Advantages of Robotic Surgery for Patients of Reproductive Age with Endometrial Cancer
Abstract
1. Introduction
2. Materials and Methods
3. Discussion
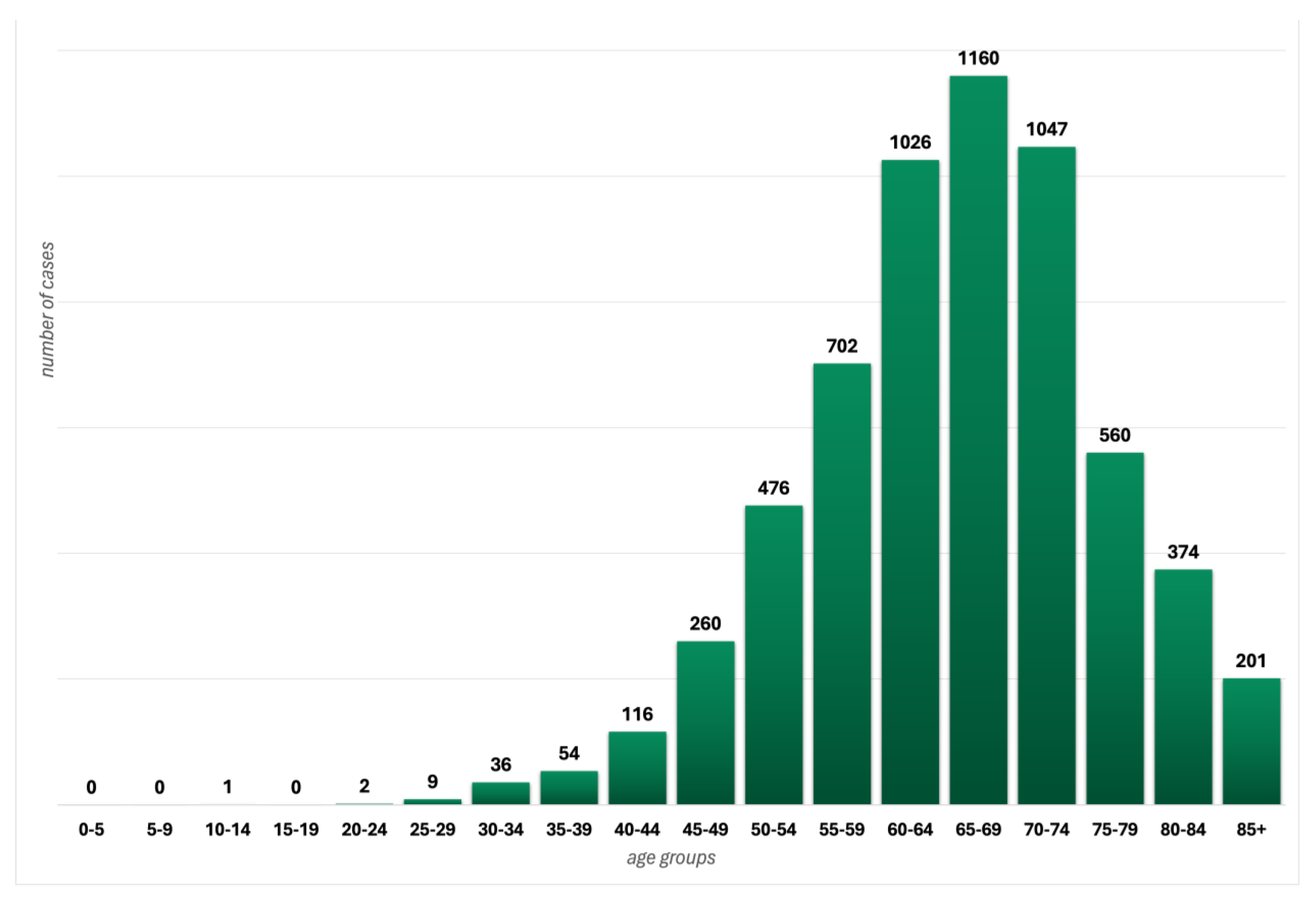
3.1. Epidemiology of Endometrial Cancer at Reproductive Age
3.2. Risk Factors of Endometrial Cancer at a Young Age
3.3. Endometrial Cancer with Genetic Mutation Background
3.4. Fertility-Sparing Treatment at a Young Age
3.5. History of Robotic Surgery
3.6. Robotic Surgery in Gynecology
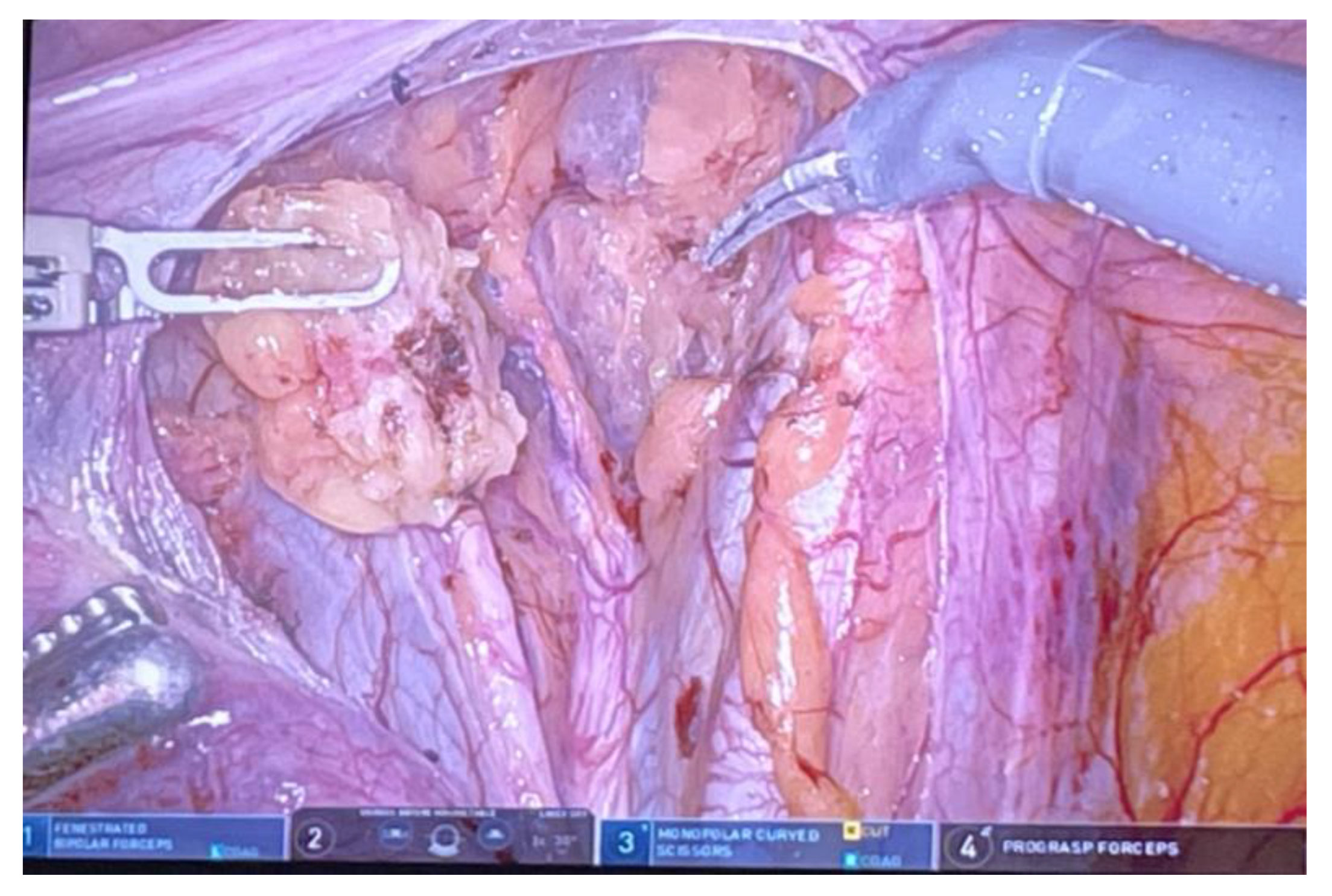
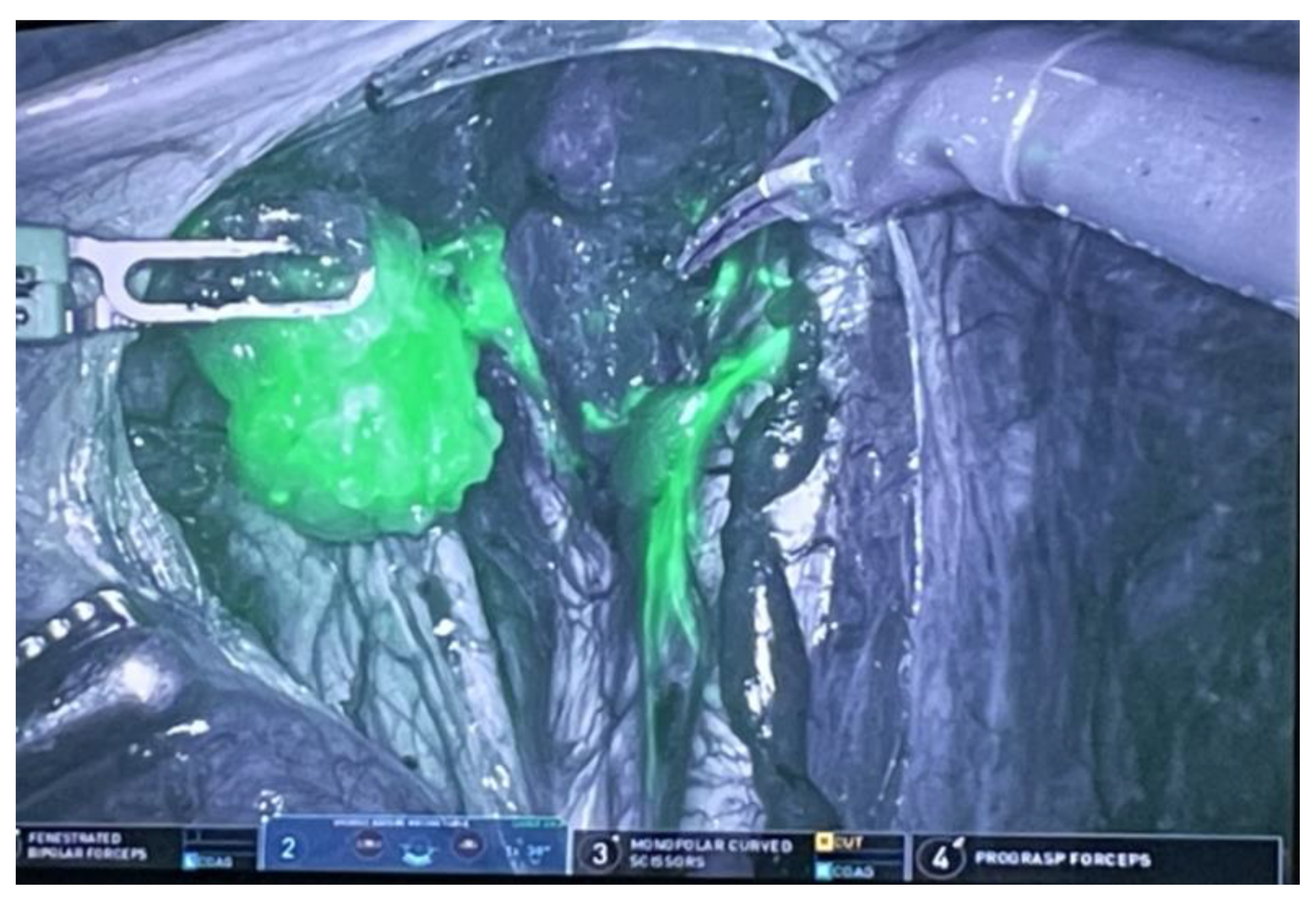
3.7. Robotic Surgery in Endometrial Cancer
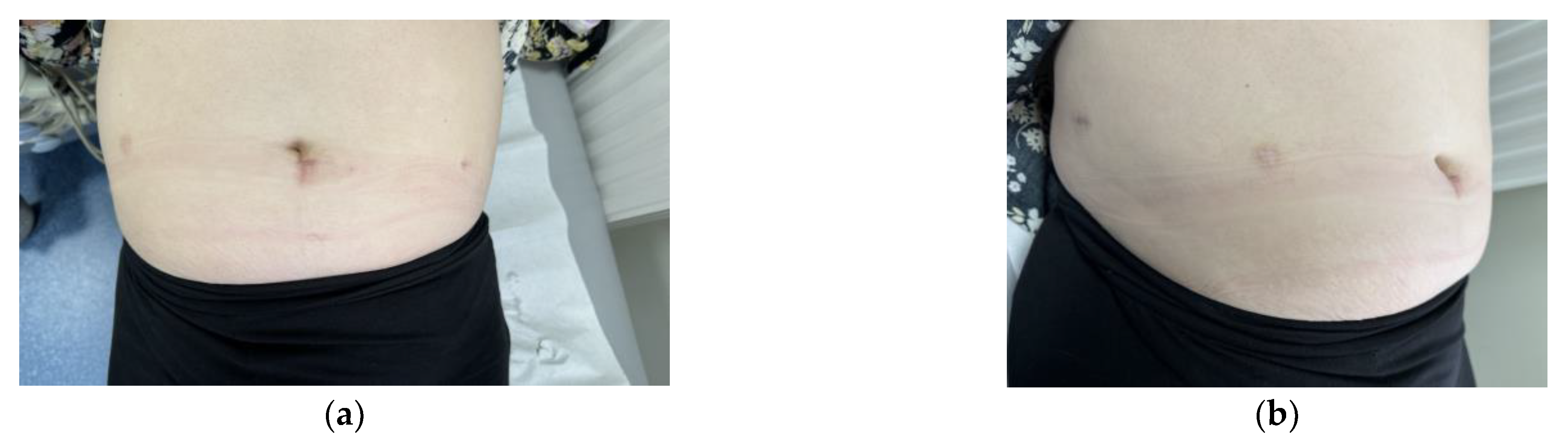
3.8. Benefits of Robotic Surgery at a Young Age
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Constantine, G.; Kessler, G.; Graham, S.; Goldstein, S. Increased incidence of endometrial cancer following the Women’s Health Initiative: An assessment of risk factors. J. Women Health 2019, 28, 237–243. [Google Scholar] [CrossRef]
- Feichitinger, M.; Rodriguez-Wallberg, K. Fertility preservation in women with cervical, endometrial or ovarian cancers. Gynecol. Oncol. Res. Pract. 2016, 3, 8. [Google Scholar] [CrossRef]
- Mukerji, B.; Baptiste, C.; Chen, L.; Tergas, A.; Hou, J.; Ananth, C.; Neugut, A.I.; Hershman, D.L.; Wright, J.D. Racial disparities in young women with endometrial cancer. Gynecol. Oncol. 2018, 148, 527–534. [Google Scholar] [CrossRef]
- Burleigh, A.; Talhouk, A.; Gilks, C.; McAlpine, J. Clinical and pathological characterization of endometrial cancer in young women: Identification of a cohort without classical risk factors. Gynecol. Oncol. 2015, 138, 141–146. [Google Scholar] [CrossRef]
- Rice, L.W. Hormone prevention strategies for breast, endometrial and ovarian cancers. Gynecol. Oncol. 2010, 118, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Concin, N.; Matias-Guiu, X.; Vergote, I.; Cibula, D.; Mirza, M.R.; Marnitz, S.; Ledermann, J.; Bosse, T.; Chargari, C.; Fagotti, A.; et al. ESGO/ESTRO/ESP guidelines for the management of patients with endometrial carcinoma. Int. J. Gynecol. Cancer 2021, 31, 12–39. [Google Scholar] [CrossRef]
- Berek, J.S.; Matias-Guiu, X.; Creutzberg, C.; Fotopoulou, C.; Gaffney, D.; Kehoe, S.; Lindemann, K.; Mutch, D.; Concin, N.; Endometrial Cancer Staging Subcommittee, FIGO Women’s Cancer Committee. FIGO staging of endometrial cancer: 2023. Int. J. Gynaecol. Obstet. 2023, 162, 383–394. [Google Scholar] [CrossRef] [PubMed]
- Colombo, N.; Creutzberg, C.; Amant, F.; Bosse, T.; Gonzalez-Martin, A.; Ledermann, J.; Marth, C.; Nout, R.; Querleu, D.; Mirza, M.; et al. ESMO-ESGO-ESTRO Endometrial Consensus Conference on Endometrial Cancer. Diagnosis, Treatment and Follow-up. Int. J. Gynecol. Cancer 2016, 26, 2–30. [Google Scholar] [CrossRef]
- Rosen, M.W.; Tasset, J.; Kobernik, E.K.; Smith, Y.R.; Johnston, C.; Quint, E.H. Risk Factors for Endometrial Cancer or Hyperplasia in Adolescents and Women 25 Years Old or Younger. J. Pediatr. Adolesc. Gynecol. 2019, 32, 546–549. [Google Scholar] [CrossRef] [PubMed]
- Kido, A.; Himoto, Y.; Kurata, Y.; Minamiguchi, S.; Nakamoto, Y. Preoperative Imaging Evaluation of Endometrial Cancer in FIGO 2023. J. Magn. Reson. Imaging 2023. [Google Scholar] [CrossRef]
- Alcazar, J.L.; Vara, J.; Usandizaga, C.; Ajossa, S.; Pascual, M.A.; Guerriero, S. Transvaginal ultrasound versus magnetic resonance imaging for diagnosing adenomyosis: A systematic review and head-to-head meta-analysis. Int. J. Gynaecol. Obstet. 2023, 161, 397–405. [Google Scholar] [CrossRef]
- Gambadauro, P.; Gudmundsson, J. Endometrial cancer in a woman undergoing hysteroscopy for recurrent IVF failure. Gynecol. Surg. 2017, 14, 4. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Corzo, C.; Santillan, N.B.; Westin, S.N.; Ramirez, P.T. Updates on Conservative Management of Endometrial Cancer. J. Minim. Invasive Gynecol. 2018, 25, 308–313. [Google Scholar] [CrossRef] [PubMed]
- Savelli, L.; Ceccarini, M.; Ludovisi, M.; Fruscella, E.; De Iaco, P.A.; Salizzoni, E.; Mabrouk, M.; Manfredi, R.; Testa, A.C.; Ferrandina, G. Preoperative local staging of endometrial cancer: Transvaginal sonography vs. magnetic resonance imaging. Ultrasound Obstet. Gynecol. 2008, 31, 560–566. [Google Scholar] [CrossRef] [PubMed]
- Savelli, L.; Testa, A.C.; Mabrouk, M.; Zannoni, L.; Ludovisi, M.; Seracchioli, R.; Scambia, G.; De Iaco, P. A prospective blinded comparison of the accuracy of transvaginal sonography and frozen section in assessment of myometrial invasion in endometrial cancer. Gynecol. Oncol. 2012, 124, 549–552. [Google Scholar] [CrossRef] [PubMed]
- Green, R.W.; Valentin, L.; Alcazar, J.L.; Chiappa, V.; Erdodi, B.; Franchi, D.; Fruhauf, F.; Fruscio, R.; Guerriero, S.; Graupera, B.; et al. Endometrial cancer off-line staging using two-dimensional transvaginal ultrasound and three-dimensional volume contrast imaging: Intermethod agreement, interrater reliability and diagnostic accuracy. Gynecol. Oncol. 2018, 150, 438–445. [Google Scholar] [CrossRef]
- Del Pup, L.; Peccatori, F.; Levi-Setti, P.; Godacci-Pisanelli, G.; Patrizio, P. Risk of cancer after assisted reproduction: A review of the available evidences and guidance to fertility counselors. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 8042–8059. [Google Scholar] [CrossRef]
- Wang, Y.; Yang, J. Fertility-preserving treatment in women with early endometrial cancer: The Chinese experience. Cancer Manag. Res. 2018, 10, 6803–6813. [Google Scholar] [CrossRef]
- Hidayat, K.; Zhou, H.; Shi, B. Influence of physical activity at a young age and lifetime physical activity on the risks of 3 obesity-related cancers: Systematic review and meta-analysis of observational studies. Nutr. Rev. 2020, 78, 1–18. [Google Scholar] [CrossRef]
- Cook, L.; Dong, Y.; Round, P.; Huang, X.; Magliocco, A.; Friedenreich, C. Hormone contraception before the first birth and endometrial cancer risk. Cancer Epidemiol. Biomark. Prev. 2014, 23, 356–361. [Google Scholar] [CrossRef]
- Kovalenko, T.; Morozova, K.; Ozolinya, L.; Lapina, I.; Patrushev, L. The PTENP1 pseudogene, unlike the PTEN gene, is methylated in normal endometrium, as well as in endometrial hyperplasias and carcinomas in middle-aged and elderly females. Acta Naturae 2018, 10, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Beiner, M.; Finch, A.; Rosen, B.; Lubinski, J.; Moller, P.; Ghadirian, P.; Lynch, H.; Friedman, E.; Sun, P.; Narod, S. The risk of endometrial cancer in women with BRCA1 and BRCA2 mutations. A prospective study. Gynecol. Oncol. 2007, 104, 7–10. [Google Scholar] [CrossRef]
- Pennington, K.; Walsh, T.; Lee, M.; Pennil, C.; Novetsky, A.; Agnew, K.; Thornton, A.; Garcia, R.; Mutch, D.; King, M.; et al. BRCA1, TP53, and CHEK2 germline mutations in uterine serous carcinoma. Cancer 2013, 119, 332–338. [Google Scholar] [CrossRef]
- Levine, D.; Lin, O.; Barakat, R.; Robson, M.; McDermott, D.; Cohen, L.; Satagopan, J.; Offit, K.; Boyd, J. Risk of endometrial carcinoma associated with BRCA mutation. Gynecol. Oncol. 2001, 80, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Laitman, Y.; Michaelson-Cohen, R.; Levi, E.; Chen-Shtoyerman, R.; Reish, O.; Ben-Yehoshua, S.; Bernstein-Molho, R.; Keinan-Boker, L.; Rosengarten, O.; Silverman, B.; et al. Uterine cancer in Jewish Israeli BRCA1/2 mutation carriers. Cancer 2019, 125, 698–703. [Google Scholar] [CrossRef] [PubMed]
- Streff, H.; Profato, J.; Ye, Y.; Nebgen, D.; Peterson, S.; Singletary, C.; Arun, B.; Litton, J. Cancer incidence in first- and second-degree relatives of BRCA1 and BRCA2 mutation carriers. Oncologist 2016, 21, 869–874. [Google Scholar] [CrossRef] [PubMed]
- Silvestris, E.; Cormio, G.; Loizzi, V.; Corrado, G.; Arezzo, F.; Petracca, E.A. Fertility Preservation in BRCA1/2 Germline Mutation Carriers: An Overview. Life 2024, 14, 615. [Google Scholar] [CrossRef]
- Ryan, N.A.J.; Glaire, M.A.; Blake, D.; Cabrera-Dandy, M.; Evans, D.G.; Crosbie, E.J. The proportion of endometrial cancers associated with Lynch syndrome: A systematic review of the literature and meta-analysis. Genet. Med. 2019, 21, 2167–2180. [Google Scholar] [CrossRef]
- Møller, P.; Seppälä, T.; Bernstein, I.; Holinski-Feder, E.; Sala, P.; Evans, D.G.; Lindblom, A.; Macrae, F.; Blanco, I.; Sijmons, R.; et al. Cancer incidence and survival in Lynch syndrome patients receiving colonoscopic and gynaecological surveillance: First report from the prospective Lynch syndrome database. Gut 2017, 66, 464–472. [Google Scholar] [CrossRef]
- Ryan, N.A.J.; Morris, J.; Green, K.; Lalloo, F.; Woodward, E.R.; Hill, J.; Crosbie, E.J.; Evans, D.G. Association of Mismatch Repair Mutation with Age at Cancer Onset in Lynch Syndrome: Implications for Stratified Surveillance Strategies. JAMA Oncol. 2017, 3, 1702–1706. [Google Scholar] [CrossRef]
- Gullo, G.; Etrusco, A.; Cucinella, G.; Perino, A.; Chiantera, V.; Laganà, A.S.; Tomaiuolo, R.; Vitagliano, A.; Giampaolino, P.; Noventa, M.; et al. Fertility-Sparing Approach in Women Affected by Stage I and Low-Grade Endometrial Carcinoma: An Updated Overview. Int. J. Mol. Sci. 2021, 22, 11825. [Google Scholar] [CrossRef]
- Garzon, S.; Uccella, S.; Zorzato, P.C.; Bosco, M.; Franchi, M.P.; Student, V.; Mariani, A. Fertility-sparing management for endometrial cancer: Review of the literature. Minerva Med. 2021, 112, 55–69. [Google Scholar] [CrossRef] [PubMed]
- Edmondson, R.J.; Crosbie, E.J.; Nickkho-Amiry, M.; Kaufmann, A.; Stelloo, E.; Nijman, H.W.; Leary, A.; Auguste, A.; Mileshkin, L.; Pollock, P.; et al. Markers of the p53 pathway further refine molecular profiling in high-risk endometrial cancer: A TransPORTEC initiative. Gynecol. Oncol. 2017, 146, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Xu, Y.; Zhu, Q.; Xie, L.; Shan, W.; Ning, C.; Xie, B.; Shi, Y.; Luo, X.; Zhang, H.; et al. Treatment efficiency of comprehensive hysteroscopic evaluation and lesion resection combined with progestin therapy in young women with endometrial atypical hyperplasia and endometrial cancer. Gynecol. Oncol. 2019, 153, 55–62. [Google Scholar] [CrossRef]
- Chae, S.H.; Shim, S.H.; Lee, S.J.; Lee, J.Y.; Kim, S.N.; Kang, S.B. Pregnancy and oncologic outcomes after fertility-sparing management for early stage endometrioid endometrial cancer. Int. J. Gynecol. Cancer 2019, 29, 77–85. [Google Scholar] [CrossRef]
- Giampaolino, P.; Di Spiezio Sardo, A.; Mollo, A.; Raffone, A.; Travaglino, A.; Boccellino, A.; Zizolfi, B.; Insabato, L.; Zullo, F.; De Placido, G.; et al. Hysteroscopic Endometrial Focal Resection followed by Levonorgestrel Intrauterine Device Insertion as a Fertility-Sparing Treatment of Atypical Endometrial Hyperplasia and Early Endometrial Cancer: A Retrospective Study. J. Minim. Invasive Gynecol. 2019, 26, 648–656. [Google Scholar] [CrossRef]
- Tamauchi, S.; Kajiyama, H.; Utsumi, F.; Suzuki, S.; Niimi, K.; Sakata, J.; Mizuno, M.; Shibata, K.; Kikkawa, F. Efficacy of medroxyprogesterone acetate treatment and retreatment for atypical endometrial hyperplasia and endometrial cancer. J. Obstet. Gynaecol. Res. 2018, 44, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.R.; van der Zanden, C.; Ikiz, H.; Kuzelijevic, B.; Havelock, J.; Kwon, J.S. Fertility-Sparing Management Using Progestin for Young Women with Endometrial Cancer From a Population-Based Study. J. Obstet. Gynaecol. Can. 2018, 40, 328–333. [Google Scholar] [CrossRef]
- Yamagami, W.; Susumu, N.; Makabe, T.; Sakai, K.; Nomura, H.; Kataoka, F.; Hirasawa, A.; Banno, K.; Aoki, D. Is repeated high-dose medroxyprogesterone acetate (MPA) therapy permissible for patients with early stage endometrial cancer or atypical endometrial hyperplasia who desire preserving fertility? J. Gynecol. Oncol. 2018, 29, e21. [Google Scholar] [CrossRef]
- Fan, Z.; Li, H.; Hu, R.; Liu, Y.; Liu, X.; Gu, L. Fertility-Preserving Treatment in Young Women With Grade 1 Presumed Stage IA Endometrial Adenocarcinoma: A Meta-Analysis. Int. J. Gynecol. Cancer 2018, 28, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Leone Roberti Maggiore, U.; Khamisy-Farah, R.; Bragazzi, N.L.; Bogani, G.; Martinelli, F.; Lopez, S.; Chiappa, V.; Signorelli, M.; Ditto, A.; Raspagliesi, F. Fertility-Sparing Treatment of Patients with Endometrial Cancer: A Review of the Literature. J. Clin. Med. 2021, 10, 4784. [Google Scholar] [CrossRef] [PubMed]
- Greenwald, Z.R.; Huang, L.N.; Wissing, M.D.; Franco, E.L.; Gotlieb, W.H. Does hormonal therapy for fertility preservation affect the survival of young women with early-stage endometrial cancer? Cancer 2017, 123, 1545–1554. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Qi, G.; Kanis, M.J.; Dong, R.; Cui, B.; Yang, X.; Kong, B. Comparison among fertility-sparing therapies for well differentiated early-stage endometrial carcinoma and complex atypical hyperplasia. Oncotarget 2017, 8, 57642–57653. [Google Scholar] [CrossRef]
- Hwang, J.Y.; Kim, D.H.; Bae, H.S.; Kim, M.L.; Jung, Y.W.; Yun, B.S.; Seong, S.J.; Shin, E.; Kim, M.K. Combined oral medroxyprogesterone/levonorgestrel-intrauterine system treatment for women with grade 2 stage IA endometrial cancer. Int. J. Gynecol. Cancer 2017, 27, 738–742. [Google Scholar] [CrossRef] [PubMed]
- Koskas, M.; Uzan, J.; Luton, D.; Rouzier, R.; Daraï, E. Prognostic factors of oncologic and reproductive outcomes in fertility-sparing management of endometrial atypical hyperplasia and adenocarcinoma: Systematic review and meta-analysis. Fertil. Steril. 2014, 101, 785–794. [Google Scholar] [CrossRef]
- Lauterbach, R.; Matanes, E.; Lowenstein, L. Review of robotic surgery in gynecology—The future is here. Rambam Maimonides Med. J. 2017, 8, 2. [Google Scholar] [CrossRef] [PubMed]
- Witkiewicz, W. Robotic surgery—A new quality and breakthrough or an expensive gadget? Nowotw. J. Oncol. 2013, 63, 423–429. [Google Scholar] [CrossRef]
- Saceanu, S.; Cela, V.; Pluchino, N.; Angelescu, C.; Surlin, V.; Genazzani, A. Robotic-assisted laparoscopic surgery in uterine pathology. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 169, 340–342. [Google Scholar] [CrossRef]
- Conrad, L.; Ramirez, P.; Burke, W.; Naumann, W.; Ring, K.; Munsell, M.; Frumovitz, M. Role of minimally invasive surgery in gynecologic oncology: An updated survey of members of the Society of Gynecologic Oncology. Int. J. Gynecol. Cancer 2015, 25, 1121–1127. [Google Scholar] [CrossRef]
- Colombo, N.; Sessa, C.; du Bois, A.; Ledermann, J.; McCluggage, W.G.; McNeish, I.; Morice, P.; Pignata, S.; Ray-Coquard, I.; Vergote, I.; et al. ESMO-ESGO consensus conference recommendations on ovarian cancer: Pathology and molecular biology, early and advanced stages, borderline tumours and recurrent disease. Ann. Oncol. 2019, 30, 672–705. [Google Scholar] [CrossRef]
- Joliniere, J.; Librino, A.; Dubuisson, J.; Khomsi, F.; Ali, N.; Fadhlaoui, A.; Ayoubi, J.; Feki, A. Robotic Surgery in Gynecology. Front. Surg. 2016, 3, 26. [Google Scholar] [CrossRef]
- Gu, H.; Li, J.; Gu, Y.; Tu, H.; Zhou, Y.; Liu, J. Survival Impact of Ovarian Preservation on Women With Early-Stage Endometrial Cancer: A Systematic Review and Meta-analysis. Int. J. Gynecol. Cancer 2017, 27, 77–84. [Google Scholar] [CrossRef]
- Anggraeni, T.D.; Al Fattah, A.N.; Surya, R. Prophylactic salpingectomy and ovarian cancer: An evidence-based analysis. S. Asian J. Cancer 2018, 7, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Peccatori, F.A.; Mangili, G.; Bergamini, A.; Filippi, F.; Martinelli, F.; Ferrari, F.; Noli, S.; Rabaiotti, E.; Candiani, M.; Somigliana, E. Fertility preservation in women harboring deleterious BRCA mutations: Ready for prime time? Hum. Reprod. 2018, 33, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Tinelli, R.; Cicinelli, E.; Tinelli, A.; Bettocchi, S.; Angioni, S.; Litta, P. Laparoscopic treatment of early-stage endometrial cancer with and without uterine manipulator: Our experience and review of literature. Surg. Oncol. 2016, 25, 98–103. [Google Scholar] [CrossRef]
- Satei, J.; Afrakhteh, A.N.; Aldecoa, K.A.T. Endometrial Adenocarcinoma in Young Women: A Case Report and Review of Literature. Cureus 2023, 15, e45287. [Google Scholar] [CrossRef]
- Rütten, H.; Verhoef, C.; van Weelden, W.J.; Smits, A.; Dhanis, J.; Ottevanger, N.; Pijnenborg, J.M.A. Recurrent Endometrial Cancer: Local and Systemic Treatment Options. Cancers 2021, 13, 6275. [Google Scholar] [CrossRef]
- Kim, S.I.; Park, D.C.; Lee, S.J.; Yoo, J.G.; Song, M.J.; Kim, C.J.; Lee, H.N.; Yoon, J.H. Minimally invasive surgery for patients with advanced stage endometrial cancer. Int. J. Med. Sci. 2021, 18, 1153–1158. [Google Scholar] [CrossRef] [PubMed]
- Eoh, K.J.; Kim, T.J.; Park, J.Y.; Kim, H.S.; Paek, J.; Kim, Y.T. Robot-assisted versus conventional laparoscopic surgery for endometrial cancer: Long-term comparison of outcomes. Front. Oncol. 2023, 13, 1219371. [Google Scholar] [CrossRef]
- Bruno, M.; Legge, F.; Gentile, C.; Carone, V.; Stabile, G.; Di Leo, F.; Ludovisi, M.; Di Florio, C.; Guido, M. Risk assessment model of complications in minimally invasive hysterectomy: A pilot study. Int. J. Environ. Res. Public Health 2023, 20, 234. [Google Scholar] [CrossRef]
- Saini, A.; Suh, L.; Gao, J.; Leung, K.; Wilkie, G.; Matteson, K.; Korets, S. Intra-operative tumor spillage in minimally invasive surgery for endometrial cancer and its impact on recurrence risk. Gynecol. Oncol. 2023, 175, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Limbachiya, D.; Tiwari, R.; Kumari, R. Prospective Study on the Use of Endo-Stapler for Enclosed Colpotomy to Prevent Tumor Spillage in Gynecologic Oncology Minimally Invasive Surgeries. JSLS J. Soc. Laparosc. Robot. Surg. 2023, 27, e2023.00019. [Google Scholar] [CrossRef] [PubMed]
- Mereu, L.; Berlanda, V.; Surico, D.; Gardella, B.; Pertile, R.; Spinillo, A.; Tateo, S. Evaluation of quality of life, body image and surgical outcomes of robotic total laparoscopic hysterectomy and sentinel lymph node mapping in low-risk endometrial cancer patients—A Robotic Gyne Club study. Acta Obstet. Gynecol. Scand. 2020, 99, 1238–1245. [Google Scholar] [CrossRef]
- Galaal, K.; Donkers, H.; Bryant, A.; Lopes, A.D. Laparoscopy versus laparotomy for the management of early stage endometrial cancer. Cochrane Database Syst. Rev. 2018, 10, CD006655. [Google Scholar] [CrossRef] [PubMed]
- Sinno, A.K.; Fader, A.N. Robotic-assisted surgery in gynecologic oncology. Fertil. Steril. 2014, 102, 922–932. [Google Scholar] [CrossRef] [PubMed]
- Bramhe, S.; Pathak, S.S. Robotic surgery: A narrative review. Cureus 2022, 14, 9. [Google Scholar] [CrossRef]
- Neto, J.S.; Siufi, D.F.; Magrina, J.F. Robotic nerve-sparing radical hysterectomy. Minerva Ginecol. 2015, 67, 281–287. Available online: https://www.minervamedica.it/en/journals/minerva-obstetrics-gynecology/article.php?cod=R09Y2015N03A0281 (accessed on 25 June 2024).
- Magrina, J.F.; Pawlina, W.; Kho, R.M.; Magtibay, P.M. Robotic nerve-sparing radical hysterectomy: Feasibility and technique. Gynecol. Oncol. 2011, 121, 605–609. [Google Scholar] [CrossRef]
- Magrina, J.; Yang, J.; Yi, J.; Wasson, M. Nerve-sparing in Gynecology. J. Minim. Invasive Gynecol. 2021, 28, 387. [Google Scholar] [CrossRef]
- Puntambekar, S.P.; Lawande, A.; Desai, R.; Kenawadekar, R.; Joshi, S.; Joshi, G.A. Nerve-sparing robotic radical hysterectomy: Our technique. J. Robot. Surg. 2014, 8, 43–47. [Google Scholar] [CrossRef]
- Paek, J.; Kang, E.; Lim, P.C. Comparative analysis of genitourinary function after type C1 robotic nerve-sparing radical hysterectomy versus type C2 robotic radical hysterectomy. Surg. Oncol. 2019, 30, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Nezhat, C.; Nguyen, K.; Ackroyd, E.; Roman, R.A.; Rambhatla, A.; Nezhat, A.; Asiaii, A. Nerve-Sparing Modified Radical Hysterectomy for Severe Endometriosis and Complex Pelvic Pathology. Cureus 2020, 12, e9882. [Google Scholar] [CrossRef] [PubMed]
- Hiramatsu, Y. Nerve-Sparing Robotic Radical Hysterectomy for the Beginner in Robotic Surgery. Surg. J. 2021, 7, S84–S96. [Google Scholar] [CrossRef] [PubMed]
- García-Pineda, V.; Hernández, A.; Garrido-Mallach, S.; Rodríguez-González, E.; Alonso-Espías, M.; Gracia, M.; Arnedo, R.; Zapardiel, I. Sentinel Lymph Node Impact on the Quality of Life of Patients with Endometrial Cancer. J. Pers. Med. 2023, 13, 847. [Google Scholar] [CrossRef]
- Salehi, S.; Brandberg, Y.; Avall-Lundqvist, E.; Suzuki, C.; Johansson, H.; Legerstam, B.; Falconer, H. Long-term quality of life after comprehensive surgical staging of high-risk endometrial cancer—Results from the RASHEC trial. Acta Oncol. 2018, 57, 1671–1676. [Google Scholar] [CrossRef]
- Bergstrom, J.; Aloisi, A.; Armbruster, S.; Yen, T.; Casarin, J.; Leitao, M.; Tanner, E.; Matsuno, R.; Machado, K.; Dowdy, S.; et al. Minimally invasive hysterectomy surgery rates for endometrial cancer performer at National Comprehensive Cancer Network (NCCN) Networks. Gynecol. Oncol. 2018, 148, 480–484. [Google Scholar] [CrossRef]
- Lee, J.; Kim, K.; Lee, Y.; Kim, H.; Nam, E.; Kim, S.; Kim, S.W.; Kim, J.W.; Kim, Y.T. Treatment preferences for routine lymphadenectomy versus no lymphadenectomy in early-stage endometrial cancer. Ann. Surg. Oncol. 2017, 24, 1336–1342. [Google Scholar] [CrossRef] [PubMed]
- Minamikawa, T.; Yachida, N.; Takahashi, K.; Saito, K.; Sekizuka, T.; Akashi, H.; Suzuki, M.; Mori, Y.; Yamawaki, K.; Suda, K.; et al. Endometrial Cancer with and without Endometriosis: Clinicopathological Differences. Cancers 2023, 15, 5635. [Google Scholar] [CrossRef]
- Sinha, R.; Rallabandi, H.; Bana, R.; Bag, M.; Raina, R.; Sridhar, D.; Deepika, H.K.; Reddy, P. Ovarian Loss in Laparoscopic and Robotic Cystectomy Compared Using Artificial Intelligence Pathology. JSLS J. Soc. Laparosc. Robot. Surg. 2024, 28, e2024.00001. [Google Scholar] [CrossRef]
- Wright, J.; Huang, Y.; Melamed, A.; Tergas, A.; St Clair, C.; Hou, Y.; Khoury-Collado, F.; Ananth, C.; Neugut, A.; Hershman, D. Use and misuse of opioids after gynecologic surgical procedures. Obstet. Gynecol. 2019, 134, 250–260. [Google Scholar] [CrossRef]
- Arms, R.G.; Sun, C.; Burzawa, J.; Fleming, N.; Nick, A.; Rallapalli, V.; Westin, S.; Meyer, L.; Ramirez, P.; Soliman, P. Improvement in quality of life after robotic surgery results in patient satisfaction. Gynecol. Oncol. 2015, 138, 727–730. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Li, Z.; Huang, R.; Xue, H. Robot-assisted versus conventional laparoscopic surgery for endometrial cancer staging: A meta-analysis. Taiwan J. Obstet. Gynecol. 2016, 55, 488–494. [Google Scholar] [CrossRef]
- So, S.C.Y.; Ng, D.W.L.; Liao, Q.; Fielding, R.; Soong, I.; Chan, K.K.L.; Lee, C.; Ng, A.W.Y.; Sze, W.K.; Chan, W.L.; et al. Return to Work and Work Productivity During the First Year After Cancer Treatment. Front. Psychol. 2022, 13, 866346. [Google Scholar] [CrossRef]
- Mamguem Kamga, A.; Bengrine-Lefevre, L.; Quipourt, V.; Favier, L.; Darut-Jouve, A.; Marilier, S.; Arveux, P.; Desmoulins, I.; Dabakuyo-Yonli, T.S. Long-term quality of life and sexual function of elderly people with endometrial or ovarian cancer. Health Qual. Life Outcomes 2021, 19, 56. [Google Scholar] [CrossRef]
- Pizetta, L.M.; Reis, A.D.C.; Méxas, M.P.; Guimarães, V.A.; de Paula, C.L. Management Strategies for Sexuality Complaints after Gynecologic Cancer: A Systematic Review. Rev. Bras. Ginecol. Obstet. 2022, 44, 962–971. [Google Scholar] [CrossRef] [PubMed]
- Quinn, B.A.; Deng, X.; Sullivan, S.A.; Carter, J.; Bandyopadhyay, D.; Fields, E.C. Change in vaginal length and sexual function in women who undergo surgery ± radiation therapy for endometrial cancer. Brachytherapy 2023, 22, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Gallardo-Rincón, D.; Toledo-Leyva, A.; Bahena-Gonzalez, A.; Montes-Servin, E.; Perez-Martin, A.R.; Montes-Servin, E.; Alamilla-Garcia, G.C.; Carmona-Herrera, D.D.; Coronel-Martinez, J.; Onate-Ocana, L.F. Validation of the QLQ-EN24 instrument for the assessment of health-related quality of life for women with endometrial cancer in Mexico. Arch. Gynecol. Obstet. 2021, 304, 773–782. [Google Scholar] [CrossRef] [PubMed]
- Datta, A.; Ram, T.S.; Karuppusami, R.; Thomas, A.; Sebastian, A.; Thomas, V.; Chandy, R.G.; Peedicayil, A. A longitudinal study of sexual health and quality of life in endometrial carcinoma survivors. Int. J. Gynecol. Cancer 2023, 33, 890–896. [Google Scholar] [CrossRef]
- Sobočan, M.; Gašpar, D.; Gjuras, E.; Knez, J. Evaluation of Patient-Reported Symptoms and Functioning after Treatment for Endometrial Cancer. Curr. Oncol. 2022, 29, 5213–5222. [Google Scholar] [CrossRef]
- Roussin, M.; Hamilton, A.; Lowe, J.; Martin, L. Sexual quality of life after gynaecological cancer: What young women want. Qual. Life Res. 2024, 33, 679–689. [Google Scholar] [CrossRef]
- Ashrafian, H.; Clancy, O.; Grover, V.; Darzi, A. The evolution of robotic surgery: Surgical and anaesthetic aspects. Br. J. Anaesth. 2017, 119, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Armbruster, S.; Song, J.; Bradford, A.; Carmack, C.; Lu, K.; Basen-Engquist, K. Sexual health of endometrial cancer survivors before and after a physical activity intervention: A retrospective cohort analysis. Gynecol. Oncol. 2016, 143, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.H.; Yun, C.Y.; Choi, S.; Park, D.S.; Kim, S.I. Is robotic surgery beneficial for the treatment of endometrial cancer? A comparison with conventional laparoscopic surgery. J. Cancer 2024, 15, 533–538. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bizoń, M.; Roszkowska, Z.; Kalisz, R.; Szarpak, Ł.; Olszewski, M. Advantages of Robotic Surgery for Patients of Reproductive Age with Endometrial Cancer. Life 2024, 14, 1108. https://doi.org/10.3390/life14091108
Bizoń M, Roszkowska Z, Kalisz R, Szarpak Ł, Olszewski M. Advantages of Robotic Surgery for Patients of Reproductive Age with Endometrial Cancer. Life. 2024; 14(9):1108. https://doi.org/10.3390/life14091108
Chicago/Turabian StyleBizoń, Magdalena, Zuzanna Roszkowska, Renata Kalisz, Łukasz Szarpak, and Maciej Olszewski. 2024. "Advantages of Robotic Surgery for Patients of Reproductive Age with Endometrial Cancer" Life 14, no. 9: 1108. https://doi.org/10.3390/life14091108
APA StyleBizoń, M., Roszkowska, Z., Kalisz, R., Szarpak, Ł., & Olszewski, M. (2024). Advantages of Robotic Surgery for Patients of Reproductive Age with Endometrial Cancer. Life, 14(9), 1108. https://doi.org/10.3390/life14091108






