Radiosensitization of Allogenic Subcutaneous C6 Glioma Model with Focused Ultrasound-Induced Mild Hyperthermia
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Design
2.2. Allogenic Subcutaneous C6 Glioma Tumor Model
2.3. Small Animal Radiation Treatment
2.4. FUS Hyperthermia Experimental Setup
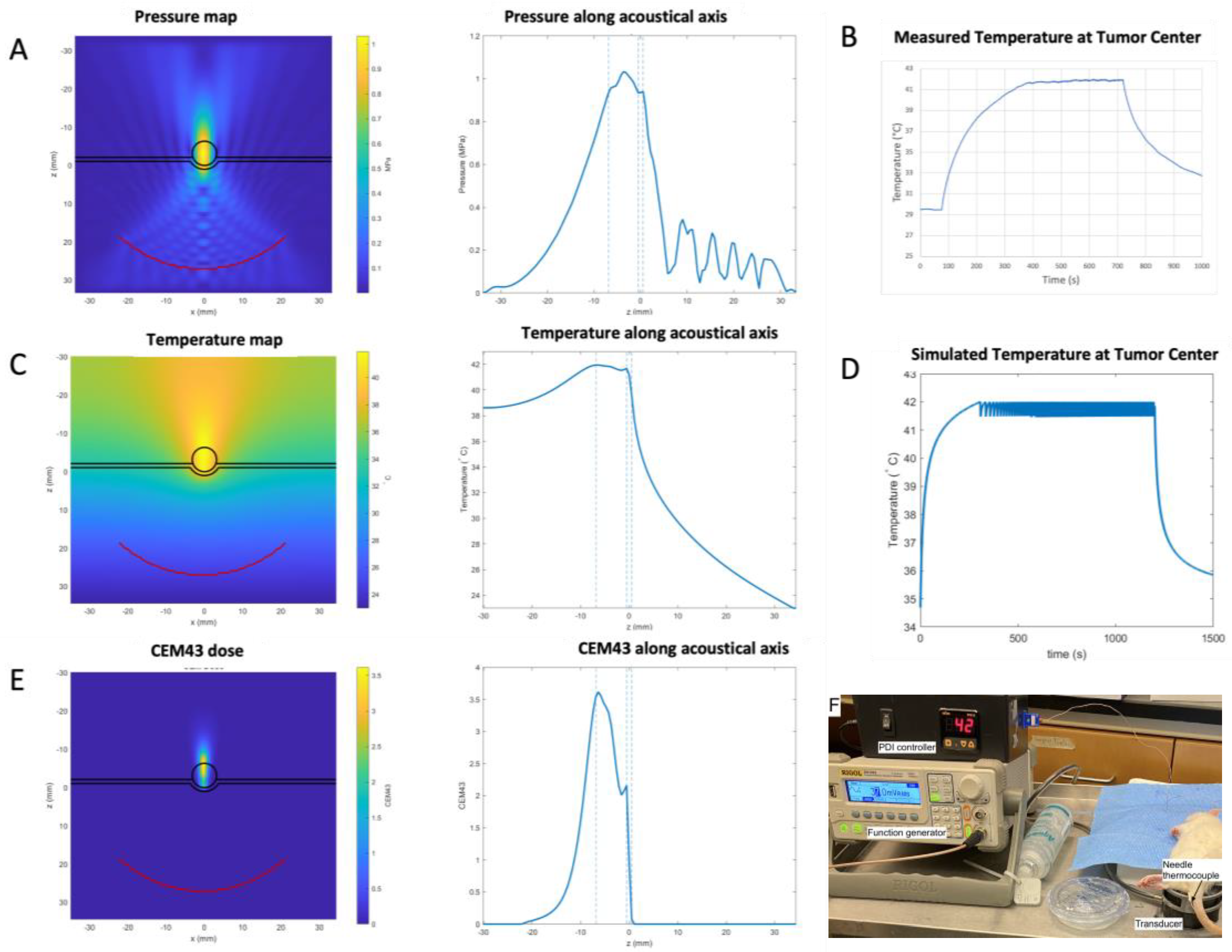
2.5. Simulations of Treatment Parameters
2.6. Immunohistochemistry
2.7. Statistical Analyses
3. Results
3.1. Treatment Parameters as Determined by Numerical Simulations
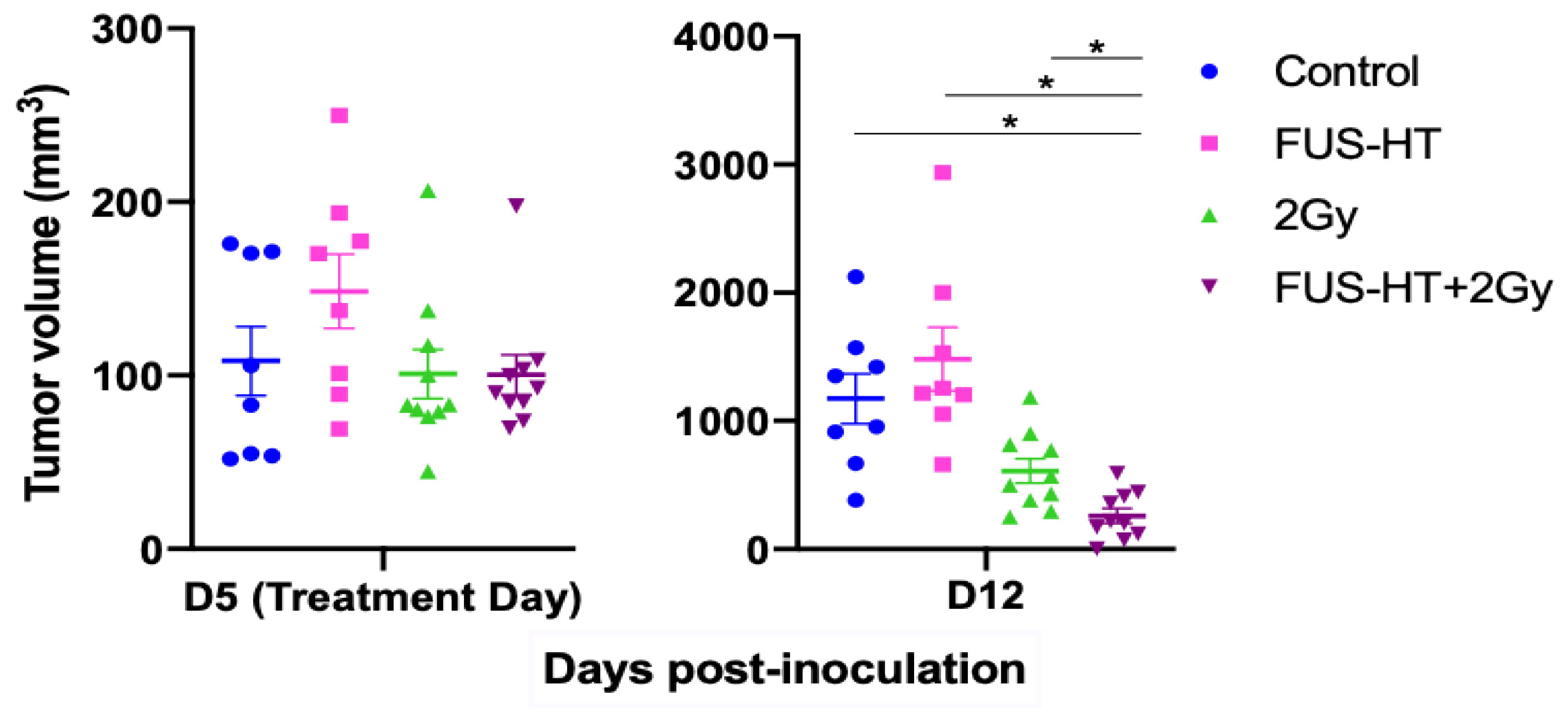
3.2. Allogenic Subcutaneous C6 Tumor Models Sensitivity to Radiation
3.3. Efficacy of FUS-Hyperthermia and RT
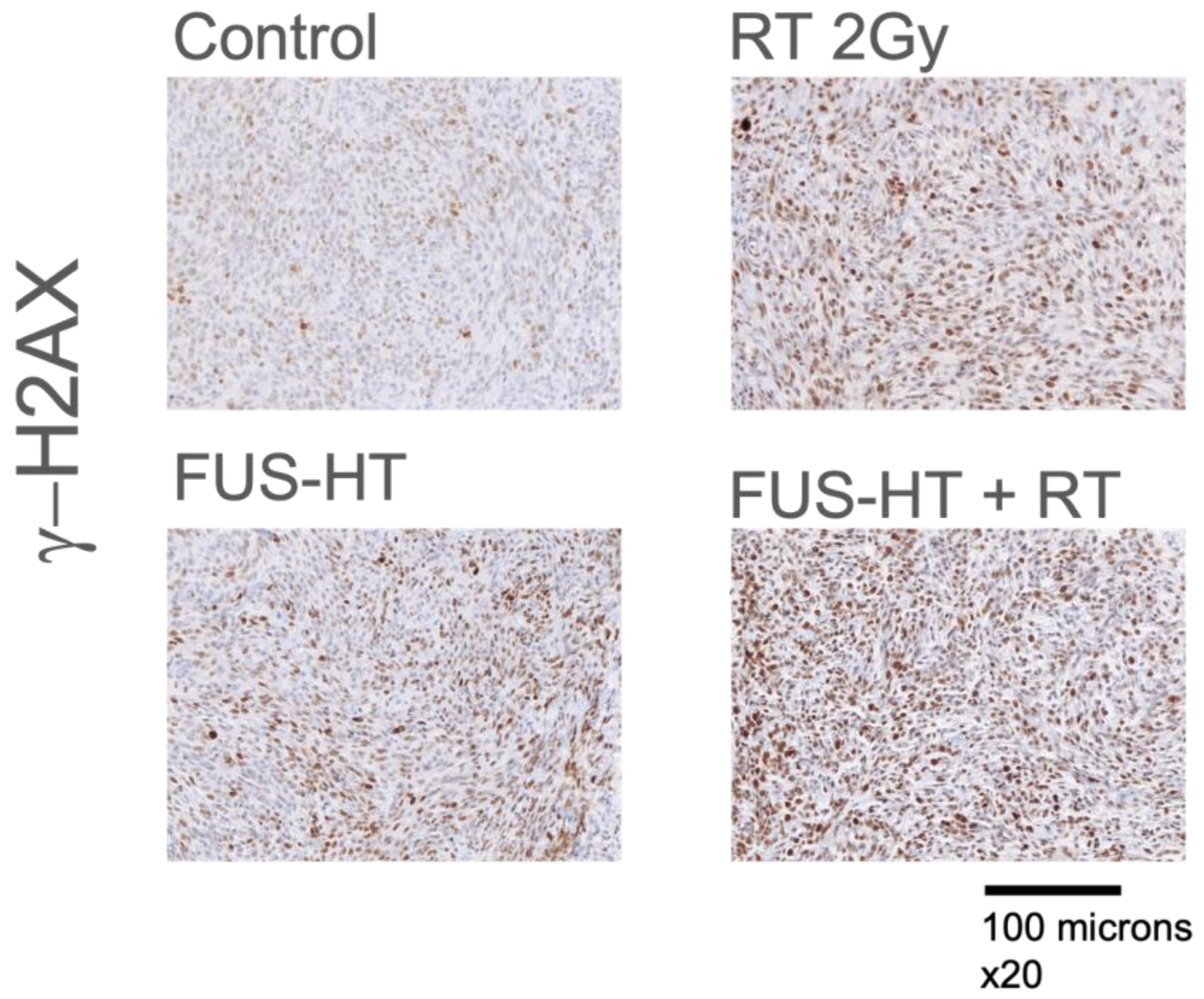
3.4. Effect of Treatments on DNA Damage Repair Mechanism
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wu, W.; Klockow, J.L.; Zhang, M.; Lafortune, F.; Chang, E.; Jin, L.; Wu, Y.; Daldrup-Link, H.E. Glioblastoma Multiforme (GBM): An Overview of Current Therapies and Mechanisms of Resistance. Pharmacol. Res. 2021, 171, 105780. [Google Scholar] [CrossRef]
- Sayan, M.; Mustafayev, T.Z.; Sahin, B.; Kefelioglu, E.S.S.; Wang, S.-J.; Kurup, V.; Balmuk, A.; Gungor, G.; Ohri, N.; Weiner, J.; et al. Evaluation of Response to Stereotactic Radiosurgery in Patients with Radioresistant Brain Metastases. Radiat. Oncol. J. 2019, 37, 265–270. [Google Scholar] [CrossRef]
- Niranjan, A.; Kano, H.; Iyer, A.; Kondziolka, D.; Flickinger, J.C.; Lunsford, L.D. Role of Adjuvant or Salvage Radiosurgery in the Management of Unresected Residual or Progressive Glioblastoma Multiforme in the Pre-Bevacizumab Era. J. Neurosurg. 2015, 122, 757–765. [Google Scholar] [CrossRef]
- Xu, Z.; Marko, N.F.; Angelov, L.; Barnett, G.H.; Chao, S.T.; Vogelbaum, M.A.; Suh, J.H.; Weil, R.J. Impact of Preexisting Tumor Necrosis on the Efficacy of Stereotactic Radiosurgery in the Treatment of Brain Metastases in Women with Breast Cancer. Cancer 2012, 118, 1323–1333. [Google Scholar] [CrossRef][Green Version]
- Wallner, K.E.; Galicich, J.H.; Krol, G.; Arbit, E.; Malkin, M.G. Patterns of Failure Following Treatment for Glioblastoma Multiforme and Anaplastic Astrocytoma. Int. J. Radiat. Oncol. Biol. Phys. 1989, 16, 1405–1409. [Google Scholar] [CrossRef]
- Schneider, C.S.; Woodworth, G.F.; Vujaskovic, Z.; Mishra, M.V. Radiosensitization of High-Grade Gliomas through Induced Hyperthermia: Review of Clinical Experience and the Potential Role of MR-Guided Focused Ultrasound. Radiother. Oncol. 2020, 142, 43–51. [Google Scholar] [CrossRef]
- Sneed, P.K.; Stauffer, P.R.; McDermott, M.W.; Diederich, C.J.; Lamborn, K.R.; Prados, M.D.; Chang, S.; Weaver, K.A.; Spry, L.; Malec, M.K.; et al. Survival Benefit of Hyperthermia in a Prospective Randomized Trial of Brachytherapy Boost ± Hyperthermia for Glioblastoma Multiforme. Int. J. Radiat. Oncol. Biol. Phys. 1998, 40, 287–295. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Altman, M.B.; Laszlo, A.; Straube, W.; Zoberi, I.; Hallahan, D.E.; Chen, H. Ultrasound Hyperthermia Technology for Radiosensitization. Ultrasound Med. Biol. 2019, 45, 1025–1043. [Google Scholar] [CrossRef] [PubMed]
- Borasi, G.; Nahum, A.; Paulides, M.M.; Powathil, G.; Russo, G.; Fariselli, L.; Lamia, D.; Cirincione, R.; Forte, G.I.; Borrazzo, C.; et al. Fast and High Temperature Hyperthermia Coupled with Radiotherapy as a Possible New Treatment for Glioblastoma. J. Ther. Ultrasound 2016, 4, 32. [Google Scholar] [CrossRef]
- Cirincione, R.; Maggio, F.M.D.; Forte, G.I.; Minafra, L.; Bravatà, V.; Castiglia, L.; Cavalieri, V.; Borasi, G.; Russo, G.; Lio, D.; et al. High-Intensity Focused Ultrasound- and Radiation Therapy-Induced Immuno-Modulation: Comparison and Potential Opportunities. Ultrasound Med. Biol. 2017, 43, 398–411. [Google Scholar] [CrossRef] [PubMed]
- Hurwitz, M.D.; Hansen, J.L.; Prokopios-Davos, S.; Manola, J.; Wang, Q.; Bornstein, B.A.; Hynynen, K.; Kaplan, I.D. Hyperthermia Combined with Radiation for the Treatment of Locally Advanced Prostate Cancer. Cancer 2011, 117, 510–516. [Google Scholar] [CrossRef] [PubMed]
- Xia, T.; Sun, Q.; Shi, X.; Fan, N.; Hiraoka, M. Relationship between Thermal Parameters and Tumor Response in Hyperthermia Combined with Radiation Therapy. Int. J. Clin. Oncol. 2001, 6, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Corry, P.M.; Barlogie, B.; Tilchen, E.J.; Armour, E.P. Ultrasound-Induced Hyperthermia for the Treatment of Human Superficial Tumors. Int. J. Radiat. Oncol. Biology Phys. 1982, 8, 1225–1229. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.-L.; Wu, S.-K.; Chiang, C.-F.; Hsu, Y.-H.; Lin, T.-H.; Liou, H.-C.; Fu, W.-M. Short-Time Focused Ultrasound Hyperthermia Enhances Liposomal Doxorubicin Delivery and Antitumor Efficacy for Brain Metastasis of Breast Cancer. Int. J. Nanomed. 2014, 9, 4485–4494. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Guthkelch, A.N.; Carter, L.P.; Cassady, J.R.; Hynynen, K.H.; Iacono, R.P.; Johnson, P.C.; Obbens, E.A.; Roemer, R.B.; Seeger, J.F.; Shimm, D.S. Treatment of Malignant Brain Tumors with Focused Ultrasound Hyperthermia and Radiation: Results of a Phase I Trial. J. Neuro-Oncol. 1991, 10, 271–284. [Google Scholar] [CrossRef] [PubMed]
- Elias, W.J.; Lipsman, N.; Ondo, W.G.; Ghanouni, P.; Kim, Y.G.; Lee, W.; Schwartz, M.; Hynynen, K.; Lozano, A.M.; Shah, B.B.; et al. A Randomized Trial of Focused Ultrasound Thalamotomy for Essential Tremor. N. Engl. J. Med. 2016, 375, 730–739. [Google Scholar] [CrossRef]
- Giakoumettis, D.; Kritis, A.; Foroglou, N. C6 Cell Line: The Gold Standard in Glioma Research. Hippokratia 2018, 3, 105–112. [Google Scholar]
- Tomayko, M.M.; Reynolds, C.P. Determination of Subcutaneous Tumor Size in Athymic (Nude) Mice. Cancer Chemother. Pharmacol. 1989, 24, 148–154. [Google Scholar] [CrossRef]
- Treeby, B.E.; Cox, B.T. K-Wave: MATLAB Toolbox for the Simulation and Reconstruction of Photoacoustic Wave Fields. J. Biomed. Opt. 2010, 15, 021314. [Google Scholar] [CrossRef]
- van Rhoon, G.C.; Samaras, T.; Yarmolenko, P.S.; Dewhirst, M.W.; Neufeld, E.; Kuster, N. CEM43°C Thermal Dose Thresholds: A Potential Guide for Magnetic Resonance Radiofrequency Exposure Levels? Eur. Radiol. 2013, 23, 2215–2227. [Google Scholar] [CrossRef] [PubMed]
- Towa, R.T.; Miller, R.J.; Frizzell, L.A.; Zachary, J.F.; O’Brien, W.D. Attenuation Coefficient and Propagation Speed Estimates of Rat and Pig Intercostal Tissue as a Function of Temperature. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2002, 49, 1411–1420. [Google Scholar] [CrossRef]
- Teotico, G.A.; Miller, R.J.; Frizzell, L.A.; Zachary, J.F.; O’Brien, W.D. Attenuation Coefficient Estimates of Mouse and Rat Chest Wall. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2001, 48, 593–601. [Google Scholar] [CrossRef]
- Duck, F.A. Physical Properties of Tissues; Academic Press: Cambridge, MA, USA, 1990; ISBN 9780122228001. [Google Scholar]
- Bashkatov, A.N.; Genina, E.A.; Korovina, I.V.; Sinichkin, Y.P.; Novikova, O.V.; Tuchin, V.V. In-Vivo and in-Vitro Study of Control of Rat Skin Optical Properties by Action of 40%-Glucose Solution. In Proceedings of the Saratov Fall Meet 2000 Optical Technologies Biophysics Medicine II, Saratov, Russia, 3–6 October 2000; pp. 223–230. [Google Scholar] [CrossRef]
- Yarmolenko, P.S.; Moon, E.J.; Landon, C.; Manzoor, A.; Hochman, D.W.; Viglianti, B.L.; Dewhirst, M.W. Thresholds for Thermal Damage to Normal Tissues: An Update. Int. J. Hyperth. 2011, 27, 320–343. [Google Scholar] [CrossRef]
- Tiennot, T.; Kamimura, H.A.S.; Lee, S.A.; Aurup, C.; Konofagou, E.E. Numerical Modeling of Ultrasound Heating for the Correction of Viscous Heating Artifacts in Soft Tissue Temperature Measurements. Appl. Phys. Lett. 2019, 114, 203702. [Google Scholar] [CrossRef]
- Hynynen, K.; Martin, C.J.; Watmough, D.J.; Mallard, J.R. Errors in Temperature Measurement by Thermocouple Probes during Ultrasound Induced Hyperthermia. Br. J. Radiol. 1983, 56, 969–970. [Google Scholar] [CrossRef]
- Morris, H.; Rivens, I.; Shaw, A.; Ter Haar, G. Investigation of the Viscous Heating Artefact Arising from the Use of Thermocouples in a Focused Ultrasound Field. Phys. Med. Biol. 2008, 53, 4759–4776. [Google Scholar] [CrossRef] [PubMed]
- Hijnen, N.M.; Heijman, E.; Köhler, M.O.; Ylihautala, M.; Ehnholm, G.J.; Simonetti, A.W.; Grüll, H. Tumour Hyperthermia and Ablation in Rats Using a Clinical MR-HIFU System Equipped with a Dedicated Small Animal Set-up. Int. J. Hyperth. 2012, 28, 141–155. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, B.; Wust, P.; Ahlers, O.; Dieing, A.; Sreenivasa, G.; Kerner, T.; Felix, R.; Riess, H. The Cellular and Molecular Basis of Hyperthermia. Crit. Rev. Oncol./Hematol. 2002, 43, 33–56. [Google Scholar] [CrossRef]
- Vince, G.H.; Bendszus, M.; Schweitzer, T.; Goldbrunner, R.H.; Hildebrandt, S.; Tilgner, J.; Klein, R.; Solymosi, L.; Tonn, J.C.; Roosen, K. Spontaneous Regression of Experimental Gliomas—An Immunohistochemical and MRI Study of the C6 Glioma Spheroid Implantation Model. Exp. Neurol. 2004, 190, 478–485. [Google Scholar] [CrossRef] [PubMed]
- Parsa, A.T.; Chakrabarti, I.; Hurley, P.T.; Chi, J.H.; Hall, J.S.; Kaiser, M.G.; Bruce, J.N. Limitations of the C6/Wistar Rat Intracerebral Glioma Model: Implications for Evaluating Immunotherapy. Neurosurgery 2000, 47, 999–1000. [Google Scholar] [CrossRef] [PubMed]
- Ayers, G.D.; McKinley, E.T.; Zhao, P.; Fritz, J.M.; Metry, R.E.; Deal, B.C.; Adlerz, K.M.; Coffey, R.J.; Manning, H.C. Volume of Preclinical Xenograft Tumors Is More Accurately Assessed by Ultrasound Imaging Than Manual Caliper Measurements. J. Ultrasound Med. 2010, 29, 891–901. [Google Scholar] [CrossRef]
- Kersemans, V.; Cornelissen, B.; Allen, P.D.; Beech, J.S.; Smart, S.C. Subcutaneous Tumor Volume Measurement in the Awake, Manually Restrained Mouse Using MRI. J. Magn. Reson. Imaging 2013, 37, 1499–1504. [Google Scholar] [CrossRef] [PubMed]
- Kaur, P.; Hurwitz, M.D.; Krishnan, S.; Asea, A. Combined Hyperthermia and Radiotherapy for the Treatment of Cancer. Cancers 2011, 3, 3799–3823. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Guo, Y.; Velalopoulou, A.; Leisen, J.; Motamarry, A.; Ramajayam, K.; Aryal, M.; Haemmerich, D.; Arvanitis, C.D. Closed-Loop Trans-Skull Ultrasound Hyperthermia Leads to Improved Drug Delivery from Thermosensitive Drugs and Promotes Changes in Vascular Transport Dynamics in Brain Tumors. Theranostics 2021, 11, 7276–7293. [Google Scholar] [CrossRef] [PubMed]
- Ozhinsky, E.; Salgaonkar, V.A.; Diederich, C.J.; Rieke, V. MR Thermometry-Guided Ultrasound Hyperthermia of User-Defined Regions Using the ExAblate Prostate Ablation Array. J. Ther. Ultrasound 2018, 6, 7. [Google Scholar] [CrossRef]
- Man, J.; Shoemake, J.D.; Ma, T.; Rizzo, A.E.; Godley, A.R.; Wu, Q.; Mohammadi, A.M.; Bao, S.; Rich, J.N.; Yu, J.S. Hyperthermia Sensitizes Glioma Stem-like Cells to Radiation by Inhibiting AKT Signaling. Cancer Res. 2015, 75, 1760–1769. [Google Scholar] [CrossRef]

| Parameter | Units | Water | Skin | Tumor | Muscle |
|---|---|---|---|---|---|
| Density | kg/m3 | 1000 | 1060 | 1060 | 1060 |
| Speed of sound | m/s | 1482 | 1624 | 1560 | 1588 |
| Attenuation | Np/(m·MHz) | 0 | 21.2 | 9.32 | 7.1 |
| Thermal Conductivity | W/(m·°C) | 0.627 | 0.5 | 0.5 | 0.52 |
| Specific Heat | J/(kg·°C) | 4118 | 3700 | 3700 | 3700 |
| Perfusion | kg/(m3·s) | 0 | 2.0 | 20 | 0.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xu, Z.; Schlesinger, D.; Drainville, R.A.; Moore, D.; Pramoonjago, P.; Sheehan, J.; Padilla, F. Radiosensitization of Allogenic Subcutaneous C6 Glioma Model with Focused Ultrasound-Induced Mild Hyperthermia. Life 2024, 14, 359. https://doi.org/10.3390/life14030359
Xu Z, Schlesinger D, Drainville RA, Moore D, Pramoonjago P, Sheehan J, Padilla F. Radiosensitization of Allogenic Subcutaneous C6 Glioma Model with Focused Ultrasound-Induced Mild Hyperthermia. Life. 2024; 14(3):359. https://doi.org/10.3390/life14030359
Chicago/Turabian StyleXu, Zhiyuan, David Schlesinger, Robert Andrew Drainville, David Moore, Patcharin Pramoonjago, Jason Sheehan, and Frederic Padilla. 2024. "Radiosensitization of Allogenic Subcutaneous C6 Glioma Model with Focused Ultrasound-Induced Mild Hyperthermia" Life 14, no. 3: 359. https://doi.org/10.3390/life14030359
APA StyleXu, Z., Schlesinger, D., Drainville, R. A., Moore, D., Pramoonjago, P., Sheehan, J., & Padilla, F. (2024). Radiosensitization of Allogenic Subcutaneous C6 Glioma Model with Focused Ultrasound-Induced Mild Hyperthermia. Life, 14(3), 359. https://doi.org/10.3390/life14030359






