Laparoscopic and Open Distal Pancreatectomy—An Initial Single-Institution Experience with a Propensity Score Matching Analysis
Abstract
1. Introduction
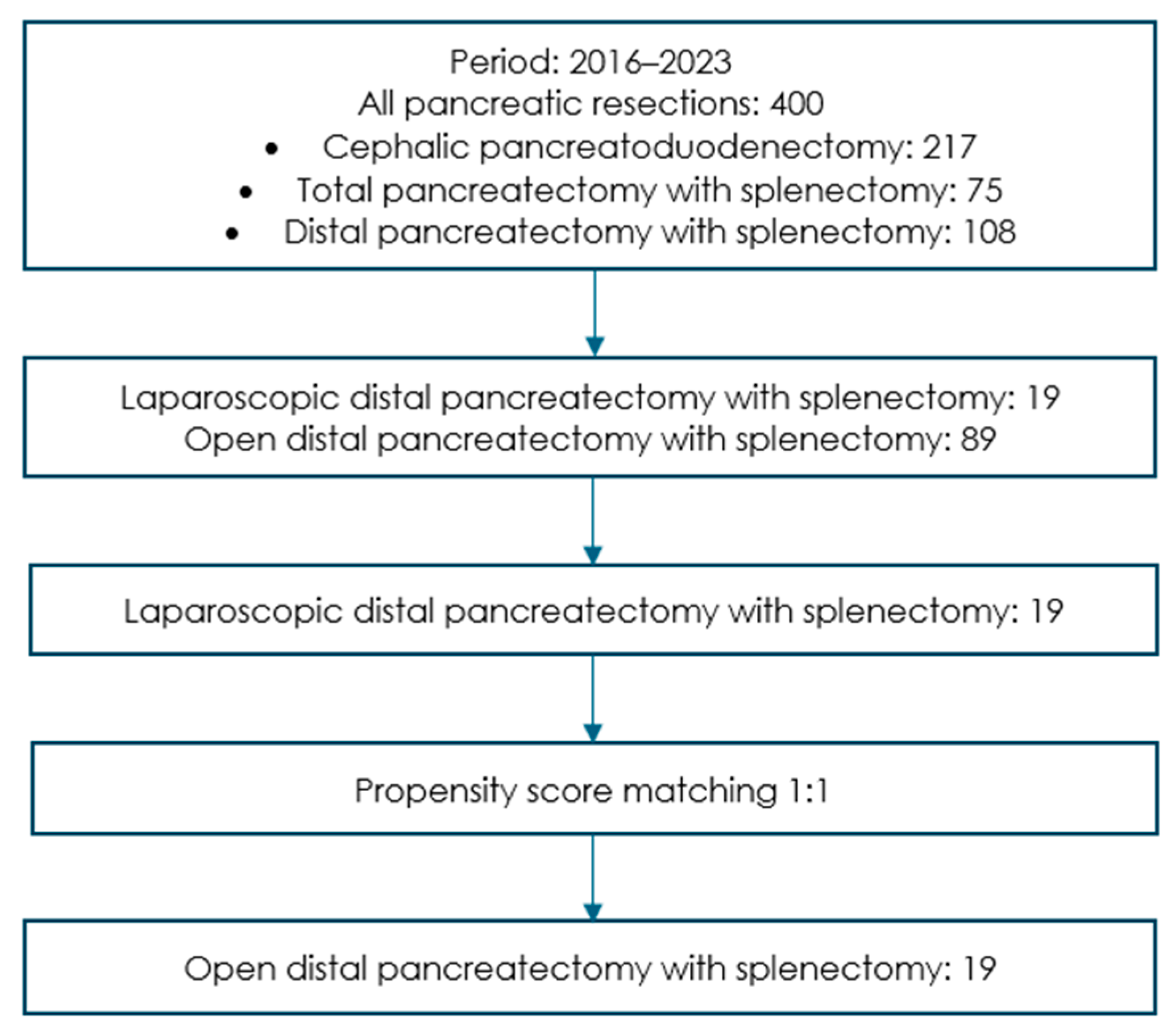
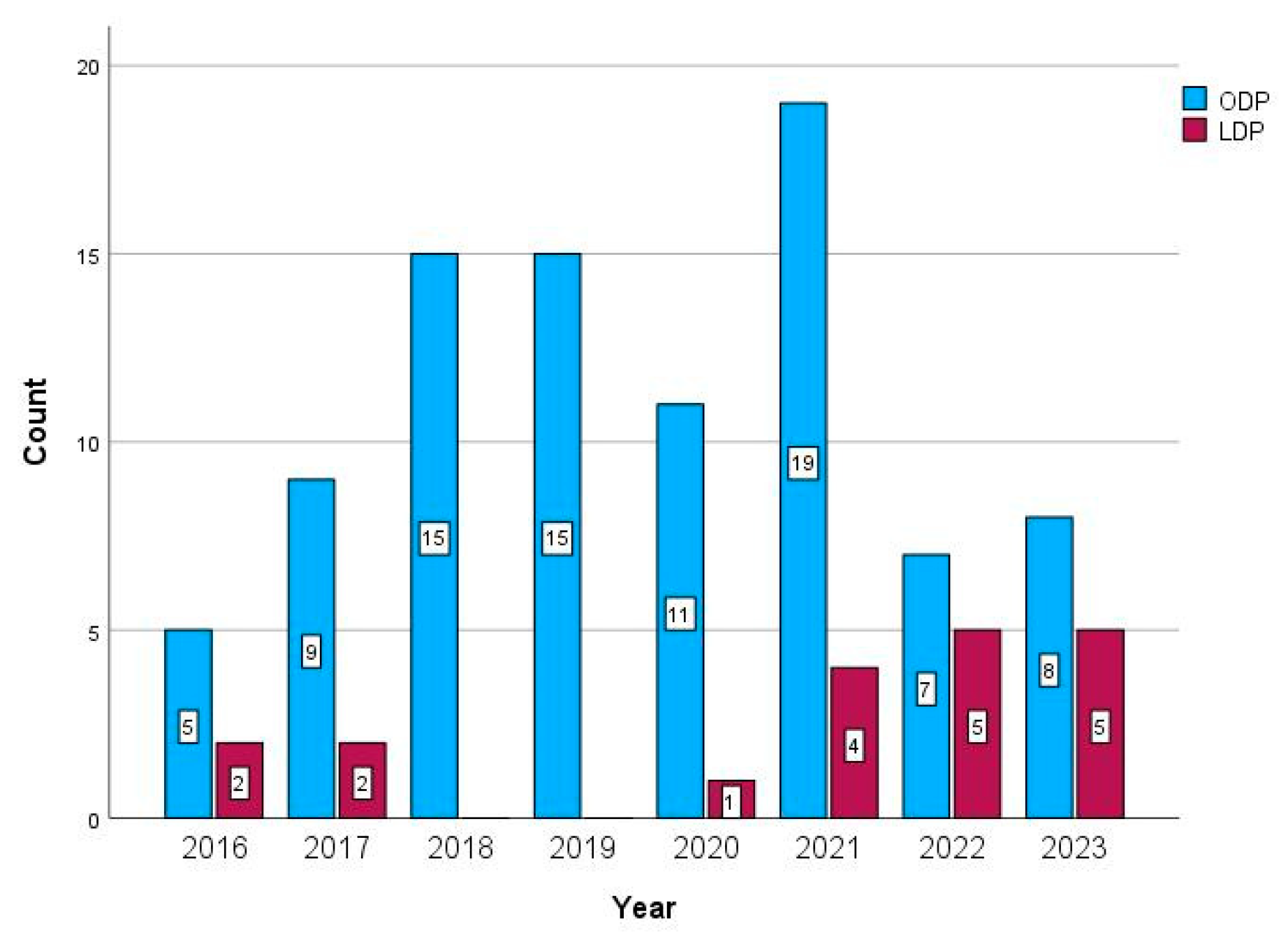
2. Materials and Methods
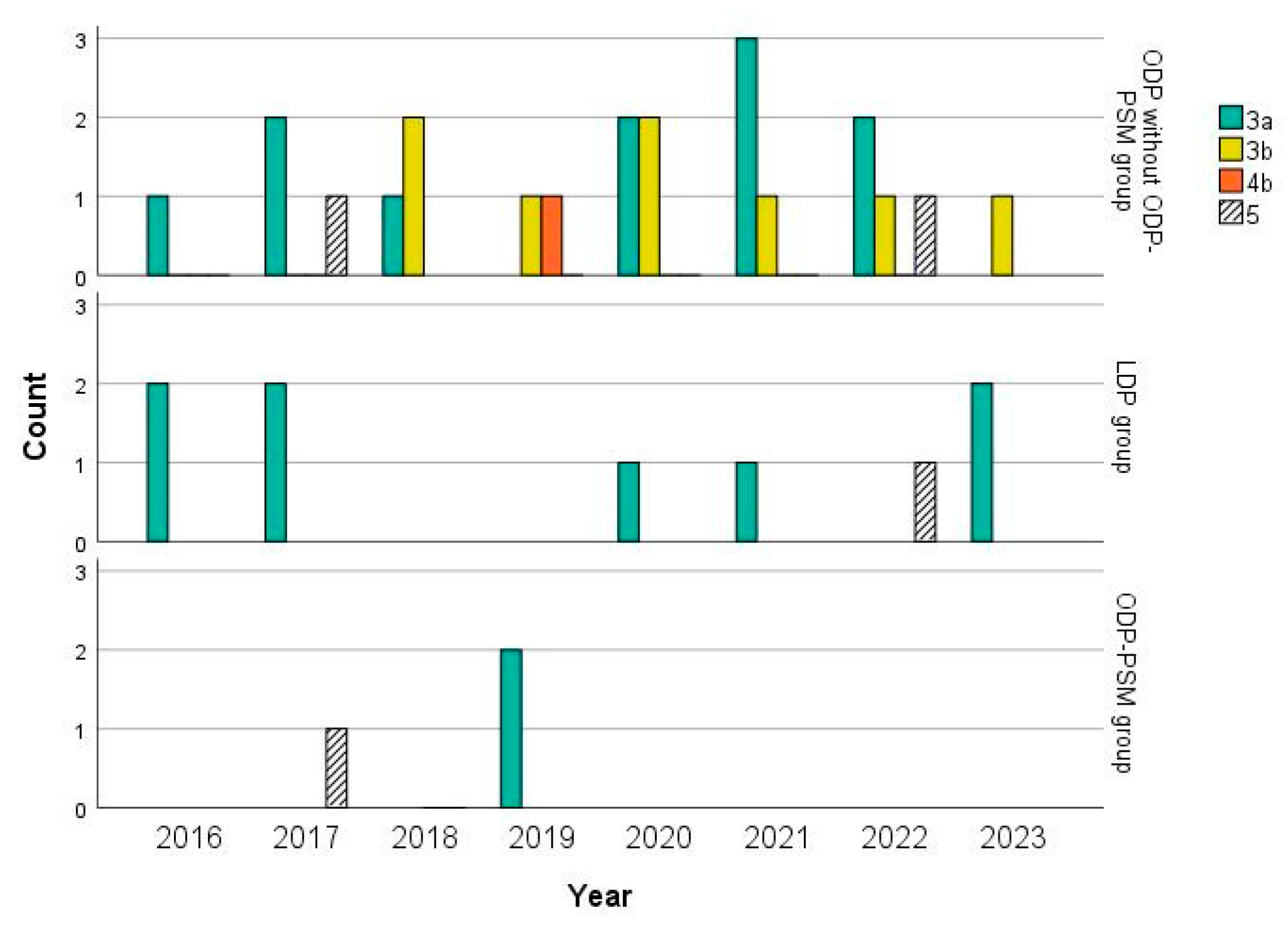
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cuschieri, A. Laparoscopic surgery of the pancreas. J. R. Coll. Surg. Edinb. 1994, 39, 178–184. [Google Scholar]
- Vollmer, C.M.; Asbun, H.J.; Barkun, J.; Besselink, M.G.; Boggi, U.; Conlon, K.C.; Han, H.S.; Hansen, P.D.; Kendrick, M.L.; Montagnini, A.L.; et al. Proceedings of the first international state-of-the-art conference on minimally-invasive pancreatic resection (MIPR). HPB 2017, 19, 171–177. [Google Scholar] [CrossRef]
- Bassi, C.; Andrianello, S. Identifying key outcome metrics in pancreatic surgery, and how to optimally achieve them. HPB 2017, 19, 178–181. [Google Scholar] [CrossRef][Green Version]
- Røsok, B.I.; de Rooij, T.; van Hilst, J.; Diener, M.K.; Allen, P.J.; Vollmer, C.M.; Kooby, D.A.; Shrikhande, S.V. Minimally invasive distal pancreatectomy. HPB 2017, 19, 205–214. [Google Scholar] [CrossRef]
- van Hilst, J.; de Rooij, T.; Klompmaker, S.; Rawashdeh, M.; Aleotti, F.; Al-Sarireh, B.; Alseidi, A.; Ateeb, Z.; Balzano, G.; Berrevoet, F.; et al. Minimally Invasive versus Open Distal Pancreatectomy for Ductal Adenocarcinoma (DIPLOMA): A Pan-European Propensity Score Matched Study. Ann. Surg. 2019, 269, 10–17. [Google Scholar] [CrossRef]
- de Rooij, T.; van Hilst, J.; van Santvoort, H.; Boerma, D.; van den Boezem, P.; Daams, F.; van Dam, R.; Dejong, C.; van Duyn, E.; Dijkgraaf, M.; et al. Minimally Invasive Versus Open Distal Pancreatectomy (LEOPARD): A Multicenter Patient-blinded Randomized Controlled Trial. Ann. Surg. 2019, 269, 2–9. [Google Scholar] [CrossRef]
- Björnsson, B.; Larsson, A.L.; Hjalmarsson, C.; Gasslander, T.; Sandström, P. Comparison of the duration of hospital stay after laparoscopic or open distal pancreatectomy: Randomized controlled trial. Br. J. Surg. 2020, 107, 1281–1288. [Google Scholar] [CrossRef]
- Asbun, H.J.; Moekotte, A.L.; Vissers, F.L.; Kunzler, F.; Cipriani, F.; Alseidi, A.; D’Angelica, M.I.; Balduzzi, A.; Bassi, C.; Björnsson, B.; et al. The Miami International Evidence-based Guidelines on Minimally Invasive Pancreas Resection. Ann. Surg. 2020, 271, 1–14. [Google Scholar] [CrossRef]
- Abu Hilal, M.; van Ramshorst, T.M.E.; Boggi, U.; Dokmak, S.; Edwin, B.; Keck, T.; Khatkov, I.; Ahmad, J.; Al Saati, H.; Alseidi, A.; et al. The Brescia Internationally Validated European Guidelines on Minimally Invasive Pancreatic Surgery (EGUMIPS). Ann. Surg. 2024, 279, 45–57. [Google Scholar] [CrossRef]
- van Ramshorst, T.M.E.; van Hilst, J.; Boggi, U.; Dokmak, S.; Edwin, B.; Keck, T.; Khatkov, I.; Balduzzi, A.; Pulvirenti, A.; Ahmad, J.; et al. Standardizing definitions and terminology of left-sided pancreatic resections through an international Delphi consensus. Br. J. Surg. 2024, 111, znae039. [Google Scholar] [CrossRef]
- Giani, A.; van Ramshorst, T.; Mazzola, M.; Bassi, C.; Esposito, A.; de Pastena, M.; Edwin, B.; Sahakyan, M.; Kleive, D.; Jah, A.; et al. Benchmarking of minimally invasive distal pancreatectomy with splenectomy: European multicentre study. Br. J. Surg. 2022, 109, 1124–1130. [Google Scholar] [CrossRef]
- Liang, S.; Hameed, U.; Jayaraman, S. Laparoscopic pancreatectomy: Indications and outcomes. World J. Gastroenterol. 2014, 20, 14246–14254. [Google Scholar] [CrossRef]
- Casadei, R.; Ricci, C.; D’Ambra, M.; Marrano, N.; Alagna, V.; Rega, D.; Monari, F.; Minni, F. Laparoscopic versus open distal pancreatectomy in pancreatic tumours: A case-control study. Updates Surg. 2010, 62, 171–174. [Google Scholar] [CrossRef]
- Casadei, R.; Ingaldi, C.; Ricci, C.; Alberici, L.; De Raffele, E.; Vaccaro, M.C.; Minni, F. Laparoscopic versus open distal pancreatectomy: A single centre propensity score matching analysis. Updates Surg. 2021, 73, 1747–1755. [Google Scholar] [CrossRef]
- Kwon, J.; Lee, S.R.; Park, S.Y.; Lee, J.H.; Song, K.B.; Hwang, D.W.; Shin, J.H.; Kim, S.C. Effect of resection margin status on recurrence pattern and survival in distal pancreatectomy for left-sided pancreatic ductal adenocarcinoma. J. Hepatobiliary Pancreat. Sci. 2023, 30, 633–643. [Google Scholar] [CrossRef]
- Malleo, G.; Maggino, L.; Casciani, F.; Lionetto, G.; Nobile, S.; Lazzarin, G.; Paiella, S.; Esposito, A.; Capelli, P.; Luchini, C.; et al. Importance of Nodal Metastases Location in Pancreatoduodenectomy for Pancreatic Ductal Adenocarcinoma: Results from a Prospective, Lymphadenectomy Protocol. Ann. Surg. Oncol. 2022, 29, 3477–3488. [Google Scholar] [CrossRef]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibanes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- Bassi, C.; Marchegiani, G.; Dervenis, C.; Sarr, M.; Abu Hilal, M.; Adham, M.; Allen, P.; Andersson, R.; Asbun, H.J.; Besselink, M.G.; et al. The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years After. Surgery 2017, 161, 584–591. [Google Scholar] [CrossRef]
- Wente, M.N.; Veit, J.A.; Bassi, C.; Dervenis, C.; Fingerhut, A.; Gouma, D.J.; Izbicki, J.R.; Neoptolemos, J.P.; Padbury, R.T.; Sarr, M.G.; et al. Postpancreatectomy hemorrhage (PPH): An International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 2007, 142, 20–25. [Google Scholar] [CrossRef]
- Wente, M.N.; Bassi, C.; Dervenis, C.; Fingerhut, A.; Gouma, D.J.; Izbicki, J.R.; Neoptolemos, J.P.; Padbury, R.T.; Sarr, M.G.; Traverso, L.W.; et al. Delayed gastric emptying (DGE) after pancreatic surgery: A suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 2007, 142, 761–768. [Google Scholar] [CrossRef]
- Breivik, H.; Borchgrevink, P.C.; Allen, S.M.; Rosseland, L.A.; Romundstad, L.; Hals, E.K.; Kvarstein, G.; Stubhaug, A. Assessment of pain. Br. J. Anaesth. 2008, 101, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Nugent, S.M.; Lovejoy, T.I.; Shull, S.; Dobscha, S.K.; Morasco, B.J. Associations of Pain Numeric Rating Scale Scores Collected during Usual Care with Research Administered Patient Reported Pain Outcomes. Pain. Med. 2021, 22, 2235–2241. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Li, J.; Weng, Y.; Deng, X.; Jin, J.; Peng, C. A new enhanced recovery after surgery pathway for left-sided pancreatic cancer patients after distal pancreatectomy. Transl. Cancer Res. 2019, 8, 2613–2620. [Google Scholar] [CrossRef] [PubMed]
- Lassen, K.; Coolsen, M.M.; Slim, K.; Carli, F.; de Aguilar-Nascimento, J.E.; Schäfer, M.; Parks, R.W.; Fearon, K.C.; Lobo, D.N.; Demartines, N.; et al. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin. Nutr. 2012, 31, 817–830. [Google Scholar] [CrossRef]
- Austin, P.C. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivar. Behav. Res. 2011, 46, 399–424. [Google Scholar] [CrossRef]
- Yao, X.I.; Wang, X.; Speicher, P.J.; Hwang, E.S.; Cheng, P.; Harpole, D.H.; Berry, M.F.; Schrag, D.; Pang, H.H. Reporting and Guidelines in Propensity Score Analysis: A Systematic Review of Cancer and Cancer Surgical Studies. J. Natl. Cancer Inst. 2017, 109, djw323. [Google Scholar] [CrossRef]
- Donner, A.; Li, K.Y. The relationship between chi-square statistics from matched and unmatched analyses. J. Clin. Epidemiol. 1990, 43, 827–831. [Google Scholar] [CrossRef]
- Dunnigan, K. Tests of marginal homogeneity and special cases. Pharm. Stat. 2013, 12, 213–216. [Google Scholar] [CrossRef]
- Jagric, T. East meets West: The initial results of laparoscopic gastric cancer resections with Eastern principles in a single Western centre—A propensity score-matched study. Langenbecks Arch. Surg. 2021, 406, 2699–2708. [Google Scholar] [CrossRef]
- Ivanecz, A.; Plahuta, I.; Mencinger, M.; Perus, I.; Magdalenic, T.; Turk, S.; Potrc, S. The learning curve of laparoscopic liver resection utilising a difficulty score. Radiol. Oncol. 2021, 56, 111–118. [Google Scholar] [CrossRef]
- Potrc, S.; Ivanecz, A.; Pivec, V.; Marolt, U.; Rudolf, S.; Iljevec, B.; Jagric, T. Impact Factors for Perioperative Morbidity and Mortality and Repercussion of Perioperative Morbidity and Long-term Survival in Pancreatic Head Resection. Radiol. Oncol. 2018, 52, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Gavriilidis, P.; Roberts, K.J.; Sutcliffe, R.P. Comparison of robotic vs laparoscopic vs open distal pancreatectomy. A systematic review and network meta-analysis. HPB 2019, 21, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- Zhun Hong Wong, N.; Wei Ting Yap, D.; Lei Ng, S.; Yu Ning Ng, J.; James, J.J.; Wei Chieh Kow, A. Oncological outcomes in minimally invasive vs. open distal pancreatectomy: A systematic review and network meta-analysis. Front. Surg. 2024, 11, 1369169. [Google Scholar] [CrossRef] [PubMed]
- Korrel, M.; Vissers, F.L.; van Hilst, J.; de Rooij, T.; Dijkgraaf, M.G.; Festen, S.; Groot Koerkamp, B.; Busch, O.R.; Luyer, M.D.; Sandström, P.; et al. Minimally invasive versus open distal pancreatectomy: An individual patient data meta-analysis of two randomized controlled trials. HPB 2021, 23, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Partelli, S.; Andreasi, V.; Rancoita, P.M.V.; Perez-Sanchez, E.; Muffatti, F.; Balzano, G.; Crippa, S.; Di Serio, C.; Falconi, M. Outcomes after distal pancreatectomy for neuroendocrine neoplasms: A retrospective comparison between minimally invasive and open approach using propensity score weighting. Surg. Endosc. 2021, 35, 165–173. [Google Scholar] [CrossRef]
- Ivanecz, A.; Plahuta, I.; Magdalenic, T.; Mencinger, M.; Perus, I.; Potrc, S.; Krebs, B. The external validation of a difficulty scoring system for predicting the risk of intraoperative complications during laparoscopic liver resection. BMC Surg. 2019, 19, 179. [Google Scholar] [CrossRef]
- Ivanecz, A.; Plahuta, I.; Magdalenic, T.; Ilijevec, B.; Mencinger, M.; Perus, I.; Potrc, S. Evaluation of the Iwate Model for Predicting the Difficulty of Laparoscopic Liver Resection: Does Tumor Size Matter? J. Gastrointest. Surg. 2021, 25, 1451–1460. [Google Scholar] [CrossRef]
- Chan, K.S.; Wang, Z.K.; Syn, N.; Goh, B.K.P. Learning curve of laparoscopic and robotic pancreas resections: A systematic review. Surgery 2021, 170, 194–206. [Google Scholar] [CrossRef]
- McCoy, C.E. Understanding the Intention-to-treat Principle in Randomized Controlled Trials. West. J. Emerg. Med. 2017, 18, 1075–1078. [Google Scholar] [CrossRef]
- Lu, Q.; Lu, J.W.; Wu, Z.; Liu, X.M.; Li, J.H.; Dong, J.; Yin, G.Z.; Lv, Y.; Zhang, X.F. Perioperative outcome of elderly versus younger patients undergoing major hepatic or pancreatic surgery. Clin. Interv. Aging 2018, 13, 133–141. [Google Scholar] [CrossRef]
- Pecorelli, N.; Guarneri, G.; Quattromani, R.; Arru, G.G.; Gozzini, L.; Lee, Y.H.; Vallorani, A.; Turi, S.; Partelli, S.; Crippa, S.; et al. The impact of preoperative anemia on pancreatic resection outcomes. HPB 2022, 24, 717–726. [Google Scholar] [CrossRef] [PubMed]
- Kowalsky, S.J.; Zenati, M.S.; Dhir, M.; Schaefer, E.G.; Dopsovic, A.; Lee, K.K.; Hogg, M.E.; Zeh, H.J.; Vollmer, C.M.; Zureikat, A.H. Postoperative narcotic use is associated with development of clinically relevant pancreatic fistulas after distal pancreatectomy. Surgery 2018, 163, 747–752. [Google Scholar] [CrossRef] [PubMed]
- Boyev, A.; Prakash, L.R.; Chiang, Y.J.; Childers, C.P.; Jain, A.J.; Newhook, T.E.; Bruno, M.L.; Arvide, E.M.; Dewhurst, W.L.; Kim, M.P.; et al. Postoperative Opioid Use Is Associated with Increased Rates of Grade B/C Pancreatic Fistula After Distal Pancreatectomy. J. Gastrointest. Surg. 2023, 27, 2135–2144. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.K.; Kim, H.; Byun, Y.; Han, Y.; Choi, Y.J.; Kang, J.S.; Kwon, W.; Han, I.W.; Shin, S.H.; Choi, D.W.; et al. Optimal stapler cartridge selection to reduce post-operative pancreatic fistula according to the pancreatic characteristics in stapler closure distal pancreatectomy. HPB 2021, 23, 633–640. [Google Scholar] [CrossRef]
- Murata, Y.; Maeda, K.; Ito, T.; Gyoten, K.; Hayasaki, A.; Iizawa, Y.; Fujii, T.; Tanemura, A.; Kuriyama, N.; Kishiwada, M.; et al. Efficacy of Reinforced Stapler Versus Hand-sewn Closure of the Pancreatic Stump During Pure Laparoscopic Distal Pancreatectomy to Reduce Pancreatic Fistula. Surg. Laparosc. Endosc. Percutan Tech. 2023, 33, 99–107. [Google Scholar] [CrossRef]
- Xia, N.; Li, J.; Huang, X.; Tian, B.; Xiong, J. Reinforced stapling does not reduce postoperative pancreatic fistula in distal pancreatectomy: A systematic review and meta-analysis. Updates Surg. 2023, 75, 2063–2074. [Google Scholar] [CrossRef]
- Quero, G.; Laterza, V.; Schena, C.A.; Massimiani, G.; Lucinato, C.; Fiorillo, C.; Mezza, T.; Taglioni, F.; Menghi, R.; Di Cesare, L.; et al. Prolonged pre-firing pancreatic compression with linear staplers in distal pancreatectomy: A valuable technique for post-operative pancreatic fistula prevention. Langenbecks Arch. Surg. 2024, 409, 184. [Google Scholar] [CrossRef]
- Kjeseth, T.; Yaqub, S.; Edwin, B.; Kleive, D.; Sahakyan, M.A. Peri-firing compression in prevention of pancreatic fistula after distal pancreatectomy: A systematic review and a cohort study. Scand. J. Surg. 2024, 113, 73–79. [Google Scholar] [CrossRef]
- Barresi, V.; Reggiani Bonetti, L.; Ieni, A.; Caruso, R.A.; Tuccari, G. Histological grading in colorectal cancer: New insights and perspectives. Histol. Histopathol. 2015, 30, 1059–1067. [Google Scholar] [CrossRef]
- Tol, J.A.; Gouma, D.J.; Bassi, C.; Dervenis, C.; Montorsi, M.; Adham, M.; Andrén-Sandberg, A.; Asbun, H.J.; Bockhorn, M.; Büchler, M.W.; et al. Definition of a standard lymphadenectomy in surgery for pancreatic ductal adenocarcinoma: A consensus statement by the International Study Group on Pancreatic Surgery (ISGPS). Surgery 2014, 156, 591–600. [Google Scholar] [CrossRef]
- Seo, S.; Uemura, K.; Sumiyoshi, T.; Kondo, N.; Okada, K.; Otsuka, H.; Murakami, Y.; Takahashi, S. Optimal lymph-node dissection for pancreatic tail cancer. Surg. Today 2022, 52, 1307–1312. [Google Scholar] [CrossRef] [PubMed]
- Ishida, H.; Ogura, T.; Takahashi, A.; Miyamoto, R.; Matsudaira, S.; Amikura, K.; Tanabe, M.; Kawashima, Y. Optimal Region of Lymph Node Dissection in Distal Pancreatectomy for Left-Sided Pancreatic Cancer Based on Tumor Location. Ann. Surg. Oncol. 2022, 29, 2414–2424. [Google Scholar] [CrossRef] [PubMed]
- Imamura, T.; Yamamoto, Y.; Sugiura, T.; Okamura, Y.; Ito, T.; Ashida, R.; Ohgi, K.; Uesaka, K. Reconsidering the Optimal Regional Lymph Node Station According to Tumor Location for Pancreatic Cancer. Ann. Surg. Oncol. 2021, 28, 1602–1611. [Google Scholar] [CrossRef] [PubMed]
| Variable | Overall Analysis | Propensity Score Matched Patients | |||||
|---|---|---|---|---|---|---|---|
| All Patients 108 (%) | LDP (n = 19, 17.6%) | ODP (n = 89, 82.4%) | p Value | LDP (n = 19, 100%) | ODP-PSM (n = 19, 100%) | p Value | |
| Male sex | 50 (46.3) | 8 (42.1) | 42 (47.2) | 0.802 a | 8 (42.1) | 7 (36.8) | 0.705 b |
| Age (years) | 66 (19) | 69 (14) | 64 (19) | 0.085 c | 69 (14) | 66 (13) | 0.090 d |
| Body mass index (kg/m2) | 27.3 (8.2) | 26.7 (8.9) | 27.3 (8) | 0.623 c | 26.7 (8.9) | 27.6 (7.4) | 0.717 d |
| ASA score III | 27 (25.0) | 5 (26.3) | 22 (24.7) | 1.000 a | 5 (26.3) | 5 (26.3) | 0.480 b |
| Comorbidities present | 75 (69.4) | 14 (73.7) | 61 (68.5) | 0.787 a | 14 (73.7) | 14 (73.7) | 1.000 b |
| Number of comorbidities | 2 (2) | 2 (2) | 2 (3) | 0.663 c | 2 (2) | 2 (4) | 0.931 d |
| Previous abdominal surgery | 42 (38.9) | 11 (57.9) | 31 (34.8) | 0.073 a | 11 (57.9) | 9 (47.4) | 0.480 b |
| C-reactive protein > 5 mg/L | 28 (25.9) | 4 (21.1) | 24 (27.0) | 0.775 a | 4 (21.1) | 5 (26.3) | 0.705 b |
| Carcinoembryonic antigen > 5 μg/L | 17 (15.7) | 1 (5.3) | 16 (18.0) | 0.297 a | 1 (5.3) | 4 (21.1) | 0.180 b |
| Carbohydrate antigen 19-9 > 37 kU/L | 42 (38.9) | 7 (36.8) | 35 (39.3) | 1.000 a | 7 (36.8) | 7 (36.8) | 1.000 b |
| Malignant tumors | 69 (63.9) | 13 (68.4) | 56 (62.9) | 0.794 a | 13 (68.4) | 11(57.9) | 0.414 b |
| Tumor size (mm) | 35 (27) | 29 (26) | 35 (25) | 0.124 c | 29 (26) | 35 (25) | 0.121 d |
| Tumor in the neck/body | 57 (52.8) | 7 (36.8) | 50 (56.2) | 0.138 a | 7 (36.8) | 5 (26.3) | 0.480 b |
| Outcome | Overall Analysis | Propensity Score Matched Patients | |||||
|---|---|---|---|---|---|---|---|
| All Patients n (%) | LDP (n = 19, 17.6%) | ODP (n = 89, 82.4%) | p Value | LDP (n = 19, 100%) | ODP-PSM (n = 19, 100%) | p Value | |
| Operative time (min) | 190 (80) | 202 (110) | 185 (90) | 0.084 c | 202 (110) | 190 (140) | 0.602 d |
| Blood loss (mL) | 209 (241) | 134 (64) | 226 (279) | 0.073 c | 134 (64) | 245 (330) | 0.121 d |
| Intraoperative blood transfusion | 6 (5.6) | 1 (5.3) | 5 (5.6) | 1.000 a | 1 (5.3) | 1 (5.3) | 1.000 b |
| No complications | 22 (20.4) | 1 (5.3) | 21 (23.6) | 0.018 e | 1 (5.3) | 6 (31.6) | 0.042 f |
| Clavien–Dindo 1 | 25 (23.1) | 7 (36.8) | 18 (20.2) | 7 (36.8) | 4 (21.1) | ||
| Clavien–Dindo 2 | 27 (25.0) | 2 (10.5) | 25 (28.1) | 2 (10.5) | 6 (31.6) | ||
| Clavien–Dindo 3a | 21 (19.4) | 8 (42.1) | 13 (14.6) | 8 (42.1) | 2 (10.5) | ||
| Clavien–Dindo 3b | 8 (7.4) | 0 (0.0) | 8 (9.0) | 0 (0.0) | 0 (0.0) | ||
| Clavien–Dindo 4b | 1 (0.9) | 0 (0.0) | 1 (1.1) | 0 (0.0) | 0 (0.0) | ||
| Clavien–Dindo 5 | 4 (3.7) | 1 (5.3) | 3 (3.3) | 1 (5.3) | 1 (5.3) | ||
| Severe morbidity (Clavien–Dindo ≥ 3a) | 34 (30.6) | 9 (47.4) | 25 (28.1) | 0.111 a | 9 (47.4) | 3 (15.8) | 0.034 b |
| 30-day mortality | 1 (0.9) | 0 (0.0) | 1 (1.1) | 1.000 a | 0 (0.0) | 1 (5.3) | 0.317 b |
| 90-day mortality | 4 (3.7) | 1 (5.3) | 3 (3.3) | 0.444 a | 1 (5.3) | 1 (5.3) | 1.000 b |
| Post-pancreatectomy hemorrhage (all three grades) | 3 (2.8) | 0 (0.0) | 3 (3.4) | 1.000 a | 0 (0.0) | 1 (5.3) | 0.317 b |
| Delayed gastric emptying | 2 (1.9) | 1 (5.3) | 1 (1.1) | 0.322 a | 1 (5.3) | 1 (5.3) | 1.000 b |
| Postoperative pancreatic fistula type B | 32 (29.6) | 7 (36.8) | 25 (28.1) | 0.580 a | 7 (36.8) | 5 (26.3) | 0.527 b |
| Postoperative pancreatic fistula type C | 8 (7.4) | 0 (0.0) | 8 (9.0) | 0.346 a | 0 (0.0) | 1 (5.3) | 0.317 b |
| Reoperation | 11 (10.2) | 1 (5.3) | 10 (11.2) | 0.685 a | 1 (5.3) | 0 (0.0) | 0.317 b |
| Readmission | 23 (21.3) | 3 (15.8) | 20 (22.5) | 0.759 a | 3 (15.8) | 1 (5.3) | 0.317 b |
| Hospital stay (days) | 11 (7) | 9 (7) | 11 (8) | 0.074 c | 9 (7) | 12 (11) | 0.538 d |
| Intensive care unit admission | 7 (6.5) | 1 (5.3) | 6 (6.7) | 1.000 a | 1 (5.3) | 1 (5.3) | 1.000 b |
| High-dependency unit stay (days) | 5 (2) | 5 (3) | 5 (2) | 0.849 c | 5 (3) | 5 (2) | 0.451 d |
| Time to oral food intake (days) | 4 (2) | 4 (2) | 4 (2) | 0.878 c | 4 (2) | 4 (3) | 0.647 d |
| Time to stool passing (days) | 4 (1) | 3 (1) | 4 (1) | 0.866 c | 3 (1) | 3 (2) | 0.523 d |
| Intravenous narcotics requirement (days) | 6 (3) | 5 (4) | 6 (3) | 0.214 c | 5 (4) | 7 (2) | 0.041 d |
| Incisional hernia | 14 (13.0) | 2 (10.5) | 12 (13.5) | 1.000 a | 2 (10.5) | 3 (15.8) | 0.655 b |
| ODP Without ODP-PSM Group | LDP Group | ODP-PSM Group | |
|---|---|---|---|
| Clavien–Dindo 3a (intervention without general anesthesia) | |||
| Thoracic drainage | 1 | ||
| Postoperative pancreatic fistula drainage | 11 | 6 | 2 |
| Subphrenic abscess drainage | 2 | 1 | |
| Gastric bleeding–endoscopic hemostasis | 1 | ||
| Clavien–Dindo 3b (intervention under general anesthesia) | |||
| Subtotal colectomy due to toxic megacolon | 1 | ||
| Reduction in internal hernia | 1 | ||
| Drainage of the abscess | 3 | 1 | |
| Duodenum-preserving pancreatectomy | 2 | ||
| Hemostasis of bleeding from lienal artery | 2 | ||
| Partial omentectomy due to necrosis | 1 | ||
| Lymphorrhea–sutures of cisterna chyli | 1 | ||
| Colostomy due to the colocutaneous fistula | 1 | ||
| Clavien–Dindo 4b (multiorgan dysfunction) | |||
| Septic shock due to portal vein thrombosis | 1 | ||
| Clavien–Dindo 5 (death) | |||
| Pulmonary embolism | 1 | ||
| Acute myocardial infarction | 1 | ||
| Septic shock | 1 | ||
| Coronavirus disease 2019 pneumonia | 1 | ||
| Outcome | Overall Analysis | Propensity Score Matched Patients | |||||
|---|---|---|---|---|---|---|---|
| All Patients n = 69 | LDP (n = 13, 68.4%) | ODP (n = 56, 62.9%) | p Value | LDP (n = 13, 68.4%) | ODP-PSM (n = 11, (57.9%) | p Value | |
| Diagnosis | |||||||
| Pancreatic ductal adenocarcinoma | 39 (56.5) | 5 (38.5) | 34 (60.7) | 0.191 e | 5 (38.5) | 6 (54.5) | 0.564 f |
| Nonfunctioning pancreatic neuroendocrine neoplasms | 27 (39.1) | 8 (61.5) | 19 (33.9) | 8 (61.5) | 4 (36.4) | ||
| Other | 3 (4.3) | 0 (0.0) | 3 (5.4) | 0 (0.0) | 1 (9.1) | ||
| Number of harvested lymph nodes | 14 (12) | 14 (9) | 15 (16) | 0.685 c | 14 (9) | 15 (22) | 0.284 d |
| Resection margin (mm) | 3 (8) | 4 (11) | 3 (9) | 0.786 c | 4 (11) | 6 (15) | 0.929 d |
| R0 resection | 57 (82.6) | 11 (84.6) | 46 (82.1) | 1.000 a | 11 (84.6) | 10 (90.9) | 1.000 b |
| Outcome | Range | Median Value | Benchmark |
|---|---|---|---|
| Duration of operation (min) | 132.5–361.5 | 232.5 | 160 |
| Conversion (%) | 0–54.5 | 12.3 | 2.5 |
| Intraoperative blood transfusion (%) | 0–10.8 | 2.6 | 0.5 |
| Overall morbidity (%) | 25.6–100 | 58.0 | 30.4 |
| Severe morbidity (%) | 4.4–54.7 | 17.4 | 8.4 |
| Postoperative pancreatic fistula (%) | 6.3–47.4 | 21.9 | 8.3 |
| Reoperations (%) | 0–20.0 | 5.4 | 1.8 |
| Duration of hospital stay (days) | 5–13 | 8 | 5 |
| Readmissions (%) | 0–40 | 13.0 | 4.1 |
| 90–days mortality | 0–17.6 | 0 | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Plahuta, I.; Šarenac, Ž.; Golob, M.; Turk, Š.; Ilijevec, B.; Magdalenić, T.; Potrč, S.; Ivanecz, A. Laparoscopic and Open Distal Pancreatectomy—An Initial Single-Institution Experience with a Propensity Score Matching Analysis. Life 2025, 15, 97. https://doi.org/10.3390/life15010097
Plahuta I, Šarenac Ž, Golob M, Turk Š, Ilijevec B, Magdalenić T, Potrč S, Ivanecz A. Laparoscopic and Open Distal Pancreatectomy—An Initial Single-Institution Experience with a Propensity Score Matching Analysis. Life. 2025; 15(1):97. https://doi.org/10.3390/life15010097
Chicago/Turabian StylePlahuta, Irena, Žan Šarenac, Medeja Golob, Špela Turk, Bojan Ilijevec, Tomislav Magdalenić, Stojan Potrč, and Arpad Ivanecz. 2025. "Laparoscopic and Open Distal Pancreatectomy—An Initial Single-Institution Experience with a Propensity Score Matching Analysis" Life 15, no. 1: 97. https://doi.org/10.3390/life15010097
APA StylePlahuta, I., Šarenac, Ž., Golob, M., Turk, Š., Ilijevec, B., Magdalenić, T., Potrč, S., & Ivanecz, A. (2025). Laparoscopic and Open Distal Pancreatectomy—An Initial Single-Institution Experience with a Propensity Score Matching Analysis. Life, 15(1), 97. https://doi.org/10.3390/life15010097







