Analysis of Refractive Errors in a Large Italian Cohort of Pediatric Subjects Post the COVID-19 Pandemic
Abstract
1. Introduction
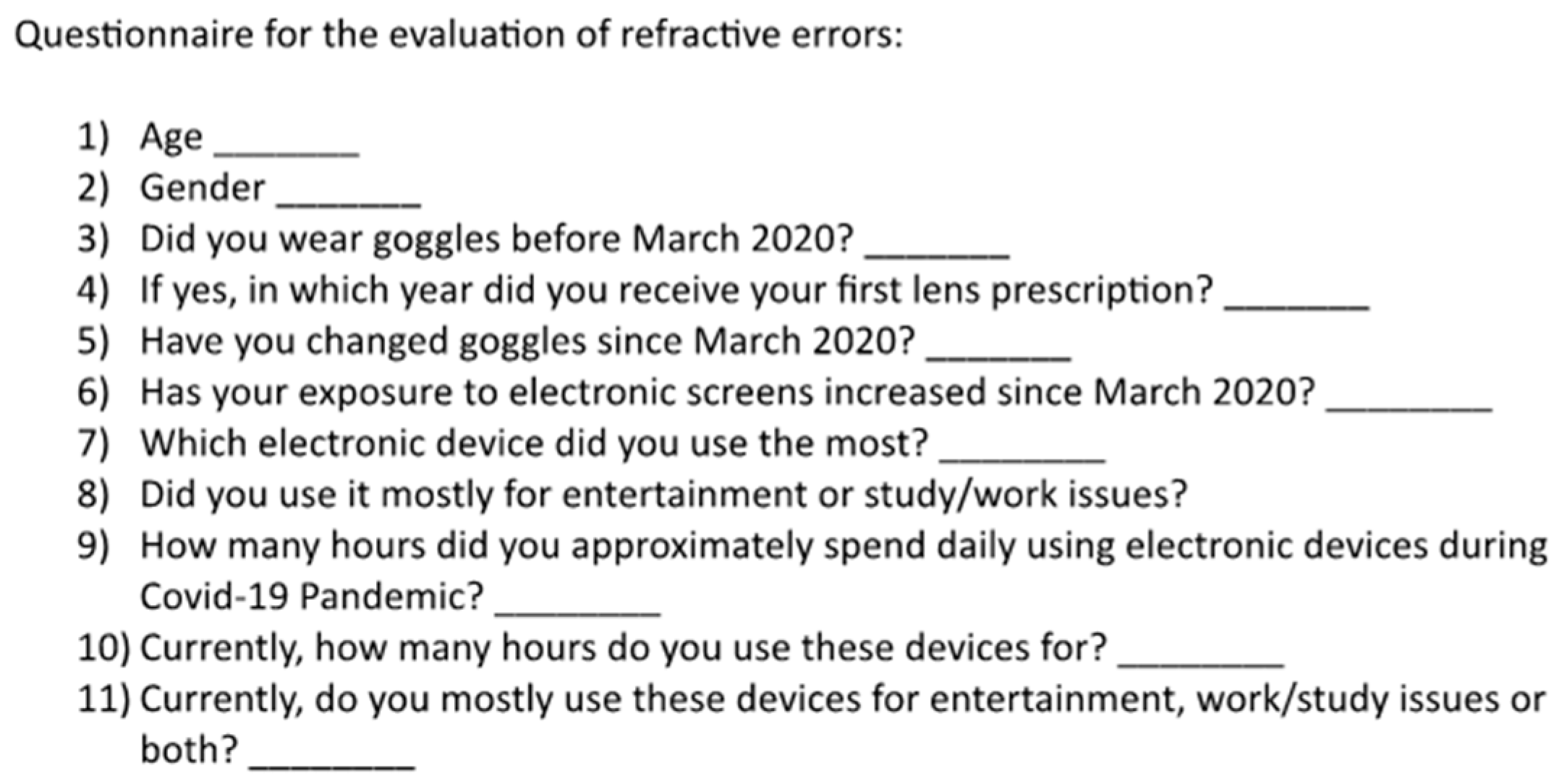
2. Materials and Methods
Patients
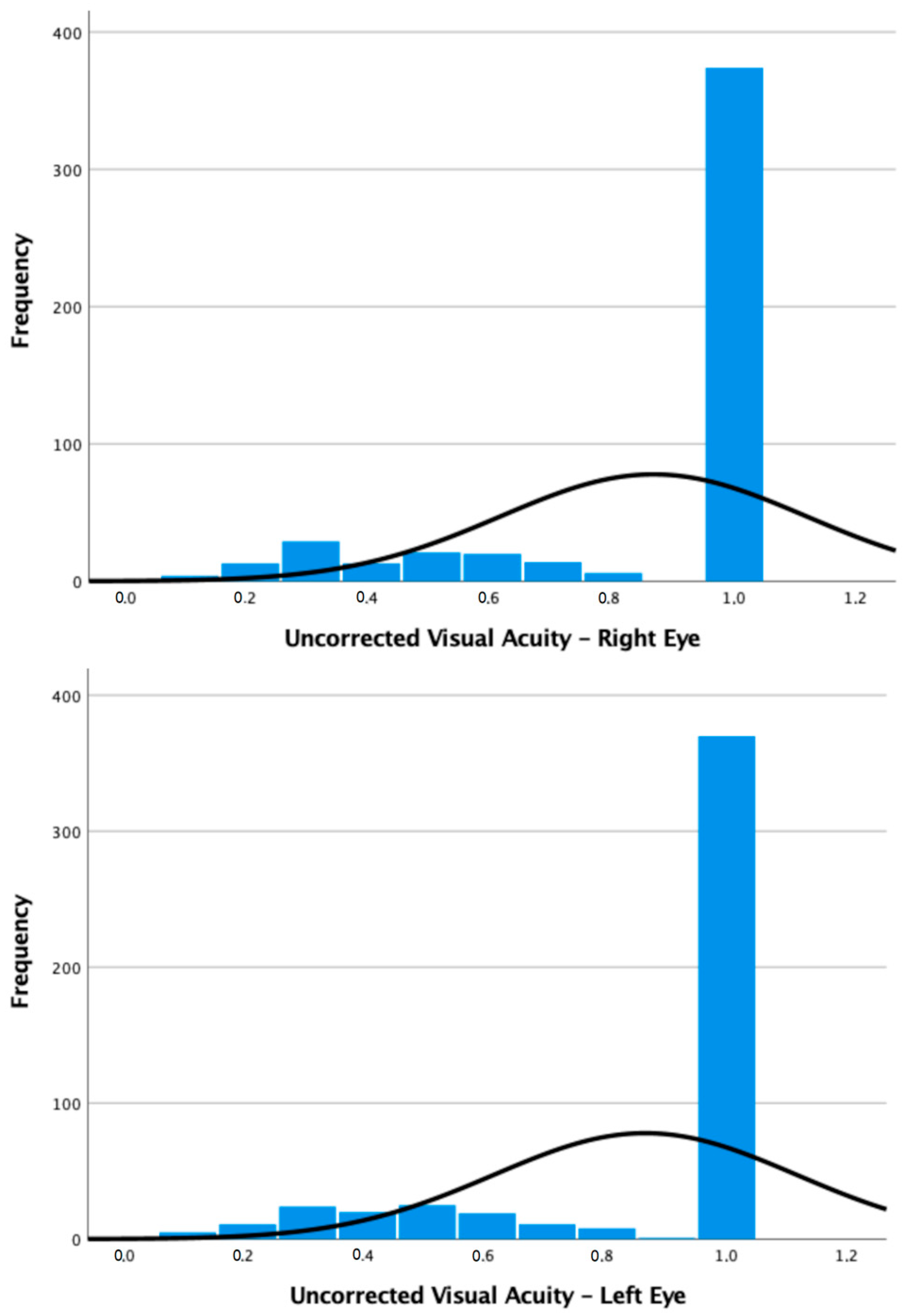
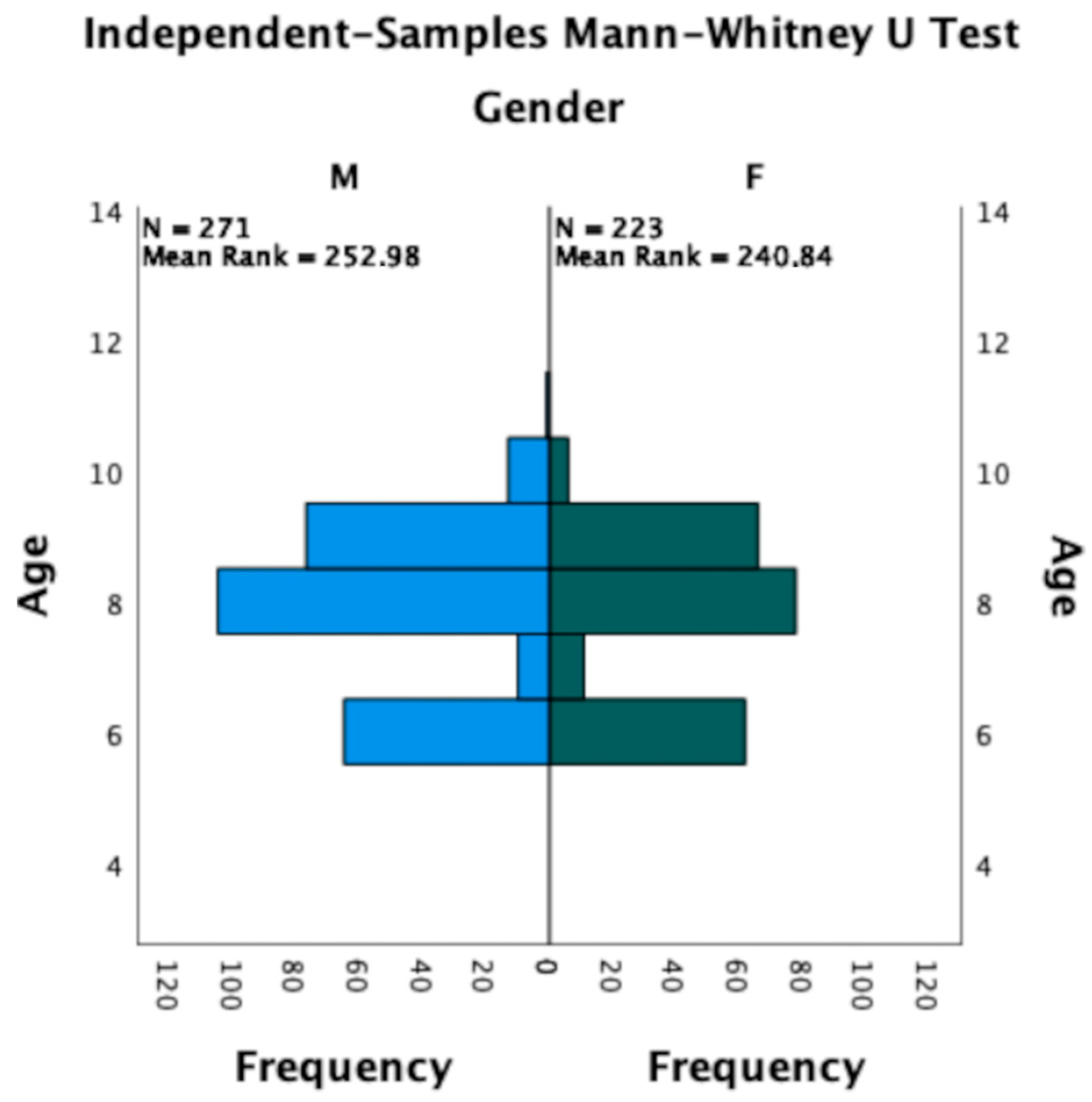
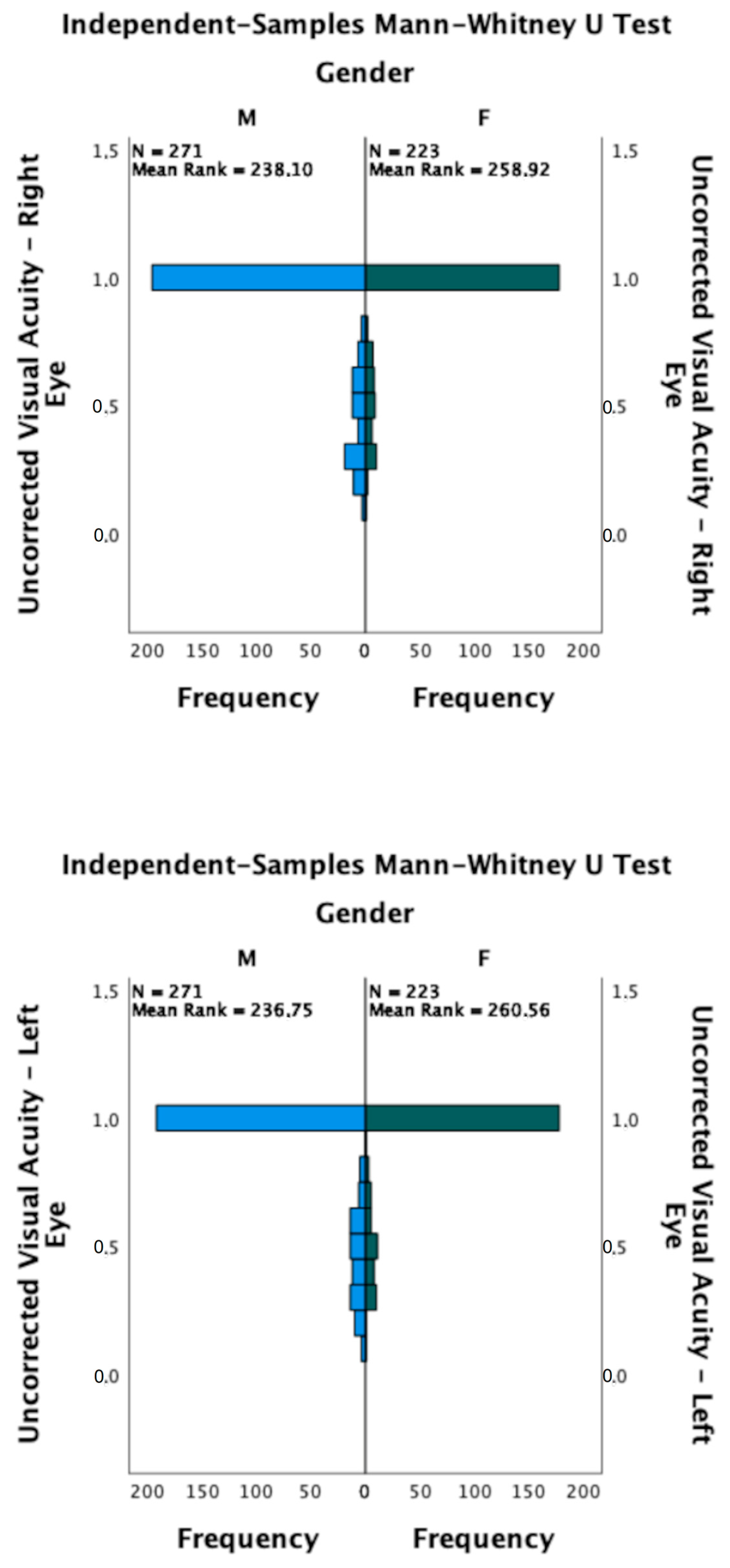
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mu, J.; Zeng, D.; Fan, J.; Liu, M.; Jiang, M.; Shuai, X.; Wang, J.; Zhang, S. Epidemiological Characteristics and Influencing Factors of Myopia Among Primary School Students in Southern China: A Longitudinal Study. Int. J. Public Health 2023, 68, 1605424. [Google Scholar] [CrossRef] [PubMed]
- Harrington, S.C.; Stack, J.; Saunders, K.; O’Dwyer, V. Refractive Error and Visual Impairment in Ireland Schoolchildren. Br. J. Ophthalmol. 2019, 103, 1112–1118. [Google Scholar] [CrossRef] [PubMed]
- Dolgin, E. The Myopia Boom. Nature 2015, 519, 276–278. [Google Scholar] [CrossRef] [PubMed]
- WHO. World Report on Vision; World Health Organisation: Geneva, Switzerland, 2019; Volume 214, pp. 180–235.
- Saw, S.M.; Matsumura, S.; Hoang, Q.V. Prevention and Management of Myopia and Myopic Pathology. Investig. Ophthalmol. Vis. Sci. 2019, 60, 488–499. [Google Scholar] [CrossRef]
- Saw, S.M.; Gazzard, G.; Shin-Yen, E.C.; Chua, W.H. Myopia and Associated Pathological Complications. Ophthalmic. Physiol. Opt. 2005, 25, 381–391. [Google Scholar] [CrossRef]
- UNESCO. UNESCO COVID-19 Education Response: How Many Students Are at Risk of Not Returning to School? Advocacy Paper; United Nations Educational, Scientific and Cultural Organization: Paris, France, 2020. [Google Scholar]
- Dong, Y.; Jan, C.; Chen, L.; Ma, T.; Liu, J.; Zhang, Y.; Ma, Q.; Zhong, P.; Song, Y.; Ma, J.; et al. The Cumulative Effect of Multilevel Factors on Myopia Prevalence, Incidence, and Progression Among Children and Adolescents in China During the COVID-19 Pandemic. Transl. Vis. Sci. Technol. 2022, 11, 9. [Google Scholar] [CrossRef]
- Wong, C.W.; Tsai, A.; Jonas, J.B.; Ohno-Matsui, K.; Chen, J.; Ang, M.; Ting, D.S.W. Digital Screen Time During the COVID-19 Pandemic: Risk for a Further Myopia Boom? Am. J. Ophthalmol. 2021, 223, 333–337. [Google Scholar] [CrossRef]
- He, M.; Zheng, Y.; Xiang, F. Prevalence of Myopia in Urban and Rural Children in Mainland China. Optom. Vis. Sci. 2009, 86, 40–44. [Google Scholar] [CrossRef]
- Theophanous, C.; Modjtahedi, B.S.; Batech, M.; Marlin, D.S.; Luong, T.Q.; Fong, D.S. Myopia Prevalence and Risk Factors in Children. Clin. Ophthalmol. 2018, 12, 1581–1587. [Google Scholar] [CrossRef]
- Ting, D.S.W.; Carin, L.; Dzau, V.; Wong, T.Y. Digital Technology and COVID-19. Nat. Med. 2020, 26, 459–461. [Google Scholar] [CrossRef]
- Zhang, X.; Cheung, S.S.L.; Chan, H.N.; Zhang, Y.; Wang, Y.M.; Yip, B.H.; Kam, K.W.; Yu, M.; Cheng, C.Y.; Young, A.L.; et al. Myopia Incidence and Lifestyle Changes among School Children during the COVID-19 Pandemic: A Population-Based Prospective Study. Br. J. Ophthalmol. 2022, 106, 1772–1778. [Google Scholar] [CrossRef] [PubMed]
- Wen, L.; Cao, Y.; Cheng, Q.; Li, X.; Pan, L.; Li, L.; Zhu, H.G.; Lan, W.; Yang, Z. Objectively Measured near Work, Outdoor Exposure and Myopia in Children. Br. J. Ophthalmol. 2020, 104, 1542–1547. [Google Scholar] [CrossRef] [PubMed]
- Lingham, G.; MacKey, D.A.; Lucas, R.; Yazar, S. How Does Spending Time Outdoors Protect against Myopia? A Review. Br. J. Ophthalmol. 2020, 104, 593–599. [Google Scholar] [CrossRef]
- Pellegrini, M.; Bernabei, F.; Scorcia, V.; Giannaccare, G. May Home Confinement during the COVID-19 Outbreak Worsen the Global Burden of Myopia? Graefes Arch. Clin. Exp. Ophthalmol. 2020, 258, 2069–2070. [Google Scholar] [CrossRef]
- Abounoori, M.; Aghajani, A.; Chaibakhsh, S.; Babakhanian, M.; Pourazizi, M.; Peyman, A. Paediatric Myopia Shift during the COVID-19 Pandemic Home Quarantine: A Systematic Review and Meta-Analysis. BMJ Paediatr. Open 2022, 6, e001755. [Google Scholar] [CrossRef] [PubMed]
- Mike, E.V.; Laroche, D. Preserving Vision in the COVID-19 Pandemic: Focus on Health Equity. Clin. Ophthalmol. 2020, 14, 2073–2077. [Google Scholar] [CrossRef] [PubMed]
- Almhdawi, K.A.; Alsalem, M.F.; Obeidat, D.; Al-Khateeb, L.T.; Al Aqarbah, M.N.; Alshiyab, W.M.; Arabiat, A.A.; Bazel, M.A.; Al-Share, Z. Evaluating Well-Being of Individuals With Chronic Visual Conditions Requiring Regular Eyecare During COVID-19 Lockdown: A Cross-Sectional Study. Eye Contact Lens 2021, 47, 559–564. [Google Scholar] [CrossRef]
- Brown, A.; Kassam, A.; Paget, M.; Blades, K.; Mercia, M.; Kahcra, R. Exploring the Global Impact of the COVID-19 Pandemic on Medical Education: An International Cross-Sectional Study of Medical Learners. Can. Med. Educ. J. 2021, 12, 28–43. [Google Scholar] [CrossRef]
- Navel, V.; Beze, S.; Dutheil, F. COVID-19, Sweat, Tears… and Myopia? Clin. Exp. Optom. 2020, 103, 555. [Google Scholar] [CrossRef]
- Ye, S.; Chen, L.; Wang, Q.; Li, Q. Correlates of Screen Time among 8-19-Year-Old Students in China. BMC Public Health 2018, 18, 467. [Google Scholar] [CrossRef]
- Harb, E.; Thorn, F.; Troilo, D. Characteristics of Accommodative Behavior during Sustained Reading in Emmetropes and Myopes. Vision Res. 2006, 46, 2581–2592. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Tang, Y.; Zhuang, J.; Liu, Y.; Wu, X.; Cai, Y.; Wang, L.; Cao, Z.B.; Chen, P. Physical Activity, Screen Viewing Time, and Overweight/Obesity among Chinese Children and Adolescents: An Update from the 2017 Physical Activity and Fitness in China-the Youth Study. BMC Public Health 2019, 19, 197. [Google Scholar] [CrossRef] [PubMed]
- Hansen, M.H.; Laigaard, P.P.; Olsen, E.M.; Skovgaard, A.M.; Larsen, M.; Kessel, L.; Munch, I.C. Low Physical Activity and Higher Use of Screen Devices Are Associated with Myopia at the Age of 16-17 Years in the CCC2000 Eye Study. Acta Ophthalmol. 2020, 98, 315–321. [Google Scholar] [CrossRef] [PubMed]
- McBrien, N.A.; Gentle, A. Role of the Sclera in the Development and Pathological Complications of Myopia. Prog. Retin. Eye Res. 2003, 22, 307–338. [Google Scholar] [CrossRef]
- Bailey, M.D.; Sinnott, L.T.; Mutti, D.O. Ciliary Body Thickness and Refractive Error in Children. Investig. Ophthalmol. Vis. Sci. 2008, 49, 4353–4360. [Google Scholar] [CrossRef]
- Smith, E.L.; Hung, L.F.; Huang, J. Relative Peripheral Hyperopic Defocus Alters Central Refractive Development in Infant Monkeys. Vision Res. 2009, 49, 2386–2392. [Google Scholar] [CrossRef]
- Han, X.; Liu, C.; Chen, Y.; He, M. Myopia Prediction: A Systematic Review. Eye 2022, 36, 921–929. [Google Scholar] [CrossRef]
- Long, J.; Cheung, R.; Duong, S.; Paynter, R.; Asper, L. Viewing Distance and Eyestrain Symptoms with Prolonged Viewing of Smartphones. Clin. Exp. Optom. 2017, 100, 133–137. [Google Scholar] [CrossRef]
- Saxena, R.; Vashist, P.; Tandon, R.; Pandey, R.M.; Bhardawaj, A.; Menon, V.; Mani, K. Prevalence of Myopia and Its Risk Factors in Urban School Children in Delhi: The North India Myopia Study (NIM Study). PLoS ONE 2015, 10, e0117349. [Google Scholar] [CrossRef]
- Hashemi, H.; Fotouhi, A.; Yekta, A.; Pakzad, R.; Ostadimoghaddam, H.; Khabazkhoob, M. Global and Regional Estimates of Prevalence of Refractive Errors: Systematic Review and Meta-Analysis. J. Curr. Ophthalmol. 2018, 30, 3. [Google Scholar] [CrossRef]
- Trovato Battagliola, E.; Mangiantini, P.; D’andrea, M.; Malvasi, M.; Loffredo, L.; Scalinci, S.Z.; Comberiati, A.M.; Migliorini, R.; Pacella, E. Effect of COVID-19 Lockdown on Refractive Errors in Italian Children Aged 5–12 Years: A Multi-Center Retrospective Study Key Points. Eur. J. Ophthalmol. 2021, 33, 112–122. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Z.; Chen, Y.; Tan, Z.; Xiong, R.; McGuinness, M.B.; Müller, A. Interventions Recommended for Myopia Prevention and Control among Children and Adolescents in China: A Systematic Review. Br. J. Ophthalmol. 2023, 107, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, H.; Khabazkhoob, M.; Asharlous, A.; Soroush, S.; Yekta, A.A.; Dadbin, N.; Fotouhi, A. Cycloplegic Autorefraction versus Subjective Refraction: The Tehran Eye Study. Br. J. Ophthalmol. 2016, 100, 1122–1127. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.K.; Guo, Y.; Liao, C.; Chen, Y.; Su, G.; Zhang, G.; Zhang, L.; He, M. Incidence of and Factors Associated With Myopia and High Myopia in Chinese Children, Based on Refraction Without Cycloplegia. JAMA Ophthalmol. 2018, 136, 1017–1024. [Google Scholar] [CrossRef]
- Zhang, J.; Li, Z.; Ren, J.; Wang, W.; Dai, J.; Li, C.; Huang, X.; Sun, X.; Liu, L.; Wang, C. Prevalence of Myopia: A Large-Scale Population-Based Study among Children and Adolescents in Weifang, China. Front. Public Health 2022, 10, 2329. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lanza, M.; Ruggiero, A.; Ruggiero, M.; Iodice, C.M.; Simonelli, F. Analysis of Refractive Errors in a Large Italian Cohort of Pediatric Subjects Post the COVID-19 Pandemic. Life 2023, 13, 1569. https://doi.org/10.3390/life13071569
Lanza M, Ruggiero A, Ruggiero M, Iodice CM, Simonelli F. Analysis of Refractive Errors in a Large Italian Cohort of Pediatric Subjects Post the COVID-19 Pandemic. Life. 2023; 13(7):1569. https://doi.org/10.3390/life13071569
Chicago/Turabian StyleLanza, Michele, Adriano Ruggiero, Matteo Ruggiero, Clemente Maria Iodice, and Francesca Simonelli. 2023. "Analysis of Refractive Errors in a Large Italian Cohort of Pediatric Subjects Post the COVID-19 Pandemic" Life 13, no. 7: 1569. https://doi.org/10.3390/life13071569
APA StyleLanza, M., Ruggiero, A., Ruggiero, M., Iodice, C. M., & Simonelli, F. (2023). Analysis of Refractive Errors in a Large Italian Cohort of Pediatric Subjects Post the COVID-19 Pandemic. Life, 13(7), 1569. https://doi.org/10.3390/life13071569







