Less Is More: Evaluating the Benefits of Minimally Invasive Spinal Surgery
Abstract
1. Introduction
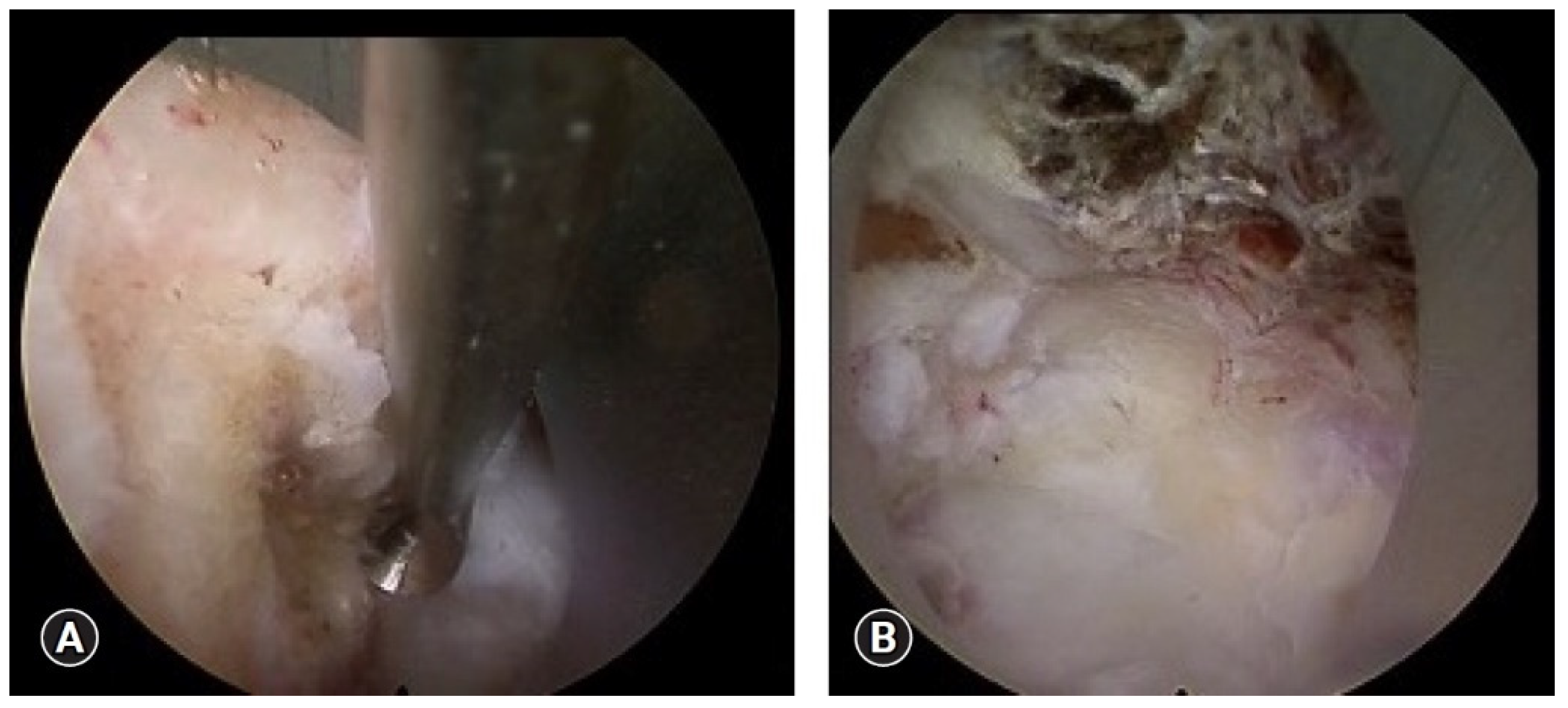
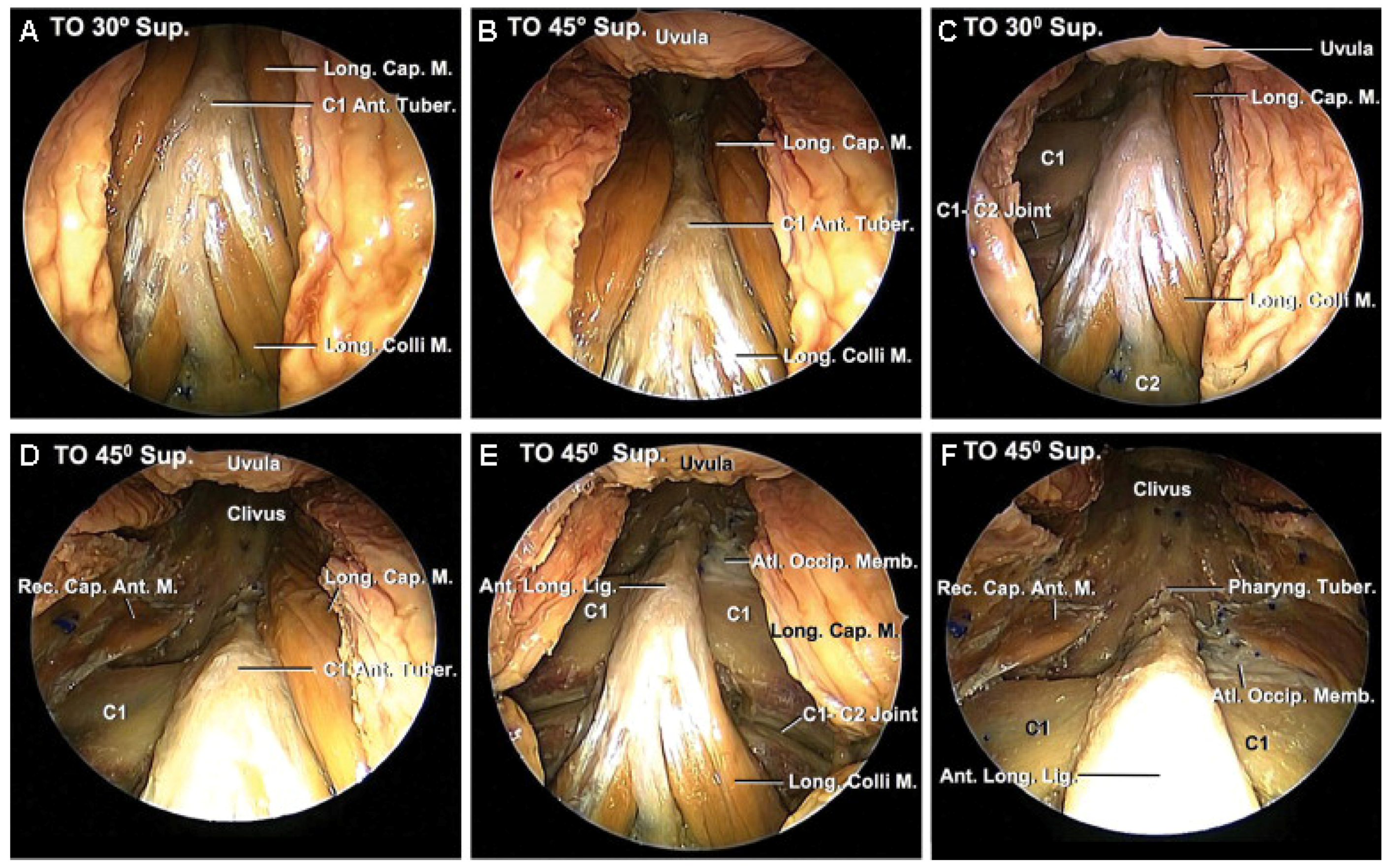
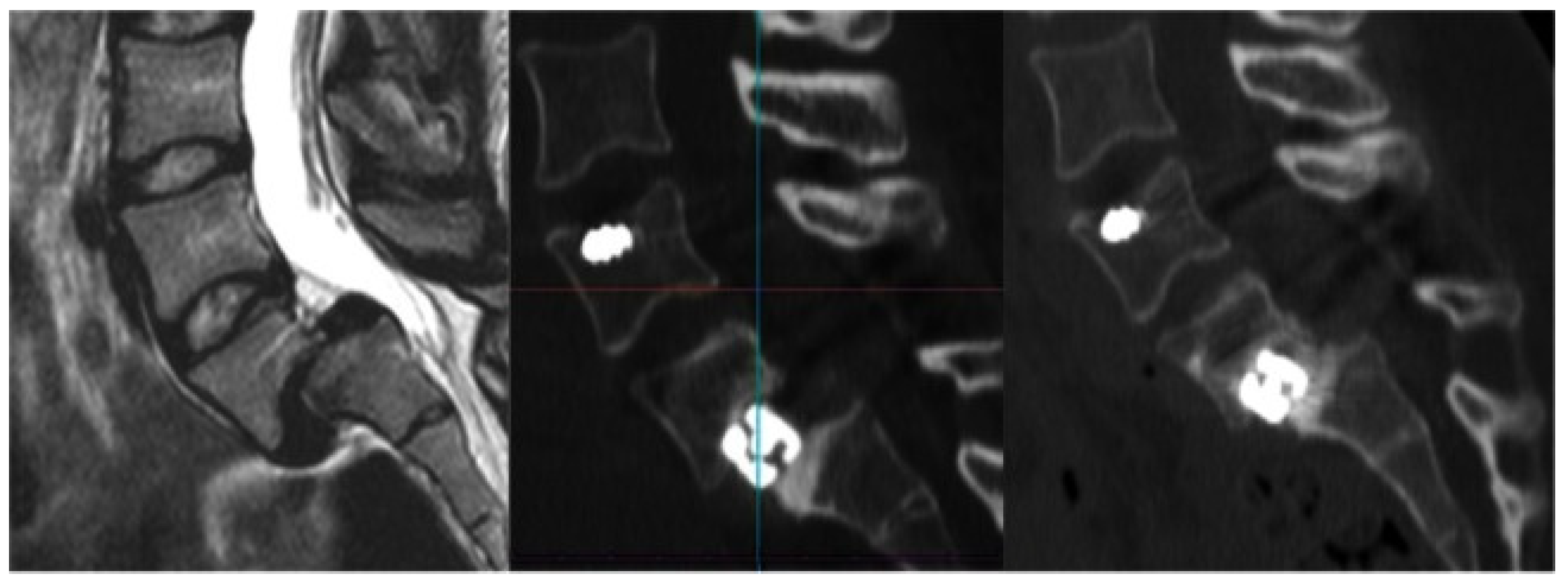
2. Endonasal Cervical Approaches for Pathologies of the Upper Cervical Spine
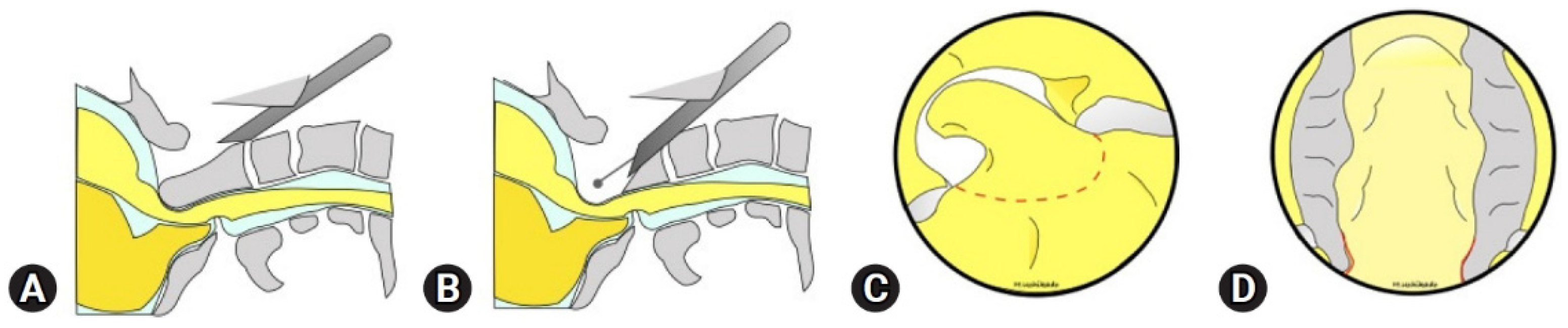
3. Transoral Cervical Approaches
4. Transcervical Approaches
5. Mini-Open/Percutaneous
6. Tubular
7. Endoscopic
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Parenteau, C.S.; Lau, E.C.; Campbell, I.C.; Courtney, A. Prevalence of Spine Degeneration Diagnosis by Type, Age, Gender, and Obesity Using Medicare Data. Sci. Rep. 2021, 11, 5389. [Google Scholar] [CrossRef]
- Kobayashi, K.; Sato, K.; Kato, F.; Kanemura, T.; Yoshihara, H.; Sakai, Y.; Shinjo, R.; Ohara, T.; Yagi, H.; Matsubara, Y.; et al. Trends in the Numbers of Spine Surgeries and Spine Surgeons over the Past 15 Years. Nagoya J. Med. Sci. 2022, 84, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Chen, M.; Wu, X.; Lin, S.; Tao, C.; Cao, H.; Shao, Z.; Xiao, G. Global, Regional and National Burden of Low Back Pain 1990–2019: A Systematic Analysis of the Global Burden of Disease Study 2019. J. Orthop. Transl. 2022, 32, 49–58. [Google Scholar] [CrossRef]
- Weiss, A.J.; Elixhauser, A.; Andrews, R.M. Characteristics of Operating Room Procedures in U.S. Hospitals, 2011: Statistical Brief #170; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2006.
- BIS Research. Minimally Invasive Spine Technologies Market—A Global and Regional Analysis: Focus on Condition, End User Analysis, and Country Analysis—Analysis and Forecast, 2022–2032; BIS Research: Fremont, CA, USA, 2023. [Google Scholar]
- Martin, B.I.; Lurie, J.D.; Tosteson, A.N.A.; Deyo, R.A.; Tosteson, T.D.; Weinstein, J.N.; Mirza, S.K. Indications for Spine Surgery: Validation of an Administrative Coding Algorithm to Classify Degenerative Diagnoses. Spine 2014, 39, 769–779. [Google Scholar] [CrossRef] [PubMed]
- Näther, P.; Kersten, J.F.; Kaden, I.; Irga, K.; Nienhaus, A. Distribution Patterns of Degeneration of the Lumbar Spine in a Cohort of 200 Patients with an Indication for Lumbar MRI. Int. J. Envrion. Res. Public Health 2022, 19, 3721. [Google Scholar] [CrossRef] [PubMed]
- Ramanathan, S.; Rapp, A.; Perez-Cruet, M.; Fahim, D.K. Long-Term Reoperation Rates After Open versus Minimally Invasive Spine Surgery for Degenerative Lumbar Disease: Five Year Follow-Up of 2130 Patients. World Neurosurg. 2023, 171, e126–e136. [Google Scholar] [CrossRef]
- Yadav, Y.; Madhariya, S.; Parihar, V.; Namdev, H.; Bhatele, P. Endoscopic Transoral Excision of Odontoid Process in Irreducible Atlantoaxial Dislocation: Our Experience of 34 Patients. J. Neurol. Surg. A Cent. Eur. Neurosurg. 2012, 74, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Baird, C.J.; Conway, J.E.; Sciubba, D.M.; Prevedello, D.M.; Quiñones-Hinojosa, A.; Kassam, A.B. Radiographic and anatomic basis of endoscopic anterior craniocervical decompression. Oper. Neurosurg. 2009, 65, ons158–ons164. [Google Scholar] [CrossRef]
- Sexton, M.A.; Abcejo, A.S.; Pasternak, J.J. Comparison of Anesthetic Management and Outcomes in Patients Having Either Transnasal or Transoral Endoscopic Odontoid Process Surgery. J. Neurosurg. Anesth. 2018, 30, 179–183. [Google Scholar] [CrossRef]
- Dlouhy, B.J.; Dahdaleh, N.S.; Menezes, A.H. Evolution of Transoral Approaches, Endoscopic Endonasal Approaches, and Reduction Strategies for Treatment of Craniovertebral Junction Pathology: A Treatment Algorithm Update. Neurosurg. Focus 2015, 38, E8. [Google Scholar] [CrossRef] [PubMed]
- Kassam, A.B.; Snyderman, C.; Gardner, P.; Carrau, R.; Spiro, R. The Expanded Endonasal Approach: A Fully Endoscopic Transnasal Approach and Resection of the Odontoid Process: Technical Case Report. Oper. Neurosurg. 2005, 57, E213. [Google Scholar] [CrossRef] [PubMed]
- Alfieri, A.; Jho, H.-D.; Tschabitscher, M. Endoscopic Endonasal Approach to the Ventral Cranio-Cervical Junction: Anatomical Study. Acta Neurochir. 2002, 144, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Botelho, R.V.; Botelho, P.B.; Hernandez, B.; Sales, M.B.; Rotta, J.M. Association between Brachycephaly, Chiari Malformation, and Basilar Invagination. J. Neurol. Surg. A Cent. Eur. Neurosurg. 2023, 84, 329–333. [Google Scholar] [CrossRef]
- Wang, X.; Ma, L.; Liu, Z.; Chen, Z.; Wu, H.; Jian, F. Reconsideration of the Transoral Odontoidectomy in Complex Craniovertebral Junction Patients with Irreducible Anterior Compression. Chin. Neurosurg. J. 2020, 6, 33. [Google Scholar] [CrossRef] [PubMed]
- Halderman, A.A.; Barnett, S.L. Endoscopic Endonasal Approach to the Craniovertebral Junction. World J. Otorhinolaryngol. Head Neck Surg. 2022, 8, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Zoli, M.; Mazzatenta, D.; Valluzzi, A.; Mascari, C.; Pasquini, E.; Frank, G. Endoscopic Endonasal Odontoidectomy. Neurosurg. Clin. N. Am. 2015, 26, 427–436. [Google Scholar] [CrossRef]
- El-Sayed, I.H.; Wu, J.-C.; Dhillon, N.; Ames, C.P.; Mummaneni, P. The Importance of Platybasia and the Palatine Line in Patient Selection for Endonasal Surgery of the Craniocervical Junction: A Radiographic Study of 12 Patients. World Neurosurg. 2011, 76, 183–188. [Google Scholar] [CrossRef]
- Husain, Q.; Kim, M.H.; Hussain, I.; Anand, V.K.; Greenfield, J.P.; Schwartz, T.H.; Kacker, A. Endoscopic Endonasal Approaches to the Craniovertebral Junction: The Otolaryngologist’s Perspective. World J. Otorhinolaryngol. Head Neck Surg. 2020, 6, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Wang, E.W.; Zanation, A.M.; Gardner, P.A.; Schwartz, T.H.; Eloy, J.A.; Adappa, N.D.; Bettag, M.; Bleier, B.S.; Cappabianca, P.; Carrau, R.L.; et al. ICAR: Endoscopic Skull-base Surgery. Int. Forum. Allergy Rhinol. 2019, 9, S145–S365. [Google Scholar] [CrossRef]
- La Corte, E.; Aldana, P.R.; Ferroli, P.; Greenfield, J.P.; Härtl, R.; Anand, V.K.; Schwartz, T.H. The Rhinopalatine Line as a Reliable Predictor of the Inferior Extent of Endonasal Odontoidectomies. Neurosurg. Focus 2015, 38, E16. [Google Scholar] [CrossRef]
- Ruiz-Garcia, H.; Gassie, K.; Marenco-Hillembrand, L.; Donaldson, A.M.; Chaichana, K.L. Endoscopic Endonasal Odontoidectomy for the Treatment of Basilar Invagination. Neurosurg. Focus Video 2020, 3, V3. [Google Scholar] [CrossRef]
- Aldana, P.R.; Naseri, I.; La Corte, E. The Naso-Axial Line. Oper. Neurosurg. 2012, 71, ons308–ons314. [Google Scholar] [CrossRef]
- Portonero, I.; Lo Bue, E.; Penner, F.; Di Perna, G.; Baldassarre, B.M.; De Marco, R.; Pesaresi, A.; Garbossa, D.; Pecorari, G.; Zenga, F. Lesson Learned in Endoscopic Endonasal Dens Resection for C1–C2 Spinal Cord Decompression. Eur. Spine J. 2023, 33, 438–443. [Google Scholar] [CrossRef] [PubMed]
- Joaquim, A.F.; Osorio, J.A.; Riew, K.D. Transoral and Endoscopic Endonasal Odontoidectomies—Surgical Techniques, Indications, and Complications. Neurospine 2019, 16, 462–469. [Google Scholar] [CrossRef] [PubMed]
- Simal-Julián, J.A.; Miranda-Lloret, P.; Sanchis-Martín, M.R.; Quiroz, A.; Botella-Asunción, C.; Kassam, A.B. Endonasal Odontoidectomy in Basilar Invagination. J. Neurol. Surg. B Skull Base 2021, 82, S14–S15. [Google Scholar] [CrossRef] [PubMed]
- Grose, E.; Moldovan, I.D.; Kilty, S.; Agbi, C.; Lamothe, A.; Alkherayf, F. Clinical Outcomes of Endoscopic Endonasal Odontoidectomy: A Single-Center Experience. World Neurosurg. 2020, 137, e406–e415. [Google Scholar] [CrossRef]
- Goldschlager, T.; Härtl, R.; Greenfield, J.P.; Anand, V.K.; Schwartz, T.H. The Endoscopic Endonasal Approach to the Odontoid and Its Impact on Early Extubation and Feeding. J. Neurosurg. 2015, 122, 511–518. [Google Scholar] [CrossRef] [PubMed]
- Fang, C.H.; Friedman, R.; Schild, S.D.; Goldstein, I.M.; Baredes, S.; Liu, J.K.; Eloy, J.A. Purely Endoscopic Endonasal Surgery of the Craniovertebral Junction: A Systematic Review. Int. Forum. Allergy Rhinol. 2015, 5, 754–760. [Google Scholar] [CrossRef] [PubMed]
- Arumalla, K.; Bansal, H.; Jadeja, J.; Batish, A.; Deora, H.; Tripathi, M.; Mohindra, S.; Behari, S. Anterior Approach to the Cervical Spine: Elegance Lies in Its Simplicity. Asian J. Neurosurg. 2021, 16, 669–684. [Google Scholar] [CrossRef]
- Eicker, S.O.; Mende, K.C.; Dührsen, L.; Schmidt, N.O. Minimally Invasive Approach for Small Ventrally Located Intradural Lesions of the Craniovertebral Junction. Neurosurg. Focus 2015, 38, E10. [Google Scholar] [CrossRef]
- Patel, P.D.; Canseco, J.A.; Houlihan, N.; Gabay, A.; Grasso, G.; Vaccaro, A.R. Overview of Minimally Invasive Spine Surgery. World Neurosurg. 2020, 142, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Hussain, I.; Schmidt, F.A.; Kirnaz, S.; Wipplinger, C.; Schwartz, T.H.; Härtl, R. MIS Approaches in the Cervical Spine. J. Spine Surg. 2019, 5, S74–S83. [Google Scholar] [CrossRef] [PubMed]
- Fong, S.; DuPlessis, S.J. Minimally Invasive Anterior Approach to Upper Cervical Spine. J. Spinal Disord Tech. 2005, 18, 321–325. [Google Scholar] [CrossRef] [PubMed]
- Rock, J.P.; Tomecek, F.J.; Ross, L. Transoral Surgery: An Anatomic Study. Skull Base Surg. 1993, 3, 109–116. [Google Scholar] [CrossRef]
- Hsu, W.; Wolinsky, J.-P.; Gokaslan, Z.L.; Sciubba, D.M. Transoral Approaches to the Cervical Spine. Neurosurgery 2010, 66, A119–A125. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.K.; Couldwell, W.T.; Apfelbaum, R.I. Transoral Approach and Extended Modifications for Lesions of the Ventral Foramen Magnum and Craniovertebral Junction. Skull Base 2008, 18, 151–166. [Google Scholar] [CrossRef] [PubMed]
- Tirelli, G.; Boscolo Nata, F.; Piovesana, M.; Quatela, E.; Gardenal, N.; Hayden, R.E. Transoral Surgery (TOS) in Oropharyngeal Cancer: Different Tools, a Single Mini-Invasive Philosophy. Surg. Oncol. 2018, 27, 643–649. [Google Scholar] [CrossRef]
- Oppenheimer, J.H.; DeCastro, I.; McDonnell, D.E. Minimally Invasive Spine Technology and Minimally Invasive Spine Surgery: A Historical Review. Neurosurg. Focus 2009, 27, E9. [Google Scholar] [CrossRef]
- Thongtrangan, I.; Le, H.; Park, J.; Kim, D.H. Minimally Invasive Spinal Surgery: A Historical Perspective. Neurosurg. Focus 2004, 16, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Tateya, I.; Shiotani, A.; Satou, Y.; Tomifuji, M.; Morita, S.; Muto, M.; Ito, J. Transoral Surgery for Laryngo-Pharyngeal Cancer—The Paradigm Shift of the Head and Cancer Treatment. Auris. Nasus. Larynx 2016, 43, 21–32. [Google Scholar] [CrossRef]
- Seker, A.; Inoue, K.; Osawa, S.; Akakin, A.; Kilic, T.; Rhoton, A.L. Comparison of Endoscopic Transnasal and Transoral Approaches to the Craniovertebral Junction. World Neurosurg. 2010, 74, 583–602. [Google Scholar] [CrossRef] [PubMed]
- Choi, D.; Crockard, H.A. Evolution of Transoral Surgery. Neurosurgery 2013, 73, 296–304. [Google Scholar] [CrossRef]
- Visocchi, M.; Mattogno, P.P.; Ciappetta, P.; Barbagallo, G.; Signorelli, F. Combined Transoral Exoscope and OArm-Assisted Approach for Craniovertebral Junction Surgery: Light and Shadows in Single-Center Experience with Improving Technologies. J. Craniovertebr. Junction Spine 2020, 11, 293–299. [Google Scholar] [CrossRef]
- Frempong-Boadu, A.K.; Faunce, W.A.; Fessler, R.G. Endoscopically Assisted Transoral-Transpharyngeal Approach to the Craniovertebral Junction. Neurosurgery 2002, 51, S2-60–S2-66. [Google Scholar] [CrossRef]
- Hagan, M.J.; Remacle, T.; Leary, O.P.; Feler, J.; Shaaya, E.; Ali, R.; Zheng, B.; Bajaj, A.; Traupe, E.; Kraus, M.; et al. Navigation Techniques in Endoscopic Spine Surgery. Biomed. Res. Int. 2022, 2022, 8419739. [Google Scholar] [CrossRef]
- Hadley, M.N.; Spetzler, R.F.; Sonntag, V.K.H. The Transoral Approach to the Superior Cervical Spine. A Review of 53 Cases of Extradural Cervicomedullary Compression. J. Neurosurg. 1989, 71, 16–23. [Google Scholar] [CrossRef]
- Shousha, M.; Mosafer, A.; Boehm, H. Infection Rate After Transoral Approach for the Upper Cervical Spine. Spine 2014, 39, 1578–1583. [Google Scholar] [CrossRef] [PubMed]
- Steinberger, J.; Skovrlj, B.; Lee, N.J.; Kothari, P.; Leven, D.M.; Guzman, J.Z.; Shin, J.; Shrivastava, R.; Caridi, J.M.; Cho, S.K. Surgical Morbidity and Mortality Associated With Transoral Approach to the Cervical Spine. Spine 2016, 41, E535–E540. [Google Scholar] [CrossRef]
- Ohara, Y.; Nakajima, Y.; Kimura, T.; Kikuchi, N.; Sagiuchi, T. Full-Endoscopic Transcervical Ventral Decompression for Pathologies of Craniovertebral Junction: Case Series. Neurospine 2020, 17, S138–S144. [Google Scholar] [CrossRef] [PubMed]
- Ohara, Y.; Uchikado, H.; Hara, T.; Nojiri, H.; Abe, E.; Kikuchi, N.; Kimura, T. Endoscopic Approach for A Difficult Cervical Area: Fully Endoscopic Uniportal Transcervical Approach for Ventral Pathologies of the Craniovertebral Junction. J. Minim. Invasive Spine Surg. Tech. 2023, 8, 21–27. [Google Scholar] [CrossRef]
- Wolinsky, J.-P.; Sciubba, D.M.; Suk, I.; Gokaslan, Z.L. Endoscopic Image-Guided Odontoidectomy for Decompression of Basilar Invagination via a Standard Anterior Cervical Approach. J. Neurosurg. Spine 2007, 6, 184–191. [Google Scholar] [CrossRef] [PubMed]
- Ruetten, S.; Hahn, P.; Oezdemir, S.; Baraliakos, X.; Merk, H.; Godolias, G.; Komp, M. Full-Endoscopic Uniportal Odontoidectomy and Decompression of the Anterior Cervicomedullary Junction Using the Retropharyngeal Approach. Spine 2018, 43, E911–E918. [Google Scholar] [CrossRef]
- Fiani, B.; Houston, R.; Siddiqi, I.; Arshad, M.; Reardon, T.; Gilliland, B.; Davati, C.; Kondilis, A. Retro-Odontoid Pseudotumor Formation in the Context of Various Acquired and Congenital Pathologies of the Craniovertebral Junction and Surgical Techniques. Neurospine 2021, 18, 67–78. [Google Scholar] [CrossRef] [PubMed]
- Mobbs, R.; Phan, K. Minimally Invasive Unilateral Laminectomy for Bilateral Decompression. JBJS Essent. Surg. Tech. 2017, 7, e9. [Google Scholar] [CrossRef]
- Ahn, Y. Anterior Endoscopic Cervical Discectomy: Surgical Technique and Literature Review. Neurospine 2023, 20, 11–18. [Google Scholar] [CrossRef]
- Vergara, P.; Timofeev, I. Minimally Invasive Anterior Cervical Discectomy and Fusion: A Valid Alternative to Open Techniques. Acta Neurochir. 2018, 160, 2467–2471. [Google Scholar] [CrossRef]
- Ye, J.; Liu, B.; Li, J.; Zheng, G.; Duan, K.; Gao, L.; Zhang, C.; Huang, J.; Tang, Y. Full-Endoscopic Uniportal Retropharyngeal Odontoidectomy: A Preliminary Case Report. Front. Surg. 2023, 9, 973064. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, R.E.; Granville, M.; Berti, A. Minimally Invasive Anterior Cervical Discectomy Without Fusion to Treat Cervical Disc Herniations in Patients with Previous Cervical Fusions. Cureus 2017, 9, e1131. [Google Scholar] [CrossRef]
- Lim, K.T. Full Endoscopic Anterior Cervical Discectomy and Interbody Fusion in Patients with Cervical Spondylotic Myelopathy. J. Spinal Surg. 2022, 9, 195. [Google Scholar] [CrossRef]
- Celestre, P.C.; Pazmiño, P.R.; Mikhael, M.M.; Wolf, C.F.; Feldman, L.A.; Lauryssen, C.; Wang, J.C. Minimally Invasive Approaches to the Cervical Spine. Orthop. Clin. N. Am. 2012, 43, 137–147. [Google Scholar] [CrossRef]
- Goldberg, J.L.; Härtl, R.; Elowitz, E. Minimally Invasive Spine Surgery: An Overview. World Neurosurg. 2022, 163, 214–227. [Google Scholar] [CrossRef] [PubMed]
- McClelland, S.; Oren, J.H.; Protopsaltis, T.S.; Passias, P.G. Outpatient Anterior Cervical Discectomy and Fusion: A Meta-Analysis. J. Clin. Neurosci. 2016, 34, 166–168. [Google Scholar] [CrossRef]
- Klingler, J.-H.; Volz, F.; Krüger, M.T.; Kogias, E.; Rölz, R.; Scholz, C.; Sircar, R.; Hubbe, U. Accidental Durotomy in Minimally Invasive Transforaminal Lumbar Interbody Fusion: Frequency, Risk Factors, and Management. Sci. World J. 2015, 2015, 532628. [Google Scholar] [CrossRef]
- Singh Grewal, I.; Singh Grewal, U.; Eadsforth, T.; Pillay, R. Incidental Spinal Durotomies Noted During Spinal Surgery: Incidence and Management. Arch. Orthop. 2020, 1, 76–82. [Google Scholar] [CrossRef]
- Morgenstern, R.; Morgenstern, C. Percutaneous Transforaminal Lumbar Interbody Fusion (PTLIF) with a Posterolateral Approach for the Treatment of Degenerative Disk Disease: Feasibility and Preliminary Results. Int. J. Spine Surg. 2015, 9, 41. [Google Scholar] [CrossRef]
- McCormack, B.M.; Bundoc, R.C.; Ver, M.R.; Ignacio, J.M.F.; Berven, S.H.; Eyster, E.F. Percutaneous Posterior Cervical Fusion with the DTRAX Facet System for Single-Level Radiculopathy: Results in 60 Patients. J. Neurosurg. Spine 2013, 18, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Archavlis, E.; Carvi Y Nievas, M. Comparison of Minimally Invasive Fusion and Instrumentation versus Open Surgery for Severe Stenotic Spondylolisthesis with High-Grade Facet Joint Osteoarthritis. Eur. Spine J. 2013, 22, 1731. [Google Scholar] [CrossRef] [PubMed]
- Villavicencio, A.T.; Burneikiene, S.; Roeca, C.M.; Nelson, E.L.; Mason, A. Minimally Invasive versus Open Transforaminal Lumbar Interbody Fusion. Surg. Neurol. Int. 2010, 1, 12. [Google Scholar] [CrossRef]
- Kotani, Y.; Abumi, K.; Ito, M.; Sudo, H.; Abe, Y.; Minami, A. Mid-Term Clinical Results of Minimally Invasive Decompression and Posterolateral Fusion with Percutaneous Pedicle Screws versus Conventional Approach for Degenerative Spondylolisthesis with Spinal Stenosis. Eur. Spine J. 2012, 21, 1171. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.Y.; Kundnani, V.G.; Merchant, Z.I.; Jain, S.; Kire, N. Superior Facet Joint Violations in Single Level Minimally Invasive and Open Transforaminal Lumbar Interbody Fusion: A Comparative Study. Asian Spine J. 2020, 14, 25. [Google Scholar] [CrossRef]
- Meyer, M.; Farah, K.; Aurélie, T.; Graillon, T.; Dufour, H.; Fuentes, S. Management of Spinal Metastasis by Minimally Invasive Surgical Techniques: Surgical Principles and Indications—A Literature Review. J. Clin. Med. 2023, 12, 5165. [Google Scholar] [CrossRef] [PubMed]
- Giorgi, H.; Blondel, B.; Adetchessi, T.; Dufour, H.; Tropiano, P.; Fuentes, S. Early Percutaneous Fixation of Spinal Thoracolumbar Fractures in Polytrauma Patients. Orthop. Traumatol. Surg. Res. 2014, 100, 449–454. [Google Scholar] [CrossRef]
- Hansen-Algenstaedt, N.; Kwan, M.K.; Algenstaedt, P.; Chiu, C.K.; Viezens, L.; Chan, T.S.; Lee, C.K.; Wellbrock, J.; Chan, C.Y.W.; Schaefer, C. Comparison Between Minimally Invasive Surgery and Conventional Open Surgery for Patients With Spinal Metastasis: A Prospective Propensity Score-Matched Study. Spine 2017, 42, 789–797. [Google Scholar] [CrossRef] [PubMed]
- Defino, H.L.A.; Costa, H.R.T.; Nunes, A.A.; Nogueira Barbosa, M.; Romero, V. Open versus Minimally Invasive Percutaneous Surgery for Surgical Treatment of Thoracolumbar Spine Fractures—A Multicenter Randomized Controlled Trial: Study Protocol. BMC Musculoskelet. Disord. 2019, 20, 397. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Fan, Y.; Dong, J.; Wang, H.; Wang, F.; Liu, Z.; Liu, H.; Feng, Y.; Chen, F.; Huang, Z.; et al. A Retrospective Study Comparing Percutaneous and Open Pedicle Screw Fixation for Thoracolumbar Fractures with Spinal Injuries. Medicine 2017, 96, e8104. [Google Scholar] [CrossRef]
- Hikata, T.; Isogai, N.; Shiono, Y.; Funao, H.; Okada, E.; Fujita, N.; Iwanami, A.; Watanabe, K.; Tsuji, T.; Nakamura, M.; et al. A Retrospective Cohort Study Comparing the Safety and Efficacy of Minimally Invasive Versus Open Surgical Techniques in the Treatment of Spinal Metastases. Clin. Spine Surg. 2017, 30, E1082–E1087. [Google Scholar] [CrossRef] [PubMed]
- Perna, A.; Smakaj, A.; Vitiello, R.; Velluto, C.; Proietti, L.; Tamburrelli, F.C.; Maccauro, G. Posterior Percutaneous Pedicle Screws Fixation Versus Open Surgical Instrumented Fusion for Thoraco-Lumbar Spinal Metastases Palliative Management: A Systematic Review and Meta-Analysis. Front. Oncol. 2022, 12, 884928. [Google Scholar] [CrossRef]
- Goldstein, C.L.; Macwan, K.; Sundararajan, K.; Rampersaud, Y.R. Perioperative Outcomes and Adverse Events of Minimally Invasive versus Open Posterior Lumbar Fusion: Meta-Analysis and Systematic Review. J. Neurosurg. Spine 2016, 24, 416–427. [Google Scholar] [CrossRef]
- Kreinest, M.; Ludes, L.; Türk, A.; Grützner, P.A.; Biglari, B.; Matschke, S. Analysis of Prehospital Care and Emergency Room Treatment of Patients with Acute Traumatic Spinal Cord Injury: A Retrospective Cohort Study on the Implementation of Current Guidelines. Spinal Cord 2017, 55, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Rillig, J.; Keil, H.; Jung, M.; Grützner, P.A.; Matschke, S.; Kreinest, M. Reduction in Traumatic Spine Injuries in the Thoracic and Lumbar Spine with Percutaneous Versus Open Dorsal Stabilization. Clin. Spine Surg. 2020, 33, E288–E293. [Google Scholar] [CrossRef]
- Clark, A.J.; Safaee, M.M.; Khan, N.R.; Brown, M.T.; Foley, K.T. Tubular Microdiscectomy: Techniques, Complication Avoidance, and Review of the Literature. Neurosurg. Focus 2017, 43, E7. [Google Scholar] [CrossRef]
- Zagzoog, N.; Alsunbul, W.; Elgheriani, A.; Takroni, R.; Reddy, K. Mini-Tubular Access Surgery: A Single Surgeon’s 12 Years in the Corridors of the Neuroaxis. J. Neurol. Surg. A Cent. Eur. Neurosurg. 2020, 81, 513–520. [Google Scholar] [CrossRef]
- Obenchain, T.G. Speculum Lumbar Extraforaminal Microdiscectomy. Spine J. 2001, 1, 415–420. [Google Scholar] [CrossRef]
- Hashizume, H.; Kawakami, M.; Kawai, M.; Tamaki, T. A Clinical Case of Endoscopically Assisted Anterior Screw Fixation for the Type II Odontoid Fracture. Spine 2003, 28, E102–E105. [Google Scholar] [CrossRef]
- Rivera, M.; Norman, S.; Sehgal, R.; Juthani, R. Updates on Surgical Management and Advances for Brain Tumors. Curr. Oncol. Rep. 2021, 23, 35. [Google Scholar] [CrossRef]
- Praveen, V.N.R.G.; Rajamani, P.A.; Kulkarni, A.G.; Bhojraj, S.Y.; Rajasekaran, S.; Chhabra, H.S.; Acharya, S.; Rajamani, A.A.; Nene, A.; Shetty, A.P.; et al. A Two-Year Outcome of Various Techniques of Discectomy On Complications: A Multicentric Retrospective Study. J. Minim. Invasive Spine Surg. Tech. 2022, 7, 53–59. [Google Scholar] [CrossRef]
- Rajamani, P.A.; Goparaju, P.; Kulkarni, A.G.; Bhojraj, S.Y.; Rajasekaran, S.; Chhabra, H.S.; Acharya, S.; Rajamani, A.; Nene, A.; Shetty, A.P.; et al. A 2-Year Outcomes and Complications of Various Techniques of Lumbar Discectomy: A Multicentric Retrospective Study. World Neurosurg. 2021, 156, e319–e328. [Google Scholar] [CrossRef] [PubMed]
- Kotheeranurak, V.; Tangdamrongtham, T.; Lin, G.X.; Singhatanadgige, W.; Limthongkul, W.; Yingsakmongkol, W.; Kim, J.S.; Jitpakdee, K. Comparison of Full-Endoscopic and Tubular-Based Microscopic Decompression in Patients with Lumbar Spinal Stenosis: A Randomized Controlled Trial. Eur. Spine J. 2023, 32, 2736–2747. [Google Scholar] [CrossRef]
- Kim, Y.B.; Hyun, S.J. Clinical Applications of the Tubular Retractor on Spinal Disorders. J. Korean Neurosurg. Soc. 2007, 42, 245–250. [Google Scholar] [CrossRef]
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Surgical Treatment for Lumbar Lateral Recess Stenosis with the Full-Endoscopic Interlaminar Approach versus Conventional Microsurgical Technique: A Prospective, Randomized, Controlled Study—Clinical Article. J. Neurosurg. Spine 2009, 10, 476–485. [Google Scholar] [CrossRef] [PubMed]
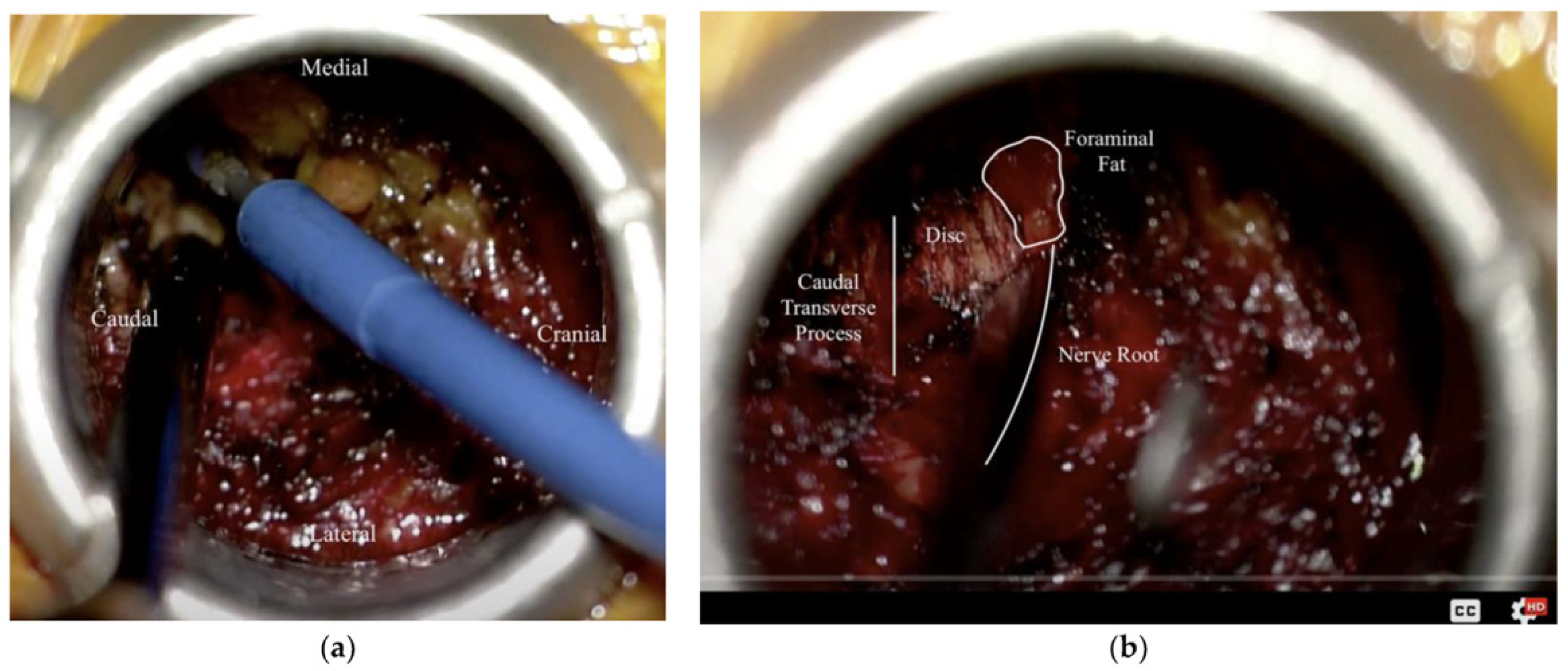
- Echt, M.; Bakare, A.; Fessler, R.G. A Modified Approach for Minimally Invasive Tubular Microdiscectomy for Far Lateral Disc Herniations: Docking at the Caudal Level Transverse Process. Medicina 2022, 58, 640. [Google Scholar] [CrossRef]
- Guinto-Nishimura, G.Y.; Caballero-Delgado, S.; Eguiluz-Meléndez, A.G.; Ortega-Porcayo, L.A.; Valencia-Ramos, C.; Aragon-Arreola, J.F.; Portocarrero-Ortiz, L.; Sangrador-Deitos, M.V.; Gómez-Amador, J.L. Combined Endoscopic Transsphenoidal and Tubular Retractor-Assisted Transventricular Approach for Giant Pituitary Adenomas. World Neurosurg. 2021, 155, e761–e769. [Google Scholar] [CrossRef] [PubMed]
- Mooney, J.; Michalopoulos, G.D.; Alvi, M.A.; Zeitouni, D.; Chan, A.K.; Mummaneni, P.V.; Bisson, E.F.; Sherrod, B.A.; Haid, R.W.; Knightly, J.J.; et al. Minimally Invasive versus Open Lumbar Spinal Fusion: A Matched Study Investigating Patient-Reported and Surgical Outcomes. J. Neurosurg. Spine 2022, 36, 753–766. [Google Scholar] [CrossRef]
- Dimar, J.R.; Carreon, L.Y. Anterior Spine Surgery for the Treatment of Complex Spine Pathology: A State-of-the-Art Review. Spine Deform. 2022, 10, 973–989. [Google Scholar] [CrossRef] [PubMed]
- He, Z.; Li, C.Y.; Mak, C.H.-K.; Tse, T.S.; Cheung, F.C. Minimally Invasive Tubular Retractor Surgery for Intradural Extramedullary Spinal Tumor Reduces Postoperative Degeneration of Paraspinal Muscle. Asian J. Neurosurg. 2022, 17, 74–84. [Google Scholar] [CrossRef] [PubMed]
- Nzokou, A.; Weil, A.G.; Shedid, D. Minimally Invasive Removal of Thoracic and Lumbar Spinal Tumors Using a Nonexpandable Tubular Retractor: Clinical Article. J. Neurosurg. Spine 2013, 19, 708–715. [Google Scholar] [CrossRef]
- Hubbe, U.; Klingler, J.H.; Roelz, R.; Scholz, C.; Argiti, K.; Fistouris, P.; Beck, J.; Vasilikos, I. Double Tubular Minimally Invasive Spine Surgery: A Novel Technique Expands the Surgical Visual Field during Resection of Intradural Pathologies. J. Neurosurg. Spine 2022, 36, 160–163. [Google Scholar] [CrossRef]
- Yu, B.; Xiao, Y.; Dai, H.; Yu, Y.; Lin, Y.; Xu, J. Spinal Intradural Extramedullary Tumors: Microscopic Keyhole Resection with the Focus on Intraoperative Neurophysiological Monitoring and Long-Term Outcome. J. Orthop. Surg. Res. 2023, 18, 598. [Google Scholar] [CrossRef] [PubMed]
- Srikantha, U.; Hari, A.; Lokanath, Y.K.; Subramanian, N.; Varma, R.G. Complete Excision of Intradural-Extraforaminal Spinal Tumors Using a Minimally Invasive 2-Incision Technique with Fixed Tubular Retractors. Clin. Spine Surg. 2021, 34, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Mi, C.; Wang, B.; Pan, Y.; Lin, Y.; Shi, X. Mini-Open Compared with the Trans-Tubular Approach in Patients with Spinal Metastases Underwent Decompression Surgery—A Retrospective Cohort Study. BMC Cancer 2023, 23, 1226. [Google Scholar] [CrossRef]
- Adamson, T.E. Microendoscopic Posterior Cervical Laminoforaminotomy for Unilateral Radiculopathy: Results of a New Technique in 100 Cases. J. Neurosurg. 2001, 95, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Chung, A.S.; Ballatori, A.; Ortega, B.; Min, E.; Formanek, B.; Liu, J.; Hsieh, P.; Hah, R.; Wang, J.C.; Buser, Z. Is Less Really More? Economic Evaluation of Minimally Invasive Surgery. Glob. Spine J. 2021, 11, 30S–36S. [Google Scholar] [CrossRef] [PubMed]
- Lubelski, D.; Mihalovich, K.E.; Skelly, A.C.; Fehlings, M.G.; Harrop, J.S.; Mummaneni, P.V.; Wang, M.Y.; Steinmetz, M.P. Is Minimal Access Spine Surgery More Cost-Effective than Conventional Spine Surgery? Spine 2014, 39, S65–S74. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Yadav, N.; Singh, S.; Chauhan, N. Minimally Invasive (Endoscopic-Computer Assisted) Surgery: Technique and Review. Ann. Maxillofac. Surg. 2016, 6, 159–164. [Google Scholar] [CrossRef]
- Choi, G.; Pophale, C.S.; Patel, B.; Uniyal, P. Endoscopic Spine Surgery. J. Korean Neurosurg. Soc. 2017, 60, 485–497. [Google Scholar] [CrossRef] [PubMed]
- Kwon, H.; Park, J.Y. The Role and Future of Endoscopic Spine Surgery: A Narrative Review. Neurospine 2023, 20, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Chung, A.S.; McKnight, B.; Wang, J.C. Scientific View on Endoscopic Spine Surgery: Can Spinal Endoscopy Become a Mainstream Surgical Tool? World Neurosurg. 2021, 145, 708–711. [Google Scholar] [CrossRef]
- Shen, J.; Telfeian, A.E.; Shaaya, E.; Oyelese, A.; Fridley, J.; Gokaslan, Z.L. Full Endoscopic Cervical Spine Surgery. J. Spine Surg. 2020, 6, 383–390. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.T.; Kim, J.S.; Huang, A.P.H.; Lin, M.H.C.; Chen, C.M. Current Indications for Spinal Endoscopic Surgery and Potential for Future Expansion. Neurospine 2023, 20, 33. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kim, H.S.; Oh, S.W.; Adsul, N.M.; Singh, R.; Kashlan, O.N.; Noh, J.H.; Jang, I.T.; Oh, S.H. Evolution of Spinal Endoscopic Surgery. Neurospine 2019, 16, 6. [Google Scholar] [CrossRef]
- Yue, J.J.; Long, W. Full Endoscopic Spinal Surgery Techniques: Advancements, Indications, and Outcomes. Int. J. Spine Surg. 2015, 9, 17. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.; Sunada, H.; Shiraishi, Y.; Hosokawa, M.; Koh, Y.; Tei, R.; Aketa, S.; Motoyama, Y.; Yonezawa, T.; Nakase, H. Navigation-Assisted Full-Endoscopic Spine Surgery: A Technical Note. J. Spine Surg. 2020, 6, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Jitpakdee, K.; Liu, Y.; Heo, D.H.; Kotheeranurak, V.; Suvithayasiri, S.; Kim, J. Minimally Invasive Endoscopy in Spine Surgery: Where Are We Now? Eur. Spine J. 2023, 32, 2755–2768. [Google Scholar] [CrossRef]
- Choi, J.-Y.; Park, S.-M.; Kim, H.-J.; Yeom, J.S. Recent Updates on Minimally Invasive Spine Surgery: Techniques, Technologies, and Indications. Asian Spine J. 2022, 16, 1013–1021. [Google Scholar] [CrossRef] [PubMed]
- Heo, D.H.; Ha, Y.; Yi, S.; Chung, H. The Future of Minimally Invasive Spine Surgery. Neurol. India 2022, 70, S104–S107. [Google Scholar] [CrossRef] [PubMed]
- Tang, K.; Goldman, S.; Avrumova, F.; Lebl, D.R. Background, Techniques, Applications, Current Trends, and Future Directions of Minimally Invasive Endoscopic Spine Surgery: A Review of Literature. World J. Orthop. 2023, 14, 197–206. [Google Scholar] [CrossRef]
- Ahn, Y. Current Techniques of Endoscopic Decompression in Spine Surgery. Ann. Transl. Med. 2019, 7, S169. [Google Scholar] [CrossRef] [PubMed]
- Birkenmaier, C.; Komp, M.; Leu, H.F.; Wegener, B.; Ruetten, S. The Current State of Endoscopic Disc Surgery: Review of Controlled Studies Comparing Full-Endoscopic Procedures for Disc Herniations to Standard Procedures. Pain Physician 2013, 16, 335. [Google Scholar] [CrossRef]
- Simpson, A.K.; Lightsey, H.M.; Xiong, G.X.; Crawford, A.M.; Minamide, A.; Schoenfeld, A.J. Spinal Endoscopy: Evidence, Techniques, Global Trends, and Future Projections. Spine J. 2022, 22, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Choi, C.M. Biportal Endoscopic Spine Surgery (Bess): Considering Merits and Pitfalls. J. Spine Surg. 2020, 6, 457–465. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.E.; Choi, D.J.; Jin Park, E.J.; Lee, H.J.; Hwang, J.H.; Kim, M.C.; Oh, J.S. Biportal Endoscopic Spinal Surgery for Lumbar Spinal Stenosis. Asian Spine J. 2019, 13, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.W.; Lee, D.G.; Park, C.K. Rationale and Advantages of Endoscopic Spine Surgery. Int. J. Spine Surg. 2021, 15, S11–S20. [Google Scholar] [CrossRef] [PubMed]
- Hasan, S.; Härtl, R.; Hofstetter, C.P. The Benefit Zone of Full-Endoscopic Spine Surgery. J. Spine Surg. 2019, 5, S11–S20. [Google Scholar] [CrossRef] [PubMed]
- Kang, K.B.; Shin, Y.S.; Seo, E.M. Endoscopic Spinal Surgery (BESS and UESS) Versus Microscopic Surgery in Lumbar Spinal Stenosis: Systematic Review and Meta-Analysis. Glob. Spine J. 2022, 12, 1943–1955. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Wu, P.H.; Jang, I.T. Current and Future of Endoscopic Spine Surgery: What Are the Common Procedures We Have Now and What Lies Ahead? World Neurosurg. 2020, 140, 642–653. [Google Scholar] [CrossRef]
- Ruetten, S.; Komp, M.; Merk, H.; Godolias, G. Full-Endoscopic Anterior Decompression versus Conventional Anterior Decompression and Fusion in Cervical Disc Herniations. Int. Orthop. 2009, 33, 1677–1682. [Google Scholar] [CrossRef]
- Ju, C., II; Kim, P.; Seo, J.H.; Kim, S.W.; Lee, S.M. Complications of Cervical Endoscopic Spinal Surgery: A Systematic Review and Narrative Analysis. World Neurosurg. 2023, 178, 330–339. [Google Scholar] [CrossRef]
- Park, M.K.; Park, J.Y.; Son, S.K. Complications of Endoscopic Thoracic Spine Surgery: Overview and Complication Avoidance. World Neurosurg. 2023, 179, 127–132. [Google Scholar] [CrossRef]
- Ju, C., II; Lee, S.M. Complications and Management of Endoscopic Spinal Surgery. Neurospine 2023, 20, 56–77. [Google Scholar] [CrossRef] [PubMed]
- Liang, J.; Lian, L.; Liang, S.; Zhao, H.; Shu, G.; Chao, J.; Yuan, C.; Zhai, M. Efficacy and Complications of Unilateral Biportal Endoscopic Spinal Surgery for Lumbar Spinal Stenosis: A Meta-Analysis and Systematic Review. World Neurosurg. 2022, 159, e91–e102. [Google Scholar] [CrossRef]
- Huang, K.T.; Hazzard, M.; Thomas, S.; Chagoya, G.; Vanden Berg, R.W.; Adogwa, O.; Bagley, C.A.; Isaacs, R.; Gottfried, O.N.; Lad, S.P. Differences in the Outcomes of Anterior versus Posterior Interbody Fusion Surgery of the Lumbar Spine: A Propensity Score-Controlled Cohort Analysis of 10,941 Patients. J. Clin. Neurosci. 2015, 22, 848–853. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohamed, A.A.; Alshaibi, R.; Faragalla, S.; Flynn, G.; Khan, A.; Sargent, E.; Mohamed, Y.; Moriconi, C.; Williams, C.; Karve, Z.; et al. Less Is More: Evaluating the Benefits of Minimally Invasive Spinal Surgery. Life 2025, 15, 8. https://doi.org/10.3390/life15010008
Mohamed AA, Alshaibi R, Faragalla S, Flynn G, Khan A, Sargent E, Mohamed Y, Moriconi C, Williams C, Karve Z, et al. Less Is More: Evaluating the Benefits of Minimally Invasive Spinal Surgery. Life. 2025; 15(1):8. https://doi.org/10.3390/life15010008
Chicago/Turabian StyleMohamed, Ali A., Rakan Alshaibi, Steven Faragalla, Garrett Flynn, Asad Khan, Emma Sargent, Youssef Mohamed, Camberly Moriconi, Cooper Williams, Zev Karve, and et al. 2025. "Less Is More: Evaluating the Benefits of Minimally Invasive Spinal Surgery" Life 15, no. 1: 8. https://doi.org/10.3390/life15010008
APA StyleMohamed, A. A., Alshaibi, R., Faragalla, S., Flynn, G., Khan, A., Sargent, E., Mohamed, Y., Moriconi, C., Williams, C., Karve, Z., Colome, D., Johansen, P. M., & Lucke-Wold, B. (2025). Less Is More: Evaluating the Benefits of Minimally Invasive Spinal Surgery. Life, 15(1), 8. https://doi.org/10.3390/life15010008







