Radiation Pneumonitis Risk Assessment Using Fractal Analyses in NSCLC Patients Treated with Curative-Intent Radiotherapy
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Data Collection
2.2. Treatment Scheme and Surveillance
2.3. CT Scanning and Morphometric Complexity Analyses
2.4. Statistical Analyses and Feature Selection
3. Results
3.1. Baseline Characteristics and RP Incidences
3.2. Changes in Fractal Dimensions Post-Radiotherapy
3.3. Feature Importance in Random Forest Model
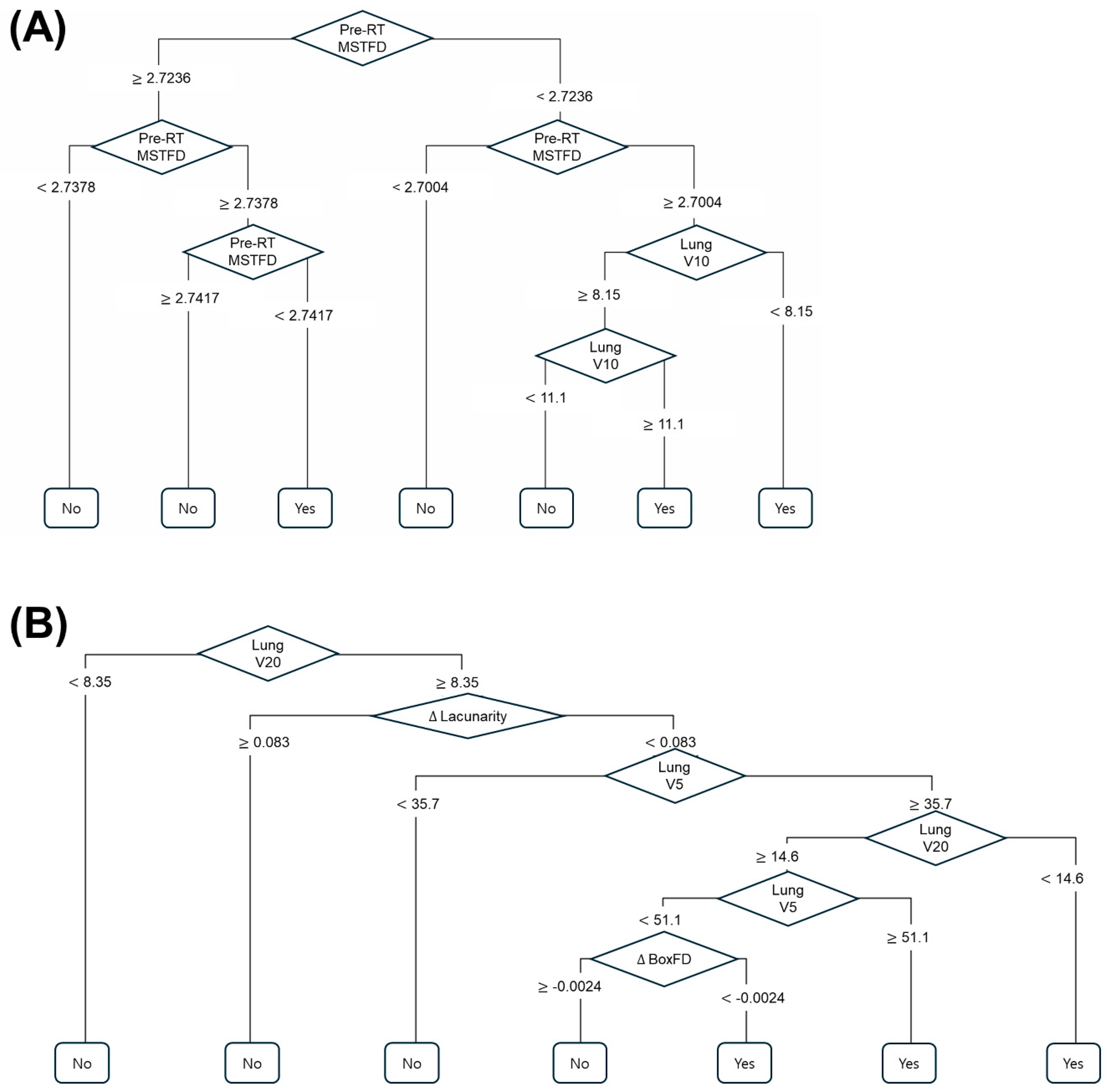
3.4. Decision Tree Model Performance for RP Prediction
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Baker, R.; Han, G.; Sarangkasiri, S.; DeMarco, M.; Turke, C.; Stevens, C.W.; Dilling, T.J. Clinical and dosimetric predictors of radiation pneumonitis in a large series of patients treated with stereotactic body radiation therapy to the lung. Int. J. Radiat. Oncol. Biol. Phys. 2013, 85, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Claude, L.; Perol, D.; Ginestet, C.; Falchero, L.; Arpin, D.; Vincent, M.; Martel, I.; Hominal, S.; Cordier, J.F.; Carrie, C. A prospective study on radiation pneumonitis following conformal radiation therapy in non-small-cell lung cancer: Clinical and dosimetric factors analysis. Radiother. Oncol. 2004, 71, 175–181. [Google Scholar] [CrossRef]
- Lee, Y.H.; Kim, Y.S.; Lee, S.N.; Lee, H.C.; Oh, S.J.; Kim, S.J.; Kim, Y.K.; Han, D.H.; Yoo Ie, R.; Kang, J.H.; et al. Interstitial Lung Change in Pre-radiation Therapy Computed Tomography Is a Risk Factor for Severe Radiation Pneumonitis. Cancer Res. Treat. 2015, 47, 676–686. [Google Scholar] [CrossRef]
- Leprieur, E.G.; Fernandez, D.; Chatellier, G.; Klotz, S.; Giraud, P.; Durdux, C. Acute radiation pneumonitis after conformational radiotherapy for nonsmall cell lung cancer: Clinical, dosimetric, and associated-treatment risk factors. J. Cancer Res. Ther. 2013, 9, 447–451. [Google Scholar] [CrossRef]
- Park, Y.H.; Kim, J.S. Predictors of radiation pneumonitis and pulmonary function changes after concurrent chemoradiotherapy of non-small cell lung cancer. Radiat. Oncol. J. 2013, 31, 34–40. [Google Scholar] [CrossRef]
- Rancati, T.; Ceresoli, G.L.; Gagliardi, G.; Schipani, S.; Cattaneo, G.M. Factors predicting radiation pneumonitis in lung cancer patients: A retrospective study. Radiother. Oncol. 2003, 67, 275–283. [Google Scholar] [CrossRef]
- Robnett, T.J.; Machtay, M.; Vines, E.F.; McKenna, M.G.; Algazy, K.M.; McKenna, W.G. Factors predicting severe radiation pneumonitis in patients receiving definitive chemoradiation for lung cancer. Int. J. Radiat. Oncol. Biol. Phys. 2000, 48, 89–94. [Google Scholar] [CrossRef]
- Shi, A.; Zhu, G.; Wu, H.; Yu, R.; Li, F.; Xu, B. Analysis of clinical and dosimetric factors associated with severe acute radiation pneumonitis in patients with locally advanced non-small cell lung cancer treated with concurrent chemotherapy and intensity-modulated radiotherapy. Radiat. Oncol. 2010, 5, 35. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Hwang, J.; Kim, S.M.; Choi, J.; Yang, D.S. Risk factor analysis of the development of severe radiation pneumonitis in patients with non-small cell lung cancer treated with curative radiotherapy, with focus on underlying pulmonary disease. BMC Cancer 2023, 23, 992. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Pyo, H.; Noh, J.M.; Lee, W.; Park, B.; Park, H.Y.; Yoo, H. Preliminary result of definitive radiotherapy in patients with non-small cell lung cancer who have underlying idiopathic pulmonary fibrosis: Comparison between X-ray and proton therapy. Radiat. Oncol. 2019, 14, 19. [Google Scholar] [CrossRef]
- Kim, H.; Yoo, H.; Pyo, H.; Ahn, Y.C.; Noh, J.M.; Ju, S.G.; Lee, W.; Park, B.; Kim, J.M.; Kang, N.; et al. Impact Of Underlying Pulmonary Diseases On Treatment Outcomes In Early-Stage Non-Small Cell Lung Cancer Treated With Definitive Radiotherapy. Int. J. Chron. Obstruct Pulmon Dis. 2019, 14, 2273–2281. [Google Scholar] [CrossRef]
- Ley, B.; Elicker, B.M.; Hartman, T.E.; Ryerson, C.J.; Vittinghoff, E.; Ryu, J.H.; Lee, J.S.; Jones, K.D.; Richeldi, L.; King, T.E., Jr.; et al. Idiopathic pulmonary fibrosis: CT and risk of death. Radiology. 2014, 273, 570–579. [Google Scholar] [CrossRef]
- Lee, T.; Park, J.Y.; Lee, H.Y.; Cho, Y.J.; Yoon, H.I.; Lee, J.H.; Jheon, S.; Lee, C.T.; Park, J.S. Lung cancer in patients with idiopathic pulmonary fibrosis: Clinical characteristics and impact on survival. Respir. Med. 2014, 108, 1549–1555. [Google Scholar] [CrossRef] [PubMed]
- Kanaji, N.; Tadokoro, A.; Kita, N.; Murota, M.; Ishii, T.; Takagi, T.; Watanabe, N.; Tojo, Y.; Harada, S.; Hasui, Y.; et al. Impact of idiopathic pulmonary fibrosis on advanced non-small cell lung cancer survival. J. Cancer Res. Clin. Oncol. 2016, 142, 1855–1865. [Google Scholar] [CrossRef] [PubMed]
- Tomassetti, S.; Gurioli, C.; Ryu, J.H.; Decker, P.A.; Ravaglia, C.; Tantalocco, P.; Buccioli, M.; Piciucchi, S.; Sverzellati, N.; Dubini, A.; et al. The impact of lung cancer on survival of idiopathic pulmonary fibrosis. Chest 2015, 147, 157–164. [Google Scholar] [CrossRef]
- Hwang, J.; Kim, H.; Kim, S.M.; Yang, D.S. Preliminary Results of Developing Imaging Complexity Biomarkers for the Incidence of Severe Radiation Pneumonitis Following Radiotherapy in Non-Small Cell Lung Cancer Patients with Underlying Idiopathic Pulmonary Fibrosis. Life 2024, 14, 897. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.; Kim, H.; Moon, J.Y.; Kim, S.M.; Yang, D.S. Development of Imaging Complexity Biomarkers for Prediction of Symptomatic Radiation Pneumonitis in Patients with Non-Small Cell Lung Cancer, Focusing on Underlying Lung Disease. Life 2024, 14, 1497. [Google Scholar] [CrossRef]
- Grassberger, P. On the fractal dimension of the Henon attractor. Phys. Lett. A 1983, 97, 224–226. [Google Scholar] [CrossRef]
- Edwards, O. Strange attractors and fractal dimensions. In In Chaos in Dynamical Systems; Cambridge University Press: Cambridge, UK, 1993; pp. 69–107. [Google Scholar]
- Kozma, G.; Lotker, Z.; Stupp, G. The minimal spanning tree and the upper box dimension. Proc. Am. Math. Soc. 2006, 134, 1183–1187. [Google Scholar] [CrossRef]
- Martinez, V.J.; Dominguez-Tenreiro, R.; Roy, L.J. Hausdorff dimension from the minimal spanning tree. Phys. Rev. E Stat. Phys. Plasmas Fluids Relat. Interdiscip. Topics 1993, 47, 735–738. [Google Scholar] [CrossRef]
- Wang, S.; Xu, D.; Xiao, L.; Liu, B.; Yuan, X. Radiation-induced lung injury: From mechanism to prognosis and drug therapy. Radiat. Oncol. 2025, 20, 39. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.; Oh, Y.M.; Lee, M.; Choi, S.; Seo, J.B.; Lee, S.M.; Kim, N. Low morphometric complexity of emphysematous lesions predicts survival in chronic obstructive pulmonary disease patients. Eur. Radiol. 2019, 29, 176–185. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Lei, Z.; Wu, H.; Lu, H. Evaluating risk factors of radiation pneumonitis after stereotactic body radiation therapy in lung tumor: Meta-analysis of 9 observational studies. PLoS ONE 2018, 13, e0208637. [Google Scholar] [CrossRef] [PubMed]
- Xie, X.; Pei, M.; Chen, M.; Zhou, Y.; Ren, D.; Guo, Y. Predictive significance of the hemoglobin, albumin, lymphocyte, and platelet score for radiation pneumonitis in lung cancer patients: A respective comparative study with dosimetric parameters. Front. Oncol. 2025, 15, 1605094. [Google Scholar] [CrossRef]
| RT Alone (N = 85) | CCRT (N = 81) | |||
|---|---|---|---|---|
| Characteristics | Number | % | Number | % |
| Age [years; median (range)] | 79 (38–93) | 74 (53–93) | ||
| Sex | ||||
| Female | 29 | 34.1% | 11 | 13.6% |
| Male | 56 | 65.9% | 70 | 86.4% |
| Smoking Status | ||||
| Never smoker | 44 | 51.8% | 33 | 40.7% |
| Current or Ex-smoker | 41 | 48.2% | 48 | 59.3% |
| Planning Parameters | ||||
| Total lung MLD [cGy; median (range)] | 423 (88–1239) | 1036 (430–1933) | ||
| Total lung V5 [%; median (range)] | 20.0 (5.3–59.1) | 49.7 (15.5–96.4) | ||
| Total lung V20 [%; median (range)] | 5.9 (0.4–21.4) | 17.5 (5.0–363.0) | ||
| ≥Grade 2 RP | 19 | 22.3% | 44 | 54.3% |
| ≥Grade 3 RP | 6 | 7.1% | 16 | 19.8% |
| Pre-RT | Post-RT | Difference (Post–Pre) | p-Value * | |
|---|---|---|---|---|
| RT alone (N = 85) | ||||
| BoxFD [median (IQR)] | 2.315 (2.266–2.363) | 2.297 (2.249–2.332) | −0.015 (−0.055–0.014) | 0.988 |
| Lacunarity [median (IQR)] | 0.139 (0.119–0.175) | 0.149 (0.131–0.181) | 0.009 (−0.012–0.026) | 0.024 |
| MSTFD [median (IQR)] | 2.734 (2.707–2.751) | 2.728 (2.701–2.751) | −0.005 (−0.028–0.011) | 0.978 |
| CCRT (N = 81) | ||||
| BoxFD [median (IQR)] | 2.349 (2.292–2.383) | 2.307 (2.266–2.349) | −0.024 (−0.073–0.006) | 0.999 |
| Lacunarity [median (IQR)] | 0.137 (0.117–0.156) | 0.152 (0.135–0.174) | 0.016 (−0.006–0.040) | 0.00004 |
| MSTFD [median (IQR)] | 2.745 (2.716–2.767) | 2.725 (2.694–2.743) | −0.015 (−0.042–0.005) | 0.999 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, J.; Kim, S.M.; Moon, J.-Y.; Lee, B.; Song, J.; Lee, S.; Kim, H. Radiation Pneumonitis Risk Assessment Using Fractal Analyses in NSCLC Patients Treated with Curative-Intent Radiotherapy. Life 2025, 15, 1596. https://doi.org/10.3390/life15101596
Hwang J, Kim SM, Moon J-Y, Lee B, Song J, Lee S, Kim H. Radiation Pneumonitis Risk Assessment Using Fractal Analyses in NSCLC Patients Treated with Curative-Intent Radiotherapy. Life. 2025; 15(10):1596. https://doi.org/10.3390/life15101596
Chicago/Turabian StyleHwang, Jeongeun, Sun Myung Kim, Joon-Young Moon, Bona Lee, Jeongmin Song, Sookyung Lee, and Hakyoung Kim. 2025. "Radiation Pneumonitis Risk Assessment Using Fractal Analyses in NSCLC Patients Treated with Curative-Intent Radiotherapy" Life 15, no. 10: 1596. https://doi.org/10.3390/life15101596
APA StyleHwang, J., Kim, S. M., Moon, J.-Y., Lee, B., Song, J., Lee, S., & Kim, H. (2025). Radiation Pneumonitis Risk Assessment Using Fractal Analyses in NSCLC Patients Treated with Curative-Intent Radiotherapy. Life, 15(10), 1596. https://doi.org/10.3390/life15101596






