Management of Sudden Sensorineural Hearing Loss in Multiple Sclerosis: A Comprehensive Case Report of a Patient with Bilateral Loss and Literature Review
Abstract
1. Introduction
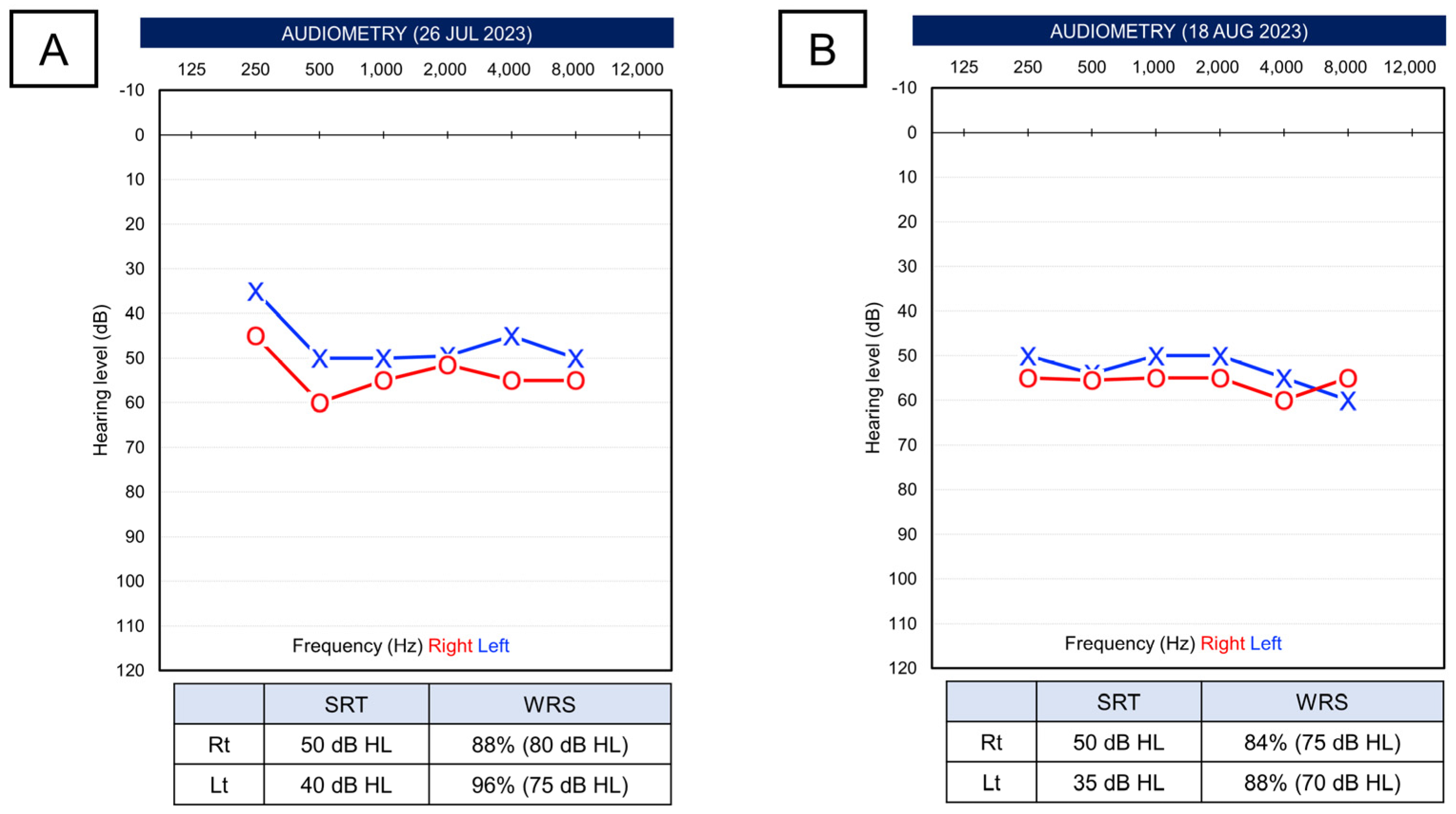
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Weiner, H.L. Multiple Sclerosis is an inflammatory T-cell–mediated autoimmune disease. Arch. Neurol. 2004, 61, 1613–1615. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi, N.; Razavi, S.; Nikzad, E. Multiple Sclerosis: Pathogenesis, Symptoms, Diagnoses and Cell-Based Therapy. Cell J. 2017, 19, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Compston, A.; Coles, A. Multiple sclerosis. Lancet 2008, 372, 1502–1517. [Google Scholar] [CrossRef] [PubMed]
- Dendrou, C.A.; Fugger, L.; Friese, M.A. Immunopathology of multiple sclerosis. Nat. Rev. Immunol. 2015, 15, 545–558. [Google Scholar] [CrossRef] [PubMed]
- Nylander, A.; Hafler, D.A. Multiple sclerosis. J. Clin. Investig. 2012, 122, 1180–1188. [Google Scholar] [CrossRef] [PubMed]
- Roach, E.S. Is multiple sclerosis an autoimmune disorder? Arch. Neurol. 2004, 61, 1615–1616. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekhar, S.S.; Tsai Do, B.S.; Schwartz, S.R.; Bontempo, L.J.; Faucett, E.A.; Finestone, S.A.; Hollingsworth, D.B.; Kelley, D.M.; Kmucha, S.T.; Moonis, G.; et al. Clinical Practice Guideline: Sudden Hearing Loss (Update) Executive Summary. Otolaryngol. Head Neck Surg. 2019, 161, 195–210. [Google Scholar] [CrossRef] [PubMed]
- Fetterman, B.L.; Luxford, W.M.; Saunders, J.E. Sudden bilateral sensorineural hearing loss. Laryngoscope 1996, 106, 1347–1350. [Google Scholar] [CrossRef]
- Chau, J.K.; Lin, J.R.; Atashband, S.; Irvine, R.A.; Westerberg, B.D. Systematic review of the evidence for the etiology of adult sudden sensorineural hearing loss. Laryngoscope 2010, 120, 1011–1021. [Google Scholar] [CrossRef]
- Schuknecht, H.F.; Donovan, E.D. The pathology of idiopathic sudden sensorineural hearing loss. Arch. Otorhinolaryngol. 1986, 243, 1–15. [Google Scholar] [CrossRef]
- Capaccio, P.; Ottaviani, F.; Cuccarini, V.; Bottero, A.; Schindler, A.; Cesana, B.M.; Censuales, S.; Pignataro, L. Genetic and acquired prothrombotic risk factors and sudden hearing loss. Laryngoscope 2007, 117, 547–551. [Google Scholar] [CrossRef]
- Wilson, W.R.; Byl, F.M.; Laird, N. The efficacy of steroids in the treatment of idiopathic sudden hearing loss. A double-blind clinical study. Arch. Otolaryngol. 1980, 106, 772–776. [Google Scholar] [CrossRef] [PubMed]
- Cvorović, L.; Deric, D.; Probst, R.; Hegemann, S. Prognostic model for predicting hearing recovery in idiopathic sudden sensorineural hearing loss. Otol. Neurotol. 2008, 29, 464–469. [Google Scholar] [CrossRef] [PubMed]
- Mattox, D.E.; Simmons, F.B. Natural history of sudden sensorineural hearing loss. Ann. Otol. Rhinol. Laryngol. 1977, 86, 463–480. [Google Scholar] [CrossRef] [PubMed]
- Psillas, G.; Rizou, A.; Rachovitsas, D.; Tsiropoulos, G.; Constantinidis, J. Hearing Outcome of Low-tone Compared to High-tone Sudden Sensorineural Hearing Loss. Int. Arch. Otorhinolaryngol. 2019, 23, 65–69. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.; Lim, H.; Lee, K.; Hong, C.E.; Choi, H.S. High Risk of Sudden Sensorineural Hearing Loss in Several Autoimmune Diseases according to a Population-Based National Sample Cohort Study. Audiol. Neurootol. 2019, 24, 224–230. [Google Scholar] [CrossRef] [PubMed]
- Atula, S.; Sinkkonen, S.T.; Saat, R.; Sairanen, T.; Atula, T. Association of multiple sclerosis and sudden sensorineural hearing loss. Mult. Scler. J. Exp. Transl. Clin. 2016, 2, 2055217316652155. [Google Scholar] [CrossRef] [PubMed]
- Franklin, D.J.; Coker, N.J.; Jenkins, H.A. Sudden sensorineural hearing loss as a presentation of multiple sclerosis. Arch. Otolaryngol. Head Neck Surg. 1989, 115, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Shea, J.J., 3rd; Brackmann, D.E. Multiple sclerosis manifesting as sudden hearing loss. Otolaryngol. Head Neck Surg. 1987, 97, 335–338. [Google Scholar] [CrossRef]
- Yamasoba, T.; Sakai, K.; Sakurai, M. Role of acute cochlear neuritis in sudden hearing loss in multiple sclerosis. J. Neurol. Sci. 1997, 146, 179–181. [Google Scholar] [CrossRef]
- Ozünlü, A.; Mus, N.; Gülhan, M. Multiple sclerosis: A cause of sudden hearing loss. Audiology 1998, 37, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Tekin, M.; Acar, G.O.; Cam, O.H.; Hanege, F.M. Sudden sensorineural hearing loss in a multiple sclerosis case. North Clin. Istanb. 2014, 1, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Hellmann, M.A.; Steiner, I.; Mosberg-Galili, R. Sudden sensorineural hearing loss in multiple sclerosis: Clinical course and possible pathogenesis. Acta Neurol. Scand. 2011, 124, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Anagnostouli, M.C.; Sotirchos, E.S.; Zalonis, I.; Christidi, F.; Korres, S.; Rentzos, M.; Davaki, P. Monosymptomatic clinically isolated syndrome with sudden sensorineural hearing loss: Case report and critical review of the literature. Neurologist 2012, 18, 302–305. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Jeon, E.S.; Cho, H.H. Auditory Evoked Potential Inconsistency in Sudden Unilateral Hearing Loss with Multiple Sclerosis. J. Int. Adv. Otol. 2019, 15, 160–164. [Google Scholar] [CrossRef] [PubMed]
- Drulović, B.; Ribarić-Jankes, K.; Kostić, V.; Sternić, N. Multiple sclerosis as the cause of sudden ‘pontine’ deafness. Audiology 1994, 33, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Furman, J.M.; Durrant, J.D.; Hirsch, W.L. Eighth nerve signs in a case of multiple sclerosis. Am. J. Otolaryngol. 1989, 10, 376–381. [Google Scholar] [CrossRef]
- Stach, B.A.; Delgado-Vilches, G. Sudden hearing loss in multiple sclerosis: Case report. J. Am. Acad. Audiol. 1993, 4, 370–375. [Google Scholar]
- Leite, H.F.; Leite, J.d.C.; Melo, M.H.; Vasconcelos, C.C.; Alvarenga, R.M. Deafness in patients with multiple sclerosis. Audiol. Neurootol. 2014, 19, 261–266. [Google Scholar] [CrossRef]
- Oh, Y.M.; Oh, D.H.; Jeong, S.H.; Koo, J.W.; Kim, J.S. Sequential bilateral hearing loss in multiple sclerosis. Ann. Otol. Rhinol. Laryngol. 2008, 117, 186–191. [Google Scholar] [CrossRef]
- Fernández-Menéndez, S.; Redondo-Robles, L.; García-Santiago, R.; García-González, M.Á.; Arés-Luque, A. Isolated deafness in multiple sclerosis patients. Am. J. Otolaryngol. 2014, 35, 810–813. [Google Scholar] [CrossRef] [PubMed]
- Valente, P.; Pinto, I.; Aguiar, C.; Castro, E.; Condé, A.; Larangeiro, J. Acute vestibular syndrome and hearing loss mimicking labyrinthitis as initial presentation of multiple sclerosis. Int. J. Pediatr. Otorhinolaryngol. 2020, 134, 110048. [Google Scholar] [CrossRef] [PubMed]
- Cruz, R.A.; Varkey, T.; Flavia, A.; Samways, A.P.A.; Garza, A.; Greenlee, G.; Friess, M.; Sconzert, J.; Aijaz, A.; Arruda, W.; et al. Hearing abnormalities in multiple sclerosis: Clinical semiology and pathophysiologic mechanisms. J. Neurol. 2022, 269, 2792–2805. [Google Scholar] [CrossRef] [PubMed]
- Peyvandi, A.; Naghibzadeh, B.; Ahmady Roozbahany, N. Neuro-otologic manifestations of multiple sclerosis. Arch. Iran Med. 2010, 13, 188–192. [Google Scholar] [PubMed]
- Protti-Patterson, E.; Young, M.L. The use of subjective and objective audiologic test procedures in the diagnosis of multiple sclerosis. Otolaryngol. Clin. North Am. 1985, 18, 241–255. [Google Scholar] [CrossRef] [PubMed]
- Crnošija, L.; Krbot Skorić, M.; Gabelić, T.; Adamec, I.; Habek, M. Vestibular evoked myogenic potentials and MRI in early multiple sclerosis: Validation of the VEMP score. J. Neurol. Sci. 2017, 372, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Gabelić, T.; Krbot Skorić, M.; Adamec, I.; Barun, B.; Zadro, I.; Habek, M. The vestibular evoked myogenic potentials (VEMP) score: A promising tool for evaluation of brainstem involvement in multiple sclerosis. Eur. J. Neurol. 2015, 22, 261–269. [Google Scholar] [CrossRef]
- Eleftheriadou, A.; Deftereos, S.N.; Zarikas, V.; Panagopoulos, G.; Sfetsos, S.; Karageorgiou, C.L.; Ferekidou, E.; Kandiloros, D.; Korres, S. The diagnostic value of earlier and later components of Vestibular Evoked Myogenic Potentials (VEMP) in multiple sclerosis. J. Vestib. Reb. 2009, 19, 59–66. [Google Scholar] [CrossRef]
- Skorić, M.K.; Adamec, I.; Mađarić, V.N.; Habek, M. Evaluation of brainstem involvement in multiple sclerosis. Can. J. Neurol. Sci. 2014, 41, 346–349. [Google Scholar] [CrossRef]
- Wei, F.Q.; Wen, L.; Chen, K.; Liu, M.; Wu, X. Different prognoses in patients with profound sudden sensorineural hearing loss. Acta Otolaryngol. 2019, 139, 598–603. [Google Scholar] [CrossRef]
- Kizkapan, D.B.; Karlidag, T.; Basar, F.; Kaygusuz, I.; Keles, E.; Akyigit, A.; Turkman, T.; Yalcin, S. Vestibular functions in patients with idiopathic sudden sensorineural hearing loss and its relation to prognosis. Auris Nasus Larynx 2022, 49, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.M.; Lo, W.C.; Young, Y.H.; Liao, L.J.; Cheng, P.W. Relationship Between Galvanic Vestibular-evoked Myogenic Potentials and the Prognosis of Unilateral Severe to Profound Idiopathic Sudden Sensorineural Hearing Loss With Vertigo. Otol. Neurotol. 2021, 42, e858–e865. [Google Scholar] [CrossRef] [PubMed]
- Ciodaro, F.; Freni, F.; Alberti, G.; Forelli, M.; Gazia, F.; Bruno, R.; Sherdell, E.P.; Galletti, B.; Galletti, F. Application of Cervical Vestibular-Evoked Myogenic Potentials in Adults with Moderate to Profound Sensorineural Hearing Loss: A Preliminary Study. Int. Arch. Otorhinolaryngol. 2020, 24, e5–e10. [Google Scholar] [CrossRef] [PubMed]
- Vollertsen, R.S.; McDonald, T.J.; Younge, B.R.; Banks, P.M.; Stanson, A.W.; Ilstrup, D.M. Cogan’s syndrome: 18 cases and a review of the literature. Mayo Clin. Proc. 1986, 61, 344–361. [Google Scholar] [CrossRef] [PubMed]
- Podder, S.; Shepherd, R.C. Cogan’s syndrome: A rare systemic vasculitis. Arch. Dis. Child. 1994, 71, 163–164. [Google Scholar] [CrossRef] [PubMed]
- Gluth, M.B.; Baratz, K.H.; Matteson, E.L.; Driscoll, C.L. Cogan syndrome: A retrospective review of 60 patients throughout a half century. Mayo Clin. Proc. 2006, 81, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Haynes, B.F.; Kaiser-Kupfer, M.I.; Mason, P.; Fauci, A.S. Cogan syndrome: Studies in thirteen patients, long-term follow-up, and a review of the literature. Medicine 1980, 59, 426–441. [Google Scholar] [CrossRef] [PubMed]
- Grasland, A.; Pouchot, J.; Hachulla, E.; Blétry, O.; Papo, T.; Vinceneux, P.; Study Group for Cogan’s Syndrome. Typical and atypical Cogan’s syndrome: 32 cases and review of the literature. Rheumatology 2004, 43, 1007–1015. [Google Scholar] [CrossRef]
- St Clair, E.W.; McCallum, R.M. Cogan’s syndrome. Curr. Opin. Rheumatol. 1999, 11, 47–52. [Google Scholar] [CrossRef]
- Bloch, D.B.; San Martin, J.E.; Rauch, S.D.; Moscicki, R.A.; Bloch, K.J. Serum antibodies to heat shock protein 70 in sensorineural hearing loss. Arch. Otolaryngol. Head Neck Surg. 1995, 121, 1167–1171. [Google Scholar] [CrossRef]


| Author (Year) | Sample Size | Age | Gender | Treatment Modality | Treatment Outcome | Recovery Period |
|---|---|---|---|---|---|---|
| Hellmann et al. (2011) [19] | Eleven | 34.5 (17–52) | M: Four F: Seven | Three: No treatment Eight: IV methylprednisolone for 3–5 days, then a tapering course of oral prednisolone over 2 weeks | Ten: Recovered One: Not recovered | 1–2 months |
| Leite et al. (2014) [29] | Seven | 35.4 (21–51) | M: One F: Six | Three: No treatment Four: Pulse therapy of methylprednisolone | Among the three without treatment, two: partially recovered and one: not recovered; Among the four with treatment, three: fully recovered and one: not recovered | Not described |
| Author (Year) | Sample Size | Age | Gender | Side | Degree of the Loss | Treatment Modality | Treatment Outcome | Recovery Period |
|---|---|---|---|---|---|---|---|---|
| Shea and Brackman (1987) [19] | 1 | 20 | F | L | Profound loss at all frequencies | Prednisolone (60 mg/day) for 1 week and hydrochlorothiazide (50 mg/day) | Recovered | 5 months |
| Drulović et al. (1994) [26] | 2 | 33 | F | L | 50–60 dB | Not described | Recovered | 1 months |
| 20 | F | R | 70–90 dB at 4–8 kHz | Corticosteroid | Recovered | 14 days | ||
| Ozünlü et al. (1998) [21] | 1 | 26 | F | L | Profound loss (SDS 42%) | Corticosteroid (60 mg/day) | Recovered | 16 days |
| Oh et al. (2008) [30] 1 | 1 | 46 | F | L → R | Profound loss | Methylprednisolone (1 g/day) for 1 week | Lt: Recovered Rt: None | 2 months |
| Anagnostouli et al. (2012) [24] | 1 | 34 | M | L | Not described | ITDI and IV methylprednisolone (1 g/day) for 5 days and tapering for 6 months | Recovered | 8 months |
| Fernández-Menéndez et al. (2014) [31] | 3 | 29 | F | L | Not described | Five-day course of IV methylprednisolone (1 g/day) | Partially recovered | Not described |
| Valente et al. (2020) [32] | 1 | 17 | F | R | 90 dB at 2–8 kHz | IV dexamethasone 8 mg and dihydrochloride 48 mg/day | Recovered | 4 days |
| Cruz et al. (2022) [33] | 4 | 26 | M | R | 65 dB at 3–8 kHz | Oral corticosteroid and then ITDI | Not recovered | Not described |
| Author (Year) | Sample Size | Age | Gender | Side | Degree of the Loss | Treatment Modality | Treatment Outcome | Recovery Period |
|---|---|---|---|---|---|---|---|---|
| Furman et al. (1989) [27] | 1 | 25 | F | R | Loss at 2–8 kHz SDS: 28% | Not described | Recovered | 5 months |
| Yamasoba et al. (1997) [20] | 1 | 30 | M | L | 22 dB SDS: 90% | Four courses of methylprednisolone (1 g/day for 3 days) | Recovered | 4 months |
| Fernández-Menéndez et al. (2014) [31] 1 | 3 | 29 | F | R | Not described | Five-day course of IV methylprednisolone (1 g/day) | Recovered | Not described |
| Tekin et al. (2014) [22] | 1 | 30 | F | R | 113 dB | Prednisolone 1 mg/kg/day with tapering Hyperbaric oxygen therapy for 10 days | Recovered | 3 months |
| Lee et al. (2019) [25] | 1 | 28 | M | R | 30 dB at 2 kHz | Steroid pulse therapy | Recovered | 1 month |
| Cruz et al. (2022) [33] 2 | 4 | 28 | F | B | 36.3 dB at Rt 40 dB at Lt | 12-day steroid with a daily dose of 80 mg prednisolone | Recovered | 4–6 weeks |
| 44 | F | L | 86.3 dB | Three-cycles of five-full-volume plasma exchange Six weekly doses of etanercept, anti-TNF agent | Partially recovered (51.3 dB) | 6 weeks |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, I.; Kim, H. Management of Sudden Sensorineural Hearing Loss in Multiple Sclerosis: A Comprehensive Case Report of a Patient with Bilateral Loss and Literature Review. Life 2024, 14, 83. https://doi.org/10.3390/life14010083
Kim I, Kim H. Management of Sudden Sensorineural Hearing Loss in Multiple Sclerosis: A Comprehensive Case Report of a Patient with Bilateral Loss and Literature Review. Life. 2024; 14(1):83. https://doi.org/10.3390/life14010083
Chicago/Turabian StyleKim, Ikhee, and Hantai Kim. 2024. "Management of Sudden Sensorineural Hearing Loss in Multiple Sclerosis: A Comprehensive Case Report of a Patient with Bilateral Loss and Literature Review" Life 14, no. 1: 83. https://doi.org/10.3390/life14010083
APA StyleKim, I., & Kim, H. (2024). Management of Sudden Sensorineural Hearing Loss in Multiple Sclerosis: A Comprehensive Case Report of a Patient with Bilateral Loss and Literature Review. Life, 14(1), 83. https://doi.org/10.3390/life14010083







