Transcatheter Tricuspid Valve Interventions: A Triumph for Transcatheter Procedures?
Abstract
1. Introduction
2. Pathophysiology of Tricuspid Regurgitation
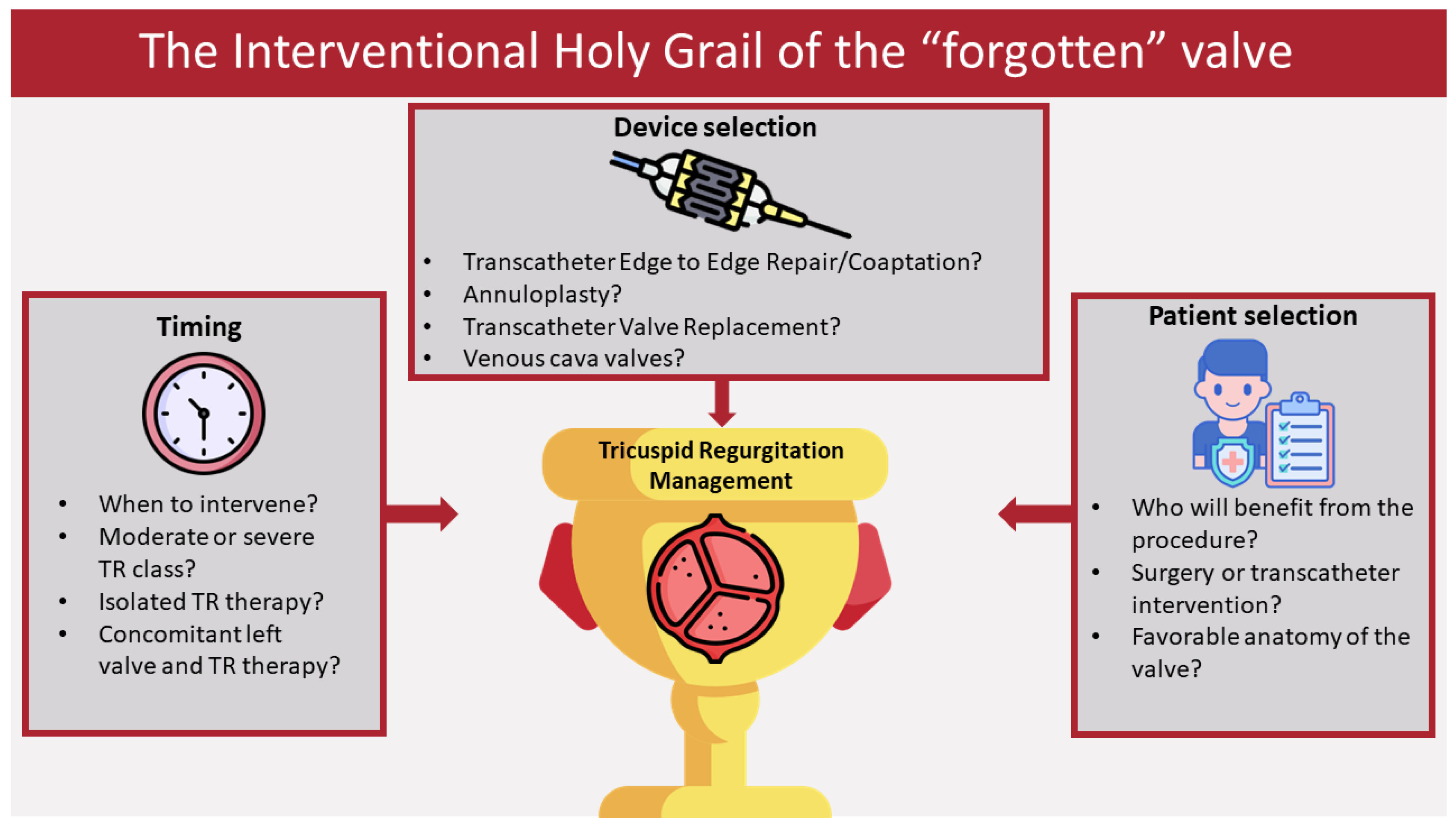
3. Need for Interventional Therapies–Transcatheter Intervention Options
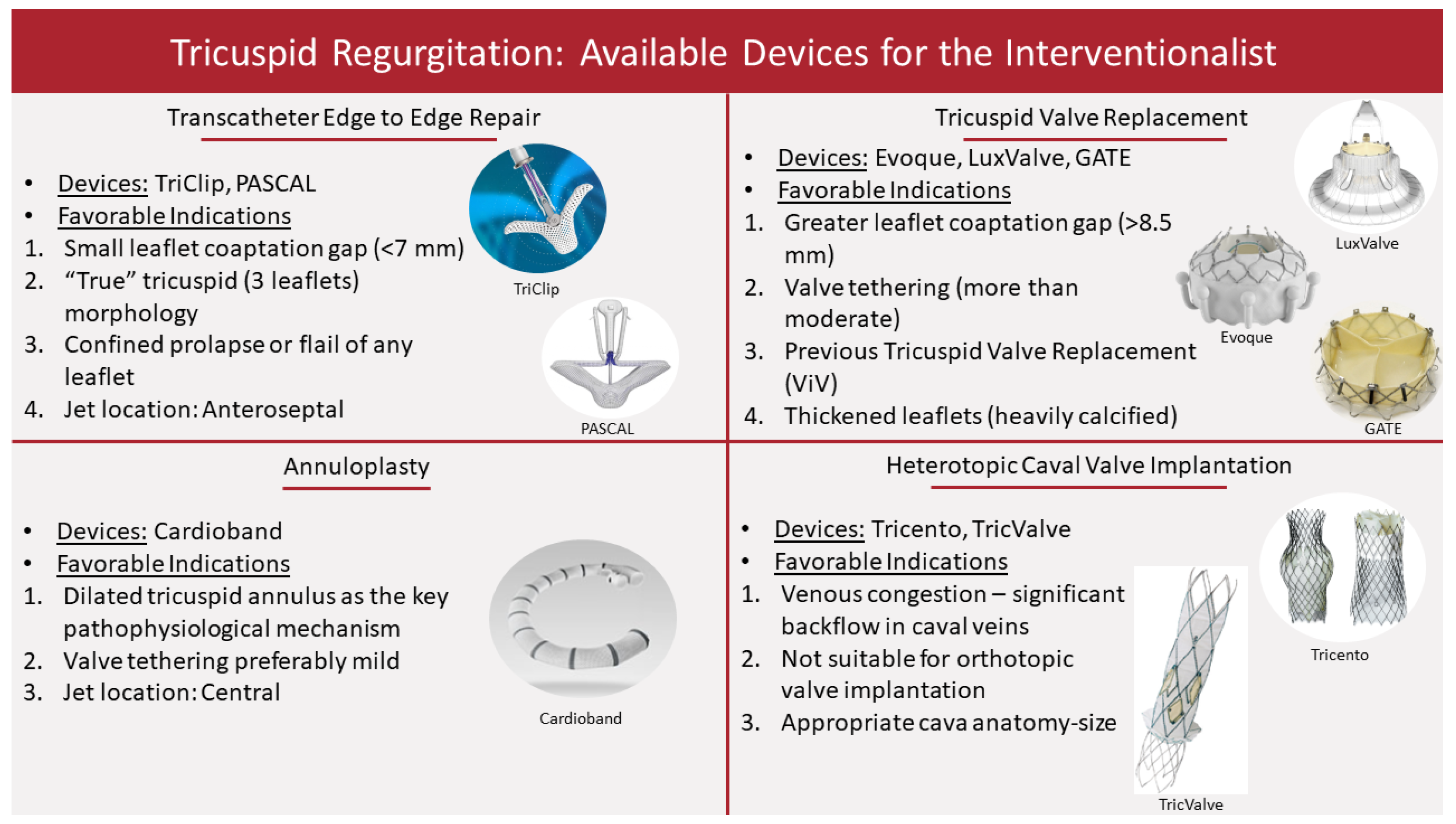
3.1. Leaflet Approximation
3.1.1. TriClip (Previously MitraClip)
3.1.2. PASCAL
3.2. Annuloplasty
Cardioband
3.3. Tricuspid Valve Replacement
3.3.1. GATE
3.3.2. Lux-Valve
3.3.3. Evoque
3.4. Heterotropic Caval Valve Implantation
4. Clinical Implications
5. Future Directions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Singh, J.P.; Evans, J.C.; Levy, D.; Larson, M.G.; Freed, L.A.; Fuller, D.L.; Lehman, B.; Benjamin, E.J. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study). Am. J. Cardiol. 1999, 83, 897–902. [Google Scholar] [CrossRef] [PubMed]
- Topilsky, Y.; Maltais, S.; Medina-Inojosa, J.; Oguz, D.; Michelena, H.; Maalouf, J.; Mahoney, D.W.; Enriquez-Sarano, M. Burden of Tricuspid Regurgitation in Patients Diagnosed in the Community Setting. JACC Cardiovasc. Imaging 2019, 12, 433–442. [Google Scholar] [CrossRef] [PubMed]
- D’Arcy, J.L.; Coffey, S.; Loudon, M.A.; Kennedy, A.; Pearson-Stuttard, J.; Birks, J.; Frangou, E.; Farmer, A.J.; Mant, D.; Wilson, J.; et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: The OxVALVE Population Cohort Study. Eur. Heart J. 2016, 37, 3515–3522. [Google Scholar] [CrossRef]
- Stuge, O.; Liddicoat, J. Emerging opportunities for cardiac surgeons within structural heart disease. J. Thorac. Cardiovasc. Surg. 2006, 132, 1258–1261. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Tuzcu, E.M.; Rodriguez, E.R.; Tan, C.D.; Rodriguez, L.L.; Kapadia, S.R. Interventional Cardiology Perspective of Functional Tricuspid Regurgitation. Circ. Cardiovasc. Interv. 2009, 2, 565–573. [Google Scholar] [CrossRef] [PubMed]
- Tung, M.; Nah, G.; Tang, J.; Marcus, G.; Delling, F.N. Valvular disease burden in the modern era of percutaneous and surgical interventions: The UK Biobank. Open Heart 2022, 9, e002039. [Google Scholar] [CrossRef]
- Cork, D.P.; McCullough, P.A.; Mehta, H.S.; Barker, C.M.; Van Houten, J.; Gunnarsson, C.; Ryan, M.P.; Baker, E.R.; Mollenkopf, S.; Verta, P. The economic impact of clinically significant tricuspid regurgitation in a large, administrative claims database. J. Med. Econ. 2020, 23, 521–528. [Google Scholar] [CrossRef]
- Nath, J.; Foster, E.; Heidenreich, P.A. Impact of tricuspid regurgitation on long-term survival. J. Am. Coll. Cardiol. 2004, 43, 405–409. [Google Scholar] [CrossRef]
- Hahn, R.T.; Asch, F.; Weissman, N.J.; Grayburn, P.; Kar, S.; Lim, S.; Ben-Yehuda, O.; Shahim, B.; Chen, S.; Liu, M.; et al. Impact of Tricuspid Regurgitation on Clinical Outcomes. J. Am. Coll. Cardiol. 2020, 76, 1305–1314. [Google Scholar] [CrossRef]
- Benfari, G.; Antoine, C.; Miller, W.L.; Thapa, P.; Topilsky, Y.; Rossi, A.; Michelena, H.I.; Pislaru, S.; Enriquez-Sarano, M. Excess Mortality Associated with Functional Tricuspid Regurgitation Complicating Heart Failure with Reduced Ejection Fraction. Circulation 2019, 140, 196–206. [Google Scholar] [CrossRef]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2021, 43, 561–632. [Google Scholar] [CrossRef] [PubMed]
- Kilic, A.; Saha-Chaudhuri, P.; Rankin, J.S.; Conte, J.V. Trends and Outcomes of Tricuspid Valve Surgery in North America: An Analysis of More Than 50,000 Patients From The Society of Thoracic Surgeons Database. Ann. Thorac. Surg. 2013, 96, 1546–1552. [Google Scholar] [CrossRef] [PubMed]
- Anselmi, A.; Ruggieri, V.G.; Harmouche, M.; Flécher, E.; Corbineau, H.; Langanay, T.; Lelong, B.; Verhoye, J.-P.; Leguerrier, A. Appraisal of Long-Term Outcomes of Tricuspid Valve Replacement in the Current Perspective. Ann. Thorac. Surg. 2015, 101, 863–871. [Google Scholar] [CrossRef] [PubMed]
- Dreyfus, J.; Ghalem, N.; Garbarz, E.; Cimadevilla, C.; Nataf, P.; Vahanian, A.; Caranhac, G.; Messika-Zeitoun, D. Timing of Referral of Patients with Severe Isolated Tricuspid Valve Regurgitation to Surgeons (from a French Nationwide Database). Am. J. Cardiol. 2018, 122, 323–326. [Google Scholar] [CrossRef]
- Zack, C.J.; Fender, E.A.; Chandrashekar, P.; Reddy, Y.N.; Bennett, C.E.; Stulak, J.M.; Miller, V.M.; Nishimura, R.A. National Trends and Outcomes in Isolated Tricuspid Valve Surgery. J. Am. Coll. Cardiol. 2017, 70, 2953–2960. [Google Scholar] [CrossRef]
- Condello, F.; Gitto, M.; Stefanini, G.G. Etiology, epidemiology, pathophysiology and management of tricuspid regurgitation: An overview. Rev. Cardiovasc. Med. 2021, 22, 1115–1142. [Google Scholar] [CrossRef]
- Ramcharan, T.K.W.; Goff, D.A.; Greenleaf, C.E.; Shebani, S.O.; Salazar, J.D.; Corno, A.F. Ebstein’s Anomaly: From Fetus to Adult—Literature Review and Pathway for Patient Care. Pediatr. Cardiol. 2022, 43, 1409–1428. [Google Scholar] [CrossRef]
- Boyle, B.; Garne, E.; Loane, M.; Addor, M.-C.; Arriola, L.; Cavero-Carbonell, C.; Gatt, M.; Lelong, N.; Lynch, C.; Nelen, V.; et al. The changing epidemiology of Ebstein’s anomaly and its relationship with maternal mental health conditions: A European registry-based study. Cardiol. Young 2016, 27, 677–685. [Google Scholar] [CrossRef]
- Lupo, P.J.; Langlois, P.H.; Mitchell, L.E. Epidemiology of Ebstein anomaly: Prevalence and patterns in Texas, 1999–2005. Am. J. Med. Genet. Part A 2011, 155, 1007–1014. [Google Scholar] [CrossRef]
- Sultan, F.A.T.; Moustafa, S.E.; Tajik, J.; Warsame, T.; Emani, U.; Alharthi, M.; Mookadam, F. Rheumatic tricuspid valve disease: An evidence-based systematic overview. J. Heart Valve Dis. 2010, 19, 374–382. [Google Scholar]
- Antunes, M.J.; Rodríguez-Palomares, J.; Prendergast, B.; De Bonis, M.; Rosenhek, R.; Al-Attar, N.; Barili, F.; Casselman, F.; Folliguet, T.; Iung, B.; et al. Management of tricuspid valve regurgitation. Eur. J. Cardio-Thoracic Surg. 2017, 52, 1022–1030. [Google Scholar] [CrossRef]
- Hassan, S.A.; Banchs, J.; Iliescu, C.; Dasari, A.; Lopez-Mattei, J.; Yusuf, S.W. Carcinoid heart disease. Heart 2017, 103, 1488–1495. [Google Scholar] [CrossRef]
- Hussain, S.T.; Witten, J.; Shrestha, N.K.; Blackstone, E.H.; Pettersson, G.B. Tricuspid valve endocarditis. Ann. Cardiothorac. Surg. 2017, 6, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Al-Mohaissen, M.A.; Chan, K.L. Prevalence and Mechanism of Tricuspid Regurgitation following Implantation of Endocardial Leads for Pacemaker or Cardioverter-Defibrillator. J. Am. Soc. Echocardiogr. 2012, 25, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Asmarats, L.; Taramasso, M.; Rodés-Cabau, J. Tricuspid valve disease: Diagnosis, prognosis and management of a rapidly evolving field. Nat. Rev. Cardiol. 2019, 16, 538–554. [Google Scholar] [CrossRef] [PubMed]
- Prihadi, E.A.; Delgado, V.; Leon, M.B.; Enriquez-Sarano, M.; Topilsky, Y.; Bax, J.J. Morphologic Types of Tricuspid Regurgitation: Characteristics and Prognostic Impli-cations. JACC Cardiovasc. Imaging 2019, 12, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Koren, O.; Darawsha, H.; Rozner, E.; Benhamou, D.; Turgeman, Y. Tricuspid regurgitation in ischemic mitral regurgitation patients: Prevalence, predictors for outcome and long-term follow-up. BMC Cardiovasc. Disord. 2021, 21, 199. [Google Scholar] [CrossRef]
- David, T.E.; David, C.M.; Fan, C.-P.S.; Manlhiot, C. Tricuspid regurgitation is uncommon after mitral valve repair for degenerative diseases. J. Thorac. Cardiovasc. Surg. 2017, 154, 110–122.e1. [Google Scholar] [CrossRef]
- Mantovani, F.; Fanti, D.; Tafciu, E.; Fezzi, S.; Setti, M.; Rossi, A.; Ribichini, F.; Benfari, G. When Aortic Stenosis Is Not Alone: Epidemiology, Pathophysiology, Diagnosis and Management in Mixed and Combined Valvular Disease. Front. Cardiovasc. Med. 2021, 8, 744497. [Google Scholar] [CrossRef]
- Utsunomiya, H.; Itabashi, Y.; Mihara, H.; Berdejo, J.; Kobayashi, S.; Siegel, R.J.; Shiota, T. Functional Tricuspid Regurgitation Caused by Chronic Atrial Fibrillation. Circ. Cardiovasc. Imaging 2017, 10, e004897. [Google Scholar] [CrossRef]
- Mutlak, D.; Lessick, J.; Reisner, S.A.; Aronson, D.; Dabbah, S.; Agmon, Y. Echocardiography-based Spectrum of Severe Tricuspid Regurgitation: The Frequency of Apparently Idiopathic Tricuspid Regurgitation. J. Am. Soc. Echocardiogr. 2007, 20, 405–408. [Google Scholar] [CrossRef] [PubMed]
- Chorin, E.; Rozenbaum, Z.; Topilsky, Y.; Konigstein, M.; Ziv-Baran, T.; Richert, E.; Keren, G.; Banai, S. Tricuspid regurgitation and long-term clinical outcomes. Eur. Heart J. Cardiovasc. Imaging 2019, 21, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Nickenig, G.; Kowalski, M.; Hausleiter, J.; Braun, D.; Schofer, J.; Yzeiraj, E.; Rudolph, V.; Friedrichs, K.; Maisano, F.; Taramasso, M.; et al. Transcatheter Treatment of Severe Tricuspid Regurgitation with the Edge-to-Edge MitraClip Technique. Circulation 2017, 135, 1802–1814. [Google Scholar] [CrossRef] [PubMed]
- Orban, M.; Besler, C.; Braun, D.; Nabauer, M.; Zimmer, M.; Orban, M.; Noack, T.; Mehilli, J.; Hagl, C.; Seeburger, J.; et al. Six-month outcome after transcatheter edge-to-edge repair of severe tricuspid regurgitation in patients with heart failure. Eur. J. Heart Fail. 2018, 20, 1055–1062. [Google Scholar] [CrossRef]
- Braun, D.; Rommel, K.-P.; Orban, M.; Karam, N.; Brinkmann, I.; Besler, C.; Massberg, S.; Nabauer, M.; Lurz, P.; Hausleiter, J. Acute and Short-Term Results of Transcatheter Edge-to-Edge Repair for Severe Tricuspid Regurgitation Using the MitraClip XTR System. JACC Cardiovasc. Interv. 2019, 12, 604–605. [Google Scholar] [CrossRef]
- Mehr, M.; Taramasso, M.; Besler, C.; Ruf, T.; Connelly, K.A.; Weber, M.; Yzeiraj, E.; Schiavi, D.; Mangieri, A.; Vaskelyte, L.; et al. 1-Year Outcomes After Edge-to-Edge Valve Repair for Symptomatic Tricuspid Regurgitation. JACC Cardiovasc. Interv. 2019, 12, 1451–1461. [Google Scholar] [CrossRef]
- Lurz, P.; von Bardeleben, R.S.; Weber, M.; Sitges, M.; Sorajja, P.; Hausleiter, J.; Denti, P.; Trochu, J.-N.; Nabauer, M.; Tang, G.H.; et al. Transcatheter Edge-to-Edge Repair for Treatment of Tricuspid Regurgitation. J. Am. Coll. Cardiol. 2021, 77, 229–239. [Google Scholar] [CrossRef]
- Lurz, P. Real-World Outcomes for Tricuspid Edge-to-Edge Repair: Initial 30-Day Results from the TriClipTM bRIGHT Study; EuroPCR: Paris, France, 2022. [Google Scholar]
- Lurz, P. Real-World Outcomes for Tricuspid Edge-to-Edge Repair: Initial 1 Year Outcomes from the bRIGHT Trial; PCR: London, UK, 2022. [Google Scholar]
- Adams, D. First Report of Outcomes in the TRILUMINATE Pivotal Clinical Trial in Patient with Severe Tricuspid Regurgitation; TCT: Boston, MA, USA, 2022. [Google Scholar]
- Sorajja, P.; Whisenant, B.; Hamid, N.; Naik, H.; Makkar, R.; Tadros, P.; Price, M.J.; Singh, G.; Fam, N.; Kar, S.; et al. Transcatheter Repair for Patients with Tricuspid Regurgitation. N. Engl. J. Med. 2023, 388, 1833–1842. [Google Scholar] [CrossRef]
- Fam, N.P.; Braun, D.; von Bardeleben, R.S.; Nabauer, M.; Ruf, T.; Connelly, K.A.; Ho, E.; Thiele, H.; Lurz, P.; Weber, M.; et al. Compassionate Use of the PASCAL Transcatheter Valve Repair System for Severe Tricuspid Regurgitation. JACC Cardiovasc. Interv. 2019, 12, 2488–2495. [Google Scholar] [CrossRef]
- Kitamura, M.; Fam, N.P.; Braun, D.; Ruf, T.; Sugiura, A.; Narang, A.; Connelly, K.A.; Ho, E.; Nabauer, M.; Hausleiter, J.; et al. 12-Month outcomes of transcatheter tricuspid valve repair with the PASCAL system for severe tricuspid regurgitation. Catheter. Cardiovasc. Interv. 2021, 97, 1281–1289. [Google Scholar] [CrossRef]
- Kodali, S.; Hahn, R.T.; Eleid, M.F.; Kipperman, R.; Smith, R.; Lim, D.S.; Gray, W.A.; Narang, A.; Pislaru, S.V.; Koulogiannis, K.; et al. Feasibility Study of the Transcatheter Valve Repair System for Severe Tricuspid Regurgitation. J. Am. Coll. Cardiol. 2021, 77, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Baldus, S. 30-Day Outcomes for Transcatheter Tricuspid Repair: TriCLASP Postmarket Study; EuroPCR: Paris, France, 2022. [Google Scholar]
- Schofer, N. Transcatheter Repair of Tricuspid Regurgitation: TriCLASP Study Six-Month Follow-Up; PCR: London, UK, 2022. [Google Scholar]
- Davidson, C. The CLASP II TR Trial: First 30-Day Procedural and Clinical Outcomes Report from the Roll-in Cohort; TCT: Boston, MA, USA, 2022. [Google Scholar]
- Hahn, R. Transcatheter Tricuspid Valve Repair: CLASP TR Study One-Year Results; EuroPCR: Paris, France, 2022. [Google Scholar]
- Nickenig, G.; Weber, M.; Schueler, R.; Hausleiter, J.; Näbauer, M.; von Bardeleben, R.S.; Sotiriou, E.; Schäfer, U.; Deuschl, F.; Kuck, K.-H.; et al. 6-Month Outcomes of Tricuspid Valve Reconstruction for Patients with Severe Tricuspid Regurgitation. J. Am. Coll. Cardiol. 2019, 73, 1905–1915. [Google Scholar] [CrossRef] [PubMed]
- Nickenig, G.; Weber, M.; Schüler, R.; Hausleiter, J.; Nabauer, M.; von Bardeleben, R.S.; Sotiriou, E.; Schäfer, U.; Deuschl, F.; Alessandrini, H.; et al. Tricuspid valve repair with the Cardioband system: Two-year outcomes of the multicentre, prospective TRI-REPAIR study. Eurointervention 2021, 16, e1264–e1271. [Google Scholar] [CrossRef] [PubMed]
- Nickenig, G.; Friedrichs, K.P.; Baldus, S.; Arnold, M.; Seidler, T.; Hakmi, S.; Linke, A.; Schäfer, U.; Dreger, H.; Reinthaler, M.; et al. Thirty-day outcomes of the Cardioband tricuspid system for patients with symptomatic functional tricuspid regurgitation: The TriBAND study. Eurointervention 2021, 17, 809–817. [Google Scholar] [CrossRef]
- Rudolph, V. Transcatheter Tricuspid Annular Reduction: The TriBAND Study One-Year Outcomes; PCR: London, UK, 2022. [Google Scholar]
- Davidson, C.J.; Lim, D.S.; Smith, R.L.; Kodali, S.K.; Kipperman, R.M.; Eleid, M.F.; Reisman, M.; Whisenant, B.; Puthumana, J.; Abramson, S.; et al. Early Feasibility Study of Cardioband Tricuspid System for Functional Tricuspid Regurgitation. JACC Cardiovasc. Interv. 2021, 14, 41–50. [Google Scholar] [CrossRef]
- Gray, W.A.; Abramson, S.V.; Lim, S.; Fowler, D.; Smith, R.L.; Grayburn, P.A.; Kodali, S.K.; Hahn, R.T.; Kipperman, R.M.; Koulogiannis, K.P.; et al. 1-Year Outcomes of Cardioband Tricuspid Valve Reconstruction System Early Feasibility Study. JACC Cardiovasc. Interv. 2022, 15, 1921–1932. [Google Scholar] [CrossRef]
- Navia, J.L.; Kapadia, S.; Elgharably, H.; Harb, S.C.; Krishnaswamy, A.; Unai, S.; Mick, S.; Rodriguez, L.; Hammer, D.; Gillinov, A.M.; et al. First-in-Human Implantations of the NaviGate Bioprosthesis in a Severely Dilated Tricuspid Annulus and in a Failed Tricuspid Annuloplasty Ring. Circ. Cardiovasc. Interv. 2017, 10, e005840. [Google Scholar] [CrossRef]
- Hahn, R.T.; George, I.; Kodali, S.K.; Nazif, T.; Khalique, O.K.; Akkoc, D.; Kantor, A.; Vahl, T.P.; Patel, A.; Elias, E.; et al. Early Single-Site Experience with Transcatheter Tricuspid Valve Replacement. JACC Cardiovasc. Imaging 2019, 12, 416–429. [Google Scholar] [CrossRef]
- Hahn, R.T.; Kodali, S.; Fam, N.; Bapat, V.; Bartus, K.; Rodés-Cabau, J.; Dagenais, F.; Estevez-Loureiro, R.; Forteza, A.; Kapadia, S.; et al. Early Multinational Experience of Transcatheter Tricuspid Valve Replacement for Treating Severe Tricuspid Regurgitation. JACC Cardiovasc. Interv. 2020, 13, 2482–2493. [Google Scholar] [CrossRef]
- Lu, F.-L.; Ma, Y.; An, Z.; Cai, C.-L.; Li, B.-L.; Song, Z.-G.; Han, L.; Wang, J.; Qiao, F.; Xu, Z.-Y. First-in-Man Experience of Transcatheter Tricuspid Valve Replacement with LuX-Valve in High-Risk Tricuspid Regurgitation Patients. JACC Cardiovasc. Interv. 2020, 13, 1614–1616. [Google Scholar] [CrossRef]
- Sun, Z.; Li, H.; Zhang, Z.; Li, Y.; Zhang, L.; Xie, Y.; Han, Z.; Wang, J.; Chen, Y.; Yang, Y.; et al. Twelve-month outcomes of the LuX-Valve for transcatheter treatment of severe tricuspid regurgitation. Eurointervention 2021, 17, 818–826. [Google Scholar] [CrossRef] [PubMed]
- Modine, T. Transcatheter Tricuspid Valve Replacement with the LuX- Valve System 1-Year Results of a Multicenter, TTVR Experience; PCR: London, UK, 2022. [Google Scholar]
- Fam, N.P.; von Bardeleben, R.S.; Hensey, M.; Kodali, S.K.; Smith, R.L.; Hausleiter, J.; Ong, G.; Boone, R.; Ruf, T.; George, I.; et al. Transfemoral Transcatheter Tricuspid Valve Replacement with the EVOQUE System. JACC Cardiovasc. Interv. 2021, 14, 501–511. [Google Scholar] [CrossRef] [PubMed]
- Webb, J.G.; Chuang, A.-Y.; Meier, D.; von Bardeleben, R.S.; Kodali, S.K.; Smith, R.L.; Hausleiter, J.; Ong, G.; Boone, R.; Ruf, T.; et al. Transcatheter Tricuspid Valve Replacement with the EVOQUE System. JACC Cardiovasc. Interv. 2022, 15, 481–491. [Google Scholar] [CrossRef]
- Kodali, S.; Hahn, R.T.; George, I.; Davidson, C.J.; Narang, A.; Zahr, F.; Chadderdon, S.; Smith, R.; Grayburn, P.A.; O’neill, W.W.; et al. Transfemoral Tricuspid Valve Replacement in Patients with Tricuspid Regurgitation. JACC Cardiovasc. Interv. 2022, 15, 471–480. [Google Scholar] [CrossRef] [PubMed]
- Windecker, S. TRISCEND Study One-Year Outcomes: Transfemoral Transcatheter Tricuspid Valve Replacement; PCR: London, UK, 2022. [Google Scholar]
- Zhang, Y.; Lu, F.; Li, W.; Chen, S.; Li, M.; Zhang, X.; Pan, C.; Qiao, F.; Zhou, D.; Pan, W.; et al. A first-in-human study of transjugular transcatheter tricuspid valve replacement with the LuX-Valve Plus system. Eurointervention 2023, 18, e1088–e1089. [Google Scholar] [CrossRef] [PubMed]
- Dreger, H.; Mattig, I.; Hewing, B.; Knebel, F.; Lauten, A.; Lembcke, A.; Thoenes, M.; Roehle, R.; Stangl, V.; Landmesser, U.; et al. Treatment of Severe TRIcuspid Regurgitation in Patients with Advanced Heart Failure with CAval Vein Implantation of the Edwards Sapien XT VALve (TRICAVAL): A randomised controlled trial. Eurointervention 2020, 15, 1506–1513. [Google Scholar] [CrossRef]
- Lauten, A.; Figulla, H.R.; Unbehaun, A.; Fam, N.; Schofer, J.; Doenst, T.; Hausleiter, J.; Franz, M.; Jung, C.; Dreger, H.; et al. Interventional Treatment of Severe Tricuspid Regurgitation. Circ. Cardiovasc. Interv. 2018, 11, e006061. [Google Scholar] [CrossRef]
- Estévez-Loureiro, R.; Sánchez-Recalde, A.; Amat-Santos, I.J.; Cruz-González, I.; Baz, J.A.; Pascual, I.; Mascherbauer, J.; Altisent, O.A.-J.; Nombela-Franco, L.; Pan, M.; et al. 6-Month Outcomes of the TricValve System in Patients with Tricuspid Regurgitation. JACC Cardiovasc. Interv. 2022, 15, 1366–1377. [Google Scholar] [CrossRef]
- Wild, M.G.; Lubos, E.; Cruz-Gonzalez, I.; Amat-Santos, I.; Ancona, M.; Andreas, M.; Boeder, N.F.; Butter, C.; Carrasco-Chinchilla, F.; Estevez-Loureiro, R.; et al. Early Clinical Experience with the TRICENTO Bicaval Valved Stent for Treatment of Symptomatic Severe Tricuspid Regurgitation: A Multicenter Registry. Circ. Cardiovasc. Interv. 2022, 15, 011302. [Google Scholar] [CrossRef]
- O’Neill, B.P.; Wheatley, G.; Bashir, R.; Edmundowicz, D.; O’Murchu, B.; O’Neill, W.W.; Patil, P.; Chen, A.; Forfia, P.; Cohen, H.A. Study design and rationale of the heterotopic implantation of the Edwards-Sapien XT transcatheter valve in the inferior VEna cava for the treatment of severe tricuspid regurgitation (HOVER) trial. Catheter. Cardiovasc. Interv. 2016, 88, 287–293. [Google Scholar] [CrossRef]
- Cruz-González, I.; González-Ferreiro, R.; Amat-Santos, I.J.; Carrasco-Chinchilla, F.; Briales, J.H.A.; Estévez-Loureiro, R. TRICENTO transcatheter heart valve for severe tricuspid regurgitation. Initial experience and mid-term follow-up. Rev. Española Cardiol. 2020, 74, 351–354. [Google Scholar] [CrossRef]
- Toggweiler, S.; De Boeck, B.; Brinkert, M.; Buhmann, R.; Bossard, M.; Kobza, R.; Cuculi, F. First-in-man implantation of the Tricento transcatheter heart valve for the treatment of severe tricuspid regurgitation. Eurointervention 2018, 14, 758–761. [Google Scholar] [CrossRef] [PubMed]
- Alperi, A.; Avanzas, P.; Almendárez, M.; León, V.; Hernández-Vaquero, D.; Silva, I.; del Valle, D.F.; Fernández, F.; Díaz, R.; Rodes-Cabau, J.; et al. Early and mid-term outcomes of transcatheter tricuspid valve repair: Systematic review and meta-analysis of observational studies. Rev. Española Cardiol. 2022, 76, 322–332. [Google Scholar] [CrossRef]
- Praz, F.; Muraru, D.; Kreidel, F.; Lurz, P.; Hahn, R.T.; Delgado, V.; Senni, M.; von Bardeleben, R.S.; Nickenig, G.; Hausleiter, J.; et al. Transcatheter treatment for tricuspid valve disease. Eurointervention 2021, 17, 791–808. [Google Scholar] [CrossRef] [PubMed]
- Besler, C.; Orban, M.; Rommel, K.-P.; Braun, D.; Patel, M.; Hagl, C.; Borger, M.; Nabauer, M.; Massberg, S.; Thiele, H.; et al. Predictors of Procedural and Clinical Outcomes in Patients with Symptomatic Tricuspid Regurgitation Undergoing Transcatheter Edge-to-Edge Repair. JACC Cardiovasc. Interv. 2018, 11, 1119–1128. [Google Scholar] [CrossRef]
- Dreyfus, J.; Audureau, E.; Bohbot, Y.; Coisne, A.; Lavie-Badie, Y.; Bouchery, M.; Flagiello, M.; Bazire, B.; Eggenspieler, F.; Viau, F.; et al. TRI-SCORE: A new risk score for in-hospital mortality prediction after isolated tricuspid valve surgery. Eur. Heart J. 2021, 43, 654–662. [Google Scholar] [CrossRef]
| Author | Device | Participants (Age) | Follow-Up Time | Outcomes | |||
|---|---|---|---|---|---|---|---|
| TR Reduction | NYHA Class | 6MWT/KCCQ Score | Safety Endpoints | ||||
| Nickenig et al. [33] | MitraClip | 64 (76.6) | 30 days | A total of 91% of patients had at least 1 TR grade reduction, and 13% of patients remained in severe/massive TR; however, there was a significant decrease compared to baseline (88%) (p = 0.01). | No patients were NYHA IV; however, 63% remained NYHA III. | A 6 min walking test was significantly improved after the procedure (16.1 m increase; p = 0.007). | The device was implanted successfully in 97% of patients. There were no intraprocedural deaths. In-hospital mortality rate was 5%. |
| Orban et al. [34] | MitraClip | 50 (77) | 6 months | A total of 90% of patients had a reduction of at least 1 TR grade and 77% had a TR grade lower than 2. | NYHA class was improved by at least 1 class in 79% of patients. | A 6MWT distance was found to be increased by 44% (84 m, p = 0.056) and KCCQ score was improved by 21 points (p < 0.0001). | The event free survival rate was 78%. There was a total of 28% of patients hospitalized for worsening heart failure during the follow-up period. |
| Braun et al. [35] | MitraClip | 31 (77) | 30 days | A total of 69% of patients had a TR grade lower or equal to 2. | A total of 69% of patients were NYHA class I/II (p < 0.001). | Not mentioned. | A total of 1 patient died due to insufficient TR reduction. |
| Mehr et al. (TriValve registry) [36] | TriClip | 249 (77) | 1 year | TR reduction was sustained in 84% of patients, and 72% of patients had a TR grade lower or equal to 2 at the time of the follow-up. | A total of 69% of patients were NYHA I/II at the follow-up (p < 0.001). | Not mentioned. | Implantations success rate was 96%. The combined endpoint of death or unplanned hospitalization for heart failure occurred in 31% of patients. One year mortality rate was 20.3%. |
| Lurz et al. (TRILUMINATE) [37] | TriClip | 85 (77.8) | 1 year | At 1 year, 87% of subjects had a sustained TR reduction of at least 1 TR severity grade, and 70% of subjects had moderate or less TR at the time of the follow-up. | A total of 83% of patients were NYHA I/II at 1 year. | A 6MWT distance increased from by 31 m at 1 year. | Hospitalization rate decreased from 1.30 to 0.78 events/patient–year. |
| Lurz et al. (bRIGHT study) [38] | TriClip | 300 (78.5) | 30 days | A total of 71% of patients had moderate or less TR (p < 0.0001). | A total of 78% of patients were NYHA class I/II (p < 0.0001). | There was a significant improvement in KCCQ score by 18 points (p < 0.0001). | Implantation success was 98%. Major adverse event rate was 1%. |
| Lurz et al. (bRIGHT study) [39] | TriClip | 200 (78) | 1 year | A total of 86% of patients had moderate or less TR at 1 year follow-up. | A total of 77% of patients were NYHA class I/II. | KCCQ score was significantly improved by 21 points (p < 0.0001). | The major adverse event rate was 11.5%. All-cause mortality was 11.0%. There was a 44% reduction in heart failure hospitalizations during the follow-up, compared to the year before the intervention. |
| Adams et al. (TRILUMINATE-Pivotal study) [40] | TriClip | 97 (79) | 30 days | A total of 74% of patients had less than moderate TR, and 67% of patients had a reduction in TR class of at least 2 grades. | A total of 76% of patients were NYHA I/II. | KCCQ score was significantly improved by 16.64 points. | The implantation success was 99%. Mortality rate was 1% 7.2% had a major bleeding during the follow-up. |
| Sorajja et al. (TRILUMINATE-Pivotal 1 year follow-up) [41] | TriClip | 350, 175 in each arm (TriClip vs. medical therapy) (78) | 30 days 1 year | TEER arm: 87.0% of the TR of no greater than moderate at 30 days. Medical therapy arm: 4.8% of the TR of no greater than moderate at 30 days. | TEER arm: 83.9% of patients were NYHA I/II at 1 year follow-up. Medical therapy arm: 59.5% of patients were NYHA I/II at 1 year follow-up. | TEER arm: KCCQ score was improved by a mean of 12.3 ± 1.8 points. Medical therapy arm: KCCQ score was improved by a mean of 0.6 ± 1.8 point. | A total of 98.3% of the patients who underwent the procedure were free from major adverse events at the 30 day follow-up. |
| Fam et al. [42] | PASCAL | 28 (78) | 30 days | A total of 85% of patients had a TR grade lower or equal to 2. | A total of 88% of patients were NYHA class I/II at the follow-up. | A 6MWT distance was increased by 95 m (p < 0.001). | Mortality rate was 7.1%. |
| Kitamura et al. [43] | PASCAL | 30 (77) | 1 year | TR reduction of at least 1 grade was sustained in 89% of patients at 1 year, and 82% and 86% of patients had moderate or less TR at the 30 day and 1 year, respectively. | A total of 90% of patients were NYHA class I/II. | A 6MWT distance was increased by72 m at 1 year (p < 0.01). | A 1 year survival rate was 93%. A total of 20% of patients required a rehospitalization due to acute heart failure during the 1 year follow-up period. Cardiovascular mortality rate was 6.7%. |
| Kodali et al. [44] | PASCAL | 34 (76) | 30 days | A total of 85% of patients had a TR severity reduction of at least 1 grade at 30 days, and 52% had moderate or less TR severity (p < 0.001). | A total of 89% of the patients followed up were NYHA class I/II (p < 0.001). | A 6MWT distance was improved by 71 m (p < 0.001) and KCCQ score improved by 15 points (p < 0.001). | The major adverse events rate was 5.9%. |
| Baldus et al. (TriClasp study) [45] | PASCAL | 74(with 72 undergoing the procedure) (80) | 30 days | A total of 88% of patients achieved at least 1 TR grade reduction, and 90% had moderate or lower TR severity. | A total of 56% of patients were NYHA class I/II. | A 6MWT distance was significantly improved by 38 m (p < 0.001) and KCCQ scire was significantly improved by 13 points (p < 0.001). | Successful implantation rate was 97%. All-cause mortality rate was 2.9%. Composite major adverse event rate was 3.0%. Cardiovascular mortality rate was 1.5%. Heart failure rehospitalization rate was 4.5%. |
| Schofer et al. (TriClasp study) [46] | Pascal | 177 (80) | 6 months | A total of 88% of patients had moderate or lower TR, and 83% of patients achieved equal or greater than 1 TR grade reduction at 6 months. | A total of 61% of patients were NYHA class I/II. | A 6MWT distance was improved by 32 m (p = 0.01) and KCCQ score was improved by 9 points (p < 0.001). | Implantation success was 99%. The composite major adverse events rate was 4%. All-cause mortality rate was 5.1%. Cardiovascular mortality rate was 2.3%. The rate of heart failure hospitalization was 7.9% at 6 months. |
| Davidson et al. (CLASP II TR roll in) [47] | PASCAL | 73 (79.8) | 30 days | A total of 83.0% of patients improved by 1 or more TR grade, 62.3% improved by 2 or more grades, and 73.6% of patients had moderate or less TR severity. | A total of 86% of patients were NYHA class I/II. | KCCQ score was significantly improved by 17.9 points (p < 0.001). | The rate of successful implantation was 84.4%. The composite major adverse events rate was 8.7%. Cardiovascular mortality rate was 0%. All-cause mortality and heart failure hospitalization rate were both 0%. |
| Hahn et al. (CLASP TR) [48] | PASCAL | 65 (46 had 1 year follow-up) (77) | 1 year | A total of 100% of patients improved by at least 1 TR grade, while 75% improved by at least 2 TR grades, and 86% of patients had moderate or less TR severity at 1 year. | A total of 92% of patients were NYHA class I/II. | A 6MWT distance was significantly increased by 94 m (p < 0.014). KCCQ score was significantly improved by 18 points (p < 0.001). | The implantation success rate was 91%. The composite major adverse events rate was 16.9%. All-cause mortality rate was 10.8%. Cardiovascular mortality rate was 7.7%. Heart failure rehospitalization rate was 18.5%. |
| Author | Device | Participants (Age) | Follow-Up Time | Outcomes | |||
|---|---|---|---|---|---|---|---|
| Annulus Reduction TR Reduction | NYHA Class | 6 MWT Distance/KCCQ Score | Safety Endpoints | ||||
| Nickenig et al. (TRI-REPAIR study) [49] | Cardioband | 30 (75) | 30 days 6 months | Significant reduction in the annulus at 30 days (37.8 ± 3.3 mm; p = 0.0004) at 6 months (37.8 ± 3.4 mm; and p = 0.0014) from baseline (41.9 ± 4.6 mm). A total of 76% at 30 days and 73% at 6 months had less than moderate TR. | A total of 82% at 30 days and 88% at 6 months were NYHA class I/II. | KCCW score was significantly improved by 12 at 30 days and 24 points at 6 months. The 6MWT distance was significantly improved by 31 m at 30 days and 60 m at 6 months. | The implantation was 100% successful. All-cause morality at 6 months was 10%. |
| Nickenig et al. (TRI-REPAIR study) [50] | Cardioband | 30 (75) | 2 years | Significant reduction in the annulus sustained at 2 years follow-up (35.2 ± 4.6 mm, p < 0.001) from baseline (41.9 ± 4.6 mm). A total of 72% at 2 years had less than moderate TR. | A total of 82% were NYHA class I/II. | KCCW score was significantly improved by 18 points at 2 years. The 6MWT distance was significantly improved by 63 m at 2 years. | The two-year survival rate was 73%. The two-year freedom from heart failure hospitalization rate was 55%. At two years, there were eight deaths. Two patients underwent device-related secondary procedures. |
| Nickenig et al. (TriBand study) [51] | Cardioband | 61 (78.6) | 30 days | A total of 69% (p < 0.001) of patients achieved less than moderate TR, and 85% of patients had at least 1 TR grade reduction. Annular diameter was reduced by 20%. | A total of 74% were in NYHA class I-II (p < 0.001). | KCCQ score was significantly improved by 17 points (p < 0.001). |
Device success rate was 96.7%. All-cause mortality rate was 1.6%. The composite major adverse event rate was 19.7%. Cardiovascular mortality was 0%. |
| Rudolph et al. (TriBand study) [52] | Cardioband | 139 (79) (62 available at follow-up) | 1 year | The annulus diameter was decreased by 22%, 86% of patients achieved greater or equal to 1 TR grade reduction, 67% had greater or equal to a 2 TR grade reduction, and 77.5% of patients had moderate or less TR severity (p < 0.001). | A total of 61.1% of patients were NYHA class I/II (p < 0.001). | KCCQ score was significantly improved by greater than 20 points in 32% and 10–19 points in 18% (p < 0.001). | Device success was 93%. The composite major adverse event rate was 20.9%. Cardiovascular mortality was 2.9%. Survival rate was 92%. Freedom from HF hospitalization was 84%. |
| Davidson et al. (Cardioband TR EFS) [53] | Cardioband | 30 (77) | 30 days | The annulus diameter was decreased by 5.7 mm (p < 0.001). A total of 85% of patients had at least 1 TR grade reduction, 56% of patients had at least 2 TR grade reduction, and 44% of patients had moderate or less TR severity. | A total of 75% of patients were NYHA class I/II (p < 0.001). |
KCCQ score improved by 16 points (p < 0.001). The 6MWT distance was not significantly different from baseline. | The device was successfully implanted in 93.3% of patients. Cardiovascular and estimated all-cause mortality were 0%. |
| Gray et al. (Cardioband TR EFS) [54] | Cardioband | 37 (78) | 1 year | Annular diameter was significantly decreased by 10.5 mm (p < 0.0001), 73.0% of patients had less than moderate TR severity(p < 0.0001), and 73.1% of patients had at least a reduction of 2 TR grades. | A total of 92.3% of patients were NYHA class I/II. | KCCQ score was significantly increased by 19.0 points (p< 0.0001). | Cardiovascular mortality rate was 8.1%. One year survival rate was 85.9%. One year freedom from heart failure rehospitalization rate was 88.7%. |
| Author | Device | Participants (Age) | Follow-Up Time | Outcomes | |||
|---|---|---|---|---|---|---|---|
| TR Reduction | NYHA Class | 6MWT Distance/KCCQ Score | Safety Endpoints | ||||
| Navia et al. [55] | GATE | 2 (71) | 3–6 months | Both patients had mild paravalvular leak. | Not mentioned. | Not mentioned. | Not mentioned. |
| Hahn et al. [56] | GATE | 5 (84,4) (follow-up for 4/5 patients) | 3–6 months | In three patients, trace to mild TR was noticed after the procedure, while in one patient, it was mild to moderate. Mild paravalvular leaks did not change in the course of the follow-up. | Not mentioned. | Not mentioned. | Implantation success was 100%. There was one death post operatively (day 28). |
| Hahn et al. [57] | GATE | 30 (75) | 30 days |
A total of 95% of patients had at least 1 TR grade reduction, and 81% of patients had at a least 2 TR grade reduction in TR severity at 30 days. A total of 74% of patients had mild or less TR at follow-up (p < 0.001). | A total of 77% were NUHA class I/II (p < 0.005). | Not mentioned. | Implantation success was 87%. A total of 5% of procedures turned into open heart surgery due to device malposition. In-hospital mortality rate was 10%. |
| Lu et al. [58] | Lux Valve | 12 (69) | 30 days | A total of 90.9% of patients had no to mild TR at follow-up. | A total of 54.5% were NYHA class II; (p < 0.05). | The 6MWT distance was improved by 99.5 m. | Procedural success was 100%. There was a total of one cardiovascular-related death during the follow-up period. |
| Sun et al. [59] | Lux Valve | 6 (56) | 12 months | There was moderate paravalvular regurgitation in one patient, mild paravalvular regurgitation in three patients, and no paravalvular regurgitation in two patients. There was no change in paravalvular leak severity at 1 year. | All alive patients (5/6) were NYHA class I/II at 1 year. | Not mentioned. | Implantation success 100%. There was 0% intraprocedural mortality at 30 days follow-up, And one patient died at 3 months due to right ventricular failure. |
| Modine et al. [60] | Lux Valve | 31 (67.8) | 1 year | All patients had no TR at 30 days follow-up, and 92.9% of patients had mild or no TR at 1 year follow-up. | A total of 82.8% of patients were NYHA class I/II. | Not mentioned. | All-cause mortality rate was 3.23% at follow-up. Survival rate was 96.8% at 1 year. |
| Fam et al. [61] | Evoque | 25 (76) | 30 days | TR grade was less or equal to 2 in 96% of patients at 30 days follow-up. | A total of 76% of patients were NYHA class I/II. | Not mentioned. |
Implantation success rate was 92%. There was a 0% mortality rate at 30 days follow-up. There was a 0% intraprocedural mortality or conversion to open surgery. |
| Webb et al. [62] | Evoque | 27 (77) | 1 year | A total of 96% of patients had a TR grade lower or equal to 2, and 87% of patients had a TR grade lower or equal to 1. | A total of 70% of patients were NYHA class I/II. | Not mentioned. | Mortality rate was 7%. Two patients required hospitalization for heart failure. |
| Kodali et al. (TRISCEND study) [63] | Evoque | 56 (79.3) | 30 days | A total of 98.1% of patients had mild or no/trace TR severity (p < 0.001). | A total of 78.8% of patients were NYHA class I/II (p < 0.001). | The 6MWT distance was increased by 48.2 m (0.001). KCCQ score was improved by 19.0 points (p < 0.001). | The composite major adverse events rate was 26.8%. |
| Windecker et al. (TRISCEND study) [64] | Evoque | 176 (78.7) | A total of 97.6% of patients had lower than mild TR severity at 1 year, and 69% of patients had non/trace TR. | A total of 93% of patients were NYHA class I/II. | The 6MWT distance was increased by 25.7 m (p < 0.001). KCCQ score was improved by 25.7 points (p < 0.001) 55%of patients had more or equal to a 20-point improvement in the KCCQ score, and 22% of patients had 10–19 points of improvement in KCCQ. | The composite major adverse events rate at 1 year was 30.2%. Survival rate was 90%. Freedom from heart failure hospitalization rate was 88%. | |
| Author | Device | Participants (Age) | Follow-Up Time | Outcomes | ||
|---|---|---|---|---|---|---|
| NYHA Class | 6MWT Distance/KCCQ Score | Safety Endpoints | ||||
| Dreger et al. [66] | Sapien | 28 (14 intervention vs. 14 medical therapy) (77) | 1 year | The trial was stopped due to safety concerns (valve dislocations) at 3 months. However, a significant (p = 0.025) improvement in NYHA class was reported. | ||
| Lauten et al. (TRICUS) [67] | TricValve and others | 25 (73.9) (TtricValve = 6) | 1 year | A total of 52.7% were NYHA class I/II. | Not mentioned. |
The 30-day mortality was 8%. In-hospital mortality was 16%. |
| Estévez-Loureiro (TRICUS EURO study) [68] | TricValve | 35 (76) | 30 days and 6 months | A total of 79.4% of patients were NYHA class I/II at 6 months (p = 0.0006). | KCCQ score was improved by 17.7 points at 6 months (p = 0.004). | All-cause mortality rate was 8.5%. Heart failure hospitalization rate was 20%. |
| Wild et al. [69] | Tricento | 21 (76) | 1 year | A total of 65% of patients were NYHA class I/II. | Not mentioned. | Technical success was 100%. In-hospital mortality was 0%. The 1-year survival rate was 76%. Heart failure rehospitalization rate was 19% at 1 year. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dimitriadis, K.; Pyrpyris, N.; Aznaouridis, K.; Iliakis, P.; Valatsou, A.; Tsioufis, P.; Beneki, E.; Mantzouranis, E.; Aggeli, K.; Tsiamis, E.; et al. Transcatheter Tricuspid Valve Interventions: A Triumph for Transcatheter Procedures? Life 2023, 13, 1417. https://doi.org/10.3390/life13061417
Dimitriadis K, Pyrpyris N, Aznaouridis K, Iliakis P, Valatsou A, Tsioufis P, Beneki E, Mantzouranis E, Aggeli K, Tsiamis E, et al. Transcatheter Tricuspid Valve Interventions: A Triumph for Transcatheter Procedures? Life. 2023; 13(6):1417. https://doi.org/10.3390/life13061417
Chicago/Turabian StyleDimitriadis, Kyriakos, Nikolaos Pyrpyris, Konstantinos Aznaouridis, Panagiotis Iliakis, Aggeliki Valatsou, Panagiotis Tsioufis, Eirini Beneki, Emmanouil Mantzouranis, Konstantina Aggeli, Eleftherios Tsiamis, and et al. 2023. "Transcatheter Tricuspid Valve Interventions: A Triumph for Transcatheter Procedures?" Life 13, no. 6: 1417. https://doi.org/10.3390/life13061417
APA StyleDimitriadis, K., Pyrpyris, N., Aznaouridis, K., Iliakis, P., Valatsou, A., Tsioufis, P., Beneki, E., Mantzouranis, E., Aggeli, K., Tsiamis, E., & Tsioufis, K. (2023). Transcatheter Tricuspid Valve Interventions: A Triumph for Transcatheter Procedures? Life, 13(6), 1417. https://doi.org/10.3390/life13061417









