Hands off Trans-Femoral Venous Intra-Abdominal Pressure Estimates in Children: Results of a Sobering Single-Center Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design of the Study
2.2. Patient Study Recruitment
2.3. Clinical Data Collection
2.4. Intra-Abdominal Pressure Measurement (IAP)
2.5. Measurement Practice
2.6. Agreement of FVP with IVP/IGP
2.7. Explorative Analysis of Confounders
- -
- Group 1: no tricuspid valve (TI) and/or no pulmonary valve insufficiency/regurgitation (PI) and no pulmonary hypertension (PHT).
- -
- Group 2: mild TI and/or mild PI and no PHT
- -
- Group 3: mild to moderate TI and/or mild to moderate PI and signs of PHT
- -
- Group 4: no echocardiographic results available
- -
- No child showed signs of severe TI and/or PI.
- -
- Group 1: IAP < 7 mmHg (corresponds to normal IAP in children)
- -
- Group 2: IAP 7–9 mmHg (corresponds to “pre-IAH” especially in neonates and infants)
- -
- Group 3: IAP 10–12 mmHg (corresponds to IAH grade I in children)
- -
- Group 4: IAP 13–15 mmHg (corresponds to IAH grade II in children)
- -
- Group 5: IAP 16–18 mmHg (corresponds to IAH grade III in children)
- -
- Group 6: IAP > 16 mmHg (corresponds to IAH grade IV in children)
2.8. Data Processing and Statistical Analysis
3. Results
3.1. Patients Characteristics
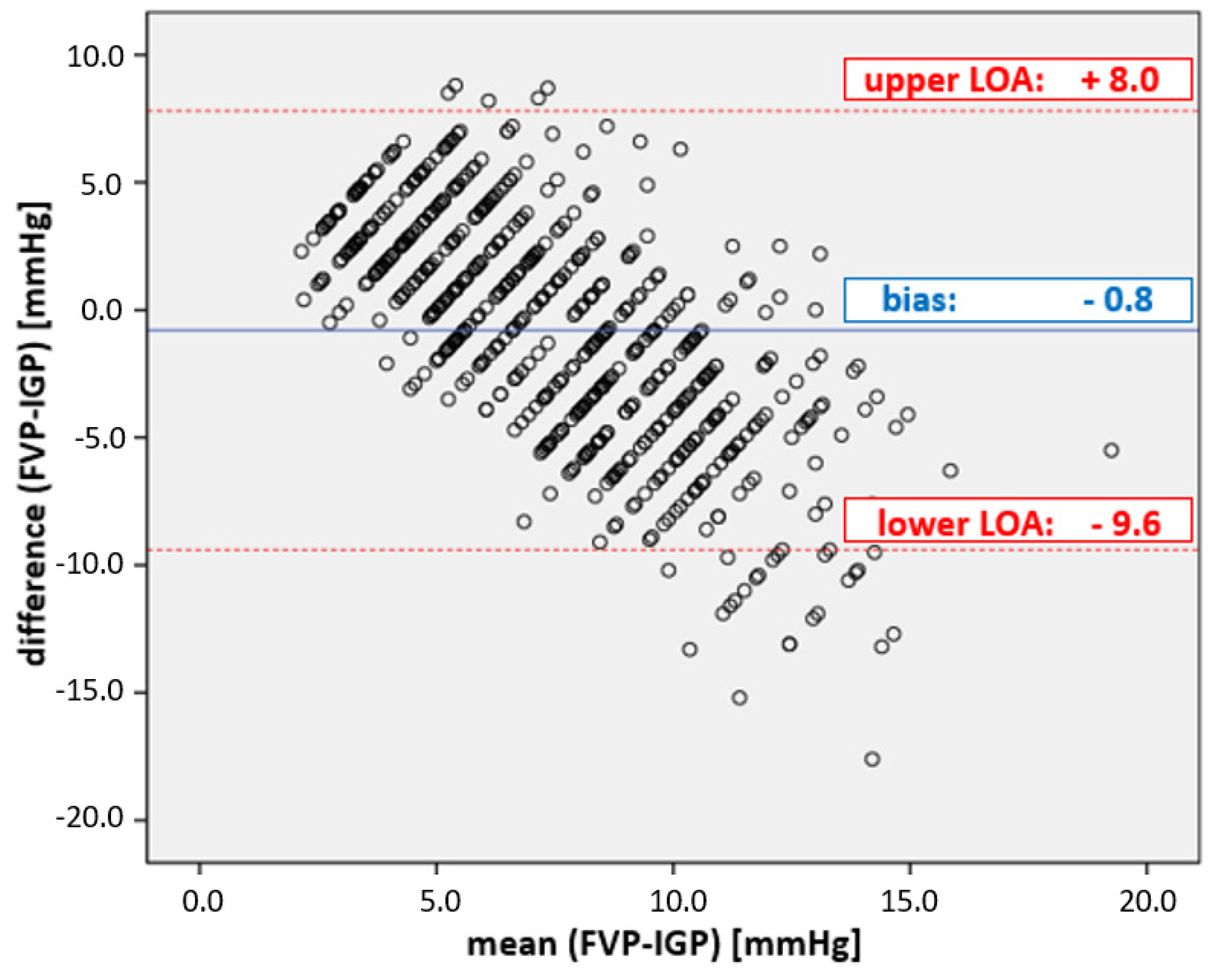
3.2. Comparison between FVP and IGP
3.2.1. Overall Results
3.2.2. Explorative Additional Examinations
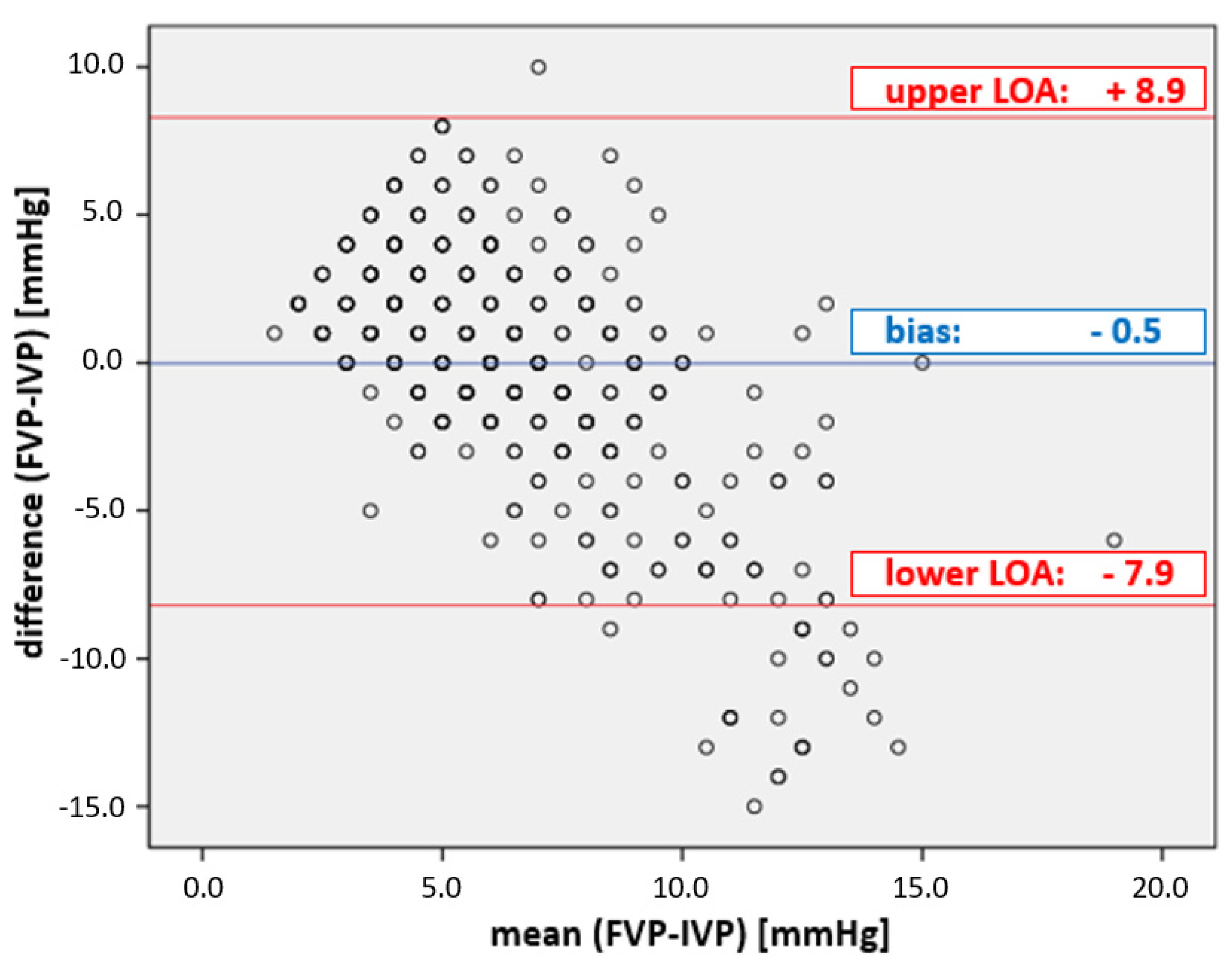
3.3. Comparison between FVP and IVP
3.3.1. Overall Results
3.3.2. Exploratory Additional Examinations
4. Discussion
4.1. Study Design and Key Messages
In this challenging population, we proved beyond doubt that IAP estimation by FVP quantification is useless in everyday clinical practice in the PICU. It is neither accurate, nor precise, reproducible or reliable against the actual medical benchmark method, bladder pressure measurement (IVP) and the validated measurement method alternative, namely, intra-gastric pressure measurement (IGP).
4.2. Medical Historical Motivations for This IAP Estimation Validation Study
4.3. Clinical Implications
- -
- lack of accuracy, sensitivity and reliability
- -
- high susceptibility to errors (e.g., due to movement artefacts and sensitivity)
- -
- lack of standardization or even lack of proof of concept
- -
- high costs.
4.4. Study limitations
| Study Type/Model | Author Year [Ref.] | Measure Methods | Methods–Statistics | No of Subjects Enrolled (No. of Paired Measures) | IAP Range (mmHg) | Comparisons | Results | Conclusion | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Correlation Coefficient | WSACS Method Validation Criteria | |||||||||||||
| Bias (mmHg) | Precision (mmHg) | LOA (mmHg) | PE (%) | |||||||||||
| in-vivo | Animals | Lacey 1987 [22] | IVCP (FVP) IVP IGP | Correlation coefficient (unspecified) | 17 rabbits (n.a.) | 0–30 | IAP versus IVCP (FVP) IAP versus IVP IAP versus IGP | >0.87 >0.85 0.7 | n.a. | n.a. | n.a. | n.a. | FVP usable | |
| Gudmundsson 2002 [11] | FVP IVCP IVP | Correlation coefficient (unspecified) | 8 pigs (n.a.) | 15–40 | IAP versus FVP IAP versus IVCP IAP versus IVP | 0.95 0.94 0.92 | n.a. | n.a. | n.a. | n.a. | FVP usable | |||
| Jakob 2010 [23] | IGP IVP IVCP (FVP) | Pearson correlation coefficient (r²) Bias LOA | 12 pigs (n.a.) | 0–22 | IGP versus IVP IGP versus IVCP IVP versus IVCP | 0.60 0.63 0.52 | n.a. | n.a. | n.a. | n.a. | FVP limited usable | |||
| Regli 2010 [24] | FVP IVP | Correlation coefficient (r²) Bias, precision | 13 pigs (n.a.) | 3–26 | IVP versus FVP | 0.89 | 5.0 | 3.8 | n.a. | n.a. | FVP limited usable | |||
| Human | Adults | Joynt 1996 [12] | SVCP IVCP (FVP) | Bias precision LOA | 19 (133) | 1–26 | SVCP versus IVCP | n.a. | 0.45 | 0.89 | −1.33 to 2.23 | n.a. | FVP usable | |
| Ho 1998 [13] | SVCP IVCP | Bias, precision LOA | 20 (140) | n.a. | SVCP versus IVCP | n.a. | 0.1 | 1.06 | −2.04 to 2.2 | n.a. | FVP usable | |||
| Markou 2004 [25] | IVCP (FVP) IVP | Pearson correlation coefficient | 38 (151) | n.a. | IVP versus IVCP 1. IAP < 10 mmHg 2. IAP 10–15 mmHg 3. IAP > 15 mmHg | 0.76 0.69 0.78 | n.a. | n.a. | n.a. | n.a. | FVP not usable | |||
| De Keulenaer 2011 [26] | IVP FVP | Bias, precision LOA | 149 (866) | 6.7–22.4 | IVP versus FVP 1. pooled IAP 2. IAP ≥ 12mmHg 2. IAP > 20 mmHg | n.a. | −1.5 0.4 0.7 | 3.6 3.9 2 | −8.6 to 5.7 −8.1 to 7.3 −3 to 4.6 | n.a. | FVP not usable | |||
| Howard 2016 [31] | IVP FVP | All WSACS method validation criteria | 11 (53) | 0–25 | IVP versus FVP pooled without weight artificially increased IAP 5 kg artificially increased IAP 10 kg | 0.8 n.a. n.a. n.a. | 2.8 3.2 2.5 2.5 | 3.42 3.63 3.92 2.26 | −4.1 to 9.6 −4.1 to 10.4 −5.4 to 10.3 −2.1 to 7 | 46.8 n.a. n.a. 27.1 | FVP not usable | |||
| Children | Present study | FVP IVP IGP | All WSACS method validation criteria | 39 (1119) | 1–23 | FVP versus IVP FVP versus IGP | 0.14 0.13 | 0.5 −0.8 | 4.2 4.4 | −7.9 to 8.9 −9.6 to 8.0 | 133 117 | FVP not usable | ||
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACM | Air capsule-based measurement |
| ACS | Abdominal compartment syndrome |
| BMI | Body mass index |
| FVP | Femoral vein pressure |
| IAH | Intra-abdominal hypertension |
| IAP | Intra-abdominal pressure |
| IGP | intra-gastric pressure |
| IVCP | Inferior Vena cava pressure |
| IVP | Intra-vesical pressure |
| LA | Limits of agreement |
| LOS-PICU | Duration of stay at PICU |
| MHH | Medizinische Hochschule Hannover |
| PE | Percentage error |
| PHT | Pulmonary hypertension |
| PI | Pulmonary valve insufficiency |
| PICU | Pediatric intensive care unit |
| PRISM-III | Pediatric risk of mortality score III |
| SD | Standard deviation |
| SVCP | Superior vena cava pressure |
| TI | Tricuspid valve insufficiency |
| WHO | World Health Organisation |
| WSACS | Abdominal Compartment Society (formerly known as World Society of Abdominal Compartment Syndrome) |
References
- Thabet, F.C.; Bougmiza, I.M.; Chehab, M.S.; Bafaqih, H.A.; Al Mohaimeed, S.A.; Malbrain, M.L. Incidence, Risk Factors, and Prognosis of Intra-Abdominal Hypertension in Critically Ill Children: A Prospective Epidemiological Study. J. Intensive Care Med. 2016, 31, 403–408. [Google Scholar] [CrossRef]
- Steinau, G.; Kaussen, T.; Bolten, B.; Schachtrupp, A.; Neumann, U.P.; Conze, J.; Boehm, G. Abdominal compartment syndrome in childhood: Diagnostics, therapy and survival rate. Pediatr. Surg. Int. 2011, 27, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Ejike, J.C.; Mathur, M.; Moores, D.C. Abdominal compartment syndrome: Focus on the children. Am. Surg. 2011, 77 (Suppl. S1), S72–S77. [Google Scholar] [PubMed]
- Ejike, J.C.; Humbert, S.; Bahjri, K.; Mathur, M. Outcomes of children with abdominal compartment syndrome. Acta Clin. Belg. 2007, 62 (Suppl. S1), 141–148. [Google Scholar] [CrossRef] [PubMed]
- Kaussen, T.; Steinau, G.; Srinivasan, P.K.; Otto, J.; Sasse, M.; Staudt, F.; Schachtrupp, A. Recognition and management of abdominal compartment syndrome among German pediatric intensivists: Results of a national survey. Ann. Intensive Care 2012, 2 (Suppl. S1), S8. [Google Scholar] [CrossRef]
- Kirkpatrick, A.W.; Roberts, D.J.; De Waele, J.; Jaeschke, R.; Malbrain, M.L.; De Keulenaer, B.; Duchesne, J.; Bjorck, M.; Leppaniemi, A.; Ejike, J.; et al. Intra-abdominal hypertension and the abdominal compartment syndrome: Updated consensus definitions and clinical practice guidelines from the World Society of the Abdominal Compartment Syndrome. Intensive Care Med. 2013, 39, 1190–1206. [Google Scholar] [CrossRef]
- Rezeni, N.; Thabet, F. Awareness and management of intra-abdominal hypertension and abdominal compartment syndrome by paediatric intensive care physicians: A national survey. Anaesthesiol. Intensive Ther. 2022, 54, 315–319. [Google Scholar] [CrossRef]
- Newcombe, J.; Mathur, M.; Bahjri, K.; Ejike, J.C. Pediatric critical care nurses’ experience with abdominal compartment syndrome. Ann. Intensive Care 2012, 2 (Suppl. S1), S6. [Google Scholar] [CrossRef]
- Kaussen, T.; Gutting, M.; Lasch, F.; Boethig, D.; von Gise, A.; Dingemann, J.; Koeditz, H.; Jack, T.; Sasse, M.; Beerbaum, P.; et al. Continuous intra-gastral monitoring of intra-abdominal pressure in critically ill children: A validation study. Intensive Care Med. Exp. 2021, 9, 24. [Google Scholar] [CrossRef]
- Lacey, S.R.; Bruce, J.; Brooks, S.P.; Griswald, J.; Ferguson, W.; Allen, J.E.; Jewett, T.C., Jr.; Karp, M.P.; Cooney, D.R. The relative merits of various methods of indirect measurement of intraabdominal pressure as a guide to closure of abdominal wall defects. J. Pediatr. Surg. 1987, 22, 1207–1211. [Google Scholar] [CrossRef]
- Gudmundsson, F.F.; Viste, A.; Gislason, H.; Svanes, K. Comparison of different methods for measuring intra-abdominal pressure. Intensive Care Med. 2002, 28, 509–514. [Google Scholar] [CrossRef]
- Joynt, G.M.; Gomersall, C.D.; Buckley, T.A.; Oh, T.E.; Young, R.J.; Freebairn, R.C. Comparison of intrathoracic and intra-abdominal measurements of central venous pressure. Lancet 1996, 347, 1155–1157. [Google Scholar] [CrossRef] [PubMed]
- Ho, K.M.; Joynt, G.M.; Tan, P. A comparison of central venous pressure and common iliac venous pressure in critically ill mechanically ventilated patients. Crit. Care Med. 1998, 26, 461–464. [Google Scholar] [CrossRef]
- Pollack, M.M.; Patel, K.M.; Ruttimann, U.E. PRISM III: An updated Pediatric Risk of Mortality score. Crit. Care Med. 1996, 24, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Kron, I.L. A simple technique to accurately determine intra-abdominal pressure. Crit. Care Med. 1989, 17, 714–715. [Google Scholar] [CrossRef] [PubMed]
- Rosenzweig, E.B.; Abman, S.H.; Adatia, I.; Beghetti, M.; Bonnet, D.; Haworth, S.; Ivy, D.D.; Berger, R. Paediatric pulmonary arterial hypertesion: Updates on definition, classification, diagnostics and management. Eur. Respir. J. 2019, 53, 1801916. [Google Scholar] [CrossRef]
- Zoghbi, W.A.; Bonow, R.O.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Hahn, R.T.; Han, Y.; Hung, J.; Lang, R.M.; Little, S.; et al. Recommendations for Noninvasive Evaluation of Native Valvular Regurgitation—A Report from the American Society of Echocardiography. Developed in Collaboration with the Society for Cardiovascular Magnetic Resonance. J. Am. Soc. Echocardiogr. 2017, 30, 303–371. [Google Scholar] [CrossRef]
- Vahanian, A.B.F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.C.L.; De Bonis, M.; De Paulis, R.; Delgado, V.; Freemantle, N.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease—Developed by the Task Force for the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2022, 43, 561–632. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986, 1, 307–310. [Google Scholar] [CrossRef]
- De Myttenaere, A.G.B.; Le Grand, B.; Rossi, F. Mean Absolute Percentage Error for regression models. Neurocomputing 2016, 192, 10. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum, L., Ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Lacey, S.R.; Carris, L.A.; Beyer, A.J.; Azizkhan, R.G. Bladder pressure monitoring significantly enhances care of infants with abdominal wall defects: A prospective clinical study. J. Pediatr. Surg. 1993, 28, 1370–1374. [Google Scholar] [CrossRef] [PubMed]
- Jakob, S.M.; Knuesel, R.; Tenhunen, J.J.; Pradl, R.; Takala, J. Increasing abdominal pressure with and without PEEP: Effects on intra-peritoneal, intra-organ and intra-vascular pressures. BMC Gastroenterol. 2010, 10, 70. [Google Scholar] [CrossRef] [PubMed]
- Regli, A.; De Keulenaer, B.L.; Hockings, L.E.; Musk, G.C.; Roberts, B.; van Heerden, P.V. The role of femoral venous pressure and femoral venous oxygen saturation in the setting of intra-abdominal hypertension: A pig model. Shock 2011, 35, 422–427. [Google Scholar] [CrossRef]
- Markou, N.; Grigorakos, L.; Myrianthefs, P.; Boutzouka, E.; Rizos, M.; Evagelopoulou, P.; Apostolakos, H.; Baltopoulos, G. Venous pressure measurements in the superior and inferior vena cava: The influence of intra-abdominal pressure. Hepatogastroenterology 2004, 51, 51–55. [Google Scholar] [PubMed]
- De Keulenaer, B.L.; Regli, A.; Dabrowski, W.; Kaloiani, V.; Bodnar, Z.; Cea, J.I.; Litvin, A.A.; Davis, W.; Palermo, A.-M.; De Waele, J.; et al. Does femoral venous pressure measurement correlate well with intrabladder pressure measurement? A multicenter observational trial. Intensive Care Med. 2011, 37, 1620–1627. [Google Scholar] [CrossRef]
- Tayebi, S.; Gutierrez, A.; Mohout, I.; Smets, E.; Wise, R.; Stiens, J.; Malbrain, M.L.N.G. A concise overview of non-invasive intra-abdominal pressure measurement techniques: From bench to bedside. J. Clin. Monit. Comput. 2021, 35, 51–70. [Google Scholar] [CrossRef]
- Tayebi, S.; Pourkazemi, A.; Malbrain, M.; Stiens, J. Non-Invasive Intra-Abdominal Pressure Measurement by Means of Transient Radar Method: In Vitro Validation of a Novel Radar-Based Sensor. Sensors 2021, 21, 18. [Google Scholar] [CrossRef]
- Malbrain, M.; De Keulenaer, B.L.; Khanna, A.K. Continuous intra-abdominal pressure: Is it ready for prime time? Intensive Care Med. 2022, 48, 1501–1504. [Google Scholar] [CrossRef]
- Tayebi, S.; Wise, R.; Pourkazemi, A.; Stiens, J.; Malbrain, M. Pre-Clinical Validation of A Novel Continuous Intra-Abdominal Pressure Measurement Equipment (SERENNO). Life 2022, 12, 1161. [Google Scholar] [CrossRef]
- Howard, A.E.; Regli, A.; Litton, E.; Malbrain, M.M.; Palermo, A.M.; De Keulenaer, B.L. Can femoral venous pressure be used as an estimate for standard vesical intra-abdominal pressure measurement? Anaesth. Intensive Care 2016, 44, 704–711. [Google Scholar] [CrossRef]
| No. of Enrolled Patients | r2 * | Bias [mmHg] | Precision [mmHg] | LOA [mmHg] | Percentage Error [%] | |
|---|---|---|---|---|---|---|
| Target values | ≥20 | ≥0.6 * | ≤|1| | ≤2 | −4 to +4 | ≤25 |
| Parameter | FVP vs. IVP | FVP vs. IVP |
|---|---|---|
| Number of patients | 19 | 20 |
| Number of girls | 6 | 7 |
| Number of paired measures | 459 | 660 |
| Age [years] | 4.9 ± 5.3 | 4.7 ± 5.3 |
| Newborn [n = 1] | Newborn [n = 2] | |
| Sucklers [n = 5] | Sucklers [n = 5] | |
| Tots [n = 6] | Tots [n = 6] | |
| School [n = 5] | Schoolkids [n = 5] | |
| Teenagers [n = 2] | Teenagers [n = 2] | |
| Body mass index * | 16.7 ± 4.2 | 16.7 ± 4.1 |
| Duration of the stay at PICU [days] | 24.3 ± 41.6 | 21.8 ± 38.9 |
| Admission-justifying diagnoses (responsible clinical department) | Ped. Cardiology [n = 4] | Ped. Cardiology [n = 6] |
| Neurosurgery [n = 3] | Neurosurgery [n = 3] | |
| Pedosurgery [n = 5] | Pedosurgery [n = 4] | |
| Ped. pulmonology [n = 1] | Ped. pulmonology [n = 1] | |
| Ped. traumatology [n = 6] | Ped. traumatology [n = 6] | |
| PRISM-III-score | ||
| - First day of enrolment | 11.4 ± 6.5 | 11.3 ± 6.5 |
| - Last day of enrolment | 2.6 ± 2.8 | 2.6 ± 2.7 * |
| Lethality | 0% | 5% [1 deceased] ** |
| No. of Measurements | IGP [mmHg] | FVP [mmHg] | r2 | Bias [mmHg] | Precision [mmHg] | LOA [mmHg] | Percentage Error [%] | Mean Absolute Percentage Error (SD) [%] | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Median [Range] | ||||||||||
| Overall Result | 660 | 7.0 (2.4–16.5) | 7.0 (1.0–23.0) | 0.13 | −0.8 | 4.4 | −9.6–8.0 | 117 | 55 (47) | |
| Explorative additional examination: influenceability by right cardiac valve insufficiency | ||||||||||
| Echo- findings | No TI, no PI and no PHT | 48 | 5.7 (4.0–10.9) | 3.0 (1.0–13.0) | 0.13 | 2.1 | 2.3 | −2.5 to 6.7 | 90 | 41 (29) |
| Mild TI, mild PI and no PHT | 271 | 7.0 (2.5–16.5) | 10.0 (1.0–23.0) | 0.10 | −2.2 | 4.2 | −10.6 to 6.2 | 102 | 62 (50) | |
| Mild to moderate TI and/or PI and/or PHT | 120 | 6.8 (3.5–12.9) | 10.0 (1.0–19.0) | 0.47 | −1.8 | 3.6 | −9.0 to 5.4 | 91 | 50 (27) | |
| No Echo findings available | 221 | 7.1 (2.4–14.2) | 5.0 (1.0–21.0) | 0.06 | 0.8 | 4.6 | −8.4 to 10.0 | 135 | 52 (53) | |
| Exploratory additional examination: influenceability by the height of intra-abdominal pressure (IAP) | ||||||||||
| IAP [mmHg] | <7 | 189 | 5.2 (2.4–6.9) | 3.0 (1.0–6.0) | 0.01 | 1.7 | 1.9 | −2.1 to 5.5 | 88 | 42 (25) |
| 7–9 | 189 | 7.8 (3.5–9.8) | 7.0 (1.0–9.0) | 0.08 | 1.6 | 3.1 | −4.6 to 7.8 | 93 | 40 (27) | |
| 10–12 | 162 | 7.8 (2.7–12.6) | 11.0 (2.0–12.0) | 0.15 | −2.3 | 3.6 | −9.5 to 4.9 | 80 | 57 (43) | |
| 13–15 | 83 | 8.3 (3.9–14.2) | 14.0 (7.0–15.0) | 0.02 | −5.2 | 2.7 | −10.6 to 0.2 | 49 | 76 (49) | |
| 16–18 | 23 | 8.4 (3.7–12.9) | 17.0 (16.0–18.0) | 0.05 | −8.5 | 2.9 | −14.3 to −2.7 | 46 | 123 (80) | |
| >16 | 14 | 8.0 (3.8–16.5) | 19.0 (19.0–23.0) | 0.05 | −11.5 | 3.2 | −17.9 to −5.3 | 46 | 170 (99) | |
| No. of Measurements | IVP [mmHg] | FVP [mmHg] | r2 | Bias [mmHg] | Precision [mmHg] | LOA [mmHg] | Percentage Error [%] | Mean Absolute Percentage Error (SD) [%] | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Median [Range] | ||||||||||
| Overall Result | 459 | 6.0 (1.0–16.0) | 5.0 (1.0–22.0) | 0.14 | 0.5 | 4.2 | −7.9 to 8.9 | 133 | 51 (55) | |
| Exploratory additional examination: influenceability by right cardiac valve insufficiency | ||||||||||
| Echo- findings | No TI, no PI and no PHT | 48 | 5.0 (3.0–12.0) | 3.0 (1.0–13.0) | 0.02 | 1.5 | 2.6 | −3.7 to 6.7 | 108 | 37 (32) |
| Mild TI, mild PI and no PHT | 117 | 6.0 (1.0–16.0) | 5.0 (1.0–22.0) | 0.30 | −0.4 | 4.0 | −8.4 to 7.6 | 123 | 56 (60) | |
| Mild to moderate TI and/or PI and/or PHT | 73 | 6.0 (2.0–11.0) | 6.0 (1.0–19.0) | 0.48 | −0.7 | 3.3 | −7.3 to 5.9 | 103 | 46 (35) | |
| No Echo findings available | 221 | 6.0 (3.0–14.0) | 5.0 (1.0–21.0) | 0.04 | 0.2 | 4.7 | −9.2 to 9.6 | 145 | 54 (61) | |
| Exploratory additional examination influenceability by the height of intra-abdominal pressure (IAP) | ||||||||||
| IAP [mmHg] | <7 | 203 | 5.0 (1.0–6.0) | 3.0 (1.0–6.0) | 0.06 | 1.3 | 1.8 | −2.3 to 4.9 | 87 | 38 (42) |
| 7–9 | 153 | 7.0 (3.0–9.0) | 6.0 (1.0–9.0) | 0.08 | 1.6 | 3.0 | −4.4 to 7.6 | 94 | 30 (40) | |
| 10–12 | 49 | 8.0 (3.0–12.0) | 10.0 (2.0–12.0) | 0.45 | −1.1 | 4.7 | −10.5 to 8.3 | 107 | 64 (62) | |
| 13–15 | 27 | 8.0 (4.0–15.0) | 14.0 (12.0–15.0) | 0.01 | −5.0 | 2.8 | −10.6 to 0.6 | 50 | 73 (50) | |
| 16–18 | 16 | 8.0 (4.0–9.0) | 17.0 (16.0–18.0) | 0.00 | −9.9 | 1.8 | −13.4 to −6.3 | 30 | 152 (73) | |
| >16 | 11 | 6.0 (4.0–16.0) | 19.0 (19.0–22.0) | 0.68 | −12.2 | 2.5 | −17.2 to −6.7 | 37 | 199 (93) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gutting, M.; Klischke, L.; Kaussen, T. Hands off Trans-Femoral Venous Intra-Abdominal Pressure Estimates in Children: Results of a Sobering Single-Center Study. Life 2023, 13, 872. https://doi.org/10.3390/life13040872
Gutting M, Klischke L, Kaussen T. Hands off Trans-Femoral Venous Intra-Abdominal Pressure Estimates in Children: Results of a Sobering Single-Center Study. Life. 2023; 13(4):872. https://doi.org/10.3390/life13040872
Chicago/Turabian StyleGutting, Miriam, Lara Klischke, and Torsten Kaussen. 2023. "Hands off Trans-Femoral Venous Intra-Abdominal Pressure Estimates in Children: Results of a Sobering Single-Center Study" Life 13, no. 4: 872. https://doi.org/10.3390/life13040872
APA StyleGutting, M., Klischke, L., & Kaussen, T. (2023). Hands off Trans-Femoral Venous Intra-Abdominal Pressure Estimates in Children: Results of a Sobering Single-Center Study. Life, 13(4), 872. https://doi.org/10.3390/life13040872







