The Influence of Fine Particulate Matter and Cold Weather on Emergency Room Interventions for Childhood Asthma
Abstract
1. Introduction
2. Materials and Methods
2.1. Pediatric Asthma Emergency Room Visits and Air Pollution
2.2. Statistical Analysis
3. Results
| AT | RH | PM2.5 | O3 | CO | SO2 | NO2 | CH4 | NMCHs | THC | |
|---|---|---|---|---|---|---|---|---|---|---|
| AT | 1 | −0.51 | −0.44 | −0.4 | −0.55 | 0.46 | −0.67 | −0.69 | −0.14 | −0.56 |
| p | 0.02 * | 0.05 | 0.08 | 0.02 * | 0.04 * | <0.01 * | <0.01 * | 0.57 | 0.01 * | |
| RH | −0.51 | 1 | 0.07 | 0.12 | 0.22 | −0.61 | 0.29 | 0.1 | −0.02 | 0.2 |
| p | 0.02 * | 0.78 | 0.62 | 0.36 | <0.01 * | 0.22 | 0.67 | 0.94 | 0.4 | |
| PM2.5 | −0.44 | 0.07 | 1 | 0.37 | 0.9 | 0.34 | 0.81 | 0.81 | 0.79 | 0.89 |
| p | 0.05 | 0.78 | 0.2 | <0.01 * | 0.14 | <0.01 * | <0.01 * | <0.01 * | <0.01 * | |
| O3 | −0.4 | 0.12 | 0.3 | 1 | 0.21 | −0.04 | 0.26 | 0.18 | −0.01 | 0.21 |
| p | 0.08 | 0.62 | 0.2 | 0.37 | 0.85 | 0.26 | 0.45 | 0.98 | 0.37 | |
| CO | −0.5 | 0.22 | 0.9 | 0.21 | 1 | 0.27 | 0.93 | 0.86 | 0.88 | 0.95 |
| p | 0.02 * | 0.35 | <0.01 * | 0.37 | 0.25 | <0.01 * | <0.01 * | <0.01 * | <0.01 * | |
| SO2 | 0.46 | −0.61 | 0.34 | −0.04 | 0.27 | 1 | 0.12 | 0.17 | 0.49 | 0.35 |
| p | 0.04 * | <0.01 * | 0.14 | 0.85 | 0.25 | 0.6 | 0.48 | 0.03 * | 0.13 | |
| NO2 | −0.67 | 0.29 | 0.81 | 0.26 | 0.93 | 0.12 | 1 | 0.89 | 0.75 | 0.96 |
| p | <0.01 * | 0.22 | <0.01 * | 0.26 | <0.01 * | 0.6 | <0.01 * | <0.01 * | <0.01 * | |
| CH4 | −0.69 | 0.1 | 0.8 | 0.18 | 0.86 | 0.17 | 0.89 | 1 | 0.67 | 0.97 |
| p | <0.01 * | 0.67 | <0.01 * | 0.45 | <0.01 * | 0.48 | <0.01 * | <0.01 * | <0.01 * | |
| NMCHs | −0.14 | −0.02 | 0.79 | −0.01 | 0.88 | 0.49 | 0.75 | 0.67 | 1 | 0.85 |
| p | 0.576 | 0.94 | <0.01 * | 0.98 | <0.01 * | 0.03 * | <0.01 * | <0.01 * | <0.01 * | |
| THC | −0.56 | 0.2 | 0.89 | 0.21 | 0.95 | 0.35 | 0.96 | 0.97 | 0.85 | 1 |
| p | 0.01 * | 0.4 | <0.01 * | 0.37 | <0.01 * | 0.13 | <0.01 * | <0.01 * | <0.01 * |
4. Discussion
5. Limitation
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Castillo, J.R.; Peters, S.P.; Busse, W.W. Asthma Exacerbations: Pathogenesis, Prevention, and Treatment. J. Allergy Clin. Immunol. Pract. 2017, 5, 918–927. [Google Scholar] [CrossRef] [PubMed]
- GBD 2019 Chronic Respiratory Diseases Collaborators. Global burden of chronic respiratory diseases and risk factors, 1990–2019: An update from the Global Burden of Disease Study 2019. EClinicalMedicine 2023, 59, 101936. [Google Scholar] [CrossRef]
- Pate CA, Zahran HS, Qin X, Johnson C, Hummelman E, Malilay J. Asthma surveillance—United States, 2006–2018. MMWR Surveill. Summ. 2021, 70, 1–32. [CrossRef] [PubMed]
- Chatkin, J.; Correa, L.; Santos, U. External Environmental Pollution as a Risk Factor for Asthma. Clin. Rev. Allergy Immunol. 2022, 62, 72–89. [Google Scholar] [CrossRef] [PubMed]
- Šulc, L.; Gregor, P.; Kalina, J.; Mikeš, O.; Janoš, T.; Čupr, P. City-scale assessment of long-term air quality impacts on the respiratory and cardiovascular health. Front. Public Health 2022, 10, 1006536. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.Y.; Tseng, Y.L.; Huang, K.C.; Chiu, I.M.; Pan, H.Y.; Cheng, F.J. Association between Ambient Air Pollution and Emergency Room Visits for Pediatric Respiratory Diseases: The Impact of COVID-19 Pandemic. Toxics 2022, 10, 247. [Google Scholar] [CrossRef] [PubMed]
- Varghese, D.; Ferris, K.; Lee, B.; Grigg, J.; Pinnock, H.; Cunningham, S. Outdoor air pollution and near-fatal/fatal asthma attacks in children: A systematic review. Pediatr. Pulmonol. 2024. [Google Scholar] [CrossRef]
- Orellano, P.; Quaranta, N.; Reynoso, J.; Balbi, B.; Vasquez, J. Effect of outdoor air pollution on asthma exacerbations in children and adults: Systematic review and multilevel meta-analysis. PLoS ONE 2017, 12, e0174050. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.G.; Yen, S.Y.; Hsiao, C.C.; Lin, Y.Y.; Chang, Y.H.; Chen, Y.H.; Cheng, C.A. Short-Term Exposure Effect of Ambient Fine Particulate Matter, Ozone and Cold Temperature on Emergency Room Visits for Asthma Patients. Toxics 2023, 11, 94. [Google Scholar] [CrossRef]
- Hsu, S.-C.; Chang, J.-W.; Lee, C.-L.; Huang, W.-C.; Hsu, Y.-P.; Liu, C.-T.; Jean, S.-S.; Huang, S.-K.; Hsu, C.-W. Differential time-lag effects of ambient PM2.5 and PM2.5-PAHs on asthma emergency department visits. Environ. Sci. Pollut. Res. Int. 2020, 27, 43117–43124. [Google Scholar] [CrossRef]
- Chankaew, K.; Sinitkul, R.; Manuyakorn, W.; Roekworachai, K.; Kamalaporn, H. Spatial Estimation of PM2.5 Exposure and its Association with Asthma Exacerbation: A Prospective Study in Thai Children. Ann. Glob. Health 2022, 88, 15. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Liu, C.; Chen, R.; Zhou, Y.; Meng, X.; Hong, J.; Cao, L.; Lu, Y.; Dong, X.; Xia, M.; et al. Associations of short-term exposure to air pollution and emergency department visits for pediatric asthma in Shanghai, China. Chemosphere 2021, 263, 127856. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Wu, J.; Lin, X. Ozone Exposure and Asthma Attack in Children. Front. Pediatr. 2022, 10, 830897. [Google Scholar] [CrossRef] [PubMed]
- Khatri, S.B.; Newman, C.; Hammel, J.P.; Dey, T.; Van Laere, J.J.; Ross, K.A.; Rose, J.A.; Anderson, T.; Mukerjee, S.; Smith, L.; et al. Associations of Air Pollution and Pediatric Asthma in Cleveland, Ohio. Sci. World J. 2021, 2021, 8881390. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, M.D.; Steele, A.R.; Parent, E.C.; Steinback, C.D. Cold air exercise screening for exercise induced bronchoconstriction in cold weather athletes. Respir. Physiol. Neurobiol. 2019, 269, 103262. [Google Scholar] [CrossRef] [PubMed]
- Tran, H.M.; Lin, Y.C.; Tsai, F.J.; Lee, K.Y.; Chang, J.H.; Chung, C.L.; Chung, K.F.; Chuang, K.J.; Chuang, H.C. Short-term mediating effects of PM2.5 on climate-associated COPD severity. Sci. Total Environ. 2023, 903, 166523. [Google Scholar] [CrossRef] [PubMed]
- Taiwanese National Health Insurance Admiration. Healthcare Quality. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=9ABC74CDF4F839F6&topn=23C660CAACAA159D (accessed on 1 September 2023).
- Taiwan Ministry of Environment. Air Pollutants Monthly Report. 2024. Available online: https://airtw.moenv.gov.tw/CHT/Query/Month_Value.aspx (accessed on 15 December 2023).
- Taipei Weather Administration. Climate Monthly Report in Taipei. 2023. Available online: https://tsis.dbas.gov.taipei/statis/webMain.aspx?k=tpemain. (accessed on 15 December 2023).
- WHO. Air Pollution Guideline Values. 2022. Available online: https://apps.who.int/iris/bitstream/handle/10665/345329/9789240034228-eng.pdf (accessed on 1 September 2023).
- Dondi, A.; Carbone, C.; Manieri, E.; Zama, D.; Del Bono, C.; Betti, L.; Biagi, C.; Lanari, M. Outdoor Air Pollution and Childhood Respiratory Disease: The Role of Oxidative Stress. Int. J. Mol. Sci. 2023, 24, 4345. [Google Scholar] [CrossRef] [PubMed]
- Taiwanese National Health Insurance Admiration. Healthcare Improvement Plan in Asthma. Available online: https://www.nhi.gov.tw/Content_List.aspx?n=3D98B91375362414&topn=5FE8C9FEAE863B46 (accessed on 1 September 2023).
- Guarnieri, M.; Balmes, J.R. Outdoor air pollution and asthma. Lancet 2014, 383, 1581–1592. [Google Scholar] [CrossRef] [PubMed]
- Mohr, L.B.; Luo, S.; Mathias, E.; Tobing, R.; Homan, S.; Sterling, D. Influence of season and temperature on the relationship of elemental carbon air pollution to pediatric asthma emergency room visits. J. Asthma. 2008, 45, 936–943. [Google Scholar] [CrossRef]
- Sly, P.D.; Cormier, S.A.; Lomnicki, S.; Harding, J.N.; Grimwood, K. Environmentally Persistent Free Radicals: Linking Air Pollution and Poor Respiratory Health? Am. J. Respir. Crit. Care Med. 2019, 200, 1062–1063. [Google Scholar] [CrossRef]
- Perez, L.; Declercq, C.; Iñiguez, C.; Aguilera, I.; Badaloni, C.; Ballester, F.; Bouland, C.; Chanel, O.; Cirarda, F.B.; Forastiere, F.; et al. Chronic burden of near-roadway traffic pollution in 10 European cities (APHEKOM network). Eur. Respir. J. 2013, 42, 594–605. [Google Scholar] [CrossRef] [PubMed]
- Li, M.H.; Fan, L.C.; Mao, B.; Yang, J.W.; Choi, A.M.K.; Cao, W.J.; Xu, J.F. Short-term Exposure to Ambient Fine Particulate Matter Increases Hospitalizations and Mortality in COPD: A Systematic Review and Meta-analysis. Chest 2016, 149, 447–458. [Google Scholar] [CrossRef] [PubMed]
- Altman, M.C.; Kattan, M.; O’Connor, G.T.; Murphy, R.C.; Whalen, E.; LeBeau, P.; Calatroni, A.; Gill, M.A.; Gruchalla, R.S.; Liu, A.H.; et al. Associations between outdoor air pollutants and non-viral asthma exacerbations and airway inflammatory responses in children and adolescents living in urban areas in the USA: A retrospective secondary analysis. Lancet Planet Health 2023, 7, e33–e44. [Google Scholar] [CrossRef] [PubMed]
- Saffari, A.; Daher, N.; Shafer, M.M.; Schauer, J.J.; Sioutas, C. Global perspective on the oxidative potential of airborne particulate matter: A synthesis of research findings. Environ. Sci. Technol. 2014, 48, 7576–7583. [Google Scholar] [CrossRef]
- Li, Z.; Xu, X.; Thompson, L.A.; Gross, H.E.; Shenkman, E.A.; DeWalt, D.A.; Huang, I.C. Longitudinal Effect of Ambient Air Pollution and Pollen Exposure on Asthma Control: The Patient-Reported Outcomes Measurement Information System (PROMIS) Pediatric Asthma Study. Acad. Pediatr. 2019, 19, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Hao, H.; Eckel, S.P.; Hosseini, A.; Van Vliet, E.D.S.; Dzubur, E.; Dunton, G.; Chang, S.Y.; Craig, K.; Rocchio, R.; Bastain, T.; et al. Daily Associations of Air Pollution and Pediatric Asthma Risk Using the Biomedical REAI-Time Health Evaluation (BREATHE) Kit. Int. J. Environ. Res. Public Health 2022, 19, 3578. [Google Scholar] [CrossRef] [PubMed]
- Strickland, M.J.; Hao, H.; Hu, X.; Chang, H.H.; Darrow, L.A.; Liu, Y. Pediatric Emergency Visits and Short-Term Changes in PM2.5 Concentrations in the U.S. State of Georgia. Environ. Health Perspect. 2016, 124, 690–696. [Google Scholar] [CrossRef] [PubMed]
- Nenna, R.; Evangelisti, M.; Frassanito, A.; Scagnolari, C.; Pierangeli, A.; Antonelli, G.; Nicolai, A.; Arima, S.; Moretti, C.; Papoff, P.; et al. Respiratory syncytial virus bronchiolitis, weather conditions and air pollution in an Italian urban area: An observational study. Environ. Res. 2017, 158, 188–193. [Google Scholar] [CrossRef] [PubMed]
- Su, W.; Wu, X.; Geng, X.; Zhao, X.; Liu, Q.; Liu, T. The short-term effects of air pollutants on influenza-like illness in Jinan, China. BMC Public Health 2019, 19, 1319. [Google Scholar] [CrossRef]
- Su, Y.T.; Lin, Y.T.; Yang, C.C.; Tsai, S.S.; Wang, J.Y.; Huang, Y.L.; Lin, T.I.; Lin, T.M.; Tsai, Y.C.; Yu, H.R.; et al. High correlation between human rhinovirus type C and children with asthma exacerbations in Taiwan. J. Microbiol. Immunol. Infect. 2020, 53, 561–568. [Google Scholar] [CrossRef]
- Bhavnani, D.; Wilkinson, M.; Zárate, R.A.; Balcer-Whaley, S.; Katz, D.S.W.; Rathouz, P.J.; Matsui, E.C. Do upper respiratory viruses contribute to racial and ethnic disparities in emergency department visits for asthma? J. Allergy Clin. Immunol. 2023, 151, 778–782.e1. [Google Scholar] [CrossRef]
- Gebski, E.B.; Parikh, V.; Lam, H.; Kim, N.; Bochkov, Y.A.; Cao, G.; Panettieri RAJr Kurten, R.; Gern, J.; An, S.S.; Koziol-White, C.J. Rhinovirus C15 Attenuates Relaxation and cAMP Production in Human Airways and Smooth Muscle. Am. J. Respir. Cell Mol. Biol. 2023, 69, 172–181. [Google Scholar] [CrossRef]
- Sharma, R.; Humphrey, J.L.; Frueh, L.; Kinnee, E.J.; Sheffield, P.E.; Clougherty, J.E. Neighborhood violence and socioeconomic deprivation influence associations between acute air pollution and temperature on childhood asthma in New York city. Environ. Res. 2023, 231 Pt 3, 116235. [Google Scholar] [CrossRef] [PubMed]
- Zafirah, Y.; Lin, Y.K.; Andhikaputra, G.; Deng, L.W.; Sung, F.C.; Wang, Y.C. Mortality and morbidity of asthma and chronic obstructive pulmonary disease associated with ambient environment in metropolitans in Taiwan. PLoS ONE 2021, 16, e0253814. [Google Scholar] [CrossRef] [PubMed]
- Kadhim Yousif, M.; Al Muhyi, A.A. Impact of weather conditions on childhood admission for wheezy chest and bronchial asthma. Med. J. Islam. Repub. Iran 2019, 33, 89. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.K.; Chang, C.K.; Chang, S.C.; Chen, P.S.; Lin, C.; Wang, Y.C. Temperature, nitrogen dioxide, circulating respiratory viruses and acute upper respiratory infections among children in Taipei, Taiwan: A population-based study. Environ. Res. 2013, 120, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Ming, T.; de Richter, R.; Shen, S.; Caillol, S. Fighting global warming by greenhouse gas removal: Destroying atmospheric nitrous oxide thanks to synergies between two breakthrough technologies. Environ. Sci. Pollut. Res. Int. 2016, 23, 6119–6138. [Google Scholar] [CrossRef] [PubMed]
- Boguslavsky, D.V.; Sharova, N.P.; Sharov, K.S. Evolutionary Challenges to Humanity Caused by Uncontrolled Carbon Emissions: The Stockholm Paradigm. Int. J. Environ. Res. Public Health 2022, 19, 16920. [Google Scholar] [CrossRef] [PubMed]
- Di Cicco, M.E.; Ferrante, G.; Amato, D.; Capizzi, A.; De Pieri, C.; Ferraro, V.A.; Furno, M.; Tranchino, V.; La Grutta, S. Climate Change and Childhood Respiratory Health: A Call to Action for Paediatricians. Int. J. Environ. Res. Public Health 2020, 17, 5344. [Google Scholar] [CrossRef]
- Thurston, G.D.; Balmes, J.R.; Garcia, E.; Gilliland, F.D.; Rice, M.B.; Schikowski, T.; Van Winkle, L.S.; Annesi-Maesano, I.; Burchard, E.G.; Carlsten, C.; et al. Outdoor Air Pollution and New-Onset Airway Disease. An Official American Thoracic Society Workshop Report. Ann. Am. Thorac. Soc. 2020, 17, 387–398. [Google Scholar] [CrossRef]
- Zhao, Y.; Hu, J.; Tan, Z.; Liu, T.; Zeng, W.; Li, X.; Huang, C.; Wang, S.; Huang, Z.; Ma, W. Ambient carbon monoxide and increased risk of daily hospital outpatient visits for respiratory diseases in Dongguan, China. Sci. Total Environ. 2019, 668, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Ciencewicki, J.; Jaspers, I. Air pollution and respiratory viral infection. Inhal. Toxicol. 2007, 19, 1135–1146. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, M. Low-to-moderate atmospheric ozone levels are negatively correlated with hospital visits by asthma patients. Medicine 2022, 101, e31737. [Google Scholar] [CrossRef] [PubMed]
- Sokolowska, M.; Quesniaux, V.F.J.; Akdis, C.A.; Chung, K.F.; Ryffel, B.; Togbe, D. Acute Respiratory Barrier Disruption by Ozone Exposure in Mice. Front. Immunol. 2019, 10, 2169. [Google Scholar] [CrossRef] [PubMed]
- McHugh, E.G.; Grady, S.T.; Collins, C.M.; Moy, M.L.; Hart, J.E.; Coull, B.A.; Schwartz, J.D.; Koutrakis, P.; Zhang, J.; Garshick, E. Pulmonary, inflammatory, and oxidative effects of indoor nitrogen dioxide in patients with COPD. Environ. Epidemiol. 2023, 7, e271. [Google Scholar] [CrossRef] [PubMed]
- Solanki, N.; Bruckman, D.; Wang, X.; Tang, A.; Attaway, A.; Khatri, S. Nitrogen dioxide, an EPA parameter, may forecast the incidence of asthma exacerbations across urban areas: An observational study. Pediatr. Pulmonol. 2023, 58, 262–270. [Google Scholar] [CrossRef]
- Zhao, Y.; Kong, D.; Fu, J.; Zhang, Y.; Chen, Y.; Liu, Y.; Chang, Z.; Liu, Y.; Liu, X.; Xu, K.; et al. Increased Risk of Hospital Admission for Asthma in Children From Short-Term Exposure to Air Pollution: Case-Crossover Evidence From Northern China. Front. Public Health 2021, 9, 798746. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ni, H.; Bai, L.; Cheng, Q.; Zhang, H.; Wang, S.; Xie, M.; Zhao, D.; Su, H. The short-term association between air pollution and childhood asthma hospital admissions in urban areas of Hefei City in China: A time-series study. Environ. Res. 2019, 169, 510–516. [Google Scholar] [CrossRef] [PubMed]
- Taylor, P.E.; Jacobson, K.W.; House, J.M.; Glovsky, M.M. Links between pollen, atopy and the asthma epidemic. Int. Arch. Allergy Immunol. 2007, 144, 162–170. [Google Scholar] [CrossRef]
- WHO. Sustainable Development Goals. Available online: https://www.who.int/data/gho/data/themes/sustainable-development-goals (accessed on 1 September 2023).
- Gleason, J.A.; Bielory, L.; Fagliano, J.A. Associations between ozone, PM2.5, and four pollen types on emergency department pediatric asthma events during the warm season in New Jersey: A case-crossover study. Environ. Res. 2014, 132, 421–429. [Google Scholar] [CrossRef]
- Juskiene, I.; Prokopciuk, N.; Franck, U.; Valiulis, A.; Valskys, V.; Mesceriakova, V.; Kvedariene, V.; Valiulyte, I.; Poluzioroviene, E.; Sauliene, I.; et al. Indoor air pollution effects on pediatric asthma are submicron aerosol particle-dependent. Eur. J. Pediatr. 2022, 181, 2469–2480. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.C.; Zou, M.L.; Chen, Y.H.; Jiang, C.B.; Wu, C.D.; Lung, S.C.; Chien, L.C.; Lo, Y.C.; Chao, H.J. Effects of indoor air quality and home environmental characteristics on allergic diseases among preschool children in the Greater Taipei Area. Sci. Total Environ. 2023, 897, 165392. [Google Scholar] [CrossRef] [PubMed]
- Abdelzaher, H.; Tawfik, S.M.; Nour, A.; Abdelkader, S.; Elbalkiny, S.T.; Abdelkader, M.; Abbas, W.A.; Abdelnaser, A. Climate change, human health, and the exposome: Utilizing OMIC technologies to navigate an era of uncertainty. Front. Public Health 2022, 10, 973000. [Google Scholar] [CrossRef] [PubMed]
- Abernethy, S.; O’Connor, F.M.; Jones, C.D.; Jackson, R.B. Methane removal and the proportional reductions in surface temperature and ozone. Philos. Trans. A Math. Phys. Eng. Sci. 2021, 379, 20210104. [Google Scholar] [CrossRef] [PubMed]
- Cordero, E.C.; Centeno, D.; Todd, A.M. The role of climate change education on individual lifetime carbon emissions. PLoS ONE 2020, 15, e0206266. [Google Scholar] [CrossRef]

| Quarter | 1 | 2 | 3 | 4 | p |
|---|---|---|---|---|---|
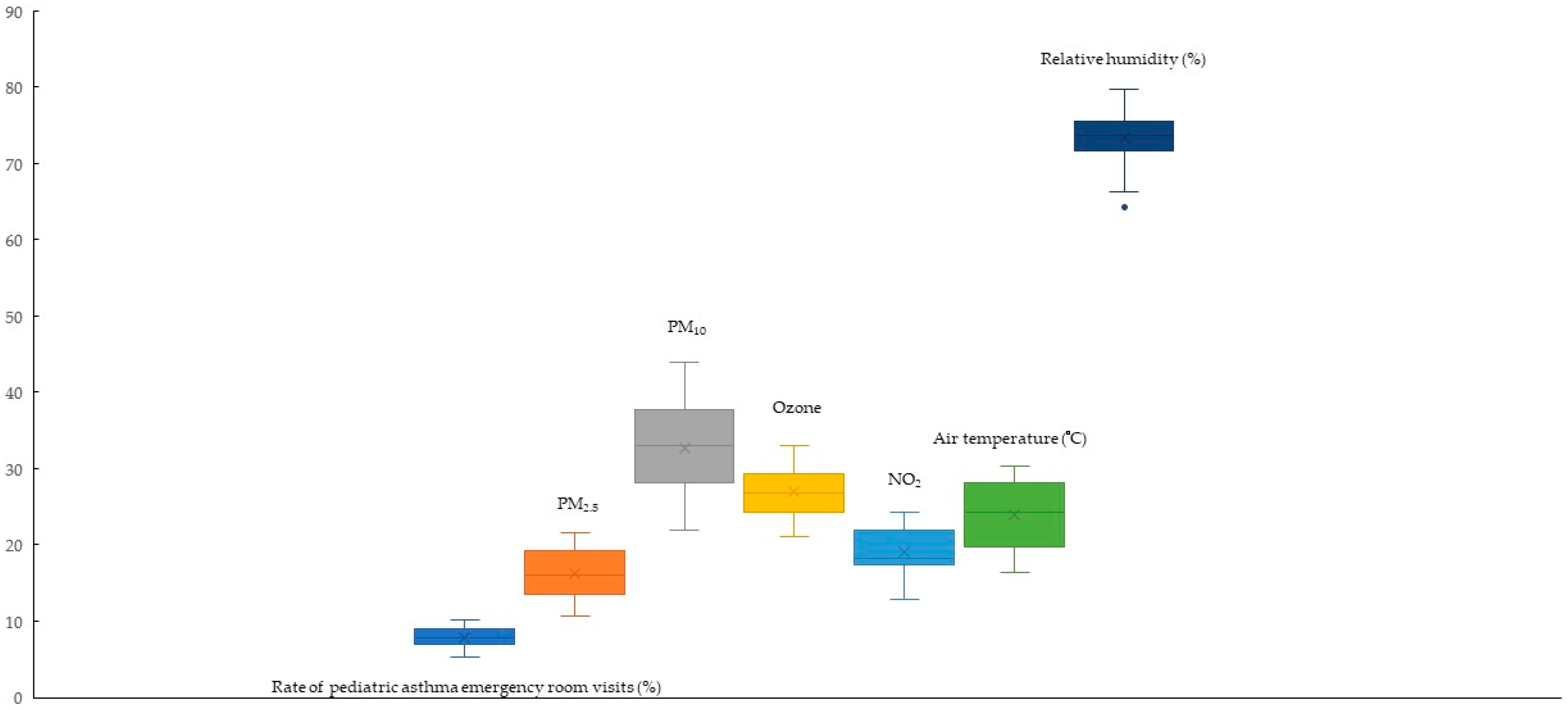
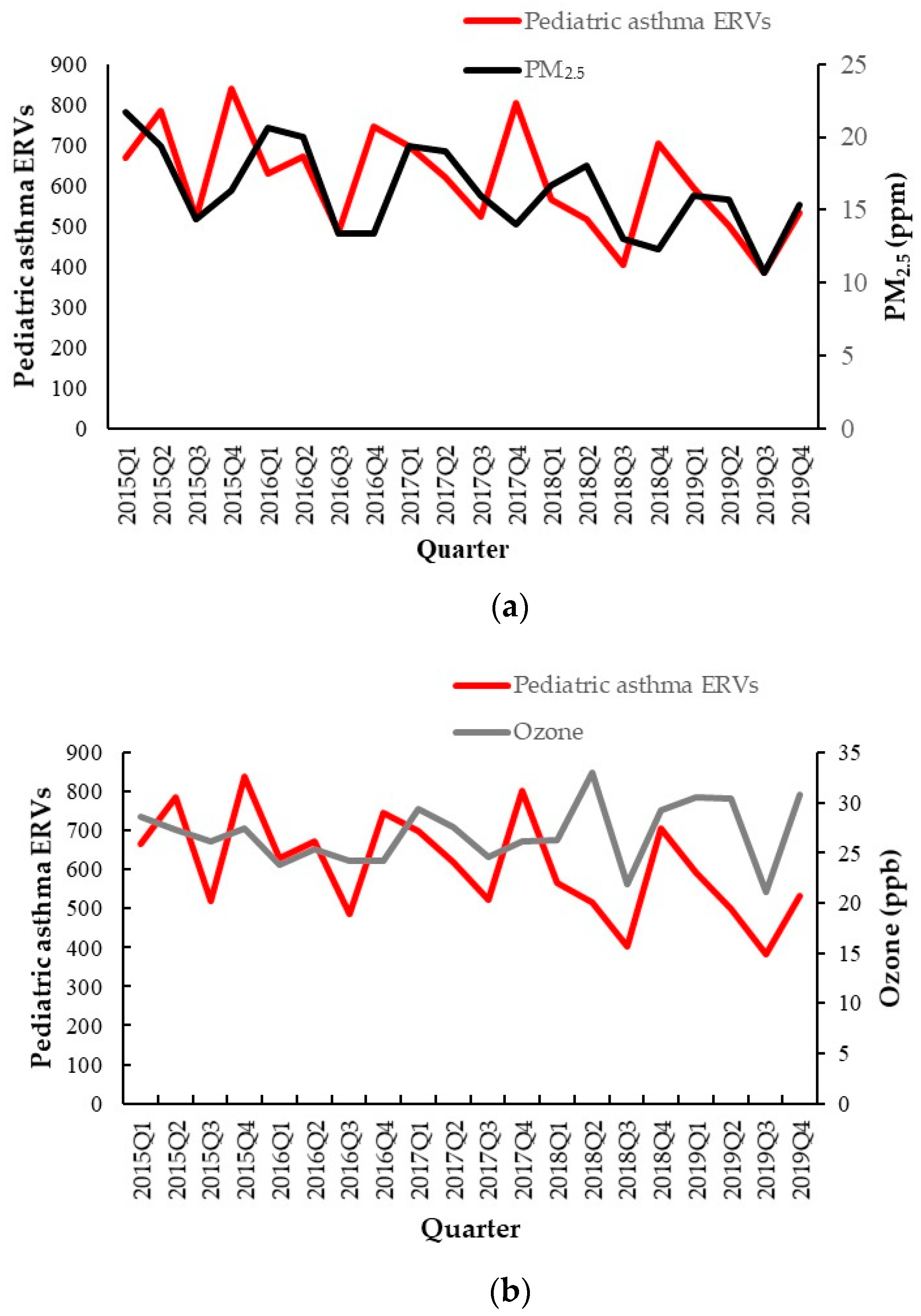
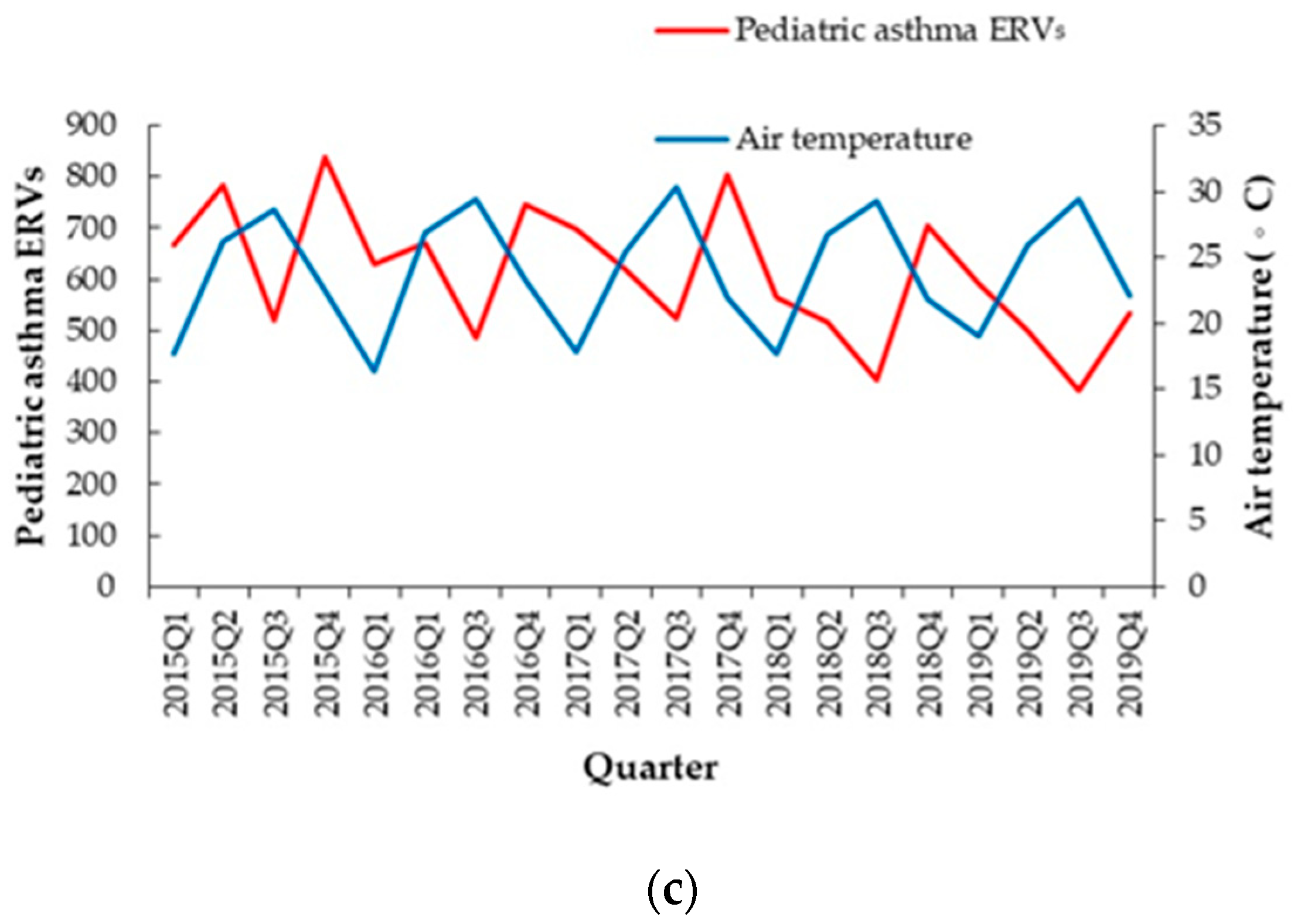
| Pediatric asthma ERVs | 631 ± 53.83 | 618 ± 117.09 | 463 ± 65.93 | 725 ± 118.87 | 0.004 * |
| PM2.5 | 18.87 ± 2.47 | 18.4 ± 1.69 | 13.47 ± 1.95 | 14.27 ± 1.59 | 0.001 * |
| PM10 | 38.47 ± 3.57 | 36.47 ± 3.23 | 26.27 ± 3.12 | 29.8 ± 4.77 | <0.001 * |
| NO2 | 22.14 ± 1.78 | 20.49 ± 2.27 | 15.57 ± 2.04 | 18.04 ± 0.7 | <0.001 * |
| O3 | 27.75 ± 2.66 | 28.74 ± 2.98 | 23.59 ± 2.11 | 27.57 ± 2.56 | 0.03 * |
| Ambient temperature | 17.72 ± 0.93 | 26.22 ± 0.61 | 29.42 ± 0.59 | 22.34 ± 0.56 | <0.001 * |
| Relative humidity | 75.4 ± 2.82 | 72.53 ± 4.03 | 70.47 ± 4.26 | 75.07 ± 2.19 | 0.119 |
| Relative Ratio | p | Adjusted Relative Ratio | p | |
|---|---|---|---|---|
| PM2.5 highest quarter | 1.162 (95% C.I.: 1.105–1.221) | <0.001 * | 1.102 (95% C.I.: 1.037–1.172) | 0.002 * |
| PM2.5 middle quarter | 1.051 (95% C.I.: 1.005–1.1) | 0.03 * | 1.037 (95% C.I.: 0.982–1.095) | 0.191 |
| PM2.5 lowest quarter | reference | reference | ||
| Ozone | 1.006 (1–1.012) | 0.049 * | 0.981 (95% C.I.: 0.972–0.99) | <0.001 * |
| Air temperature highest quarter | 0.844 (95% C.I.: 0.8–0.89) | <0.001 * | 0.813 (95% C.I.: 0.745–0.887) | <0.001 * |
| Air temperature middle quarter | 1.064 (95% C.I.: 1.02–1.11) | 0.004 | 1.1 (95% C.I.: 1.049–1.153) | <0.001 * |
| Air temperature lowest quarter | reference | reference | ||
| Relative humidity | 1.011 (95% C.I.: 1.005–1.016) | <0.001 * | 0.977 (95% C.I.: 0.99–1.003) | 0.288 |
| First Quarter | p | Second Quarter | p | Third Quarter | p | Fourth Quarter | p | |
|---|---|---|---|---|---|---|---|---|
| PM2.5 | 0.98 (95% C.I.: 0.939–1.023) | 0.356 | 1.188 (95% C.I.: 1.114–1.268) | <0.001 * | 0.896 (95% C.I.: 0.727–1.103) | 0.3 | 0.893 (95% C.I.: 0.833–0.957) | 0.001 * |
| O3 | 1.108 (95% C.I.: 1.019–1.205) | 0.016 * | 1.053 (95% C.I.: 1.012–1.096) | 0.011 * | 1.157 (95% C.I.: 1.008–1.329) | 0.038 * | 0.941 (95% C.I.: 0.92–0.963) | <0.001 * |
| AT | 0.726 (95% C.I.: 0.56–0.943) | 0.016 * | 0.952 (95% C.I.: 0.885–1.023) | 0.181 | 1.03 (95% C.I.: 0.88–1.205) | 0.714 | 0.937 (95% C.I.: 0.849–1.034) | 0.195 |
| RH | 1 (95% C.I.: 0.974–1.027) | 0.983 | 1.04 (95% C.I.: 1.018–1.062) | <0.001 * | 0.96 (95% C.I.: 0.897–1.028) | 0.241 | 1.107 (95% C.I.: 1.056–1.16) | <0.001 * |
| Reference | Finding | Outcome | Place | Year |
|---|---|---|---|---|
| Present study | PM2.5: RR of 1.102 (95% C.I.: 1.037–1.1722) Air temperature: RR of 0.813 (95% CI: 0.745–0.887) | Pediatric asthma emergency room visits | Taipei, Taiwan | 2015–2019 |
| [8] | NO2: OR: 1.04 (95% C.I.: 1.001, 1.081) SO2: OR 1.047 (95% C.I.: 1.009, 1.086) PM2.5: OR 1.022 (95% C.I.: 1.000, 1.045) | Pediatric asthma exacerbations in high-income cities | Meta-analysis | 2000–2016 |
| [9] | 10 units PM2.5: RR 1.195 (95% C.I.: 1.001–1.426) at a 2-day lag | Pediatric asthma emergency room visits | Taoyuan, Taiwan | 2016–2019 |
| [10] | 10 units PM2.5: RR 1.310 (95% C.I.: 1.069–1.606) 10 units PM2.5-PAH: RR 1.576 (95% C.I.: 1.371–1.810) on 1-day lag | Pediatric asthma emergency room visits | Taipei, Taiwan | 2012–2015 |
| [11] | 10 units PM2.5: 0.2 events increasing | Pediatric asthma exacerbation | Bangkok and Chiang Mai, Thailand | 2020–2021 |
| [12] | 10 units PM2.5: RR 1.011 (95% C.I.: 1.002–1.021), 10 units NO2: 1.030 (95% C.I.: 1.017–1.043), 10 units SO2: 1.106 (95% C.I.: 1.041–1.174), 10 units O3: 1.009 (95% C.I.: 1.001, 1.017) | Pediatric asthma ERVs | Shanghai, China | 2016–2018 |
| [13] | 10 units O3-8 h increased 6.33% in ≥100 μg/m3 O3-8 h 10 units O3-8 h increased 2.36% in 80–99 μg/m3 O3-8 h PM2.5: OR: 1.0503 (95% C.I.: 1.0277–1.073) in ≥100 μg/m3 O3-8 h | Pediatric asthma attacks | Xiamen, China | 2016–2019 |
| [14] | Higher quartile TRAPs-PM2.5: RR 1.789 (1.517–2.109) Higher quartile TRAPs-NO2:1.893 (1.589–2.256) | Pediatric asthma emergency room visits | Cleveland, OH, USA | 2009–2010 |
| [31] | O3: rate ratio 1.52 (95% C.I.: 1.02–2.27) NOx: rate ratio 1.61 (95% C.I.: 1.23–2.11) NO: rate ratio 1.80 (95%C.I.: 1.37–2.35) | Rescue inhaler use | Los Angeles, CA, USA | 2019 |
| [38] | Cold season PM2.5: 4.90% (95% C.I.: 3.77–6.04) on 1-day lag SO2: 8.57% (5.99–11.21) on 1-day lag Warm season NO2: 7.86% (95% C.I.: 6.66–9.07) on 1-day lag O3: 4.75% (95% C.I.: 3.53–5.97) on 2 days lag Minimum air temperature: 2.26% (95% C.I.: 1.25–3.28) in the cold season | Pediatric asthma emergency room visits | New York, NY, USA | 2005–2011 |
| [32] | 10 units PM2.5: OR 1.013 (95% C.I.: 1.003–1.023) | Pediatric asthma or wheeze | GA, USA | 2002–2010 |
| [40] | Relative humidity: correlation coefficients of 0.795 Rain days: 0.890 Wind speed: −0.763 Air temperature: −0.837 | Pediatric asthma hospitalization | Basra, Iraq | 2014–2016 |
| [51] | NO2 correlation coefficient: 0.4619 in Buffalo; −0.543 in Detroit, 0.1924–0.3113 Phoenix, 0.2244 in Tucso | Pediatric asthma hospitalization | Buffalo, NY, Detroit, MI, Phoenix, AZ and Tucson, AZ, USA | 2009–2011 |
| [52] | NO2: RR 1.25 (95% C.I.: 1.06–1.48) at lag06 SO2: RR 1.17 (95% C.I.: 1.05–1.31) at lag05 | Pediatric asthma hospitalization, | Beijing, China | 2013–2016 |
| [53] | NO2: cumulative effects 1.580 (95% C.I.: 1.315–1.899, lag 0–3 days | Pediatric asthma hospitalization | Hefei, China | 2015–2016 |
| [56] | O3: rate ratio 1.05 (95% C.I.: 1.04–1.06) PM2.5: rate ratio 1.03 (95% C.I.: 1.02–1.04) The 5-day average values of tree and weed pollen: rate ratio 1.23 (95% C.I.: 1.21–1.25) | Pediatric asthma emergency room visits | NJ, USA | 2004–2007 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsiao, C.-C.; Cheng, C.-G.; Hong, Z.-T.; Chen, Y.-H.; Cheng, C.-A. The Influence of Fine Particulate Matter and Cold Weather on Emergency Room Interventions for Childhood Asthma. Life 2024, 14, 570. https://doi.org/10.3390/life14050570
Hsiao C-C, Cheng C-G, Hong Z-T, Chen Y-H, Cheng C-A. The Influence of Fine Particulate Matter and Cold Weather on Emergency Room Interventions for Childhood Asthma. Life. 2024; 14(5):570. https://doi.org/10.3390/life14050570
Chicago/Turabian StyleHsiao, Chih-Chun, Chun-Gu Cheng, Zih-Tai Hong, Yu-Hsuan Chen, and Chun-An Cheng. 2024. "The Influence of Fine Particulate Matter and Cold Weather on Emergency Room Interventions for Childhood Asthma" Life 14, no. 5: 570. https://doi.org/10.3390/life14050570
APA StyleHsiao, C.-C., Cheng, C.-G., Hong, Z.-T., Chen, Y.-H., & Cheng, C.-A. (2024). The Influence of Fine Particulate Matter and Cold Weather on Emergency Room Interventions for Childhood Asthma. Life, 14(5), 570. https://doi.org/10.3390/life14050570






