Current Insights into Diagnosis, Prevention Strategies, Treatment, Therapeutic Targets, and Challenges of Monkeypox (Mpox) Infections in Human Populations
Abstract
1. Introduction
2. Survey Methodology
3. History
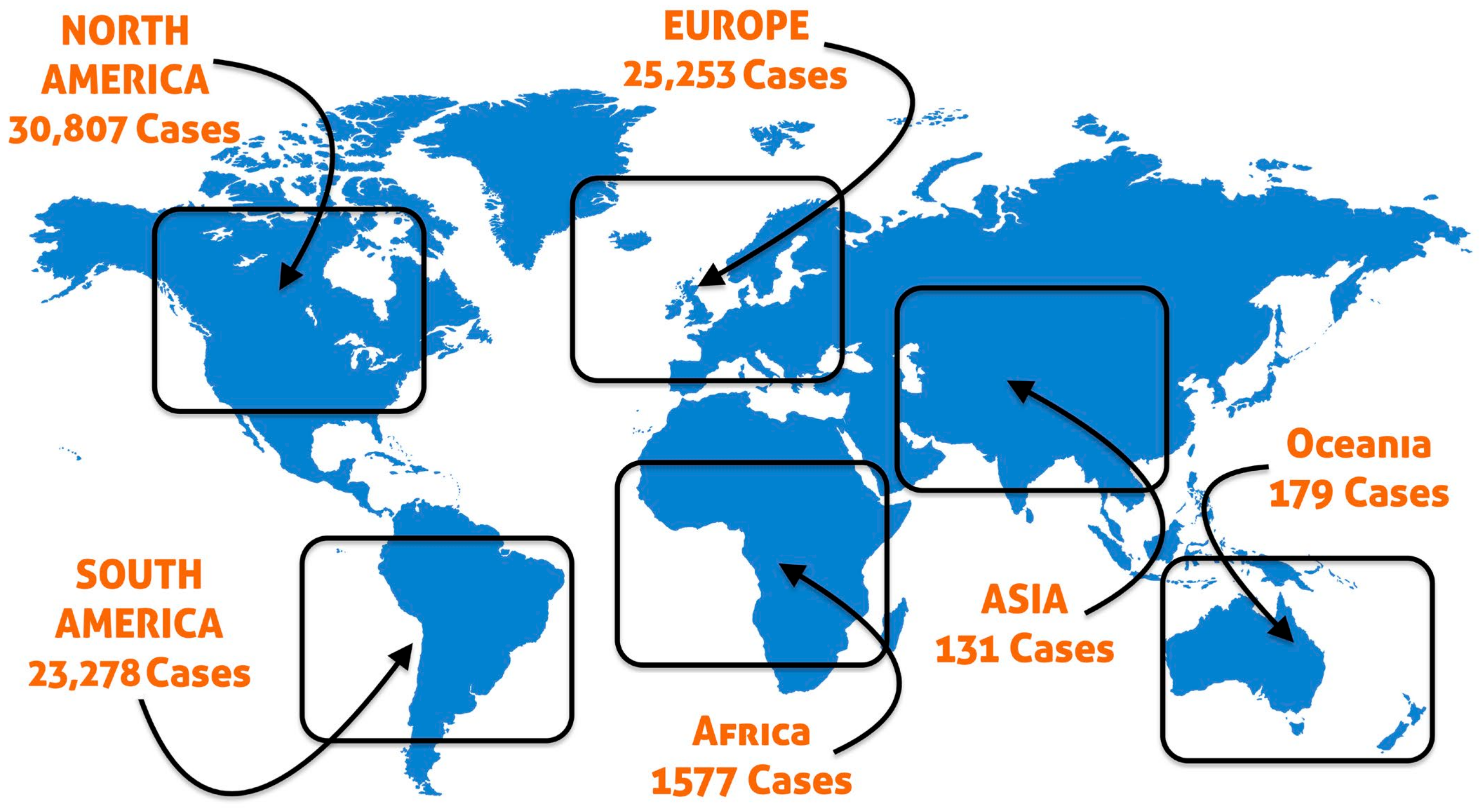
4. Origin and Spread of Mpox Virus
5. Transmission and Circulation of Mpox in Human Populations
5.1. United States Outbreak (2003)
5.2. Nigeria Outbreak (2017–2019)
5.3. United Kingdom Cases (2018)
5.4. Singapore Case (2019)
5.5. 2021 Cases
5.6. Current Outbreak (2022)
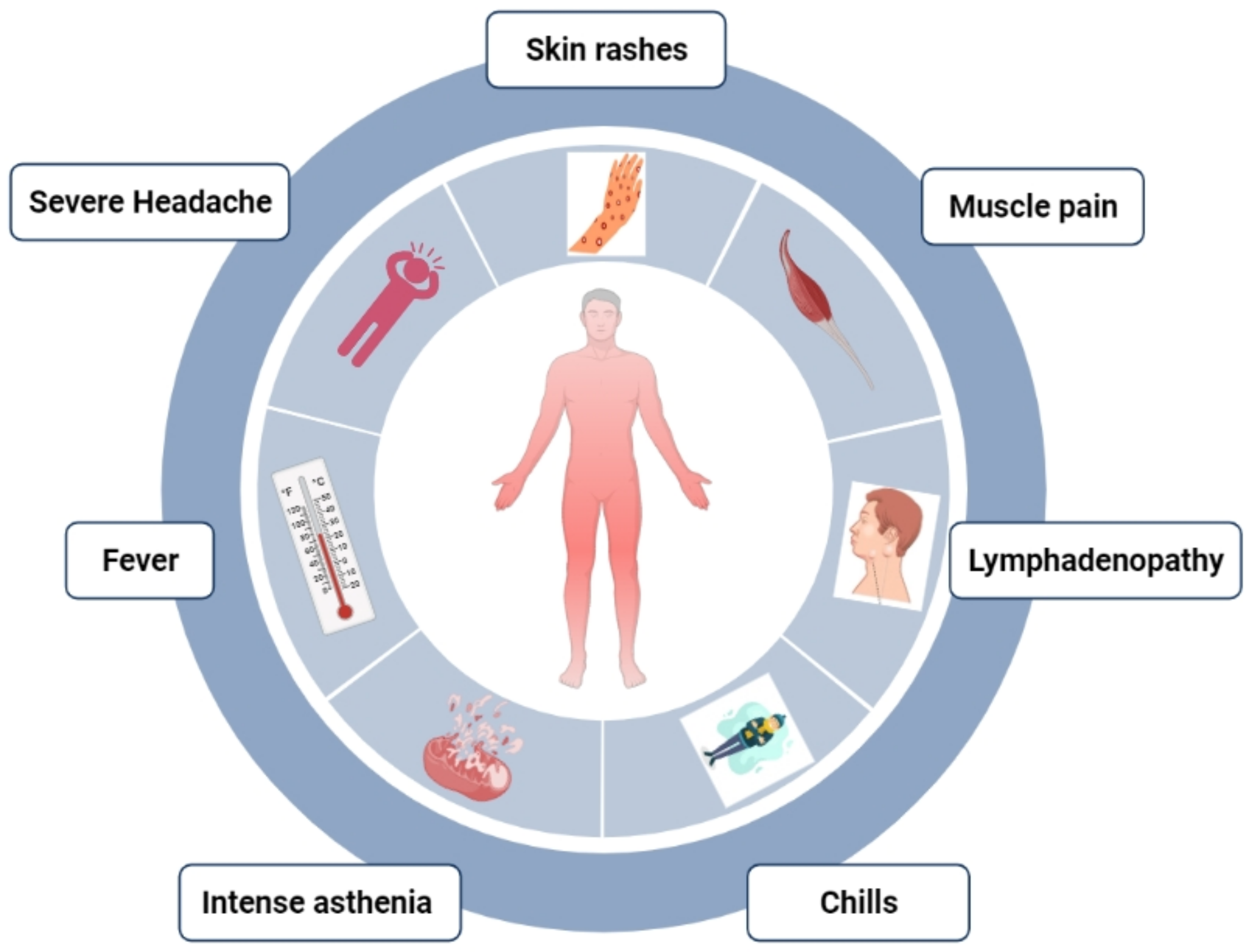
6. Clinical Features
7. Diagnosis
8. Therapeutics and Vaccines
8.1. Tecovirimat (TPOXX, ST-246)
8.2. Cidofovir
8.3. Brincidofovir (CMX001 or Tembexa)
8.4. Potential Therapeutic Targets
8.5. Thymidylate Kinase
8.6. DNA Ligase
8.7. D13L (Protein Trimer Complex)
8.8. F13L (Major Envelope Protein)
8.9. I7L (Cysteine Proteinase)
9. Prevention
10. Research Challenges with Mpox
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Adler, H.; Gould, S.; Hine, P.; Snell, L.B.; Wong, W.; Houlihan, C.F.; Osborne, J.C.; Rampling, T.; Beadsworth, M.B.J.; Duncan, C.J.A. Clinical Features and Management of Human Monkeypox: A Retrospective Observational Study in the UK. Lancet Infect. Dis. 2022, 22, 1153–1162. [Google Scholar] [CrossRef] [PubMed]
- Ladnyj, I.D.; Ziegler, P.; Kima, E. A Human Infection Caused by Monkeypox Virus in Basankusu Territory, Democratic Republic of the Congo. Bull. World Health Organ. 1972, 46, 593. [Google Scholar]
- Breman, J.G.; Henderson, D.A. Diagnosis and Management of Smallpox. N. Engl. J. Med. 2002, 346, 1300–1308. [Google Scholar] [CrossRef] [PubMed]
- Breman, J.G.; Steniowski, M.V.; Zanotto, E.; Gromyko, A.I.; Arita, I. Human Monkeypox, 1970–1979. Bull. World Health Organ. 1980, 58, 165. [Google Scholar] [PubMed]
- Damon, I.K. Status of Human Monkeypox: Clinical Disease, Epidemiology and Research. Vaccine 2011, 29, D54–D59. [Google Scholar] [CrossRef]
- Reuters. Germany Orders 40,000 Vaccine Doses as Precaution against Monkeypox Spread; Reuters: Canary Wharf, UK, 2022. [Google Scholar]
- Reuters. Britain’s UKHSA Says It Has Procured 20,000 Doses of Vaccine against Monkeypox; Reuters: Canary Wharf, UK, 2022. [Google Scholar]
- Breman, J.G.; Henderson, D.A. Poxvirus Dilemmas—Monkeypox, Smallpox, and Biologic Terrorism. N. Engl. J. Med. 1998, 339, 556–559. [Google Scholar] [CrossRef]
- Rao, A.K.; Petersen, B.W.; Whitehill, F.; Razeq, J.H.; Isaacs, S.N.; Merchlinsky, M.J.; Campos-Outcalt, D.; Morgan, R.L.; Damon, I.; Sánchez, P.J. Use of JYNNEOS (Smallpox and Monkeypox Vaccine, Live, Nonreplicating) for Preexposure Vaccination of Persons at Risk for Occupational Exposure to Orthopoxviruses: Recommendations of the Advisory Committee on Immunization Practices—United States, 2022. Morb. Mortal. Wkly. Rep. 2022, 71, 734. [Google Scholar] [CrossRef]
- Zumla, A.; Valdoleiros, S.R.; Haider, N.; Asogun, D.; Ntoumi, F.; Petersen, E.; Kock, R. Monkeypox Outbreaks Outside Endemic Regions: Scientific and Social Priorities. Lancet. Infect. Dis. 2022, 22, 929–931. [Google Scholar] [CrossRef]
- Brownworth, V.A. Analysis: Media Must Separate Monkeypox Risk from Stigma. Philadelphia Gay News 2022. Available online: https://epgn.com/2022/05/25/analysis-media-must-separate-monkeypox-risk-from-stigma/ (accessed on 24 September 2022).
- Petersen, B.W.; Damon, I.K. Smallpox, Mpox, and Other Poxvirus Infections. In Goldman-Cecil Medicine, 26th ed.; Elsevier: Philadelphia, PA, USA, 2020. [Google Scholar]
- Monkeypox: UNAIDS “Concerned” about Stigmatizing Language against LGTBI People. UN News. Available online: https://news.un.org/en/story/2022/05/1118762 (accessed on 24 September 2022).
- Monkeypox Spreads in West, Baffling African Scientists. TET News, 2022. Available online: https://economictimes.indiatimes.com/news/international/world-news/monkeypox-spreads-in-west-baffling-african-scientists/articleshow/91691647.cms (accessed on 24 September 2022).
- As Monkeypox Panic Spreads, Doctors in Africa See a Double Standard. Available online: www.washingtonpost.com (accessed on 24 September 2022).
- Monkeypox Conspiracy Theories: Five False Claims about the Virus Debunked as Misinformation Spreads Online. Available online: https://inews.co.uk/news/monkeypox-conspiracy-theories-false-claims-virus-debunked-misinformation-online-1645306 (accessed on 24 September 2022).
- US Let Monkeypox Loose’ Conspiracy Theories Swirl on China’s Weibo Platform. South China Morning Post, 2022. Available online: https://www.scmp.com/news/asia/article/3178814/us-let-monkeypox-loose-conspiracy-theories-swirl-chinas-weibo-platform (accessed on 24 September 2022).
- Hutson, C.L.; Lee, K.N.; Abel, J.; Carroll, D.S.; Montgomery, J.M.; Olson, V.A.; Li, Y.U.; Davidson, W.; Hughes, C.; Dillon, M. Monkeypox Zoonotic Associations: Insights from Laboratory Evaluation of Animals Associated with the Multi-State US Outbreak. Am. J. Trop. Med. Hyg. 2007, 76, 757–768. [Google Scholar] [CrossRef]
- Devaux, C.A.; Mediannikov, O.; Medkour, H.; Raoult, D. Infectious Disease Risk across the Growing Human-Non Human Primate Interface: A Review of the Evidence. Front. Public Health 2019, 7, 305. [Google Scholar] [CrossRef]
- Hutin, Y.J.; Williams, R.J.; Malfait, P.; Pebody, R.; Loparev, V.N.; Ropp, S.L.; Rodriguez, M.; Knight, J.C.; Tshioko, F.K.; Khan, A.S. Outbreak of Human Monkeypox, Democratic Republic of Congo, 1996 to 1997. Emerg. Infect. Dis. 2001, 7, 434. [Google Scholar] [CrossRef]
- Khodakevich, L.; Ježek, Z.; Messinger, D. Monkeypox Virus: Ecology and Public Health Significance. Bull. World Health Organ. 1988, 66, 747. [Google Scholar]
- Khodakevich, L.; Szczeniowski, M.; Jezek, Z.; Marennikova, S.; Nakano, J.; Messinger, D. The Role of Squirrels in Sustaining Monkeypox Virus Transmission. Trop. Geogr. Med. 1987, 39, 115–122. [Google Scholar]
- Von Magnus, P.; Andersen, E.K.; Petersen, K.B.; Birch-Andersen, A. A Pox-like Disease in Cynomolgus Monkeys. Acta Pathol. Microbiol. Scand. 1959, 46, 156–176. [Google Scholar] [CrossRef]
- Arita, I.; Henderson, D.A. Smallpox and Monkeypox in Non-Human Primates. Bull. World Health Organ. 1968, 39, 277. [Google Scholar]
- Radonić, A.; Metzger, S.; Dabrowski, P.W.; Couacy-Hymann, E.; Schuenadel, L.; Kurth, A.; Mätz-Rensing, K.; Boesch, C.; Leendertz, F.H.; Nitsche, A. Fatal Monkeypox in Wild-Living Sooty Mangabey, Cote d’Ivoire, 2012. Emerg. Infect. Dis. 2014, 20, 1009. [Google Scholar] [CrossRef]
- Foster, S.O.; Brink, E.W.; Hutchins, D.L.; Pifer, J.M.; Lourie, B.; Moser, C.R.; Cummings, E.C.; Kuteyi, O.E.K.; Eke, R.E.A.; Titus, J.B. Human Monkeypox. Bull. World Health Organ. 1972, 46, 569. [Google Scholar]
- Arita, I.; Jezek, Z.; Khodakevich, L.; Ruti, K. Human Monkeypox: A Newly Emerged Orthopoxvirus Zoonosis in the Tropical Rain Forests of Africa. Am. J. Trop. Med. Hyg. 1985, 34, 781–789. [Google Scholar] [CrossRef]
- Mbala, P.K.; Huggins, J.W.; Riu-Rovira, T.; Ahuka, S.M.; Mulembakani, P.; Rimoin, A.W.; Martin, J.W.; Muyembe, J.-J.T. Maternal and Fetal Outcomes among Pregnant Women with Human Monkeypox Infection in the Democratic Republic of Congo. J. Infect. Dis. 2017, 216, 824–828. [Google Scholar] [CrossRef]
- Sah, R.; Abdelaal, A.; Reda, A.; Katamesh, B.E.; Manirambona, E.; Abdelmonem, H.; Mehta, R.; Rabaan, A.A.; Alhumaid, S.; Alfouzan, W.A. Monkeypox and Its Possible Sexual Transmission: Where Are We Now with Its Evidence? Pathogens 2022, 11, 924. [Google Scholar] [CrossRef]
- Marennikova, S.S.; Šeluhina, E.M.; Mal’Ceva, N.N.; Čimiškjan, K.L.; Macevič, G.R. Isolation and Properties of the Causal Agent of a New Variola-like Disease (Monkeypox) in Man. Bull. World Health Organ. 1972, 46, 599. [Google Scholar] [PubMed]
- Kozlov, M. Monkeypox Goes Global: Why Scientists Are on Alert. Nature 2022, 606, 15–16. [Google Scholar] [CrossRef] [PubMed]
- Nolen, L.D.; Osadebe, L.; Katomba, J.; Likofata, J.; Mukadi, D.; Monroe, B.; Doty, J.; Hughes, C.M.; Kabamba, J.; Malekani, J. Extended Human-to-Human Transmission during a Monkeypox Outbreak in the Democratic Republic of the Congo. Emerg. Infect. Dis. 2016, 22, 1014. [Google Scholar] [CrossRef] [PubMed]
- Fuller, T.; Thomassen, H.A.; Mulembakani, P.M.; Johnston, S.C.; Lloyd-Smith, J.O.; Kisalu, N.K.; Lutete, T.K.; Blumberg, S.; Fair, J.N.; Wolfe, N.D. Using Remote Sensing to Map the Risk of Human Monkeypox Virus in the Congo Basin. Ecohealth 2011, 8, 14–25. [Google Scholar] [CrossRef] [PubMed]
- Bunge, E.M.; Hoet, B.; Chen, L.; Lienert, F.; Weidenthaler, H.; Baer, L.R.; Steffen, R. The Changing Epidemiology of Human Monkeypox—A Potential Threat? A Systematic Review. PLoS Negl. Trop. Dis. 2022, 16, e0010141. [Google Scholar] [CrossRef]
- Reynolds, M.G.; Davidson, W.B.; Curns, A.T.; Conover, C.S.; Huhn, G.; Davis, J.P.; Wegner, M.; Croft, D.R.; Newman, A.; Obiesie, N.N. Spectrum of Infection and Risk Factors for Human Monkeypox, United States, 2003. Emerg. Infect. Dis. 2007, 13, 1332. [Google Scholar] [CrossRef]
- Minhaj, F.S.; Ogale, Y.P.; Whitehill, F.; Schultz, J.; Foote, M.; Davidson, W.; Hughes, C.M.; Wilkins, K.; Bachmann, L.; Chatelain, R. Monkeypox Outbreak—Nine States, May 2022. Morb. Mortal. Wkly. Rep. 2022, 71, 764. [Google Scholar] [CrossRef]
- Kabuga, A.I.; El Zowalaty, M.E. A Review of the Monkeypox Virus and a Recent Outbreak of Skin Rash Disease in Nigeria. J. Med. Virol. 2019, 91, 533–540. [Google Scholar] [CrossRef]
- Yinka-Ogunleye, A.; Aruna, O.; Ogoina, D.; Aworabhi, N.; Eteng, W.; Badaru, S.; Mohammed, A.; Agenyi, J.; Etebu, E.N.; Numbere, T.-W. Reemergence of Human Monkeypox in Nigeria, 2017. Emerg. Infect. Dis. 2018, 24, 1149. [Google Scholar] [CrossRef]
- Okareh, O.T.; Morakinyo, O.M. Monkeypox in Nigeria: A Case Report of Re-Emerged Disease Outbreak. J. Microbiol. Exp. 2018, 6, 89–91. [Google Scholar]
- Fowotade, A.; Fasuyi, T.O.; Bakare, R.A. Re-Emergence of Monkeypox in Nigeria: A Cause for Concern and Public Enlightenment. African J. Clin. Exp. Microbiol. 2018, 19, 307–313. [Google Scholar] [CrossRef]
- Okanume, O. Ben Perception of Warri Metropolitan Residents on Online Newspaper Reportage of the Monkey Pox Virus Vaccination Hoax. Int. J. Multidiscip. Res. Publ. 2018, 1, 1–8. [Google Scholar]
- Silenou, B.C.; Tom-Aba, D.; Adeoye, O.; Arinze, C.C.; Oyiri, F.; Suleman, A.K.; Yinka-Ogunleye, A.; Dörrbecker, J.; Ihekweazu, C.; Krause, G. Use of Surveillance Outbreak Response Management and Analysis System for Human Monkeypox Outbreak, Nigeria, 2017–2019. Emerg. Infect. Dis. 2020, 26, 345. [Google Scholar] [CrossRef]
- Alakunle, E.; Moens, U.; Nchinda, G.; Okeke, M.I. Monkeypox Virus in Nigeria: Infection Biology, Epidemiology, and Evolution. Viruses 2020, 12, 1257. [Google Scholar] [CrossRef]
- Vivancos, R.; Anderson, C.; Blomquist, P.; Balasegaram, S.; Bell, A.; Bishop, L.; Brown, C.S.; Chow, Y.; Edeghere, O.; Florence, I. Community Transmission of Monkeypox in the United Kingdom, April to May 2022. Eurosurveillance 2022, 27, 2200422. [Google Scholar] [CrossRef]
- Vaughan, A.; Aarons, E.; Astbury, J.; Balasegaram, S.; Beadsworth, M.; Beck, C.R.; Chand, M.; O’connor, C.; Dunning, J.; Ghebrehewet, S. Two Cases of Monkeypox Imported to the United Kingdom, September 2018. Eurosurveillance 2018, 23, 1800509. [Google Scholar] [CrossRef]
- Hobson, G.; Adamson, J.; Adler, H.; Firth, R.; Gould, S.; Houlihan, C.; Johnson, C.; Porter, D.; Rampling, T.; Ratcliffe, L. Family Cluster of Three Cases of Monkeypox Imported from Nigeria to the United Kingdom, May 2021. Eurosurveillance 2021, 26, 2100745. [Google Scholar] [CrossRef]
- Monkeypox Outbreak: Epidemiological Overview 2023. Available online: https://www.gov.uk/government/publications/monkeypox-outbreak-epidemiological-overview/mpox-monkeypox-outbreak-epidemiological-overview-20-december-2022 (accessed on 24 September 2022).
- Ward, T.; Christie, R.; Paton, R.S.; Cumming, F.; Overton, C.E. Transmission Dynamics of Monekypox in the United Kingdom: Contact Tracing Study. BMJ 2022, 379, e073153. [Google Scholar] [CrossRef]
- Yong, S.E.F.; Ng, O.T.; Ho, Z.J.M.; Mak, T.M.; Marimuthu, K.; Vasoo, S.; Yeo, T.W.; Ng, Y.K.; Cui, L.; Ferdous, Z. Imported Monkeypox, Singapore. Emerg. Infect. Dis. 2020, 26, 1826. [Google Scholar] [CrossRef]
- Velavan, T.P.; Meyer, C.G. Monkeypox 2022 Outbreak: An Update. Trop. Med. Int. Health 2022, 27, 604–605. [Google Scholar] [CrossRef]
- Miura, F.; van Ewijk, C.E.; Backer, J.A.; Xiridou, M.; Franz, E.; de Coul, E.O.; Brandwagt, D.; van Cleef, B.; van Rijckevorsel, G.; Swaan, C. Estimated Incubation Period for Monkeypox Cases Confirmed in the Netherlands, May 2022. Eurosurveillance 2022, 27, 2200448. [Google Scholar] [CrossRef] [PubMed]
- Simoes, P.; Bhagani, S. A Viewpoint: The 2022 Monkeypox Outbreak 2022. J. Virus Erad. 2022, 8, 100078. [Google Scholar] [CrossRef] [PubMed]
- Jezek, Z.; Grab, B.; Paluku, K.M.; Szczeniowski, M.V. Human Monkeypox: Disease Pattern, Incidence and Attack Rates in a Rural Area of Northern Zaire. Trop. Geogr. Med. 1988, 40, 73–83. [Google Scholar] [PubMed]
- Ihekweazu, C.; Yinka-Ogunleye, A.; Lule, S.; Ibrahim, A. Importance of Epidemiological Research of Monkeypox: Is Incidence Increasing? Expert Rev. Anti. Infect. Ther. 2020, 18, 389–392. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO: Factsheet; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Sklenovska, N.; Van Ranst, M. Emergence of Monkeypox as the Most Important Orthopoxvirus Infection in Humans. Front. Public Health 2018, 6, 241. [Google Scholar] [CrossRef] [PubMed]
- Ježek, Z.; Szczeniowski, M.; Paluku, K.M.; Mutombo, M. Human Monkeypox: Clinical Features of 282 Patients. J. Infect. Dis. 1987, 156, 293–298. [Google Scholar] [CrossRef]
- Outbreak, M.-C.M. Situation Update; WHO: Geneva, Switzerland, 2022. [Google Scholar]
- Gilbourne, M. Monkeypox: Symptoms, Treatment, and Outcome—DermNet. Oakley, A.; Ed.; 2022. Available online: https://dermnetnz.org/ (accessed on 24 September 2022).
- Kulesh, D.A.; Loveless, B.M.; Norwood, D.; Garrison, J.; Whitehouse, C.A.; Hartmann, C.; Mucker, E.; Miller, D.; Wasieloski, L.P.; Huggins, J. Monkeypox Virus Detection in Rodents Using Real-Time 3′-Minor Groove Binder TaqMan® Assays on the Roche LightCycler. Lab. Investig. 2004, 84, 1200–1208. [Google Scholar] [CrossRef]
- Li, Y.; Olson, V.A.; Laue, T.; Laker, M.T.; Damon, I.K. Detection of Monkeypox Virus with Real-Time PCR Assays. J. Clin. Virol. 2006, 36, 194–203. [Google Scholar] [CrossRef]
- Olson, V.A.; Laue, T.; Laker, M.T.; Babkin, I.V.; Drosten, C.; Shchelkunov, S.N.; Niedrig, M.; Damon, I.K.; Meyer, H. Real-Time PCR System for Detection of Orthopoxviruses and Simultaneous Identification of Smallpox Virus. J. Clin. Microbiol. 2004, 42, 1940–1946. [Google Scholar] [CrossRef]
- Shchelkunov, S.N.; Shcherbakov, D.N.; Maksyutov, R.A.; Gavrilova, E. V Species-Specific Identification of Variola, Monkeypox, Cowpox, and Vaccinia Viruses by Multiplex Real-Time PCR Assay. J. Virol. Methods 2011, 175, 163–169. [Google Scholar] [CrossRef]
- Karem, K.L.; Reynolds, M.; Braden, Z.; Lou, G.; Bernard, N.; Patton, J.; Damon, I.K. Characterization of Acute-Phase Humoral Immunity to Monkeypox: Use of Immunoglobulin M Enzyme-Linked Immunosorbent Assay for Detection of Mpox Infection during the 2003 North American Outbreak. Clin. Vaccine Immunol. 2005, 12, 867–872. [Google Scholar] [CrossRef]
- McCollum, A.M.; Damon, I.K. Human Monkeypox. Clin. Infect. Dis. 2014, 58, 260–267. [Google Scholar] [CrossRef]
- World Health Organization. Laboratory Testing for the Monkeypox Virus: Interim Guidance; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Bazaid, A.S.; Barnawi, H.; Qanash, H.; Alsaif, G.; Aldarhami, A.; Gattan, H.; Alharbi, B.; Alrashidi, A.; Al-Soud, W.A.; Moussa, S. Bacterial Coinfection and Antibiotic Resistance Profiles among Hospitalised COVID-19 Patients. Microorganisms 2022, 10, 495. [Google Scholar] [CrossRef]
- Hadda, T.B.; Berredjem, M.; Almalki, F.A.; Rastija, V.; Jamalis, J.; Emran, T.B.; Abu-Izneid, T.; Esharkawy, E.; Rodriguez, L.C.; Alqahtani, A.M. How to Face COVID-19: Proposed Treatments Based on Remdesivir and Hydroxychloroquine in the Presence of Zinc Sulfate. Docking/DFT/POM Structural Analysis. J. Biomol. Struct. Dyn. 2021, 1–14. [Google Scholar]
- FDA Approves the First Drug with an Indication for Treatment of Smallpox. Available online: https://www.fda.gov/news-events/press-announcements/fda-approves-first-drug-indication-treatment-smallpox (accessed on 24 September 2022).
- Parker, S.; Handley, L.; Buller, R.M. Therapeutic and Prophylactic Drugs to Treat Orthopoxvirus Infections. Future Med. 2008, 3. [Google Scholar] [CrossRef]
- Lederman, E.R.; Davidson, W.; Groff, H.L.; Smith, S.K.; Warkentien, T.; Li, Y.; Wilkins, K.A.; Karem, K.L.; Akondy, R.S.; Ahmed, R. Progressive Vaccinia: Case Description and Laboratory-Guided Therapy with Vaccinia Immune Globulin, ST-246, and CMX001. J. Infect. Dis. 2012, 206, 1372–1385. [Google Scholar] [CrossRef]
- CDC. Mpox Treatment Information for Healthcare Professionals Interim Clinical Guidance for the Treatment of Monkeypox Medical Countermeasures Available for the Treatment of Monkeypox; CDC: Atlanta, GA, USA, 2022.
- Grosenbach, D.W.; Honeychurch, K.; Rose, E.A.; Chinsangaram, J.; Frimm, A.; Maiti, B.; Lovejoy, C.; Meara, I.; Long, P.; Hruby, D.E. Oral Tecovirimat for the Treatment of Smallpox. N. Engl. J. Med. 2018, 379, 44–53. [Google Scholar] [CrossRef]
- O’Laughlin, K.; Tobolowsky, F.A.; Elmor, R.; Overton, R.; O’Connor, S.M.; Damon, I.K.; Petersen, B.W.; Rao, A.K.; Chatham-Stephens, K.; Yu, P. Clinical Use of Tecovirimat (Tpoxx) for Treatment of Monkeypox under an Investigational New Drug Protocol—United States, May–August 2022; CDC: Atlanta, GA, USA, 2022.
- Stittelaar, K.J.; Neyts, J.; Naesens, L.; Van Amerongen, G.; Van Lavieren, R.F.; Holý, A.; De Clercq, E.; Niesters, H.G.M.; Fries, E.; Maas, C. Antiviral Treatment Is More Effective than Smallpox Vaccination upon Lethal Monkeypox Virus Infection. Nature 2006, 439, 745–748. [Google Scholar] [CrossRef]
- Smee, D.F. Progress in the Discovery of Compounds Inhibiting Orthopoxviruses in Animal Models. Antivir. Chem. Chemother. 2008, 19, 115–124. [Google Scholar] [CrossRef]
- Baker, R.O.; Bray, M.; Huggins, J.W. Potential Antiviral Therapeutics for Smallpox, Monkeypox and Other Orthopoxvirus Infections. Antivir. Res. 2003, 57, 13–23. [Google Scholar] [CrossRef]
- FDA. FDA Approves Drug to Treat Smallpox; FDA: Silver Spring, MD, USA, 2022.
- Parker, S.; Chen, N.G.; Foster, S.; Hartzler, H.; Hembrador, E.; Hruby, D.; Jordan, R.; Lanier, R.; Painter, G.; Painter, W. Evaluation of Disease and Viral Biomarkers as Triggers for Therapeutic Intervention in Respiratory Mousepox–an Animal Model of Smallpox. Antivir. Res. 2012, 94, 44–53. [Google Scholar] [CrossRef] [PubMed]
- Hutson, C.L.; Kondas, A.V.; Mauldin, M.R.; Doty, J.B.; Grossi, I.M.; Morgan, C.N.; Ostergaard, S.D.; Hughes, C.M.; Nakazawa, Y.; Kling, C. Pharmacokinetics and Efficacy of a Potential Smallpox Therapeutic, Brincidofovir, in a Lethal Monkeypox Virus Animal Model. MSphere 2021, 6, e00927-20. [Google Scholar] [CrossRef] [PubMed]
- Rice, A.D.; Adams, M.M.; Wallace, G.; Burrage, A.M.; Lindsey, S.F.; Smith, A.J.; Swetnam, D.; Manning, B.R.; Gray, S.A.; Lampert, B. Efficacy of CMX001 as a Post Exposure Antiviral in New Zealand White Rabbits Infected with Rabbitpox Virus, a Model for Orthopoxvirus Infections of Humans. Viruses 2011, 3, 47–62. [Google Scholar] [CrossRef] [PubMed]
- Sherwat, A.; Brooks, J.T.; Birnkrant, D.; Kim, P. Tecovirimat and the Treatment of Mpox—Past, Present, and Future Considerations. N. Engl. J. Med. 2022, 387, 579–581. [Google Scholar] [CrossRef] [PubMed]
- Vora, S.; Damon, I.; Fulginiti, V.; Weber, S.G.; Kahana, M.; Stein, S.L.; Gerber, S.I.; Garcia-Houchins, S.; Lederman, E.; Hruby, D. Severe Eczema Vaccinatum in a Household Contact of a Smallpox Vaccinee. Clin. Infect. Dis. 2008, 46, 1555–1561. [Google Scholar] [CrossRef]
- Khalid, S.; Almalki, F.A.; Hadda, T.B.; Bader, A.; Abu-Izneid, T.; Berredjem, M.; Elsharkawy, E.R.; Alqahtani, A.M. Medicinal Applications of Cannabinoids Extracted from Cannabis sativa (L.): A New Route in the Fight against COVID-19? Curr. Pharm. Des. 2021, 27, 1564–1578. [Google Scholar] [CrossRef]
- Alandijany, T.A.; El-Kafrawy, S.A.; Al-Ghamdi, A.A.; Qashqari, F.S.; Faizo, A.A.; Tolah, A.M.; Hassan, A.M.; Sohrab, S.S.; Hindawi, S.I.; Badawi, M.A. Lack of Antibodies to SARS-CoV-2 among Blood Donors during COVID-19 Lockdown: A Study from Saudi Arabia. Healthcare 2021, 9, 51. [Google Scholar] [CrossRef]
- Control, C. for D.; Prevention Vaccinia (Smallpox) Vaccine, Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2001. Mortal Morb Wkly Rep. 2001, 50, 1–25. [Google Scholar]
- Stittelaar, K.J.; van Amerongen, G.; Kondova, I.; Kuiken, T.; van Lavieren, R.F.; Pistoor, F.H.M.; Niesters, H.G.M.; van Doornum, G.; van der Zeijst, B.A.M.; Mateo, L. Modified Vaccinia Virus Ankara Protects Macaques against Respiratory Challenge with Monkeypox Virus. J. Virol. 2005, 79, 7845–7851. [Google Scholar] [CrossRef]
- Petersen, B.W.; Damon, I.K.; Pertowski, C.A.; Meaney-Delman, D.; Guarnizo, J.T.; Beigi, R.H.; Edwards, K.M.; Fisher, M.C.; Frey, S.E.; Lynfield, R. Clinical Guidance for Smallpox Vaccine Use in a Postevent Vaccination Program. Morb. Mortal. Wkly. Rep. Recomm. Rep. 2015, 64, 1–26. [Google Scholar]
- Petersen, B.W.; Kabamba, J.; McCollum, A.M.; Lushima, R.S.; Wemakoy, E.O.; Tamfum, J.-J.M.; Nguete, B.; Hughes, C.M.; Monroe, B.P.; Reynolds, M.G. Vaccinating against Monkeypox in the Democratic Republic of the Congo. Antiviral Res. 2019, 162, 171–177. [Google Scholar] [CrossRef]
- Shchelkunov, S.N.; Totmenin, A.V.; Babkin, I.V.; Safronov, P.F.; Ryazankina, O.I.; Petrov, N.A.; Gutorov, V.V.; Uvarova, E.A.; Mikheev, M.V.; Sisler, J.R. Human Monkeypox and Smallpox Viruses: Genomic Comparison. FEBS Lett. 2001, 509, 66–70. [Google Scholar] [CrossRef]
- Caillat, C.; Topalis, D.; Agrofoglio, L.A.; Pochet, S.; Balzarini, J.; Deville-Bonne, D.; Meyer, P. Crystal Structure of Poxvirus Thymidylate Kinase: An Unexpected Dimerization Has Implications for Antiviral Therapy. Proc. Natl. Acad. Sci. USA 2008, 105, 16900–16905. [Google Scholar] [CrossRef]
- Prichard, M.N.; Kern, E.R. Orthopoxvirus Targets for the Development of New Antiviral Agents. Antivir. Res. 2012, 94, 111–125. [Google Scholar] [CrossRef]
- Deng, L.; Dai, P.; Ciro, A.; Smee, D.F.; Djaballah, H.; Shuman, S. Identification of Novel Antipoxviral Agents: Mitoxantrone Inhibits Vaccinia Virus Replication by Blocking Virion Assembly. J. Virol. 2007, 81, 13392–13402. [Google Scholar] [CrossRef]
- Bahar, M.W.; Graham, S.C.; Stuart, D.I.; Grimes, J.M. Insights into the Evolution of a Complex Virus from the Crystal Structure of Vaccinia Virus D13. Structure 2011, 19, 1011–1020. [Google Scholar] [CrossRef]
- Garriga, D.; Headey, S.; Accurso, C.; Gunzburg, M.; Scanlon, M.; Coulibaly, F. Structural Basis for the Inhibition of Poxvirus Assembly by the Antibiotic Rifampicin. Proc. Natl. Acad. Sci. USA 2018, 115, 8424–8429. [Google Scholar] [CrossRef]
- Moss, B. Membrane Fusion during Poxvirus Entry. In Proceedings of the Seminars in Cell & Developmental Biology; Elsevier: Amsterdam, The Netherlands, 2016; Volume 60, pp. 89–96. [Google Scholar]
- Byrd, C.M.; Bolken, T.; Mjalli, A.M.; Arimilli, M.N.; Andrews, R.C.; Rothlein, R.; Andrea, T.; Rao, M.; Owens, K.L.; Hruby, D.E. New Class of Orthopoxvirus Antiviral Drugs That Block Viral Maturation. J. Virol. 2004, 78, 12147–12156. [Google Scholar] [CrossRef]
- Zephyr, J.; Yilmaz, N.K.; Schiffer, C.A. Viral Proteases: Structure, Mechanism and Inhibition. In The Enzymes; Elsevier: Amsterdam, The Netherlands, 2021; Volume 50, pp. 301–333. ISBN 1874–6047. [Google Scholar]
- Tufail, A.; Pullan, S.; Amini, A.; Komath, D. Deep Masseteric Layer. Br. Dent. J. 2022, 232, 760. [Google Scholar] [CrossRef]
- Petersen, E.; Kantele, A.; Koopmans, M.; Asogun, D.; Yinka-Ogunleye, A.; Ihekweazu, C.; Zumla, A. Human Monkeypox: Epidemiologic and Clinical Characteristics, Diagnosis, and Prevention. Infect. Dis. Clin. 2019, 33, 1027–1043. [Google Scholar] [CrossRef]
- Roess, A.A.; Monroe, B.P.; Kinzoni, E.A.; Gallagher, S.; Ibata, S.R.; Badinga, N.; Molouania, T.M.; Mabola, F.S.; Mombouli, J.V.; Carroll, D.S. Assessing the Effectiveness of a Community Intervention for Monkeypox Prevention in the Congo Basin. PLoS Negl. Trop. Dis. 2011, 5, e1356. [Google Scholar] [CrossRef] [PubMed]
- Lederman, E.R.; Reynolds, M.G.; Karem, K.; Braden, Z.; Learned-Orozco, L.A.; Wassa-Wassa, D.; Moundeli, O.; Hughes, C.; Harvey, J.; Regnery, R. Prevalence of Antibodies against Orthopoxviruses among Residents of Likouala Region, Republic of Congo: Evidence for Monkeypox Virus Exposure. Am. J. Trop. Med. Hyg. 2007, 77, 1150–1156. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patel, M.; Adnan, M.; Aldarhami, A.; Bazaid, A.S.; Saeedi, N.H.; Alkayyal, A.A.; Saleh, F.M.; Awadh, I.B.; Saeed, A.; Alshaghdali, K. Current Insights into Diagnosis, Prevention Strategies, Treatment, Therapeutic Targets, and Challenges of Monkeypox (Mpox) Infections in Human Populations. Life 2023, 13, 249. https://doi.org/10.3390/life13010249
Patel M, Adnan M, Aldarhami A, Bazaid AS, Saeedi NH, Alkayyal AA, Saleh FM, Awadh IB, Saeed A, Alshaghdali K. Current Insights into Diagnosis, Prevention Strategies, Treatment, Therapeutic Targets, and Challenges of Monkeypox (Mpox) Infections in Human Populations. Life. 2023; 13(1):249. https://doi.org/10.3390/life13010249
Chicago/Turabian StylePatel, Mitesh, Mohd Adnan, Abdu Aldarhami, Abdulrahman S. Bazaid, Nizar H. Saeedi, Almohanad A. Alkayyal, Fayez M. Saleh, Ibrahim B. Awadh, Amir Saeed, and Khalid Alshaghdali. 2023. "Current Insights into Diagnosis, Prevention Strategies, Treatment, Therapeutic Targets, and Challenges of Monkeypox (Mpox) Infections in Human Populations" Life 13, no. 1: 249. https://doi.org/10.3390/life13010249
APA StylePatel, M., Adnan, M., Aldarhami, A., Bazaid, A. S., Saeedi, N. H., Alkayyal, A. A., Saleh, F. M., Awadh, I. B., Saeed, A., & Alshaghdali, K. (2023). Current Insights into Diagnosis, Prevention Strategies, Treatment, Therapeutic Targets, and Challenges of Monkeypox (Mpox) Infections in Human Populations. Life, 13(1), 249. https://doi.org/10.3390/life13010249








