Functional and Clinical Outcomes in Acute Wound Management: Measuring the Impact of Negative Pressure Wound Therapy and Specialized Physical Therapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Inclusion and Exclusion Criteria
2.3. Data Collection and Questionnaires
2.4. Statistical Analysis
3. Results
3.1. Patient Demographics
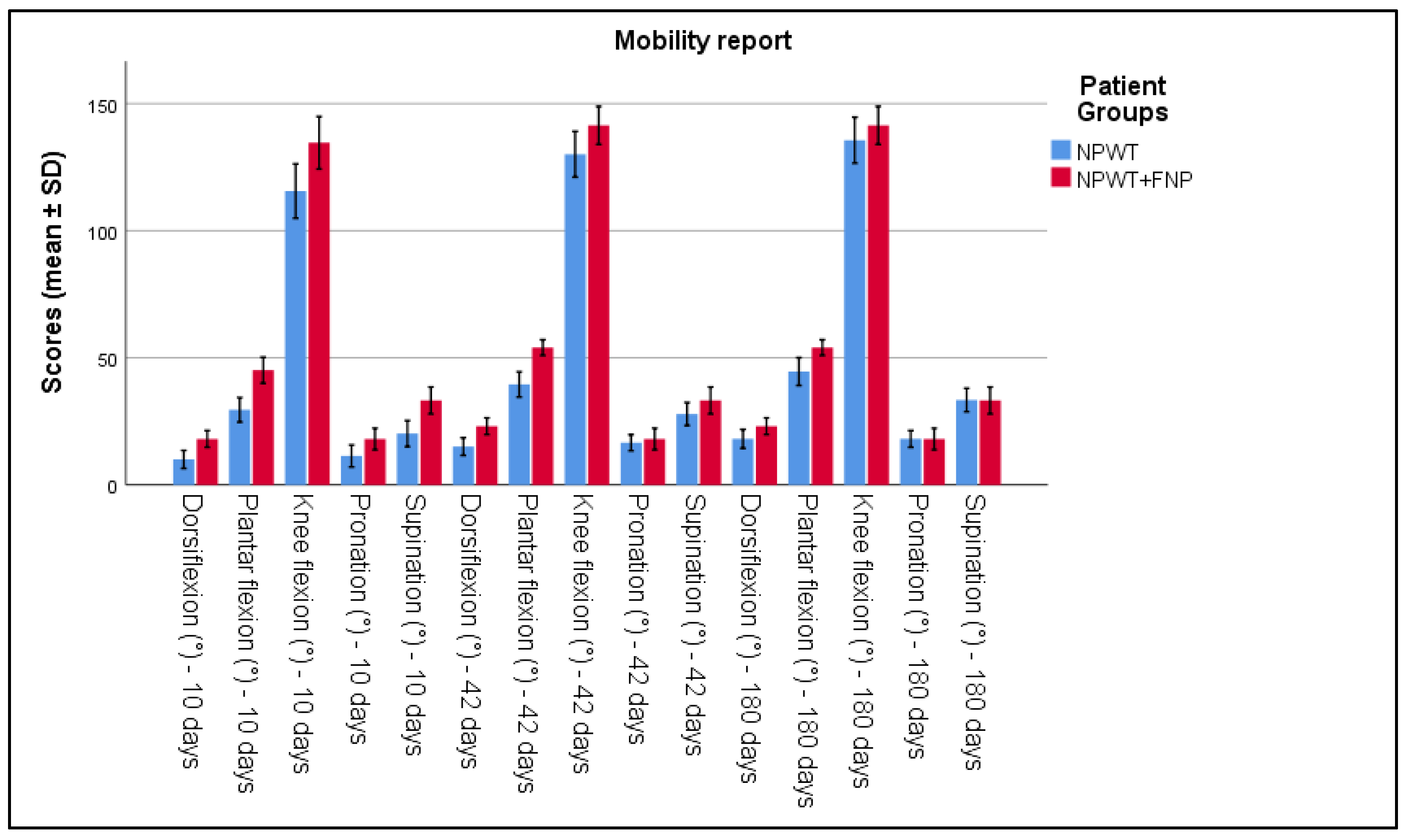
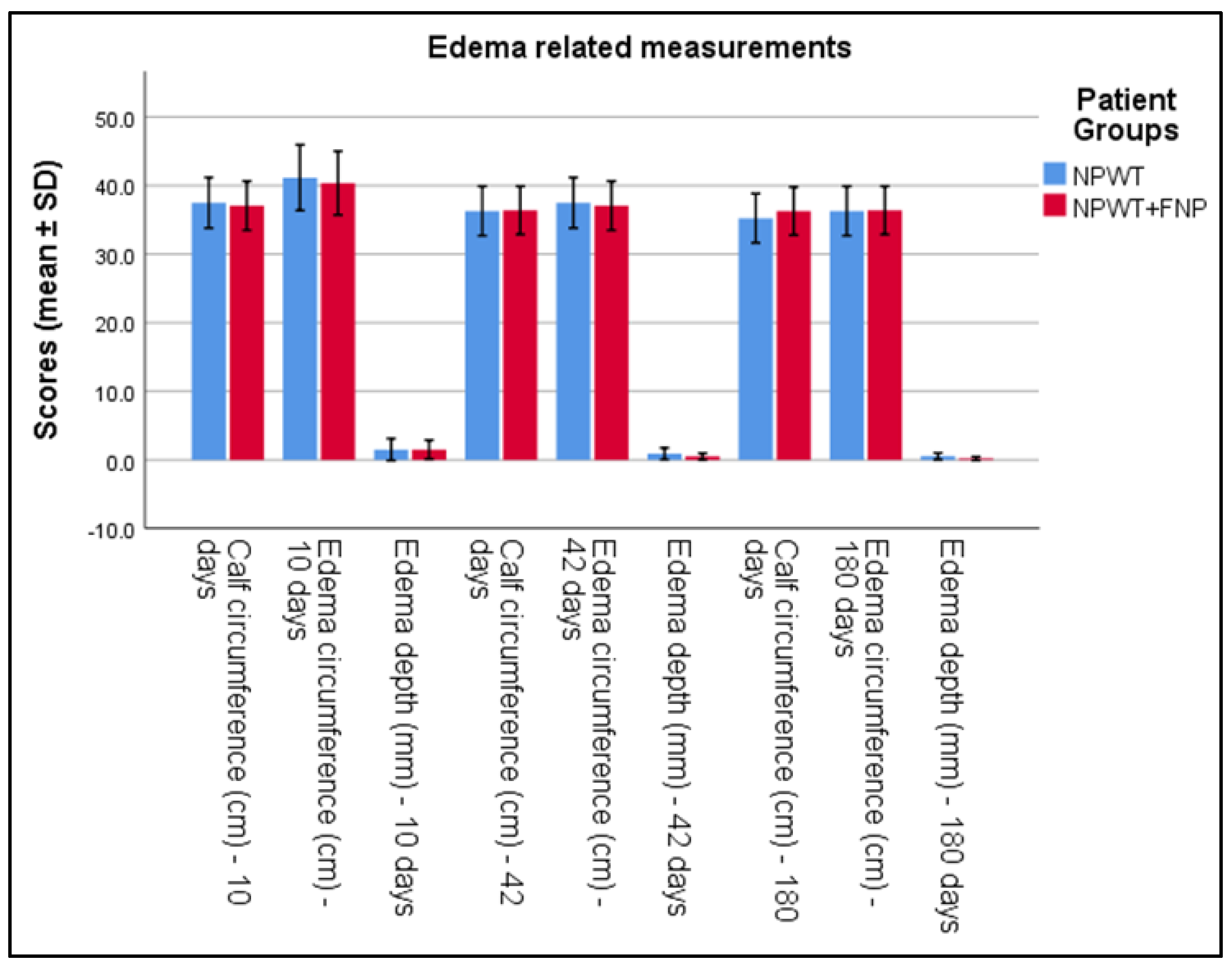
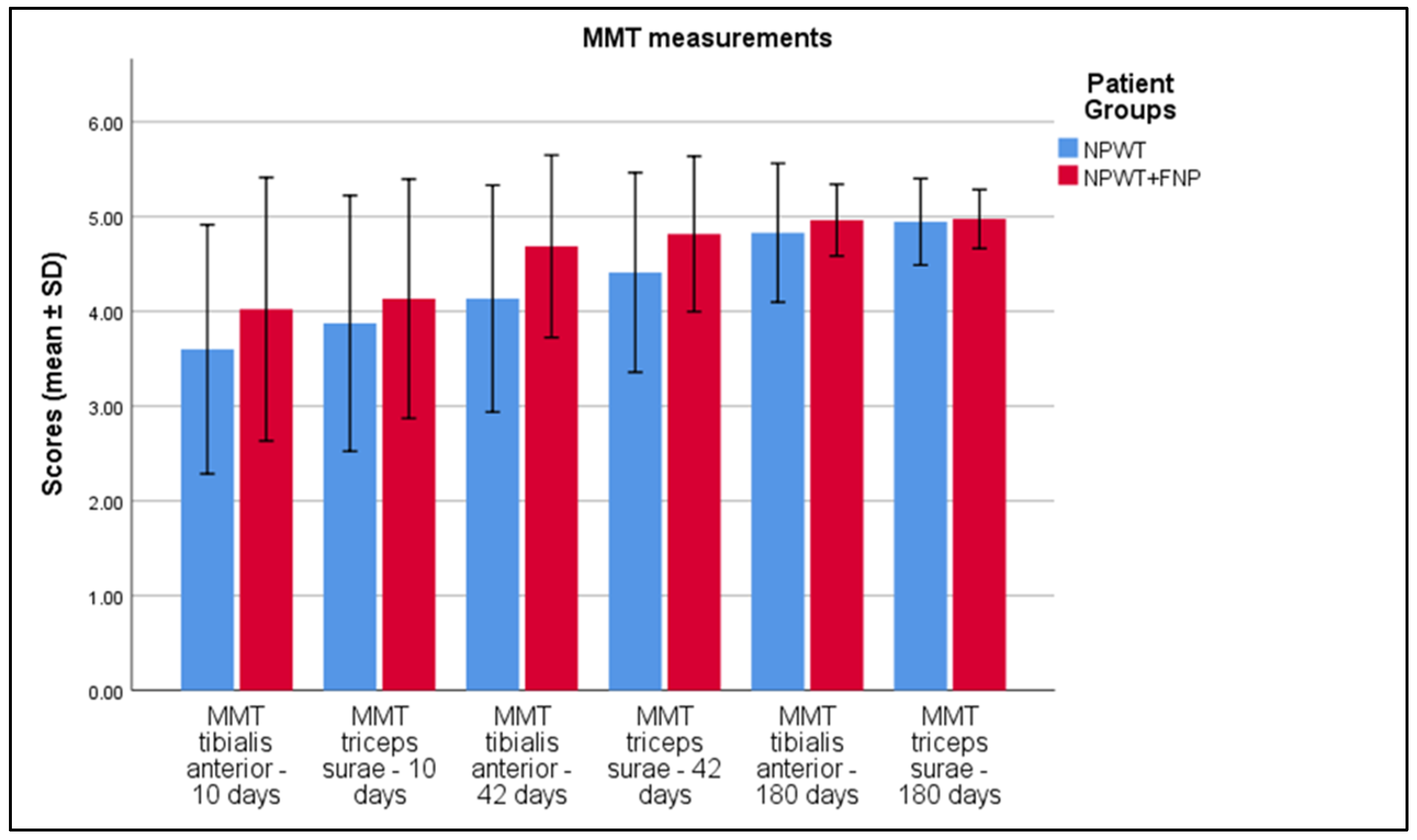
3.2. Evolution of Functional Parameters
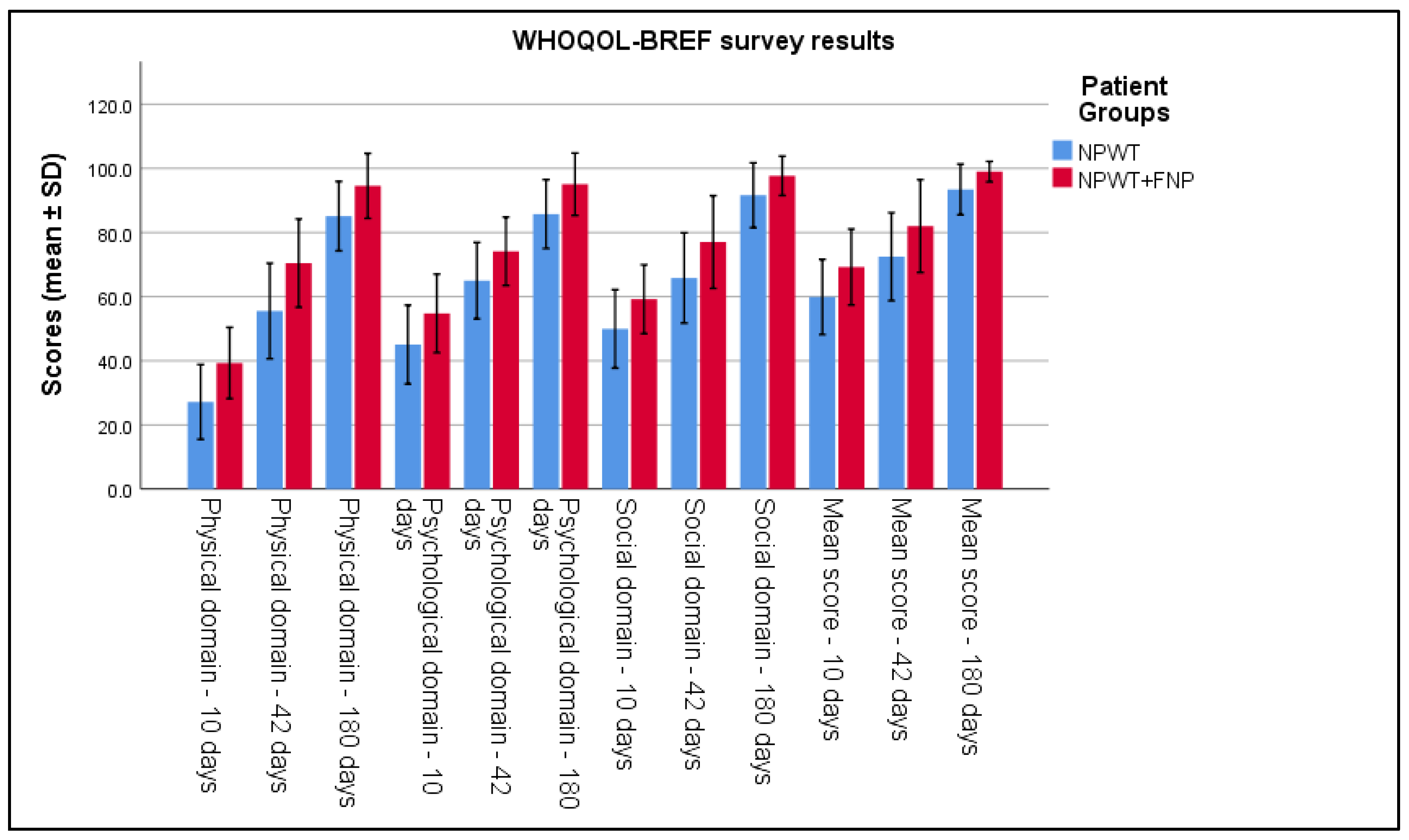
3.3. Analysis of Quality of Life Questionnaires and Functional Parameters
4. Discussion
4.1. Analysis of Literature
4.2. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Orgill, D.P.; Bayer, L.R. Update on negative pressure wound therapy. Clin. Plast. Surg. 2012, 39, 569–585. [Google Scholar] [CrossRef] [PubMed]
- Kisner, C.; Colby, L.A. Therapeutic Exercise: Foundations and Techniques, 6th ed.; F.A. Davis Company: Philadelphia, PA, USA, 2012. [Google Scholar]
- Teixeira, A.L.; Campos, A.C.L. Use of negative-pressure therapy in wound healing. Rev. Col. Bras. Cir. 2013, 40, 178–182. [Google Scholar]
- Argenta, L.C.; Morykwas, M.J. Vacuum-assisted closure: A new method for wound control and treatment. Ann. Plast. Surg. 1997, 38, 563–577. [Google Scholar] [PubMed]
- Krug, E.; Berg, L.; Lee, C.; Hudson, D.; Birke-Sorensen, H.; Depoorter, M.; Dunn, R.; Jeffery, S.; Duteille, F.; Bruhin, A.; et al. Evidence-based recommendations for the use of negative pressure wound therapy in traumatic wounds and reconstructive surgery: Steps towards an international consensus. Injury 2011, 42 (Suppl. S1), S1–S12. [Google Scholar]
- Liu, C.; Xie, H.; Wei, P.; Gong, T.; Wu, G.; Xu, Z.; Chen, S. Clinical study of early rehabilitation training combined with negative pressure wound therapy for the treatment of deep partial-thickness hand burns. Front. Surg. 2023, 10, 1040407. [Google Scholar] [CrossRef]
- Stannard, J.P.; Volgas, D.A.; Stewart, R.; McGwin, G., Jr.; Alonso, J.E. Negative pressure wound therapy after severe open fractures: A prospective randomized study. J. Orthop. Trauma 2009, 23, 552–557. [Google Scholar]
- World Health Organization. International Classification of Diseases (ICD-10); WHO: Geneva, Switzerland, 1992. [Google Scholar]
- Leduc, O.; Leduc, A.; Bourgeois, P.; Belgrado, J.P. The physical treatment of upper limb edema. Cancer 1998, 83 (Suppl. S12), 2835–2839. [Google Scholar]
- World Health Organization. WHOQOL-BREF: Introduction, Administration, Scoring and Generic Version of the Assessment; WHO: Geneva, Switzerland, 1996. [Google Scholar]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar]
- Altman, D.G.; Bland, J.M. Standard deviations and standard errors. BMJ 2005, 331, 903. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 5th ed.; Sage Publications: London, UK, 2017. [Google Scholar]
- Zhang, Z.; Weng, Y.; Cao, W.; Ge, Z. The combined use of negative-pressure wound therapy and dermal substitutes for tissue repair: A comprehensive review. Int. J. Low Extrem. Wounds 2020, 19, 366–374. [Google Scholar]
- Dumville, J.C.; Owens, G.L.; Crosbie, E.J.; Peinemann, F.; Liu, Z. Negative pressure wound therapy for treating surgical wounds healing by secondary intention. Cochrane Database Syst. Rev. 2015, 6, CD011278. [Google Scholar] [CrossRef] [PubMed]
- Goss, S.G.; Schwartz, J.A.; Facchin, F.; Avdagic, E.; Gendics, C.; Lantis, J.C., 2nd. Negative pressure wound therapy with instillation (NPWTi) better reduces post-debridement bioburden in chronically infected wounds than NPWT alone. J. Am. Coll. Clin. Wound Spec. 2014, 4, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Morykwas, M.J.; Argenta, L.C.; Shelton-Brown, E.I.; McGuirt, W. Vacuum-assisted closure: Animal studies and basic foundation. Ann. Plast. Surg. 1997, 38, 553–562. [Google Scholar] [CrossRef] [PubMed]
- Shan, G.; Wang, W. Advanced statistical methods and designs for clinical trials for COVID-19. Int. J. Antimicrob. Agents 2021, 57, 106167. [Google Scholar] [CrossRef]
- Dumville, J.C.; Munson, C.; Christie, J. Negative pressure wound therapy for partial-thickness burns. Cochrane Database Syst. Rev. 2014, 2014, CD006215. [Google Scholar] [CrossRef]
- Zhu, X.; Olsson, M.M.; Bajpai, R.; Järbrink, K.; Tang, W.E.; Car, J. Health-Related Quality of Life and Chronic Wound Characteristics among Patients with Chronic Wounds Treated in Primary Care: A Cross-Sectional Study in Singapore. Int. Wound J. 2022, 19, 1121–1132. [Google Scholar] [CrossRef]
- Peters, M.L.; Sommer, M.; van Kleef, M. Predictors of physical and emotional recovery in patients undergoing surgery: A systematic review. Psychol. Med. 2010, 40, 187–200. [Google Scholar]
- Zens, Y.; Barth, M.; Bucher, H.C.; Dreck, K.; Felsch, M.; Groß, W.; Jaschinski, T.; Kölsch, H.; Kromp, M.; Overesch, I.; et al. Negative pressure wound therapy in patients with wounds healing by secondary intention: A systematic review and meta-analysis of randomised controlled trials. Syst. Rev. 2020, 9, 238. [Google Scholar] [CrossRef]
- Zhao, J.; Shi, K.; Zhang, N.; Hong, L.; Yu, J. Assessment between antiseptic and normal saline for negative pressure wound therapy with instillation and dwell time in diabetic foot infections. Sci. Rep. 2024, 14, 11423. [Google Scholar] [CrossRef]
- Webster, J.; Scuffham, P.; Sherriff, K.L.; Stankiewicz, M.; Chaboyer, W.P. Negative pressure wound therapy for skin grafts and surgical wounds healing by primary intention. Cochrane Database Syst. Rev. 2012, 4, CD009261, Update in: Cochrane Database Syst. Rev. 2014, 10, CD009261. https://doi.org/10.1002/14651858.CD009261.pub3. [Google Scholar] [CrossRef] [PubMed]
- Norman, G.; Shi, C.; Goh, E.L.; Murphy, E.M.; Reid, A.; Chiverton, L.; Stankiewicz, M.; Dumville, J.C. Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database Syst. Rev. 2022, 4, CD009261. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Characteristics | NPWT (n = 110) | NPWT+FNP (n = 82) | p-Value | Cohen’s d |
|---|---|---|---|---|
| Age, years | 37.86 ± 4.53 | 36.54 ± 5.50 | 0.069 | 0.28 |
| Sex, men (%) | 58 (52.7%) | 47 (57.3%) | 0.063 | |
| Overweight (>25.0 kg/m2) | 51 (46.36%) | 54 (56.84%) | 0.103 | |
| Smoking | 43 (39.1%) | 31 (37.8%) | 0.717 | |
| CCI > 2 | 2 (1.81%) | 2 (2.4%) | 0.554 | |
| Wound type | 0.688 | |||
| 41 (37.3%) | 27 (32.9%) | ||
| 47 (42.7%) | 41 (50%) | ||
| 22 (20%) | 14 (17.1%) |
| Variables | NPWT (n = 110) | NPWT+FNP (n = 82) | p-Value | Cohen’s d |
|---|---|---|---|---|
| Dorsiflexion (°)—10 days | 10.05 ± 1.76 | 18.10 ± 1.63 | <0.001 | 4.65 |
| Plantar flexion (°)—10 days | 29.58 ± 2.42 | 45.13 ± 2.56 | <0.001 | 5.98 |
| Knee flexion (°)—10 days | 115.57 ± 5.32 | 134.58 ± 5.15 | <0.001 | 3.50 |
| Pronation (°)—10 days | 11.40 ± 2.16 | 18.06 ± 2.12 | <0.001 | 3.10 |
| Supination (°)—10 days | 20.22 ± 2.56 | 33.24 ± 2.65 | <0.001 | 4.90 |
| Dorsiflexion (°)—42 days | 15.12 ± 1.73 | 23.10 ± 1.64 | <0.001 | 4.75 |
| Plantar flexion (°)—42 days | 35.56 ± 2.48 | 54.05 ± 1.54 | <0.001 | 6.73 |
| Knee flexion (°)—42 days | 130.01 ± 4.49 | 141.42 ± 3.74 | <0.001 | 2.68 |
| Pronation (°)—42 days | 16.61 ± 1.59 | 18.06 ± 2.12 | 0.001 | 0.74 |
| Supination (°)—42 days | 27.90 ± 2.25 | 33.24 ± 2.65 | 0.980 | 0.01 |
| Dorsiflexion (°)—180 days | 18.15 ± 1.86 | 23.10 ± 1.64 | <0.001 | 2.75 |
| Plantar flexion (°)—180 days | 44.60 ± 2.73 | 54.05 ± 1.54 | <0.001 | 4.20 |
| Knee flexion (°)—180 days | 135.59 ± 4.52 | 141.42 ± 3.74 | <0.001 | 1.40 |
| Pronation (°)—180 days | 18.11 ± 1.63 | 18.06 ± 2.12 | 0.838 | 0.03 |
| Supination (°)—180 days | 33.42 ± 2.31 | 33.24 ± 2.65 | 0.618 | 0.07 |
| Variables | NPWT (n = 110) | NPWT+FNP (n = 82) | p-Value | Cohen’s d |
|---|---|---|---|---|
| Calf circumference (cm)—10 days | 37.48 ± 1.84 | 37.06 ± 1.79 | 0.115 | 0.23 |
| Edema circumference (cm)—10 days | 41.15 ± 2.39 | 40.36 ± 2.32 | 0.023 | 0.33 |
| Edema depth (mm)—10 days | 1.49 ± 0.8 | 1.50 ± 0.69 | 0.957 | 0.01 |
| Calf circumference (cm)—42 days | 36.28 ± 1.8 | 36.39 ± 1.75 | 0.695 | 0.06 |
| Edema circumference (cm)—42 days | 37.49 ± 1.84 | 37.06 ± 1.80 | 0.115 | 0.23 |
| Edema depth (mm)—42 days | 0.9 ± 0.042 | 0.50 ± 0.23 | <0.001 | 1.21 |
| Calf circumference (cm)—180 days | 35.23 ± 1.79 | 36.28 ± 1.76 | <0.001 | 0.59 |
| Edema circumference (cm)—180 days | 36.29 ± 1.8 | 36.39 ± 1.75 | 0.695 | 0.06 |
| Edema depth (mm)—180 days | 0.53 ± 0.24 | 0.19 ± 0.14 | <0.001 | 1.69 |
| Variables | NPWT (n = 110) | NPWT+FNP (n = 82) | p-Value | Cohen’s d |
|---|---|---|---|---|
| Initial MMT tibialis anterior | 3.27 ± 0.67 | 3.08 ± 0.68 | 0.058 | 0.28 |
| Initial MMT triceps surae | 3.46 ± 0.67 | 3.18 ± 0.64 | 0.004 | 0.43 |
| MMT tibialis anterior—10 days | 3.60 ± 0.66 | 4.02 ± 0.69 | <0.001 | 0.63 |
| MMT triceps surae—10 days | 3.88 ± 0.67 | 4.13± 0.63 | 0.007 | 0.38 |
| MMT tibialis anterior—42 days | 4.14 ± 0.60 | 4.69 ± 0.48 | <0.001 | 1.02 |
| MMT triceps surae—42 days | 4.41 ± 0.53 | 4.82 ± 0.41 | <0.001 | 0.86 |
| MMT tibialis anterior—180 days | 4.83 ± 0.37 | 4.96 ± 0.19 | 0.003 | 0.48 |
| MMT triceps surae—180 days | 4.95 ± 0.23 | 4.98 ± 0.16 | 0.303 | 0.16 |
| Variables | NPWT (n = 110) | NPWT+FNP (n = 82) | p-Value | Cohen’s d |
|---|---|---|---|---|
| Physical domain—10 days | 27.17 ± 5.83 | 39.30 ± 5.56 | <0.001 | 2.15 |
| Physical domain—42 days | 55.52 ± 7.44 | 70.45 ± 6.88 | <0.001 | 2.06 |
| Physical domain—180 days | 85.12 ± 5.41 | 94.53 ± 5.07 | <0.001 | 1.77 |
| Psychological domain—10 days | 45.04 ± 6.14 | 54.78 ± 6.12 | <0.001 | 1.61 |
| Psychological domain—42 days | 64.98 ± 5.96 | 74.13 ± 5.33 | <0.001 | 1.63 |
| Psychological domain—180 days | 85.74 ± 5.37 | 95.06 ± 4.87 | <0.001 | 1.83 |
| Social domain—10 days | 49.93 ± 6.11 | 59.21 ± 5.36 | <0.001 | 1.64 |
| Social domain—42 days | 65.84 ± 7.03 | 77.02 ± 7.22 | <0.001 | 1.59 |
| Social domain—180 days | 91.61 ± 5.05 | 97.66 ± 3.07 | <0.001 | 1.44 |
| Mean score—10 days | 59.89 ± 5.86 | 69.24 ± 5.92 | <0.001 | 1.59 |
| Mean score—42 days | 72.47 ± 6.86 | 82.02 ± 7.23 | <0.001 | 1.37 |
| Mean score—180 days | 93.40 ± 3.95 | 98.99 ± 1.59 | <0.001 | 1.67 |
| Variables | NPWT (n = 110) | NPWT+FNP (n = 82) | p-Value | Cohen’s d |
|---|---|---|---|---|
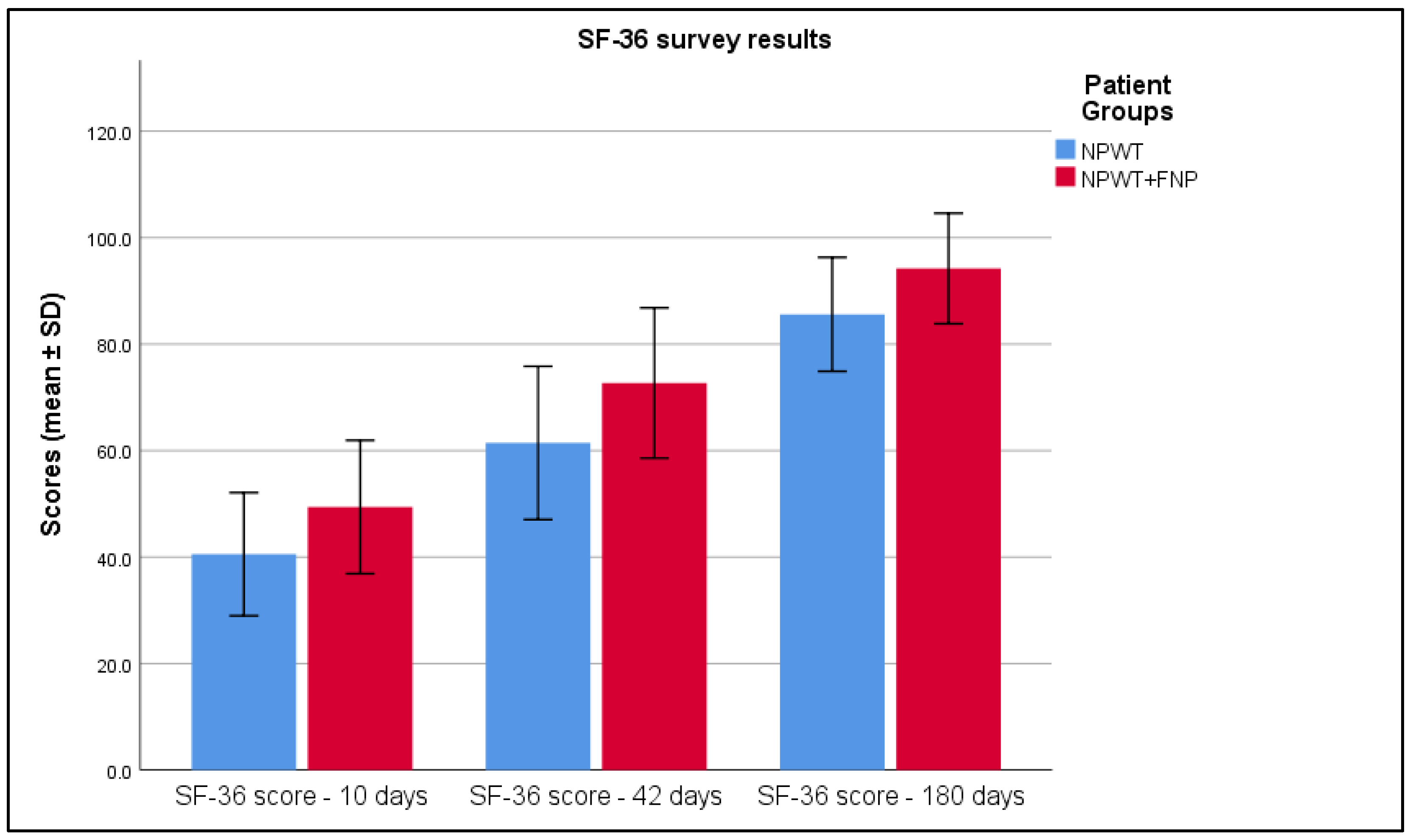
| SF-36 score—10 days | 40.54 ± 5.78 | 49.40 ± 6.26 | <0.001 | 1.51 |
| SF-36 score—42 days | 61.44 ± 7.2 | 72.69 ± 7.06 | <0.001 | 1.59 |
| SF-36 score—180 days | 85.60 ± 5.35 | 94.21 ± 5.19 | <0.001 | 1.77 |
| Variables | NPWT (n = 110) | NPWT+FNP (n = 82) | p-Value | Cohen’s d |
|---|---|---|---|---|
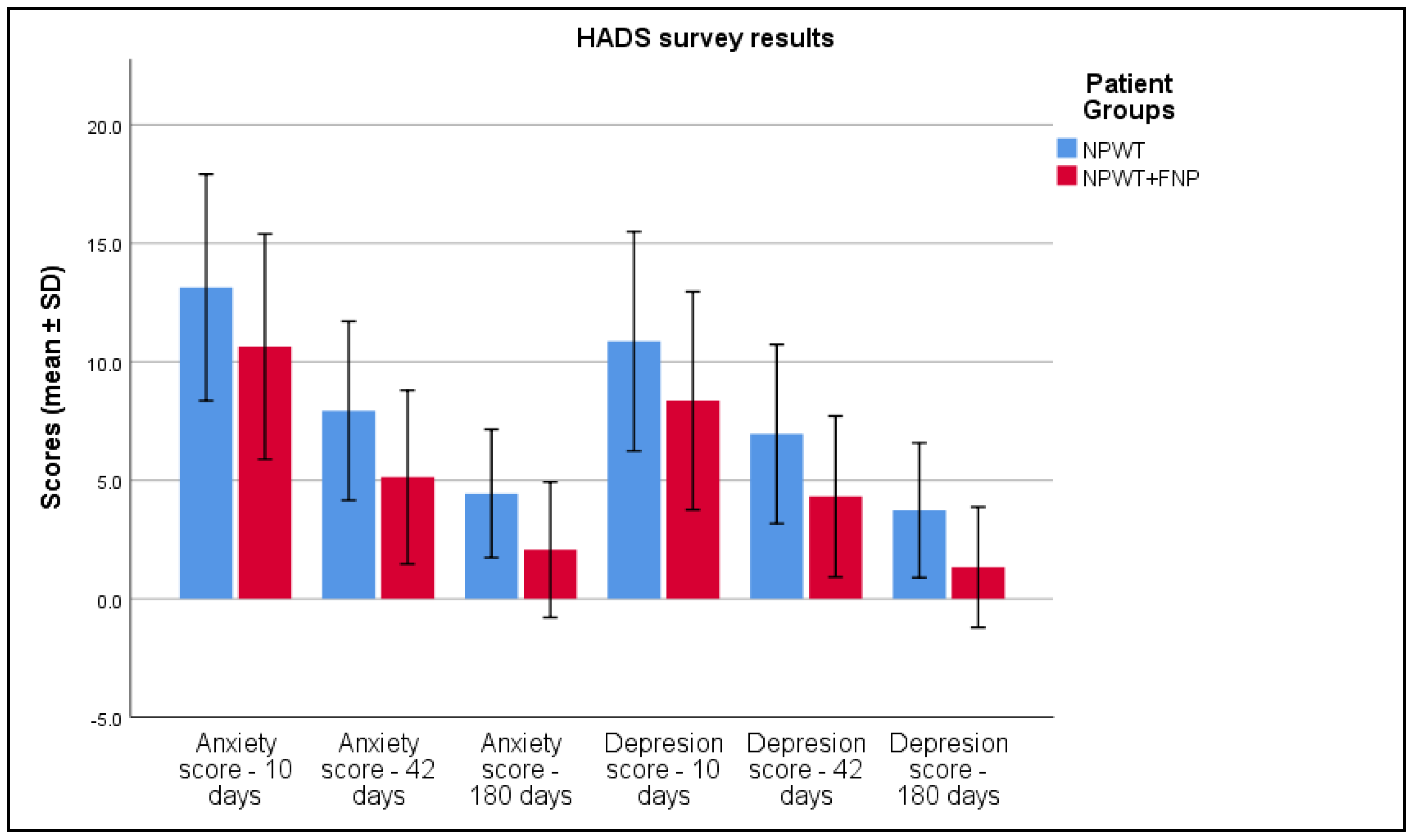
| Anxiety score—10 days | 13.14 ± 2.39 | 10.64 ± 2.38 | <0.001 | 1.05 |
| Anxiety score—42 days | 7.93 ± 1.89 | 5.13 ± 1.83 | <0.001 | 1.48 |
| Anxiety score—180 days | 4.44 ± 1.35 | 2.08 ± 1.43 | <0.001 | 1.68 |
| Depression score—10 days | 10.87 ± 2.31 | 8.36 ± 2.30 | <0.001 | 1.09 |
| Depression score—42 days | 6.95 ± 1.89 | 4.32 ± 1.70 | <0.001 | 1.43 |
| Depression score—180 days | 3.74 ± 1.42 | 1.33 ± 1.27 | <0.001 | 1.66 |
| Variables | NPWT (n = 110) | NPWT+FNP (n = 82) | p-Value | Cohen’s d |
|---|---|---|---|---|
| VAS score—10 days | 6.7 ± 1.05 | 5.52 ± 1.01 | <0.001 | 1.14 |
| VAS score—42 days | 3.31 ± 1.34 | 1.35 ± 1.03 | <0.001 | 1.63 |
| VAS score—180 days | 0.05 ± 0.31 | 0 ± 0 | 0.137 | 0.19 |
| Time | Variable | Correlated Outcome | Coefficient (r) | p-Value |
|---|---|---|---|---|
| 10 Days | MMT tibialis anterior | SF-36 | 0.090 | 0.214 |
| 10 Days | MMT triceps surae | SF-36 | 0.012 | 0.870 |
| 10 Days | MMT tibialis anterior | WHOQOL-BREF | 0.162 | 0.025 |
| 10 Days | MMT triceps surae | WHOQOL-BREF | 0.056 | 0.438 |
| 10 Days | MMT tibialis anterior | HADS Anxiety | −0.089 | 0.221 |
| 10 Days | MMT triceps surae | HADS Anxiety | −0.113 | 0.117 |
| 10 Days | MMT tibialis anterior | VAS | −0.203 | 0.005 |
| 10 Days | MMT triceps surae | VAS | −0.138 | 0.056 |
| 10 Days | Pronation | SF-36 | −0.248 | 0.001 |
| 10 Days | Pronation | WHOQOL-BREF | 0.517 | <0.001 |
| 10 Days | Pronation | HADS Anxiety | −0.381 | <0.001 |
| 10 Days | Pronation | VAS | −0.460 | <0.001 |
| 10 Days | Supination | SF-36 | 0.560 | <0.001 |
| 10 Days | Supination | WHOQOL-BREF | 0.596 | <0.001 |
| 10 Days | Supination | HADS Anxiety | −0.450 | <0.001 |
| 10 Days | Supination | VAS | −0.476 | <0.001 |
| 10 Days | Edema circumference | SF-36 | −0.011 | 0.879 |
| 10 Days | Edema circumference | WHOQOL-BREF | −0.049 | 0.497 |
| 10 Days | Edema circumference | HADS Anxiety | 0.070 | 0.334 |
| 10 Days | Edema circumference | VAS | 0.165 | 0.023 |
| 6 Weeks | MMT tibialis anterior | SF-36 | 0.231 | 0.001 |
| 6 Weeks | MMT triceps surae | SF-36 | 0.195 | 0.007 |
| 6 Weeks | MMT tibialis anterior | WHOQOL-BREF | 0.218 | 0.002 |
| 6 Weeks | MMT triceps surae | WHOQOL-BREF | 0.207 | 0.004 |
| 6 Weeks | MMT tibialis anterior | HADS Anxiety | −0.210 | 0.004 |
| 6 Weeks | MMT triceps surae | HADS Anxiety | −0.170 | 0.019 |
| 6 Weeks | MMT tibialis anterior | VAS | −0.303 | <0.001 |
| 6 Weeks | MMT triceps surae | VAS | −0.260 | <0.001 |
| 6 Weeks | Pronation | SF-36 | 0.355 | <0.001 |
| 6 Weeks | Pronation | WHOQOL-BREF | 0.093 | 0.198 |
| 6 Weeks | Pronation | HADS Anxiety | −0.310 | <0.001 |
| 6 Weeks | Pronation | VAS | −0.365 | <0.001 |
| 6 Weeks | Supination | SF-36 | 0.451 | <0.001 |
| 6 Weeks | Supination | WHOQOL-BREF | 0.429 | <0.001 |
| 6 Weeks | Supination | HADS Anxiety | −0.451 | <0.001 |
| 6 Weeks | Supination | VAS | −0.448 | <0.001 |
| 6 Weeks | Edema circumference | SF-36 | −0.179 | 0.013 |
| 6 Weeks | Edema circumference | WHOQOL-BREF | −0.076 | 0.295 |
| 6 Weeks | Edema circumference | HADS Anxiety | 0.153 | 0.034 |
| 6 Weeks | Edema circumference | VAS | 0.168 | 0.020 |
| 6 Months | MMT tibialis anterior | SF-36 | 0.205 | 0.004 |
| 6 Months | MMT triceps surae | SF-36 | 0.032 | 0.656 |
| 6 Months | MMT tibialis anterior | WHOQOL-BREF | 0.076 | 0.297 |
| 6 Months | MMT triceps surae | WHOQOL-BREF | −0.010 | 0.887 |
| 6 Months | MMT tibialis anterior | HADS Anxiety | −0.117 | 0.105 |
| 6 Months | MMT triceps surae | HADS Anxiety | 0.017 | 0.820 |
| 6 Months | MMT tibialis anterior | VAS | 0.036 | 0.619 |
| 6 Months | MMT triceps surae | VAS | 0.026 | 0.720 |
| 6 Months | Pronation | SF-36 | −0.017 | 0.814 |
| 6 Months | Pronation | WHOQOL-BREF | 0.044 | 0.543 |
| 6 Months | Pronation | HADS Anxiety | 0.073 | 0.312 |
| 6 Months | Pronation | VAS | −0.024 | 0.738 |
| 6 Months | Supination | SF-36 | −0.044 | 0.544 |
| 6 Months | Supination | WHOQOL-BREF | −0.053 | 0.461 |
| 6 Months | Supination | HADS Anxiety | −0.036 | 0.621 |
| 6 Months | Supination | VAS | −0.086 | 0.238 |
| 6 Months | Edema circumference | SF-36 | 0.057 | 0.435 |
| 6 Months | Edema circumference | WHOQOL-BREF | 0.051 | 0.486 |
| 6 Months | Edema circumference | HADS Anxiety | −0.088 | 0.226 |
| 6 Months | Edema circumference | VAS | 0.084 | 0.249 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stanciu, C.-T.; Vermesan, D.; Pop, D.L.; Hogea, B.; Vlad, S.V. Functional and Clinical Outcomes in Acute Wound Management: Measuring the Impact of Negative Pressure Wound Therapy and Specialized Physical Therapy. Life 2025, 15, 511. https://doi.org/10.3390/life15040511
Stanciu C-T, Vermesan D, Pop DL, Hogea B, Vlad SV. Functional and Clinical Outcomes in Acute Wound Management: Measuring the Impact of Negative Pressure Wound Therapy and Specialized Physical Therapy. Life. 2025; 15(4):511. https://doi.org/10.3390/life15040511
Chicago/Turabian StyleStanciu, Cristina-Teodora, Dinu Vermesan, Daniel Laurentiu Pop, Bogdan Hogea, and Silviu Valentin Vlad. 2025. "Functional and Clinical Outcomes in Acute Wound Management: Measuring the Impact of Negative Pressure Wound Therapy and Specialized Physical Therapy" Life 15, no. 4: 511. https://doi.org/10.3390/life15040511
APA StyleStanciu, C.-T., Vermesan, D., Pop, D. L., Hogea, B., & Vlad, S. V. (2025). Functional and Clinical Outcomes in Acute Wound Management: Measuring the Impact of Negative Pressure Wound Therapy and Specialized Physical Therapy. Life, 15(4), 511. https://doi.org/10.3390/life15040511







