The Effects of the COVID-19 Pandemic on Trends and Types of Pediatric Burn Injuries: Lessons from a National Burn Center and the Role of Strategic Resource Allocation
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Żwierełło, W.; Piorun, K.; Skórka-Majewicz, M.; Maruszewska, A.; Antoniewski, J.; Gutowska, I. Burns: Classification, Pathophysiology, and Treatment: A Review. Int. J. Mol. Sci. 2023, 24, 3749. [Google Scholar] [CrossRef] [PubMed]
- Bordeanu-Diaconescu, E.-M.; Grosu-Bularda, A.; Frunza, A.; Grama, S.; Andrei, M.-C.; Neagu, T.P.; Hariga, C.-S.; Lascar, I. Venous Thromboembolism in Burn Patients: A 5-Year Retrospective Study. Medicina 2024, 60, 258. [Google Scholar] [CrossRef]
- Badoiu, S.C.; Enescu, D.M.; Tatar, R.; Miricescu, D.; Stanescu-Spinu, I.-I.; Greabu, M.; Coricovac, A.M.; Badoiu, S.E.; Jinga, V. Adipokines—A Cohort Prospective Study in Children with Severe Burns. Int. J. Mol. Sci. 2024, 25, 7630. [Google Scholar] [CrossRef]
- Bordeanu-Diaconescu, E.M.; Grosu-Bularda, A.; Frunza, A.; Grama, S.; Andrei, M.C.; Neagu, T.P.; Lascar, I.; Hariga, C.S. Diagnostic and Prognostic Value of Thrombocytopenia in Severe Burn Injuries. Diagnostics 2024, 14, 582. [Google Scholar] [CrossRef] [PubMed]
- Pelizzo, G.; Lanfranchi, G.; Pantaloni, M.; Camporesi, A.; Tommasi, P.; Durante, E.; Costanzo, S.; Canonica, C.M.P.; Zoia, E.; Zuccotti, G.; et al. Epidemiological and Clinical Profile of Pediatric Burns in the COVID-19 Era: The Experience of a Reference Center. Children 2022, 9, 1735. [Google Scholar] [CrossRef]
- Jeschke, M.G.; van Baar, M.E.; Choudhry, M.A.; Chung, K.K.; Gibran, N.S.; Logsetty, S. Burn injury. Nat. Rev. Dis. Primers 2020, 6, 11. [Google Scholar] [CrossRef] [PubMed]
- Badoiu, S.C.; Enescu, D.M.; Tatar, R.; Stanescu-Spinu, I.-I.; Miricescu, D.; Greabu, M.; Ionel, I.P.; Jinga, V. Serum Plasminogen Activator Inhibitor-1, α 1-Acid Glycoprotein, C-Reactive Protein, and Platelet Factor 4 Levels—Promising Molecules That Can Complete the “Puzzle” of the Biochemical Milieu in Severe Burns: Preliminary Results of a Cohort Prospective Study. J. Clin. Med. 2024, 13, 2794. [Google Scholar] [CrossRef]
- Erturk, A.; Demir, S.; Oztorun, C.İ.; Erten, E.E.; Guney, D.; Bostanci, S.A.; Sahin, V.S.; Kiris, A.G.; Bay, H.K.; Bedir Demirdag, T.; et al. Management of a Pediatric Burn Center During the COVID-19 Pandemic. J. Burn Care Res. 2022, 43, 468–473. [Google Scholar] [CrossRef]
- Delfani, F.; Shoghi, M. Burn care strategy in the COVID-19 pandemic: A narrative review study. Int. J. Burns Trauma 2021, 11, 289–295. [Google Scholar]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. China Novel Coronavirus Investigating and Research Team. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar]
- Crăciun, M.D.; Nițescu, G.V.; Golumbeanu, M.; Tănase, A.A.; Pițigoi, D.; Săndulescu, O.; Crăciun, P.; Enciu, B.G.; Bălănescu, R.N.; Ulici, A. mRNA COVID-19 Vaccine Reactogenicity among Healthcare Workers: Results from an Active Survey in a Pediatric Hospital from Bucharest, January–February 2021. Vaccines 2022, 10, 836. [Google Scholar] [CrossRef]
- Barret, J.P.; Chong, S.J.; Depetris, N.; Fisher, M.D.; Luo, G.; Moiemen, N.; Pham, T.; Qiao, L.; Wibbenmeyer, L.; Matsumura, H. Burn center function during the COVID-19 pandemic: An international multi-center report of strategy and experience. Burns 2020, 46, 1021–1035. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Kain, R.; More, A.; Sheth, S.; Arumugam, P.K. Burns and COVID-19-Initial Experience and Challenges. J. Burn Care Res. 2021, 42, 794–800. [Google Scholar] [CrossRef]
- Laura, P.; José, A.; Nikki, A.; Khaled, A.; Barret, J.; Jeffery, C.; Shobha, C.; Jack, C.S.; Scott, C.; Nadia, D.; et al. Impact of COVID-19 on global burn care. Burns 2022, 48, 1301–1310. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Liu, T.; Chen, H.; Liao, J.; Li, H.; Luo, Q.; Song, H.; Xiang, F.; Tan, J.; Zhou, J.; et al. Management strategies for the burn ward during COVID-19 pandemic. Burns 2020, 46, 756–761. [Google Scholar] [CrossRef] [PubMed]
- Farroha, A. Effects of COVID-19 pandemic on burns epidemiology. Burns 2020, 46, 1466. [Google Scholar] [CrossRef] [PubMed]
- Chu, H.; Reid, G.; Sack, A.; Heryet, R.; Mackie, I.; Sen, S.K. Changes in burn referrals and injuries during COVID-19. Burns 2020, 46, 1469–1470. [Google Scholar] [CrossRef]
- Monte-Soldado, A.; López-Masramon, B.; Rivas-Nicolls, D.; Andrés-Collado, A.; Aguilera-Sáez, J.; Serracanta, J.; Barret, J.P. Changes in the epidemiologic profile of burn patients during the lockdown in Catalonia (Spain): A warning call to strengthen prevention strategies in our community. Burns 2022, 48, 228–233. [Google Scholar] [CrossRef]
- Akkoç, M.F.; Bülbüloğlu, S.; Özdemir, M. The effects of lockdown measures due to COVID-19 pandemic on burn cases. Int. Wound J. 2021, 18, 367–374. [Google Scholar] [CrossRef]
- Kruchevsky, D.; Levanon, S.; Givon, A.; Bodas, M.; Israeli Trauma Group; Ramon, Y.; Ullmann, Y.; Zeltzer, A.A. Burns During Coronavirus Disease 19 Lockdown: A Multi-Center Retrospective Study in Israel. J. Burn Care Res. 2023, 44, 75–80. [Google Scholar] [CrossRef]
- Yamamoto, R.; Sato, Y.; Matsumura, K.; Sasaki, J. Characteristics of burn injury during COVID-19 pandemic in Tokyo: A descriptive study. Burns Open 2021, 5, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Charvillat, O.; Plancq, M.C.; Haraux, E.; Gouron, R.; Klein, C. Epidemiological analysis of burn injuries in children during the first COVID-19 lockdown, and a comparison with the previous five years. Ann. Chir. Plast. Esthet. 2021, 66, 285–290. [Google Scholar]
- Yaacobi Shilo, D.; Ad-El, D.; Kalish, E.; Yaacobi, E.; Olshinka, A. Management Strategies for Pediatric Burns During the COVID-19 Pandemic. J. Burn Care Res. 2021, 42, 141–143. [Google Scholar] [CrossRef] [PubMed]
- Kruchevsky, D.; Arraf, M.; Levanon, S.; Capucha, T.; Ramon, Y.; Ullmann, Y. Trends in Burn Injuries in Northern Israel During the COVID-19 Lockdown. J. Burn Care Res. 2021, 42, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Kawalec, A.M. The changes in the number of patients admissions due to burns in Paediatric Trauma Centre in Wroclaw (Poland) in March 2020. Burns 2020, 46, 1713–1714. [Google Scholar]
- Amin, D.; Manhan, A.J.; Mittal, R.; Abramowicz, S. Pediatric head and neck burns increased during early COVID-19 pandemic. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2022, 134, 528–532. [Google Scholar] [CrossRef]
- Keays, G.; Friedman, D.; Gagnon, I. Injuries in the time of COVID-19. Health Promot. Chronic. Dis. Prev. Can. 2020, 40, 336–341. [Google Scholar] [CrossRef]
- Solís, F.F.; Saavedra, O.R.; Zalavari, P.K.; Paredes, M.C. Effects of COVID-19 lockdown on the demand for health care of children and adolescents with burns in three specialized outpatient centers in Chile. Andes. Pediatr. 2021, 92, 854–861. [Google Scholar]
- D’Asta, F.; Choong, J.; Thomas, C.; Adamson, J.; Wilson, Y.; Wilson, D.; Moiemen, N.; Farroha, A. Paediatric burns epidemiology during COVID-19 pandemic and “stay home” era. Burns 2020, 6, 1471–1472. [Google Scholar]
- Altıner, S.; Tuncal, S.; Ünal, Y.; Çöl, M.; Büyükkasap, Ç.; Pekcici, M.R. The effect of COVID-19 pandemic on the number of patients in burns services. Int. Wound J. 2022, 19, 1975–1979. [Google Scholar] [CrossRef]
- World Health Organization. The International Statistical Classification of Diseases and Related Health Problems, Twelfth Revision, Australian Modification (ICD-10-AM); World Health Organisation: Geneva, Switzerland, 2022; ISBN 1864874130-9. [Google Scholar]
- Kohlhauser, M.; Luze, H.; Nischwitz, S.P.; Kamolz, L.-P. Challenges in Burn Care during the COVID-19 Pandemic—A Scoping Review. J. Clin. Med. 2022, 11, 3410. [Google Scholar] [CrossRef]
- Tatar, R.; Enescu, D.M. The impact of COVID-19 pandemic on the activity of a pediatric burn center in Bucharest, Romania. Burns. 2020, 46, 1977–1978. [Google Scholar] [CrossRef] [PubMed]
- Diab, J.; Pye, M.; Diab, V.; Hopkins, Z.; Cha, J.; Maitz, P.K.; Issler-Fisher, A.C. The impact of COVID-19 on adult burns: A statewide review of epidemiology and clinical outcomes. Burns 2024, 50, 381–387. [Google Scholar] [CrossRef]
- Rogers, A.D.; Cartotto, R. The Impact of COVID-19 on Burn Care at a Major Regional Burn Center. J. Burn Care Res. 2021, 42, 110–111. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Shi, K.; Zhang, N.; Chen, X.; Yu, J. The changing pattern of pediatric burns in a territory burn center before and during the COVID-19 pandemic in China: A retrospective study. J. Tissue Viability 2024, 33, 185–189. [Google Scholar] [CrossRef]
- Demircan, M. Increased admissions and hospitalizations to pediatric burn center during COVID 19 pandemic. Burns 2021, 47, 487–488. [Google Scholar] [CrossRef] [PubMed]
- Lancien, U.; Voisin, A.; Faraj, S.; Duteille, F.; Perrot, P. Impact of the 2020 French lockdown due to the SARS-CoV-2 pandemic on emergency consultations for pediatric burns in a regional referral hospital. Ann. Chir. Plast. Esthet. 2022, 67, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Chakera, H.; Zuccaro, J.; Gus, E.; Kelly, C.; Fish, J.S. Investigating the impact of COVID-19 on the provision of pediatric burn care. Burns 2024, 50, 388–394. [Google Scholar] [CrossRef]
- Bressan, S.; Gallo, E.; Tirelli, F.; Gregori, D.; Da Dalt, L. Lockdown: More domestic accidents than COVID-19 in children. Arch. Dis. Child. 2021, 106, e3. [Google Scholar] [CrossRef]
- Sethuraman, U.; Stankovic, C.; Singer, A.; Vitale, L.; Krouse, C.B.; Cloutier, D.; Donoghue, L.; Klein, J.; Kannikeswaran, N. Burn visits to a pediatric burn center during the COVID-19 pandemic and ‘Stay at home’ period. Burns 2021, 47, 491–492. [Google Scholar] [CrossRef]
- Binet, A.; Tartrou, H.; Bousquet, M.; Touze, A.L. No lockdown for pediatric burns. Arch. Pediatr. 2024, 31, 44–47. [Google Scholar] [CrossRef] [PubMed]
- Peck, M.D.; Toppi, J.T. Epidemiology and Prevention of Burns Throughout the World. In Handbook of Burns, 2nd ed.; Jeschke, M., Kamolz, L.P., Sjöberg, F., Wolf, S., Eds.; Springer: Cham, Switzerland, 2020; Volume 1, pp. 17–57. [Google Scholar]
- Koç, Z.; Sağlam, Z. Burn epidemiology and cost of medication in paediatric burn patients. Burns 2012, 38, 813–819. [Google Scholar] [CrossRef]
- Saeman, M.R.; Hodgman, E.I.; Burris, A.; Wolf, S.E.; Arnoldo, B.D.; Kowalske, K.J.; Phelan, H.A. Epidemiology and outcomes of pediatric burns over 35 years at Parkland Hospital. Burns. 2016, 42, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Jordan, K.C.; Di Gennaro, J.L.; von Saint André-von Arnim, A.; Stewart, B.T. Global trends in pediatric burn injuries and care capacity from the World Health Organization Global Burn Registry. Front. Pediatr. 2022, 10, 954995. [Google Scholar] [CrossRef]
- Nassar, J.Y.; Al Qurashi, A.A.; Albalawi, I.A.; Nukaly, H.Y.; Halawani, I.R.; Abumelha, A.F.; Osama Al Dwehji, A.M.; Alhartani, M.M.; Asaad, A.; Alnajashi, A.; et al. Pediatric Burns: A Systematic Review and Meta-Analysis on Epidemiology, Gender Distribution, Risk Factors, Management, and Outcomes in Emergency Departments. Cureus 2023, 15, e49012. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, M.; Wheeler, K.K.; Shi, J.; Thakkar, R.K.; Fabia, R.B.; Groner, J.I.; Noffsinger, D.; Giles, S.A.; Xiang, H. Epidemiology and trend of US pediatric burn hospitalizations, 2003–2016. Burns 2021, 47, 551–559. [Google Scholar] [CrossRef]
- Vasudevan, A.; Bailey, H.M.; Sager, A.; Kazis, L.E. Impact of the Early COVID-19 Pandemic on Burn Care: A Multi-National Study. J. Burn Care Res. 2023, 44, 580–589. [Google Scholar] [CrossRef]
- Tracy, L.M.; Lo, C.H.; Cleland, H.J.; Teague, W.J.; Gabbe, B.J. Early Impact of COVID-19 Pandemic on Burn Injuries, Admissions, and Care in a Statewide Burn Service. Eur. Burn J. 2022, 3, 447–456. [Google Scholar] [CrossRef]
- Mathias, E.; Srinivas Murthy, M. Pediatric Thermal Burns and Treatment: A Review of Progress and Future Prospects. Medicines 2017, 4, 91. [Google Scholar] [CrossRef]
- García-Díaz, A.; Gacto-Sánchez, P.; Durán-Romero, A.J.; Carrasco-García, S.; Ruiz-Moya, A.; Molina-Morales, J.; Sánchez-Tatay, M.-V.; Gómez-Cía, T.; Pereyra-Rodríguez, J.-J. Pediatric major burns: A monocentric retrospective review of etiology and outcomes (2008–2020). Eur. J. Plast. Surg. 2022, 45, 967–975. [Google Scholar] [CrossRef]
- Georgeades, C.M.; Collings, A.T.; Farazi, M.; Fallat, M.E.; Minneci, P.C.; Sato, T.T.; Speck, K.E.; Van Arendonk, K.; Deans, K.J.; Falcone, R.A.; et al. A Multi-institutional Study Evaluating Pediatric Burn Injuries During the COVID-19 Pandemic. J. Burn Care Res. 2023, 44, 399–407. [Google Scholar] [CrossRef]
- Braithwaite, J. Quality of care in the COVID-19 era: A global perspective. IJQHC Commun. 2021, 1, lyab003. [Google Scholar] [CrossRef]
- Corral-Gudino, L. Tools to Reduce Low-Value Care: Lessons From COVID-19 Pandemic Comment on “Key Factors that Promote Low-Value Care: Views of Experts from the United States, Canada, and the Netherlands”. Int. J. Health Policy Manag. 2022, 11, 1967–1970. [Google Scholar] [CrossRef]
- Tuczyńska, M.; Staszewski, R.; Matthews-Kozanecka, M.; Żok, A.; Baum, E. Quality of the Healthcare Services During COVID-19 Pandemic in Selected European Countries. Front. Public Health 2022, 10, 870314. [Google Scholar] [CrossRef]
- Kamolz, L.P.; Schiefer, J.L.; Horter, J.; Plock, J.A. COVID-19 and burns: Lessons learned? Burns 2020, 46, 1467–1468. [Google Scholar] [CrossRef] [PubMed]
- McGowan, R.J.; Ang, J.Y. Coronavirus Disease 2019 (COVID-19) in Children, Updated: 6 March 2024. Available online: https://emedicine.medscape.com/article/2500132-overview (accessed on 15 January 2025).
- Vivisenco, I.C.; Lescaie, A.; Dragomirescu, A.; Ioniță, I.C.; Florescu, I.; Ciocea, B.; Grama, A.R.; Crăciun, M.-D.; Chivu, C.-D.; Ulmeanu, C.E.; et al. Neurological Manifestations of Acute SARS-CoV-2 Infection in Pediatric Patients: A 3-Year Study on Differences between Pandemic Waves. Viruses 2024, 16, 967. [Google Scholar] [CrossRef] [PubMed]
- Hesamirostami, M.; Nazarian, R.; Asghari, H.; Jafarirad, A.; Khosravi, A.; Nouranibaladezaei, S.; Radfar, A. A case series of concomitant burn and COVID-19. Burns Open 2021, 5, 34–38. [Google Scholar] [CrossRef]
- Aggarwal, N.; Srivastava, R.K. Impact of COVID-19 on Patient Trends and Outcome: Results from a Tertiary Care Burn and Plastic Unit in Northern India. Indian J. Plast. Surg. 2021, 54, 172–176. [Google Scholar] [CrossRef]
| Variable | Admitted in 2019 (n = 412) | Admitted in 2020 (n = 264) | p-Value | |
|---|---|---|---|---|
| Sex distribution: | ||||
| Males, n (%) | 267 (64.8) | 159 (60.2) | 0.29 | |
| Females, n (%) | 145 (35.2) | 105 (39.8) | ||
| Age distribution: | ||||
| Median age, years (IQR) | 2.5 (1.33–8) | 2.29 (1.48–7) | 0.64 | |
| <1 year, n (%) | 34 (8.3%) | 19 (7.2%) | 0.79 | |
| 1–4 years, n (%) | 237 (57.5%) | 159 (60.2%) | ||
| 5–9 years, n (%) | 61 (14.8%) | 41 (15.5%) | ||
| 10–14 years, n (%) | 49 (11.9%) | 31 (11.7%) | ||
| 15–18 years, n (%) | 31 (7.5%) | 14 (5.3%) | ||
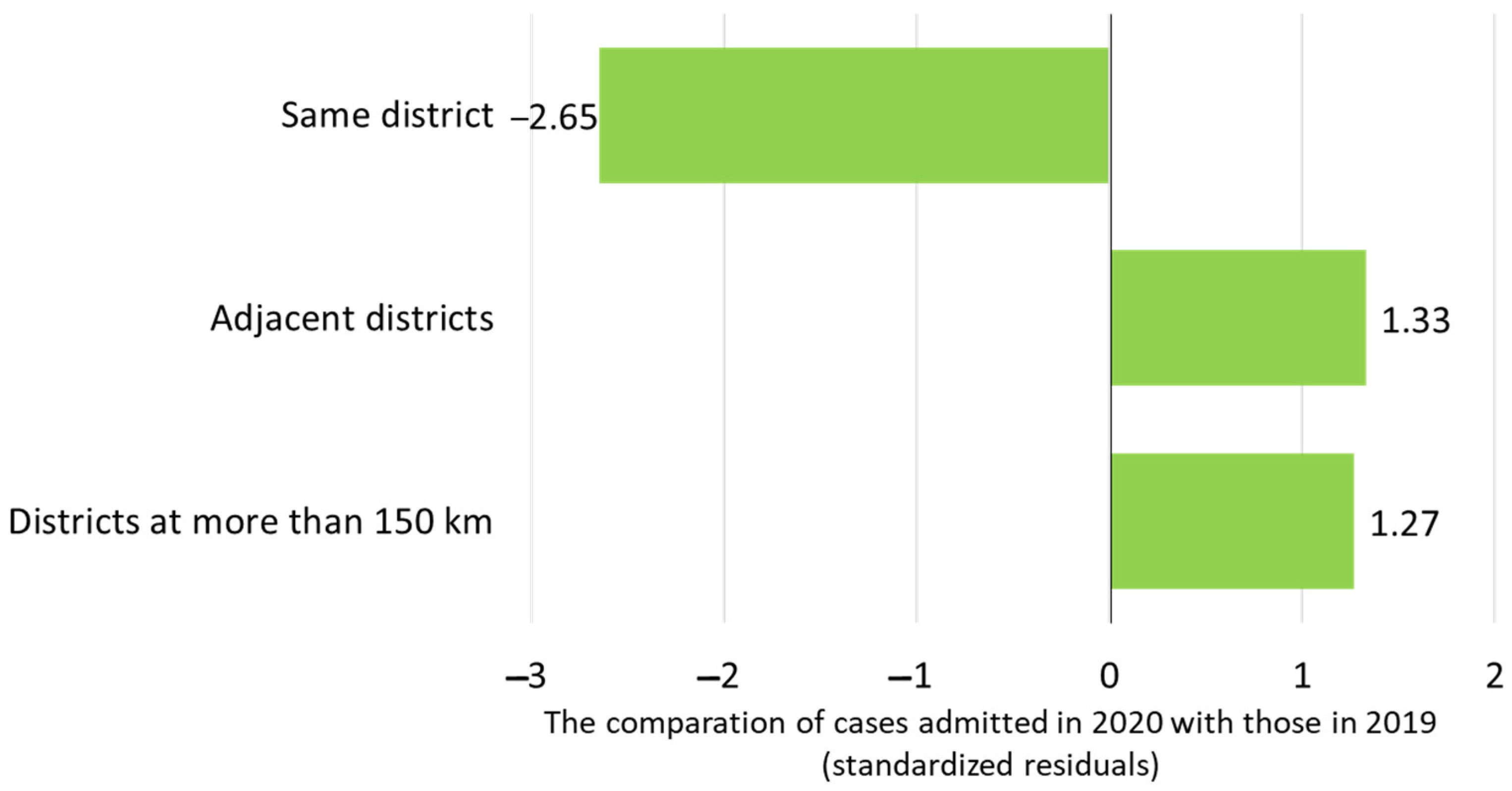
| Residential area distribution: | ||||
| Urban, n (%) | 203 (49.3) | 115 (43.6) | 0.17 | |
| Rural, n (%) | 209 (50.7) | 149 (56.4) | ||
| Residential location of patients relative to the burn center: | ||||
| Same district, n (%) | 158 (38.3%) | 61 (23.1%) | 0.002 | |
| Adjacent districts, n (%) | 148 (35.9%) | 117 (44.3%) | ||
| Districts at more than 150 km, n (%) | 106 (25.7%) | 86 (32.6%) | ||
| Time from burn injury to admission: | ||||
| Median time, hours (IQR) | 5 (2–24) | 5 (3–18) | 0.51 | |
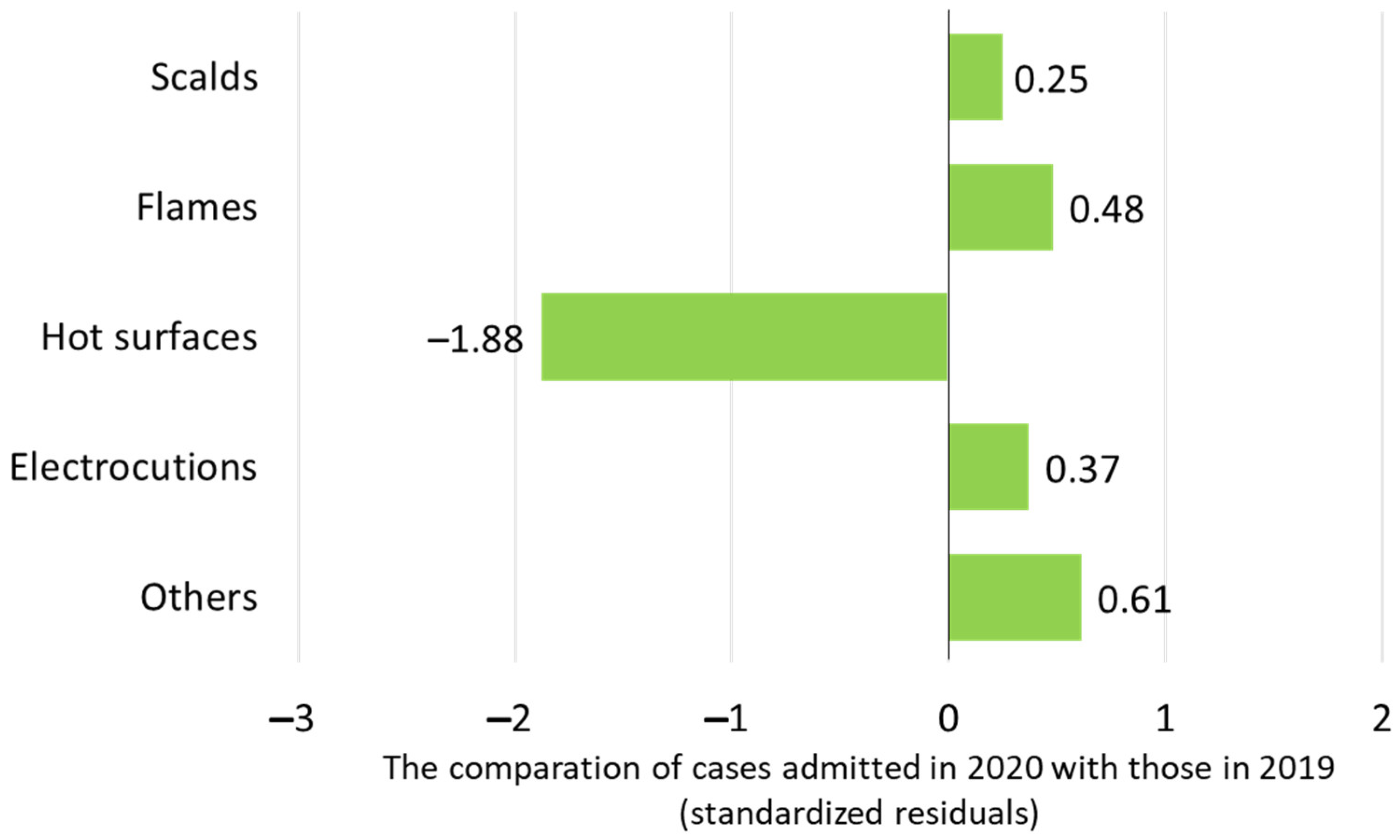
| Etiological agents: | ||||
| Scalds, n (%) | 277 (67.2%) | 183 (69.3%) | 0.13 | |
| Flames, n (%) | 74 (18.0%) | 53 (20.1%) | ||
| Hot surfaces, n (%) | 45 (10.9%) | 14 (5.3%) | ||
| Electrocutions, n (%) | 10 (2.4%) | 8 (3.0%) | ||
| Other—sun, n (%) | 3 (0.7%) | 5 (1.9%) | ||
| Other—chemicals, n (%) | 3 (0.7%) | 1 (0.4%) | ||
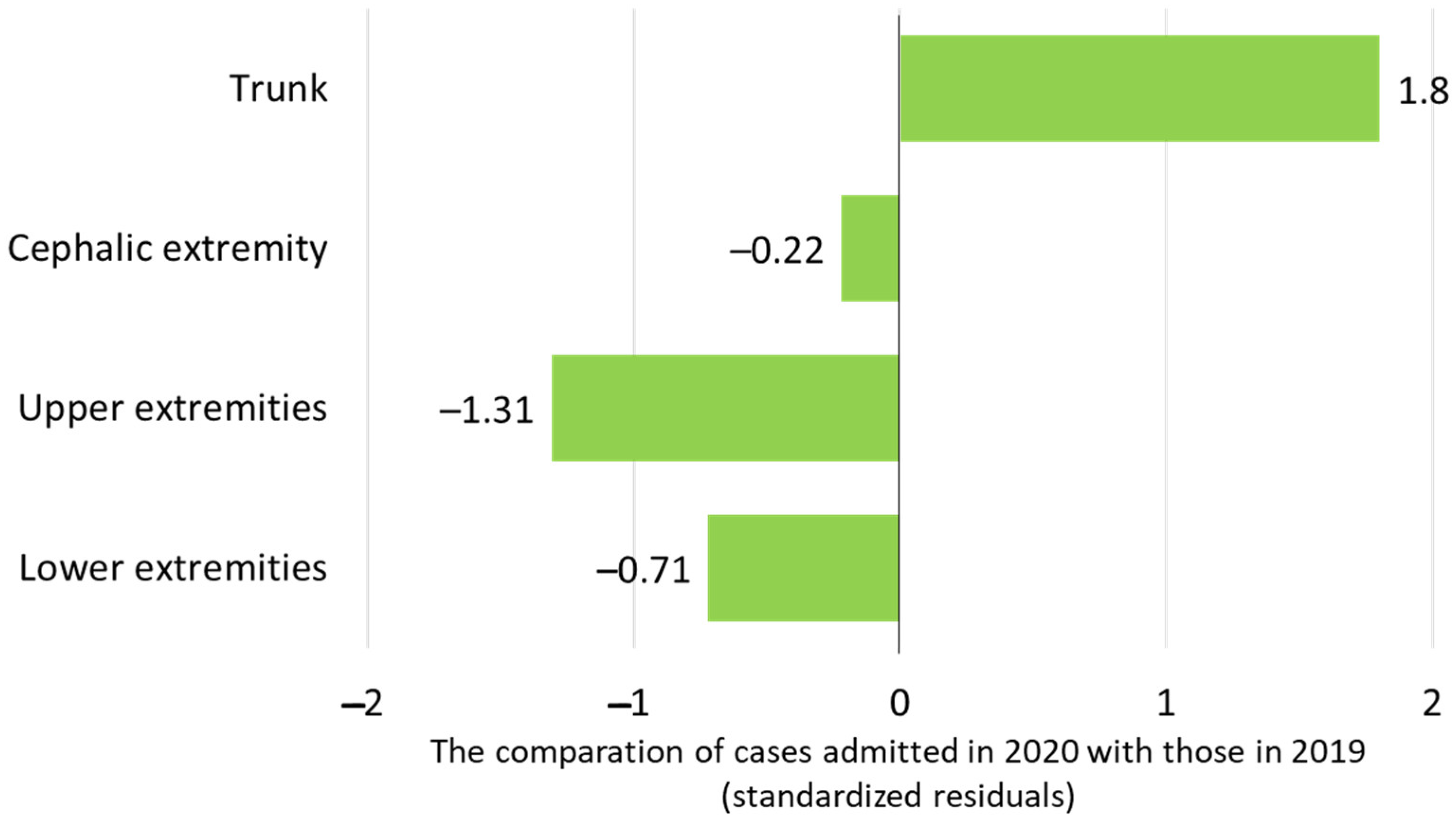
| Type of involved body regions: | ||||
| Trunk, n (%) | 199 (48.3%) | 165 (62.5%) | 0.027 | |
| Cephalic extremity, n (%) | 73 (17.7%) | 50 (18.9%) | ||
| Upper extremities, n (%) | 225 (4.6%) | 121 (5.8%) | ||
| Lower extremities, n (%) | 189 (45.9%) | 110 (41.7%) | ||
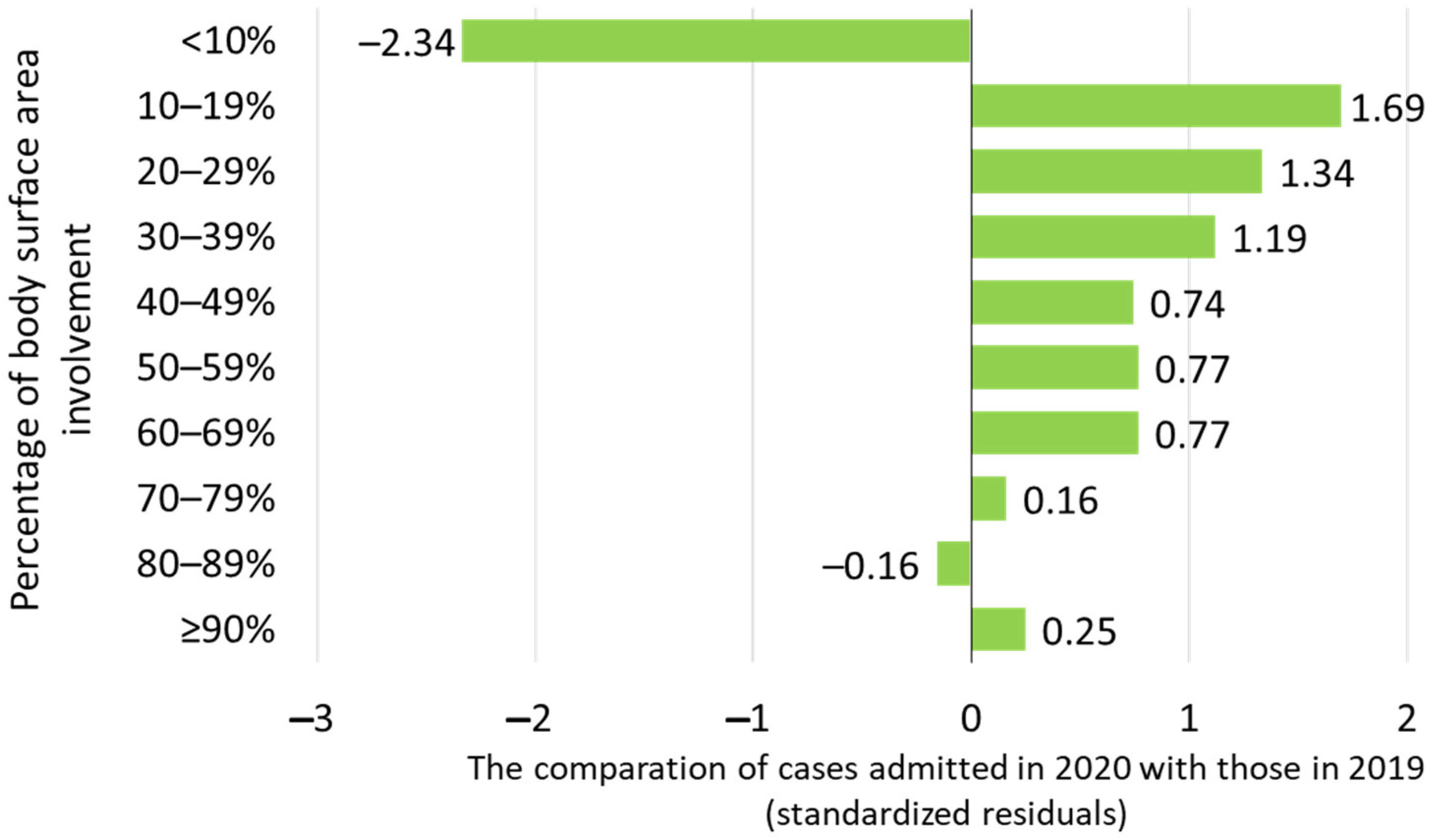
| Percentage of body surface area involvement: | ||||
| Median percentage, % (IQR) | 6 (4–12) | 10 (5–20) | 0.0004 | |
| Intensive Care Unit admission: | ||||
| Number of patients (%) | 22 (5.3%) | 24 (9.1%) | 0.08 | |
| Median time, days (IQR) | 4 (2–5) | 3 (1–5.75) | 0.72 | |
| Management type: | ||||
| Surgical | 74 (18.0%) | 64 (39.0%) | 0.048 | |
| Conservative | 338 (82.0%) | 200 (61.0%) | ||
| Overall hospitalization time: | ||||
| Median time, days (IQR) | 7 (2–14) | 11 (6–18) | 0.0003 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tatar, R.; Enescu, D.M.; Nacea, D.I.; Nițescu, G.V.; Lescaie, A.; Pertea, M.; Mitrache, P.; Diaconu, L.S. The Effects of the COVID-19 Pandemic on Trends and Types of Pediatric Burn Injuries: Lessons from a National Burn Center and the Role of Strategic Resource Allocation. Life 2025, 15, 544. https://doi.org/10.3390/life15040544
Tatar R, Enescu DM, Nacea DI, Nițescu GV, Lescaie A, Pertea M, Mitrache P, Diaconu LS. The Effects of the COVID-19 Pandemic on Trends and Types of Pediatric Burn Injuries: Lessons from a National Burn Center and the Role of Strategic Resource Allocation. Life. 2025; 15(4):544. https://doi.org/10.3390/life15040544
Chicago/Turabian StyleTatar, Raluca, Dan Mircea Enescu, Doina Iulia Nacea, Gabriela Viorela Nițescu, Andreea Lescaie, Mihaela Pertea, Petruța Mitrache, and Laura Sorina Diaconu. 2025. "The Effects of the COVID-19 Pandemic on Trends and Types of Pediatric Burn Injuries: Lessons from a National Burn Center and the Role of Strategic Resource Allocation" Life 15, no. 4: 544. https://doi.org/10.3390/life15040544
APA StyleTatar, R., Enescu, D. M., Nacea, D. I., Nițescu, G. V., Lescaie, A., Pertea, M., Mitrache, P., & Diaconu, L. S. (2025). The Effects of the COVID-19 Pandemic on Trends and Types of Pediatric Burn Injuries: Lessons from a National Burn Center and the Role of Strategic Resource Allocation. Life, 15(4), 544. https://doi.org/10.3390/life15040544







