Effect of Malignancy on Semen Parameters
Abstract
1. Introduction
2. Materials and Methods
Statistical Analyses
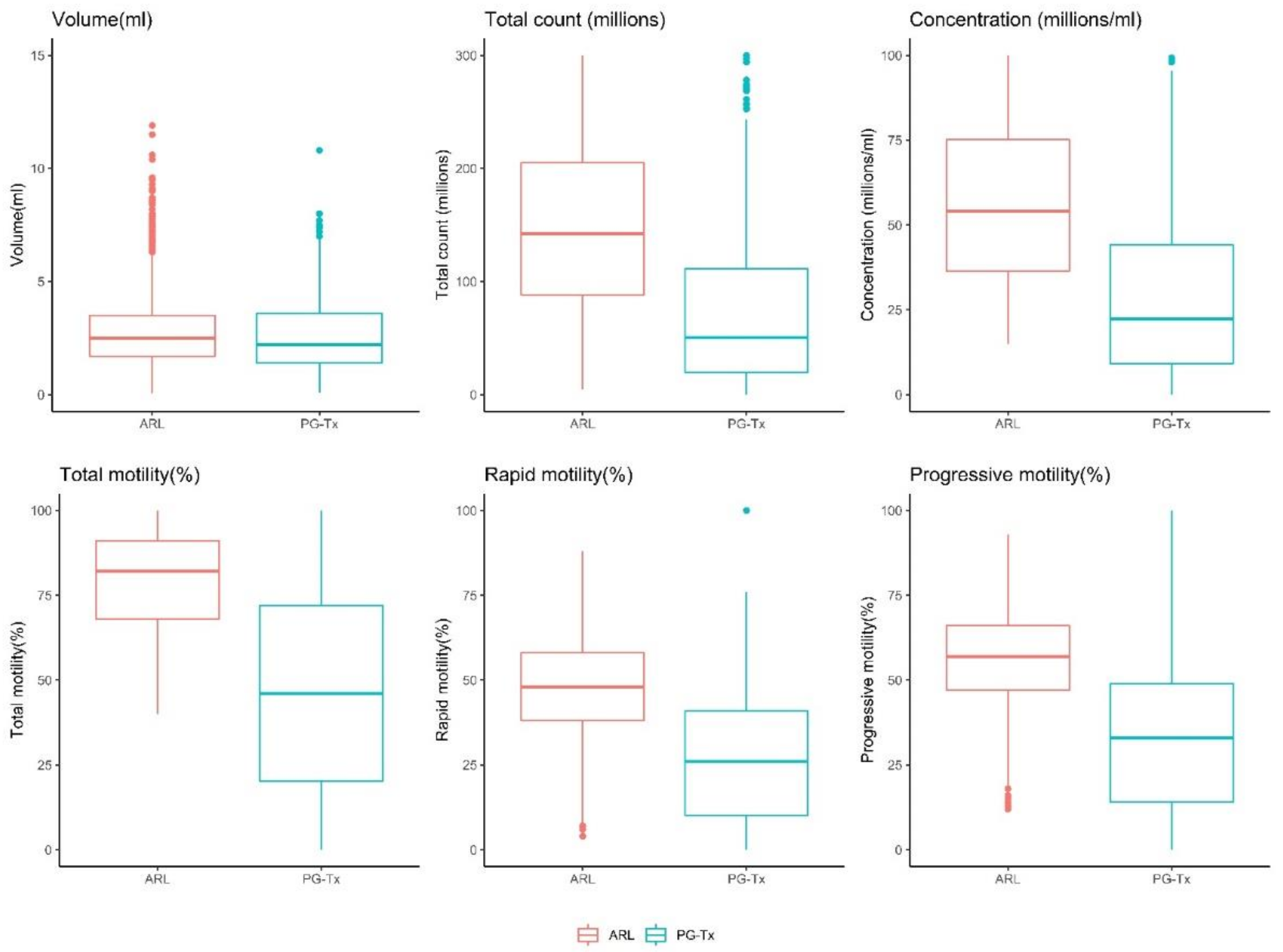
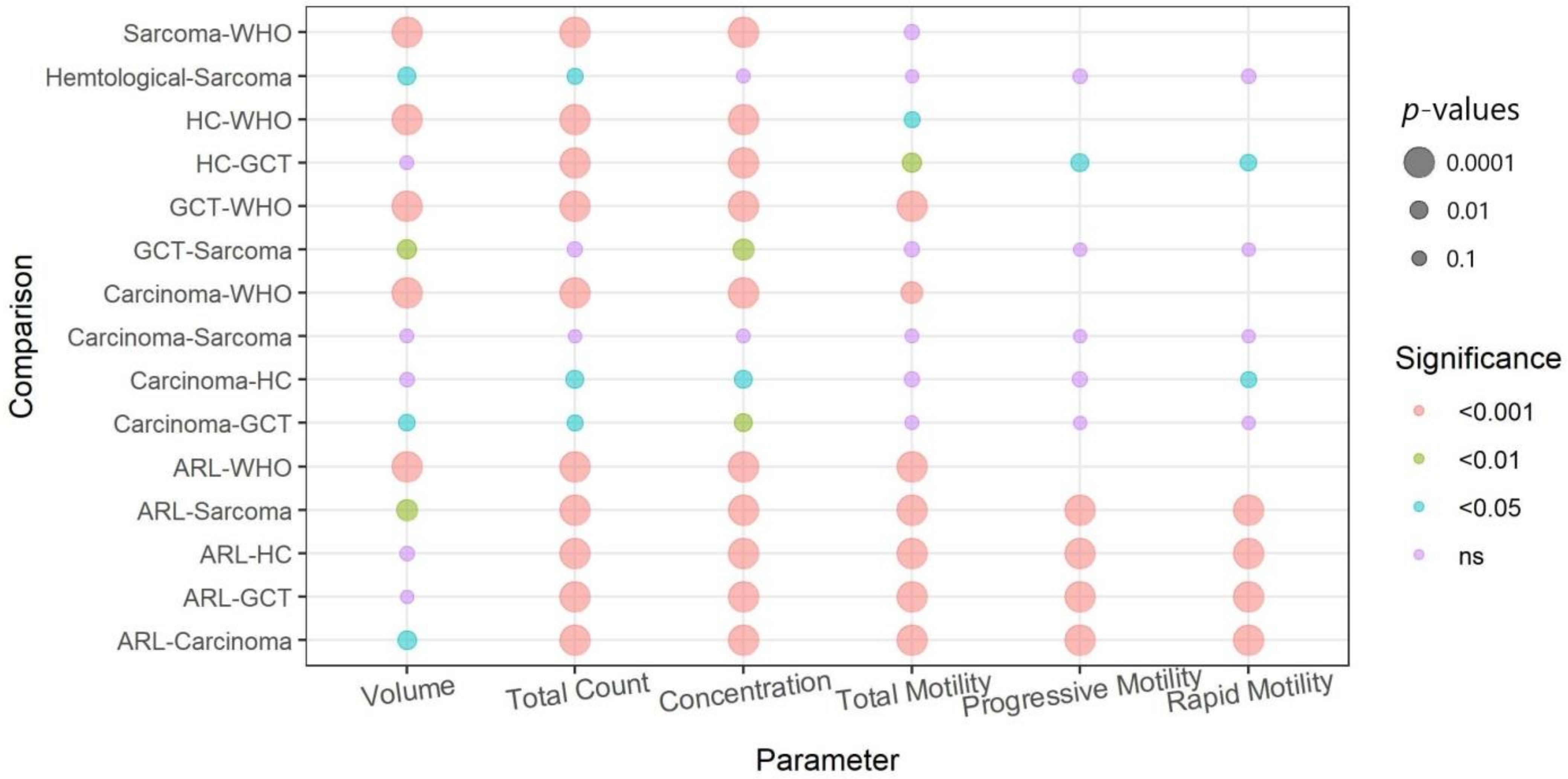
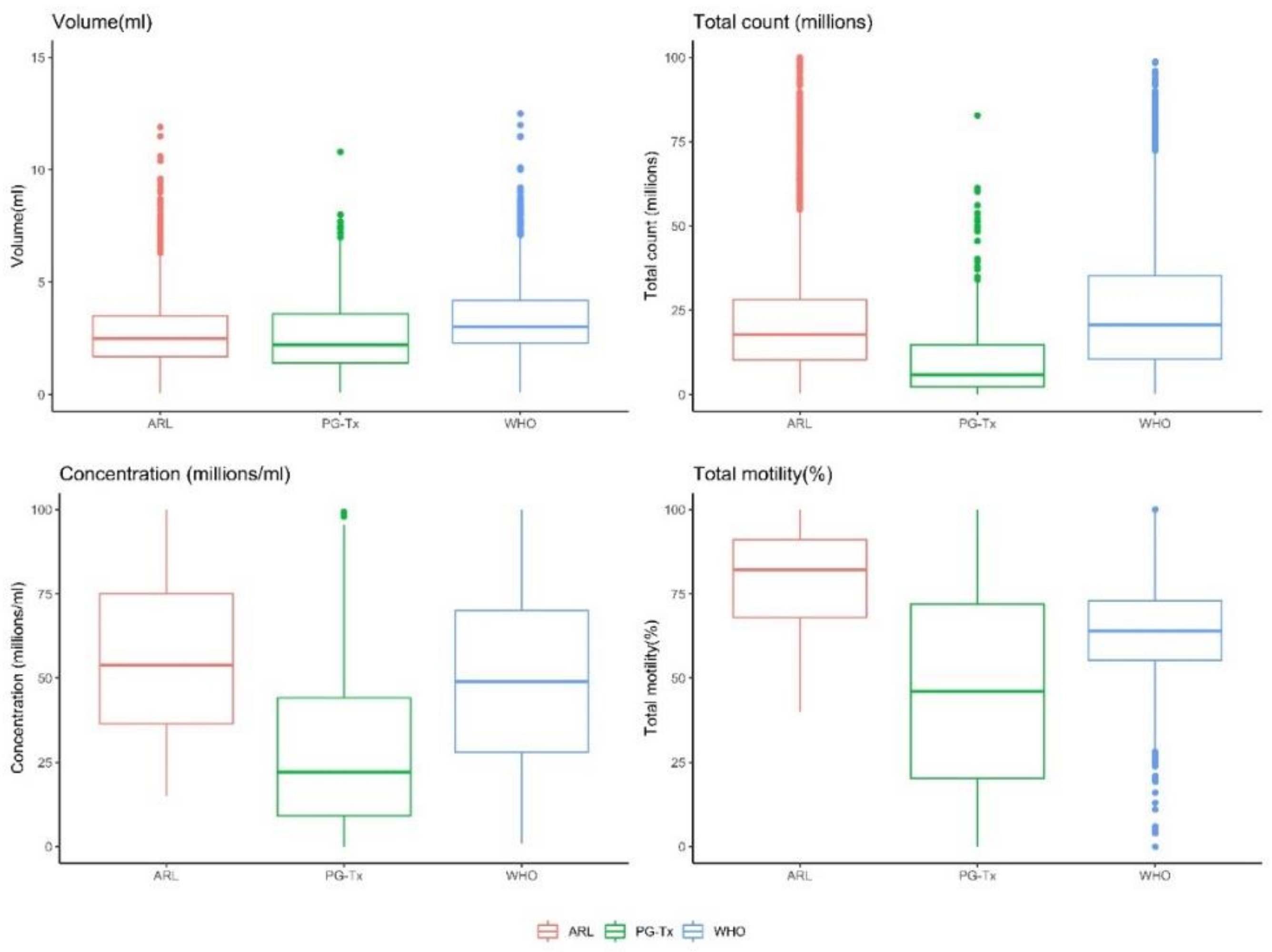
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Miller, K.D.; Fidler-Benaoudia, M.; Keegan, T.H.; Hipp, H.S.; Jemal, A.; Siegel, R.L. Cancer statistics for adolescents and young adults, 2020. CA Cancer J. Clin. 2020, 70, 443–459. [Google Scholar] [CrossRef] [PubMed]
- Oktay, K.; Harvey, B.E.; Partridge, A.H.; Quinn, G.P.; Reinecke, J.; Taylor, H.S.; Wallace, W.H.; Wang, E.T.; Loren, A.W. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J. Clin. Oncol. 2018, 36, 1994–2001. [Google Scholar] [CrossRef] [PubMed]
- Trottmann, M.; Becker, A.J.; Stadler, T.; Straub, J.; Soljanik, I.; Schlenker, B.; Stief, C.G. Semen quality in men with malignant diseases before and after therapy and the role of cryopreservation. Eur. Urol. 2007, 52, 355–367. [Google Scholar] [CrossRef] [PubMed]
- Padron, O.F.; Sharma, R.K.; Thomas, A.J.; Agarwal, A. Effects of cancer on spermatozoa quality after cryopreservation: A 12-year experience. Fertil. Steril. 1997, 67, 326–331. [Google Scholar] [CrossRef]
- Pourmasumi, S.; Sabeti, P.; Rahiminia, T.; Mangoli, E.; Tabibnejad, N.; Talebi, A.R. The etiologies of DNA abnormalities in male infertility: An assessment and review. Int. J. Reprod. Biomed. 2017, 15, 331–344. [Google Scholar] [CrossRef] [PubMed]
- MacKenna, A.; Crosby, J.; Huidobro, C.; Correa, E.; Duque, G. Semen quality before cryopreservation and after thawing in 543 patients with testicular cancer. JBRA Assist. Reprod. 2017, 21, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Hamano, I.; Hatakeyama, S.; Nakamura, R.; Fukuhara, R.; Noro, D.; Tanaka, T.; Yoneyama, T.; Yamamoto, H.; Yoneyama, T.; Hashimoto, Y.; et al. Differences in semen characteristics between patients with testicular cancer and other malignancies using various cut-off values. Int. J. Urol. 2018, 25, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Caponecchia, L.; Cimino, G.; Sacchetto, R.; Fiori, C.; Sebastianelli, A.; Salacone, P.; Marcucci, I.; Tomassini, S.; Rago, R. Do malignant diseases affect semen quality? Sperm parameters of men with cancers. Andrologia 2016, 48, 333–340. [Google Scholar] [PubMed]
- Xu, R.; Centola, G.M.; Tanrikut, C. Genitourinary cancer patients have worse baseline semen parameters than healthy sperm bankers. Andrology 2019, 7, 449–453. [Google Scholar] [CrossRef]
- Bizet, P.; Saias-Magnan, J.; Jouve, E.; Grillo, J.M.; Karsenty, G.; Metzler-Guillemain, C.; Perrin, J. Sperm cryopreservation before cancer treatment: A 15-year monocentric experience. Reprod. Biomed. Online 2012, 24, 321–330. [Google Scholar] [CrossRef]
- Carlsen, E.; Andersson, A.-M.; Petersen, J.H.; Skakkebaek, N.E. History of febrile illness and variation in semen quality. Hum. Reprod. 2003, 18, 2089–2092. [Google Scholar] [CrossRef]
- Van der Kaaij, M.A.E.; Heutte, N.; van Echten-Arends, J.; Raemaekers, J.M.M.; Carde, P.; Noordijk, E.M.; Christophe, F.; Tomas, J.; Eghbali, H.; Brice, P.; et al. Sperm quality before treatment in patients with early stage Hodgkin’s lymphoma enrolled in EORTC-GELA Lymphoma Group trials. Haematologica 2009, 94, 1691–1697. [Google Scholar] [CrossRef]
- Sieniawski, M.; Reineke, T.; Josting, A.; Nogova, L.; Behringer, K.; Halbsguth, T.; Fuchs, M.; Diehl, V.; Engert, A. Assessment of male fertility in patients with Hodgkin’s lymphoma treated in the German Hodgkin Study Group (GHSG) clinical trials. Ann. Oncol. 2008, 19, 1795–1801. [Google Scholar] [CrossRef]
- Rueffer, U.; Breuer, K.; Josting, A.; Lathan, B.; Sieber, M.; Manzke, O.; Grotenhermen, F.J.; Tesch, H.; Bredenfeld, H.; Koch, P.; et al. Male gonadal dysfunction in patients with Hodgkin’s disease prior to treatment. Ann. Oncol. 2001, 12, 1307–1311. [Google Scholar] [CrossRef]
- Xavier, R.; de Carvalho, R.C.; Fraietta, R. Semen quality from patients affected by seminomatous and non-seminomatous testicular tumor. Int. Braz. J. Urol. 2021, 47, 495–502. [Google Scholar] [CrossRef]
- Sposito, C.; Camargo, M.; Tibaldi, D.S.; Barradas, V.; Cedenho, A.P.; Nichi, M.; Bertolla, R.P.; Spaine, D.M. Antioxidant enzyme profile and lipid peroxidation products in semen samples of testicular germ cell tumor patients submitted to orchiectomy. Int. Braz. J. Urol. 2017, 43, 644–651. [Google Scholar] [CrossRef][Green Version]
- Dias, T.R.; Agarwal, A.; Pushparaj, P.N.; Ahmad, G.; Sharma, R. Reduced semen quality in patients with testicular cancer seminoma is associated with alterations in the expression of sperm proteins. Asian J. Androl. 2020, 22, 88–93. [Google Scholar]
- Cheng, C.Y.; Mruk, D.D. The blood-testis barrier and its implications for male contraception. Pharmacol. Rev. 2012, 64, 16–64. [Google Scholar] [CrossRef]
- Pallotti, F.; Pelloni, M.; Faja, F.; Di Chiano, S.; Di Rocco, A.; Lenzi, A.; Lombardo, F.; Paoli, D. Semen quality in non-Hodgkin lymphoma survivors: A monocentric retrospective study. Hum. Reprod. 2021, 36, 16–25. [Google Scholar] [CrossRef]
- Williams, D.H.; Karpman, E.; Sander, J.C.; Spiess, P.E.; Pisters, L.L.; Lipshultz, L.I. Pretreatment semen parameters in men with cancer. J. Urol. 2009, 181, 736–740. [Google Scholar] [CrossRef]
- Hallak, J.; Mahran, A.; Chae, J.; Agarwal, A. Poor semen quality from patients with malignancies does not rule out sperm banking. Urol. Res. 2000, 28, 281–284. [Google Scholar] [CrossRef] [PubMed]
- Van Casteren, N.J.; Boellaard, W.P.A.; Romijn, J.C.; Dohle, G.R. Gonadal dysfunction in male cancer patients before cytotoxic treatment. Int. J. Androl. 2010, 33, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Amirjannati, N.; Sadeghi, M.; Hosseini Jadda, S.H.; Ranjbar, F.; Kamali, K.; Akhondi, M.A. Evaluation of semen quality in patients with malignancies referred for sperm banking before cancer treatment. Andrologia 2011, 43, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Ferlay, J.; Colombet, M.; Soerjomataram, I.; Mathers, C.; Parkin, D.M.; Piñeros, M.; Znaor, A.; Bray, F. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 2019, 144, 1941–1953. [Google Scholar] [CrossRef] [PubMed]
- Salmon-Divon, M.; Shrem, G.; Balayla, J.; Nehushtan, T.; Volodarsky-Perel, A.; Steiner, N.; Son, W.-Y.; Dahan, M.H. An age-based sperm nomogram: The McGill reference guide. Hum. Reprod. 2020, 35, 2213–2225. [Google Scholar] [CrossRef]
- Cooper, T.G.; Noonan, E.; von Eckardstein, S.; Auger, J.; Baker, H.W.G.; Behre, H.M.; Haugen, T.B.; Kruger, T.; Wang, C.; Mbizvo, M.T. World Health Organization reference values for human semen characteristics. Hum. Reprod. Update 2010, 16, 231–245. [Google Scholar] [CrossRef]
- Campbell, M.J.; Lotti, F.; Baldi, E.; Schlatt, S.; Festin, M.P.R.; Björndahl, L.; Toskin, I.; Barratt, C.L.R. Distribution of semen examination results 2020—A follow up of data collated for the WHO semen analysis manual 2010. Andrology 2021, 9, 817–822. [Google Scholar] [CrossRef]
- Hazra, A.; Gogtay, N. IJD® module on biostatistics and research methodology for the dermatologist—Module editor: SAUMYA panda. Indian J. Dermatol. 2016, 61, 251–260. [Google Scholar] [CrossRef]
- rapidtable.com. Pie Chart Maker. 2022. Available online: https://www.rapidtables.com/tools/pie-chart.html (accessed on 17 February 2022).
- Brannigan, R.E.; Fantus, R.J.; Halpern, J.A. Fertility preservation in men: A contemporary overview and a look toward emerging technologies. Fertil. Steril. 2021, 115, 1126–1139. [Google Scholar] [CrossRef]
- Gandini, L.; Lombardo, F.; Salacone, P.; Paoli, D.; Anselmo, A.P.; Culasso, F.; Dondero, F.; Lenzi, A. Testicular cancer and Hodgkin’s disease: Evaluation of semen quality. Hum. Reprod. 2003, 18, 796–801. [Google Scholar] [CrossRef]
- Meirow, D.; Schenker, J.G. Cancer and male infertility. Hum. Reprod. 1995, 10, 2017–2022. [Google Scholar] [CrossRef]
- Bahadur, G.; Ozturk, O.; Muneer, A.; Wafa, R.; Ashraf, A.; Jaman, N.; Patel, S.; Oyede, A.W.; Ralph, D.J. Semen quality before and after gonadotoxic treatment. Hum. Reprod. 2005, 20, 774–781. [Google Scholar] [CrossRef]
- Degl’Innocenti, S.; Filimberti, E.; Magini, A.; Krausz, C.; Lombardi, G.; Fino, M.G.; Rastrelli, G.; Maggi, M.; Baldi, E. Semen cryopreservation for men banking for oligospermia, cancers, and other pathologies: Prediction of post-thaw outcome using basal semen quality. Fertil. Steril. 2013, 100, 1555–1563. [Google Scholar] [CrossRef]
- Di Bisceglie, C.; Bertagna, A.; Composto, E.R.; Lanfranco, F.; Baldi, M.; Motta, G.; Barberis, A.M.; Napolitano, E.; Castellano, E.; Manieri, C. Effects of oncological treatments on semen quality in patients with testicular neoplasia or lymphoproliferative disorders. Asian J. Androl. 2013, 15, 425–429. [Google Scholar] [CrossRef]
- Nagler, H.M. Male factor infertility: A solitary semen analysis can never predict normal fertility. Nat. Rev. Urol. 2011, 8, 16–17. [Google Scholar] [CrossRef]
- Borges, E., Jr. Total motile sperm count: A better way to rate the severity of male factor infertility? JBRA Assist. Reprod. 2016, 20, 47–48. [Google Scholar] [CrossRef]
- Guzick, D.S.; Overstreet, J.W.; Factor-Litvak, P.; Brazil, C.K.; Nakajima, S.T.; Coutifaris, C.; Carson, S.A.; Cisneros, P.; Steinkampf, M.P.; Hill, J.A.; et al. Sperm morphology, motility, and concentration in fertile and infertile men. N. Engl. J. Med. 2001, 345, 1388–1393. [Google Scholar] [CrossRef]
- Buck Louis, G.M.; Sundaram, R.; Schisterman, E.F.; Sweeney, A.; Lynch, C.D.; Kim, S.; Maisog, J.M.; Gore-Langton, R.; Eisenberg, M.L.; Chen, Z. Semen quality and time to pregnancy: The Longitudinal Investigation of Fertility and the Environment Study. Fertil. Steril. 2014, 101, 453–462. [Google Scholar] [CrossRef]
- Slama, R.; Eustache, F.; Ducot, B.; Jensen, T.K.; Jørgensen, N.; Horte, A.; Irvine, S.; Suominen, J.; Andersen, A.G.; Auger, J.; et al. Time to pregnancy and semen parameters: A cross-sectional study among fertile couples from four European cities. Hum. Reprod. 2002, 17, 503–515. [Google Scholar] [CrossRef]
- Ayala, C.; Steinberger, E.; Smith, D.P. The influence of semen analysis parameters on the fertility potential of infertile couples. J. Androl. 1996, 17, 718–725. [Google Scholar]
- Keihani, S.; Verrilli, L.E.; Zhang, C.; Presson, A.P.; Hanson, H.A.; Pastuszak, A.W.; Johnstone, E.B.; Hotaling, J.M. Semen parameter thresholds and time-to-conception in subfertile couples: How high is high enough? Hum. Reprod. 2021, 36, 2121–2133. [Google Scholar] [CrossRef]



| Beta | 95% CI | p | R2 | |
|---|---|---|---|---|
| Volume * | −12.1% | −16.3%, −8.6% | <0.001 | 0.02 |
| Concentration * | −65.6% | −68.3%, −62.8% | <0.001 | 0.10 |
| Total count (millions) * | −72.7% | −75.0%, −69.0% | <0.001 | 0.09 |
| Total motility (%) | −33 | −34.9, −31.1 | <0.001 | 0.15 |
| Rapid motility (%) | −22.2 | −23.8, −20.6 | <0.001 | 0.10 |
| Progressive Motility (%) | −24.7 | −26.3, −23.1 | <0.001 | 0.09 |
| Semen Parameter | Cancer Type | Beta | 95% CI | p |
|---|---|---|---|---|
| Total count (millions) * | Carcinoma | −73.3% | −78.3%, −67.2% | <0.001 |
| Hematological cancer | −57.6% | −63.8%, −50.4% | <0.001 | |
| Germ cell tumor | −82.7% | −85.4%, −79.4% | <0.001 | |
| Sarcoma | −76.8% | −82.4%, −69.3% | <0.001 | |
| Volume (mL) * | Carcinoma | −11.6% | −19.4%, −3.11% | <0.01 |
| Hematological cancer | −12.4% | −18.4%, −5.9% | <0.001 | |
| Germ cell tumor | −7.4% | −14.3%, −0.007% | <0.05 | |
| Sarcoma | −27.3% | −35.9%, −17.6% | <0.001 | |
| Concentration (mil/mL) * | Carcinoma | −69.4% | −74%, −64.1% | <0.001 |
| Hematological cancer | −48.5% | −54.5%, −41.7% | <0.001 | |
| Germ cell tumor | −78.8% | −81.5%, −75.7% | <0.001 | |
| Sarcoma | −57.9% | −66.2%, −47.5% | <0.001 | |
| Total motility (%) | Carcinoma | −33.3 | −37.2, −29.4 | <0.001 |
| Hematological cancer | −28.7 | −31.7, −25.7% | <0.001 | |
| Germ cell tumor | −38.7 | −42, −35.4 | <0.001 | |
| Sarcoma | −31.2 | −36.5, −25.8 | <0.001 | |
| Rapid motility(%) | Carcinoma | −22.5 | −25.9, −19.2 | <0.001 |
| Hematological cancer | −19.8 | −22.3, −17.2 | <0.001 | |
| Germ cell tumor | −24.4 | −27.3,−21.6 | <0.001 | |
| Sarcoma | −23.4 | −27.9,−18.9 | <0.001 | |
| Progressive Motility (%) | Carcinoma | −24.4 | −27.8, −21 | <0.001 |
| Hematological cancer | −21.7 | −24.3, −19.1 | <0.001 | |
| Germ cell tumor | −28.1 | −31, −25.2 | <0.001 | |
| Sarcoma | −26.2 | −30.8, −21.6 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shrem, G.; Azani, L.; Feferkorn, I.; Listovsky, T.; Hussaini, S.; Farber, B.; Dahan, M.H.; Salmon-Divon, M. Effect of Malignancy on Semen Parameters. Life 2022, 12, 922. https://doi.org/10.3390/life12060922
Shrem G, Azani L, Feferkorn I, Listovsky T, Hussaini S, Farber B, Dahan MH, Salmon-Divon M. Effect of Malignancy on Semen Parameters. Life. 2022; 12(6):922. https://doi.org/10.3390/life12060922
Chicago/Turabian StyleShrem, Guy, Liat Azani, Ido Feferkorn, Tamar Listovsky, Sofia Hussaini, Benjamin Farber, Michael H. Dahan, and Mali Salmon-Divon. 2022. "Effect of Malignancy on Semen Parameters" Life 12, no. 6: 922. https://doi.org/10.3390/life12060922
APA StyleShrem, G., Azani, L., Feferkorn, I., Listovsky, T., Hussaini, S., Farber, B., Dahan, M. H., & Salmon-Divon, M. (2022). Effect of Malignancy on Semen Parameters. Life, 12(6), 922. https://doi.org/10.3390/life12060922







