The Role of Different Methods in Defining Cardiometabolic Risk and Metabolic Syndrome in Women with Polycystic Ovary Syndrome
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Demographic Characteristics, Anthropometric Measurements, and the Calculation of Indices
2.3. Clinical and Biochemical Parameters
2.4. Statistical Analysis
3. Results
3.1. Demographic Characteristics of Participants
3.2. Anthropometric Measurements and Indices
3.3. Biochemical Parameters and Blood Pressure Measurements
3.4. Correlations among Biochemical, Clinical, and Anthropometric Parameters
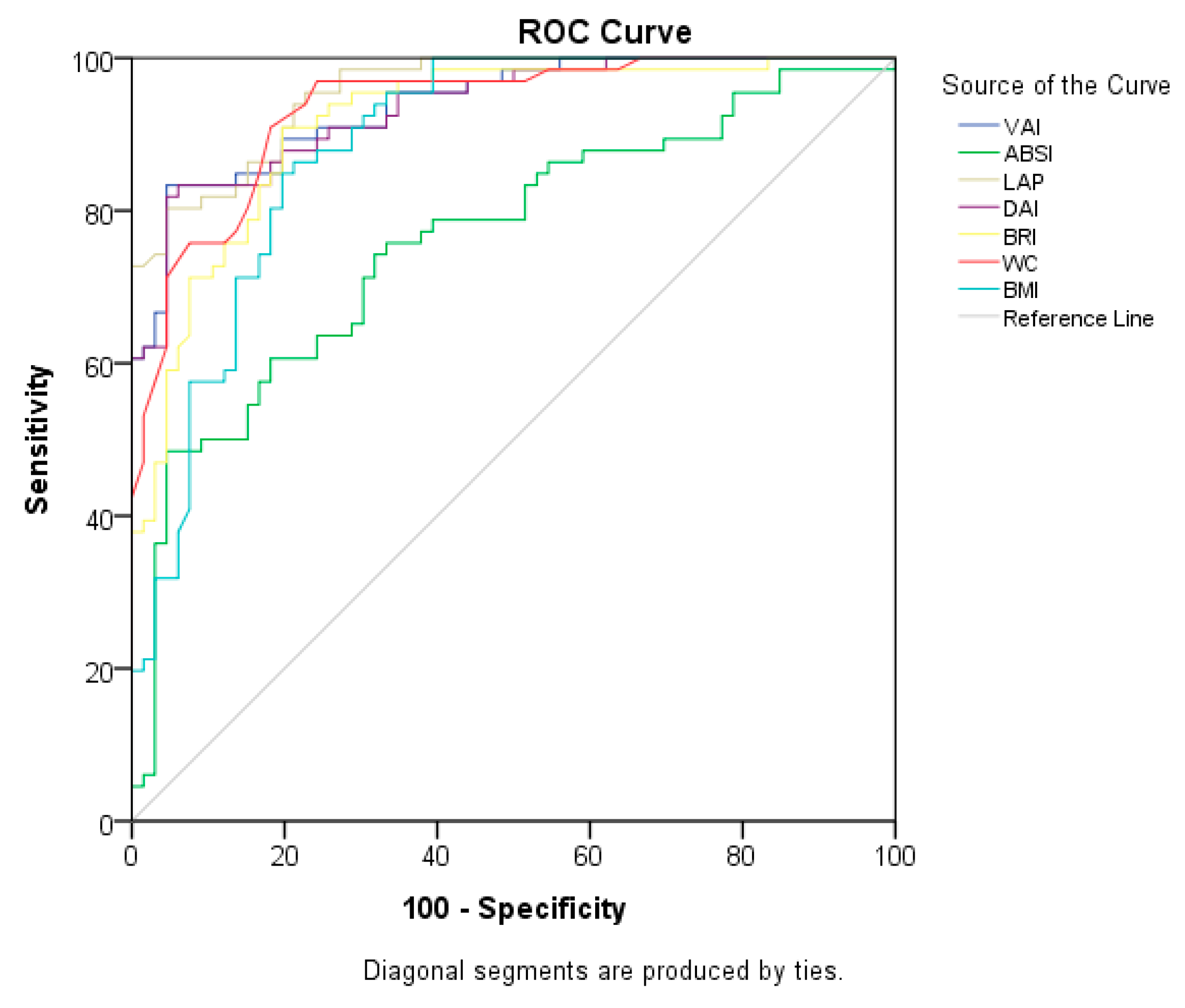
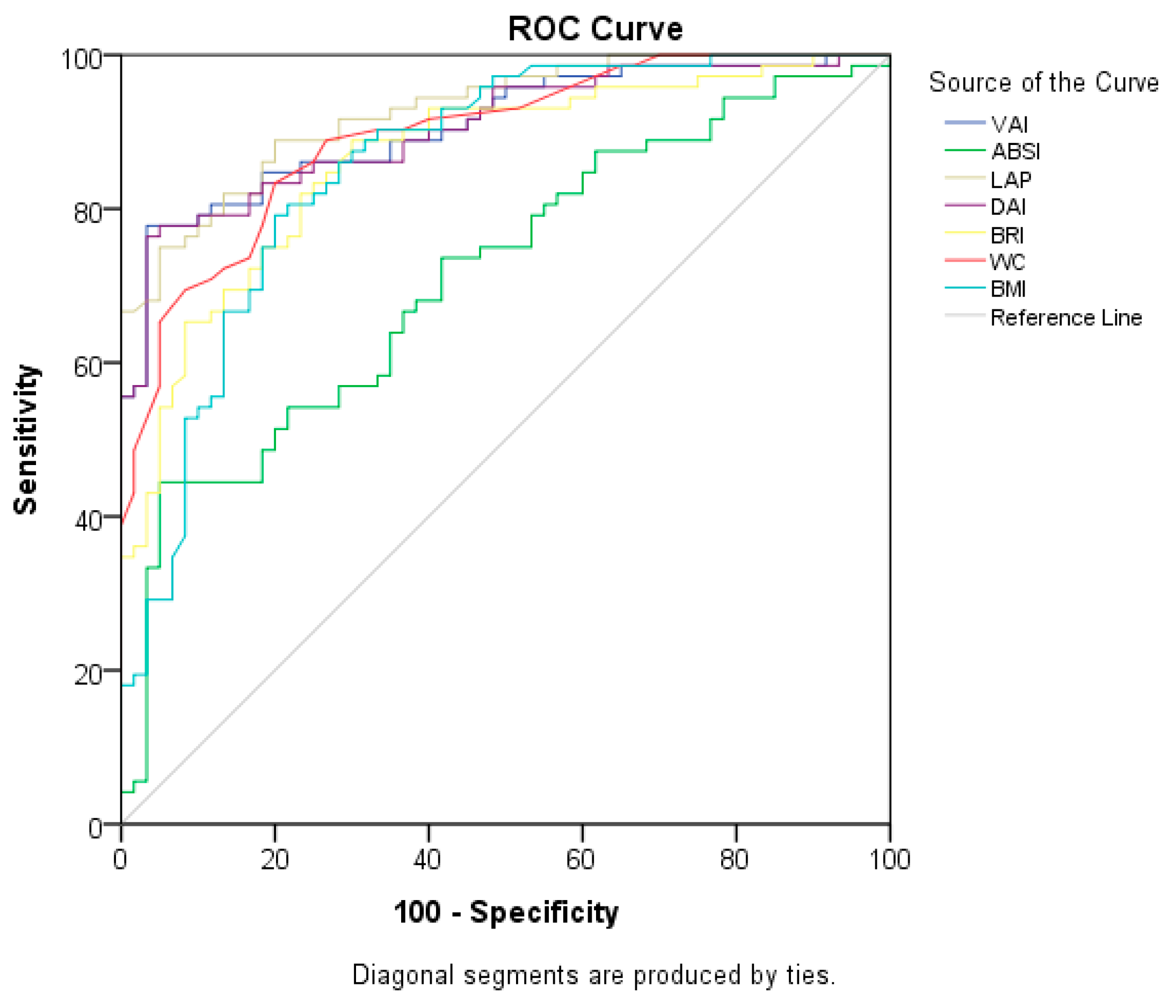
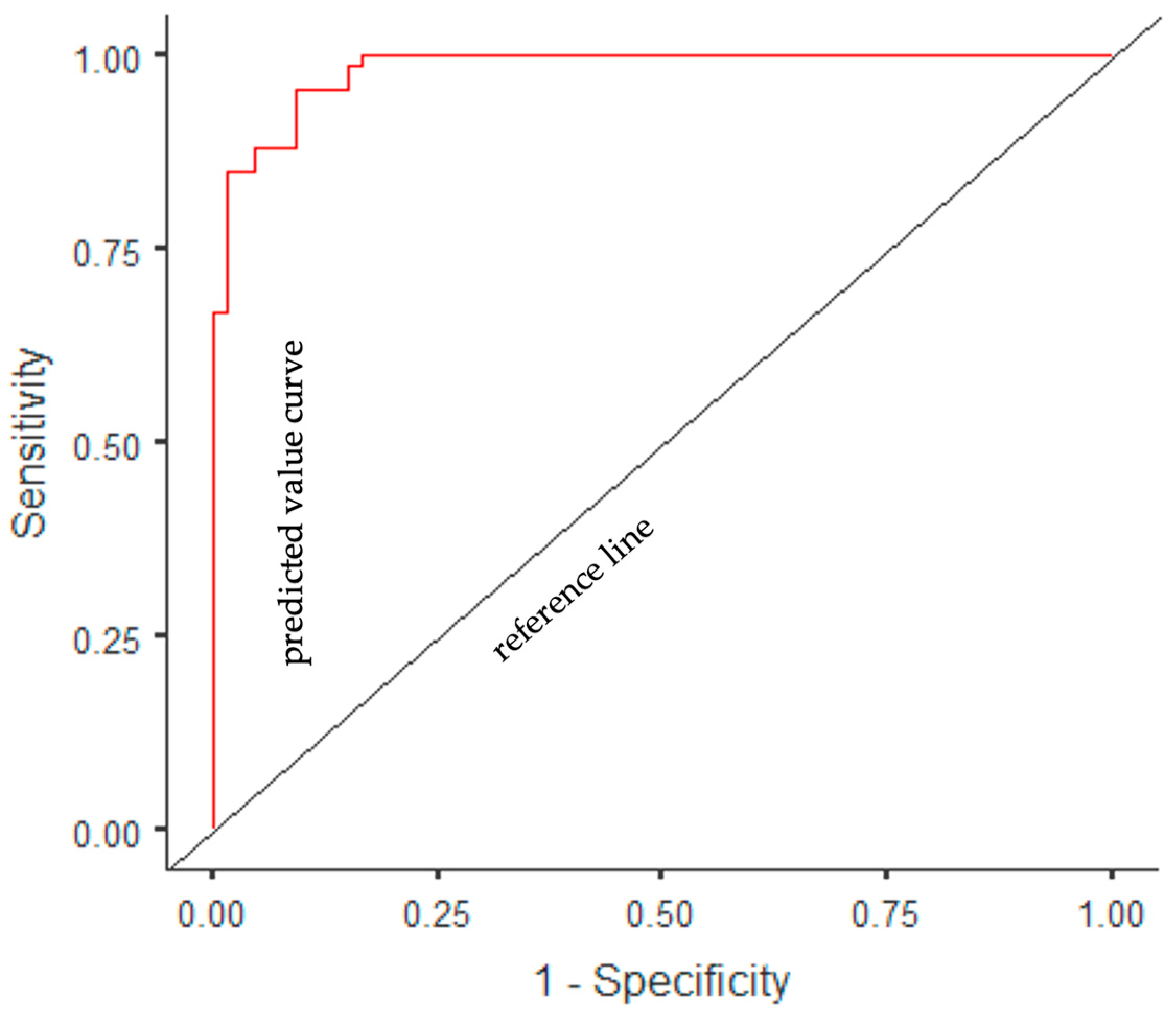
3.5. Assessing the Ability of Indices to Predict the Existence of PCOS and MetS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fauser, B.C.; Tarlatzis, B.C.; Rebar, R.W.; Legro, R.S.; Balen, A.H.; Lobo, R.; Carmina, E.; Chang, J.; Yildiz, B.O.; Laven, J.S.; et al. Consensus on women’s health aspects of polycystic ovary syndrome (PCOS): The Amsterdam ESHRE/ASRM-Sponsored 3rd PCOS Consensus Workshop Group. Fertil. Steril. 2012, 97, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Nandi, A.; Chen, Z.; Patel, R.; Poretsky, L. Polycystic ovary syndrome. Endocrinol. Metab. Clin. N. Am. 2014, 43, 123–147. [Google Scholar] [CrossRef] [PubMed]
- Başar Gökcen, B.; Akdevelioğlu, Y.; Canan, S.; Bozkurt, N. Evaluation of the relationship between serum ferritin and insulin resistance and visceral adiposity index (VAI) in women with polycystic ovary syndrome. Eat. Weight Disord. 2021, 26, 1581–1593. [Google Scholar] [CrossRef] [PubMed]
- Palomba, S.; Dewailly, D. PCOS: From infertility to pregnancy. Front. Endocrinol. 2023, 14, 1220014. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Liu, L.; Yin, T.L.; Yang, J.; Xiong, C.L. Follicular metabolic changes and effects on oocyte quality in polycystic ovary syndrome patients. Oncotarget 2017, 8, 80472–80480. [Google Scholar] [CrossRef]
- Zhang, X.; Miao, H.; Zhou, J.; Chen, Y.; Ou, Y.; Song, Y.; Peng, X.; Li, Y.; Li, L. Association between preconception anti-androgen therapy and pregnancy outcomes of patients with PCOS: A prospective cohort study. Front. Endocrinol. 2023, 14, 1109861. [Google Scholar] [CrossRef]
- Teede, H.J.; Tay, C.T.; Laven, J.J.; Dokras, A.; Moran, L.J.; Piltonen, T.T.; Costello, M.F.; Boivin, J.; Redman, L.M.; Boyle, J.A.; et al. Recommendations from the 2023 international evidence-based guideline for the assessment and management of polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 2023, 189, G43–G64. [Google Scholar] [CrossRef]
- Teede, H.J.; Misso, M.L.; Costello, M.F.; Dokras, A.; Laven, J.; Moran, L.; Piltonen, T.; Norman, R.J. International PCOS Network. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Hum. Reprod. 2018, 33, 1602–1618. [Google Scholar] [CrossRef]
- Durmus, U.; Duran, C.; Ecirli, S. Visceral adiposity index levels in overweight and/or obese, and non-obese patients with polycystic ovary syndrome and its relationship with metabolic and inflammatory parameters. J. Endocrinol. Investig. 2017, 40, 487–497. [Google Scholar] [CrossRef]
- Rochlani, Y.; Pothineni, N.V.; Kovelamudi, S.; Mehta, J.L. Metabolic syndrome: Pathophysiology, management, and modulation by natural compounds. Ther. Adv. Cardiovasc. Dis. 2017, 11, 215–225. [Google Scholar] [CrossRef]
- Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z. The metabolic syndrome. Lancet 2005, 365, 1415–1428. [Google Scholar] [CrossRef] [PubMed]
- Macut, D.; Antić, I.B.; Bjekić-Macut, J.; Panidis, D.; Tziomalos, K.; Milutinović, D.V.; Stanojlović, O.; Kastratović-Kotlica, B.; Petakov, M.; Milić, N. Lipid accumulation product is associated with metabolic syndrome in women with polycystic ovary syndrome. Hormones 2016, 15, 35–44. [Google Scholar] [CrossRef] [PubMed]
- Gambineri, A.; Pelusi, C.; Vicennati, V.; Pagotto, U.; Pasquali, R. Obesity and the polycystic ovary syndrome. Int. J. Obes. Relat. Metab. Disord. 2002, 26, 883–896. [Google Scholar] [CrossRef]
- Zheng, S.H.; Li, X.L. Visceral adiposity index as a predictor of clinical severity and therapeutic outcome of PCOS. Gynecol. Endocrinol. 2016, 32, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Mu, L.; Zhao, Y.; Li, R.; Lai, Y.; Qiao, J. Metabolic characteristics of normal weight central obesity phenotype polycystic ovary syndrome women: A large-scale national epidemiological survey. Reprod. Biomed. Online 2018, 37, 498–504. [Google Scholar] [CrossRef] [PubMed]
- Randeva, H.S.; Tan, B.K.; Weickert, M.O.; Lois, K.; Nestler, J.E.; Sattar, N.; Lehnert, H. Cardiometabolic aspects of the polycystic ovary syndrome. Endocr. Rev. 2012, 33, 812–841. [Google Scholar] [CrossRef] [PubMed]
- De Lorenzo, A.; Bianchi, A.; Maroni, P.; Iannarelli, A.; Di Daniele, N.; Iacopino, L.; Di Renzo, L. Adiposity rather than BMI determines metabolic risk. Int. J. Cardiol. 2013, 166, 111–117. [Google Scholar] [CrossRef]
- Jeanes, Y.M.; Reeves, S. Metabolic consequences of obesity and insulin resistance in polycystic ovary syndrome: Diagnostic and methodological challenges. Nutr. Res. Rev. 2017, 30, 97. [Google Scholar] [CrossRef]
- Goodman, N.F.; Cobin, R.H.; Futterweit, W.; Glueck, J.S.; Legro, R.S.; Carmina, E. American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and PCOS Society Disease State Clinical Review: Guide to the best practices in the evaluation and treatment of polycystic ovary syndrome-part 1. Endocr. Pract. 2015, 21, 1291–1300. [Google Scholar] [CrossRef]
- Goodpaster, B.H.; Krishnaswami, S.; Harris, T.B.; Katsiaras, A.; Kritchevsky, S.B.; Simonsick, E.M.; Nevitt, M.; Holvoet, P.; Newman, A.B. Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Arch. Intern. Med. 2005, 165, 777–783. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. Metabolic syndrome—A new world-wide definition. A consensus statement from the international diabetes federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Krakauer, N.Y.; Krakauer, J.C. A new body shape index predicts mortality hazard independently of body mass index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.M.; Bredlau, C.; Bosy-Westphal, A.; Mueller, M.; Shen, W.; Gallagher, D.; Maeda, Y.; McDougall, A.; Peterson, C.M.; Ravussin, E.; et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013, 21, 2264–2271. [Google Scholar] [CrossRef]
- Reyes-Barrera, J.; Sainz-Escárrega, V.H.; Medina-Urritia, A.X.; Jorge-Galarza, E.; Osorio-Alonso, H.; Torres-Tamayo, M.; Leal-Escobar, G.; Posadas-Romero, C.; Torre-Villalvazo, I.; Juárez-Rojas, J.G. Dysfunctional adiposity index as a useful clinical tool for early identification of adipose tissue morpho-functional abnormalities and cardiometabolic disorders in apparently healthy subjects. Adipocyte 2021, 10, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Kahn, H.S. The “lipid accumulation product” performs better than the body mass index for recognizing cardiovascular risk: A population-based comparison. BMC Cardiovasc. Disord. 2005, 5, 26. [Google Scholar] [CrossRef] [PubMed]
- Amato, M.C.; Giordano, C.; Galia, M.; Criscimanna, A.; Vitabile, S.; Midiri, M.; Galluzzo, A.; AlkaMeSy Study Group. Visceral Adiposity Index: A reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care 2010, 33, 920–922. [Google Scholar] [CrossRef]
- Ryu, K.; Suliman, M.E.; Qureshi, A.R.; Chen, Z.; Avesani, C.M.; Brismar, T.B.; Ripsweden, J.; Barany, P.; Heimbürger, O.; Stenvinkel, P.; et al. Central obesity as assessed by conicity index and a-body shape index associates with cardiovascular risk factors and mortality in kidney failure patients. Front. Nutr. 2023, 10, 1035343. [Google Scholar] [CrossRef]
- Ji, M.; Zhang, S.; An, R. Effectiveness of A Body Shape Index (ABSI) in predicting chronic diseases and mortality: A systematic review and meta-analysis. Obes. Rev. 2018, 19, 737–759. [Google Scholar] [CrossRef]
- Gönülalan, G.; Saçkan, F. The importance of new anthropometric measurements in detecting cardio metabolic risk and insulin resistance in patients with polycystic ovary syndrome: Single center experience. Türkiye Diyabet Obezite Derg. 2021, 5, 25–32. [Google Scholar] [CrossRef]
- Li, G.; Wu, H.K.; Wu, X.W.; Cao, Z.; Tu, Y.C.; Ma, Y.; Li, B.N.; Peng, Q.Y.; Cheng, J.; Wu, B.; et al. The feasibility of two anthropometric indices to identify metabolic syndrome, insulin resistance and inflammatory factors in obese and overweight adults. Nutrition 2019, 57, 194–201. [Google Scholar] [CrossRef]
- López-González, A.A.; Jover, A.M.; Martínez, C.S.; Artal, P.M.; Bote, S.A.; Jané, B.A.; Ramírez-Manent, J.I. The CUN-BAE, Deurenberg Fat Mass, and visceral adiposity index as confident anthropometric indices for early detection of metabolic syndrome components in adults. Sci. Rep. 2022, 12, 15486. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Sánchez, F.D.; Diaz-Jarquin, A.; Vargas-Abonce, V.P.; Torres-Cuevas, J.L.; Guerrero-Castillo, A.P.; Medina-Julio, D.; Meza-Arana, C.E.; Gulias-Herrero, A.; Gómez-Sámano, M.Á. Comparison of adiposity indices and their association with insulin resistance and β-cell dysfunction in primary prevention for diabetes in Mexican population. Diabetes Epidemiol. Manag. 2022, 8, 100091. [Google Scholar] [CrossRef]
- Mazidi, M.; Kengne, A.P.; Katsiki, N.; Mikhailidis, D.P.; Banach, M. Lipid accumulation product and triglycerides/glucose index are useful predictors of insulin resistance. J. Diabetes Complicat. 2018, 32, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Wiltgen, D.; Benedetto, I.G.; Mastella, L.S.; Spritzer, P.M. Lipid accumulation product index: A reliable marker of cardiovascular risk in polycystic ovary syndrome. Hum. Reprod. 2009, 24, 1726–1731. [Google Scholar] [CrossRef]
- Amato, M.C.; Guarnotta, V.; Forti, D.; Donatelli, M.; Dolcimascolo, S.; Giordano, C. Metabolically healthy polycystic ovary syndrome (MH-PCOS) and metabolically unhealthy polycystic ovary syndrome (MU-PCOS): A comparative analysis of four simple methods useful for metabolic assessment. Hum. Reprod. 2013, 28, 1919–1928. [Google Scholar] [CrossRef][Green Version]
- Abruzzese, G.A.; Cerrone, G.E.; Gamez, J.M.; Graffigna, M.N.; Belli, S.; Lioy, G.; Mormandi, E.; Otero, P.; Levalle, O.A.; Motta, A.B. Lipid accumulation product (LAP) and visceral adiposity index (VAI) as markers of insulin resistance and metabolic associated disturbances in young argentine women with polycystic ovary syndrome. Horm. Metab. Res. 2017, 49, 23–29. [Google Scholar] [CrossRef]
- Banu, H.; Morshed, M.S.; Sultana, T.; Shah, S.; Afrine, S.; Hasanat, M.A. Lipid accumulation product better predicts metabolic status in lean polycystic ovary syndrome than that by visceral adiposity index. J. Hum. Reprod. Sci. 2022, 15, 27–33. [Google Scholar] [CrossRef]
- Dai, D.; Chang, Y.; Chen, Y.; Chen, S.; Yu, S.; Guo, X.; Sun, Y. Visceral adiposity index and lipid accumulation product index: Two alternate body indices to identify chronic kidney disease among the rural population in Northeast China. Int. J. Environ. Res. Public Health 2016, 13, 1231. [Google Scholar] [CrossRef]
- Ray, L.; Ravichandran, K.; Nanda, S.K. Comparison of lipid accumulation product index with body mass index and waist circumference as a predictor of metabolic syndrome in Indian population. Metab. Syndr. Relat. Disord. 2018, 16, 240–245. [Google Scholar] [CrossRef]
- Knowles, K.M.; Paiva, L.L.; Sanchez, S.E.; Revilla, L.; Lopez, T.; Yasuda, M.B.; Yanez, N.D.; Gelaye, B.; Williams, M.A. Waist circumference, body mass index, and other measures of adiposity in predicting cardiovascular disease risk factors among Peruvian adults. Int. J. Hypertens. 2011, 2011, 931402. [Google Scholar] [CrossRef]
- Tehrani, F.R.; Minooee, S.; Azizi, F. Comparison of various adiposity indexes in women with polycystic ovary syndrome and normo-ovulatory non-hirsute women: A population-based study. Eur. J. Endocrinol. 2014, 171, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Ismaiel, A.; Jaaouani, A.; Leucuta, D.C.; Popa, S.L.; Dumitrascu, D.L. The visceral adiposity index in non-alcoholic fatty liver disease and liver fibrosis—Systematic review and meta-analysis. Biomedicines 2021, 9, 1890. [Google Scholar] [CrossRef] [PubMed]
- Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum. Reprod. 2004, 19, 41–47. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation (IDF). The IDF Consensus Worldwide Definition of the Metabolic Syndrome. 2006. Available online: https://idf.org/about-diabetes/resources/?type=364 (accessed on 20 July 2023).
- World Health Organisation (WHO). Physical Status: The Use and Interpretation of Anthropometry. 1995. Available online: http://apps.who.int/iris/bitstream/handle/10665/37003/WHO_TRS_854.pdf?sequence=1 (accessed on 20 July 2023).
- Muntner, P.; Shimbo, D.; Carey, R.M.; Charleston, J.B.; Gaillard, T.; Misra, S.; Myers, M.G.; Ogedegbe, G.; Schwartz, J.E.; Townsend, R.R.; et al. Measurement of blood pressure in humans: A scientific statement from the American Heart Association. Hypertension 2019, 73, e35–e66. [Google Scholar] [CrossRef] [PubMed]
- Vassilatou, E.; Lafoyianni, S.; Vassiliadi, D.A.; Ioannidis, D.; Paschou, S.A.; Mizamtsidi, M.; Panagou, M.; Vryonidou, A. Visceral adiposity index for the diagnosis of nonalcoholic fatty liver disease in premenopausal women with and without polycystic ovary syndrome. Maturitas 2018, 116, 1–7. [Google Scholar] [CrossRef]
- Dunaif, A.; Graf, M.; Mandeli, J.; Laumas, V.; Dobrjansky, A. Characterization of groups of hyperandrogenic women with acanthosis nigricans, impaired glucose tolerance, and/or hyperinsulinemia. J. Clin. Endocrinol. Metab. 1987, 65, 499–507. [Google Scholar] [CrossRef]
- Anik Ilhan, G.; Yildizhan, B.; Pekin, T. The impact of lipid accumulation product (LAP) and visceral adiposity index (VAI) on clinical, hormonal and metabolic parameters in lean women with polycystic ovary syndrome. Gynecol. Endocrinol. 2019, 35, 233–236. [Google Scholar] [CrossRef]
- Delitala, A.P.; Capobianco, G.; Delitala, G.; Cherchi, P.L.; Dessole, S. Polycystic ovary syndrome, adipose tissue and metabolic syndrome. Arch. Gynecol. Obstet. 2017, 296, 405–419. [Google Scholar] [CrossRef]
- Tchernof, A.; Després, J.P. Pathophysiology of human visceral obesity: An update. Physiol. Rev. 2013, 93, 359–404. [Google Scholar] [CrossRef]
- Norman, R.J.; Davies, M.J.; Lord, J.; Moran, L.J. The role of lifestyle modification in polycystic ovary syndrome. Trends Endocrinol. Metab. 2002, 13, 251–257. [Google Scholar] [CrossRef]
- Lee, W.Y.; Jung, C.H.; Park, J.S.; Rhee, E.J.; Kim, S.W. Effects of smoking, alcohol, exercise, education, and family history on the metabolic syndrome as defined by the ATP III. Diabetes Res. Clin. Pract. 2005, 67, 70–77. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Noncommunicable Diseases Country Profiles 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Ching, Y.K.; Chin, Y.S.; Appukutty, M.; Gan, W.Y.; Ramanchadran, V.; Chan, Y.M. Prevalence of metabolic syndrome and its associated factors among vegetarians in Malaysia. Int. J. Environ. Res. Public Health 2018, 15, 2031. [Google Scholar] [CrossRef] [PubMed]
- Bedel, A.; Tuhan, H.; İsmailoğlu, E.; Kizilay, D.Ö.; Sezer, A. Obez ve obez olmayan polikistik over sendromlu adolesanların klinik ve laboratuvar özelliklerinin karşılaştırılması. Akdeniz Tıp Derg. 2022, 8, 75–81. [Google Scholar] [CrossRef]
- Legro, R.S.; Castracane, V.D.; Kauffman, R.P. Detecting insulin resistance in polycystic ovary syndrome: Purposes and pitfalls. Obstet. Gynecol. Surv. 2004, 59, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Essah, P.A.; Wickham, E.P.; Nestler, J.E. The metabolic syndrome in polycystic ovary syndrome. Clin. Obstet. Gynecol. 2007, 50, 205–225. [Google Scholar] [CrossRef]
- Cosar, E.; Üçok, K.; Akgün, L.; Köken, G.; Sahin, F.K.; Arioz, D.T.; Baş, O. Body fat composition and distribution in women with polycystic ovary syndrome. Gynecol. Endocrinol. 2008, 24, 428–432. [Google Scholar] [CrossRef] [PubMed]
- Karabulut, A.; Yaylali, G.F.; Demirlenk, S.; Sevket, O.; Acun, A. Evaluation of body fat distribution in PCOS and its association with carotid atherosclerosis and insulin resistance. Gynecol. Endocrinol. 2012, 28, 111–114. [Google Scholar] [CrossRef]
- Svendsen, P.F.; Nilas, L.; Nørgaard, K.; Jensen, J.E.B.; Madsbad, S. Obesity, body composition and metabolic disturbances in polycystic ovary syndrome. Hum. Reprod. 2008, 23, 2113–2121. [Google Scholar] [CrossRef]
- Yucel, A.; Noyan, V.; Sagsoz, N. The association of serum androgens and insulin resistance with fat distribution in polycystic ovary syndrome. Eur. J. Obstet. Gynecol. Reprod. Biol. 2006, 126, 81–86. [Google Scholar] [CrossRef]
- Godoy-Matos, A.F.; Vaisman, F.; Pedrosa, A.P.; Farias, M.L.; Mendonça, L.M.C.; Pinheiro, M.F.M.C. Central-to-peripheral fat ratio, but not peripheral body fat, is related to insulin resistance and androgen markers in polycystic ovary syndrome. Gynecol. Endocrinol. 2009, 25, 793–798. [Google Scholar] [CrossRef]
- Dutkowska, A.; Konieczna, A.; Breska-Kruszewska, J.; Sendrakowska, M.; Kowalska, I.; Rachoń, D. Recomendations on non-pharmacological interventions in women with PCOS to reduce body weight and improve metabolic disorders [Zalecenia dotyczące postępowania niefarmakologicznego u kobiet z PCOS celem zmniejszenia masy ciała i poprawy zaburzeń metabolicznych]. Endokrynol. Pol. 2019, 70, 198–212. [Google Scholar] [CrossRef] [PubMed]
- Kaluzna, M.; Czlapka-Matyasik, M.; Bykowska-Derda, A.; Moczko, J.; Ruchala, M.; Ziemnicka, K. Indirect predictors of visceral adipose tissue in women with polycystic ovary syndrome: A comparison of methods. Nutrients 2021, 13, 2494. [Google Scholar] [CrossRef] [PubMed]
- Perna, S.; Spadaccini, D.; Nichetti, M.; Avanzato, I.; Faliva, M.A.; Rondanelli, M. Osteosarcopenic visceral obesity and osteosarcopenic subcutaneous obesity, two new phenotypes of sarcopenia: Prevalence, metabolic profile, and risk factors. J. Aging Res. 2018, 16, 6147426. [Google Scholar] [CrossRef] [PubMed]
- Beatriz Motta, A. The role of obesity in the development of polycystic ovary syndrome. Curr. Pharm. Des. 2012, 18, 2482–2491. [Google Scholar] [CrossRef]
- Silveira, E.A.; Kliemann, N.; Noll, M.; Sarrafzadegan, N.; de Oliveira, C. Visceral obesity and incident cancer and cardiovascular disease: An integrative review of the epidemiological evidence. Obes. Rev. 2021, 22, e13088. [Google Scholar] [CrossRef]
- Kozan, O.; Oguz, A.; Abaci, A.; Erol, C.; Ongen, Z.; Temizhan, A.; Celik, S. Prevalence of the metabolic syndrome among Turkish adults. Eur. J. Clin. Nutr. 2007, 61, 548–553. [Google Scholar] [CrossRef]
- Süleymanlar, G.; Utaş, C.; Arinsoy, T.; Ateş, K.; Altun, B.; Altiparmak, M.R.; Ecder, T.; Yilmaz, M.E.; Camsari, T.; Basci, A.; et al. A population-based survey of Chronic REnal Disease In Turkey—The CREDIT study. Nephrol. Dial. Transplant. 2011, 26, 1862–1871. [Google Scholar] [CrossRef]
- Sağlık Bakanlığı, T.C. Türkiye Kronik Hastalıklar ve Risk Faktörleri Sıklığı Çalışması; Sağlık Bakanlığı Yayın No. 909; T.C. Sağlık Bakanlığı: Ankara, Turkey, 2013. [Google Scholar]
- Gundogan, K.; Bayram, F.; Gedik, V.; Kaya, A.; Karaman, A.; Demir, Ö.; Sabuncu, T.; Kocer, D.; Coskun, R. Metabolic syndrome prevalence according to ATP III and IDF criteria and related factors in Turkish adults. Arch. Med. Sci. 2013, 9, 243–253. [Google Scholar] [CrossRef]
- Abacı, A.; Kılıçkap, M.; Göksülük, H.; Karaaslan, D.; Barçın, C.; Kayıkçıoğlu, M.; Özer, N.; Yılmaz, M.B.; Şahin, M.; Tokgözoğlu, L. Data on prevalence of metabolic syndrome in Turkey: Systematic review, meta-analysis and meta-regression of epidemiological studies on cardiovascular risk factors. Turk Kardiyol. Dern. Ars. 2018, 46, 591–601. [Google Scholar] [CrossRef]
- Ehrmann, D.A.; Liljenquist, D.R.; Kasza, K.; Azziz, R.; Legro, R.S.; Ghazzi, M.N.; PCOS/Troglitazone Study Group. Prevalence and predictors of the metabolic syndrome in women with polycystic ovary syndrome. J. Clin. Endocrinol. Metab. 2006, 91, 48–53. [Google Scholar] [CrossRef]
- Boyle, J.A.; Cunningham, J.; Norman, R.J.; Dunbar, T.; O’Dea, K. Polycystic ovary syndrome and metabolic syndrome in Indigenous Australian women. Intern. Med. J. 2015, 45, 1247–1254. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, B.O.; Bozdag, G.; Yapici, Z.; Esinler, I.; Yarali, H. Prevalence, phenotype and cardiometabolic risk of polycystic ovary syndrome under different diagnostic criteria. Hum. Reprod. 2012, 27, 3067–3073. [Google Scholar] [CrossRef] [PubMed]
- Drøyvold, W.B.; Midthjell, K.; Nilsen, T.I.L.; Holmen, J. Change in body mass index and its impact on blood pressure: A prospective population study. Int. J. Obes. 2005, 29, 650–655. [Google Scholar] [CrossRef]
- Onat, A.; Can, G.; Yüksel, H.; Ademoğlu, E.; Erginel-Ünaltuna, N.; Kaya, A.; Altay, S. TEKHARF 2017 Tıp Dünyasının Kronik Hastalıklara Yaklaşımına Öncülük; Logos Yayıncılık: Istanbul, Turkey, 2017; Available online: https://file.tkd.org.tr/PDFs/TEKHARF-2017.pdf (accessed on 20 July 2023).
- Christ, J.P.; Cedars, M.I. Current guidelines for diagnosing PCOS. Diagnostics 2023, 13, 1113. [Google Scholar] [CrossRef] [PubMed]
- Azziz, R.; Carmina, E.; Dewailly, D.; Diamanti-Kandarakis, E.; Escobar-Morreale, H.F.; Futterweit, W.; Janssen, O.E.; Legro, R.S.; Norman, R.J.; Taylor, A.E.; et al. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: The complete task force report. Fertil. Steril. 2009, 91, 456–488. [Google Scholar] [CrossRef]
- Diamanti-Kandarakis, E.; Panidis, D. Unravelling the phenotypic map of polycystic ovary syndrome (PCOS): A prospective study of 634 women with PCOS. Clin. Endocrinol. 2007, 67, 735–742. [Google Scholar] [CrossRef]
- Hahn, S.; Tan, S.; Elsenbruch, S.; Quadbeck, B.; Herrmann, B.L.; Mann, K.; Janssen, O.E. Clinical and biochemical characterization of women with polycystic ovary syndrome in North Rhine-Westphalia. Horm. Metab. Res. 2005, 37, 438–444. [Google Scholar] [CrossRef]
- Wild, R.A.; Carmina, E.; Diamanti-Kandarakis, E.; Dokras, A.; Escobar-Morreale, H.F.; Futterweit, W.; Lobo, R.; Norman, R.J.; Talbott, E.; Dumesic, D.A. Assessment of cardiovascular risk and prevention of cardiovascular disease in women with the polycystic ovary syndrome: A consensus statement by the Androgen Excess and Polycystic Ovary Syndrome (AE-PCOS) Society. J. Clin. Endocrinol. Metab. 2010, 95, 2038–2049. [Google Scholar] [CrossRef]
- Behboudi-Gandevani, S.; Tehrani, F.R.; Cheraghi, L.; Azizi, F. Could “a body shape index” and “waist to height ratio” predict insulin resistance and metabolic syndrome in polycystic ovary syndrome? Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 205, 110–114. [Google Scholar] [CrossRef]
- Ortega, F.B.; Sui, X.; Lavie, C.J.; Blair, S.N. Body mass index, the most widely used but also widely criticized index: Would a criterion standard measure of total body fat be a better predictor of cardiovascular disease mortality? Mayo Clin. Proc. 2016, 91, 443–455. [Google Scholar] [CrossRef]
- Christakoudi, S.; Tsilidis, K.K.; Muller, D.C.; Freisling, H.; Weiderpass, E.; Overvad, K.; Söderberg, S.; Häggström, C.; Pischon, T.; Dahm, C.C.; et al. A Body Shape Index (ABSI) achieves better mortality risk stratification than alternative indices of abdominal obesity: Results from a large European cohort. Sci. Rep. 2020, 10, 14541. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). World Health Organization Consultation on Obesity (1999: Geneva, Switzerland) & World Health Organization. (2000). Obesity: Preventing and Managing the Global Epidemic: Report of a WHO Consultation; World Health Organization: Geneva, Switzerland, 2020; Available online: https://apps.who.int/iris/handle/10665/42330 (accessed on 20 July 2023).
- Carmina, E.; Bucchieri, S.; Esposito, A.; Del Puente, A.; Mansueto, P.; Orio, F.; Di Fede, G.; Rini, G. Abdominal fat quantity and distribution in women with polycystic ovary syndrome and extent of its relation to insulin resistance. J. Clin. Endocrinol. Metab. 2007, 92, 2500–2505. [Google Scholar] [CrossRef] [PubMed]
- Macruz, C.F.; Lima, S.M.; Salles, J.E.; da Silva, G.M.; Scalissi, N.M. Assessment of the body composition of patients with polycystic ovary syndrome using dual-energy X-ray absorptiometry. Int. J. Gynecol. Obstet. 2017, 136, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Ezeh, U.; Pall, M.; Mathur, R.; Azziz, R. Association of fat to lean mass ratio with metabolic dysfunction in women with polycystic ovary syndrome. Hum. Reprod. 2014, 29, 1508–1517. [Google Scholar] [CrossRef]
- Taverna, M.J.; Martínez-Larrad, M.T.; Frechtel, G.D.; Serrano-Ríos, M. Lipid accumulation product: A powerful marker of metabolic syndrome in healthy population. Eur. J. Endocrinol. 2011, 164, 559–567. [Google Scholar] [CrossRef]
- Nascimento, J.X.P.T.; Chein, M.B.D.C.; de Sousa, R.M.L.; Ferreira, A.D.S.; Navarro, P.A.; Brito, L.M.O. Importance of lipid accumulation product index as a marker of CVD risk in PCOS women. Lipids Health Dis. 2015, 14, 62. [Google Scholar] [CrossRef]
- Baveicy, K.; Mostafaei, S.; Darbandi, M.; Hamzeh, B.; Najafi, F.; Pasdar, Y. Predicting metabolic syndrome by visceral adiposity index, body roundness index and a body shape index in adults: A cross-sectional study from the Iranian RaNCD cohort data. Diabetes Metab. Syndr. Obes. 2020, 13, 879. [Google Scholar] [CrossRef]
- Jabczyk, M.; Nowak, J.; Jagielski, P.; Hudzik, B.; Kulik-Kupka, K.; Włodarczyk, A.; Lar, K.; Zubelewicz-Szkodzińska, B. Metabolic Deregulations in Patients with Polycystic Ovary Syndrome. Metabolites 2023, 13, 302. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. Expansion of waist circumference in medical literature: Potential clinical application of a body shape index. J. Obes. Weight Loss Ther. 2014, 4, 2. [Google Scholar] [CrossRef]

| A body shape index (ABSI) [22] |
| ABSI = WC (m)/[BMI2/3 (kg/m2) height1/2 (m)] |
| Body roundness index (BRI) [23] |
| Dysfunctional adiposity index (DAI) [24] |
|
| Lipid accumulation (LAP) index [25] |
| LAP female = [WC (cm) − 58] × TG (mmol/L) |
| Visceral adiposity index (VAI) [26] |
| PCOS (+) (n = 66) | Control (n = 66) | p-Value | |||
|---|---|---|---|---|---|
| Mean ± SD | Median (Min–Max) | Mean ± SD | Median (Min–Max) | ||
| Age (year) | 30.98 ± 7.52 | 31 (18.00–45.00) | 36.00 ± 7.20 | 37.5 (19.00–48.00) | <0.001 *a |
| n | % | n | % | ||
| BMI | <0.001 *b | ||||
| Normal | 0 | 0.0 | 16 | 24.2 | |
| Overweight | 9 | 13.6 | 36 | 54.5 | |
| Obese | 57 | 86.4 | 14 | 21.2 | |
| MetS | |||||
| MetS (−) | 1 | 1.5 | 59 | 89.4 | <0.001 *b |
| MetS (+) | 65 | 98.5 | 7 | 10.6 | |
| Chronic disease | |||||
| Yes | 45 | 68.2 | 23 | 34.8 | <0.001 *b |
| No | 21 | 31.8 | 43 | 65.2 | |
| Chronic disease type | |||||
| CVD | 5 | 7.6 | 1 | 1.5 | 0.208 b |
| Type 2 diabetes | 19 | 28.8 | 2 | 3.0 | <0.001 *b |
| Hypercholesterolemia | 7 | 10.6 | 2 | 3.0 | 0.164 b |
| Hypertriglyceridemia | 2 | 3.0 | 0 | 0.0 | 0.496 b |
| Hypertension | 19 | 28.8 | 4 | 6.1 | 0.001 *b |
| Rheumatic disease | 3 | 4.5 | 2 | 3.0 | 0.999 b |
| Kidney disease | 2 | 3.0 | 1 | 1.5 | 0.999 b |
| Gastrointestinal disease | 6 | 9.1 | 5 | 7.6 | 0.999 b |
| Other | 1 | 1.5 | 0 | 0.0 | 0.999 b |
| Smoking | |||||
| Yes | 21 | 31.8 | 7 | 10.6 | 0.003 *b |
| No | 45 | 68.2 | 59 | 89.4 | |
| Alcohol consumption | |||||
| Yes | 28 | 42.4 | 0 | 0.0 | <0.001 *b |
| No | 38 | 57.6 | 66 | 100.0 | |
| Smoking/alcohol | |||||
| Yes | 37 | 56.1 | 7 | 10.6 | <0.001 *b |
| No | 29 | 43.9 | 59 | 89.4 | |
| Regular physical activity | |||||
| Yes | 15 | 22.7 | 15 | 22.7 | 1.000 b |
| No | 51 | 77.3 | 51 | 77.3 | |
| PCOS (+) (n = 66) | Control (n = 66) | ||||||
|---|---|---|---|---|---|---|---|
| Anthropometric Measurement and Indices | Mean ± SD | Median (Min–Max) | Mean ± SD | Median(Min–Max) | t a/Z b | p-Value | Adjusted p-Value ** |
| BMI (kg/m2) | 32.59 ± 3.09 | 32.29 (27.12–39.78) | 26.95 ± 3.42 | 26.43 (21.19 ± 35.01) | −9.918 a | <0.001 * | <0.001 * |
| WC (cm) | 103.71 ± 10.33 | 103.50 (82.00–128.00) | 84.78 ± 7.55 | 85.00 (71.00–105.00) | 8.605 b | <0.001 * | <0.001 * |
| Body fat mass (kg) | 38.90 ± 10.76 | 37.25 (18.40–68.60) | 28.87 ± 9.30 | 27.80 (13.00–59.10) | 5.359 b | <0.001 * | <0.001 * |
| Lean body mass (kg) | 50.69 ± 8.22 | 49.55 (11.50–78.90) | 47.82 ± 4.26 | 47.10 (37.60–60.80) | 3.141 b | 0.014 * | 0.041 * |
| Body fat percentage (%) | 41.76 ± 5.45 | 42.35 (26.90–51.60) | 37.23 ± 6.85 | 37.60 (22.20–65.00) | −4.203 a | <0.001 * | 0.001 * |
| ABSI | 0.0798 ± 0.0065 | 0.0797 (0.0603–0.0933) | 0.0738 ± 0.0058 | 0.0742 (0.0605–0.0906) | 5.518 a | <0.001 * | <0.001 * |
| BRI | 6.44 ± 1.72 | 6.30 (2.74–10.83) | 3.73 ± 1.10 | 3.50 (2.06–6.70) | 8.236 b | <0.001 * | <0.001 * |
| DAI | 2.11 ± 1.52 | 1.80 (0.51–8.53) | 0.64 ± 0.27 | 0.56 (0.26–1.41) | 8.615 b | <0.001 * | <0.001 * |
| LAP | 87.21 ± 43.97 | 85.51 (24.00–249.14) | 24.66 ± 12.21 | 21.85 (8.95–57.29) | 9.041 b | <0.001 * | <0.001 * |
| VAI | 3.77 ± 2.73 | 3.26 (0.92–15.39) | 1.11 ± 0.48 | 0.99 (0.45–2.49) | 8.693 b | <0.001 * | <0.001 * |
| PCOS (+) (n = 66) | Control (n = 66) | ||||||
|---|---|---|---|---|---|---|---|
| Mean ± SD | Median (Min–Max) | Mean ± SD | Median (Min–Max) | t a/Z b | p-Value | Adjusted p-Value ** | |
| FPG (mg/dL) | 96.69 ± 12.49 | 95.00 (75.00–151.00) | 91.51 ± 7.76 | 91.00 (74.00–112.00) | 2.539 b | 0.011 * | 0.190 |
| Insulin (mg/dL) | 11.18 ± 3.39 | 11.40 (4.20–19.60) | 9.02 ± 3.52 | 7.90 (3.10–17.70) | 3.624 b | <0.001 * | 0.004 * |
| HbA1 c (%) | 5.53 ± 0.61 | 5.45 (4.20–8.50) | 5.21 ± 0.39 | 5.20 (4.20–6.20) | 3.651 b | <0.001 * | 0.025 * |
| HOMA-IR | 2.71 ± 1.04 | 2.42 (0.94–6.75) | 2.04 ± 0.84 | 1.77 (0.73–4.24) | 3.754 b | <0.001 * | 0.003 * |
| FSH (mlU/mL) | 7.15 ± 2.67 | 7.07 (2.23–11.49) | 5.87 ± 2.38 | 6.10 (0.43–10.29) | 2.713 b | 0.007 * | 0.069 |
| LH (mlU/mL) | 8.40 ± 3.26 | 7.47 (4.50–23.42) | 7.60 ± 3.63 | 7.07 (0.37–23.42) | 1.385 b | 0.166 | 0.256 |
| SHBG (nmol/L) | 32.94 ± 16.36 | 33.84 (10.16–75.80) | 68.22 ± 48.66 | 49.40 (12.20–229.00) | −5.554 b | <0.001 * | <0.001 * |
| Testosterone (ng/mL) | 85.34 ± 31.41 | 80.50 (36.00–174.00) | 60.00 ± 10.65 | 60.00 (36.00–101.00) | 5.056 b | <0.001 * | <0.001 * |
| DHEAS (mcg/dL) | 311.12 ± 109.00 | 307.00 (164.00–778.00) | 247.53 ± 126.57 | 214.50 (111.00–778.00) | 4.482 b | <0.001 * | 0.011 * |
| LH:FSH ratio | 1.41 ± 0.88 | 1.10 (0.39–4.60) | 1.53 ± 1.04 | 1.33 (0.05–6.56) | −0.856 b | 0.392 | 0.553 |
| CRP (mg/L) | 2.25 ± 1.38 | 2.05 (0.0–5.80) | 0.92 ± 0.62 | 0.80 (0.0–4.50) | 6.445 b | <0.001 * | <0.001 * |
| Total cholesterol (mg/dL) | 213.87 ± 43.15 | 212.50 (109.00–315.00) | 182.57 ± 35.06 | 182.00 (106.00–263.00) | −4.573 a | <0.001 * | <0.001 * |
| HDL-C (mg/dL) | 43.45 ± 9.94 | 44.00 (14.00–71.00) | 60.00 ± 10.65 | 60.00 (36.00–101.00) | 9.227 a | <0.001 * | <0.001 * |
| LDL-C (mg/dL) | 137.34 ± 38.89 | 137.50 (41.00–239.00) | 111.60 ± 31.34 | 109.00 (47.00–190.00) | −4.186 a | <0.001 * | <0.001 * |
| VLDL-C (mg/dL) | 33.81 ± 15.46 | 32.50 (10.00–85.00) | 16.17 ± 6.43 | 14.50 (6.00–35.00) | 7.403 b | <0.001 * | <0.001 * |
| TGs (mg/dL) | 169.26 ± 78.26 | 160.00 (52.00–424.00) | 81.88 ± 31.98 | 76.50 (36.00–174.00) | 7.314 b | <0.001 * | <0.001 * |
| SBP (mmHg) | 129.18 ± 13.14 | 130.00 (80.00–155.00) | 116.21 ± 11.69 | 117.50 (98.00–140.00) | 5.740 b | <0.001 * | <0.001 * |
| DBP (mmHg) | 81.46 ± 8.50 | 80.00 (60.00–110.00) | 74.46 ± 8.04 | 73.50 (60.00–100.00) | 4.872 b | <0.001 * | <0.001 * |
| BMI | WC | ABSI | VAI | LAP | DAI | BRI | ||
|---|---|---|---|---|---|---|---|---|
| FPG (mg/dL) | r | 0.263 | 0.214 | 0.006 | 0.126 | 0.138 | 0.122 | 0.205 |
| p | 0.002 ** | 0.014 * | 0.941 | 0.150 | 0.115 | 0.165 | 0.018 * | |
| Insulin (mg/dL) | r | 0.299 | 0.249 | 0.075 | 0.212 | 0.245 | 0.206 | 0.272 |
| p | <0.001 ** | 0.004 ** | 0.390 | 0.015 * | 0.005 ** | 0.018 * | 0.002 ** | |
| HbA1c (%) | r | 0.284 | 0.358 | 0.256 | 0.149 | 0.234 | 0.142 | 0.351 |
| p | 0.001 ** | <0.001 ** | 0.003 ** | 0.088 | 0.007 ** | 0.104 | <0.001 ** | |
| HOMA-IR | r | 0.338 | 0.268 | 0.060 | 0.216 | 0.251 | 0.210 | 0.287 |
| p | <0.001 ** | 0.002 ** | 0.497 | 0.013 * | 0.004 ** | 0.016 * | 0.001 ** | |
| FSH (mlU/mL) | r | 0.069 | 0.131 | 0.065 | 0.153 | 0.158 | 0.153 | 0.127 |
| p | 0.434 | 0.135 | 0.462 | 0.080 | 0.070 | 0.079 | 0.148 | |
| LH (mlU/mL) | r | 0.049 | 0.172 | 0.106 | 0.095 | 0.122 | 0.094 | 0.121 |
| p | 0.580 | 0.049 * | 0.226 | 0.278 | 0.163 | 0.284 | 0.166 | |
| SHBG (nmol/L) | r | −0.305 | −0.286 | −0.097 | −0.361 | −0.328 | −0.362 | −0.282 |
| p | <0.001 ** | 0.001 ** | 0.268 | <0.001 ** | <0.001 ** | <0.001 ** | 0.001 ** | |
| Testosterone (ng/mL) | r | 0.198 | 0.288 | 0.228 | 0.247 | 0.348 | 0.247 | 0.294 |
| p | 0.023 * | 0.001 ** | 0.008 ** | 0.004 ** | <0.001 ** | 0.004 ** | 0.001 ** | |
| DHEAS (nmol/L) | r | 0.275 | 0.328 | 0.197 | 0.311 | 0.340 | 0.307 | 0.299 |
| p | 0.001 ** | <0.001 ** | 0.024 * | <0.001 ** | <0.001 ** | <0.001 ** | 0.001 ** | |
| LH:FSH ratio | r | 0.032 | 0.035 | 0.007 | −0.039 | −0.027 | −0.041 | 0.005 |
| p | 0.717 | 0.692 | 0.937 | 0.657 | 0.762 | 0.642 | 0.955 | |
| CRP (mg/L) | r | 0.391 | 0.461 | 0.290 | 0.491 | 0.511 | 0.488 | 0.440 |
| p | <0.001 ** | <0.001 ** | 0.001 * | <0.001 ** | <0.001 ** | <0.001 ** | <0.001 ** | |
| Total cholesterol (mg/dL) | r | 0.345 | 0.370 | 0.181 | 0.545 | 0.598 | 0.544 | 0.394 |
| p | <0.001 ** | <0.001 ** | 0.038 * | <0.001 ** | <0.001 ** | <0.001 ** | <0.001 ** | |
| HDL-C (mg/dL) | r | −0.517 | −0.538 | −0.183 | −0.748 | −0.607 | −0.745 | −0.520 |
| p | <0.001 ** | <0.001 ** | 0.036 * | <0.001 ** | <0.001 ** | <0.001 ** | <0.001 ** | |
| LDL-C (mg/dL) | r | 0.316 | 0.363 | 0.186 | 0.513 | 0.526 | 0.514 | 0.375 |
| p | <0.001 ** | <0.001 ** | 0.033 * | <0.001 ** | <0.001 ** | <0.001 ** | <0.001 ** | |
| VLDL-C (mg/dL) | r | 0.465 | 0.475 | 0.254 | 0.903 | 0.861 | 0.905 | 0.479 |
| p | <0.001 ** | <0.001 ** | 0.003 ** | <0.001 ** | <0.001 ** | <0.001 ** | <0.001 ** | |
| TGs (mg/dL) | r | 0.485 | 0.485 | 0.256 | 0.943 | 0.903 | 0.945 | 0.497 |
| p | <0.001 ** | <0.001 ** | 0.003 ** | <0.001 ** | <0.001 ** | <0.001 ** | <0.001 ** | |
| SBP (mmHg) | r | 0.306 | 0.380 | 0.263 | 0.221 | 0.270 | 0.219 | 0.325 |
| p | <0.001 ** | <0.001 ** | 0.002 ** | 0.011 * | 0.002 ** | 0.012 * | <0.001 ** | |
| DBP (mmHg) | r | 0.199 | 0.261 | 0.201 | 0.249 | 0.226 | 0.250 | 0.247 |
| p | 0.022 * | 0.002 ** | 0.021 * | 0.004 ** | 0.009 ** | 0.004 ** | 0.004 ** |
| AUC (95%) | Cut-Off | p | Sensitivity (%) | Specificity (%) | |
|---|---|---|---|---|---|
| BMI | 0.887 (0.830–0.942) | 30.41 | 0.000 * | 80.3 | 80.3 |
| WC | 0.934 (0.894–0.974) | 91.50 | 0.000 * | 84.8 | 83.3 |
| ABSI | 0.762 (0.680–0.845) | 0.0772 | 0.000 * | 69.7 | 69.7 |
| BRI | 0.915 (0.868–0.963) | 4.7497 | 0.000 * | 83.3 | 83.3 |
| DAI | 0.935 (0.895–0.974) | 0.9432 | 0.000 * | 83.3 | 83.3 |
| LAP | 0.956 (0.927–0.985) | 40.3749 | 0.000 * | 84.8 | 84.8 |
| VAI | 0.938 (0.901–0.976) | 1.6556 | 0.000 * | 84.8 | 84.8 |
| AUC (95%) | Cut-Off | p | Sensitivity (%) | Specificity (%) | |
|---|---|---|---|---|---|
| BMI | 0.857 (0.792–0.922) | 30.18 | 0.000 * | 79.2 | 80.0 |
| WC | 0.895 (0.843–0.947) | 90.50 | 0.000 * | 83.3 | 80.0 |
| ABSI | 0.714 (0.627–0.801) | 0.0769 | 0.000 * | 66.7 | 63.3 |
| BRI | 0.866 (0.804–0.927) | 4.6383 | 0.000 * | 76.4 | 76.7 |
| DAI | 0.905 (0.855–0.956) | 0.8774 | 0.000 * | 81.9 | 81.7 |
| LAP | 0.927 (0.886–0.968) | 37.1488 | 0.000 * | 81.9 | 81.7 |
| VAI | 0.908 (0.858–0.957) | 1.5711 | 0.000 * | 81.9 | 81.7 |
| 95% Confidence Interval | 95% Confidence Interval | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor | Estimate | Lower | Upper | SE | Z | p-Value | Odds Ratio | Lower | Upper |
| Intercept | −16.415 | −26.5647 | −6.2661 | 5.1783 | −3.17 | 0.002 | 7.43 × 10−8 | 2.90 × 10−12 | 0.00190 |
| Age | −0.150 | −0.2709 | −0.0292 | 0.0617 | −2.43 | 0.015 * | 0.861 | 0.763 | 0.97119 |
| WC | 0.168 | 0.0700 | 0.2669 | 0.0502 | 3.35 | < 0.001 * | 1.183 | 1.072 | 1.305 |
| VAI | 3.171 | 1.4670 | 4.8749 | 0.8694 | 3.65 | < 0.001 * | 23.831 | 4.336 | 130.967 |
| 95% Confidence Interval | 95% Confidence Interval | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor | Estimate | Lower | Upper | SE | Z | p-Value | Odds Ratio | Lower | Upper |
| Intercept | −26.5558 | −40.3005 | −12.811 | 7.0127 | −3.79 | <0.001 | 2.93 × 10−12 | 3.15 × 10−18 | 2.73 × 10−6 |
| WC | 0.3468 | 0.1428 | 0.551 | 0.1041 | 3.33 | <0.001 * | 1.415 | 1.1534 | 1.735 |
| BRI | −1.8832 | −3.1668 | −0.600 | 0.6549 | −2.88 | 0.004 * | 0.152 | 0.0421 | 0.549 |
| LAP | 0.0909 | 0.0431 | 0.139 | 0.0244 | 3.73 | <0.001 * | 1.095 | 1.0441 | 1.149 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Çakır Biçer, N.; Ermiş, A.A.; Baş, D. The Role of Different Methods in Defining Cardiometabolic Risk and Metabolic Syndrome in Women with Polycystic Ovary Syndrome. Life 2023, 13, 1959. https://doi.org/10.3390/life13101959
Çakır Biçer N, Ermiş AA, Baş D. The Role of Different Methods in Defining Cardiometabolic Risk and Metabolic Syndrome in Women with Polycystic Ovary Syndrome. Life. 2023; 13(10):1959. https://doi.org/10.3390/life13101959
Chicago/Turabian StyleÇakır Biçer, Nihan, Asime Aleyna Ermiş, and Dilşat Baş. 2023. "The Role of Different Methods in Defining Cardiometabolic Risk and Metabolic Syndrome in Women with Polycystic Ovary Syndrome" Life 13, no. 10: 1959. https://doi.org/10.3390/life13101959
APA StyleÇakır Biçer, N., Ermiş, A. A., & Baş, D. (2023). The Role of Different Methods in Defining Cardiometabolic Risk and Metabolic Syndrome in Women with Polycystic Ovary Syndrome. Life, 13(10), 1959. https://doi.org/10.3390/life13101959






