Off-Label Sildenafil Citrate as a Rescue Therapy for Areolar Venous Congestion Post–Breast Reduction: Case Series and Outcomes
Abstract
1. Introduction
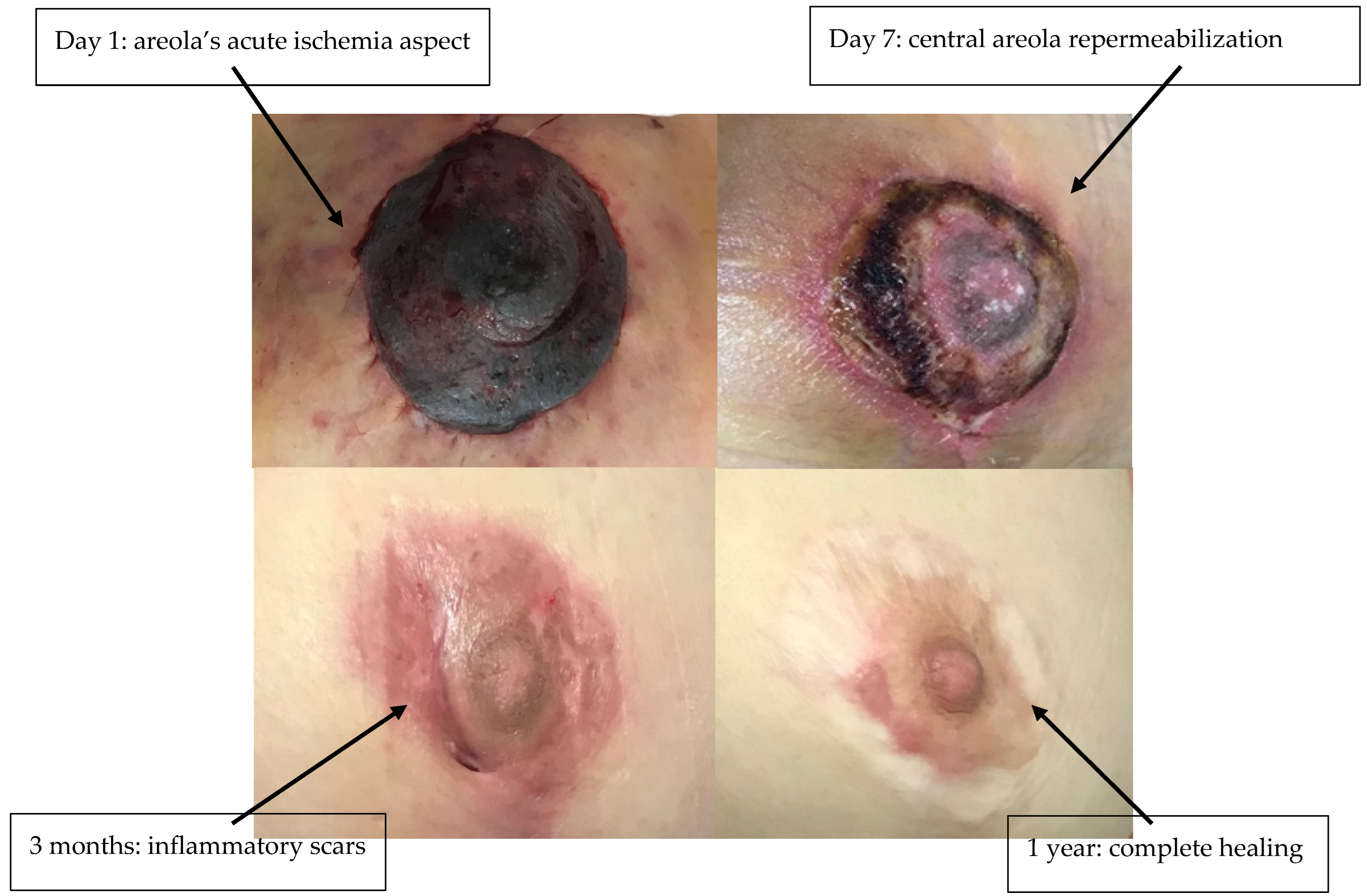
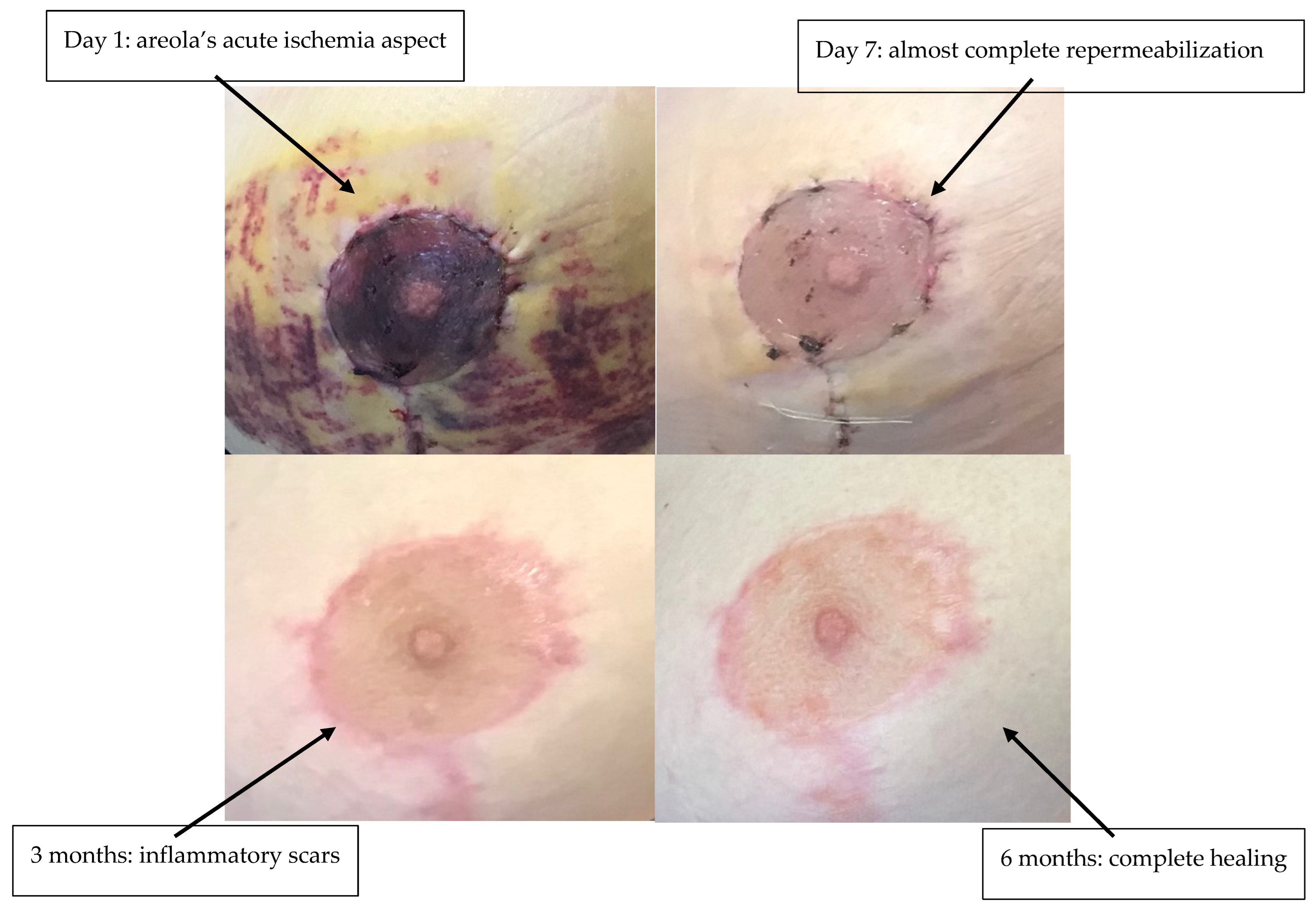
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Balogun, O.T.; Wanzel, K.R. Areolar Contractility as a Sign of Nipple-Areolar Complex Vascular Insufficiency in Reduction Mammoplasty—Bridging the Gap in Breast Surgery for Diverse Skin Tones. Plast. Surg. 2025, 22925503251326276. [Google Scholar] [CrossRef]
- Lai, H.W.; Lee, Y.Y.; Chen, S.T.; Liao, C.Y.; Tsai, T.L.; Chen, D.R.; Lai, Y.C.; Kao, W.P.; Wu, W.P. Nipple-Areolar Complex (NAC) or Skin Flap Ischemia Necrosis Post Nipple-Sparing Mastectomy (NSM)—Analysis of Clinicopathologic Factors and Breast Magnetic Resonance Imaging (MRI) Features. World J. Surg. Oncol. 2023, 21, 23. [Google Scholar] [CrossRef]
- Zhang, M.X.; Chen, C.Y.; Fang, Q.Q.; Xu, J.H.; Wang, X.F.; Shi, B.H.; Wu, L.H.; Tan, W.Q. Risk Factors for Complications after Reduction Mammoplasty: A Meta-Analysis. PLoS ONE 2016, 11, e0167746. [Google Scholar] [CrossRef]
- Lewin, R.; Göransson, M.; Elander, A.; Thorarinsson, A.; Lundberg, J.; Lidén, M. Risk Factors for Complications after Breast Reduction Surgery. J. Plast. Surg. Hand Surg. 2014, 48, 10–14. [Google Scholar] [CrossRef] [PubMed]
- Park, J.K.; Myung, Y. Treatment of Delayed Venous Congestion of the Nipple-Areolar Complex after Reduction Mammoplasty. Arch. Aesthetic Plast. Surg. 2021, 27, 39–42. [Google Scholar] [CrossRef]
- Stead, T.S.; Laspro, M.; Ramirez-Arroyo, G.; Ganti, L.; Mitra, A. Mitigating Nipple Areolar Complex (NAC) Ischemia Following Mastopexy Augmentation Using Nitroglycerin Application and Methylprednisolone: A Case Report. Case Rep. Plast. Surg. Hand Surg. 2023, 10, 2285056. [Google Scholar] [CrossRef] [PubMed]
- Reichert, R.; Weitgasser, L.; Schoeller, T.; Wimmer, F.; Russe, E.; Mahrhofer, M. Compromised Nipple-Areola Complex Perfusion after Reduction Mammaplasty or Mastopexy: A Retrospective Evaluation of Different Treatments. Aesthetic Plast. Surg. 2025, 49, 3425–3432. [Google Scholar] [CrossRef]
- Rajaram, R.; Cevik, J.; Bhindi, N.; Seth, I.; Rozen, W.M. The Use of Medicinal Leeching in Breast Surgery: A Systematic Review. J. Clin. Med. 2024, 13, 1243. [Google Scholar] [CrossRef]
- Salibian, A.A.; Frey, J.D.; Bekisz, J.M.; Karp, N.S.; Choi, M. Ischemic Complications after Nipple-Sparing Mastectomy: Predictors of Reconstructive Failure in Implant-Based Reconstruction and Implications for Decision-Making. Plast. Reconstr. Surg. Glob. Open 2019, 7, E2280. [Google Scholar] [CrossRef]
- Lee, P.L.; Ma, I.T.; Schusterman, M.A.; Beiriger, J.; Ahrendt, G.; De La Cruz, C.; Diego, E.J.; Steiman, J.G.; McAuliffe, P.F.; Gimbel, M.L. Surgical Nipple Delay and Its Expanded Indications for Nipple-Sparing Mastectomy. Plast. Reconstr. Surg. Glob. Open 2023, 11, E4783. [Google Scholar] [CrossRef]
- Pușcașu, C.; Zanfirescu, A.; Negreș, S.; Șeremet, O.C. Exploring the Multifaceted Potential of Sildenafil in Medicine. Medicina 2023, 59, 2190. [Google Scholar] [CrossRef]
- Chrysant, S.G.; Chrysant, G.S. The Pleiotropic Effects of Phosphodiesterase 5 Inhibitors on Function and Safety in Patients with Cardiovascular Disease and Hypertension. J. Clin. Hypertens. 2012, 14, 644. [Google Scholar] [CrossRef]
- Shahrokhi, M.; Naghibi, F.; Moraghebi, S.; Khorrami, P.; Mashayekhi-sardoo, H. Efficacy of Topical Sildenafil Formulations in Enhancing Wound Healing Outcomes: A Narrative Review. Arch. Dermatol. Res. 2025, 317, 642. [Google Scholar] [CrossRef] [PubMed]
- Hart, K.; Baur, D.; Hodam, J.; Lesoon-Wood, L.; Parham, M.; Keith, K.; Vazquez, R.; Ager, E.; Pizarro, J. Short- and Long-Term Effects of Sildenafil on Skin Flap Survival in Rats. Laryngoscope 2006, 116, 522–528. [Google Scholar] [CrossRef]
- Sarifakioglu, N.; Gokrem, S.; Ates, L.; Akbuga, U.B.; Aslan, G. The Influence of Sildenafil on Random Skin Flap Survival in Rats: An Experimental Study. Br. J. Plast. Surg. 2004, 57, 769–772. [Google Scholar] [CrossRef] [PubMed]
- Kara, M.; Baykan, H.; Karabulut, D. Investigation of the Effect of Sildenafil on Flap Survival in a Diabetic Rat Model. Ann. Chir. Plast. Esthétique 2022, 67, 232–238. [Google Scholar] [CrossRef]
- Pfaff, M.; Shah, A.; Steinbacher, D. Does Phosphodiesterase Inhibition Lessen Facial Flap Necrosis in Tobacco Cigarette Users? Facial Plast. Surg. 2014, 30, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Matin, T.; Seyffert, J.; Katz, B.; Rivlin, D. Tadalafil to Improve Cutaneous Flap Perfusion in Smokers: A Case Series and Literature Review. JAAD Case Rep. 2021, 15, 126. [Google Scholar] [CrossRef]
- Perdikis, G.; Dillingham, C.; Boukovalas, S.; Ogunleye, A.A.; Casambre, F.; Dal Cin, A.; Davidson, C.; Davies, C.C.; Donnelly, K.C.; Fischer, J.P.; et al. American Society of Plastic Surgeons Evidence-Based Clinical Practice Guideline Revision: Reduction Mammaplasty. Plast. Reconstr. Surg. 2022, 149, 392e–409e. [Google Scholar] [CrossRef]
- Faulkner, H.R.; Merceron, T.; Wang, J.; Losken, A. Safe Reproducible Breast Reduction. Plast. Reconstr. Surg. Glob. Open 2023, 11, E5245. [Google Scholar] [CrossRef]
- Wang, P.; Gu, L.; Qin, Z.; Wang, Q.; Ma, J. Efficacy and Safety of Topical Nitroglycerin in the Prevention of Mastectomy Flap Necrosis: A Systematic Review and Meta-Analysis. Sci. Rep. 2020, 10, 6753. [Google Scholar] [CrossRef]
- Hackenberger, P.N.; Janis, J.E. A Comprehensive Review of Medicinal Leeches in Plastic and Reconstructive Surgery. Plast. Reconstr. Surg. Glob. Open 2019, 7, E2555. [Google Scholar] [CrossRef] [PubMed]
- Masters, M.C.; Gupta, A.R.; Rhodes, N.J.; Flaherty, J.P.; Zembower, T.R.; Alghoul, M.; Krueger, K.M. Multidrug Resistant Aeromonas Infection Following Medical Leech Therapy: A Case Report and Development of a Joint Antimicrobial Stewardship and Infection Prevention Protocol. J. Glob. Antimicrob. Resist. 2020, 23, 349–351. [Google Scholar] [CrossRef]
- Ferrando, P.M.; Ala, A.; Bussone, R.; Bergamasco, L.; Perinetti, F.A.; Malan, F. Closed Incision Negative Pressure Therapy in Oncological Breast Surgery: Comparison with Standard Care Dressings. Plast. Reconstr. Surg. Glob. Open 2018, 6, e1732. [Google Scholar] [CrossRef]
- Esen, E.; Morkavuk, S.B.; Turan, M.; Akyuz, S.; Guler, S.; Akgul, G.G.; Bahcecioglu, I.B.; Gulcelik, M.A.; Yilmaz, K.B. The Use of Incisional Negative-Pressure Wound Therapy on High-Risk Patients with Breast Cancer after Mastectomy. Asian J. Surg. 2025, 48, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.Y.; Park, S.J.; Bang, S.I.; Mun, G.H.; Pyon, J.K. Does the Use of Incisional Negative-Pressure Wound Therapy Prevent Mastectomy Flap Necrosis in Immediate Expander-Based Breast Reconstruction? Plast. Reconstr. Surg. 2016, 138, 558–566. [Google Scholar] [CrossRef]
- Levit, T.; Olaiya, O.; Lavoie, D.C.T.; Avram, R.; Coroneos, C.J. The Use of Negative Pressure Wound Therapy for Breast Surgeries: A Systematic Review and Meta-Analysis. Plast. Surg. 2025, 22925503251336253. [Google Scholar] [CrossRef] [PubMed]
- Yaguas, K.; Bautista, R.; Quiroz, Y.; Ferrebuz, A.; Pons, H.; Franco, M.; Vaziri, N.D.; Rodriguez-Iturbe, B. Chronic Sildenafil Treatment Corrects Endothelial Dysfunction and Improves Hypertension. Am. J. Nephrol. 2010, 31, 283–291. [Google Scholar] [CrossRef]
- Benza, R.L.; Simonneau, G.; Grünig, E.; Sandner, P.; Stasch, J.P. The Nitric Oxide–Soluble Guanylate Cyclase–CGMP Pathway in Pulmonary Hypertension: From PDE5 to Soluble Guanylate Cyclase. Eur. Respir. Rev. 2024, 33, 230183. [Google Scholar] [CrossRef]
- Semen, K.; Yelisyeyeva, O.; Jarocka-Karpowicz, I.; Kaminskyy, D.; Solovey, L.; Skrzydlewska, E.; Yavorskyi, O. Sildenafil Reduces Signs of Oxidative Stress in Pulmonary Arterial Hypertension: Evaluation by Fatty Acid Composition, Level of Hydroxynonenal and Heart Rate Variability. Redox Biol. 2016, 7, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Kniotek, M.; Boguska, A. Sildenafil Can Affect Innate and Adaptive Immune System in Both Experimental Animals and Patients. J. Immunol. Res. 2017, 2017, 4541958. [Google Scholar] [CrossRef] [PubMed]
- Dias, A.T.; Rodrigues, B.P.; Porto, M.L.; Gava, A.L.; Balarini, C.M.; Freitas, F.P.S.; Palomino, Z.; Casarini, D.E.; Campagnaro, B.P.; Pereira, T.M.C.; et al. Sildenafil Ameliorates Oxidative Stress and DNA Damage in the Stenotic Kidneys in Mice with Renovascular Hypertension. J. Transl. Med. 2014, 12, 35. [Google Scholar] [CrossRef]
- Irigo, M.; Coscarelli, L.; Rancati, A. Anatomical Basis of Pedicles in Breast Reduction. Gland. Surg. 2017, 6, 154–162. [Google Scholar] [CrossRef]
- Hosny, H.; Mansour, S.; El-Essawy, N.M. Duplex Study of the Nipple–Areola Complex Blood Supply in the Female Breast. Aesthet. Surg. J. Open Forum 2025, 7, ojae090. [Google Scholar] [CrossRef]
- Ellabban, M.A.; Fattah, I.O.A.; Kader, G.A.; Eldeen, O.S.; Mehana, A.E.; Khodeer, D.M.; Hosny, H.; Elbasiouny, M.S.; Masadeh, S. The Effects of Sildenafil and/or Nitroglycerin on Random-Pattern Skin Flaps After Nicotine Application in Rats. Sci. Rep. 2020, 10, 3212. [Google Scholar] [CrossRef]
- Souza, R.A.C.; Martinelli-Kläy, C.P.; d’Acampora, A.J.; Bernardes, G.J.S.; Sgrott, S.M.; Souza, L.A.C.; Lombardi, T.; Sudbrack, T.R. Effects of Sildenafil and Tadalafil on Skin Flap Viability. Arch. Dermatol. Res. 2021, 314, 151. [Google Scholar] [CrossRef]
- Gürhan Ulusoy, M.; Uysal, A.; Koçer, U.; Karaaslan, Ö.; Sedat Cuzdan, S.; Ayyildiz, A.; Üstün, H. Improved Flap Viability with Site-Specific Delivery of Sildenafil Citrate Using Fibrin Glue. Ann. Plast. Surg. 2005, 55, 292–296. [Google Scholar] [CrossRef]
- Valencia, G.A.; Krishnan, U. Idiopathic Pulmonary Arterial Hypertension in Children: A Review. Pulm. Ther. 2017, 3, 67–92. [Google Scholar] [CrossRef]
- Dodgen, A.L.; Hill, K.D. Safety and Tolerability Considerations in the Use of Sildenafil for Children with Pulmonary Arterial Hypertension. Drug Healthc. Patient Saf. 2015, 7, 175–183. [Google Scholar] [CrossRef]
- Papathanasiou, M.; Ruhparwar, A.; Kamler, M.; Rassaf, T.; Luedike, P. Off-Label Use of Pulmonary Vasodilators after Left Ventricular Assist Device Implantation: Calling in the Evidence. Pharmacol. Ther. 2020, 214, 107619. [Google Scholar] [CrossRef]
- Varghese, R.; Digholkar, G.; Karsiya, J.; Salvi, S.; Shah, J.; Kumar, D.; Sharma, R. PDE5 Inhibitors: Breaking New Grounds in the Treatment of COVID-19. Drug Metab. Pers. Ther. 2023, 38, 295–307. [Google Scholar] [CrossRef]
- Santamarina, M.G.; Beddings, I.; Lomakin, F.M.; Boisier Riscal, D.; Gutiérrez Claveria, M.; Vidal Marambio, J.; Retamal Báez, N.; Pavez Novoa, C.; Reyes Allende, C.; Ferreira Perey, P.; et al. Sildenafil for Treating Patients with COVID-19 and Perfusion Mismatch: A Pilot Randomized Trial. Crit. Care 2022, 26, 1. [Google Scholar] [CrossRef] [PubMed]
- Cesta, C.E.; Segovia Chacón, S.; Engeland, A.; Broe, A.; Damkier, P.; Furu, K.; Kieler, H.; Karlsson, P. Use of Sildenafil and Other Phosphodiesterase Type 5 Inhibitors among Pregnant Women in Scandinavia. Acta Obstet. Gynecol. Scand. 2021, 100, 2111–2118. [Google Scholar] [CrossRef]
- Zimmermann, L.M.; Baptista, M.S.; Tardivo, J.P.; Pinhal, M.A. Type II Diabetes Patients under Sildenafil Citrate: Case Series Showing Benefits and a Side Effect. Case Rep. Med. 2020, 2020, 4065452. [Google Scholar] [CrossRef]
- Ko, W.J.; Han, H.H.; Ham, W.S.; Lee, H.W. Daily Use of Sildenafil 50mg at Night Effectively Ameliorates Nocturia in Patients with Lower Urinary Tract Symptoms Associated with Benign Prostatic Hyperplasia: An Exploratory Multicenter, Double-Blind, Randomized, Placebo-Controlled Study. Aging Male 2017, 20, 81–88. [Google Scholar] [CrossRef]
- Samudra, N.; Motes, M.; Lu, H.; Sheng, M.; Diaz-Arrastia, R.; Devous, M.; Hart, J.; Womack, K.B. A Pilot Study of Changes in Medial Temporal Lobe Fractional Amplitude of Low Frequency Fluctuations after Sildenafil Administration in Patients with Alzheimer’s Disease. J. Alzheimers Dis. 2019, 70, 163. [Google Scholar] [CrossRef] [PubMed]
- Dhariwal, A.K.; Bavdekar, S.B. Sildenafil in Pediatric Pulmonary Arterial Hypertension. J. Postgrad. Med. 2015, 61, 181. [Google Scholar] [CrossRef] [PubMed]

| Patient | 1 | 2 | 3 |
|---|---|---|---|
| Age (years) | 42 | 26 | 30 |
| BMI (kg/m2) | 29 | 26.74 | 25.8 |
| Smoking | No | No | No |
| Diabetes mellitus | No | No | No |
| Arterial hypertension | No | No | No |
| Breast delta (resection weight) | Right side: 1009 g Left side: 1049 g | Right side: 855 g Left side: 819 g | Right side: 635 g Left side: 1008 g |
| Postoperative time before management of areolar pain | 24 h | 24 h | 24 h |
| Duration of treatment | 5 days | 5 days | 5 days |
| Side effects | Hot flashes, palpitations | Hot flashes, palpitations | Hot flashes, palpitations |
| Areolar rescue | 95% | 95% | 95% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bilha, S.C.; Ramelli, E.; Huttin, C.; Hogas, S.M.; Ringenbach, P.; Branisteanu, D.D.; Ioniuc, I.K.; Popescu, I.-R.; Nastasa, M.E.; Hogas, M. Off-Label Sildenafil Citrate as a Rescue Therapy for Areolar Venous Congestion Post–Breast Reduction: Case Series and Outcomes. Life 2025, 15, 1644. https://doi.org/10.3390/life15111644
Bilha SC, Ramelli E, Huttin C, Hogas SM, Ringenbach P, Branisteanu DD, Ioniuc IK, Popescu I-R, Nastasa ME, Hogas M. Off-Label Sildenafil Citrate as a Rescue Therapy for Areolar Venous Congestion Post–Breast Reduction: Case Series and Outcomes. Life. 2025; 15(11):1644. https://doi.org/10.3390/life15111644
Chicago/Turabian StyleBilha, Stefana Catalina, Eloi Ramelli, Charline Huttin, Simona Mihaela Hogas, Patrick Ringenbach, Dumitru D. Branisteanu, Ileana Katerina Ioniuc, Ionut-Raducu Popescu, Mihaela Elena Nastasa, and Mihai Hogas. 2025. "Off-Label Sildenafil Citrate as a Rescue Therapy for Areolar Venous Congestion Post–Breast Reduction: Case Series and Outcomes" Life 15, no. 11: 1644. https://doi.org/10.3390/life15111644
APA StyleBilha, S. C., Ramelli, E., Huttin, C., Hogas, S. M., Ringenbach, P., Branisteanu, D. D., Ioniuc, I. K., Popescu, I.-R., Nastasa, M. E., & Hogas, M. (2025). Off-Label Sildenafil Citrate as a Rescue Therapy for Areolar Venous Congestion Post–Breast Reduction: Case Series and Outcomes. Life, 15(11), 1644. https://doi.org/10.3390/life15111644





