Artificial Intelligence and Precision Medicine: A New Frontier for the Treatment of Brain Tumors
Abstract
1. Introduction
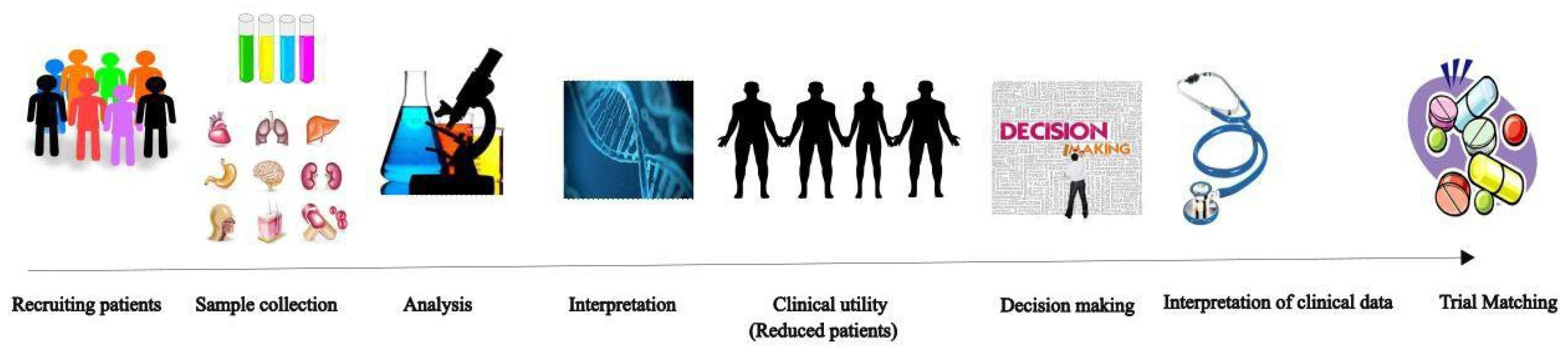
1.1. Molecular and Genomic Profiling of Brain Tumors and the Use of PM
1.2. MicroRNA (miRNA) Panels as Markers in Brain Tumors
2. AI in Brain Tumor Imaging
2.1. Quantitative Imaging of Brain Tumors
2.2. Radiomics in Brain Tumor Diagnosis
2.3. Convolutional Neural Networks for Clinical Diagnostics
3. Future of AI in Brain Tumor
4. Challenges for Using AI with Brain Tumors
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Alnaami, I.; Sarhan, L.; Alqahtani, A.; Alghamdi, A.; Alkhashrami, S.; Mostafa, O. Does brain tumor epidemiology differ from place to another? Saudi single tertiary care center experience. Biomed. Res. 2018, 29, 2982–2987. [Google Scholar] [CrossRef]
- Chang, J.; Guo, C.; Li, J.; Liang, Z.; Wang, Y.; Yu, A.; Liu, R.; Guo, Y.; Chen, J.; Huang, S. EN1 regulates cell growth and proliferation in human glioma cells via Hedgehog signaling. Int. J. Mol. Sci. 2022, 23, 1123. [Google Scholar] [CrossRef] [PubMed]
- Chevli, N.; Hunt, A.; Haque, W.; Farach, A.M.; Messer, J.A.; Sukpraprut-Braaten, S.; Bernicker, E.H.; Zhang, J.; Butler, E.B.; Teh, B.S. Time Interval to Initiation of Whole-Brain Radiation Therapy in Patients With Small Cell Lung Cancer With Brain Metastasis. Adv. Rad. Oncol. 2021, 6, 100783. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Song, S.; Su, X.; Wu, J.; Dai, Z.; Cui, D.; Reng, Y.; Fan, J.; Shen, Y.; Wu, Q.; et al. Radiation-induced glioblastoma with rhabdoid characteristics following treatment for medulloblastoma: A case report and review of the literature. Mol. Clin. Oncol. 2018, 9, 415–418. [Google Scholar] [CrossRef] [PubMed]
- de Sousa e Melo, F.; Vermeulen, L.; Fessler, E.; Medema, J.P. Cancer heterogeneity-a multifaceted view. EMBO Rep. 2013, 14, 686–695. [Google Scholar] [CrossRef]
- Zhu, X.; Sun, Y.; Liu, H.; Li, Q.; Xu, H. Simulation of the spiking neural network based on practical memristor. MATEC Web Conf. 2018, 173, 1–4. [Google Scholar] [CrossRef][Green Version]
- Shoeibi, A.; Khodatars, M.; Alizadehsani, R.; Ghassemi, N.; Jafari, M.; Moridian, P.; Khadem, A.; Sadeghi, D.; Hussain, S.; Zare, A.; et al. Automated detection and forecasting of COVID-19 using deep learning techniques: A review. arXiv 2020, arXiv:2007.10785. [Google Scholar] [CrossRef]
- Mittal, A.; Kumar, D. Ai CNNs (Artificially-integrated convolutional neural networks) for brain tumor prediction. PHAT 2019, 17, e5. [Google Scholar] [CrossRef]
- Jian, A.; Liu, S.; Ieva, A.D. Artificial intelligence for survival prediction in brain tumors on neuroimaging. Neurosurgery 2022, 91, 8–26. [Google Scholar] [CrossRef]
- Sun, Y.; Zhu, S.; Ma, K.; Liu, W.; Yue, Y.; Hu, G.; Lu, H.; Chen, W. Identification of 12 cancer types through genome deep learning. Sci. Rep. 2019, 9, 17256. [Google Scholar] [CrossRef]
- Johnson, K.B.; Wei, W.Q.; Weeraratne, D.; Frisse, M.E.; Misulis, K.; Rhee, K.; Zhao, J.; Snowdon, J.L. Precision medicine, AI, and the future of personalized health care. Clin. Transl. Sci. 2020, 14, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Nwoye, E.O.; Woo, W.L.; Gao, B.; Anyanwu, T. Artificial intelligence for emerging technology in surgery: Systematic review and validation. IEEE Rev. Biomed. Eng. 2022, 16, 1–22. [Google Scholar] [CrossRef]
- Owoyemi, A.; Owoyemi, J.; Osiyemi, A.; Boyd, A. Artificial Intelligence for Healthcare in Africa. Front. Digit. Health 2020, 2, 6. [Google Scholar] [CrossRef] [PubMed]
- Soellner, M.; Koenigstorfer, J. Compliance with medical recommendations depending on the use of artificial intelligence as a diagnostic method. BMC Med. Inform. Decis. Mak. 2021, 21, 236. [Google Scholar] [CrossRef]
- Carrillo-Perez, F.; Pecho, O.E.; Morales, J.C.; Paravina, R.D.; Bona, A.D.; Ghinea, R.; Pulgar, R.; del Mar Pérez, M.; Herrera, L.J. Applications of artificial intelligence in dentistry: A comprehensive review. J. Esthet. Restor. Dent. 2021, 34, 259–280. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, A.; Dar, G.M. A comprehensive review on the application of artificial intelligence in drug discovery. Appl. Biol. Chem. J. 2021, 2, 34–48. [Google Scholar] [CrossRef]
- Paul, D.; Sanap, G.; Shenoy, S.; Kalyane, D.; Kalia, K.; Tekade, R.K. Artificial intelligence in drug discovery and development. Drug Discov. Today 2021, 26, 80–93. [Google Scholar] [CrossRef]
- Barinov, L.; Jairaj, A.; Becker, M.D.; Seymour, S.; Lee, E.; Schram, A.W.; Lane, E.; Goldszal, A.F.; Quigley, D.; Paster, L. Impact of data presentation on physician performance utilizing artificial intelligence-based computer-aided diagnosis and decision support systems. J. Digit. Imaging 2019, 32, 408–416. [Google Scholar] [CrossRef]
- Karnuta, J.M.; Luu, B.C.; Haeberle, H.S.; Saluan, P.M.; Frangiamore, S.J.; Stearns, K.L.; Farrow, L.D.; Nwachukwu, B.U.; Verma, N.N.; Makhni, E.C.; et al. Machine learning outperforms regression analysis to predict next-season major league baseball player injuries: Epidemiology and validation of 13, 982 player-years from performance and injury profile trends, 2000–2017. Orthop. J. Sport. Med. 2020, 8, 2325967120963046. [Google Scholar] [CrossRef]
- Bohr, A.; Memarzadeh, K. The rise of artificial intelligence in healthcare applications. In Artificial Intelligence in Healthcare; Academic Press: Cambridge, MA, USA, 2020; pp. 25–60. [Google Scholar] [CrossRef]
- Lee, M.S.; Flammer, A.J.; Lerman, L.O.; Lerman, A. Personalized medicine in cardiovascular diseases. Korean Circ. J. 2012, 42, 583. [Google Scholar] [CrossRef]
- Chowkwanyun, M.; Bayer, R.; Galea, S. Public health-between novelty and hype. N. Engl. J. Med. 2018, 379, 1398–1400. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, K.C.K.; Khanna, C.; Hendricks, W.; Trent, J.; Kotlikoff, M. Precision medicine: An opportunity for a paradigm shift in veterinary medicine. J. Am. Vet. Med. Assoc. 2016, 248, 45–48. [Google Scholar] [CrossRef] [PubMed]
- Amedei, A.; Boem, F. I’ve Gut A Feeling: Microbiota impacting the conceptual and experimental perspectives of personalized medicine. Int. J. Mol. Sci. 2018, 19, 3756. [Google Scholar] [CrossRef]
- Gourraud, P.A.; Henry, R.G.; Cree, B.A.C.; Crane, J.C.; Lizee, A.; Olson, M.P.; Santaniello, A.V.; Datta, E.; Zhu, A.H.; Bevan, C.J.; et al. Precision medicine in chronic disease management: The multiple sclerosis BioScreen. Ann. Neurol. 2014, 76, 633–642. [Google Scholar] [CrossRef]
- Leopold, J.A.; Maron, B.A.; Loscalzo, J. The application of big data to cardiovascular disease: Paths to precision medicine. J. Clin. Investig. 2020, 130, 29–38. [Google Scholar] [CrossRef]
- Narimatsu, H. Gene interactions in preventive medicine: Current status and expectations for the future. Int. J. Mol. Sci. 2017, 18, 302. [Google Scholar] [CrossRef] [PubMed]
- Vargas, A.J.; Harris, C.C. Biomarker development in the precision medicine era: Lung cancer as a case study. Nat. Rev. Cancer 2016, 16, 525–537. [Google Scholar] [CrossRef]
- Simmons, M.; Singhal, A.; Lu, Z. Text mining for precision medicine: Bringing structure to EHRs and biomedical literature to understand genes and health. Adv. Exp. Med. Biol. 2016, 939, 139–166. [Google Scholar] [CrossRef]
- Roberts, K.; Demner-Fushman, D.; Voorhees, E.M.; Hersh, W.R.; Bedrick, S.; Lazar, A.J.; Pant, S. Overview of the TREC 2020 precision medicine track. Text Retr. Conf. 2020, 1266, 1–10. [Google Scholar]
- Lauko, A.J.; Lo, A.; Ahluwalia, M.S.; Lathia, J.D. Cancer cell heterogeneity & plasticity in glioblastoma and brain tumors. Semin. Cancer Biol. 2022, 82, 162–175. [Google Scholar] [CrossRef]
- Schmelz, K.; Toedling, J.; Huska, M.R.; Cwikla, M.C.; Kruetzfeldt, L.M.; Proba, J.; Ambros, P.F.; Ambros, I.M.; Boral, S.; Lodrini, M.; et al. Spatial and temporal intratumour heterogeneity has potential consequences for single biopsy-based neuroblastoma treatment decisions. Nat. Commun. 2021, 12, 6804. [Google Scholar] [CrossRef] [PubMed]
- Pribluda, A.; de la Cruz, C.C.; Jackson, E.L. Intratumoral heterogeneity: From diversity comes resistance. Clin. Cancer Res. 2015, 21, 2916–2923. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.; Nilendu, P.; Jahagirdar, D.; Pal, J.K.; Sharma, N.K. Modulating secreted components of tumor microenvironment: A masterstroke in tumor therapeutics. Cancer Biol. Ther. 2017, 19, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Woldu, S.L.; Amatruda, J.F.; Bagrodia, A. Testicular germ cell tumor genomics. Curr. Opin. Urol. 2017, 27, 41–47. [Google Scholar] [CrossRef]
- Tu, S.M.; Bilen, M.A.; Hess, K.R.; Broaddus, R.R.; Kopetz, S.; Wei, C.; Pagliaro, L.C.; Karam, J.A.; Ward, J.F.; Wood, C.G.; et al. Intratumoral heterogeneity: Role of differentiation in a potentially lethal phenotype of testicular cancer. Cancer 2016, 122, 1836–1843. [Google Scholar] [CrossRef]
- Ghiaseddin, A.; Minh, L.B.H.; Janiszewska, M.; Shin, D.; Wick, W.; Mitchell, D.A.; Wen, P.Y.; Grossman, S.A. Adult precision medicine: Learning from the past to enhance the future. Neurooncol. Adv. 2020, 3, vdaa145. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, C.D.; Alnahhas, I.; Gonzalez, J.; Giglio, P.; Puduvalli, V.K. Changing Paradigms for Targeted Therapies against Diffuse Infiltrative Gliomas: Tackling a Moving Target. Expert Rev. Neurother. 2019, 19, 663–677. [Google Scholar] [CrossRef]
- Wu, J.; Zhang, J.; Wei, J.; Zhao, Y.; Gao, Y. Urinary biomarker discovery in gliomas using mass spectrometry-based clinical proteomics. Chin. Neurosurg. J. 2020, 6, 11. [Google Scholar] [CrossRef]
- Pantel, K.; Alix-Panabières, C. Liquid biopsy and minimal residual disease—Latest advances and implications for cure. Nat. Rev. Clin. Oncol. 2019, 16, 409–424. [Google Scholar] [CrossRef]
- Sheng, Z.; Yu, J.; Deng, K.; Andrade-Barazarte, H.; Zemmar, A.; Li, S.; Li, N.; Yan, Z.; Chen, Z.; Sun, Y.; et al. Characterizing the genomic landscape of brain glioma with circulating tumor DNA from tumor in situ fluid. Front. Oncol. 2021, 11, 584988. [Google Scholar] [CrossRef]
- Molinari, C.; Marisi, G.; Passardi, A.; Matteucci, L.; De Maio, G.; Ulivi, P. Heterogeneity in colorectal cancer: A challenge for personalized medicine? Int. J. Mol. Sci. 2018, 19, 3733. [Google Scholar] [CrossRef] [PubMed]
- Schork, N.J. Personalized medicine: Time for one-person trials. Nature 2015, 520, 609–611. [Google Scholar] [CrossRef] [PubMed]
- Deluche, E.; Onesti, E.; Andre, F. Precision medicine for metastatic breast cancer. Am. Soc. Clin. Oncol. Educ. Book 2015, 35, e2–e7. [Google Scholar] [CrossRef] [PubMed]
- Kuderer, N.M.; Burton, K.A.; Blau, S.; Senecal, F.; Gadi, V.K.; Parker, S.; Mahen, E.; Veenstra, D.; Carlson, J.J.; Lyman, G.H.; et al. Participant attitudes toward an intensive trial of multiple biopsies, multidimensional molecular analysis, and reporting of results in metastatic triple-negative breast cancer. JCO Precis. Oncol. 2017, 1, 1–13. [Google Scholar] [CrossRef]
- Che, J.Y.; Chen, L.; Guo, Z.H.; Wang, S.; Aorigele. Drug target group prediction with multiple drug networks. Comb. Chem. High Throughput Screen. 2020, 23, 274–284. [Google Scholar] [CrossRef]
- Zagidullin, B.; Wang, Z.; Guan, Y.; Pitkänen, E.; Tang, J. Comparative analysis of molecular fingerprints in prediction of drug combination effects. Brief. Bioinform. 2021, 22, bbab291. [Google Scholar] [CrossRef]
- Reardon, B.; Van Allen, E.M. Molecular Profile to Cancer Cell Line Matchmaking. 2021. Available online: https://protocolexchange.researchsquare.com/article/pex-1539/v1 (accessed on 2 December 2022).
- Udrescu, L.; Bogdan, P.; Chis¸, A.; Sirbu, I.O.; Topirceanu, A.; Varu¸t, R.M.; Udrescu, M. Uncovering new drug properties in target-based drug-drug similarity networks. Pharmaceutics 2020, 12, 879. [Google Scholar] [CrossRef]
- McNeil, C. NCI-MATCH launch highlights new trial design in precision-medicine era. J. Nat. Cancer Inst. 2015, 107, djv193. [Google Scholar] [CrossRef]
- Goyal, H.; Mann, R.; Gandhi, Z.; Perisetti, A.; Ali, A.; Ali, K.A.; Sharma, N.; Saligram, S.; Tharian, B.; Inamdar, S. Scope of artificial intelligence in screening and diagnosis of colorectal cancer. J. Clin. Med. Res. 2020, 9, 3313. [Google Scholar] [CrossRef]
- Minato, J.; Tokunaga, H.; Okamoto, S.; Shibuya, Y.; Niikura, H.; Yaegashi, N. Is imprint cytology useful to diagnose malignancy for Brenner tumors? A case series at a single institute. Acta Cytol. 2017, 61, 153–159. [Google Scholar] [CrossRef]
- Cruz, J.; López-Yáñez, I.; Argüelles-Cruz, A.J.; Marquez, C. Risk detection of malignant tumors in mammograms using unconventional computing. Res. Comp. Sci. 2014, 78, 55–66. [Google Scholar] [CrossRef]
- Zhu, J.; Strickler, J.H. Clinical applications of liquid biopsies in gastrointestinal oncology. J. Gastrointest. Oncol. 2016, 7, 675–686. [Google Scholar] [CrossRef]
- Marron, J.M.; DuBois, S.G.; Bender, J.G.; Kim, A.; Crompton, B.D.; Meyer, S.C.; Janeway, K.A.; Mack, J.W. Patient/parent perspectives on genomic tumor profiling of pediatric solid tumors: The individualized cancer therapy (iCat) experience. Pediatr. Blood Cancer 2016, 63, 1974–1982. [Google Scholar] [CrossRef] [PubMed]
- Haughton, M.E.; Chan, M.D.; Watabe, K.; Bonomi, M.; Debinski, W.; Lesser, G.J.; Ruiz, J. Treatment of brain metastases of lung cancer in the era of precision medicine. Front. Biosci. 2016, 8, 219–232. [Google Scholar] [CrossRef]
- Chen, W.; Hoffmann, A.D.; Liu, H.; Liu, X. Organotropism: New insights into molecular mechanisms of breast cancer metastasis. NPJ Precis. Oncol. 2018, 2, 4. [Google Scholar] [CrossRef] [PubMed]
- Montero-Conde, C.; Graña-Castro, O.; Martín-Serrano, G.; Martínez-Montes, Á.M.; Zarzuela, E.; Muñoz, J.; Torres-Perez, R.; Pita, G.; Cordero-Barreal, A.; Leandro-García, L.J.; et al. Hsa-miR-139-5p is a prognostic thyroid cancer marker involved in HNRNPF-mediated alternative splicing. Int. J. Cancer 2019, 146, 521–530. [Google Scholar] [CrossRef]
- Blee, S.M.; Shah, R.P.; Pinheiro, A.P.; Switchenko, J.; Dixon, M.; Owonikoko, T.K.; Hill, C.E.; Szabo, S.M.; Pentz, R.D. Physician communication and patient understanding of molecular testing terminology. Oncologist 2021, 26, 934–940. [Google Scholar] [CrossRef]
- Zhou, C.; Yuan, Z.; Ma, W.; Qi, L.; Mahavongtrakul, A.; Li, Y.; Li, H.; Gong, J.; Fan, R.R.; Li, J.; et al. Clinical utility of tumor genomic profiling in patients with high plasma circulating tumor DNA burden or metabolically active tumors. J. Hematol. Oncol. 2018, 11, 129. [Google Scholar] [CrossRef]
- Sini, G.; Colombino, M.; Lissia, A.; Maxia, S.; Gulino, M.; Paliogiannis, P.; Palomba, G.; Palmieri, G.; Cossu, A.; Rubino, C. Primary dermal melanoma in a patient with a history of multiple malignancies: A case report with molecular characterization. Case Rep. Dermatol. 2013, 5, 192–197. [Google Scholar] [CrossRef]
- Nishimura, S.; Sugimoto, A.; Kushiyama, S.; Togano, S.; Kuroda, K.; Yamamoto, Y.; Yamauchi, M.; Sumi, T.; Kaneda, H.; Kawaguchi, T.; et al. Clinical benefit for clinical sequencing using cancer panel testing. PLoS ONE 2021, 16, e0247090. [Google Scholar] [CrossRef]
- Matsumura, Y.; Owada-Ozaki, Y.; Suzuki, H. Significance of testing for TP53 gene mutations in lung adenocarcinoma using targeted gene sequencing. J. Thorac. Dis. 2018, 10, 4147–4150. [Google Scholar] [CrossRef] [PubMed]
- Baptiste, M.; Moinuddeen, S.S.; Soliz, C.L.; Ehsan, H.; Kaneko, G. Making sense of genetic information: The promising evolution of clinical stratification and precision oncology using machine learning. Genes 2021, 12, 722. [Google Scholar] [CrossRef] [PubMed]
- Baydoun, M.; Moralès, O.; Frochot, C.; Ludovic, C.; Leroux, B.; Thecua, E.; Ziane, L.; Grabarz, A.; Kumar, A.; de Schutter, C.; et al. Photodynamic therapy using a new folate receptor-targeted photosensitizer on peritoneal ovarian cancer cells induces the release of extracellular vesicles with immunoactivating properties. J. Clin. Med. 2020, 9, 1185. [Google Scholar] [CrossRef]
- Prados, M.D.; Byron, S.A.; Tran, N.L.; Phillips, J.J.; Molinaro, A.M.; Ligon, K.L.; Wen, P.Y.; Kuhn, J.G.; Mellinghoff, I.K.; de Groot, J.F.; et al. Toward precision medicine in glioblastoma: The promise and the challenges. Neuro. Oncol. 2015, 17, 1051–1063. [Google Scholar] [CrossRef] [PubMed]
- Geifman, N.; Haviv, I.; Kurzrock, R.; Rubin, E. Promoting precision cancer medicine through a community-driven knowledge-base. J. Pers. Med. 2014, 4, 475–488. [Google Scholar] [CrossRef]
- Auffray, C.; Caulfield, T.; Griffin, J.L.; Khoury, M.J.; Lupski, J.R.; Schwab, M. From genomic medicine to precision medicine: Highlights of 2015. Genome Med. 2016, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- Eden, C.; Johnson, K.W.; Gottesman, O.; Bottinger, E.P.; Abul-Husn, N.S. Medical student preparedness for an era of personalized medicine: Findings from one US medical school. Pers. Med. 2016, 13, 129–141. [Google Scholar] [CrossRef]
- Ye, P.; Chi, X.; Cha, J.H.; Luo, S.; Yang, G.; Yan, X.; Yang, W.H. Potential of e3 ubiquitin ligases in cancer immunity: Opportunities and challenges. Cells 2021, 10, 3309. [Google Scholar] [CrossRef]
- Kiyotani, K.; Toyoshima, Y.; Nakamura, Y. Personalized immunotherapy in cancer precision medicine. Cancer Biol. Med. 2021, 18, 955–965. [Google Scholar] [CrossRef]
- Aramini, B.; Masciale, V.; Banchelli, F.; D’Amico, R.; Dominici, M.; Husnain Haider, K. Precision medicine in lung cancer: Challenges and opportunities in diagnostic and therapeutic purposes. In Lung Cancer—Modern Multidisciplinary Management; Park, S.H., Ed.; IntechOpen: London, UK, 2021. [Google Scholar] [CrossRef]
- Costa, F.F. Basic research, applied medicine and EHRs—Are we on the right track? J. Cancer Sci. Ther. 2011, 3, i–ii. [Google Scholar] [CrossRef]
- Rubin, M.A. Health: Make precision medicine work for cancer care. Nature 2015, 520, 290–291. [Google Scholar] [CrossRef]
- Felsky, D.; Sariya, S.; Santa-Maria, I.; French, L.; Schneider, J.A.; Bennett, D.A.; Mayeux, R.; De Jager, P.L.; Tosto, G. The caribbean-hispanic alzheimer’s brain transcriptome reveals ancestry-specific disease mechanisms. Alzheimers Dement. 2020, 16, e043068. [Google Scholar] [CrossRef]
- Karadas, A.K.; Dilmac, S.; Aytac, G.; Tanriover, G. Melatonin decreases metastasis, primary tumor growth and angiogenesis in a mice model of breast cancer. Human Exp. Toxicol. 2021, 40, 1545–1557. [Google Scholar] [CrossRef] [PubMed]
- Pinker, K.; Chin, J.; Melsaether, A.N.; Morris, E.A.; Moy, L. Precision medicine and radiogenomics in breast cancer: New approaches toward diagnosis and treatment. Radiology 2018, 287, 732–747. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, A.; McHale, J.; Oettl, A. Finding Needles in Haystacks: Artificial Intelligence and Recombinant Growth; National Bureau of Economic Research: Cambridge, MA, USA, 2018. [Google Scholar] [CrossRef]
- Williams, S.; Horsfall, H.L.; Funnell, J.P.; Hanrahan, J.G.; Khan, D.Z.; Muirhead, W.; Stoyanov, D.; Marcus, H.J. Artificial intelligence in brain tumour surgery-an emerging paradigm. Cancers 2021, 13, 5010. [Google Scholar] [CrossRef]
- Zhao, J.; Cheng, F.; Wang, Y.; Arteaga, C.L.; Zhao, Z. Systematic prioritization of druggable mutations in 5000 genomes across 16 cancer types using a structural genomics-based approach. Mol. Cell. Proteom. 2015, 15, 642–656. [Google Scholar] [CrossRef] [PubMed]
- Bai, R.; Lv, Z.; Chen, X.; Guo, H.; Bai, L.; Tian, H.; Li, W.; Cui, J. Precision detection technology: Equipping precision oncology with wings. J. Oncol. 2020, 2020, 9068121. [Google Scholar] [CrossRef] [PubMed]
- Lourenco, R.D.A.; McCarthy, M.C.; McMillan, L.J.; Sullivan, M.; Gillam, L. Understanding decisions to participate in genomic medicine in childrencancer care: A comparison of what influences parents, health care providers, and the general community. Pediatr. Blood Cancer 2021, 68, e29101. [Google Scholar] [CrossRef]
- Malone, E.R.; Oliva, M.; Sabatini, P.J.B.; Stockley, T.L.; Siu, L.L. Molecular profiling for precision cancer therapies. Genome Med. 2020, 12, 8. [Google Scholar] [CrossRef]
- Klein, H.; Mazor, T.; Siegel, E.; Trukhanov, P.; Ovalle, A.; Fitz, C.D.V.; Zwiesler, Z.; Kumari, P.; Van Der Veen, B.; Marriott, E.; et al. MatchMiner: An open-source platform for cancer precision medicine. NPJ Precis. Med. 2022, 6, 69. [Google Scholar] [CrossRef]
- Lopez-Chavez, A.; Thomas, A.; Rajan, A.; Raffeld, M.; Morrow, B.; Kelly, R.; Carter, C.A.; Guha, U.; Killian, K.; Lau, C.C.; et al. Molecular profiling and targeted therapy for advanced thoracic malignancies: A biomarker-derived, multiarm, multihistology phase ii basket trial. J. Clin. Oncol. 2015, 33, 1000–1007. [Google Scholar] [CrossRef] [PubMed]
- Redig, A.J.; Jänne, P.A. Basket trials and the evolution of clinical trial design in an era of genomic medicine. J. Clin. Oncol. 2015, 33, 975–977. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, R.; Roll, J.D.; Rivenbark, A.G.; Coleman, W.B. Dysregulation of the epigenome in human breast cancer. Am. J. Pathol. 2015, 185, 282–292. [Google Scholar] [CrossRef] [PubMed]
- Sottoriva, A.; Spiteri, I.; Piccirillo, S.G.M.; Touloumis, A.; Collins, V.P.; Marioni, J.C.; Curtis, C.; Watts, C.; Tavaré, S. Intratumor heterogeneity in human glioblastoma reflects cancer evolutionary dynamics. Proc. Natl. Acad. Sci. USA 2013, 110, 4009–4014. [Google Scholar] [CrossRef] [PubMed]
- Snyder, J.; Poisson, L.M.; Noushmehr, H.; Castro, A.V.; deCarvalho, A.C.; Robin, A.; Mukherjee, A.; Lee, I.; Walbert, T. Clinical and research applications of a brain tumor tissue bank in the age of precision medicine. Per. Med. 2019, 16, 145–156. [Google Scholar] [CrossRef]
- Lambrechts, D.; Lenz, H.J.; de Haas, S.; Carmeliet, P.; Scherer, S.J. Markers of response for the antiangiogenic agent bevacizumab. J. Clin. Oncol. 2013, 31, 1219–1230. [Google Scholar] [CrossRef]
- Humbert, O.; Riedinger, J.M.; Vrigneaud, J.M.; Kanoun, S.; Dygai-Cochet, I.; Berriolo-Riedinger, A.; Toubeau, M.; Depardon, E.; Lassere, M.; Tisserand, S.; et al. 18F-fdg pet tumor blood flow changes after 1 cycle of neoadjuvant chemotherapy predicts outcome in triple-negative breast cancer. J. Nuc. Med. 2016, 57, 1707–1712. [Google Scholar] [CrossRef][Green Version]
- Hunter, D.J. Uncertainty in the era of precision medicine. N. Engl. J. Med. 2016, 375, 711–713. [Google Scholar] [CrossRef]
- Zhang, X.; Yang, H.; Zhang, R. Challenges and future of precision medicine strategies for breast cancer based on a database on drug reactions. Biosci. Rep. 2019, 39, BSR20190230. [Google Scholar] [CrossRef]
- Xu, J.; Liao, X.; Wong, C. Downregulations of B-cell lymphoma 2 and myeloid cell leukemia sequence 1 by microRNA 153 induce apoptosis in a glioblastoma cell line DBTRG-05MG. Int. J. Cancer 2010, 126, 1029–1035. [Google Scholar] [CrossRef]
- Schwarzenbach, H.; Nishida, N.; Calin, G.A.; Pantel, K. Clinical relevance of circulating cell-free microRNAs in cancer. Nat. Rev. Clin. Oncol. 2014, 11, 145–156. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Liu, Z.; Lin, Q.; Luo, Q.; Cen, Y.; Li, J.; Fang, X.; Gong, C. MiRNAs and cancer: Key link in diagnosis and therapy. Genes 2021, 12, 1289. [Google Scholar] [CrossRef] [PubMed]
- Aalami, A.H.; Abdeahad, H.; Shoghi, A.; Mesgari, M.; Amirabadi, A.; Sahebkar, A. Brain tumors and circulating micrornas: A systematic review and diagnostic meta-analysis. Expert Rev. Mol. Diagn. 2021, 22, 201–211. [Google Scholar] [CrossRef]
- He, J.; Jiang, Y.; Liu, L.; Zuo, Z.; Zeng, C. Circulating micrornas as promising diagnostic biomarkers for patients with glioma: A meta-analysis. Front. Neurol. 2020, 11, 610163. [Google Scholar] [CrossRef]
- Curtaz, C.J.; Reifschläger, L.; Strähle, L.; Feldheim, J.; Feldheim, J.J.; Schmitt, C.; Kiesel, M.; Herbert, S.L.; Wöckel, A.; Meybohm, P.; et al. Analysis of micrornas in exosomes of breast cancer patients in search of molecular prognostic factors in brain metastases. Int. J. Mol. Sci. 2022, 23, 3683. [Google Scholar] [CrossRef]
- Eibl, R.H.; Schneemann, M. Liquid biopsy and primary brain tumors. Cancers 2021, 13, 5429. [Google Scholar] [CrossRef]
- Wang, Q.; Li, P.; Li, A.; Jiang, W.; Wang, H.; Wang, J.; Xie, K. Plasma specific miRNAs as predictive biomarkers for diagnosis and prognosis of glioma. J. Exp. Clin. Cancer Res 2012, 31, 97. [Google Scholar] [CrossRef] [PubMed]
- Siegal, T.; Charbit, H.; Paldor, I.; Zelikovitch, B.; Canello, T.; Benis, A.; Wong, M.L.; Morokoff, A.P.; Kaye, A.H.; Lavon, I. Dynamics of circulating hypoxia-mediated miRNAs and tumor response in patients with high-grade glioma treated with bevacizumab. J. Neurosur. 2016, 125, 1008–1015. [Google Scholar] [CrossRef] [PubMed]
- Ali, H.; Harting, R.; de Vries, R.; Ali, M.; Wurdinger, T.; Best, M.G. Blood-based biomarkers for glioma in the context of gliomagenesis: A systematic review. Front. Oncol. 2021, 11, 665235. [Google Scholar] [CrossRef]
- Ohno, M.; Matsuzaki, J.; Kawauchi, J.; Aoki, Y.; Miura, J.; Takizawa, S.; Kato, K.; Sakamoto, H.; Matsushita, Y.; Takahashi, M.; et al. Assessment of the diagnostic utility of serum microrna classification in patients with diffuse glioma. JAMA Netw. Open 2019, 2, e1916953. [Google Scholar] [CrossRef]
- Gareev, I.F.; Beylerli, O.; Liang, Y.; Xiang, H.; Liu, C.; Xu, X.; Yuan, C.; Ahmad, A.; Yang, G. The role of micrornas in therapeutic resistance of malignant primary brain tumors. Front. Cell Dev. Biol. 2021, 9, 740303. [Google Scholar] [CrossRef]
- Li, N.; Shi, H.; Zhang, L.; Li, X.; Gao, L.; Zhang, G.; Shi, Y.; Guo, S. MiR-188 Inhibits glioma cell proliferation and cell cycle progression through targeting β-catenin. Oncol. Res. Featur. Preclin. Clin. Cancer Ther. 2018, 26, 785–794. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.; Wu, R.; Zhao, M.; Garcia-Gomez, A.; Ballestar, E. miRNAs as therapeutic targets in inflammatory disease. Trends Pharmacol. Sci. 2019, 40, 853–865. [Google Scholar] [CrossRef] [PubMed]
- El-Sayed, S.R.; Cristante, J.; Guyon, L.; Denis, J.; Chabre, O.; Cherradi, N. MicroRNA therapeutics in cancer: Current advances and challenges. Cancers 2021, 13, 2680. [Google Scholar] [CrossRef] [PubMed]
- Papagiannakopoulos, T.; Friedmann-Morvinski, D.; Neveu, P.; Dugas, J.C.; Gill, R.M.; Huillard, E.; Liu, C.; Zong, H.; Rowitch, D.H.; Barres, B.A.; et al. Pro-neural miR-128 is a glioma tumor suppressor that targets mitogenic kinases. Oncogene 2012, 31, 1884–1895. [Google Scholar] [CrossRef]
- Mathew, L.K.; Skuli, N.; Mucaj, V.; Lee, S.S.; Zinn, P.O.; Sathyan, P.; Imtiyaz, H.Z.; Zhang, Z.; Davuluri, R.V.; Rao, S.; et al. miR-218 opposes a critical RTK-HIF pathway in mesenchymal glioblastoma. Proc. Natl. Acad. Sci. USA 2014, 111, 291–296. [Google Scholar] [CrossRef]
- Tomei, S.; Volontè, A.; Ravindran, S.; Mazzoleni, S.; Wang, E.; Galli, R.; Maccalli, C. MicroRNA expression profile distinguishes glioblastoma stem cells from differentiated tumor cells. J. Pers. Med. 2021, 11, 264. [Google Scholar] [CrossRef]
- Chen, M.; Medarova, Z.; Moore, A. Role of microRNAs in glioblastoma. Oncotarget 2021, 12, 1707–1723. [Google Scholar] [CrossRef]
- Aloizou, A.M.; Pateraki, G.; Siokas, V.; Mentis, A.F.A.; Liampas, I.; Lazopoulos, G.; Kovatsi, L.; Mitsias, P.D.; Bogdanos, D.P.; Paterakis, K.; et al. The role of MiRNA-21 in gliomas: Hope for a novel therapeutic intervention? Toxicol. Rep. 2020, 7, 1514–1530. [Google Scholar] [CrossRef]
- Min, R.Q.; Ma, Q. MicroRNA-381 inhibits metastasis and epithelial-mesenchymal transition of glioblastoma cells through targeting LEF1. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 6825–6833. [Google Scholar] [CrossRef]
- Kaswa, R.; Nair, A.; Murphy, S.; Von Pressentin, K.B. Artificial intelligence: A strategic opportunity for enhancing primary care in south africa. S. Afr. Fam. Pract. 2022, 64, a5596. [Google Scholar] [CrossRef] [PubMed]
- Matheny, M.E.; Whicher, D.; Israni, S.T. Artificial intelligence in health care: A report from the national academy of medicine. JAMA 2019, 323, 509–510. [Google Scholar] [CrossRef]
- Buch, V.H.; Ahmed, I.; Maruthappu, M. Artificial intelligence in medicine: Current trends and future possibilities. Br. J. Gen. Pract. 2018, 68, 143–144. [Google Scholar] [CrossRef] [PubMed]
- Research and Markets, Insights on the Brain Cancer Diagnostics Global Market to 2028—Increase in Prevalence of Brain Cancer Worldwide Is Driving Growth. Available online: https://www.globenewswire.com/en/news-release/2021/11/09/2329989/28124/en/Insights-on-the-Brain-Cancer-Diagnostics-Global-Market-to-2028-Increase-in-Prevalence-of-Brain-Cancer-Worldwide-is-Driving-Growth.html (accessed on 3 December 2022).
- Battineni, G.; Sagaro, G.G.; Chinatalapudi, N.; Amenta, F. Applications of machine learning predictive models in the chronic disease diagnosis. J. Pers. Med. 2020, 10, 21. [Google Scholar] [CrossRef] [PubMed]
- Iuga, A.I.; Carolus, H.; Höink, A.J.; Brosch, T.; Klinder, T.; Maintz, D.; Persigehl, T.; Bae, B.; Püsken, M. Automated detection and segmentation of thoracic lymph nodes from CT using 3D foveal fully convolutional neural networks. BMC Med. Imaging 2021, 21, 69. [Google Scholar] [CrossRef] [PubMed]
- Asif, S.; Yi, W.; ul Ain, Q.; Hou, J.; Yi, T.; Si, J. Improving effectiveness of different deep transfer learning-based models for detecting brain tumors from mr images. IEEE Access 2022, 10, 34716–34730. [Google Scholar] [CrossRef]
- Sandu, N.; Schaller, B. Stem cell transplantation in brain tumors: A new field for molecular imaging? Mol. Med. 2010, 16, 433–437. [Google Scholar] [CrossRef][Green Version]
- Zarzeczny, A.; Babyn, P.; Adams, S.J.; Longo, J. Artificial intelligence-based imaging analytics and lung cancer diagnostics: Considerations for health system leaders. Healthc. Manag. Forum 2020, 34, 169–174. [Google Scholar] [CrossRef]
- Liu, T.; Yuan, Z.; Wu, L.; Badami, B. Optimal brain tumor diagnosis based on deep learning and balanced sparrow search algorithm. Int. J. Imaging Syst. Technol. 2021, 31, 1921–1935. [Google Scholar] [CrossRef]
- Zhou, M.; Scott, J.; Chaudhury, B.; Hall, L.; Goldgof, D.; Yeom, K.W.; Iv, M.; Ou, Y.; Kalpathy-Cramer, J.; Napel, S.; et al. Radiomics in brain tumor: Image assessment, quantitative feature descriptors, and machine-learning approaches. Am. J. Neuroradiol. 2018, 39, 208–216. [Google Scholar] [CrossRef]
- Arif, M.; Ajesh, F.; Shamsudheen, S.; Geman, O.; Izdrui, D.; Vicoveanu, D. Brain tumor detection and classification by mri using biologically inspired orthogonal wavelet transform and deep learning techniques. J. Healthc. Eng. 2022, 2022, e2693621. [Google Scholar] [CrossRef] [PubMed]
- Kader, I.A.E.; Xu, G.; Shuai, Z.; Saminu, S.; Javaid, I.; Ahmad, I.S.; Kamhi, S. Brain tumor detection and classification on mr images by a deep wavelet auto-encoder model. Diagnostics 2021, 11, 1589. [Google Scholar] [CrossRef] [PubMed]
- Gui, L.; Li, C.; Yang, X. Medical image segmentation based on level set and isoperimetric constraint. Phys. Medica 2017, 42, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Işın, A.; Direkoglu, C.; Şah, M. Review of MRI-based brain tumor image segmentation using deep learning methods. Procedia Comput. Sci. 2016, 102, 317–324. [Google Scholar] [CrossRef]
- Lee, J.; Shin, D.; Oh, S.H.; Kim, H. Method to minimize the errors of ai: Quantifying and exploiting uncertainty of deep learning in brain tumor segmentation. Sensors 2022, 22, 2406. [Google Scholar] [CrossRef]
- Kato, Y.; Nishihara, H.; Yuzawa, S.; Mohri, H.; Kanno, H.; Hatanaka, Y.; Kimura, T.; Tanino, M.; Tanaka, S. Immunohistochemical molecular expression profile of metastatic brain tumor for potent personalized medicine. Brain Tumor Pathol. 2012, 30, 167–174. [Google Scholar] [CrossRef][Green Version]
- Krafft, C.; Rösch, P.; Popp, J. Raman Spectroscopy in Medicine. In digital Encyclopedia of Applied Physics; Wiley-VCH Verlag GmbH & Co. KGaA, Ed.; Wiley-VCH Verlag GmbH & Co. KGaA: Weinheim, Germany, 2009; p. 985. [Google Scholar] [CrossRef]
- Groothuis, D.R.; Lapin, G.D.; Vriesendorp, F.J.; Mikhael, M.A.; Patlak, C.S. A method to quantitatively measure transcapillary transport of iodinated compounds in canine brain tumors with computed tomography. J. Cereb. Blood Flow Metab. 1991, 11, 939–948. [Google Scholar] [CrossRef]
- Rhodes, C.S.; Zhang, H.; Patel, K.; Mistry, N.; Kwok, Y.; D’Souza, W.D.; Regine, W.F.; Gullapalli, R.P. The feasibility of integrating resting-state fmri networks into radiotherapy treatment planning. J. Med. Imaging Rad. Sci. 2019, 50, 119–128. [Google Scholar] [CrossRef]
- Apostolova, I.; Wedel, F.; Brenner, W. Imaging of tumor metabolism using positron emission tomography (pet). recent results in cancer research. Recent Results Cancer Res. 2016, 207, 177–205. [Google Scholar] [CrossRef]
- Herholz, K.; Langen, K.J.; Schiepers, C.; Mountz, J.M. Brain Tumors. Semin. Nucl. Med. 2012, 42, 356–370. [Google Scholar] [CrossRef]
- Blanc-Durand, P.; Gucht, A.V.D.; Schaefer, N.; Itti, E.; Prior, J.O. Automatic lesion detection and segmentation of 18F-FET PET in gliomas: A full 3D U-Net convolutional neural network study. PLoS ONE 2018, 13, e0195798. [Google Scholar] [CrossRef] [PubMed]
- Joe, N.S.; Hodgdon, C.; Kraemer, L.; Redmond, K.J.; Stearns, V.; Gilkes, D.M. A common goal to CARE: Cancer advocates, researchers, and clinicians explore current treatments and clinical trials for breast cancer brain metastases. NPJ Breast Cancer 2021, 7, 121. [Google Scholar] [CrossRef] [PubMed]
- Bhanumurthy, M.Y.; Anne, K. An automated detection and segmentation of tumor in brain MRI using artificial intelligence. In Proceedings of the 2014 IEEE International Conference on Computational Intelligence and Computing Research, Coimbatore, India, 18–20 December 2014; pp. 1–6. [Google Scholar] [CrossRef]
- Amero, P.; Khatua, S.; Rodriguez-Aguayo, C.; Lopez-Berestein, G. Aptamers: Novel therapeutics and potential role in neuro-oncology. Cancers 2020, 12, 2889. [Google Scholar] [CrossRef] [PubMed]
- Goujon, D.; Zellweger, M.; Radu, A.; Grosjean, P.; Weber, B.C.; van den Bergh, H.; Monnier, P.; Wagnier`es, G. In vivo autofluorescence imaging of early cancers in the human tracheobronchial tree with a spectrally optimized system. J. Biomed. Opt. 2003, 8, 17. [Google Scholar] [CrossRef]
- Majd, S.; Power, J.; Majd, Z. Alzheimer’s disease and cancer: When two monsters cannot be together. Front. Neurosci. 2019, 13, 155. [Google Scholar] [CrossRef] [PubMed]
- Hudáá, M.; Hamuá, S.; Konkoá, E.; Jendý, R.; Vargová, J.; Ševc, J.; Fedoro, P.; Soukup, O.; Janoá, J.; Ihnatova, V.; et al. Synthesis of new biscoumarin derivatives, in vitro cholinesterase inhibition, molecular modelling and antiproliferative effect in a549 human lung carcinoma cells. Int. J. Mol. Sci. 2021, 22, 3830. [Google Scholar] [CrossRef]
- Attia, N.M.; Sayed, S.A.A.; Riad, K.F.; Korany, G.M. Magnetic resonance spectroscopy in pediatric brain tumors: How to make a more confident diagnosis. Egypt. J. Rad. Nuc. Med. 2020, 51, 14. [Google Scholar] [CrossRef]
- Akatsuka, J.; Numata, Y.; Morikawa, H.; Sekine, T.; Kayama, S.; Mikami, H.; Yanagi, M.; Endo, Y.; Takeda, H.; Toyama, Y.; et al. A data-driven ultrasound approach discriminates pathological high grade prostate cancer. Sci. Rep. 2022, 12, 860. [Google Scholar] [CrossRef]
- Bulten, W.; Pinckaers, H.; van Boven, H.; Vink, R.; de Bel, T.; van Ginneken, B.; van der Laak, J.; Hulsbergen-van de Kaa, C.; Litjens, G. Automated deep-learning system for gleason grading of prostate cancer using biopsies: A diagnostic study. Lancet Oncol. 2020, 21, 233–241. [Google Scholar] [CrossRef]
- Khazaee, Z.; Langarizadeh, M.; Shiri Ahmadabadi, M.E. Developing an artificial intelligence model for tumor grading and classification, based on mri sequences of human brain gliomas. Int. J. Cancer Manag. 2022, 15, e120638. [Google Scholar] [CrossRef]
- Tandel, G.S.; Biswas, M.; Kakde, O.G.; Tiwari, A.; Suri, H.S.; Turk, M.; Laird, J.; Asare, C.; Ankrah, A.A.; Khanna, N.N.; et al. A review on a deep learning perspective in brain cancer classification. Cancers 2019, 11, 111. [Google Scholar] [CrossRef] [PubMed]
- Abdel Razek, A.A.K.; Alksas, A.; Shehata, M.; AbdelKhalek, A.; Abdel Baky, K.; El-Baz, A.; Helmy, E. Clinical applications of artificial intelligence and radiomics in neuro-oncology imaging. Insights Imaging 2021, 12, 152. [Google Scholar] [CrossRef] [PubMed]
- Cho, H.-H.; Park, H. Classification of low-grade and high-grade glioma using multi-modal image radiomics features. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2017, 2017, 3081–3084. [Google Scholar] [CrossRef]
- Bi, W.L.; Hosny, A.; Schabath, M.B.; Giger, M.L.; Birkbak, N.J.; Mehrtash, A.; Allison, T.; Arnaout, O.; Abbosh, C.; Dunn, I.F.; et al. Artificial Intelligence in Cancer Imaging: Clinical Challenges and Applications. CA Cancer J. Clin. 2019, 69, 127–157. [Google Scholar] [CrossRef]
- Spraker, M.B.; Wootton, L.S.; Hippe, D.S.; Ball, K.C.; Peeken, J.C.; Macomber, M.W.; Chapman, T.R.; Hoff, M.N.; Kim, E.Y.; Pollack, S.M.; et al. MRI radiomic features are independently associated with overall survival in soft tissue sarcoma. Adv. Radiat. Oncol. 2019, 4, 413–421. [Google Scholar] [CrossRef]
- Lambin, P.; Leijenaar, R.T.H.; Deist, T.M.; Peerlings, J.; de Jong, E.E.C.; van Timmeren, J.; Sanduleanu, S.; Larue, R.T.H.M.; Even, A.J.G.; Jochems, A.; et al. Radiomics: The bridge between medical imaging and personalized medicine. Nat. Rev. Clin. Oncol. 2017, 14, 749–762. [Google Scholar] [CrossRef]
- Gaddamanugu, S.; Shafaat, O.; Sotoudeh, H.; Sarrami, A.H.; Rezaei, A.; Saadatpour, Z.; Singhal, A. Clinical applications of diffusion-weighted sequence in brain imaging: Beyond stroke. Neuroradiology 2022, 64, 15–30. [Google Scholar] [CrossRef]
- Chaddad, A.; Zhang, M.; Desrosiers, C.; Niazi, T. Deep radiomic features from mri scans predict survival outcome of recurrent glioblastoma. In Proceedings of the Radiomics and Radiogenomics in Neurooncology; Mohy-ud-Din, H., Rathore, S., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 36–43. [Google Scholar] [CrossRef]
- Kickingereder, P.; Burth, S.; Wick, A.; Götz, M.; Eidel, O.; Schlemmer, H.P.; Maier-Hein, K.H.; Wick, W.; Bendszus, M.; Radbruch, A.; et al. Radiomic profiling of glioblastoma: Identifying an imaging predictor of patient survival with improved performance over established clinical and radiologic risk models. Radiology 2016, 280, 880–889. [Google Scholar] [CrossRef]
- Liu, Z.; Wang, S.; Dong, D.; Wei, J.; Fang, C.; Zhou, X.; Sun, K.; Li, L.; Li, B.; Wang, M.; et al. The applications of radiomics in precision diagnosis and treatment of oncology: Opportunities and challenges. Theranostics 2019, 9, 1303–1322. [Google Scholar] [CrossRef]
- Singh, G.; Manjila, S.; Sakla, N.; True, A.; Wardeh, A.H.; Beig, N.; Vaysberg, A.; Matthews, J.; Prasanna, P.; Spektor, V. Radiomics and radiogenomics in gliomas: A contemporary update. Br. J. Cancer 2021, 125, 641–657. [Google Scholar] [CrossRef]
- Sotoudeh, H.; Shafaat, O.; Bernstock, J.D.; Brooks, M.D.; Elsayed, G.A.; Chen, J.A.; Szerip, P.; Chagoya, G.; Gessler, F.; Sotoudeh, E.; et al. Artificial intelligence in the management of glioma: Era of personalized medicine. Front. Oncol. 2019, 9, 768. [Google Scholar] [CrossRef] [PubMed]
- Aytac, U.C.; Gunes, A.; Ajlouni, N. A novel adaptive momentum method for medical image classification using convolutional neural network. BMC Med. Imaging 2022, 22, 34. [Google Scholar] [CrossRef] [PubMed]
- Gao, J.; Jiang, Q.; Zhou, B.; Chen, D. Convolutional neural networks for computer-aided detection or diagnosis in medical image analysis: An overview. Math. Biosci. Eng. 2019, 16, 6536–6561. [Google Scholar] [CrossRef] [PubMed]
- Ker, J.; Bai, Y.; Lee, H.Y.; Rao, J.; Wang, L. Automated brain histology classification using machine learning. J. Clin. Neurosci. 2019, 66, 239–245. [Google Scholar] [CrossRef]
- Yonekura, A.; Kawanaka, H.; Prasath, V.B.S.; Aronow, B.J.; Takase, H. Automatic disease stage classification of glioblastoma multiforme histopathological images using deep convolutional neural network. Biomed. Eng. Lett. 2018, 8, 321–327. [Google Scholar] [CrossRef]
- Jermyn, M.; Mok, K.; Mercier, J.; Desroches, J.; Pichette, J.; Saint-Arnaud, K.; Bernstein, L.; Guiot, M.C.; Petrecca, K.; Leblond, F. Intraoperative brain cancer detection with raman spectroscopy in humans. Sci. Transl. Med. 2015, 7, 274ra219. [Google Scholar] [CrossRef]
- Shabestri, B.; Anastasio, M.A.; Fei, B.; Leblond, F. Special series guest editorial: Artificial intelligence and machine learning in biomedical optics. J. Biomed. Opt. 2021, 26, 052901. [Google Scholar] [CrossRef]
- Iakab, S.A.; Ràfols, P.; Correig-Blanchar, X.; García-Altares, M. Perspective on multimodal imaging techniques coupling mass spectrometry and vibrational spectroscopy: Picturing the best of both worlds. Anal. Chem. 2021, 93, 6301–6310. [Google Scholar] [CrossRef]
- Mzoughi, H.; Njeh, I.; Wali, A.; Slima, M.B.; BenHamida, A.; Mhiri, C.; Mahfoudhe, K.B. Deep multi-scale 3d convolutional neural network (cnn) for mri gliomas brain tumor classification. J. Digit. Imaging 2020, 33, 903–915. [Google Scholar] [CrossRef]
- Abd-Ellah, M.K.; Awad, A.I.; Khalaf, A.A.M.; Hamed, H.F.A. A review on brain tumor diagnosis from MRI images: Practical implications, key achievements, and lessons learned. Magn. Reason. Imaging 2019, 61, 300–318. [Google Scholar] [CrossRef]
- Juluru, K.; Shih, H.H.; Keshava Murthy, K.N.; Elnajjar, P.; El-Rowmeim, A.; Roth, C.; Genereaux, B.; Fox, J.; Siegel, E.; Rubin, D.L. Integrating Al algorithms into the clinical workflow. Radiol. Artif. Intell. 2021, 3, e210013. [Google Scholar] [CrossRef] [PubMed]
- Parker, A.L.; Benguigui, M.; Fornetti, J.; Goddard, E.; Lucotti, S.; Insua-Rodriguez, J.; Wiegmans, A.P. Current challenges in metastasis research and future innovation for clinical translation. Clin. Exp. Metastasis 2022, 39, 263–277. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.J.; Liu, W.; Wang, X.; Fang, Q.; Wang, R.; Wang, Y.; Chen, H.; Chen, H.; Meng, D.; Wang, L. Rectifying supporting regions with mixed and active supervision for rib fracture recognition. IEEE Trans. Med. Imaging 2020, 39, 3843–3854. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, B.; Goldenholz, D.M. Machine learning applications in epilepsy. Epilepsia 2019, 60, 2037–2047. [Google Scholar] [CrossRef]
- Kocher, M.; Ruge, M.I.; Galldiks, N.; Lohmann, P. Applications of radiomics and machine learning for radiotherapy of malignant brain tumors. Strahlenther. Onkol. 2020, 196, 856–867. [Google Scholar] [CrossRef]
- Mlynarski, P.; Delingette, H.; Criminisi, A.; Ayache, N. Deep learning with mixed supervision for brain tumor segmentation. J. Med. Imaging 2019, 6, 1. [Google Scholar] [CrossRef]
- Ryu, J.Y.; Chung, H.Y.; Choi, K.Y. Potential role of artificial intelligence in craniofacial surgery. Arch. Craniofac. Surg. 2021, 22, 223–231. [Google Scholar] [CrossRef]
- Chen, H.; Qin, Z.; Ding, Y.; Tian, L.; Qin, Z. Brain tumor segmentation with deep convolutional symmetric neural network. Neurocomputing 2020, 392, 305–313. [Google Scholar] [CrossRef]
- Hyysalo, J.; Dasanayake, S.; Hannu, J.; Schuss, C.; Rajanen, M.; Leppänen, T.; Doermann, D.; Sauvola, J. Smart Mask—Wearable IoT Solution for Improved Protection and Personal Health. Internet Things 2022, 18, 100511. [Google Scholar] [CrossRef]
- Tedeschini, B.C.; Savazzi, S.; Stoklasa, R.; Barbieri, L.; Stathopoulos, I.; Nicoli, M.; Serio, L. Decentralized federated learning for healthcare networks: A case study on tumor segmentation. IEEE Access 2022, 10, 8693–8708. [Google Scholar] [CrossRef]
- Okal, C.O.; Loice, H.T. Usability of big data analytics within clinical decision support systems. Int. J. Eng. Appl. Sci. Technol. 2019, 4, 64–73. [Google Scholar] [CrossRef]
- Khawaldeh, S.; Pervaiz, U.; Rafiq, A.; Alkhawaldeh, R. Noninvasive grading of glioma tumor using magnetic resonance imaging with convolutional neural networks. Appl. Sci. 2018, 8, 27. [Google Scholar] [CrossRef]
| Tumor Type | miRNA | Gene-Target | Biological Function | Signalling Pathway | References | |
|---|---|---|---|---|---|---|
| Glioblastoma | miR-128-3p | platelet-derived growth factor alpha receptor | promotes glioblastoma | Down | receptor tyrosine kinase | [109] |
| Glioblastoma | miR-218 | hypoxia-inducible factor 2 alpha | promotes glioblastoma | Down | receptor tyrosine kinase | [110] |
| Glioblastoma | miR-95 | Hepatocyte Growth Factor and Mitogen-Activated Protein Kinase Kinase 3 | improved clinical outcome in the neural subtype | Down | Signal transducer and activator of transcription 3 | [111] |
| Glioblastoma | miR-21 | Integrin b8 [112] | improved clinical outcome in the neural subtype | Up | Signal Transducer and Activator of Transcription [113] | [111] |
| Glioblastoma | miR-381 | lymphoid enhancer- | Inhibits metastases | Down | Wnt | [114] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Philip, A.K.; Samuel, B.A.; Bhatia, S.; Khalifa, S.A.M.; El-Seedi, H.R. Artificial Intelligence and Precision Medicine: A New Frontier for the Treatment of Brain Tumors. Life 2023, 13, 24. https://doi.org/10.3390/life13010024
Philip AK, Samuel BA, Bhatia S, Khalifa SAM, El-Seedi HR. Artificial Intelligence and Precision Medicine: A New Frontier for the Treatment of Brain Tumors. Life. 2023; 13(1):24. https://doi.org/10.3390/life13010024
Chicago/Turabian StylePhilip, Anil K., Betty Annie Samuel, Saurabh Bhatia, Shaden A. M. Khalifa, and Hesham R. El-Seedi. 2023. "Artificial Intelligence and Precision Medicine: A New Frontier for the Treatment of Brain Tumors" Life 13, no. 1: 24. https://doi.org/10.3390/life13010024
APA StylePhilip, A. K., Samuel, B. A., Bhatia, S., Khalifa, S. A. M., & El-Seedi, H. R. (2023). Artificial Intelligence and Precision Medicine: A New Frontier for the Treatment of Brain Tumors. Life, 13(1), 24. https://doi.org/10.3390/life13010024








