Hemorrhagic Fever with Renal Syndrome Patients Exhibit Increased Levels of Lipocalin-2, Endothelin-1 and NT-proBNP
Abstract
:1. Introduction
2. Materials and Methods
2.1. Test Subjects
2.2. Laboratory Measurements
2.3. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
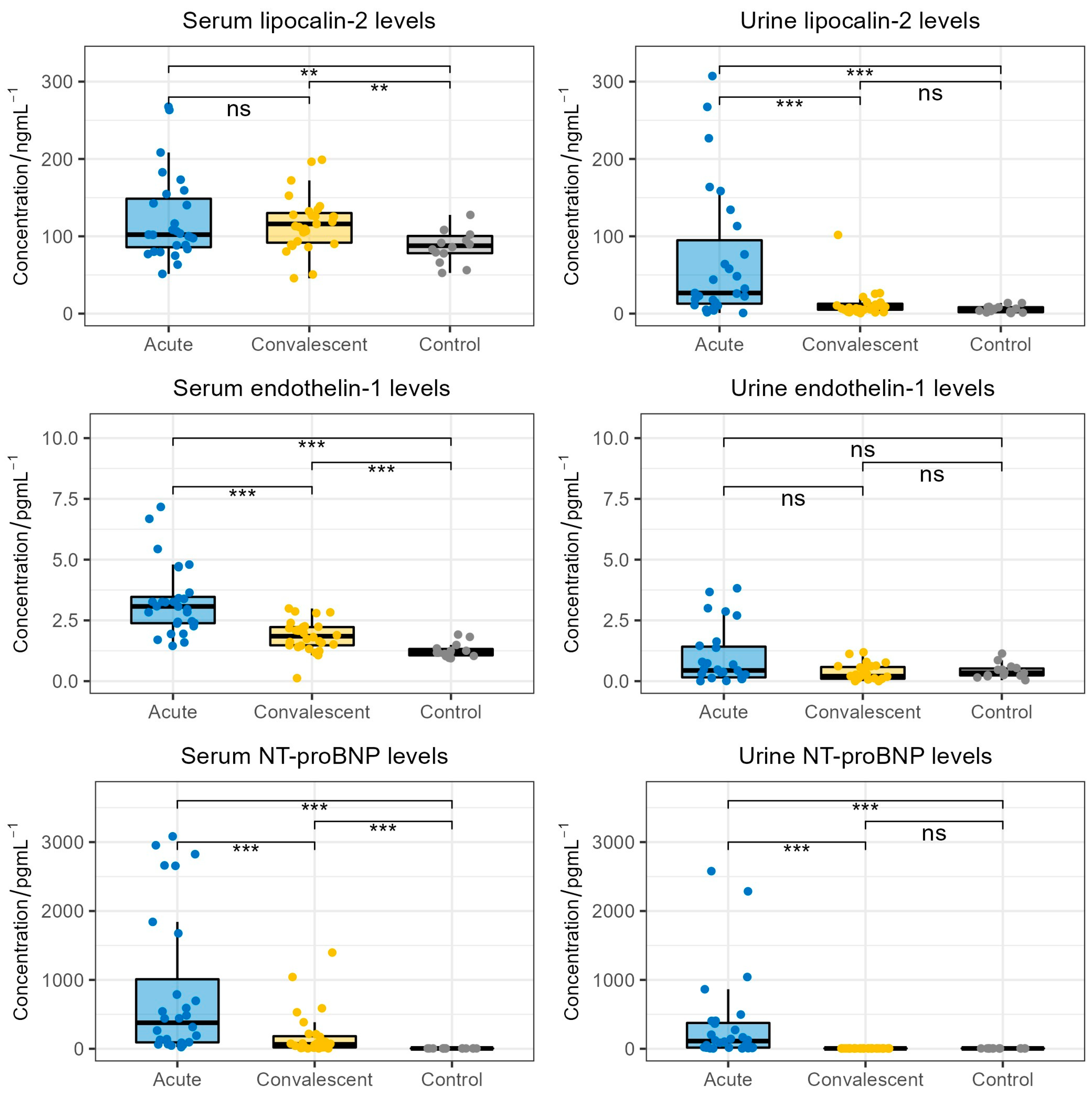
3.2. Lipocalin-2, Endothelin-1 and NT-proBNP Serum and Urine Levels in HFRS
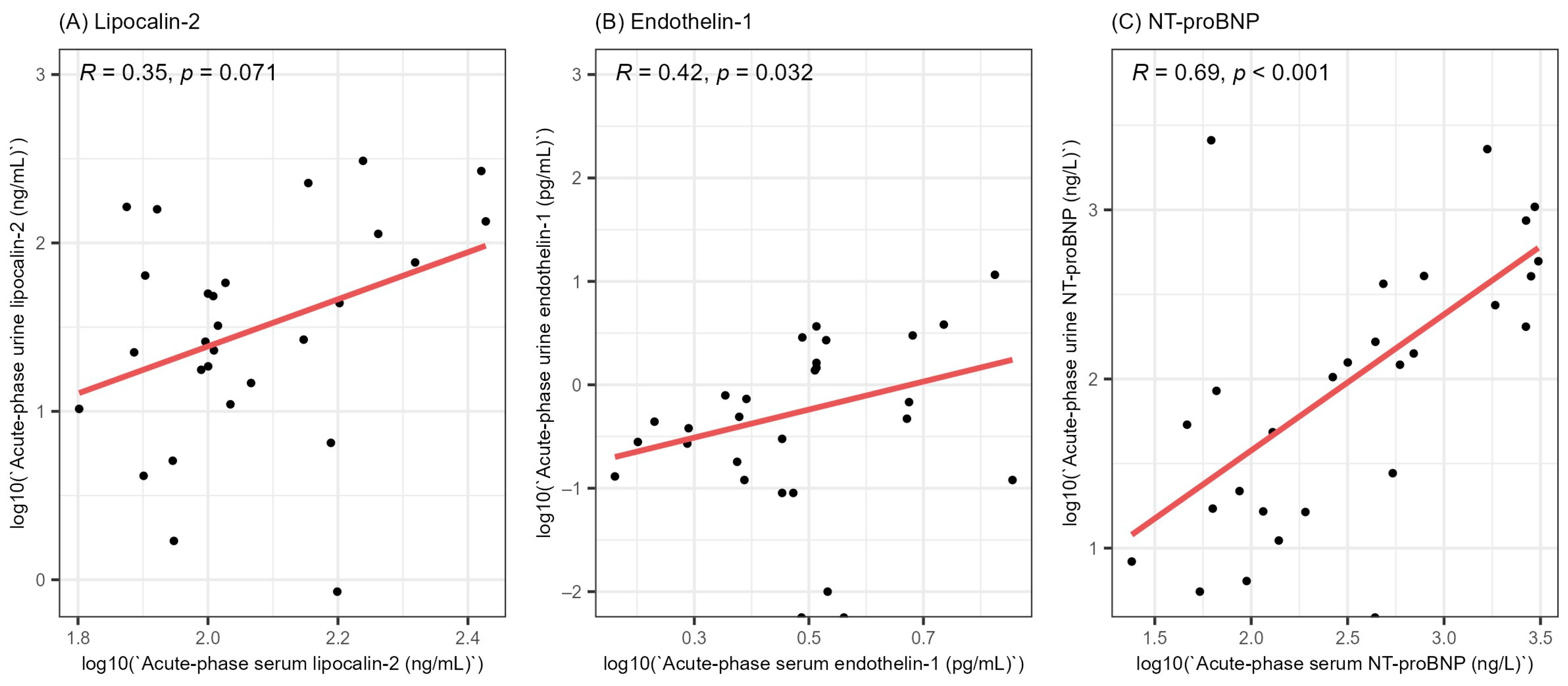
3.3. Correlation between Serum and Urine Levels of Lipocalin-2, Endothelin-1 and NT-proBNP
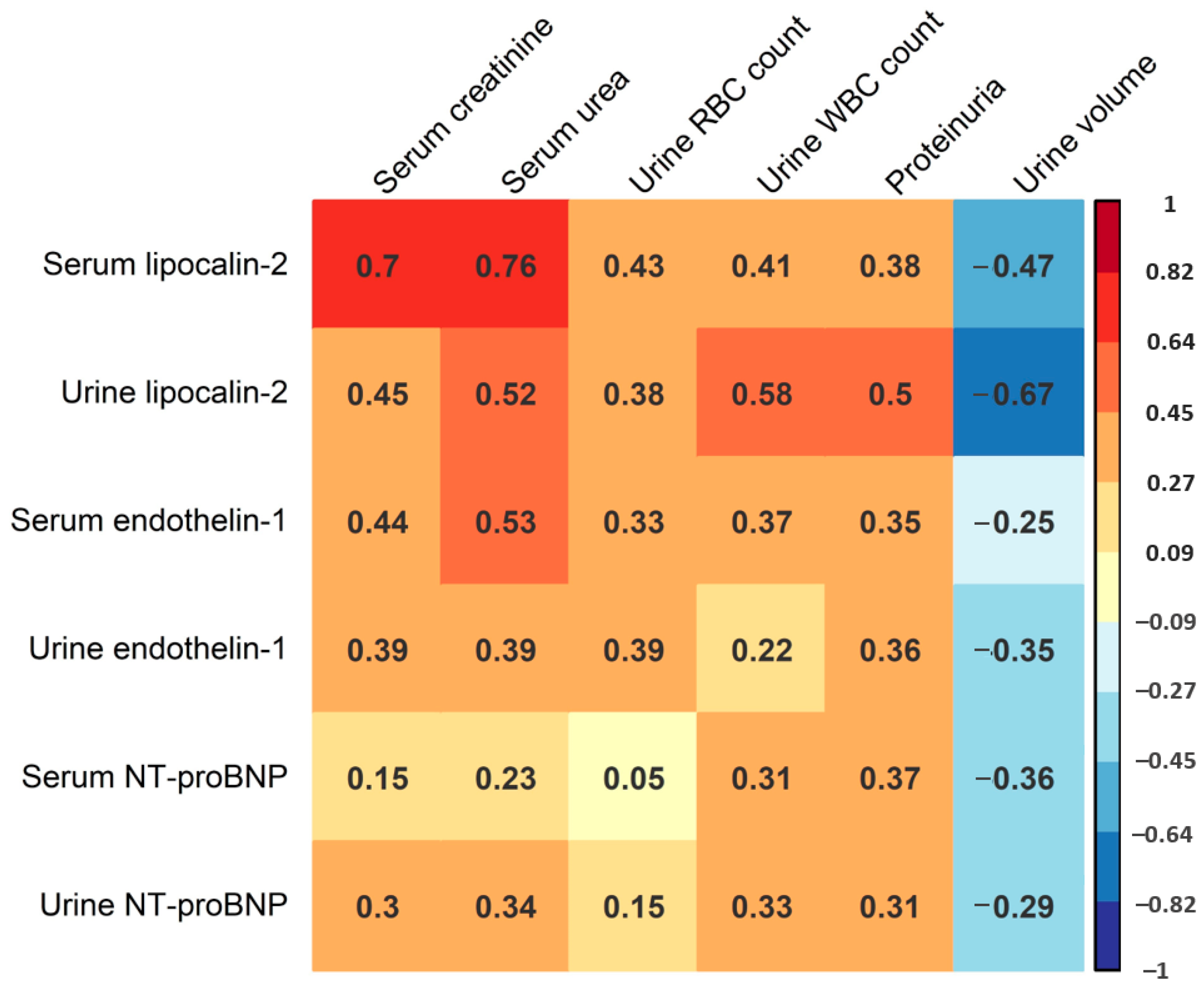
3.4. Correlation of Lipocalin-2, Endothelin-1 and NT-proBNP Levels with HFRS Severity
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vaheri, A.; Mills, J.N.; Spiropoulou, C.F.; Hjelle, B. Oxford Textbook of Zoonoses: Biology, Clinical Practice and Public Health Control, 2nd ed.; Oxford University Press: Oxford, UK, 2011; pp. 307–322. [Google Scholar]
- Jonsson, C.B.; Figueiredo, L.T.M.; Vapalahti, O. A global perspective on hantavirus ecology, epidemiology, and disease. Clin. Microbiol. Rev. 2010, 23, 412–441. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control. Annual Epidemiological Report 2016—Hantavirus Infection. Available online: http://ecdc.europa.eu/en/healthtopics/hantavirus/Pages/Annual-epidemiological-report-2016.aspx (accessed on 3 April 2021).
- Linderholm, M.; Elgh, F. Clinical Characteristics of Hantavirus Infections on the Eurasian Continent. In Hantaviruses. Current Topics in Microbiology and Immunology, 1st ed.; Schmaljohn, C.S., Nichol, S.T., Eds.; Springer: Berlin/Heidelberg, Germany, 2001; Volume 256, pp. 135–153. [Google Scholar]
- Papa, A. Dobrava-Belgrade virus: Phylogeny, epidemiology, disease. Antivir. Res. 2012, 95, 104–117. [Google Scholar] [CrossRef] [PubMed]
- Turčinov, D.; Puljiz, I.; Markotić, A.; Kuzman, I.; Begovac, J. Clinical and laboratory findings in patients with oliguric and non-oliguric Hantavirus haemorrhagic fever with renal syndrome: An analysis of 128 patients. Clin. Microbiol. Infect. 2013, 19, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Huttunen, N.P.; Mäkelä, S.; Pokka, T.; Mustonen, J.; Uhari, M. Systematic literature review of symptoms, signs and severity of serologically confirmed nephropathia epidemica in paediatric and adult patients. Scand. J. Infect. Dis. 2011, 43, 405–410. [Google Scholar] [CrossRef]
- Markotić, A.; Nichol, S.T.; Kuzman, I.; Sanchez, A.J.; Ksiazek, T.G.; Gagro, A.; Rabatić, S.; Zgorelec, R.; Avšić-Županc, I.; Beus, I.; et al. Characteristics of Puumala and Dobrava infections in Croatia. J. Med. Virol. 2002, 66, 542–551. [Google Scholar] [CrossRef]
- Mustonen, J.; Brummer-Korvenkontio, M.; Hedman, K.; Pasternack, A.; Pietilä, K.; Vaheri, A. Nephropathia epidemica in Finland: A retrospective study of 126 cases. Scand. J. Infect. Dis. 1994, 26, 7–13. [Google Scholar] [CrossRef]
- Kanerva, M.; Mustonen, J.; Vaheri, A. Pathogenesis of Puumala and other hantavirus infections. Rev. Med. Virol. 1998, 8, 67–86. [Google Scholar] [CrossRef]
- Temonen, M.; Mustonen, J.; Helin, H.; Pasternack, A.; Vaheri, A.; Holthöfer, H. Cytokines, adhesion molecules, and cellular infiltration in nephropathia epidemica kidneys: An immunohistochemical study. J. Clin. Immunol. Immunopathol. 1996, 78, 47–55. [Google Scholar] [CrossRef]
- Linderholm, M.; Ahlm, C.; Settergren, B.; Waage, A.; Tärnvik, A. Elevated plasma levels of tumor necrosis factor (TNF)-α, soluble TNF receptors, interleukin (IL)-6, and IL-10 in patients with hemorrhagic fever with renal syndrome. J. Infect. Dis. 1996, 173, 38–43. [Google Scholar] [CrossRef]
- Sadeghi, M.; Eckerle, I.; Daniel, V.; Burkhardt, U.; Opelz, G.; Schnitzler, P. Cytokine expression during early and late phase of acute Puumala hantavirus infection. BMC Immunol. 2001, 12, 65. [Google Scholar] [CrossRef]
- Bunz, H.; Weyrich, P.; Peter, A.; Baumann, D.; Tschritter, O.; Guthoff, M.; Beck, R.; Jahn, G.; Artunc, F.; Häring, H.U.; et al. Urinary Neutrophil Gelatinase-Associated Lipocalin (NGAL) and proteinuria predict severity of acute kidney injury in Puumala virus infection. BMC Infect. Dis. 2015, 15, 464. [Google Scholar] [CrossRef]
- Helanova, K.; Spinar, J.; Parenica, J. Diagnostic and prognostic utility of Neutrophil Gelatinase-Associated Lipocalin (NGAL) in patients with cardiovascular diseases—Review. Kidney Blood. Press. Res. 2014, 39, 623–629. [Google Scholar] [CrossRef] [PubMed]
- Mishra, J.; Qing, M.A.; Prada, A.; Mitsnefes, M.; Zahedi, K.; Yang, J.; Barasch, J.; Devarajan, P. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J. Am. Soc. Nephrol. 2003, 14, 2534–2543. [Google Scholar] [CrossRef] [PubMed]
- Grigoryev, D.N.; Liu, M.; Hassoun, H.T.; Cheadle, C.; Barnes, K.C.; Rabb, H. The local and systemic inflammatory transcriptome after acute kidney injury. J. Am. Soc. Nephrol. 2008, 19, 547–558. [Google Scholar] [CrossRef]
- Davenport, A.P.; Hyndman, K.A.; Dhaun, N.; Southan, C.; Kohan, D.E.; Pollock, J.S.; Pollock, D.M.; Webb, D.J.; Maguire, J.J. Endothelin. Pharmacol. Rev. 2016, 68, 357–418. [Google Scholar] [CrossRef] [PubMed]
- Nambi, P. Endothelin and the kidney. Adv. Organ. Biol. 2000, 9, 207–218. [Google Scholar]
- Barton, M. Therapeutic potential of endothelin receptor antagonists for chronic proteinuric renal disease in humans. Biochim. Biophys. Acta. Mol. Basis. Dis. 2010, 1802, 1203–1213. [Google Scholar] [CrossRef]
- Zager, R.A.; Johnson, A.C.; Adress, D.; Becker, K. Progressive endothelin-1 gene activation initiates chronic/end stage renal disease following experimental ischemic-reperfusion injury. Kidney Int. 2013, 84, 703–712. [Google Scholar] [CrossRef]
- Zymliński, R.; Sierpiński, R.; Metra, M.; Cotter, G.; Sokolski, M.; Siwołowski, P.; Garus, M.; Gajewski, P.; Trba, J.; Samorek, M.; et al. Elevated plasma endothelin-1 is related to low natriuresis, clinical signs of congestion, and poor outcome in acute heart failure. ESC Heart Fail. 2020, 7, 3536–3544. [Google Scholar] [CrossRef]
- Forslund, T.; Liisanantti, R.; Saijonmaa, O.; Fyhrquist, F. Raised plasma endothelin-1 concentration in patients with nephropathia epidemica. Clin. Nephrol. 1993, 40, 69–73. [Google Scholar]
- Tagore, R.; Ling, L.H.; Yang, H.; Daw, H.Y.; Chan, Y.H.; Sethi, S.K. Natriuretic peptides in chronic kidney disease. Clin. J. Am. Soc. Nephrol. 2008, 3, 1644–1651. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, X.; Xiao, W.; Liu, Y.; Wu, H.; Ye, P.; Sheng, L. NT-proBNP is associated with age, gender and glomerular filtration rate in a community-dwelling population. Int. J. Clin. Exp. Med. 2019, 12, 12220–12227. [Google Scholar]
- Palmer, S.C.; Endre, Z.H.; Richards, A.M.; Yandle, T.M. Characterization of NT-proBNP in human urine. Clin. Chem. 2009, 55, 1126–1134. [Google Scholar] [CrossRef]
- Rajaniemi, S.M.; Hautala, N.; Sironen, T.; Vainio, O.; Vapalahti, O.; Vaheri, A.; Vuolteenaho, O.; Ruskoaho, H.; Kauma, H.; Hautala, T. Plasma B-type natriuretic peptide (BNP) in acute Puumala hantavirus infection. Ann. Med. 2014, 46, 38–43. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 23 June 2022).
- Michielsen, E.C.H.J.; Bakker, J.A.; Van Kimmenade, R.R.J.; Pinto, Y.M.; Van Dieijen-Visser, M.P. The diagnostic value of serum and urinary NT-proBNP for heart failure. Ann. Clin. Biochem. 2008, 45, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.H.; He, X.J.; Chen, S.R.; Wang, L.; Li, E.M.; Xu, L.Y. Changes of serum and urine neutrophil gelatinase-associated lipocalin in type-2 diabetic patients with nepropathy: One year observational follow-up study. Endocr 2009, 36, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Dhaun, N.; Lilitkarntakul, P.; Macintyre, I.M.; Muilwijk, E.; Jonhston, N.R.; Kluth, D.C.; Webb, D.J.; Goddard, J. Urinary endothelin-1 in chronic kidney disease and as a marker of disease activity in lupus nephritis. Am. J. Physiol. Renal Physiol. 2009, 296, 1477–1483. [Google Scholar] [CrossRef]
| Parameter | Number of Patients (%, 95% CI) | ||
| Fever | 28 (100.0, 87.7–100.0) | ||
| Headache | 27 (96.4, 81.7–100.0) | ||
| Proteinuria | 25 (89.3, 71.8–97.8) | ||
| Myalgia | 25 (89.3, 71.8–97.8) | ||
| Nausea | 19 (67.9, 47.7–84.1) | ||
| ECG abnormalities | 17 (60.7, 40.6–78.5) | ||
| Hepatomegaly | 15 (53.6, 33.9–72.5) | ||
| Abdominal pain | 11 (39.3, 21.5–59.4) | ||
| Hyperpyrexia | 8 (28.6, 13.3–48.7) | ||
| Hypotension | 6 (21.4, 8.3–41.0) | ||
| Oliguria | 3 (10.7, 2.3–28.2) | ||
| Parameter | Median | IQR | Range |
| Length of hospitalization (days) | 12.5 | 10–14 | 8–23 |
| Duration of fever (days) | 7 | 5.75–8 | 4–13 |
| Day of disease of acute-phase sample collection | 5 | 4–6.25 | 3–11 |
| Day of disease of convalescent-phase sample collection | 17.5 | 15.75–19.25 | 12–27 |
| Maximal serum RBC count (×1012/L) | 5.05 | 4.6–5.3 | 3.90–6.13 |
| Minimal platelet count (×109/L) | 48.50 | 35.5–67.25 | 16.01–166.02 |
| Maximal sedimentation rate (mm/h) | 35 | 27–50.25 | 10–68 |
| Maximal serum WBC count (×109/L) | 11.20 | 8.85–12.75 | 6.22–23.37 |
| Maximal CRP (mg/L) | 80.5 | 48.75–122.5 | 20.0–178.0 |
| Maximal creatinine (µmol/L) | 269 | 146–374.5 | 82–1238 |
| Maximal urea (mmol/L) | 13.6 | 8.25–18.05 | 4.6–35.1 |
| Minimal urine volume (mL/day) | 1050 | 600–1400 | 0–1650 |
| Maximal urine RBC count (RBC/HPF) | 10 | 5–15 | 1–30 |
| Maximal urine WBC count (WBC/HPF) | 5.5 | 2–10 | 2–30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cvetko Krajinović, L.; Bodulić, K.; Laškaj, R.; Žibrat, B.; Svoboda Karić, P.; Kurolt, I.-C.; Kordun, M.; Topić, A.; Čivljak, R.; Skuhala, T.; et al. Hemorrhagic Fever with Renal Syndrome Patients Exhibit Increased Levels of Lipocalin-2, Endothelin-1 and NT-proBNP. Life 2023, 13, 2189. https://doi.org/10.3390/life13112189
Cvetko Krajinović L, Bodulić K, Laškaj R, Žibrat B, Svoboda Karić P, Kurolt I-C, Kordun M, Topić A, Čivljak R, Skuhala T, et al. Hemorrhagic Fever with Renal Syndrome Patients Exhibit Increased Levels of Lipocalin-2, Endothelin-1 and NT-proBNP. Life. 2023; 13(11):2189. https://doi.org/10.3390/life13112189
Chicago/Turabian StyleCvetko Krajinović, Lidija, Kristian Bodulić, Renata Laškaj, Branka Žibrat, Petra Svoboda Karić, Ivan-Christian Kurolt, Mihaela Kordun, Antea Topić, Rok Čivljak, Tomislava Skuhala, and et al. 2023. "Hemorrhagic Fever with Renal Syndrome Patients Exhibit Increased Levels of Lipocalin-2, Endothelin-1 and NT-proBNP" Life 13, no. 11: 2189. https://doi.org/10.3390/life13112189
APA StyleCvetko Krajinović, L., Bodulić, K., Laškaj, R., Žibrat, B., Svoboda Karić, P., Kurolt, I.-C., Kordun, M., Topić, A., Čivljak, R., Skuhala, T., & Markotić, A. (2023). Hemorrhagic Fever with Renal Syndrome Patients Exhibit Increased Levels of Lipocalin-2, Endothelin-1 and NT-proBNP. Life, 13(11), 2189. https://doi.org/10.3390/life13112189










