The State of Extracorporeal Shockwave Therapy for Myofascial Pain Syndrome—A Scoping Review and a Call for Standardized Protocols
Abstract
1. Introduction
1.1. Myofascial Pain Syndrome
1.2. Basics of Extracorporeal Shockwave Therapy
1.3. Specific Mechanisms of Action of ESWT on Myofascial Tissue
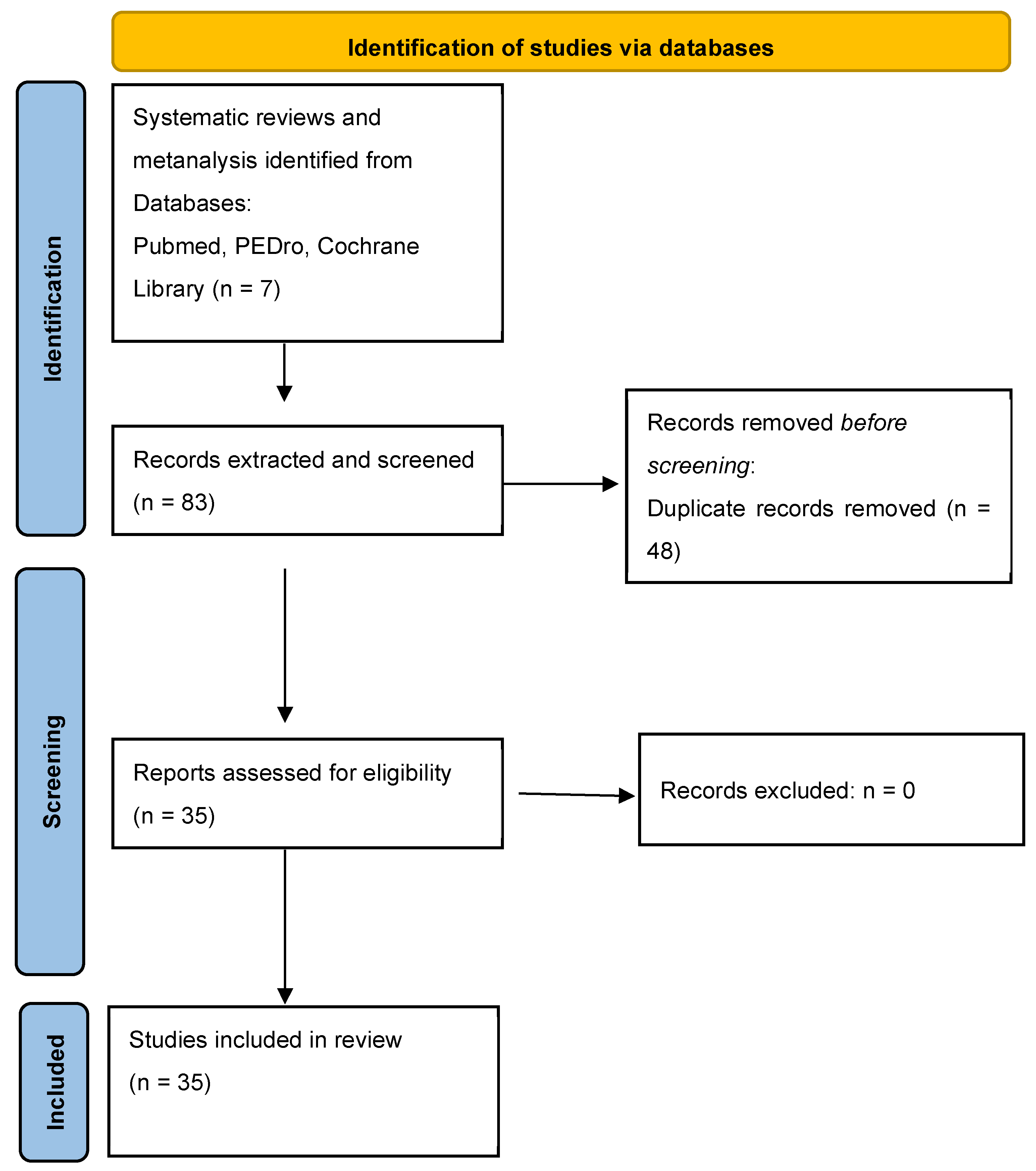
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Appendix A
| Reference | Study Design | Sample Size | Examiner Experience | Operator Experience with ESWT | Diagnostic Criteria of MPS | Diagnostic Criteria by Manual Palpation | Region of Application | Targeted Muscle | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Years | Qualification | Years | Qualification | |||||||
| Ali. 2016 [82] | RCT | 30 | n.m. | n.m. | n.m. | n.m. | n.m. | TrP | shoulder | Rot cuff |
| Anwar 2022 [83] | RCT | 45 | n.m. | Physiatrist | n.m. | Physiatrist | TrP | TrP | neck, shoulder | Up Trap |
| Aktürk 2018 [84] | RCT | 30 | n.m. | Medical Doctor | n.m. | Physiatrist | Trav-Simons | n.m. | n.m. | n.m. |
| Carlisi 2021 [85] | RCT | 55 | >5 | Rehab Specialist | >5 | Rehab Specialist | Trav Simons | n.m. | calf, foot | Gastroc, soleus |
| Cho 2012 [86] | RCT | 36 | n.m. | Orthopeadic Specialist | n.m. | n.m. | n.m. | n.m. | neck, shoulder | Up Trap |
| Damian 2011 [87] | RCT | 26 | n.m. | n.m. | n.m. | Physiotherapist | n.m. | TrP | neck, shoulder, head, TMJ | Temp, Mass, Trap, SCM, rhomb |
| Elhafez 2021 [89] | RCT | 60 | n.m. | n.m. | n.m. | n.m. | n.m. | TB, TrP, Ref, Rec | neck, shoulder | Up Trap |
| Elhafez 2022 [88] | RCT | 60 | n.m. | n.m. | n.m. | n.m. | n.m. | TrP, LT | neck, shoulder | Up Trap |
| Eftekharsadat 2020 [90] | RCT | 54 | n.m. | n.m. | n.m. | n.m. | Trav Simons | TB, TrP, Ref, LT | low back | Quad Lumb |
| Gezginaslan 2020 [91] | RCT | 94 | n.m. | n.m. | n.m. | n.m. | Trav Simons | TrP | neck, shoulder | Up Trap, infra, supra |
| Gur 2013 [92] | RCT | 60 | n.m. | Medical Doctor | n.m. | Physiotherapist | Trav Simons | TrP | neck, shoulder | Up Trap |
| Hong 2017 [93] | Retrospective study | 30 | n.m. | n.m. | n.m. | n.m. | Trav Simons | TB, TrP, Ref | lower back, | Quad Lomb |
| Huang 2014 [94] | RCT | 90 | n.m. | n.m. | n.m. | n.m. | n.m. | n.m. | neck, shoulder, lower back | n.m. |
| Ibrahim 2017 [95] | RCT | 30 | n.m. | n.m. | n.m. | n.m. | Trav Simons | TB, TrP, Ref | cervical | Up Trap |
| Jeon 2012 [80] | RCT | 30 | n.m. | n.m. | n.m. | n.m. | n.m. | TB, TrP, Ref, Rec | neck, shoulder | Up Trap |
| Ji 2012 [96] | RCT | 20 | n.m. | Medical Doctor | n.m. | Medical Doctor | Trav Simons | TB, TrP, Ref | neck, shoulder | Up Trap |
| Kamel 2020 [97] | RCT | 46 | n.m. | Orthopeadic Specialist | n.m. | n.m. | Trav Simons | TB, TrP, Ref | neck | Up Trap |
| Kiraly 2018 [98] | RCT | 61 | n.m. | n.m. | n.m. | n.m. | Trav Simons | TB, TrP, Ref | neck, shoulder | Up Trap |
| Lee 2012 [99] | RCT | 31 | n.m. | n.m. | n.m. | n.m. | Trav Simons | TB, Ref | neck, shoulder | Up Trap |
| Lee and Han 2013 [100] | RCT | 33 | n.m. | n.m. | n.m. | n.m. | Trav Simons | n.m. | neck, shoulder | Up Trap |
| Li 2020 [101] | RCT | 80 | n.m. | n.m. | n.m. | n.m. | n.m. | n.m. | TMJ | n.m. |
| Luan 2019 [102] | RCT | 65 | 20 | Clinician | n.m. | Physiotherapist | Trav Simons | TB, TrP, Ref, Rec, LT | neck, shoulder | Up Trap |
| Manafnezhad 2019 [103] | RCT | 70 | 5 | Physiotherapist | 5 | Physiotherapist | Trav Simons | TB, TrP, | neck, shoulder | Up Trap |
| Moghtaderi 2014 [104] | RCT | 40 | n.m. | n.m. | n.m. | n.m. | n.m. | TrP | foot, calf | Gastroc, soleus |
| Mohamed 2021 [105] | RCT | 60 | n.m. | n.m. | n.m. | n.m. | n.m. | TB, TrP | neck, shoulder | Up Trap |
| Park 2018 [106] | RCT | 30 | 3 | Physiatrist | >3 | Physiatrist | Trav Simons | TB, TrP, Ref, LT | neck, shoulder | Up Trap |
| Rahbar 2021 [107] | RCT | 48 | n.m. | Physiatrist | n.m. | Physiatrist | n.m. | TB, TrP, Ref | neck, shoulder | Up Trap, Mid Trap, lev scap, rot cuff |
| Sukareechai 2019 [108] | RCT | 42 | n.m. | n.m. | n.m. | n.m. | Trav Simons | TB, TrP, Ref, Rec | neck, shoulder | Up Trap, infra, rhomb |
| Sugawara 2021 [109] | Retrospective study | 1580 | n.m. | Physiatrist | n.m. | Physician | n.m. | n.m. | limbs | n.m. |
| Suputtitada 2022 [110] | RCT | 60 | >5 | Physiatrist | n.m. | n.m. | Trav Simons | TrP | neck, shoulder | Up Trap |
| Taheri 2016 [111] | RCT | 46 | n.m. | n.m. | n.m. | n.m. | Trav Simons | TB, TrP, Rec | neck, shoulder | Up Trap |
| Taheri 2021 [112] | RCT | 37 | n.m. | Physician | n.m. | Therapist | n.m. | TrP | neck, shoulder | Up Trap |
| Toghtamesh 2021 [113] | RCT | 16 | n.m. | Experienced Therapist | n.m. | n.m | n.m. | TB, TrP, Ref, Rec | neck, shoulder | Up Trap |
| Walsh 2019 [114] | RCT | 21 | 3 | Athletic Therapist | 2 | Athletic Therapist | Trav Simons | TB, TrP, latent TrP | lower limb | Vast Med, Vast Lat |
| Yalcin 2021 [115] | Retrospective study | 262 | n.m. | Physician | n.m. | Physician | Trav Simons | TrP | neck, upper back | Up Trap |
Appendix B
| Reference | Shockwave Device | Sessions | Interval Between Sessions (days) | Energy | Frequence (Hz) | Impulses/TrP | Impulses/session | Total Impulses | Diagnostic Criteria by Shockwave Application | Follow-up (Weeks After Last Session) |
|---|---|---|---|---|---|---|---|---|---|---|
| Ali. 2016 [82] | Radial | 3 | 7 | 0.38 mJ/mm2; 1.6 bar | 10 | <500 | 2000 | 6000 | TrP | 4 |
| Anwar 2022 [83] | Radial | 3 | 7 | 1.2 bar | 5 | 1000 | 1000 | 3000 | n.m. | 1 and 4 |
| Aktürk 2018 [84] | Radial | 4 | 3 | 6 bar | 4 | 200–400 | 2000–3000 | 8000–12,000 | n.m. | 6 |
| Carlisi 2021 [85] | Focused | 3 | 7 | 0.15 mJ/mm2 | 8 | 400 | 1200–1700 | 8700 | n.m. | 8 |
| Cho 2012 [86] | Radial | 12 | 2 | 0.12 bar | n.m. | 1000 | 1000 | 12,000 | n.m. | 0 |
| Damian 2011 [87] | Radial | 5–6 | 7 | n.m. | n.m. | n.m. | n.m. | n.m. | n.m. | 0 |
| Elhafez 2021 [89] | Radial | 4 | 7 | 1.5 bar | 1 | 300 | 300 | 1200 | TrP | 4 |
| Elhafez 2022 [88] | Radial | 4 | 3 | 0.056 mJ/mm2 | 10 | 400 | 700 | 2800 | TrP | 0 |
| Eftekharsadat 2020 [90] | Radial | 5 | 7 | 0.1 mJ/mm2 | 10–16 | 1500 | 1500 | 7500 | n.m. | 4 |
| Gezginaslan 2020 [91] | Radial | 7 | 3 | 1.5–3 bar | n.m. | 500 | 1500–4500 | 10,500–44,500 | TrP | 4 |
| Gur 2013 [92] | Focused | 3 | 3 | 0.25 mJ/mm2 | n.m. | n.m. | 1000 | 3000 | TrP | 3 and 12 |
| Hong 2017 [93] | Focused | 3 | 3 | 0.085–0.148 mJ/mm2 | n.m. | 2000 | 2000 | 6000 | TrP | 4 |
| Huang 2014 [94] | Focused | 30 | 3 | 0.18–0.25 mJ/mm2 | 1 | 700 | n.m | n.m. | TrP, Ref | 2.4 and 12 |
| Ibrahim 2017 [95] | Radial | 4 | 3 | 2.0–2.6 bar | 4–20 | 1000 | 2000 | 8000 | TrP | 4 |
| Jeon 2012 [80] | Focused | 3 | 7 | 0.10 mJ/mm2 | n.m. | n.m. | 1500 | 4500 | TrP, Ref, LT | 0 |
| Ji 2012 [96] | Focused | 4 | 3 | 0.056 mJ/mm2 | n.m. | 700 | 1000 | 4000 | TB | 0 |
| Kamel 2020 [97] | Focused | 4 | 7 | 0.25 mJ/mm2 | n.m. | 1000 | 1000 | 4000 | TrP | 4 |
| Kiraly 2018 [98] | Radial | 3 | 7 | 1.5–2.5 bar | 10 | 1000 | 2000 | 6000 | n.m. | 3 and 15 |
| Lee 2012 [99] | Radial | 2 | n.m. | n.m. | 5 | n.m | 800 | 1600 | n.m. | 0 |
| Lee and Han 2013 [100] | Radial | 8 | 4 | n.m. | 5 | 1000 | 1000 | 1000 | TrP | n.m. |
| Li 2020 [101] | Radial | 4 | 7 | n.m. | 8 | n.m. | 1000–1500 | 4000–6000 | n.m. | 4 |
| Luan 2019 [102] | Radial | 3 | 7 | 0.10 bar | n.m. | 1500 | 2000 | 6000 | TrP, LT | 4 and 12 |
| Manafnezhad 2019 [103] | Radial | 3 | 1 | 60 mJ | 16 | 1000 | 1000 | 3000 | n.m. | 1 |
| Moghtaderi 2014 [104] | Focused | 3 | 2 | 0.2 mJ/mm2 | n.m. | 400 | >3400 | >10,200 | TrP | 8 |
| Mohamed 2021 [105] | Radial | 4 | 7 | 1.5 bar | 8 | 1000 | 1000 | 4000 | n.m. | 4 |
| Park 2018 [106] | Focused | 2 | 7 | 0.068–0.21 mJ/mm2 | n.m. | 1500 | 1500 | 3000 | Ref, LT | 2 |
| Rahbar 2021 [107] | Radial | 4 | 7 | 60 mJ/m2 | 5 | 500–2000 | 2000 | 8000 | TrP | 1 and 4 |
| Sukareechai 2019 [108] | Radial | 3 | 7 | 1–2 bar | 12 | 300 | up to 6000 | up to 18,000 | TrP | 0 |
| Sugawara 2021 [109] | Radial | 2 | 7 | variable | variable | variable | variable | variable | n.m. | 1 |
| Suputtitada 2022 [110] | Radial | 3 | 7 | 2.5 bar | 12 | 2000 | 2000 | 6000 | TrP | 1 |
| Taheri 2016 [111] | Focused | 3 | 7 | 0.003 mJ/mm2 | 10 | n.m. | 1000 | 3000 | TrP | 4 |
| Taheri 2021 [112] | Focused | 3 | 7 | 0.2 mJ/mm2 | 10 | n.m. | 2000 | 6000 | TrP | 4 |
| Toghtamesh 2021 [113] | Radial | 1 | 0 | 0.038 mJ/mm2 | 10 | 700 | 1000 | 1000 | TB, TrP | 0 |
| Walsh 2019 [114] | Radial | 3 | 2 | up to 5 bar | 20 | 2000 | 3000 | 9000 | TrP | 1 |
| Yalcin 2021 [115] | Radial | 3 | 7 | 0.056 mJ/mm2 | n.m. | 1500 | 1500 | 4500 | TrP | 12 |
References
- Fede, C.; Petrelli, L.; Guidolin, D.; Porzionato, A.; Pirri, C.; Fan, C.; De Caro, R.; Stecco, C. Evidence of a new hidden neural network into deep fasciae. Sci. Rep. 2021, 11, 12623. [Google Scholar] [CrossRef]
- Tesarz, J.; Hoheisel, U.; Wiedenhöfer, B.; Mense, S. Sensory innervation of the thoracolumbar fascia in rats and humans. Neuroscience 2011, 194, 302–308. [Google Scholar] [CrossRef]
- Mense, S. Innervation of the thoracolumbar fascia. Eur. J. Transl. Myol. 2019, 29, 151–158. [Google Scholar] [CrossRef] [PubMed]
- Simons, D.G.; Travell, J.G.; Simons, L.S.; Travell, J.G. Travell & Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual, 2nd ed.; Williams & Wilkins: Philadelphia, PA, USA, 1999. [Google Scholar]
- Mense, S. Muscle pain: Mechanisms and clinical significance. Dtsch. Arztebl. Int. 2008, 105, 214–219. [Google Scholar] [CrossRef] [PubMed]
- Mense, S.; Simons, D.G.; Russell, I.J. Muscle Pain: Understanding Its Nature, Diagnosis, and Treatment; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2001. [Google Scholar]
- d’Agostino, M.C.; Craig, K.; Tibalt, E.; Respizzi, S. Shock wave as biological therapeutic tool: From mechanical stimulation to recovery and healing, through mechanotransduction. Int. J. Surg. 2015, 24, 147–153. [Google Scholar] [CrossRef]
- Moya, D.; Ramón, S.; Schaden, W.; Wang, C.J.; Guiloff, L.; Cheng, J.H. The Role of Extracorporeal Shockwave Treatment in Musculoskeletal Disorders. J. Bone Jt. Surg. 2018, 100, 251–263. [Google Scholar] [CrossRef]
- Ramon, S.; Gleitz, M.; Hernandez, L.; Romero, L.D. Update on the efficacy of extracorporeal shockwave treatment for myofascial pain syndrome and fibromyalgia. Int. J. Surg. 2015, 24, 201–206. [Google Scholar] [CrossRef]
- Yoo, J.I.; Oh, M.K.; Chun, S.W.; Lee, S.U.; Lee, C.H. The effect of focused extracorporeal shock wave therapy on myofascial pain syndrome of trapezius: A systematic review and meta-analysis. Medicine 2020, 99, e19085. [Google Scholar] [CrossRef]
- Paoletta, M.; Moretti, A.; Liguori, S.; Toro, G.; Gimigliano, F.; Iolascon, G. Efficacy and Effectiveness of Extracorporeal Shockwave Therapy in Patients with Myofascial Pain or Fibromyalgia: A Scoping Review. Medicina 2022, 58, 1014. [Google Scholar] [CrossRef]
- Wu, T.; Li, S.; Ren, J.; Wang, D.; Ai, Y. Efficacy of extracorporeal shock waves in the treatment of myofascial pain syndrome: A systematic review and meta-analysis of controlled clinical studies. Ann. Transl. Med. 2022, 10, 165. [Google Scholar] [CrossRef]
- Zhang, Q.; Fu, C.; Huang, L.; Xiong, F.; Peng, L.; Liang, Z.; Chen, L.; He, C.; Wei, Q. Efficacy of Extracorporeal Shockwave Therapy on Pain and Function in Myofascial Pain Syndrome of the Trapezius: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2020, 101, 1437–1446. [Google Scholar] [CrossRef]
- Avendaño-López, C.; Megía-García, Á.; Beltran-Alacreu, H.; Serrano-Muñoz, D.; Arroyo-Fernández, R.; Comino-Suárez, N.; Avendaño-Coy, J. Efficacy of Extracorporeal Shockwave Therapy on Pain and Function in Myofascial Pain Syndrome: A Systematic Review and Meta-analysis of Randomized Clinical Trials. Am. J. Phys. Med. Rehabil. 2024, 103, 89–98. [Google Scholar] [CrossRef]
- Jun, J.H.; Park, G.Y.; Chae, C.S.; Suh, D.C. The Effect of Extracorporeal Shock Wave Therapy on Pain Intensity and Neck Disability for Patients With Myofascial Pain Syndrome in the Neck and Shoulder: A Meta-Analysis of Randomized Controlled Trials. Am. J. Phys. Med. Rehabil. 2021, 100, 120–129. [Google Scholar] [CrossRef]
- Liu, C.; Wang, Y.; Yu, W.; Xiang, J.; Ding, G.; Liu, W. Comparative effectiveness of noninvasive therapeutic interventions for myofascial pain syndrome: A network meta-analysis of randomized controlled trials. Int. J. Surg. 2024, 110, 1099–1112. [Google Scholar] [CrossRef]
- Romeo, P.; Lavanga, V.; Pagani, D.; Sansone, V. Extracorporeal Shock Wave Therapy in Musculoskeletal Disorders: A Review. Med. Princ. Pract. 2014, 23, 7–13. [Google Scholar] [CrossRef]
- Wang, C.J. Extracorporeal shockwave therapy in musculoskeletal disorders. J. Orthop. Surg. Res. 2012, 7, 11. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, A.H. Myofascial Pain Disorders: Theory to Therapy. Drugs 2004, 64, 45–62. [Google Scholar] [CrossRef] [PubMed]
- Skootsky, S.A.; Jaeger, B.; Oye, R.K. Prevalence of myofascial pain in general internal medicine practice. West. J. Med. 1989, 151, 157–160. [Google Scholar]
- Galasso, A.; Urits, I.; An, D.; Nguyen, D.; Borchart, M.; Yazdi, C.; Manchikanti, L.; Kaye, R.J.; Kaye, A.D.; Mancuso, K.F.; et al. A Comprehensive Review of the Treatment and Management of Myofascial Pain Syndrome. Curr. Pain Headache Rep. 2020, 24, 43. [Google Scholar] [CrossRef] [PubMed]
- Simons, D.G.; Mense, S. Diagnosis and therapy of myofascial trigger points. Schmerz 2003, 17, 419–424. [Google Scholar] [CrossRef]
- Shah, J.P.; Thaker, N.; Heimur, J.; Aredo, J.V.; Sikdar, S.; Gerber, L. Myofascial Trigger Points Then and Now: A Historical and Scientific Perspective. Phys. Med. Rehabil. 2015, 7, 746–761. [Google Scholar] [CrossRef]
- Dommerholt, J.; Bron, C.; Franssen, J. Myofascial Trigger Points: An Evidence-Informed Review. J. Man. Manip. Ther. 2006, 14, 203–221. [Google Scholar] [CrossRef]
- Çelik, D.; Kaya Mutlu, E. The relationship between latent trigger points and depression levels in healthy subjects. Clin. Rheumatol. 2012, 31, 907–911. [Google Scholar] [CrossRef]
- Fernández-de-Las-Peñas, C.; Dommerholt, J. International Consensus on Diagnostic Criteria and Clinical Considerations of Myofascial Trigger Points: A Delphi Study. Pain Med. 2018, 19, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Gerwin, R.D.; Shannon, S.; Hong, C.Z.; Hubbard, D.; Gevirtz, R. Interrater reliability in myofascial trigger point examination. Pain 1997, 69, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Myburgh, C.; Larsen, A.H.; Hartvigsen, J. A Systematic, Critical Review of Manual Palpation for Identifying Myofascial Trigger Points: Evidence and Clinical Significance. Arch. Phys. Med. Rehabil. 2008, 89, 1169–1176. [Google Scholar] [CrossRef]
- Mazza, D.F.; Boutin, R.D.; Chaudhari, A.J. Assessment of Myofascial Trigger Points via Imaging: A Systematic Review. Am. J. Phys. Med. Rehabil. 2021, 100, 1003–1014. [Google Scholar] [CrossRef]
- Sikdar, S.; Shah, J.P.; Gebreab, T.; Yen, R.-H.; Gilliams, E.; Danoff, J.; Gerber, L.H. Novel Applications of Ultrasound Technology to Visualize and Characterize Myofascial Trigger Points and Surrounding Soft Tissue. Arch. Phys. Med. Rehabil. 2009, 90, 1829–1838. [Google Scholar] [CrossRef]
- Sollmann, N.; Mathonia, N.; Weidlich, D.; Bonfert, M.; Schroeder, S.A.; Badura, K.A.; Renner, T.; Trepte-Freisleder, F.; Ganter, C.; Krieg, S.M.; et al. Quantitative magnetic resonance imaging of the upper trapezius muscles—Assessment of myofascial trigger points in patients with migraine. J. Headache Pain 2019, 20, 8. [Google Scholar] [CrossRef]
- Zhang, X.F.; Liu, L.; Wang, B.B.; Liu, X.; Li, P. Evidence for kinesio taping in management of myofascial pain syndrome: A systematic review and meta-analysis. Clin. Rehabil. 2019, 33, 865–874. [Google Scholar] [CrossRef]
- Nouged, E.; Dajani, J.; Ku, B.; Al-Eryani, K.; Padilla, M.; Enciso, R. Local Anesthetic Injections for the Short-Term Treatment of Head and Neck Myofascial Pain Syndrome: A Systematic Review with Meta-Analysis. J. Oral Facial Pain Headache 2019, 33, 183–198. [Google Scholar] [CrossRef]
- Munguia, F.; Jang, J.; Salem, M.; Clark, G.; Enciso, R. Efficacy of Low-Level Laser Therapy in the Treatment of Temporomandibular Myofascial Pain: A Systematic Review and Meta-Analysis. J. Oral Facial Pain Headache 2018, 32, 287–297. [Google Scholar] [CrossRef]
- Xia, P.; Wang, X.; Lin, Q.; Cheng, K.; Li, X. Effectiveness of ultrasound therapy for myofascial pain syndrome: A systematic review and meta-analysis. J. Pain Res. 2017, 10, 545–555. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Mansilla, J.; González-Sánchez, B.; De Toro García, Á.; Valera-Donoso, E.; Garrido-Ardila, E.M.; Jiménez-Palomares, M.; López-Arza, M.V.G. Effectiveness of dry needling on reducing pain intensity in patients with myofascial pain syndrome: A Meta-analysis. J. Tradit. Chin. Med. 2016, 36, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Marcus, N.J. Failure to diagnose pain of muscular origin leads to unnecessary surgery. Pain Med. 2002, 3, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Barbero, M.; Schneebeli, A.; Koetsier, E.; Maino, P. Myofascial pain syndrome and trigger points: Evaluation and treatment in patients with musculoskeletal pain. Curr. Opin. Support. Palliat. Care 2019, 13, 270–276. [Google Scholar] [CrossRef]
- Chaussy, C.; Brendel, W.; Schmiedt, E. Extracorporeally induced destruction of kidney stones by shock waves. Lancet 1980, 316, 1265–1268. [Google Scholar] [CrossRef]
- Loew, M.; Jurgowski, W.; Mau, H.C.; Thomsen, M. Treatment of calcifying tendinitis of rotator cuff by extracorporeal shock waves: A preliminary report. J. Shoulder Elb. Surg. 1995, 4, 101–106. [Google Scholar] [CrossRef]
- Holfeld, J.; Tepeköylü, C.; Kozaryn, R.; Urbschat, A.; Zacharowski, K.; Grimm, M.; Paulus, P. Shockwave Therapy Differentially Stimulates Endothelial Cells: Implications on the Control of Inflammation via Toll-Like Receptor 3. Inflammation 2014, 37, 65–70. [Google Scholar] [CrossRef]
- Cui, H.; Hong, A.R.; Kim, J.B.; Yu, J.H.; Cho, Y.S.; Joo, S.Y.; Seo, C.H. Extracorporeal Shock Wave Therapy Alters the Expression of Fibrosis-Related Molecules in Fibroblast Derived from Human Hypertrophic Scar. Int. J. Mol. Sci. 2018, 19, 124. [Google Scholar] [CrossRef]
- Hausner, T.; Nógrádi, A. The Use of Shock Waves in Peripheral Nerve Regeneration. In International Review of Neurobiology; Elsevier: Amsterdam, The Netherlands, 2013; Volume 109, pp. 85–98. [Google Scholar] [CrossRef]
- Wang, C.; Wang, F.; Yang, K.D.; Weng, L.; Hsu, C.; Huang, C.; Yang, L. Shock wave therapy induces neovascularization at the tendon–bone junction. A study in rabbits. J. Orthop. Res. 2003, 21, 984–989. [Google Scholar] [CrossRef]
- Ogden, J.A.; Tóth-Kischkat, A.; Schultheiss, R. Principles of Shock Wave Therapy. Clin. Orthop. Relat. Res. 2001, 387, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Katz, J.E.; Clavijo, R.I.; Rizk, P.; Ramasamy, R. The Basic Physics of Waves, Soundwaves, and Shockwaves for Erectile Dysfunction. Sex. Med. Rev. 2020, 8, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Cleveland, R.O.; Chitnis, P.V.; McClure, S.R. Acoustic Field of a Ballistic Shock Wave Therapy Device. Ultrasound Med. Biol. 2007, 33, 1327–1335. [Google Scholar] [CrossRef]
- Auersperg, V.; Trieb, K. Extracorporeal shock wave therapy: An update. EFORT Open Rev. 2020, 5, 584–592. [Google Scholar] [CrossRef]
- Yan, X.; Zeng, B.; Chai, Y.; Luo, C.; Li, X. Improvement of Blood Flow, Expression of Nitric Oxide, and Vascular Endothelial Growth Factor by Low-Energy Shockwave Therapy in Random-Pattern Skin Flap Model. Ann. Plast. Surg. 2008, 61, 646–653. [Google Scholar] [CrossRef]
- Antonic, V.; Mittermayr, R.; Schaden, W.; Stojadinovic, A. Evidence supporting extracorporeal shock wave therapy for acute and chronic soft tissue wounds. Wounds 2011, 23, 204–215. [Google Scholar]
- D’Agostino, M.C.; Frairia, R.; Romeo, P.; Amelio, E. Extracorporeal shockwaves as regenerative therapy in orthopedic traumatology: A narrative review from basic research to clinical practice. J. Biol. Regul. Homeost. Agents 2016, 30, 323–332. [Google Scholar]
- Wang, F.S.; Yang, K.D.; Chen, R.F.; Wang, C.J.; Sheen-Chen, S.M. Extracorporeal shock wave promotes growth and differentiation of bone-marrow stromal cells towards osteoprogenitors associated with induction of TGF-β1. J. Bone Jt. Surg. Br. 2002, 84, 457–461. [Google Scholar] [CrossRef]
- Suhr, F.; Delhasse, Y.; Bungartz, G.; Schmidt, A.; Pfannkuche, K.; Bloch, W. Cell biological effects of mechanical stimulations generated by focused extracorporeal shock wave applications on cultured human bone marrow stromal cells. Stem Cell Res. 2013, 11, 951–964. [Google Scholar] [CrossRef]
- Sukubo, N.G.; Tibalt, E.; Respizzi, S.; Locati, M.; d’Agostino, M.C. Effect of shock waves on macrophages: A possible role in tissue regeneration and remodeling. Int. J. Surg. 2015, 24, 124–130. [Google Scholar] [CrossRef]
- Hausdorf, J.; Lemmens, M.A.M.; Kaplan, S.; Marangoz, C.; Milz, S.; Odaci, E.; Korr, H.; Schmitz, C.; Maier, M. Extracorporeal shockwave application to the distal femur of rabbits diminishes the number of neurons immunoreactive for substance P in dorsal root ganglia L5. Brain Res. 2008, 1207, 96–101. [Google Scholar] [CrossRef]
- Maier, M.; Averbeck, B.; Milz, S.; Refior, H.J.; Schmitz, C. Substance P and prostaglandin E2 release after shock wave application to the rabbit femur. Clin. Orthop. Relat. Res. 2003, 406, 237–245. [Google Scholar] [CrossRef]
- Takahashi, N.; Wada, Y.; Ohtori, S.; Saisu, T.; Moriya, H. Application of shock waves to rat skin decreases calcitonin gene-related peptide immunoreactivity in dorsal root ganglion neurons. Auton. Neurosci. 2003, 107, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Adstrum, S.; Hedley, G.; Schleip, R.; Stecco, C.; Yucesoy, C.A. Defining the fascial system. J. Bodyw. Mov. Ther. 2017, 21, 173–177. [Google Scholar] [CrossRef] [PubMed]
- Klingler, W.; Jurkat-Rott, K.; Lehmann-Horn, F.; Schleip, R. The role of fibrosis in Duchenne muscular dystrophy. Acta Myol. 2012, 31, 184–195. [Google Scholar] [PubMed]
- DeLeon-Pennell, K.Y.; Barker, T.H.; Lindsey, M.L. Fibroblasts: The arbiters of extracellular matrix remodeling. Matrix Biol. 2020, 91–92, 1–7. [Google Scholar] [CrossRef]
- Frairia, R.; Berta, L. Biological effects of extracorporeal shock waves on fibroblasts. A review. Muscles Ligaments Tendons J. 2011, 1, 138–147. [Google Scholar]
- Aschermann, I.; Noor, S.; Venturelli, S.; Sinnberg, T.; Busch, C.; Mnich, C.D. Extracorporal Shock Waves Activate Migration, Proliferation and Inflammatory Pathways in Fibroblasts and Keratinocytes, and Improve Wound Healing in an Open-Label, Single-Arm Study in Patients with Therapy-Refractory Chronic Leg Ulcers. Cell. Physiol. Biochem. 2017, 41, 890–906. [Google Scholar] [CrossRef]
- Pirri, C.; Fede, C.; Petrelli, L.; De Rose, E.; Biz, C.; Guidolin, D.; De Caro, R.; Stecco, C. Immediate Effects of Extracorporeal Shock Wave Therapy in Fascial Fibroblasts: An In Vitro Study. Biomedicines 2022, 10, 1732. [Google Scholar] [CrossRef]
- Gollmann-Tepeköylü, C.; Lobenwein, D.; Theurl, M.; Primessnig, U.; Lener, D.; Kirchmair, E.; Mathes, W.; Graber, M.; Pölzl, L.; An, A.; et al. Shock Wave Therapy Improves Cardiac Function in a Model of Chronic Ischemic Heart Failure: Evidence for a Mechanism Involving VEGF Signaling and the Extracellular Matrix. J. Am. Hear. Assoc. 2018, 7, e010025. [Google Scholar] [CrossRef] [PubMed]
- Moortgat, P.; Anthonissen, M.; Van Daele, U.; Meirte, J.; Vanhullebusch, T.; Maertens, K. Shock Wave Therapy for Wound Healing and Scar Treatment. In Textbook on Scar Management; Téot, L., Mustoe, T.A., Middelkoop, E., Gauglitz, G.G., Eds.; Springer International Publishing: Berlin/Heidelberg, Germany, 2020; pp. 485–490. [Google Scholar] [CrossRef]
- Knobloch, K.; Kuehn, M.; Vogt, P.M. Focused extracorporeal shockwave therapy in Dupuytren’s disease—A hypothesis. Med. Hypotheses 2011, 76, 635–637. [Google Scholar] [CrossRef] [PubMed]
- Fulceri, F.; Ryskalin, L.; Morucci, G.; Busoni, F.; Soldani, P.; Gesi, M. Pain-Relieving Effects of Shockwave Therapy for Ledderhose Disease: An Ultrasound-Based Study of an Unusual Bilateral Case. Life 2024, 14, 169. [Google Scholar] [CrossRef]
- Mazin, Y.; Lemos, C.; Paiva, C.; Amaral Oliveira, L.; Borges, A.; Lopes, T. The Role of Extracorporeal Shock Wave Therapy in the Treatment of Muscle Injuries: A Systematic Review. Cureus 2023, 15, e44196. [Google Scholar] [CrossRef]
- Rinella, L.; Marano, F.; Berta, L.; Bosco, O.; Fraccalvieri, M.; Fortunati, N.; Frairia, R.; Catalano, M.G. Extracorporeal shock waves modulate myofibroblast differentiation of adipose-derived stem cells. Wound Repair Regen. 2016, 24, 275–286. [Google Scholar] [CrossRef]
- Saggini, R.; Saggini, A.; Spagnoli, A.M.; Dodaj, I.; Cigna, E.; Maruccia, M.; Soda, G.; Bellomo, R.G.; Scuderi, N. Extracorporeal Shock Wave Therapy: An Emerging Treatment Modality for Retracting Scars of the Hands. Ultrasound Med. Biol. 2016, 42, 185–195. [Google Scholar] [CrossRef]
- Stecco, C.; Fede, C.; Macchi, V.; Dodaj, I.; Cigna, E.; Maruccia, M.; Soda, G.; Bellomo, R.G.; Scuderi, N. The fasciacytes: A new cell devoted to fascial gliding regulation. Clin. Anat. 2018, 31, 667–676. [Google Scholar] [CrossRef]
- Wang, C.J.; Wang, F.S.; Yang, K.D. Biological effects of extracorporeal shockwave in bone healing: A study in rabbits. Arch. Orthop. Trauma Surg. 2008, 128, 879–884. [Google Scholar] [CrossRef]
- Shah, J.P.; Phillips, T.M.; Danoff, J.V.; Gerber, L.H. An in vivo microanalytical technique for measuring the local biochemical milieu of human skeletal muscle. J. Appl. Physiol. 2005, 99, 1977–1984. [Google Scholar] [CrossRef]
- Liu, K.; Zhang, Q.; Chen, L.; Zhang, H.; Xu, X.; Yuan, Z.; Dong, J. Efficacy and safety of extracorporeal shockwave therapy in chronic low back pain: A systematic review and meta-analysis of 632 patients. J. Orthop. Surg. Res. 2023, 18, 455. [Google Scholar] [CrossRef]
- Lohse-Busch, H.; Kraemer, M.; Reime, U. A pilot investigation into the effects of extracorporeal shock waves on muscular dysfunction in children with spastic movement disorders. Schmerz 1997, 11, 108–112. [Google Scholar] [CrossRef] [PubMed]
- Manganotti, P.; Amelio, E. Long-Term Effect of Shock Wave Therapy on Upper Limb Hypertonia in Patients Affected by Stroke. Stroke 2005, 36, 1967–1971. [Google Scholar] [CrossRef] [PubMed]
- Fleckenstein, J.; Friton, M.; Himmelreich, H.; Banzer, W. Effect of a Single Administration of Focused Extracorporeal Shock Wave in the Relief of Delayed-Onset Muscle Soreness: Results of a Partially Blinded Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2017, 98, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Zissler, A.; Steinbacher, P.; Zimmermann, R.; Zhang, H.; Xu, X.; Yuan, Z.; Dong, J. Extracorporeal Shock Wave Therapy Accelerates Regeneration After Acute Skeletal Muscle Injury. Am. J. Sports Med. 2017, 45, 676–684. [Google Scholar] [CrossRef]
- Astur, D.C.; Santos, B.; Moraes, E.R.D.; Arliani, G.G.; Santos, P.R.D.D.; Pochini, A.D.C. Extracorporeal shockwave terapy to treat chronic muscle injury. Acta Ortop. Bras. 2015, 23, 247–250. [Google Scholar] [CrossRef]
- Jeon, J.H.; Jung, Y.J.; Lee, J.Y.; Choi, J.S.; Mun, J.H.; Park, W.Y.; Seo, C.H.; Jang, K.U. The Effect of Extracorporeal Shock Wave Therapy on Myofascial Pain Syndrome. Ann. Rehabil. Med. 2012, 36, 665. [Google Scholar] [CrossRef]
- Kong, L.; Tian, X.; Yao, X. Effects of extracorporeal shock wave therapy on chronic low back pain and quality of life. Minerva Surg. 2023, 78, 305–306. [Google Scholar] [CrossRef]
- Ali, S.A.; Lasheen, Y.R.; Kamel, R.M.; Genaidy, A.F. Efficacy of shockwave therapy in treatment of myofascial trigger points of rotator cuff muscle dysfunction. Int. J. PharmTech Res. 2016, 9, 115–126. [Google Scholar]
- Anwar, N.; Li, S.; Long, L.; Zhou, L.; Fan, M.; Zhou, Y.; Wang, S.; Yu, L. Combined effectiveness of extracorporeal radial shockwave therapy and ultrasound-guided trigger point injection of lidocaine in upper trapezius myofascial pain syndrome. Am. J. Transl. Res. 2022, 14, 182–196. [Google Scholar]
- Aktürk, S.; Kaya, A.; Çetintaş, D.; Akgöl, G.; Gülkesen, A.; Kal, G.A.; Güçer, T. Comparision of the effectiveness of ESWT and ultrasound treatments in myofascial pain syndrome: Randomized, sham-controlled study. J. Phys. Ther. Sci. 2018, 30, 448–453. [Google Scholar] [CrossRef]
- Carlisi, E.; Manzoni, F.; Maestri, G.; Boschi, L.M.R.; Lisi, C. Short-Term Outcome of Focused Shock Wave Therapy for Sural Myofascial Pain Syndrome associated with Plantar Fasciitis: A Randomized Controlled. Muscle Ligaments Tendons J. 2021, 11, 517. [Google Scholar] [CrossRef]
- Cho, Y.S.; Park, S.J.; Jang, S.H.; Choi, Y.C.; Lee, J.H.; Kim, J.S. Effects of the Combined Treatment of Extracorporeal Shock Wave Therapy (ESWT) and Stabilization Exercises on Pain and Functions of Patients with Myofascial Pain Syndrome. J. Phys. Ther. Sci. 2012, 24, 1319–1323. [Google Scholar] [CrossRef]
- Damian, M.; Zalpour, C. Trigger point treatment with radial shock waves in musicians with nonspecific shoulder-neck pain: Data from a special physio outpatient clinic for musicians. Med. Probl. Perform. Art. 2011, 26, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Elhafez, H.; Abu El Kasem, S.; Abdelhay, M. Effect of high-power pain threshold ultrasound versus extracorporeal shock wave on upper trapezius myofascial trigger points. Egypt. J. Chem. 2022, 65, 473–479. [Google Scholar] [CrossRef]
- Elhafez, H.; Sayed, B.; Grace, M. Effect of Extracorporeal Shock ave versus high power pain threshold ultrasound in treating myofascial trigger point in upper trapezius. Int. J. Recent Adv. Multidiscip. Res. 2021, 8, 7043–7047. [Google Scholar]
- Eftekharsadat, B.; Fasaie, N.; Golalizadeh, D.; Babaei-Ghazani, A.; Jahanjou, F.; Eslampoor, Y.; Dolatkhah, N. Comparison of efficacy of corticosteroid injection versus extracorporeal shock wave therapy on inferior trigger points in the quadratus lumborum muscle: A randomized clinical trial. BMC Musculoskelet. Disord. 2020, 21, 695. [Google Scholar] [CrossRef]
- Gezginaslan, Ö. High-Energy Flux Density Extracorporeal Shock Wave Therapy Versus Traditional Physical Therapy Modalities in Myofascial Pain Syndrome: A Randomized-controlled, Single-Blind Trial. Arch. Rheumatol. 2020, 35, 78–89. [Google Scholar] [CrossRef]
- Gur, A.; Koca, I.; Karagullu, H.; Altindag, O.; Madenci, E. Comparison of the Efficacy of Ultrasound and Extracorporeal Shock Wave Therapies in Patients with Myofascial Pain Syndrome: A Randomized Controlled Study. J. Musculoskelet. Pain 2013, 21, 210–216. [Google Scholar] [CrossRef]
- Hong, J.O.; Park, J.S.; Jeon, D.G.; Yoon, W.H.; Park, J.H. Extracorporeal Shock Wave Therapy Versus Trigger Point Injection in the Treatment of Myofascial Pain Syndrome in the Quadratus Lumborum. Ann. Rehabil. Med. 2017, 41, 582–588. [Google Scholar] [CrossRef]
- Huang, F.; Chen, X.; Mu, J. Clinical study on extracorporeal shock wave therapy plus electroacupuncture for myofascial pain syndrome. J. Acupunct. Tuina Sci. 2014, 12, 55–59. [Google Scholar] [CrossRef]
- Ibrahim, D.; Amin, D.; Raoof, P. Shock Wave Therapy versus Progressive Pressure Release on myofascial trigger points. Int. J. Ther. Rehabil. Res. 2017, 6, 5. [Google Scholar] [CrossRef]
- Ji, H.M.; Kim, H.J.; Han, S.J. Extracorporeal shock wave therapy in myofascial pain syndrome of upper trapezius. Ann. Rehabil. Med. 2012, 36, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Kamel, F.H.; Basha, M.; Alsharidah, A.; Hewidy, I.M.; Ezzat, M.; Aboelnour, N.H. Efficacy of Extracorporeal Shockwave Therapy on Cervical Myofascial Pain Following Neck Dissection Surgery: A Randomized Controlled Trial. Ann. Rehabil. Med. 2020, 44, 393–401. [Google Scholar] [CrossRef] [PubMed]
- Király, M.; Bender, T.; Hodosi, K. Comparative study of shockwave therapy and low-level laser therapy effects in patients with myofascial pain syndrome of the trapezius. Rheumatol. Int. 2018, 38, 2045–2052. [Google Scholar] [CrossRef]
- Lee, J.H.; Jang, S.H.; Cho, S.H.; Kim, J.S. Comparison of Extracorporeal Shock Wave Therapy and Trigger Point Injection in Terms of Their Effects on Pain and Bodily Functions of Myofascial Pain Syndrome Patients. J. Phys. Ther. Sci. 2012, 24, 1069–1072. [Google Scholar] [CrossRef][Green Version]
- Lee, J.H.; Han, E.Y. A Comparison of the Effects of PNF, ESWT, and TPI on Pain and Function of Patients with Myofascial Pain Syndrome. J. Phys. Ther. Sci. 2013, 25, 341–344. [Google Scholar] [CrossRef]
- Li, W.; Wu, J. Treatment of Temporomandibular Joint Disorders by Ultrashort Wave and Extracorporeal Shock Wave: A Comparative Study. Med. Sci. Monit. 2020, 26, e923461. [Google Scholar] [CrossRef]
- Luan, S.; Zhu, Z.M.; Ruan, J.L.; Lin, C.-N.; Ke, S.-J.; Xin, W.-J.; Liu, C.-C.; Wu, S.-L.; Ma, C. Randomized Trial on Comparison of the Efficacy of Extracorporeal Shock Wave Therapy and Dry Needling in Myofascial Trigger Points. Am. J. Phys. Med. Rehabil. 2019, 98, 677–684. [Google Scholar] [CrossRef]
- Manafnezhad, J.; Salahzadeh, Z.; Salimi, M.; Ghaderi, F.; Ghojazadeh, M. The effects of shock wave and dry needling on active trigger points of upper trapezius muscle in patients with non-specific neck pain: A randomized clinical trial. BMR 2019, 32, 811–818. [Google Scholar] [CrossRef]
- Moghtaderi, A.; Khosrawi, S.; Dehghan, F. Extracorporeal shock wave therapy of gastroc-soleus trigger points in patients with plantar fasciitis: A randomized, placebo-controlled trial. Adv. Biomed. Res. 2014, 3, 99. [Google Scholar] [CrossRef]
- Mohamed, D.A.A.; Kamal, R.M.; Gaber, M.M.; Aneis, Y.M. Combined Effects of Extracorporeal Shockwave Therapy and Integrated Neuromuscular Inhibition on Myofascial Trigger Points of Upper Trapezius: A Randomized Controlled Trial. Ann. Rehabil. Med. 2021, 45, 284–293. [Google Scholar] [CrossRef]
- Park, K.D.; Lee, W.Y.; Park, M.-H.; Ahn, J.K.; Park, Y. High- versus low-energy extracorporeal shock-wave therapy for myofascial pain syndrome of upper trapezius: A prospective randomized single blinded pilot study. Medicine 2018, 97, e11432. [Google Scholar] [CrossRef] [PubMed]
- Rahbar, M.; Samandarian, M.; Salekzamani, Y.; Khamnian, Z.; Dolatkhah, N. Effectiveness of extracorporeal shock wave therapy versus standard care in the treatment of neck and upper back myofascial pain: A single blinded randomised clinical trial. Clin. Rehabil. 2021, 35, 102–113. [Google Scholar] [CrossRef]
- Sukareechai, C.; Sukareechai, S. Comparison of radial shockwave and dry needling therapies in the treatment of myofascial pain syndrome. Int. J. Ther. Rehabil. 2019, 26, 1–8. [Google Scholar] [CrossRef]
- Sugawara, A.T.; Lima, M.D.C.; Dias, C.B. Predictive factors of response in radial Extracorporeal Shock-waves Therapy for Myofascial and Articular Pain: A retrospective cohort study. BMR 2021, 34, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Suputtitada, A.; Chen, C.P.C.; Ngamrungsiri, N.; Schmitz, C. Effects of Repeated Injection of 1% Lidocaine vs. Radial Extracorporeal Shock Wave Therapy for Treating Myofascial Trigger Points: A Randomized Controlled Trial. Medicina 2022, 58, 479. [Google Scholar] [CrossRef]
- Taheri, P.; Vahdatpour, B.; Andalib, S. Comparative study of shock wave therapy and Laser therapy effect in elimination of symptoms among patients with myofascial pain syndrome in upper trapezius. Adv. Biomed. Res. 2016, 5, 138. [Google Scholar] [CrossRef]
- Taheri, P.; Naderi, M.; Khosravi, S. Extracorporeal Shock Wave Therapy Versus Phonophoresis Therapy for Neck Myofascial Pain Syndrome: A Randomized Clinical Trial. Anesth. Pain. Med. 2021, 11, e112592. [Google Scholar] [CrossRef]
- Toghtamesh, M.; Bashardoust Tajali, S.; Jalaei, S. Comparing Between the Effects of Dry Needling and Shock Wave in the Treatment of Trapezius Myofascial Pain. J. Mod. Rehabil. 2021, 14, 225–232. [Google Scholar] [CrossRef]
- Walsh, R.; Kinsella, S.; McEvoy, J. The effects of dry needling and radial extracorporeal shockwave therapy on latent trigger point sensitivity in the quadriceps: A randomised control pilot study. J. Bodyw. Mov. Ther. 2019, 23, 82–88. [Google Scholar] [CrossRef]
- Yalçın, Ü. Comparison of the effects of extracorporeal shockwave treatment with kinesiological taping treatments added to exercise treatment in myofascial pain syndrome. BMR 2021, 34, 623–630. [Google Scholar] [CrossRef]
- Tough, E.A.; White, A.R.; Richards, S.; Campbell, J. Variability of Criteria Used to Diagnose Myofascial Trigger Point Pain Syndrome—Evidence From a Review of the Literature. Clin. J. Pain 2007, 23, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Stoop, R.; Clijsen, R.; Hohenauer, E.; Fernández-De-Las-Peñas, C.; Huang, Q.; Barbero, M. Criteria Used for the Diagnosis of Myofascial Trigger Points in Clinical Trials on Physical Therapy: Updated Systematic Review. Clin. J. Pain 2020, 36, 955–967. [Google Scholar] [CrossRef] [PubMed]
- Sciotti, V.M.; Mittak, V.L.; DiMarco, L.; Ford, L.M.; Plezbert, J.; Santipadri, E.; Wigglesworth, J.; Ball, K. Clinical precision of myofascial trigger point location in the trapezius muscle. Pain 2001, 93, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Fernández-de-las-Peñas, C.; Ge, H.; Arendt-Nielsen, L.; Cuadrado, M.L.; Pareja, J.A. Referred pain from trapezius muscle trigger points shares similar characteristics with chronic tension type headache. Eur. J. Pain 2007, 11, 475–482. [Google Scholar] [CrossRef]
- Licht, G.; Müller-Ehrenberg, H.; Mathis, J.; Berg, G.; Greitemann, G. Untersuchung myofaszialer Triggerpunkte ist zuverlässig: Intertester-Reliabilität an insgesamt 304 Muskeln überprüft. Man. Med. 2007, 45, 402–408. [Google Scholar] [CrossRef]
- Myburgh, C.; Lauridsen, H.H.; Larsen, A.H.; Hartvigsen, J. Standardized manual palpation of myofascial trigger points in relation to neck/shoulder pain; the influence of clinical experience on inter-examiner reproducibility. Man. Ther. 2011, 16, 136–140. [Google Scholar] [CrossRef]
- Tenforde, A.S.; Borgstrom, H.E.; DeLuca, S.; McCormack, M.; Singh, M.; Hoo, J.S.; Yun, P.H. Best practices for extracorporeal shockwave therapy in musculoskeletal medicine: Clinical application and training consideration. Phys. Med. Rehabil. 2022, 14, 611–619. [Google Scholar] [CrossRef]
- Tognolo, L.; Giordani, F.; Biz, C.; Bernini, A.; Ruggieri, P.; Stecco, C.; Frigo, A.C.; Masiero, S. Myofascial points treatment with focused extracorporeal shock wave therapy (f-ESWT) for plantar fasciitis: An open label randomized clinical trial. Eur. J. Phys. Rehabil. Med. 2022, 58, 85–93. [Google Scholar] [CrossRef]
- Giordani, F.; Bernini, A.; Müller-Ehrenberg, H.; Stecco, C.; Masiero, S. A global approach for plantar fasciitis with extracorporeal shockwaves treatment. Eur. J. Transl. Myol. 2019, 29, 8372. [Google Scholar] [CrossRef]
- Gleitz, M.; Hornig, K. Triggerpunkte—Diagnose und Behandlungskonzepte unter besonderer Berücksichtigung extrakorporaler Stoßwellen. Orthopäde 2012, 41, 113–125. [Google Scholar] [CrossRef]
- Müller-Ehrenberg, H.; Licht, G. Diagnostik Und Therapie von Myofaszialen Schmerzsyndromen Mittels Der Fokussierten Stoßwelle (ESWT). MOT 2005, 5, 75–82. [Google Scholar]
- Müller-Ehrenberg, H.; Giordani, F.; Müller-Ehrenberg, A.; Stange, R. The Use and Benefits of Focused Shockwaves for the Diagnosis of Myofascial Pain Syndrome by Examining Myofascial Trigger Points in Low Back Pain. Biomedicines 2024, 12, 2909. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Müller-Ehrenberg, H.; Bonavita, J.; Sun, Y.; Stecco, C.; Giordani, F. The State of Extracorporeal Shockwave Therapy for Myofascial Pain Syndrome—A Scoping Review and a Call for Standardized Protocols. Life 2025, 15, 1501. https://doi.org/10.3390/life15101501
Müller-Ehrenberg H, Bonavita J, Sun Y, Stecco C, Giordani F. The State of Extracorporeal Shockwave Therapy for Myofascial Pain Syndrome—A Scoping Review and a Call for Standardized Protocols. Life. 2025; 15(10):1501. https://doi.org/10.3390/life15101501
Chicago/Turabian StyleMüller-Ehrenberg, Hannes, Jacopo Bonavita, Yunfeng Sun, Carla Stecco, and Federico Giordani. 2025. "The State of Extracorporeal Shockwave Therapy for Myofascial Pain Syndrome—A Scoping Review and a Call for Standardized Protocols" Life 15, no. 10: 1501. https://doi.org/10.3390/life15101501
APA StyleMüller-Ehrenberg, H., Bonavita, J., Sun, Y., Stecco, C., & Giordani, F. (2025). The State of Extracorporeal Shockwave Therapy for Myofascial Pain Syndrome—A Scoping Review and a Call for Standardized Protocols. Life, 15(10), 1501. https://doi.org/10.3390/life15101501







