Depressive Disorders, Cognitive and Physical Function of Older People in Early Dementia Detection
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Desing and Procedure
2.3. Instruments
2.4. Statistical Analysis
3. Results
3.1. Characteristics of the Study Group
3.2. Spearman Correlation Test
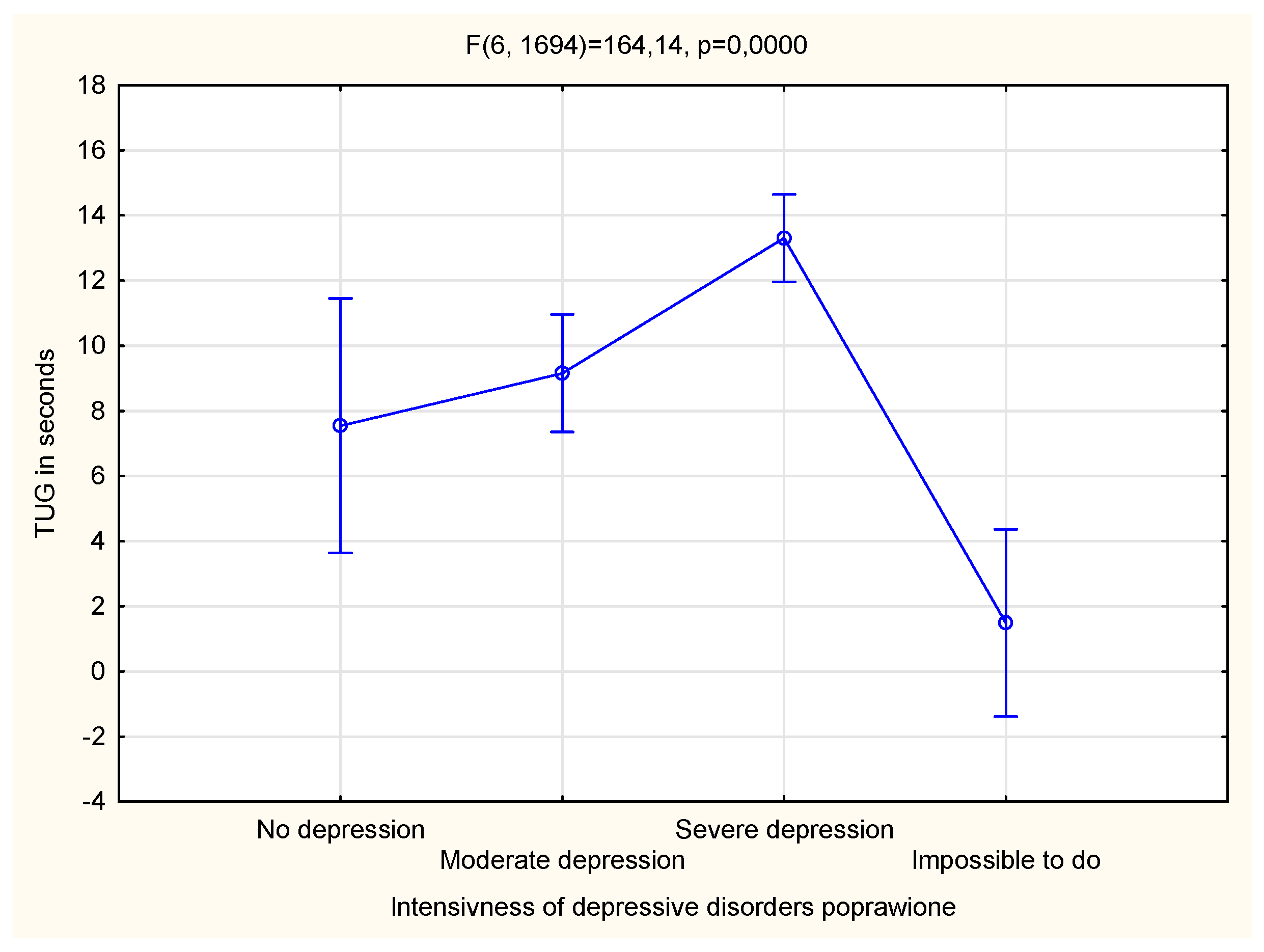
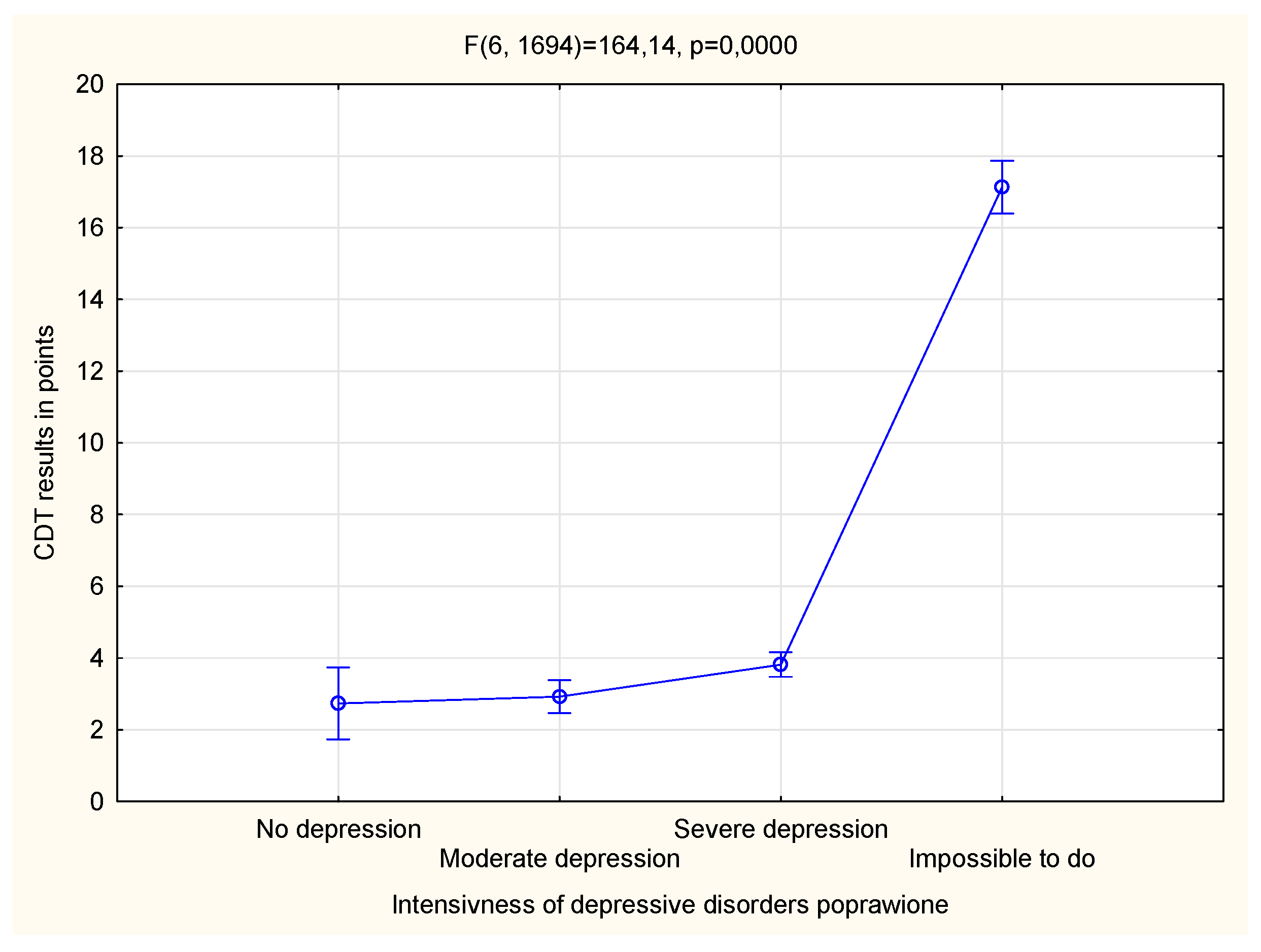
3.3. Relationship between the Level of Depressive Disorders and Cognitive and Physical Function
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rasiñska, R.; Nowakowska, I. Obraz ludzi starszych w raportach i zestawieniach. Now. Lek. 2012, 81, 84–88. [Google Scholar]
- Gallou-Guyot, M.; Mandigout, S.; Combourieu-Donnezan, L.; Bherer, L.; Perrochon, A. Cognitive and physical impact of cognitive-motor dual-task training in cognitively impaired older adults: An overview. Neurophysiol. Clin. 2020, 50, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Reher, D.S. Baby booms, busts, and population aging in the developed world. Popul. Stud. 2015, 69, S57–S68. [Google Scholar] [CrossRef] [PubMed]
- Wright, A.E.H.; Harrell, H.E. Physical Examination in the Evaluation of Dementia. Med. Clin. N. Am. 2022, 106, 471–482. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.M.; Cohen, A.; Ein-Mor, E.; Maaravi, Y.; Stessman, J.E. Frailty, cognitive impairment and mortality among the oldest old. J. Nutr. Health Aging 2011, 15, 678–682. [Google Scholar] [CrossRef] [PubMed]
- Johnson, N.E. The racial crossover in comorbidity, disability, and mortality. Demography 2000, 37, 267–283. [Google Scholar] [CrossRef]
- Ávila-Funes, J.A.; Amieva, H.; Barberger-Gateau, P.; Le Goff, M.; Raoux, N.; Ritchie, K.; Carrière, I.; Tavernier, B.; Tzourio, C.; Gutiérrez-Robledo, L.M.; et al. Cognitive impairment improves the predictive validity of the phenotype of frailty for adverse health outcomes: The Three-City Study. J. Am. Geriatr. Soc. 2009, 57, 453–461. [Google Scholar] [CrossRef]
- Montero-Odasso, M.M.; Barnes, B.; Speechley, M.; Muir Hunter, S.W.; Doherty, T.J.; Duque, G.; Gopaul, K.; Sposato, L.A.; Casas-Herrero, A.; Borrie, M.J.; et al. Disentangling cognitive-frailty Results from the Gait and Brain Study. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 1476–1482. [Google Scholar] [CrossRef]
- McGough, E.L.; Cochrane, B.B.; Pike, K.C.; Logsdon, R.G.; McCurry, S.M.; Teri, L. Dimensions of physical frailty and cognitive function in older adults with amnestic mil cognitive impairment. Ann. Phys. Reabil. Med. 2013, 56, 329–341. [Google Scholar] [CrossRef]
- Brach, J.S.; Van Swearingen, J.M.; Newman, A.B.; Kriska, A.M. Identifying early decline of physical function in community-dwelling older women: Performance-based and self-report measures. Phys. Ther. 2002, 82, 320–328. [Google Scholar] [CrossRef]
- Dong, X.; Chang, E.S.; Wong, E.; Wong, B.; Skarupski, K.A.; Simon, M.A. Assessing the Health Needs of Chinese Older Adults: Findings from a Community-Based Participatory Research Study in Chicago’s Chinatown. J. Aging Res. 2011, 2010, 124246. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Chang, E.S.; Wong, E.; Simon, M. The perceptions, social determinants, and negative health outcomes associated with depressive symptoms among U.S. Chinese older adults. Gerontologist 2012, 52, 650–663. [Google Scholar] [CrossRef] [PubMed]
- Robertson, D.A.; Savva, G.M.; Kenny, R.A. Frailty and cognitive impairment—A review of the evidence and causal mechanisms. Ageing Res. Rev. 2013, 12, 840–851. [Google Scholar] [CrossRef]
- Wdowiak, L.; Ćwikła, S.; Bojar, I.; Kapka, L.; Woźnica, I. Starość jako problem społeczno—Demograficzny oraz zdrowotny. Med. Ogólna 2009, 15, 451–462. [Google Scholar]
- Callegari, C.; Bertù, L.; Caselli, I.; Isella, C.; Ielmini, M.; Bonalumi, C.; Ferrario, M.; Vender, S. Resilience in older adults: Influence of the admission in nursing home and psychopathology. Neuropsychiatry 2016, 6, 117–123. [Google Scholar] [CrossRef]
- Panella, L.; Incorvaia, C.; Caserta, A.V.; Amata, O.; Consonni, D.; Pessina, L.; Leo, G.; Caselli, I.; Callegari, C. A bio-psycho-social approach in elderly population: Outcome of adapted physical activity in patients with osteoarthritis. Clin. Ter. 2019, 1, e74–e77. [Google Scholar]
- McPhee, J.S.; French, D.P.; Jackson, D.; Nazroo, J.; Pendleton, N.; Degens, H. Physical activity in older age: Perspectives for healthy ageing and frailty. Biogerontology 2016, 17, 567–580. [Google Scholar] [CrossRef]
- Starczewska, M.E.; Prociak, L.; Rybicka, A.; Stanisławska, M.; Grochans, E. Ocena sprawności funkcjonalnej i występowania ryzyka depresji wśród seniorów. Pol. Nurs. Pielegniarstwo Pol. 2019, 73, 258–264. [Google Scholar]
- Gureje, O.; Ogunniyi, A.; Kola, L.; Afolabi, E. Functional disability in elderly Nigerians: Results from the Ibadan Study of Aging. J. Am. Geriatr. Soc. 2006, 54, 1784–1789. [Google Scholar] [CrossRef]
- Liang, J.; Wang, C.N.; Xu, X.; Hsu, H.C.; Lin, H.S.; Lin, Y.H. Trajectory of functional status among older Taiwanese: Gender and age variations. Soc. Sci. Med. 2010, 71, 1208–1217. [Google Scholar] [CrossRef]
- Chen, S.W.; Chippendale, T. Factors associated with IADL independence: Implications for OT practice. Scand. J. Occup. Ther. 2017, 24, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Wysokiński, M.; Fidecki, W.; Gębala, S. Ocena samodzielności osób starszych hospitalizowanych na oddziałach internistycznych. Gerontol. Pol. 2013, 21, 89–97. [Google Scholar]
- Teixeira-Leite, H.; Manhães, A.C. Association between functional alterations of senescence and senility and disorders of gait and balance. Clinics 2012, 67, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Giannouli, V.; Stamovlasis, D.; Tsolaki, M. Exploring the role of cognitive factors in a new instrument for elders’ financial capacity assessment. J. Alzheimer’s Dis. 2018, 62, 1579–1594. [Google Scholar] [CrossRef] [PubMed]
- Giannouli, V.; Tsolaki, M. Mild Alzheimer Disease, financial capacity, and the role of depression: Eyes wide shut? Alzheimer Dis. Assoc. Disord. 2021, 35, 360–362. [Google Scholar] [CrossRef] [PubMed]
- Giannouli, V.; Tsolaki, M. Vascular dementia, depression, and financial capacity assessment. Alzheimer Dis. Assoc. Disord. 2021, 35, 84–87. [Google Scholar] [CrossRef]
- Giannouli, V.; Tsolaki, M. Are left angular gyrus and amygdala volumes important for financial capacity in mild cognitive impairment? Hell. J. Nucl. Med. 2019, 22, 160–164. [Google Scholar]
- Giannouli, V.; Tsolaki, M. Unraveling Ariadne’s Thread Into the Labyrinth of aMCI: Depression and Financial Capacity. Alzheimer Dis. Assoc. Disord. 2021, 35, 363–365. [Google Scholar] [CrossRef]
- Giannouli, V.; Tsolaki, M. Beneath the Top of the Iceberg: Financial Capacity Deficits in Mixed Dementia with and without Depression. Healthcare 2023, 11, 505. [Google Scholar] [CrossRef]
- Maqsood, F.; Flatt, J.D.; Albert, S.M.; Maqsood, S.; Nizamuddin, M. Correlates of self-reported depressive symptoms: A study of older persons of Punjab, Pakistan. J. Cross Cult. Gerontol. 2013, 28, 65–74. [Google Scholar] [CrossRef][Green Version]
- Broczek, K.; Mossakowska, M.; Szybalska, A.; Kozak-Szkopek, E.; Ślusarczyk, P.; Wieczorkowska-Tobis, K.; Parnowski, T. Występowanie objawów depresyjnych u osób starszych. In Aspekty Medyczne, Psychologiczne, Socjologiczne i Ekonomiczne Starzenia Się Ludzi w Polsce; Mossakowska, M., Więcek, A., Błędowski, P., Eds.; Termedia: Poznan, Poland, 2012; pp. 123–136. [Google Scholar]
- Busch, T.A.; Duarte, Y.A.; Nunes, D.P.; Lebrão, M.L.; Naslavsky, M.S.; dos Santos Rodrigues, A.; Amaro, E., Jr. Factors associated with lower gait speed among the elderly living in a developing country: A cross-sectional population-based study. BMC Geriatr. 2015, 15, 35. [Google Scholar] [CrossRef] [PubMed]
- Domańska, Ł. Depresja wieku podeszłego–wyzwania diagnostyczne. Ann. Univ. Mariae Curie Skłodowska Sect. J. Paedagog. Psychol. 2019, 31, 327–338. [Google Scholar] [CrossRef]
- Bidzan, L. Depresyjne zaburzenia nastroju u osób w wieku podeszłym. Med. Wieku Podeszłego 2011, 1, 31–41. [Google Scholar]
- Rzewuska, M. Leczenie zaburzeń psychicznych. Wydaw. Lek. PZWL 2003, 257–264. [Google Scholar]
- Piwoński, J.; Piwońska, A.; Głuszek, J.; Bielecki, W.; Pająk, A.; Kozakiewicz, K.; Wyrzykowski, B.; Rywik, S. Ocena częstości występowania niskiego poziomu wsparcia społecznego oraz objawów depresji w populacji polskiej. Wyniki Programu WOBASZ Kardiol. Pol. 2005, 63, 645–648. [Google Scholar]
- Sekhon, S.; Patel, J.; Sapra, A. Late-Life Depression. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Shin, J.M.; Sims, R.C.; Bradley, D.L.; Pohlig, R.T.; Harrison, B.E. Prevalence of depressive symptoms and associated factorsin older adult public housing residents. Res. Gerontol. Nurs. 2014, 7, 249–255. [Google Scholar] [CrossRef]
- Bhamani, M.A.; Karim, M.S.; Khan, M.M. Depression in the elderly in Karachi, Pakistan: A cross sectional study. BMC Psychiatry 2013, 13, 181. [Google Scholar] [CrossRef]
- Płaszewska-Żywko, L.; Brzuzan, P.; Malinowska-Lipień, I.; Gabryś, T. Sprawność funkcjonalna u osób w wieku podeszłym w domach pomocy społecznej. Probl. Hig. Epidemiol. 2008, 89, 62–66. [Google Scholar]
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, C.; Banerjee, S.; Burns, A.; Cohen-Mansfield, J.; et al. Dementia prevention, intervention, and care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef]
- Zou, C.; Yu, Q.; Wang, C.; Ding, M.; Chen, L. Association of depression with cognitive frailty: A systematic review and meta-analysis. J. Affect. Disord. 2023, 320, 133–139. [Google Scholar] [CrossRef]
- Perini, G.; Cotta Ramusino, M.; Sinforiani, E.; Bernini, S.; Petrachi, R.; Costa, A. Cognitive impairment in depression: Recent advances and novel treatments. Neuropsychiatr. Dis. Treat. 2019, 15, 1249–1258. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.; Zhao, F.; You, L.; Giorgetta, C.D.V.; Sarkhel, S.; Prakash, R. Pseudo-dementia: A neuropsychological review. Ann. Indian Acad. Neurol. 2014, 17, 147–154. [Google Scholar] [PubMed]
- Mirza, S.S.; de Bruijn, R.F.A.G.; Direk, N.; Hofman, A.; Peter, J.; Koudstaal, P.J.; Ikram, M.A.; Tiemeier, H. Depressive symptoms predict incident dementia during short- but not long-term follow-up period. Alzheimer’s Dement. 2014, 10, S323–S329. [Google Scholar] [CrossRef] [PubMed]
- Steffens, D.C.; Skoog, I.; Norton, M.C.; Hart, A.D.; Tschanz, J.T.; Plassman, B.L.; Wyse, B.W.; Welsh-Bohmer, K.A.; Breitner, J.C. Prevalence of depression and its treatment in an elderly population. The Cache County Study. Arch. Gen. Psychiatry 2000, 57, 601–607. [Google Scholar] [CrossRef]
- Weterle, K.; Sołtysiak, J. Objawy depresji i ich wykrywalność przez lekarzy podstawowej opieki zdrowotnej u pacjentów po 65. roku życia. Now. Lek. 2006, 75, 433–437. [Google Scholar]
- The National Health Fund Organization. The Order of the President of the National Health Fund of 3 January 2022 on Defining the Conditions for Concluding and Implementing Contracts such as Hospital Treatment and Hospital Treatment—Highly Specialized Services. Available online: https://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-32022dsoz,7476.html (accessed on 3 August 2023).
- Pedraza, O.; Dotson, V.M.; Willis, F.B.; Graff-Radford, N.R.; Lucas, J.A. Internal Consistency and Test-Retest Stability of the Geriatric Depression Scale-Short Form in African American Older Adults. J. Psychopathol. Behav. Assess. 2009, 31, 412–416. [Google Scholar] [CrossRef]
- Kroemeke, A. Perceived Autonomy in Old Age scale: Factor structure and psychometric properties of the Polish adaptation. Psychiatr. Pol. 2015, 49, 107–117. [Google Scholar] [CrossRef]
- Shulman, K.I.; Gold, D.P.; Cohen, C.A.; Zucchero, C.A. Clock-drawing and dementia in the community: A longitudinal study. Int. J. Geriatr. Psychiatry 1993, 8, 487–496. [Google Scholar] [CrossRef]
- Gale, S.A.; Acar, D.; Daffner, K.R. Dementia. Am. J. Med. 2018, 131, 1161–1169. [Google Scholar] [CrossRef]
- World Health Organization. Risk Reduction of Cognitive Decline and Dementia: WHO Guidelines. 2019. Available online: https://www.who.int/publications/i/item/9789241550543 (accessed on 3 August 2023).
- World Health Organization. Dementia. Available online: https://www.who.int/health-topics/dementia#tab=tab_3 (accessed on 3 August 2023).
- Swedish Council on Health Technology Assessment. Dementia—Caring, Ethics, Ethnical and Economical Aspects: A Systematic Review; SBU Assessment No. 172; Swedish Council on Health Technology Assessment (SBU): Stockholm, Sweden, 2008. [Google Scholar]
- Kasa, A.S.; Lee, S.C.; Chang, H.R. Prevalence and factors associated with depression among older adults in the case of a low-income country, Ethiopia: A systematic review and meta-analysis. BMC Psychiatry 2022, 22, 675. [Google Scholar] [CrossRef]
- Fernández Martínez, M.; Castro Flores, J.; Pérez de Las Heras, S.; Mandaluniz Lekumberri, M.; Gordejuela Menocal, M.; Zarranz Imirizaldu, J.J. Risk factors for dementia in the epidemiological study of Munguialde County (Basque Country-Spain). BMC Neurol. 2008, 8, 39. [Google Scholar] [CrossRef] [PubMed]
- Rajtar-Zembaty, A.; Sałakowski, A.; Rajtar-Zembaty, J.; Starowicz-Filip, A. Executive dysfunction in late-life depression. Psychiatr. Pol. 2017, 51, 705–718. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Jin, Y.; Liu, R.; Zhang, Q.; Su, Z.; Ungvari, G.S.; Tang, Y.L.; Ng, C.H.; Li, X.H.; Xiang, Y.T. Global prevalence of depression in older adults: A systematic review and meta-analysis of epidemiological surveys. Asian J. Psychiatr. 2023, 80, 103417. [Google Scholar] [CrossRef] [PubMed]
- Babiarczyk, B.; Schlegel-Zawadzka, M.; Turbiarz, A. Ocena częstości występowania objawów depresji w populacji osób powyżej 65 roku życia. Med. Og. Nauk. Zdr. 2013, 19, 453–457. [Google Scholar]
- Han, Y.F.; Yang, Y.T.; Fang, Y. Association between depression tendency and cognitive trajectory in the elderly in rural area in China. Zhonghua Liu Xing Bing Xue Za Zhi 2022, 43, 1491–1496. (In Chinese) [Google Scholar] [CrossRef]
- Chippa, V.; Roy, K. Geriatric Cognitive Decline and Polypharmacy; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Reppermund, S.; Brodaty, H.; Crawford, J.D.; Kochan, N.A.; Slavin, M.J.; Trollor, J.N.; Draper, B.; Sachdev, P.S. The relationship of current depressive symptoms and past depression with cognitive impairment and instrumental activities of daily living in an elderly population: The Sydney Memory and Ageing Study. J. Psychiatr. Res. 2011, 45, 1600–1607. [Google Scholar] [CrossRef]
- Hesseberg, K.; Bentzen, H.; Ranhoff, A.H.; Engedal, K.; Bergland, A. Physical Fitness in Older People with Mild Cognitive Impairment and Dementia. J. Aging Phys. Act. 2016, 24, 92–100. [Google Scholar] [CrossRef]
- Li, R.; Singh, M. Sex differences in cognitive impairment and Alzheimer’s disease. Front. Neuroendocrinol. 2014, 35, 385–403. [Google Scholar] [CrossRef]
- Doraiswamy, P.M.; Bieber, F.; Kaiser, L.; Krishnan, K.R.; Reuning-Scherer, J.; Gulanski, B. The Alzheimer’s Disease Assessment Scale: Patterns and predictors of baseline cognitive performance in multicenter Alzheimer’s disease trials. Neurology 1997, 48, 1511–1517. [Google Scholar] [CrossRef]
- Pitts, B.L.; Wen, V.; Whealin, J.M.; Fogle, B.M.; Southwick, S.M.; Esterlis, I.; Pietrzak, R.H. Depression and cognitive dysfunction in older U.S. military veterans: Moderating effects of BDNF Val66Met polymorphism and physical exercise. Am. J. Geriatr. Psychiatry 2020, 28, 959–967. [Google Scholar] [CrossRef]
- Bellou, V.; Belbasis, L.; Tzoulaki, I.; Middleton, L.T.; Ioannidis, J.P.; Evangelou, E. Systematic evaluation of the associations between environmental risk factors and dementia: An umbrella review of systematic reviews and meta-analyses. Alzheimers Dement. 2017, 13, 406–418. [Google Scholar] [CrossRef] [PubMed]
- van Milligen, B.A.; Vogelzangs, N.; Smit, J.H.; Penninx, B.W. Physical function as predictor for the persistence of depressive and anxiety disorders. J. Affect. Disord. 2012, 136, 828–832. [Google Scholar] [CrossRef] [PubMed]
| ALL | MALES | FEMALES | |
|---|---|---|---|
| N (%) | |||
| GDS | |||
| No depression | 452 (52.99) * | 177 (57.65) * | 275 (50.37) * |
| Moderate depression | 250 (29.31) * | 84 (27.36) * | 166 (30.40) * |
| Severe depression | 53 (6.21) | 15 (4.88) | 38 (6.96) |
| Impossible to do | 98 (11.49) | 31 (10.10) | 67 (12.27) |
| IADL | |||
| Severe disability | 255 (29.89) * | 88 (28.66) | 167 (30.59) |
| Moderate disability | 146 (17.12) | 49 (15.96) | 97 (17.76) |
| No disability | 452 (52.99) * | 170 (55.37) | 282 (51.65) |
| TUG | |||
| Correct functional efficiency | 436 (51.11) * | 163 (53.09) * | 273 (50.00) * |
| Low risk of falls | 281 (32.94) * | 105 (34.20) * | 176 (32.23) * |
| High risk of fall | 136 (15.94) | 39 (12.70) | 97 (17.76) |
| CDT | |||
| Correct drawing | 186 (21.80) | 53 (17.26) | 133 (24.36) |
| Minor visual-spatial errors | 86 (10.08) | 17 (5.54) | 69 (12.64) |
| Wrong designation 10 after 11 | 128 (15.01) | 38 (12.38) | 90 (16.48) |
| Visuospatial difficulties | 111 (13.01 | 53 (17.26) | 58 (10.62) |
| Inability to draw a clock | 258 (30.25) * | 119 (38.76) * | 139 (25.46) * |
| Impossible to do | 83 (9.73) | 27 (8.77) | 57 (10.44) |
| ALL (N = 853) | MALES (N = 307) | FEMALES (N = 546) | t | df | p | |
|---|---|---|---|---|---|---|
| Mean (±SD) | ||||||
| Geriatric Depression Scale (GDS) | 7.02 ± 6.18 | 6.32 ± 6.03 | 7.41 ± 6.24 | −2.47 | 853 | 0.014 * |
| Instrumental Activities of Daily Living (IADL) | 4.53 ± 2.98 | 4.75 ± 3.01 | 4.41 ± 2.96 | 1.57 | 853 | 0.116 |
| The Timed Up And Go (TUG) | 10.36 ± 14.97 | 9.01 ± 10.32 | 11.13 ± 17.00 | −1.98 | 853 | 0.048 * |
| Clock-Drawing Test (CDT) | 5.02 ± 5.74 | 5.16 ± 5.34 | 4.94 ± 5.96 | −2.17 | 853 | 0.030 * |
| ALL (N = 853) | MALES (N = 307) | FEMALES (N = 546) | ||||
|---|---|---|---|---|---|---|
| N (%) | ||||||
| Yes | No | Yes | No | Yes | No | |
| IADL 1 ACTIVITY: USING A PHONE | 716 (83.94) | 137 (16.06) * | 258 (84.04) | 49 (15.96) * | 458 (83.88) | 88 (16.12) * |
| IADL 2 ACTIVITY: DOING SHOPPING | 350 (41.03) | 503 (58.97) | 156 (50.81) | 151 (49.18) | 194 (35.53) | 352 (64.47) * |
| IADL 3 ACTIVITY: PREPARING MEALS | 446 (52.29) | 407 (47.71) | 154 (50.16) | 153 (48.84) | 292 (53.48) | 254 (46.52) |
| IADL 4 ACTIVITY: CLEANING | 405 (47.48) | 448 (52.52) | 153 (49.84) | 154 (50.16) | 256 (46.15) | 290 (53.85) |
| IADL 5 ACTIVITY: WASHING | 456 (53.46) | 397 (46.54) | 151 (49.18) | 156 (50.81) | 305 (55.86) | 241 (44.14) |
| IADL 6 ACTIVITY: USING DIFFERENT FORMS OF TRANSPORT | 303 (35.52) | 550 (64.48) * | 144 (46.90) | 163 (53.09) | 159 (29.12) | 387 (70.88) * |
| IADL 7 ACTIVITY: USING MEDICATIONS | 574 (67.29) | 279 (32.71) * | 206 (67.10) | 101 (32.90) * | 368 (67.40) | 178 (32.60) * |
| IADL 8 ACTIVITY: USING MONEY | 621 (72.80) | 232 (27.20) * | 235 (76.55) | 72 (23.45) * | 386 (70.70) | 160 (29.30) * |
| GDS | IADL | TUG | CDT | |
|---|---|---|---|---|
| GDS | 1.00 | −0.61 * | −0.24 | 0.74 * |
| IADL | −0.61 * | 1.00 | 0.28 | −0.54 * |
| TUG | −0.24 | 0.28 | 1.00 | −0.25 |
| CDT | 0.74 * | −0.54 * | −0.25 | 1.00 |
| GDS | IADL | TUG | CDT | |
|---|---|---|---|---|
| GDS | 1.00 | −0.62 * | −0.34 | 0.75 * |
| IADL | −0.62 * | 1.00 | 0.34 | −0.53 * |
| TUG | −0.34 | 0.34 | 1.00 | −0.28 |
| CDT | 0.75 * | −0.53 * | −0.28 | 1.00 |
| GDS | IADL | TUG | CDT | |
|---|---|---|---|---|
| GDS | 1.00 | −0.61 * | −0.22 | 0.73 * |
| IADL | −0.61 * | 1.00 | 0.27 | −0.54 * |
| TUG | −0.22 | 0.27 | 1.00 | −0.25 |
| CDT | 0.73 * | −0.54 * | −0.25 | 1.00 |
| GDS | |||
|---|---|---|---|
| ALL | MALES | FEMALES | |
| IADL 1 | −0.46 * | −0.48 * | −0.45 * |
| IADL 2 | −0.42 | −0.45 | −0.38 * |
| IADL 3 | −0.40 | −0.43 | −0.40 |
| IADL 4 | −0.41 | −0.42 | −0.40 |
| IADL 5 | −0.41 | −0.42 | −0.43 |
| IADL 6 | −0.42 * | −0.47 | −0.37 * |
| IADL 7 | −0.47 * | −0.46 * | −0.49 * |
| IADL 8 | −0.51 * | −0.53 * | −0.49 * |
| Value | F | df | Mean Square | p | |
|---|---|---|---|---|---|
| SEX | 0.979 | 4.32 | 4 | 841.000 | 0.002 * |
| GDS | 0.293 | 109.38 | 12 | 2225.368 | 0.001 * |
| GDS × SEX | 0.993 | 0.47 | 12 | 2225.368 | 0.934 |
| GDS × TUG | 0.975 | 1.12 | 18 | 1624 | 0.320 |
| GDS × IDAL | 0.922 | 3.82 | 18 | 2370.707 | 0.001 * |
| GDS × CDT | 0.975 | 1.12 | 18 | 1624 | 0.319 |
| GDS × SEX × TUG | 0.974 | 1.17 | 18 | 1624 | 0.280 |
| GDS × SEX × IADL | 0.974 | 1.78 | 12 | 2190.974 | 0.046 * |
| GDS × SEX × CDT | 0.974 | 1.17 | 18 | 1624 | 0.279 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pietrzak, B.; Kujawa, J.; Lipert, A. Depressive Disorders, Cognitive and Physical Function of Older People in Early Dementia Detection. Life 2023, 13, 2010. https://doi.org/10.3390/life13102010
Pietrzak B, Kujawa J, Lipert A. Depressive Disorders, Cognitive and Physical Function of Older People in Early Dementia Detection. Life. 2023; 13(10):2010. https://doi.org/10.3390/life13102010
Chicago/Turabian StylePietrzak, Beata, Jolanta Kujawa, and Anna Lipert. 2023. "Depressive Disorders, Cognitive and Physical Function of Older People in Early Dementia Detection" Life 13, no. 10: 2010. https://doi.org/10.3390/life13102010
APA StylePietrzak, B., Kujawa, J., & Lipert, A. (2023). Depressive Disorders, Cognitive and Physical Function of Older People in Early Dementia Detection. Life, 13(10), 2010. https://doi.org/10.3390/life13102010







