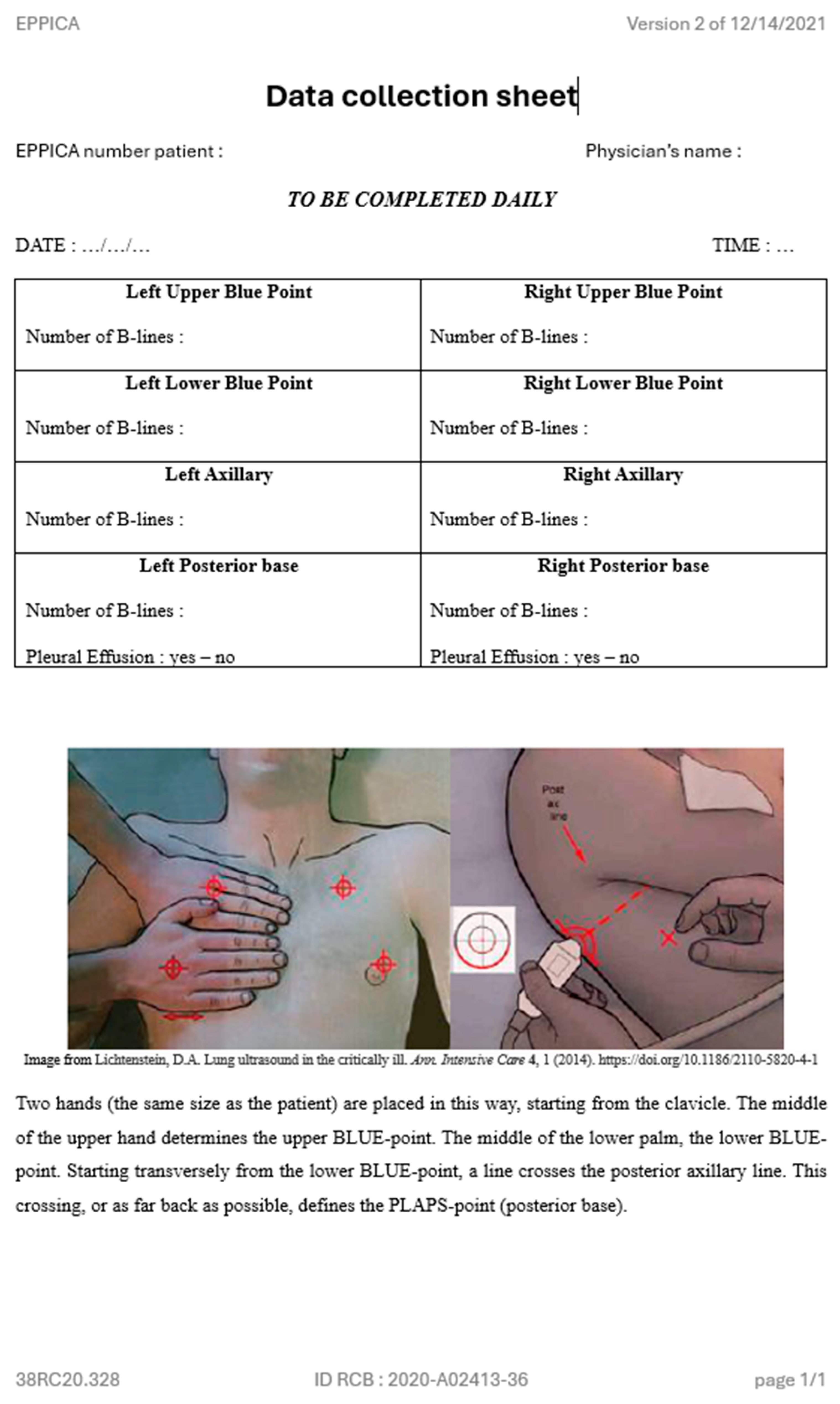
2.4. Lung Ultrasound Protocol
2.5. Follow-Up/Data Collection
2.6. Study Outcomes
2.7. Statistical Analysis
2.8. Ethical Aspects
3. Results
3.1. General Characteristics
3.2. Reproducibility and Feasibility
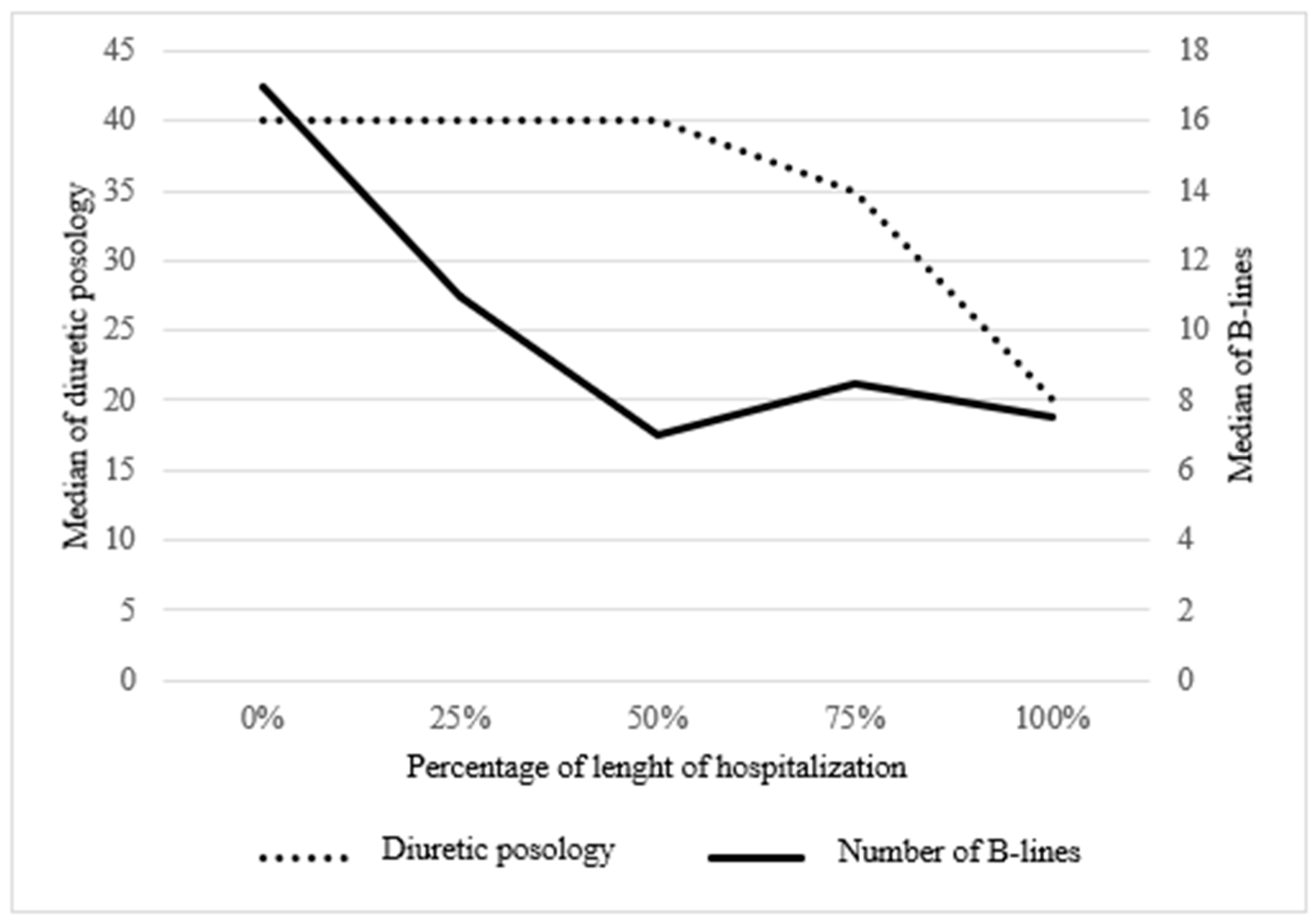
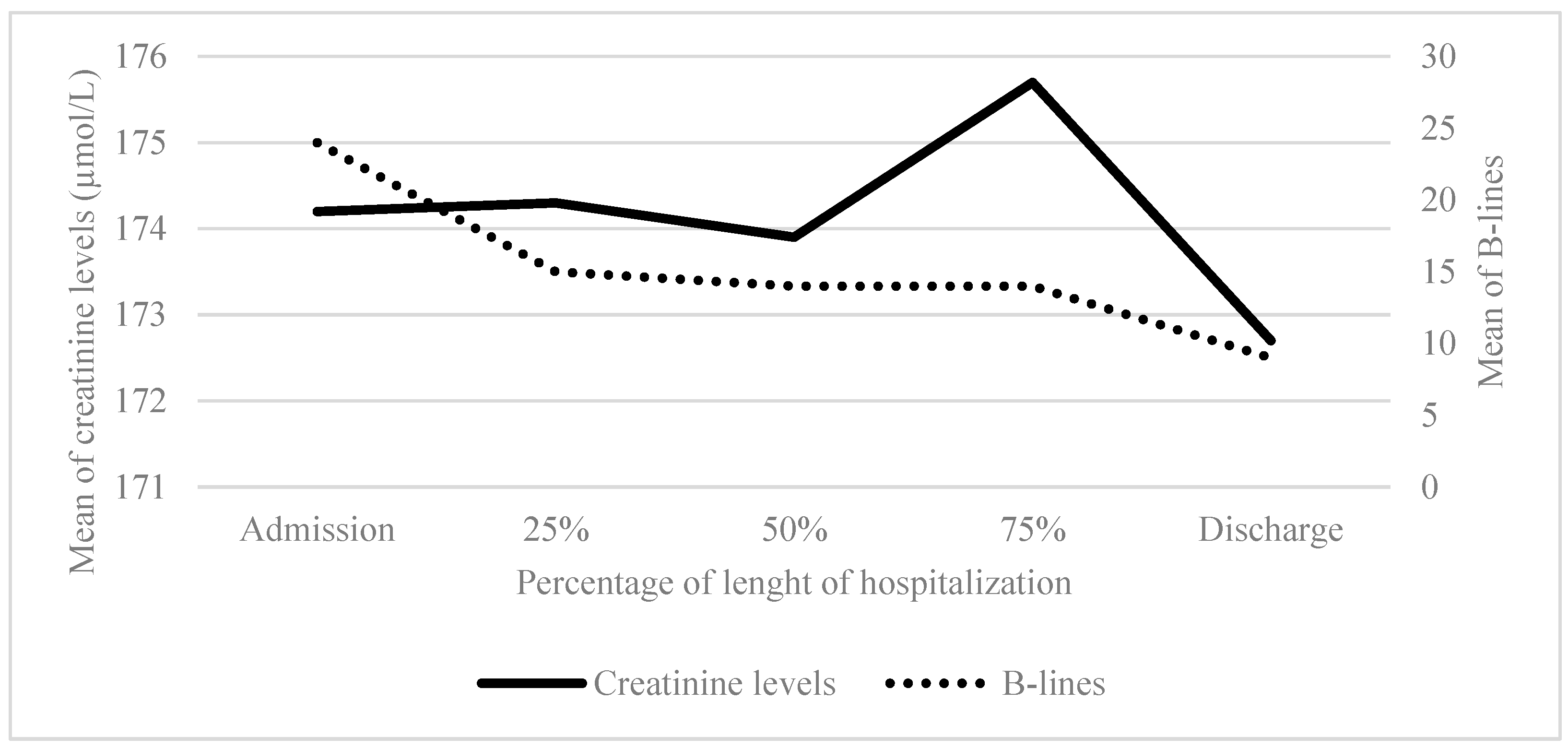
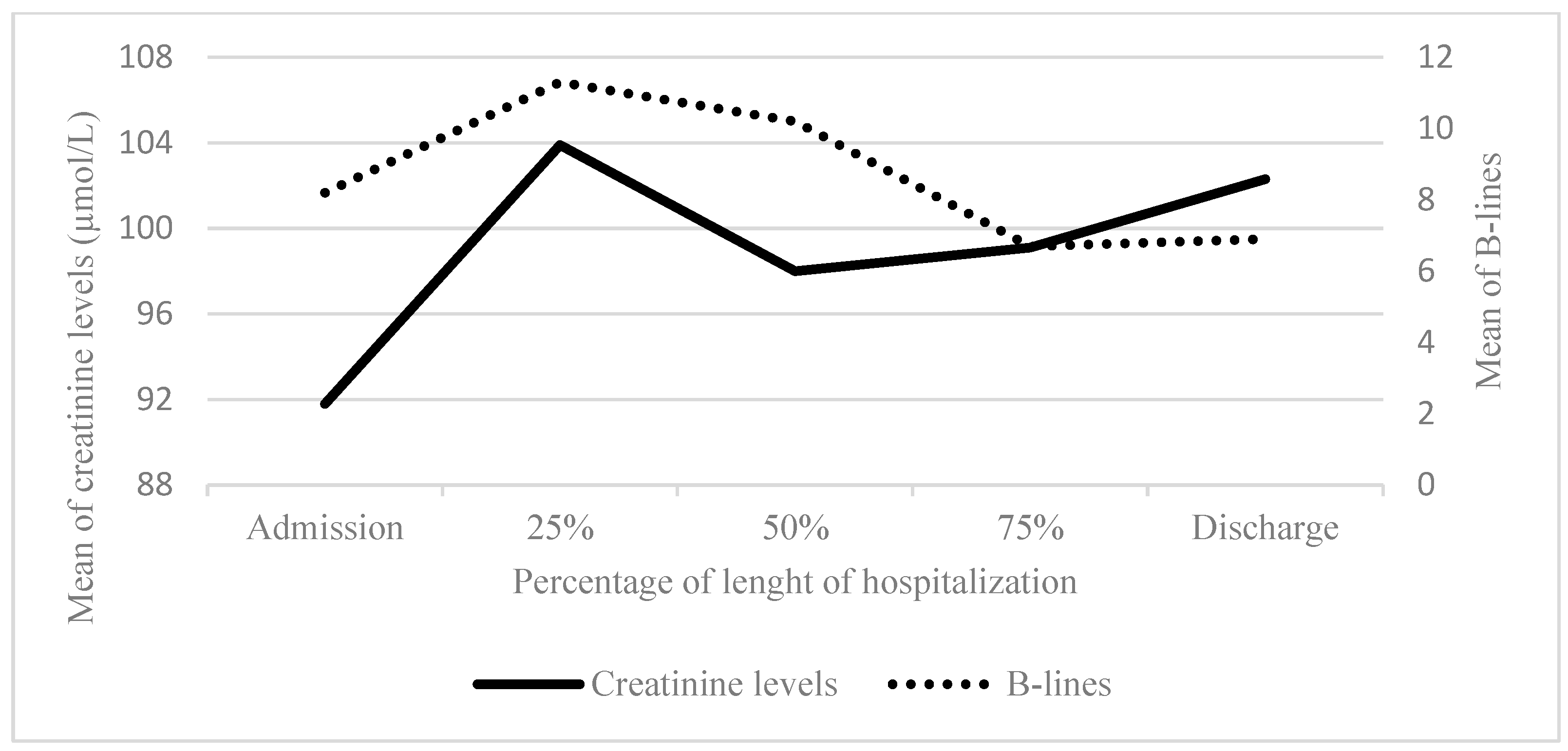
3.3. LUS B-Lines, Posology Diuretics, Clinical and Biological Parameters
4. Discussion
4.1. Strenghs
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AHF | Acute Heart Failure |
| AKI | Acute Kidney Injury |
| ARDS | Acute Respiratory Distress Syndrome |
| BNP | Brain Natriuretic Peptide |
| CCI | Charlson Comorbidity Index |
| CKD | Chronic Kidney Disease |
| ED | Emergency Department |
| EF | Ejection Fraction |
| GFR | Glomerular Filtration Rate |
| HFrEF | Heart Failure Reduced Ejection Fraction |
| HFpEF | Heart Failure Preserved Ejection Fraction |
| HR | Hazard Ratio |
| IV | Intra-venous |
| LEVF | Left ventricular ejection fraction |
| LUS | Lung ultrasound |
| NHYA | New York Heart Association |
| VM | Vesicular murmur |
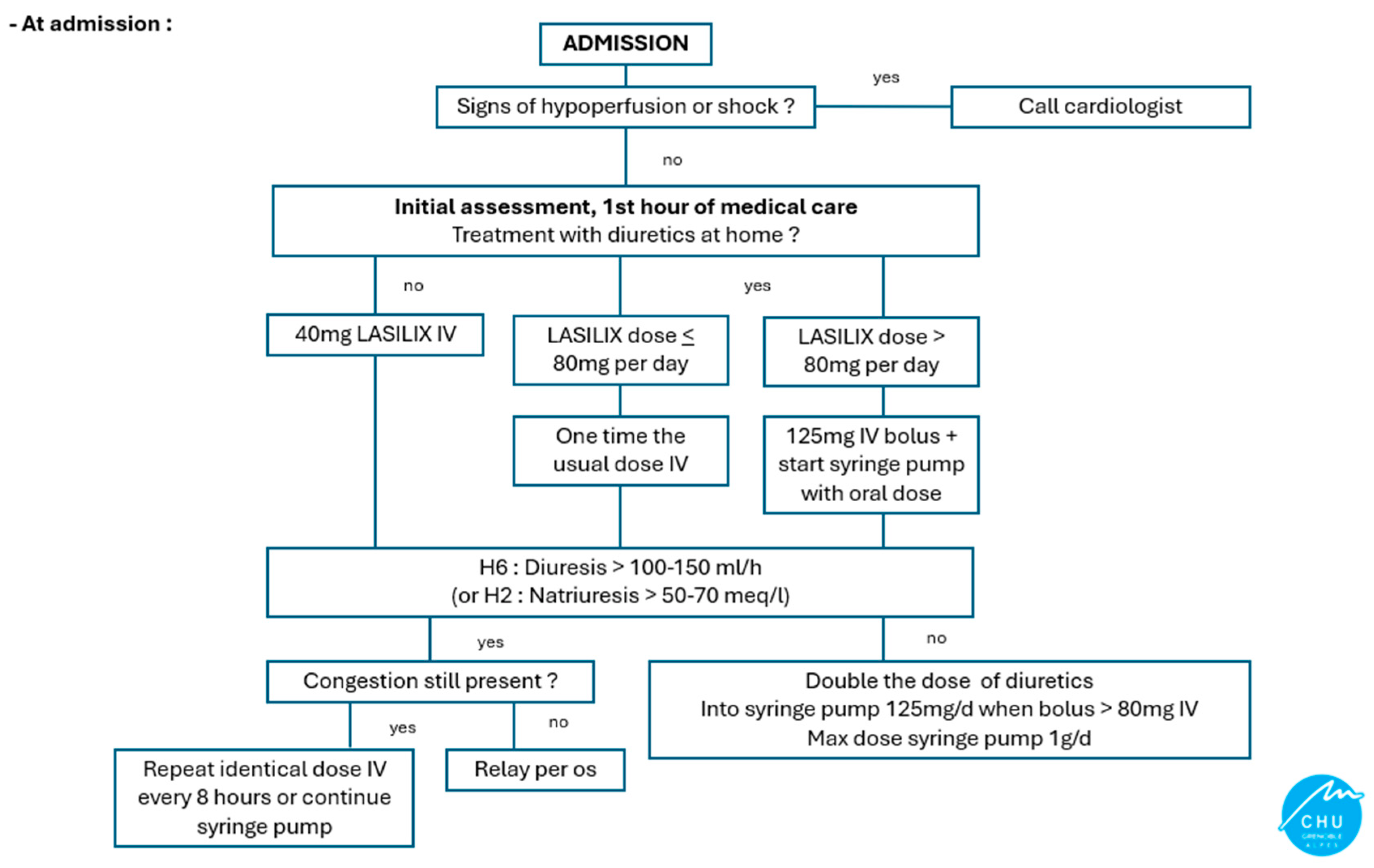
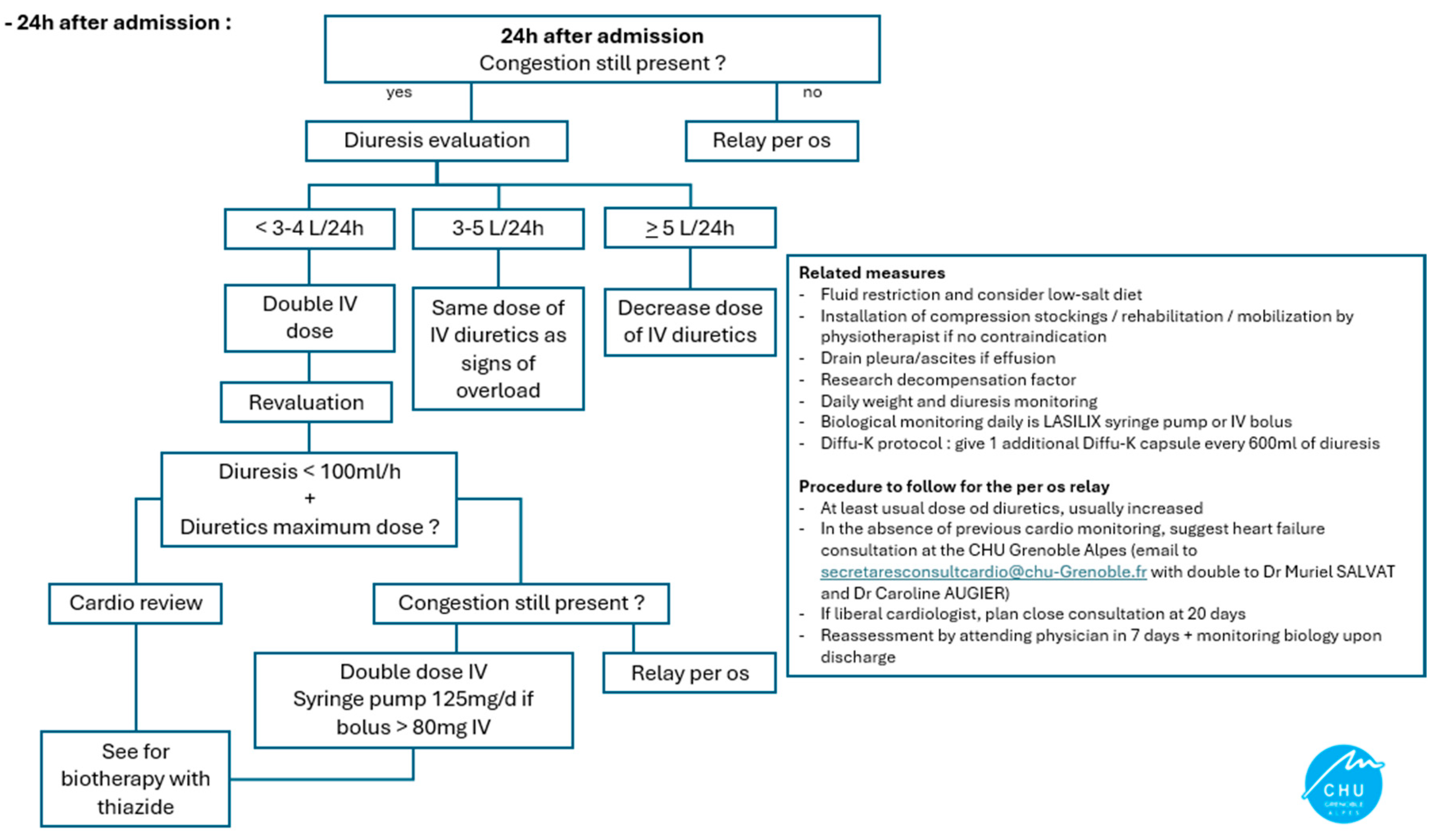
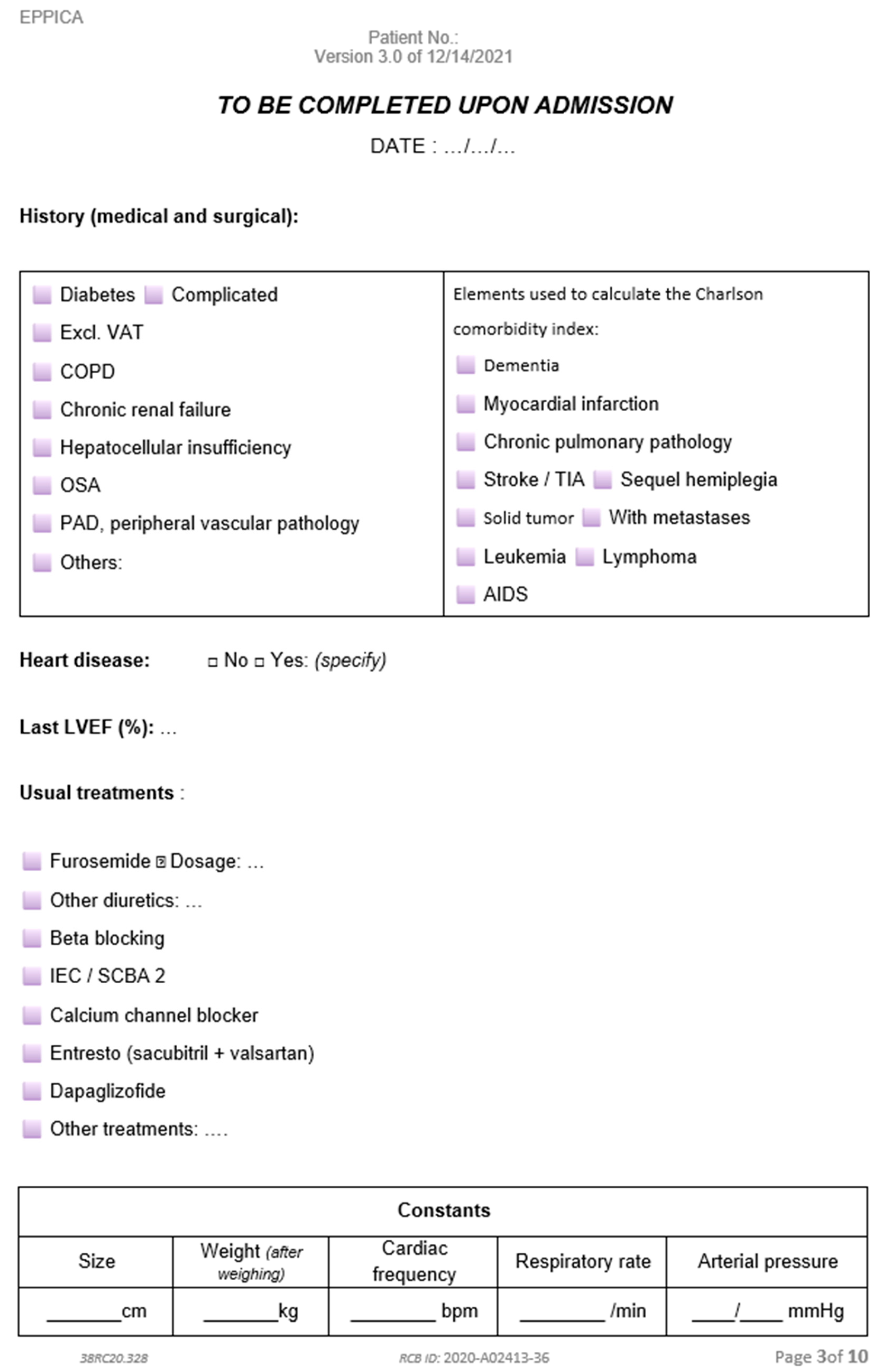
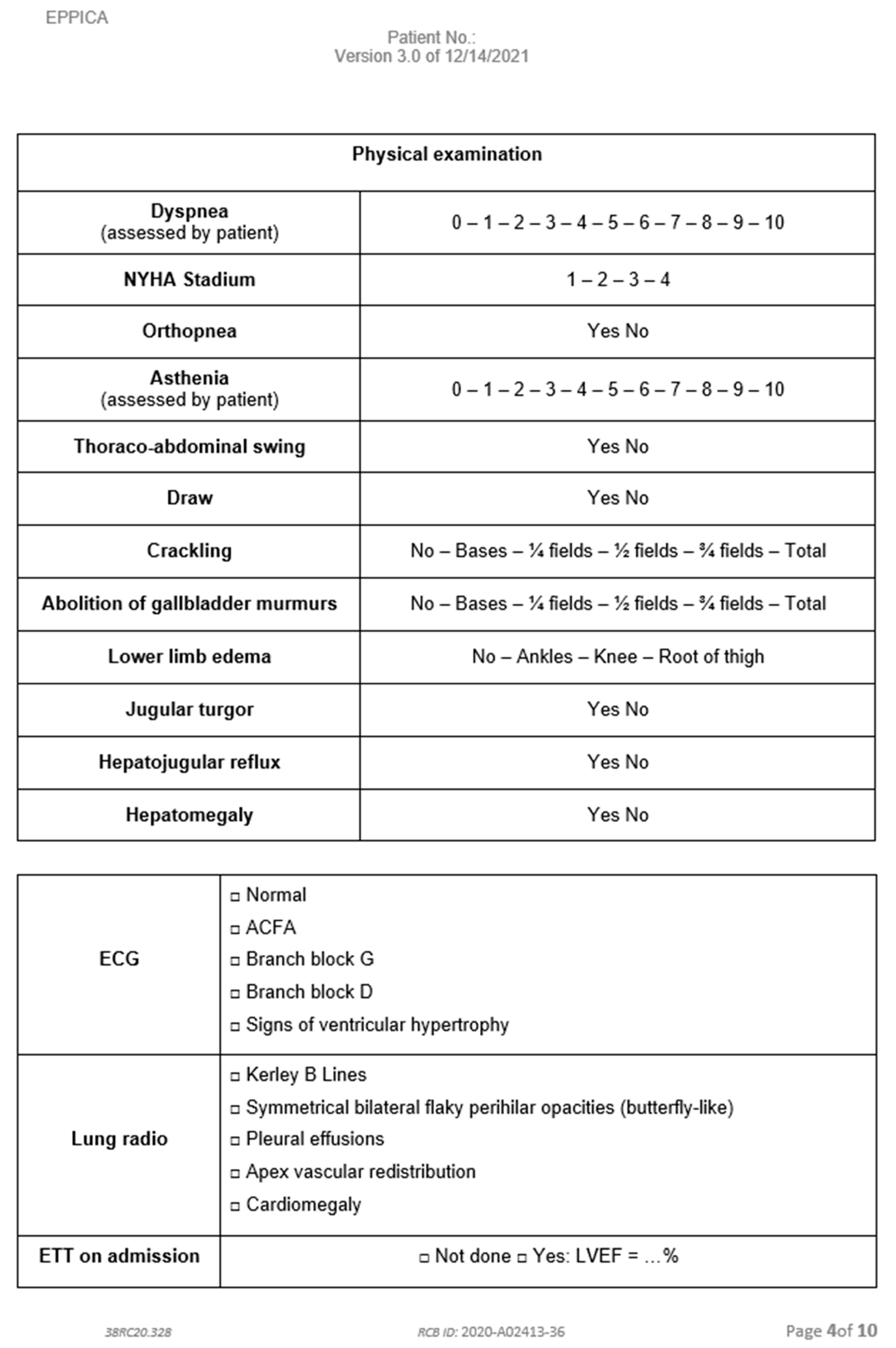
Appendix A. Diuretic Adaptation Protocol
Appendix A.1. At Admission
Appendix A.2. 24 h After Admission
Appendix B. Paper Form to Report LUS Results
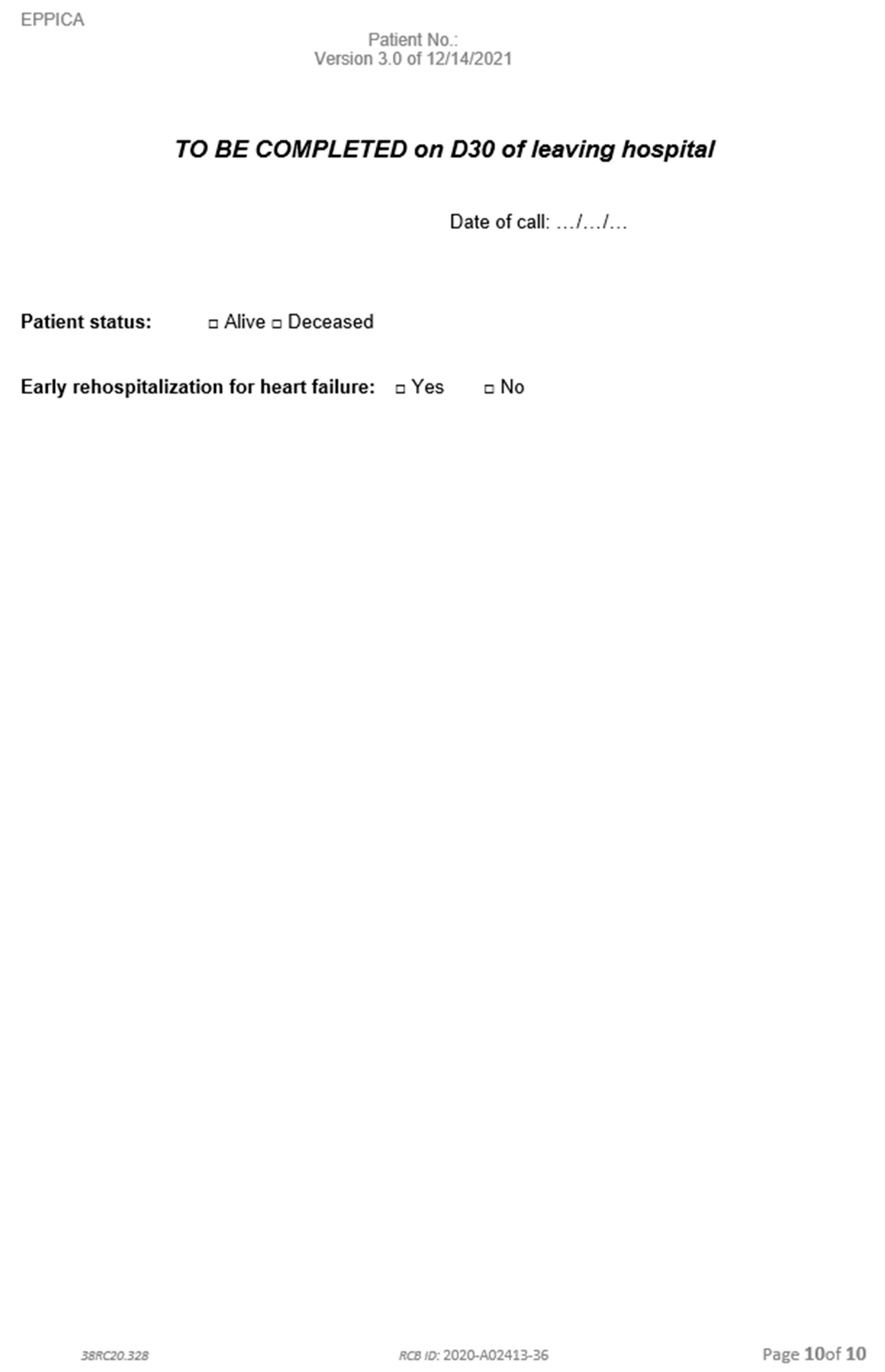
Appendix C. Follow-Up Table
| Description of the Data Collected | Pre Inclusion J0 (Entry Into Service) | Inclusion T0 | Daily During Hospitalization | Follow-Up Visit 30 days (+/− 3 Days) After the Last Ultrasound |
| Subject Information | ✔ | |||
| Checking eligibility criteria | ✔ | ✔ | ||
| Collection of clinical data | ✔ | ✔ | ||
| Collection of biological data | ✔ | ✔ * | ||
| Ultrasound | ✔ | ✔ | ||
| Collection of rehospitalizations or vital status | ✔ | |||
| Medical record review | ✔ |
Appendix D. Data Collection Notebook



Appendix E. Notice of the Committee for the Protection of Persons—4 November 2020
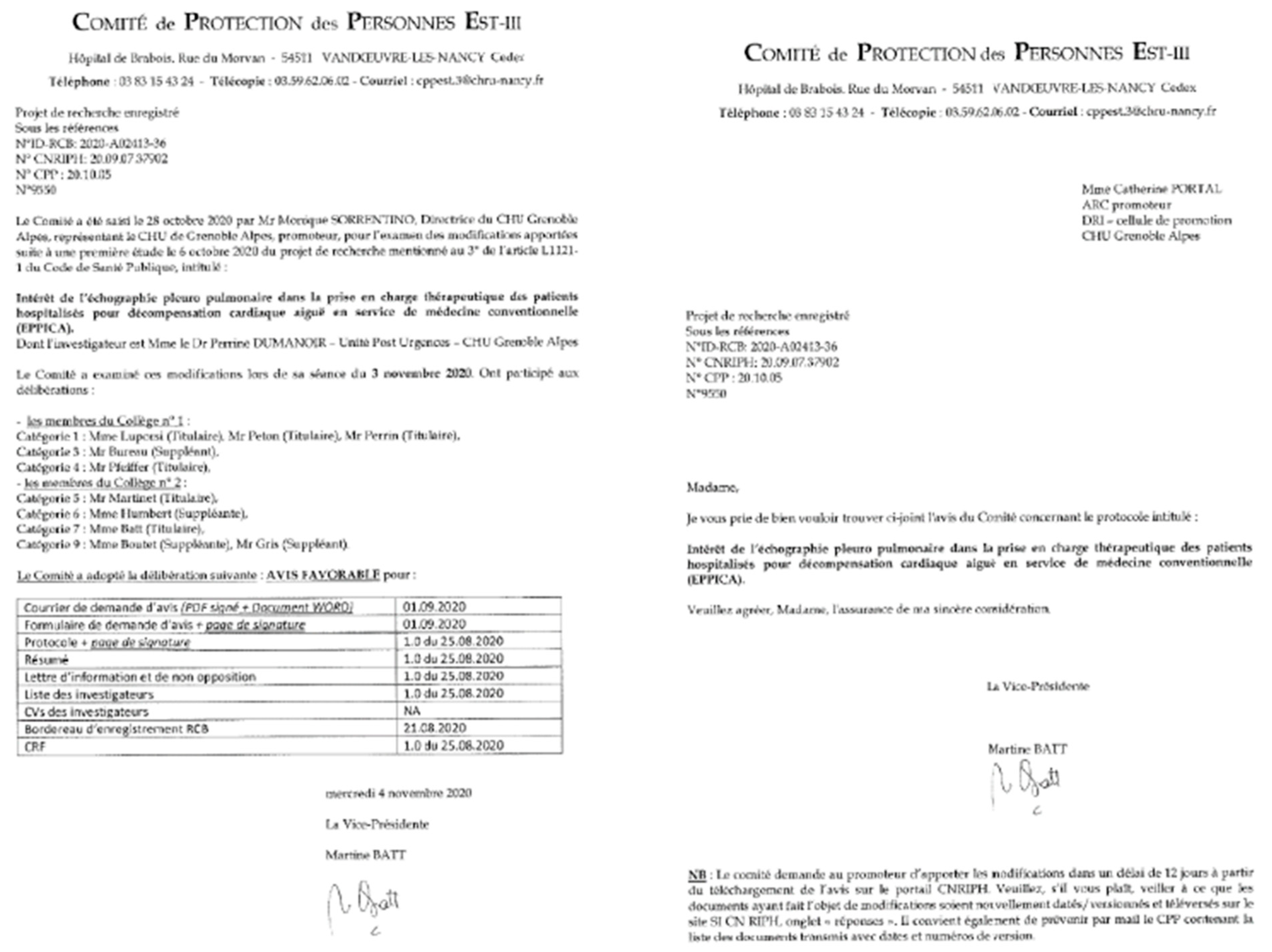
Appendix F. Notice of the Committee for the Protection of Persons—Review of Protocol on 3 March 2022

References
- L’état de Santé de la Population en France—Rapport 2017|Direction de la Recherche, des Études, de L’évaluation et des Statistiques. Available online: https://drees.solidarites-sante.gouv.fr/publications-documents-de-reference/rapports/letat-de-sante-de-la-population-en-france-rapport-2017 (accessed on 18 March 2022).
- Coiro, S.; Rossignol, P.; Ambrosio, G.; Carluccio, E.; Alunni, G.; Murrone, A.; Tritto, I.; Zannad, F.; Girerd, N. Prognostic value of residual pulmonary congestion at discharge assessed by lung ultrasound imaging in heart failure. Eur. J. Heart Fail. 2015, 17, 1172–1181. [Google Scholar] [CrossRef] [PubMed]
- Cogliati, C.; Casazza, G.; Ceriani, E.; Torzillo, D.; Furlotti, S.; Bossi, I.; Vago, T.; Costantino, G.; Montano, N. Lung ultrasound and short-term prognosis in heart failure patients. Int. J. Cardiol. 2016, 218, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Gargani, L.; Pang, P.S.; Frassi, F.; Miglioranza, M.H.; Dini, F.L.; Landi, P.; Picano, E. Persistent pulmonary congestion before discharge predicts rehospitalization in heart failure: A lung ultrasound study. Cardiovasc. Ultrasound 2015, 13, 40. [Google Scholar] [CrossRef] [PubMed]
- Torino, C.; Gargani, L.; Sicari, R.; Letachowicz, K.; Ekart, R.; Fliser, D.; Covic, A.; Siamopoulos, K.; Stavroulopoulos, A.; Massy, Z.A.; et al. The Agreement between Auscultation and Lung Ultrasound in Hemodialysis Patients: The LUST Study. Clin. J. Am. Soc. Nephrol. CJASN 2016, 11, 2005–2011. [Google Scholar] [CrossRef]
- Riocreux, C.A.M. Thèse de Médecine: Optimisation des Diurétiques Dans la Décompensation de L’insuffisance Cardiaque Chronique: Rationnel e Tdescription de L’étude ProDUCT-HF. Ph.D. Thesis, Université Clermont Auvergne, Clermont-Ferrand, France, 2019. [Google Scholar]
- Platz, E.; Merz, A.A.; Jhund, P.S.; Vazir, A.; Campbell, R.; McMurray, J.J. Dynamic changes and prognostic value of pulmonary congestion by lung ultrasound in acute and chronic heart failure: A systematic review. Eur. J. Heart Fail. 2017, 19, 1154–1163. [Google Scholar] [CrossRef]
- Girerd, N.; Seronde, M.-F.; Coiro, S.; Chouihed, T.; Bilbault, P.; Braun, F.; Kenizou, D.; Maillier, B.; Nazeyrollas, P.; Roul, G.; et al. Integrative Assessment of Congestion in Heart Failure Throughout the Patient Journey. JACC Heart Fail. 2018, 6, 273–285. [Google Scholar] [CrossRef]
- Martindale, J.L.; Wakai, A.; Collins, S.P.; Levy, P.D.; Diercks, D.; Hiestand, B.C.; Fermann, G.J.; deSouza, I.; Sinert, R. Diagnosing Acute Heart Failure in the Emergency Department: A Systematic Review and Meta-analysis. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2016, 23, 223–242. [Google Scholar] [CrossRef]
- Lichtenstein, D.A.; Mezière, G.A. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest 2008, 134, 117–125. [Google Scholar] [CrossRef]
- Öhman, J.; Harjola, V.-P.; Karjalainen, P.; Lassus, J. Focused echocardiography and lung ultrasound protocol for guiding treatment in acute heart failure. ESC Heart Fail. 2018, 5, 120–128. [Google Scholar] [CrossRef]
- Oxford Academic. 2021 ESC Guidelines for the Diagnosis and Treatment of Acute and Chronic Heart Failure. Eur. Heart J. 2021, 42, 3599–3726. Available online: https://academic.oup.com/eurheartj/article/42/36/3599/6358045?login=true (accessed on 1 June 2022). [CrossRef]
- Frasure, S.E.; Matilsky, D.K.; Siadecki, S.D.; Platz, E.; Saul, T.; Lewiss, R.E. Impact of patient positioning on lung ultrasound findings in acute heart failure. Eur. Heart J. Acute Cardiovasc. Care 2015, 4, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Buessler, A.; Chouihed, T.; Duarte, K.; Bassand, A.; Huot-Marchand, M.; Gottwalles, Y.; Pénine, A.; André, E.; Nace, L.; Jaeger, D.; et al. Accuracy of Several Lung Ultrasound Methods for the Diagnosis of Acute Heart Failure in the ED: A Multicenter Prospective Study. Chest 2020, 157, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Platz, E.; Jhund, P.S.; Girerd, N.; Pivetta, E.; McMurray, J.J.V.; Peacock, W.F.; Masip, J.; Martin-Sanchez, F.J.; Miró, Ò.; Price, S.; et al. Expert consensus document: Reporting checklist for quantification of pulmonary congestion by lung ultrasound in heart failure. Eur. J. Heart Fail. 2019, 21, 844–851. [Google Scholar] [CrossRef] [PubMed]
- Pang, P.S.; Russell, F.M.; Ehrman, R.; Ferre, R.; Gargani, L.; Levy, P.D.; Noble, V.; Lane, K.A.; Li, X.; Collins, S.P. Lung Ultrasound-Guided Emergency Department Management of Acute Heart Failure (BLUSHED-AHF): A Randomized Controlled Pilot Trial. JACC Heart Fail. 2021, 9, 638–648. [Google Scholar] [CrossRef]
- Panuccio, V.; Tripepi, R.; Parlongo, G.; Mafrica, A.; Caridi, G.; Catalano, F.; Marino, F.; Tripepi, G.; Mallamaci, F.; Zoccali, C. Lung ultrasound to detect and monitor pulmonary congestion in patients with acute kidney injury in nephrology wards: A pilot study. J. Nephrol. 2020, 33, 335–341. [Google Scholar] [CrossRef]
- Rivas-Lasarte, M.; Álvarez-García, J.; Fernández-Martínez, J.; Maestro, A.; López-López, L.; Solé-González, E.; Pirla, M.J.; Mesado, N.; Mirabet, S.; Fluvià, P.; et al. Lung ultrasound-guided treatment in ambulatory patients with heart failure: A randomized controlled clinical trial (LUS-HF study). Eur. J. Heart Fail. 2019, 21, 1605–1613. [Google Scholar] [CrossRef]
- Rivas-Lasarte, M.; Maestro, A.; Fernández-Martínez, J.; López-López, L.; Solé-González, E.; Vives-Borrás, M.; Montero, S.; Mesado, N.; Pirla, M.J.; Mirabet, S.; et al. Prevalence and prognostic impact of subclinical pulmonary congestion at discharge in patients with acute heart failure. ESC Heart Fail. 2020, 7, 2621–2628. [Google Scholar] [CrossRef]
- Ramos-Hernández, C.; Botana-Rial, M.; Núñez-Fernández, M.; Lojo-Rodríguez, I.; Mouronte-Roibas, C.; Salgado-Barreira, Á.; Ruano-Raviña, A.; Fernández-Villar, A. Validity of Lung Ultrasound: Is an Image Worth More Than a Thousand Sounds? J. Clin. Med. 2021, 10, 2292. [Google Scholar] [CrossRef]
- Ruggenenti, P.; Remuzzi, G. Worsening kidney function in decompensated heart failure: Treat the heart, don’t mind the kidney. Eur. Heart J. 2011, 32, 2476–2478. [Google Scholar] [CrossRef]
- Blair, J.E.A.; Pang, P.S.; Schrier, R.W.; Metra, M.; Traver, B.; Cook, T.; Campia, U.; Ambrosy, A.; Burnett, J.C.; Grinfeld, L.; et al. Changes in renal function during hospitalization and soon after discharge in patients admitted for worsening heart failure in the placebo group of the EVEREST trial. Eur. Heart J. 2011, 32, 2563–2572. [Google Scholar] [CrossRef]
- Virani, S.S.; Alonso, A.; Aparicio, H.J.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2021 Update. Circulation 2021, 143, e254–e743. [Google Scholar] [PubMed]
- Platz, E.; Campbell, R.T.; Claggett, B.; Lewis, E.F.; Groarke, J.D.; Docherty, K.F.; Lee, M.M.Y.; Merz, A.A.; Silverman, M.; Swamy, V.; et al. Lung Ultrasound in Acute Heart Failure: Prevalence of Pulmonary Congestion and Short- and Long-Term Outcomes. JACC Heart Fail. 2019, 7, 849–858. [Google Scholar] [CrossRef] [PubMed]
- Miglioranza, M.H.; Gargani, L.; Sant’Anna, R.T.; Rover, M.M.; Martins, V.M.; Mantovani, A.; Weber, C.; Moraes, M.A.; Feldman, C.J.; Kalil, R.A.K.; et al. Lung ultrasound for the evaluation of pulmonary congestion in outpatients: A comparison with clinical assessment, natriuretic peptides, and echocardiography. JACC Cardiovasc. Imaging 2013, 6, 1141–1151. [Google Scholar] [CrossRef]
- Komajda, M.; Hanon, O.; Hochadel, M.; Lopez-Sendon, J.L.; Follath, F.; Ponikowski, P.; Harjola, V.-P.; Drexler, H.; Dickstein, K.; Tavazzi, L.; et al. Contemporary management of octogenarians hospitalized for heart failure in Europe: Euro Heart Failure Survey II. Eur. Heart J. 2009, 30, 478–486. [Google Scholar] [CrossRef]
- Formiga, F.; Moreno-Gonzalez, R.; Chivite, D.; Franco, J.; Montero, A.; Corbella, X. High comorbidity, measured by the Charlson Comorbidity Index, associates with higher 1-year mortality risks in elderly patients experiencing a first acute heart failure hospitalization. Aging Clin. Exp. Res. 2018, 30, 927–933. [Google Scholar] [CrossRef]
- Bannay, A.; Chaignot, C.; Blotière, P.-O.; Basson, M.; Weill, A.; Ricordeau, P.; Alla, F. The Best Use of the Charlson Comorbidity Index with Electronic Health Care Database to Predict Mortality. Med. Care 2016, 54, 188–194. [Google Scholar] [CrossRef]
- Freund, Y.; Cachanado, M.; Delannoy, Q.; Laribi, S.; Yordanov, Y.; Gorlicki, J.; Chouihed, T.; Féral-Pierssens, A.-L.; Truchot, J.; Desmettre, T.; et al. Effect of an Emergency Department Care Bundle on 30-Day Hospital Discharge and Survival Among Elderly Patients with Acute Heart Failure: The ELISABETH Randomized Clinical Trial. JAMA 2020, 324, 1948–1956. [Google Scholar] [CrossRef]
- Teixeira, A.; Parenica, J.; Park, J.J.; Ishihara, S.; AlHabib, K.F.; Laribi, S.; Maggioni, A.; Miró, Ò.; Sato, N.; Kajimoto, K.; et al. Clinical presentation and outcome by age categories in acute heart failure: Results from an international observational cohort. Eur. J. Heart Fail. 2015, 17, 1114–1123. [Google Scholar] [CrossRef]
- Russell, F.M.; Ferre, R.; Ehrman, R.R.; Noble, V.; Gargani, L.; Collins, S.P.; Levy, P.D.; Fabre, K.L.; Eckert, G.J.; Pang, P.S. What are the minimum requirements to establish proficiency in lung ultrasound training for quantifying B-lines? ESC Heart Fail. 2020, 7, 2941–2947. [Google Scholar] [CrossRef]
- Mazzola, M.; Pugliese, N.R.; Zavagli, M.; De Biase, N.; Bandini, G.; Barbarisi, G.; D’Angelo, G.; Sollazzo, M.; Piazzai, C.; David, S.; et al. Diagnostic and Prognostic Value of Lung Ultrasound B-Lines in Acute Heart Failure with Concomitant Pneumonia. Front. Cardiovasc. Med. 2021, 8, 693912. [Google Scholar] [CrossRef]
- Yang, F.; Wang, Q.; Zhi, G.; Zhang, L.; Huang, D.; Shen, D.; Zhang, M. The application of lung ultrasound in acute decompensated heart failure in heart failure with preserved and reduced ejection fraction. Echocardiography 2017, 34, 1462–1469. [Google Scholar] [CrossRef] [PubMed]
- Palazzuoli, A.; Ruocco, G.; Beltrami, M.; Nuti, R.; Cleland, J.G. Combined use of lung ultrasound, B-type natriuretic peptide, and echocardiography for outcome prediction in patients with acute HFrEF and HFpEF. Clin. Res. Cardiol. Off. J. Ger. Card. Soc. 2018, 107, 586–596. [Google Scholar] [CrossRef]

| No. | Mean (SD) or No. (%) | |
|---|---|---|
| Baseline characteristics | ||
| Age, years (extremes) | 42 | 85.8 (SD 8.2) (71.7–98.8) |
| Male gender | 42 | 26 (61.9%) |
| BMI (kg/m2) | 39 | 26.5 (SD 6.2) |
| Charlson Comorbidity Index | 42 | 8.5 (SD 2.3) |
| Chronic kidney disease | 42 | 22 (52%) |
| Hypertension | 42 | 32 (76%) |
| Diabetes | 42 | 18 (43%) |
| Previous cardiac history | ||
| Know heart disease | 42 | 31 (73.8%) |
| LVEF | 25 | 49.8 (SD 13.5) |
| Daily per os furosemide posology (mg) | 42 | 132.5 (SD 231.5) |
| Triggering factor of AHF | ||
| Unknown | 42 | 8 (19.0%) |
| Anemia | 42 | 9 (21.4%) |
| Pneumopathy | 42 | 8 (21.4%) |
| Atrial fibrillation | 42 | 5 (11.9%) |
| Other bacterial infections (pyelonephritis, erysipelas) | 42 | 4 (9.5%) |
| Recent decrease in diuretic treatment | 42 | 2 (4.8%) |
| Non-compliance in healthcare | 42 | 2 (4.8%) |
| Pulmonary embolism | 42 | 1 (2.4%) |
| Altitude hypoxemia | 42 | 1 (2.4%) |
| COVID-19 | 42 | 1 (2.4%) |
| Biological and radiography characteristics at admission | ||
| Hemoglobin (g/dL) | 42 | 11.2 (SD 1.9) |
| Ferritin (ng/mL) | 30 | 167.1 (SD 199.2) |
| Transferrin saturation (%) | 30 | 12.4 (SD 9.1) |
| Creatinine (µmol/L) | 42 | 134.9 (SD 55.0) |
| Urea (mmol/L) | 42 | 14.7 (SD 9.5) |
| Natremia (mmol/L) | 42 | 139.8 (SD 3.8) |
| Kalemia (mmol/L) | 41 | 4.2 (SD 0.7) |
| NT-pro BNP (ng/L) | 41 | 9041 (SD 8770.6) |
| Albumin (g/L) | 35 | 32.1 (SD 5.6) |
| Signs of pulmonary oedema on chest radiography | 36 | 30 (83.3%) |
| During hospitalization | ||
| Length of hospitalization (days) | 42 | 8.0 (5.1) |
| Furosemide posology IV received in ED (mg) | 42 | 122.4 (SD 214.5) |
| Furosemide posology IV/24h on admission (mg) | 42 | 159.2 (SD 256.5) |
| Intra-venous iron supplementation | 42 | 24 (57.1%) |
| Dietetic consultation | 42 | 15 (35.7%) |
| Physiotherapy | 42 | 25 (59.5%) |
| Therapeutic patient education | 42 | 5 (11.9%) |
| At discharge | ||
| Daily per os furosemide posology (mg) | 42 | 153.9 (SD 268.5) |
| Biological check-up at 7 days | 42 | 22 (52.4%) |
| Consultation with attending physician at 7 days | 42 | 18 (42.9%) |
| Consultation with cardiologist at 20 days | 42 | 20 (47.6%) |
| Admission (0%) | 25% | 50% | 75% | Discharge (100%) | ||
|---|---|---|---|---|---|---|
| Weight loss Mean (SD) [n] | - | −0.8 (−0.4) [24] | −1.7 (−0.8) [22] | −1.6 (−1.2) [21] | −2.7 (−1.6) [20] | |
| Dyspnea (self-evaluation) Mean (SD) [n] | 5.1 (3.2) [34] | 3.3 (2.9) [25] | 2.1 (2.5) [26] | 1.8 (2.3) [25] | 1.7 (2.2) [28] | |
| NYHA Mean (SD) [n] | 3.1 (1.0) [35] | 2.3 (1.0) [27] | 2.2 (1.0) [27] | 2.1 (0.9) [23] | 2.2 (0.9) [27] | |
| Orthopnea % of total [n] | Yes | 36.6% [15] | 14.7% [5] | 9.7% [3] | 7.4% [2] | 2.6% [1] |
| No | 63.4% [26] | 85.3% [29] | 90.3% [28] | 92.6% [25] | 97.4% [37] | |
| Asthenia (self-evaluation) Mean (SD) [n] | 5.6 (3.0) [31] | 4.4 (2.7) [23] | 3.9 (3.0) [20] | 3.3 (3.2) [18] | 3.2 (2.6) [21] | |
| Crackles % of total [n] | No | 24.4% [10] | 32.3% [10] | 35.5% [11] | 30.0% [9] | 44.7% [17] |
| Base | 26.8% [11] | 38.7% [12] | 48.4% [15] | 53.3% [16] | 31.6% [12] | |
| 1/4 lung | 12.2% [5] | 6.5% [2] | 6.5% [2] | 10.0% [3] | 21.1% [8] | |
| 1/2 lung | 29.3% [12] | 22.6% [7] | 9.7% [3] | 6.7% [2] | 2.6% [1] | |
| 3/4 lung | 7.3% [3] | 0.0% [0] | 0.0% [0] | 0.0% [0] | 0.0% [0] | |
| VM abolition % of total [n] | No | 61.0% [25] | 75.0% [24] | 63.3% [19] | 63.3% [19] | 84.2% [32] |
| Base | 22.0% [9] | 9.4% [3] | 23.3% [7] | 26.7% [8] | 10.5% [4] | |
| 1/4 lung | 4.9% [2] | 6.2% [2] | 3.3% [1] | 3.3% [1] | 5.3% [2] | |
| 1/2 lung | 7.3% [3] | 6.2% [2] | 6.7% [2] | 6.7% [2] | 0.0% [0] | |
| 3/4 lung | 2.4% [1] | 3.1% [1] | 3.3% [1] | 0.0% [0] | 0.0% [0] | |
| All lung | 2.4% [1] | 0.0% [0] | 0.0% [0] | 0.0% [0] | 0.0% [0] | |
| Lower limbs oedema % of total [n] | No | 33.3% [14] | 50.0% [16] | 14 (46.7%) | 48.3% [14] | 56.8% [21] |
| Ankle | 28.6% [12] | 21.9% [7] | 12 (40.0%) | 44.8% [13] | 45.1% [13] | |
| Knee | 28.6% [12] | 25.0% [8] | 3 (10.0%) | 6.9% [2] | 5.4% [2] | |
| Thigh | 9.5% [4] | 3.1% [1] | 1 (3.3%) | 0.0% [0] | 2.7% [1] | |
| Creatinine (µmol/L) Mean (SD) [n] | 133.7 (55.1) [42] | 139.1 (51.8) [30] | 139.8 (54.0) [26] | 144.1 (58.5) [21] | 142.8 (57.5) [30] | |
| Furosemide posology (IV, mg) Mean (SD) [n] | 162.1 (SD 259.0) [42] | 147.4 (224.7) [35] | 124.0 (220.2) [36] | 80.5 (137.4) [34] | 77.0 (134.2) [42] | |
| Pleural effusion % of total [n] | Yes | 61.5% [8] | 60.0% [15] | 48.0% [12] | 46.2% [12] | 35.7% [10] |
| No | 38.5% [5] | 40.0% [10] | 52.0% [13] | 53.8% [14] | 64.3% [18] | |
| B-lines left Mean (SD) [n] | 9.1 (7.5) [13] | 6.8 (5.1) [25] | 5.6 (5.1) [25] | 4.8 (4.1) [26] | 4.5 (3.5) [28] | |
| B-lines right Mean (SD) [n] | 9.8 (7.1) [13] | 8.2 (6.9) [25] | 6.3 (4.8) [25] | 6.0 (4.2) [26] | 3.9 (4.0) [28] | |
| Total B-lines Mean (SD) [n] | 18.1 (13.0) [13] | 13.4 (10.2) [25] | 11.9 (9.4) [25] | 10.8 (7.8) [26] | 8.4 (6.8) [28] | |
| Hospitalization Time | Median of B-Lines | Median of Diuretic Posology | B-Lines Tendency | Diuretic Posology Tendency | p-Value Univariate | p-Value multivariate 1 |
|---|---|---|---|---|---|---|
| 0% | 17 | 40 | 0.941 | 0.869 | ||
| 25% | 11 | 40 | 0.65 | 1 | 0.901 | 0.960 |
| 50% | 7 | 40 | 0.64 | 1 | 0.216 | 0.396 |
| 75% | 8.5 | 35 | 1.21 | 0.88 | 0.306 | 0.591 |
| 100% | 7.5 | 20 | 0.88 | 0.57 | 0.305 | 0.737 |
| Hospitalization Time | Intensity of Clinic Sign | No. | B-Lines Mean (SD) [Count] | p Value 1 |
|---|---|---|---|---|
| Admission (0%) | Absent | 13 | 14.7 (9.1) [3] | 0.295 |
| Moderate a | 12.8 (14.4) [5] | |||
| Severe b | 25.4(12.3) [5] | |||
| 25% | Absent | 31 | 10.3 (11.4) [10] | 0.824 |
| Moderate a | 8.7 (9.9) [14] | |||
| Severe b | 11.7 (11.1) [7] | |||
| 50% | Absent | 31 | 9.8 (11.8) [11] | 0.539 |
| Moderate a | 9.1 (8.3) [17] | |||
| Severe b | 3.0 (3.6) [3] | |||
| 75% | Absent | 30 | 12.8 (9.4) [9] | 0.223 |
| Moderate a | 7.4 (7.9) [19] | |||
| Severe b | 4.5 (6.4) [2] | |||
| At discharge (100%) | Absent | 39 | 6.6 (7.1) [17] | 0.055 |
| Moderate a | 3.9 (6.4) [21] | |||
| Severe b | 20.0 (NA) [1] |
| At Discharge | No Crackles | Bases Crackles | ¼ Lung Crackles | ½ Lung Crackles | ¾ Lung Crackles | All Lung Crackles | p-Value 1 |
|---|---|---|---|---|---|---|---|
| B lines Mean (SD) [n] | 6.6 (7.1) [17] | 4.1 (7.2) [13] | 3.6 (5.4) [8] | 20.0 (NA) [1] | 0.0 (NA) [0] | 0.0 (NA) [0] | 0.124 |
| Hospitalization Time | CDK History | No. | Creatinine in µmol/L Mean (SD) [n] | B-Lines Mean (SD) [n] | p Value 1 |
|---|---|---|---|---|---|
| Admission (0%) | Yes | 22 | 174.2 (43.1) [22] | 24.2 (11.6) [8] | 0.023 |
| No | 20 | 91.8 (26.9) [20] | 8.2 (8.8) [5] | ||
| 25% | Yes | 22 | 174.3 (43.8) [15] | 14.6 (9.4) [16] | 0.450 |
| No | 20 | 103.9 (31.4) [15] | 11.3 (11.7) [9] | ||
| 50% | Yes | 22 | 170.5 (49.8) [15] | 13.7 (10.2) [12] | 0.373 |
| No | 20 | 98.0 (21.7) [11] | 10.2 (8.7) [13] | ||
| 75% | Yes | 22 | 171.8 (56.6) [13] | 14.4 (8.5) [14] | 0.008 |
| No | 20 | 99.1 (23.3) [8] | 6.7 (3.9) [12] | ||
| At discharge (100%) | Yes | 22 | 169.8 (57) [18] | 9.2 (7.5) [18] | 0.406 |
| No | 20 | 102.3 (26.9) [12] | 6.9 (5.2) [10] |
| At 30-Days After Discharge | B-Lines Mean (SD) [n] at Discharge | p-Value 1 | |
|---|---|---|---|
| Vital status | Death (all causes) | 15.2 (10.1) [5] | <0.001 |
| Alive | 3.9 (5.4) [37] | ||
| Hospital status for AHF | Readmission | 4.9 (5.4) [8] | 0.469 |
| No readmission | 4.1 (5.7) [30] | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bel Alonso, E.; Grember, A.; Cheval, C.; Papillon, R.; Mairot, L.; Deroux, A.; Bouillet, L.; Bellier, A.; Dumanoir, P. Interest of Lung Ultrasound in the Management of Acute Heart Failure in Post-Emergency Service. Life 2025, 15, 752. https://doi.org/10.3390/life15050752
Bel Alonso E, Grember A, Cheval C, Papillon R, Mairot L, Deroux A, Bouillet L, Bellier A, Dumanoir P. Interest of Lung Ultrasound in the Management of Acute Heart Failure in Post-Emergency Service. Life. 2025; 15(5):752. https://doi.org/10.3390/life15050752
Chicago/Turabian StyleBel Alonso, E., A. Grember, C. Cheval, R. Papillon, L. Mairot, A. Deroux, L. Bouillet, A. Bellier, and P. Dumanoir. 2025. "Interest of Lung Ultrasound in the Management of Acute Heart Failure in Post-Emergency Service" Life 15, no. 5: 752. https://doi.org/10.3390/life15050752
APA StyleBel Alonso, E., Grember, A., Cheval, C., Papillon, R., Mairot, L., Deroux, A., Bouillet, L., Bellier, A., & Dumanoir, P. (2025). Interest of Lung Ultrasound in the Management of Acute Heart Failure in Post-Emergency Service. Life, 15(5), 752. https://doi.org/10.3390/life15050752





