Comparative Susceptibility of Pathogenic Methicillin-Resistant and Methicillin-Susceptible Staphylococcus pseudintermedius to Empirical Co-Trimoxazole for Canine Pyoderma
Abstract
1. Introduction
2. Materials and Methods
2.1. Studied Specimen and Ethical Approval
2.2. Primary Identification of Coagulase-Positive Staphylococci
2.3. Antimicrobial Susceptibility Testing
2.4. Confirmation of Staphylococcus pseudintermedius
2.5. Determination of Minimum Inhibitory Concentration Values
2.6. Target Attainment of Pharmacokinetic and Pharmacodynamics
2.7. Statistical Analysis
3. Results
3.1. Cotrimazole Susceptibility among Coagulase-Positive Staphylococci
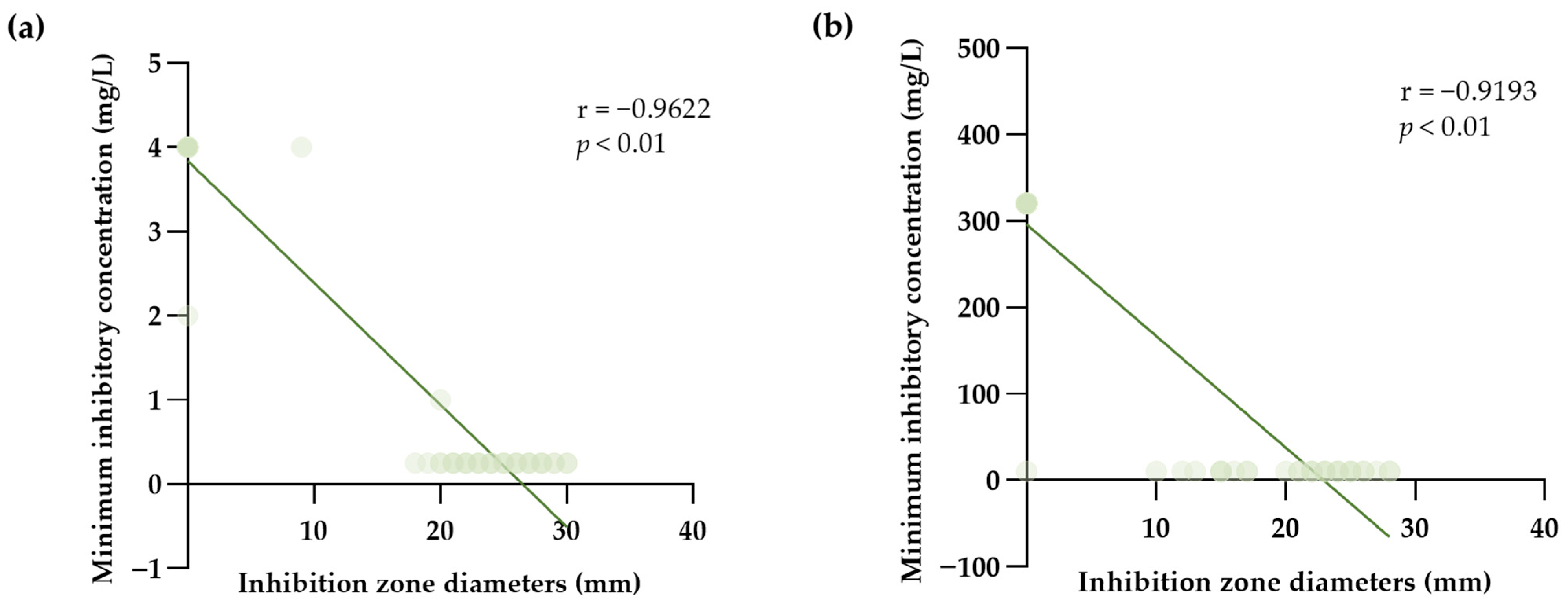
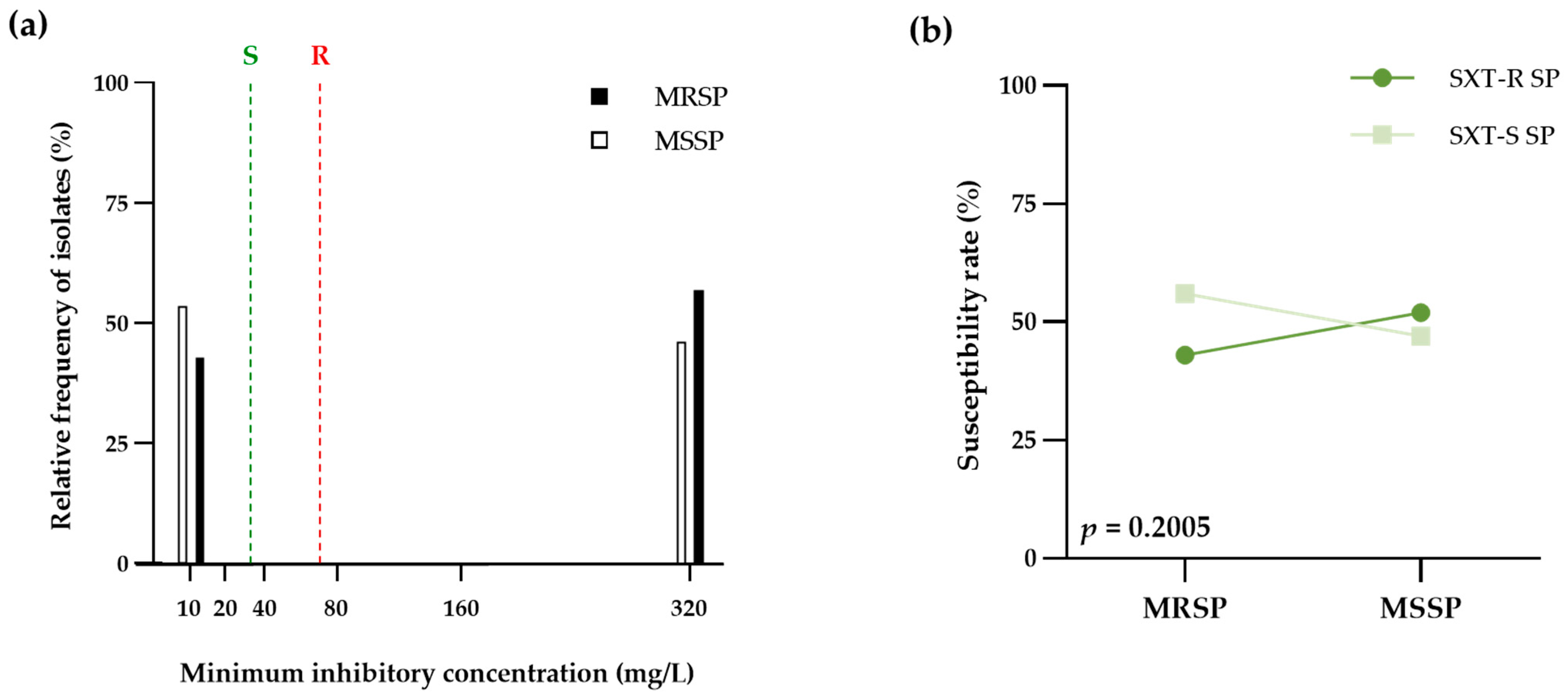
3.2. Cotrimazole Susceptibility among Pathogenic S. pseudintermedius
3.3. PK-PD Target Achieving of Cotrimazole on Pathogenic S. pseudintermedius
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Gortel, K. Recognizing pyoderma: More difficult than it may seem. Vet. Clin. North Am. Small Anim. Pract. 2013, 43, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Nocera, F.P.; Ambrosio, M.; Fiorito, F.; Cortese, L.; De Martino, L. On Gram-Positive- and Gram-Negative-Bacteria-Associated Canine and Feline Skin Infections: A 4-Year Retrospective Study of the University Veterinary Microbiology Diagnostic Laboratory of Naples, Italy. Animals 2021, 11, 1603. [Google Scholar] [CrossRef] [PubMed]
- Bannoehr, J.; Guardabassi, L. Staphylococcus pseudintermedius in the dog: Taxonomy, diagnostics, ecology, epidemiology and pathogenicity. Vet. Dermatol. 2012, 23, 253–266, e51–e52. [Google Scholar] [CrossRef] [PubMed]
- Weese, J.S.; Giguere, S.; Guardabassi, L.; Morley, P.S.; Papich, M.; Ricciuto, D.R.; Sykes, J.E. ACVIM consensus statement on therapeutic antimicrobial use in animals and antimicrobial resistance. J. Vet. Intern. Med. 2015, 29, 487–498. [Google Scholar] [CrossRef]
- Gronthal, T.; Eklund, M.; Thomson, K.; Piiparinen, H.; Sironen, T.; Rantala, M. Antimicrobial resistance in Staphylococcus pseudintermedius and the molecular epidemiology of methicillin-resistant S. pseudintermedius in small animals in Finland. J. Antimicrob. Chemother. 2017, 72, 1021–1030. [Google Scholar] [CrossRef]
- Platenik, M.O.; Archer, L.; Kher, L.; Santoro, D. Prevalence of mecA, mecC and Panton-Valentine-Leukocidin Genes in Clinical Isolates of Coagulase Positive Staphylococci from Dermatological Canine Patients. Microorganisms 2022, 10, 2239. [Google Scholar] [CrossRef]
- Gonzalez-Dominguez, M.S.; Carvajal, H.D.; Calle-Echeverri, D.A.; Chinchilla-Cardenas, D. Molecular Detection and Characterization of the mecA and nuc Genes from Staphylococcus Species (S. aureus, S. pseudintermedius, and S. schleiferi) Isolated from Dogs Suffering Superficial Pyoderma and Their Antimicrobial Resistance Profiles. Front. Vet. Sci. 2020, 7, 376. [Google Scholar] [CrossRef]
- Chanayat, Y.; Akatvipat, A.; Bender, J.B.; Punyapornwithaya, V.; Meeyam, T.; Anukool, U.; Pichpol, D. The SCCmec Types and Antimicrobial Resistance among Methicillin-Resistant Staphylococcus Species Isolated from Dogs with Superficial Pyoderma. Vet. Sci. 2021, 8, 85. [Google Scholar] [CrossRef]
- Janos, D.; Viorel, H.; Ionica, I.; Corina, P.; Tiana, F.; Roxana, D. Carriage of Multidrug Resistance Staphylococci in Shelter Dogs in Timisoara, Romania. Antibiotics 2021, 10, 801. [Google Scholar] [CrossRef]
- McCarthy, A.J.; Harrison, E.M.; Stanczak-Mrozek, K.; Leggett, B.; Waller, A.; Holmes, M.A.; Lloyd, D.H.; Lindsay, J.A.; Loeffler, A. Genomic insights into the rapid emergence and evolution of MDR in Staphylococcus pseudintermedius. J. Antimicrob. Chemother. 2015, 70, 997–1007. [Google Scholar] [CrossRef]
- Jones, R.D.; Kania, S.A.; Rohrbach, B.W.; Frank, L.A.; Bemis, D.A. Prevalence of oxacillin- and multidrug-resistant staphylococci in clinical samples from dogs: 1772 samples (2001–2005). J. Am. Vet. Med. Assoc. 2007, 230, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Somayaji, R.; Priyantha, M.A.; Rubin, J.E.; Church, D. Human infections due to Staphylococcus pseudintermedius, an emerging zoonosis of canine origin: Report of 24 cases. Diagn. Microbiol. Infect. Dis. 2016, 85, 471–476. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.H.; Ma, Y.C.; Shia, W.Y.; Hsieh, Y.L.; Wang, C.M. Risk Factors for Antimicrobial Resistance of Staphylococcus Species Isolated from Dogs with Superficial Pyoderma and Their Owners. Vet. Sci. 2022, 9, 306. [Google Scholar] [CrossRef] [PubMed]
- Carroll, K.C.; Burnham, C.D.; Westblade, L.F. From canines to humans: Clinical importance of Staphylococcus pseudintermedius. PLoS Pathog. 2021, 17, e1009961. [Google Scholar] [CrossRef] [PubMed]
- Bhooshan, S.; Negi, V.; Khatri, P.K. Staphylococcus pseudintermedius: An undocumented, emerging pathogen in humans. GMS Hyg. Infect. Control 2020, 15, Doc32. [Google Scholar] [CrossRef]
- Liu, C.; Bayer, A.; Cosgrove, S.E.; Daum, R.S.; Fridkin, S.K.; Gorwitz, R.J.; Kaplan, S.L.; Karchmer, A.W.; Levine, D.P.; Murray, B.E.; et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: Executive summary. Clin. Infect. Dis. 2011, 52, 285–292. [Google Scholar] [CrossRef]
- Jackson, H.A.; Marsella, R. Manual of Canine and Feline Dermatology, 3rd ed.; British Small Animal Veterinary Association ProQuest Ebook Central: Quedgeley, Gloucester, UK; Ann Arbor, MI, USA, 2012. [Google Scholar]
- Morris, D.O.; Loeffler, A.; Davis, M.F.; Guardabassi, L.; Weese, J.S. Recommendations for approaches to meticillin-resistant staphylococcal infections of small animals: Diagnosis, therapeutic considerations and preventative measures: Clinical Consensus Guidelines of the World Association for Veterinary Dermatology. Vet. Dermatol. 2017, 28, 304-e69. [Google Scholar] [CrossRef]
- Yoo, J.H.; Yoon, J.W.; Lee, S.Y.; Park, H.M. High prevalence of Fluoroquinolone- and Methicillin-resistant Staphylococcus pseudintermedius isolates from canine pyoderma and otitis externa in veterinary teaching hospital. J. Microbiol. Biotechnol. 2010, 20, 798–802. [Google Scholar]
- Faires, M.C.; Gard, S.; Aucoin, D.; Weese, J.S. Inducible clindamycin-resistance in methicillin-resistant Staphylococcus aureus and methicillin-resistant Staphylococcus pseudintermedius isolates from dogs and cats. Vet. Microbiol. 2009, 139, 419–420. [Google Scholar] [CrossRef]
- Batra, P.; Deo, V.; Mathur, P.; Gupta, A.K. Cotrimoxazole, a wonder drug in the era of multiresistance: Case report and review of literature. J. Lab. Physicians 2017, 9, 210–213. [Google Scholar] [CrossRef]
- MacDougall, C. Sulfonamides, Trimethoprim-Sulfamethoxazole, Quinolones, and Agents for Urinary Tract Infections. In Goodman & Gilman's: The Pharmacological Basis of Therapeutics, 13e; Brunton, L.L., Hilal-Dandan, R., Knollmann, B.C., Eds.; McGraw-Hill Education: New York, NY, USA, 2017. [Google Scholar]
- Prescott, J.F. Sulfonamides, Diaminopyrimidines, and Their Combinations. In Antimicrobial Therapy in Veterinary Medicine; Giguère, S., Prescott, J.F., Dowling, P.M., Eds.; John Wiley & Sons: Ames, IA, USA, 2013; pp. 279–294. [Google Scholar] [CrossRef]
- Brown, N.M.; Brown, E.M.; Guideline Development, G. Treatment of methicillin-resistant Staphylococcus aureus (MRSA): Updated guidelines from the UK. J. Antimicrob. Chemother. 2021, 76, 1377–1378. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, E.; Paul, M.; Talker, O.; Samra, Z.; Raskin, M.; Hazzan, R.; Leibovici, L.; Bishara, J. Co-trimoxazole versus vancomycin for the treatment of methicillin-resistant Staphylococcus aureus bacteraemia: A retrospective cohort study. J. Antimicrob. Chemother. 2010, 65, 1779–1783. [Google Scholar] [CrossRef] [PubMed]
- Bowen, A.C.; Carapetis, J.R.; Currie, B.J.; Fowler, V., Jr.; Chambers, H.F.; Tong, S.Y.C. Sulfamethoxazole-Trimethoprim (Cotrimoxazole) for Skin and Soft Tissue Infections Including Impetigo, Cellulitis, and Abscess. Open Forum Infect. Dis. 2017, 4, ofx232. [Google Scholar] [CrossRef] [PubMed]
- Plumb, D.C. Plumb's Veterinary Drug Handbook, 9th ed.; PharmaVet Inc. John Wiley & Sons, Inc.: Stockholm, Sweden, WI, USA; Hoboken, NJ, USA, 2018; p. 1428. [Google Scholar]
- Ling, G.V.; Rohrich, P.J.; Ruby, A.L.; Johnson, D.L.; Jang, S.S. Canine urinary tract infections: A comparison of in vitro antimicrobial susceptibility test results and response to oral therapy with ampicillin or with trimethoprim-sulfa. J. Am. Vet. Med. Assoc. 1984, 185, 277–281. [Google Scholar]
- Shevchenko, M.; Savcheniuk, M.; Yarchuk, B.; Sakhniuk, N.; Tsarenko, T. Coagulase-positive staphylococci in dogs and their antimicrobial resistance (systematic review). Nauk. Vìsn. Vet. Med. 2021, 1, 104–118. [Google Scholar] [CrossRef]
- Morris, D.O.; Rook, K.A.; Shofer, F.S.; Rankin, S.C. Screening of Staphylococcus aureus, Staphylococcus intermedius, and Staphylococcus schleiferi isolates obtained from small companion animals for antimicrobial resistance: A retrospective review of 749 isolates (2003-04). Vet. Dermatol. 2006, 17, 332–337. [Google Scholar] [CrossRef]
- Rana, E.A.; Islam, M.Z.; Das, T.; Dutta, A.; Ahad, A.; Biswas, P.K.; Barua, H. Prevalence of coagulase-positive methicillin-resistant Staphylococcus aureus and Staphylococcus pseudintermedius in dogs in Bangladesh. Vet. Med. Sci. 2022, 8, 498–508. [Google Scholar] [CrossRef]
- Joffe, D.; Goulding, F.; Langelier, K.; Magyar, G.; McCurdy, L.; Milstein, M.; Nielsen, K.; Villemaire, S. Prevalence of methicillin-resistant staphylococci in canine pyoderma cases in primary care veterinary practices in Canada: A preliminary study. Can. Vet. J. 2015, 56, 1084–1086. [Google Scholar]
- CLSI. Performance Standards for Antimicrobial Disk and Dilution Susceptibility Tests for Bacteria Isolated from Animals, 4th ed.; CLSI Supplement VET08; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2018. [Google Scholar]
- Delmas, J.; Chacornac, J.P.; Robin, F.; Giammarinaro, P.; Talon, R.; Bonnet, R. Evaluation of the Vitek 2 system with a variety of Staphylococcus species. J. Clin. Microbiol. 2008, 46, 311–313. [Google Scholar] [CrossRef]
- Crowley, E.; Bird, P.; Fisher, K.; Goetz, K.; Boyle, M.; Benzinger, M.J., Jr.; Juenger, M.; Agin, J.; Goins, D.; Johnson, R.L. Evaluation of the VITEK 2 gram positive (GP) microbial identification test card: Collaborative study. J. AOAC Int. 2012, 95, 1425–1432. [Google Scholar] [CrossRef]
- Kim, M.; Heo, S.R.; Choi, S.H.; Kwon, H.; Park, J.S.; Seong, M.W.; Lee, D.H.; Park, K.U.; Song, J.; Kim, E.C. Comparison of the MicroScan, VITEK 2, and Crystal GP with 16S rRNA sequencing and MicroSeq 500 v2.0 analysis for coagulase-negative Staphylococci. BMC Microbiol. 2008, 8, 233. [Google Scholar] [CrossRef] [PubMed]
- Skov, R.; Varga, A.; Matuschek, E.; Ahman, J.; Bemis, D.; Bengtsson, B.; Sunde, M.; Humphries, R.; Westblade, L.; Guardabassi, L.; et al. EUCAST disc diffusion criteria for the detection of mecA-Mediated beta-lactam resistance in Staphylococcus pseudintermedius: Oxacillin versus cefoxitin. Clin. Microbiol. Infect. 2020, 26, 122.e1–122.e6. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.T.; Burnham, C.A.; Westblade, L.F.; Dien Bard, J.; Lawhon, S.D.; Wallace, M.A.; Stanley, T.; Burd, E.; Hindler, J.; Humphries, R.M. Evaluation of Oxacillin and Cefoxitin Disk and MIC Breakpoints for Prediction of Methicillin Resistance in Human and Veterinary Isolates of Staphylococcus intermedius Group. J. Clin. Microbiol. 2016, 54, 535–542. [Google Scholar] [CrossRef] [PubMed]
- Badger, S.; Abraham, S.; O'Dea, M.; Saputra, S.; Abraham, R.J.; Worthing, K.A.; Norris, J.M.; Trott, D.J.; Jordan, D.; Caraguel, C.G.B. Diagnostic accuracy of phenotypic assays for determining antimicrobial resistance status in Staphylococcus pseudintermedius isolates from canine clinical cases. Vet. Microbiol. 2019, 234, 101–109. [Google Scholar] [CrossRef]
- Fernandes, C.J.; Fernandes, L.A.; Collignon, P.; Australian Group on Antimicrobial, R. Cefoxitin resistance as a surrogate marker for the detection of methicillin-resistant Staphylococcus aureus. J. Antimicrob. Chemother. 2005, 55, 506–510. [Google Scholar] [CrossRef]
- Roisin, S.; Nonhoff, C.; Denis, O.; Struelens, M.J. Evaluation of new Vitek 2 card and disk diffusion method for determining susceptibility of Staphylococcus aureus to oxacillin. J. Clin. Microbiol. 2008, 46, 2525–2528. [Google Scholar] [CrossRef]
- Junkins, A.D.; Lockhart, S.R.; Heilmann, K.P.; Dohrn, C.L.; Von Stein, D.L.; Winokur, P.L.; Doern, G.V.; Richter, S.S. BD Phoenix and Vitek 2 detection of mecA-mediated resistance in Staphylococcus aureus with cefoxitin. J. Clin. Microbiol. 2009, 47, 2879–2882. [Google Scholar] [CrossRef]
- Cartwright, E.J.; Paterson, G.K.; Raven, K.E.; Harrison, E.M.; Gouliouris, T.; Kearns, A.; Pichon, B.; Edwards, G.; Skov, R.L.; Larsen, A.R.; et al. Use of Vitek 2 antimicrobial susceptibility profile to identify mecC in methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 2013, 51, 2732–2734. [Google Scholar] [CrossRef]
- Scherer, C.B.; Botoni, L.S.; Coura, F.M.; Silva, R.O.; Santos, R.D.d.; Heinemann, M.B.; Costa-Val, A.P. Frequency and antimicrobial susceptibility of Staphylococcus pseudintermedius in dogs with otitis externa. Ciência Rural 2018, 48. [Google Scholar] [CrossRef]
- Viegas, F.M.; Santana, J.A.; Silva, B.A.; Xavier, R.G.C.; Bonisson, C.T.; Camara, J.L.S.; Renno, M.C.; Cunha, J.L.R.; Figueiredo, H.C.P.; Lobato, F.C.F.; et al. Occurrence and characterization of methicillin-resistant Staphylococcus spp. in diseased dogs in Brazil. PLoS ONE 2022, 17, e0269422. [Google Scholar] [CrossRef]
- Lord, J.; Millis, N.; Jones, R.D.; Johnson, B.; Kania, S.A.; Odoi, A. Patterns of antimicrobial, multidrug and methicillin resistance among Staphylococcus spp. isolated from canine specimens submitted to a diagnostic laboratory in Tennessee, USA: A descriptive study. BMC Vet. Res. 2022, 18, 91. [Google Scholar] [CrossRef] [PubMed]
- Saputra, S.; Jordan, D.; Worthing, K.A.; Norris, J.M.; Wong, H.S.; Abraham, R.; Trott, D.J.; Abraham, S. Antimicrobial resistance in coagulase-positive staphylococci isolated from companion animals in Australia: A one year study. PLoS ONE 2017, 12, e0176379. [Google Scholar] [CrossRef]
- Priyantha, R.; Gaunt, M.C.; Rubin, J.E. Antimicrobial susceptibility of Staphylococcus pseudintermedius colonizing healthy dogs in Saskatoon, Canada. Can. Vet. J. 2016, 57, 65–69. [Google Scholar] [PubMed]
- Humphries, R.M.; Wu, M.T.; Westblade, L.F.; Robertson, A.E.; Burnham, C.A.; Wallace, M.A.; Burd, E.M.; Lawhon, S.; Hindler, J.A. In Vitro Antimicrobial Susceptibility of Staphylococcus pseudintermedius Isolates of Human and Animal Origin. J. Clin. Microbiol. 2016, 54, 1391–1394. [Google Scholar] [CrossRef] [PubMed]
- Maluping, R.P.; Paul, N.C.; Moodley, A. Antimicrobial susceptibility of methicillin-resistant Staphylococcus pseudintermedius isolated from veterinary clinical cases in the UK. Br. J. Biomed. Sci. 2014, 71, 55–57. [Google Scholar] [CrossRef] [PubMed]
- Mlynarczyk-Bonikowska, B.; Kowalewski, C.; Krolak-Ulinska, A.; Marusza, W. Molecular Mechanisms of Drug Resistance in Staphylococcus aureus. Int. J. Mol. Sci. 2022, 23, 88. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Ito, R.; Kawamura, M.; Fujimura, S. The Risk of Emerging Resistance to Trimethoprim/Sulfamethoxazole in Staphylococcus aureus. Infect. Drug Resist. 2022, 15, 4779–4784. [Google Scholar] [CrossRef]
- Bobenchik, A.M.; Hindler, J.A.; Giltner, C.L.; Saeki, S.; Humphries, R.M. Performance of Vitek 2 for antimicrobial susceptibility testing of Staphylococcus spp. and Enterococcus spp. J. Clin. Microbiol. 2014, 52, 392–397. [Google Scholar] [CrossRef]
- Buchan, B.W.; Anderson, N.W.; Ledeboer, N.A. Comparison of BD Phoenix and bioMerieux Vitek 2 automated systems for the detection of macrolide-lincosamide-streptogramin B resistance among clinical isolates of Staphylococcus. Diagn. Microbiol. Infect. Dis. 2012, 72, 291–294. [Google Scholar] [CrossRef]
- Rampacci, E.; Trotta, M.; Fani, C.; Silvestri, S.; Stefanetti, V.; Brachelente, C.; Mencacci, A.; Passamonti, F. Comparative Performances of Vitek-2, Disk Diffusion, and Broth Microdilution for Antimicrobial Susceptibility Testing of Canine Staphylococcus pseudintermedius. J. Clin. Microbiol. 2021, 59, e0034921. [Google Scholar] [CrossRef]
- Hillier, A.; Lloyd, D.H.; Weese, J.S.; Blondeau, J.M.; Boothe, D.; Breitschwerdt, E.; Guardabassi, L.; Papich, M.G.; Rankin, S.; Turnidge, J.D.; et al. Guidelines for the diagnosis and antimicrobial therapy of canine superficial bacterial folliculitis (Antimicrobial Guidelines Working Group of the International Society for Companion Animal Infectious Diseases). Vet. Dermatol. 2014, 25, 163-e43. [Google Scholar] [CrossRef] [PubMed]
- Eyler, R.F.; Shvets, K. Clinical Pharmacology of Antibiotics. Clin. J. Am. Soc. Nephrol. 2019, 14, 1080–1090. [Google Scholar] [CrossRef]
- Brown, G.R. Cotrimoxazole—Optimal dosing in the critically ill. Ann. Intensive Care 2014, 4, 13. [Google Scholar] [CrossRef] [PubMed]
- Summers, J.F.; Brodbelt, D.C.; Forsythe, P.J.; Loeffler, A.; Hendricks, A. The effectiveness of systemic antimicrobial treatment in canine superficial and deep pyoderma: A systematic review. Vet. Dermatol. 2012, 23, 305–329, e61. [Google Scholar] [CrossRef]
- Diaz, R.; Afreixo, V.; Ramalheira, E.; Rodrigues, C.; Gago, B. Evaluation of vancomycin MIC creep in methicillin-resistant Staphylococcus aureus infections-a systematic review and meta-analysis. Clin. Microbiol. Infect. 2018, 24, 97–104. [Google Scholar] [CrossRef]
- Pires Dos Santos, T.; Damborg, P.; Moodley, A.; Guardabassi, L. Systematic Review on Global Epidemiology of Methicillin-Resistant Staphylococcus pseudintermedius: Inference of Population Structure from Multilocus Sequence Typing Data. Front. Microbiol. 2016, 7, 1599. [Google Scholar] [CrossRef] [PubMed]
- Loeffler, A.; Lloyd, D.H. What has changed in canine pyoderma? A narrative review. Vet. J. 2018, 235, 73–82. [Google Scholar] [CrossRef]
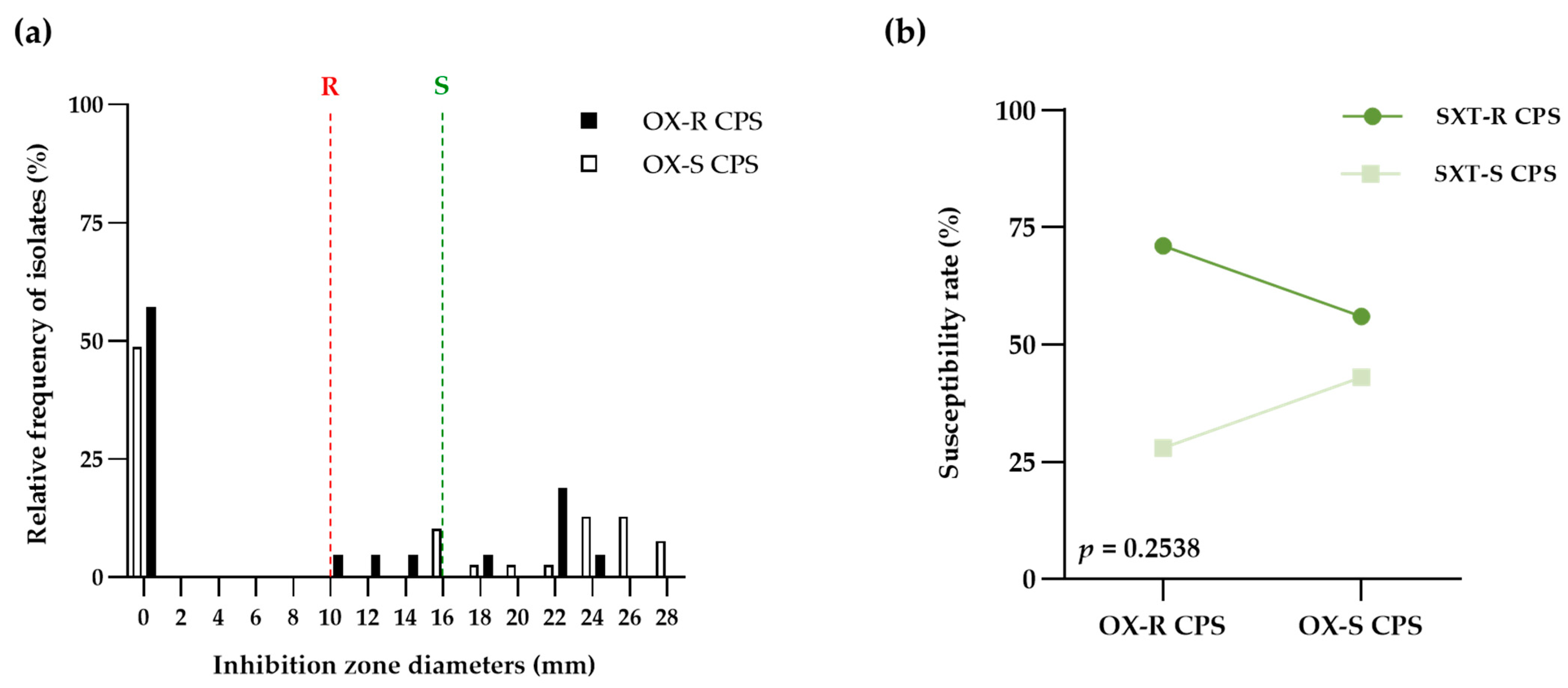
| SXT-R CPS | SXT-S CPS | Total | |
|---|---|---|---|
| OX-R CPS | 15 | 6 | 21 |
| OX-S CPS | 22 | 17 | 39 |
| Total | 37 | 23 | 60 |
| Susceptibility | Pathogenic Bacteria | ||
|---|---|---|---|
| OX-R CPS | OX-S CPS | Total | |
| Range | 0–24 | 0–28 | 0–28 |
| Mean ± SD | 7.71 ns ± 9.69 | 11.46 ns ± 11.75 | 10.15 ± 11.13 |
| Median (IQR) | 0 ns (0–19) | 15 ns (0–24) | 0 (0–22) |
| SXT-R SP | SXT-S SP | Total | |
|---|---|---|---|
| MRSP | 7 | 9 | 16 |
| MSSP | 23 | 21 | 44 |
| Total | 30 | 30 | 60 |
| Susceptibility | Pathogenic Bacteria | ||
|---|---|---|---|
| MRSP | MSSP | Total | |
| Median (IQR) | ≥320 ns (10–320) | ≤10 ns (10–320) | ≤10 (10–320) |
| 50th percentile | ≥320 | ≤10 | ≤10 |
| 90th percentile | ≥320 | ≥320 | ≥320 |
| MIC90: MIC50 | 1 | 32 | 32 |
| Dosing Interval | %Time above MIC | Attainment (%) | ||
|---|---|---|---|---|
| MRSP | MSSP | p-Value | ||
| q 24 h | 33.33 | 0.00 | 0.00 | >0.9999 |
| q 12 h | 66.66 | 43.75 | 52.27 | 0.7710 |
| q 8 h | 100.00 | 43.75 | 52.27 | 0.7710 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khongsri, U.; Chongrattanameteekul, P.; Chantarachart, S.; Photichai, K.; Chanayat, N.; Varinrak, T.; Mektrirat, R.; Srifawattana, N. Comparative Susceptibility of Pathogenic Methicillin-Resistant and Methicillin-Susceptible Staphylococcus pseudintermedius to Empirical Co-Trimoxazole for Canine Pyoderma. Life 2023, 13, 1210. https://doi.org/10.3390/life13051210
Khongsri U, Chongrattanameteekul P, Chantarachart S, Photichai K, Chanayat N, Varinrak T, Mektrirat R, Srifawattana N. Comparative Susceptibility of Pathogenic Methicillin-Resistant and Methicillin-Susceptible Staphylococcus pseudintermedius to Empirical Co-Trimoxazole for Canine Pyoderma. Life. 2023; 13(5):1210. https://doi.org/10.3390/life13051210
Chicago/Turabian StyleKhongsri, Usasom, Peerawit Chongrattanameteekul, Sineenart Chantarachart, Kornravee Photichai, Nittaya Chanayat, Thanya Varinrak, Raktham Mektrirat, and Nuttawan Srifawattana. 2023. "Comparative Susceptibility of Pathogenic Methicillin-Resistant and Methicillin-Susceptible Staphylococcus pseudintermedius to Empirical Co-Trimoxazole for Canine Pyoderma" Life 13, no. 5: 1210. https://doi.org/10.3390/life13051210
APA StyleKhongsri, U., Chongrattanameteekul, P., Chantarachart, S., Photichai, K., Chanayat, N., Varinrak, T., Mektrirat, R., & Srifawattana, N. (2023). Comparative Susceptibility of Pathogenic Methicillin-Resistant and Methicillin-Susceptible Staphylococcus pseudintermedius to Empirical Co-Trimoxazole for Canine Pyoderma. Life, 13(5), 1210. https://doi.org/10.3390/life13051210







