Abstract
Systemic sclerosis is a connective tissue disease of unknown origin that is characterized by immune system abnormalities, vascular damage, and extensive fibrosis of the skin and visceral organs. α2-antiplasmin is known to be the main plasmin inhibitor and has various functions such as cell differentiation and cytokine production, as well as the regulation of the maintenance of the immune system, endothelial homeostasis, and extracellular matrix metabolism. The expression of α2-antiplasmin is elevated in dermal fibroblasts from systemic sclerosis patients, and the blockade of α2-antiplasmin suppresses fibrosis progression and vascular dysfunction in systemic sclerosis model mice. α2-antiplasmin may have promise as a potential therapeutic target for systemic sclerosis. This review considers the role of α2-antiplasmin in the progression of systemic sclerosis.
1. Introduction
Systemic sclerosis (SSc) is an autoimmune rheumatic disease of an unknown origin characterized by immune abnormalities, vascular damage, and fibrosis of the skin and visceral organs [1]. This process usually occurs over many months or years and can lead to organ damage or death. The precise mechanism of SSc progression remains unclear, and there are no therapies to halt the progression of the disease.
The fibrinolytic system dissolves fibrin and maintains vascular homeostasis. The regulators of fibrinolysis contain plasminogen (Plg), a proenzyme which is converted into plasmin by urokinase-type PA (uPA)/uPA receptor (uPAR) or tissue-type plasminogen activator (tPA). The converted-plasmin digests fibrin clots, and fibrin degradation products (FDP) of different molecular weights, including D-dimer, are released into the bloodstream. In contrast, α2-antiplasmin (α2AP) functions as the main inhibitor of plasmin, forming a stable complex plasmin-α2AP (PAP), and results in the inhibition of fibrinolysis [2] (Figure 1). Plasminogen activator inhibitor-1 (PAI-1) binds tPA and uPA and inhibits the generation of plasmin. It has been reported that an uPAR deficiency promotes endothelial dysfunction and fibrosis progression [3,4], and a α2AP deficiency and PAI-1 neutralization attenuate dermal inflammation and fibrosis progression in the bleomycin-induced SSc model mice, and multiple studies suggest that the fibrinolytic factors are associated with the pathology of SSc [5,6,7].

Figure 1.
Fibrinolytic system. The fibrinolytic system dissolves fibrin. Plg is converted into plasmin by tPA or uPA/uPAR. The converted-plasmin digests fibrin clots, and FDP (D-dimer) is released into the bloodstream. α2AP functions as the main inhibitor of plasmin and inhibits fibrinolysis. PAI-1 binds and blocks tPA and uPA and inhibits the conversion of Plg to plasmin.
α2AP is a serine protease inhibitor (serpin) that rapidly inactivates plasmin on the fibrin clots or in the circulation [2,8,9]. α2AP has various biological functions independent of plasmin and is associated with thrombosis, angiogenesis, vascular remodeling, fibrosis, brain functions, and bone homeostasis [10,11,12,13,14,15,16,17]. The expression of α2AP is elevated in SSc dermal fibroblasts, and the blockade of α2AP suppresses the progression of pathology in SSc dermal fibroblasts and SSc model mice [18,19]. This review describes the biological functions of α2AP and summarizes the role of α2AP in the progression of SSc.
2. Systemic Sclerosis
SSc is a connective tissue disease of unknown origin characterized by the fibrosis of skin and visceral organs and peripheral circulatory disturbance. The progression of SSc is associated with immune abnormalities (immune cell activation and auto-antibodies production), vascular dysfunction (defective angiogenesis and vasculogenesis, vascular tone alteration, coagulation abnormalities, and endothelial to mesenchymal transition (EndoMT)), and fibrosis (extracellular matrix (ECM) over-production and ECM degradation inhibition) [1]. These abnormalities occur in the various stages of the disease, and these features influence each other and lead to extensive fibrosis and involvement of multiple organs [20,21]. However, the progression of this disease is not completely understood, and there are no therapies to halt the progression of this disease.
3. α2AP
α2AP is a serpin with a molecular weight of 65–70 kd [2] and functions as the main inhibitor of plasmin, a principal component of the fibrinolytic system [2,8,9]. α2AP has been observed in a number of tissues, such as the liver and kidney [22]. Congenital deficiency of α2AP is inherited in an autosomal recessive condition, and individuals with a homozygous α2AP deficiency exhibit severe bleeding symptoms, while heterozygous individuals have mild bleeding tendencies or may be asymptomatic [23,24]. It has been reported that α2AP is associated with pulmonary embolism, ischemic stroke, thrombotic thrombocytopenic purpura (TTP), and arterial thrombosis, and the removal of venous thrombi, wound healing, and fibrosis in several animal studies [6,23,25]. The N-terminal sequence is crosslinked to fibrin by Factor XIIIa (FXIIIa), and the C-terminal region regulates the interaction with plasmin. An antiplasmin-cleaving enzyme (APCE) or fibroblast activation protein (FAP), such as dipeptidyl peptidase 4 (DPP4), causes the cleaving of Met-α2AP to Asn-α2AP (12-amino-acid residue shorter form) [26,27]. It has been reported that Asn-α2AP becomes cross-linked to fibrin approximately 13 times faster than Met-α2AP during clot formation (Figure 2) [28]. In addition, matrix metalloproteinases-3 (MMP-3) inactivates α2AP by cleaving its Pro19-Leu20 peptide bond [29].
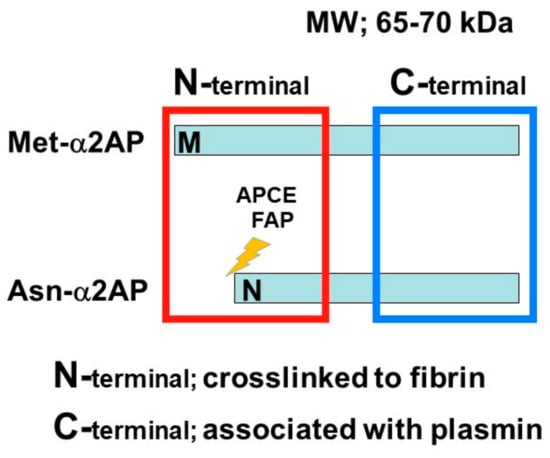
Figure 2.
α2AP α2AP is a serpin with a molecular weight of 65–70 kd. The N-terminal sequence is crosslinked to fibrin, and the C-terminal region regulates the interaction with plasmin. Antiplasmin-cleaving enzyme (APCE) or fibroblast activation protein (FAP) causes the cleaving of Met-α2AP to Asn-α2AP (12-amino-acid residue shorter form).
α2AP is most closely related to the noninhibitory serpin pigment epithelium-derived factor (PEDF) [30]. Both α2AP and PEDF have three β-sheets and nine α-helices, and their positions are similar (Figure 3) [31,32]. α2AP and PEDF have very similar structures, and α2AP can bind and activate adipose triglyceride lipase (ATGL), which is known to be a receptor for PEDF [33] and regulates cell signaling, cytokine production, ECM production, cell differentiation, and cell proliferation [5,10,11,34,35]. PEDF has been shown to cause anti-angiogenic effects by inhibiting VEGF signaling [36] and α2AP also inhibits VEGF signaling [19]. α2AP and PEDF may bind the same protein and have similar functions. Furthermore, α2AP contains an arginine-glycine-aspartic acid (RGD) sequence, which is a recognition sequence for integrins [37].

Figure 3.
The structure of α2AP and PEDF. The structures of α2AP and PEDF are based on 2R9Y.pdb and 1IMV.pdb, respectively. The three β-sheets are shown in yellow (labeled sA-sC) and the 9 α-helices are shown in pink (labeled hA-hI).
4. α2AP Intracellular Signaling
α2AP can activate multiple intracellular signaling pathways, such as c-Jun N-terminal kinase (JNK), extracellular signal-regulated kinase 1/2 (ERK1/2), p38 mitogen-activated protein kinase (MAPK), and src-homology domain-2, containing tyrosine phosphatase 2 (SHP2) [11,13,19,38,39]. In addition, α2AP affects the vascular endothelial growth factor (VEGF) signaling [19], the angiotensin II (AngII) signaling [15], and the advanced glycation end products (AGEs)-induced smad signaling [40]. α2AP and PEDF have a similar structure, and α2AP can activate the adipose triglyceride lipase (ATGL), which is one of the PEDF receptors. PEDF can bind to ATGL, laminin receptor (LR), low-density lipoprotein-related protein 6 (LRP6), and the Notch receptor, and activate various cell signal pathways such as JNK and p38 MAPK [36]. α2AP activates phospholipase A2 (PLA2) through ATGL, which then promotes prostaglandin F2α (PGF2α) synthesis and transforming growth factor-β (TGF-β) production [34]. In addition, α2AP deficiency promotes the expression status of β-catenin, and α2AP attenuates Wnt-3a-induced β-catenin expression and LRP6 activation [12]. Thus, α2AP can activate cell signaling through PEDF-binding proteins, such as ATGL and LRP6, and α2AP may also bind other PEDF-binding proteins and activate various cell signal pathways. On the other hand, α2AP has an RGD sequence at its C-terminus [37], and the RGD sequence affects cell recognition and platelet activation through integrin signaling [41,42].
Plasmin regulates the various signal pathways such as ERK1/2, p38 MAPK, Akt nuclear factor-κB (NF-κB), adenosine monophosphate-activated protein kinase (AMPK), signal transducers, and activators of transcription (STAT) pathways [9,43,44,45]. In addition, plasmin can activate growth factors such as TGF-β, VEGF, basic fibroblast growth factor (bFGF), pro-brain derived neurotrophic factor (proBDNF), insulin-like growth factor-binding protein 5 (IGFBP-5), and hepatocyte growth factor (HGF) [31,46,47]. Furthermore, plasmin can activate MMP-1, MMP-3, MMP-9, and protease-activated receptor-1 (PAR-1), PAR-4, platelets, factors V, VIII, and X [9,48,49,50]. α2AP may regulate various biological functions through plasmin inhibition and α2AP’s self-mediated signaling (Figure 4).
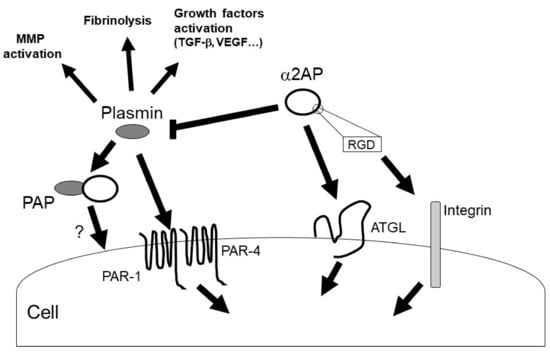
Figure 4.
α2AP signaling. α2AP rapidly inactivates plasmin in fibrin clots or in the circulation, resulting in the formation of PAP. α2AP not only inhibits plasmin activity but also activates ATGL and regulates cell signaling. In addition, α2AP contains an RGD sequence and regulates integrin signaling. On the other hand, plasmin has various functions such as fibrinolysis, growth factors and MMPs activation.
5. α2AP Deposition in SSc
The expression of α2AP is elevated in dermal fibroblasts obtained from SSc patients and in the fibrotic tissue of SSc model mice [11,18]. In addition, the levels of PAP in plasma are elevated in patients with SSc [51]. The deposition of α2AP may affect the progression of SSc.
Connective tissue growth factor (CTGF) and interferon-γ (IFN-γ) induce α2AP production through the ERK1/2 and JNK pathways in fibroblasts [11]. In addition, high-mobility group box 1 (HMGB1) induced the production of α2AP through the receptor for advanced glycation end products (RAGE) in fibroblasts [11]. Serum CTGF, IFN-γ, and HMGB1 levels in SSc patients are higher than those in healthy controls [52,53,54]. The blockade of these factors by neutralizing antibodies or inhibitors attenuates dermal fibrosis in bleomycin-induced SSc model mice [54,55]. The increase in these factors may cause the induction of α2AP expression and be associated with the pathogenesis of SSc.
The cleavage of α2AP by MMP-3 inactivates α2AP functions [29,56]. Serum levels of anti-MMP-3 autoantibody and MMP-3 inhibitor, tissue inhibitors of metalloproteinase-1 (TIMP-1) are elevated in SSc patients [57,58]. In addition, the ratio of MMP-3/TIMP-1 is decreased in SSc dermal fibroblasts [56]. The decrease in MMP-3 activity by MMP-3 autoantibody and inhibitors in SSc may suppress α2AP degradation and cause α2AP deposition.
6. α2AP and Immune Abnormalities in SSc
Immune cells such as T cells, B cells, and macrophages have been found in the skin and blood of SSc patients and SSc model mice [59,60,61], and these immune cells have often been observed preceding the fibrotic process [62]. In SSc, B cells cause the production of autoantibodies and the secretion of pro-inflammatory and pro-fibrotic cytokines such as TGF-β, tumor necrosis factor-α (TNF-α), and interleukin-6 (IL-6). B cells also cooperate with fibroblasts, endothelial cells (ECs), and T cells [61], and B cells are associated with EC apoptosis, fibroblast activation, the upregulation of type I collagen synthesis, and regulate the progression of fibrosis and vascular dysfunction in SSc [63,64]. T cells produce various cytokines such as IL-4, IL-5, IL-6, IL-10, and IL-13 [64], and T cell-produced cytokines regulate macrophage activation. In contrast, dermal fibrosis progression is induced in the bleomycin-administrated T and B cell-deficient severe combined immune deficiency (SCID) mice [65,66]. T cells contribute to macrophage activation, but T and B cells may not be essential for the development of fibrosis. Classically (M1) and alternatively (M2) activated macrophages induce pro-fibrotic cytokines such as TGF-β and IL-6 and TIMPs production, fibroblast activation, and collagen production and collagen deposition, and macrophages play a pivotal role in the development of fibrosis in SSc [63,67]. In particular, M2 macrophages are elevated in SSc patients [68]. M2 macrophages are known to be induced by IL-4 and IL-13 [69], and the blockade of IL-4 and IL-13 signaling by IL-4Rα neutralizing antibodies attenuates the progression of fibrosis in SSc model mice [66]. The increase in pro-fibrotic cytokine expression caused by these immune cells is associated with myofibroblast conversion from tissue-resident fibroblast and bone marrow-derived mesenchymal stem cells (MSC), epithelial-to-mesenchymal transition (EMT), and EndoMT. Myofibroblast deposition subsequently promotes excessive ECM production [70,71]. On the other hand, autoantibodies such as anti-MMP-1, anti-MMP-3, and anti-fibrin bound tPA antibodies have been identified in SSc patients, and TIMPs are elevated in SSc [58,72,73,74,75,76], and these factors suppress ECM degradation. Over-production and suppressed degradation of ECM cause fibrosis. Thus, these immune cells are associated with the overproduction of ECM and suppression of ECM degradation and have a major role in the onset of fibrosis in SSc. The correlation between fibrosis progression and the existence of specific autoantibodies such as anti-centromere antibodies and anti-Scl70 antibodies in SSc patients is unknown.
α2AP induces inflammatory cytokine production such as IL-1β and TNF-α [38,39], and α2AP deficiency affects neutrophil recruitment, lymphocyte infiltration, and IgE production [16,77,78]. In addition, PAP causes an increase in IgG and IgM secretion [79]. The blockade of α2AP by α2AP neutralizing antibodies attenuates anti-Scl70 antibody production in SSc model mice [18]. On the other hand, plasmin directly and indirectly regulates cell migration, cell proliferation, cell adhesion, monocyte chemotaxis, macrophage phagocytosis, neutrophil aggregation, monocyte/macrophage infiltration into tissues, and the release of cytokines, growth factors, and other inflammatory mediators [43,80,81,82,83,84,85,86]. In addition, plasmin can activate protease-activated receptor (PAR), platelets, factors V, VIII, and X, and mediate inflammation response [9,48,49]. Furthermore, plasmin effectively cleaves complement factors C3 and C5, thereby releasing the respective chemotactic anaphylatoxin fragments [87], which results in potentiation of TLR4 signaling [88]. α2AP contributes to inflammatory response, immune modulation, antibody production, and plasmin inhibition, and may play an important role as a mediator of inflammation and the immune system in SSc.
7. α2AP and Vascular Damage in SSc
Vascular damage in SSc includes morphological and functional changes. Microvascular disorders, including Raynaud’s phenomenon, telangiectasias, and digital ulcers, frequently occur in SSc patients [21,89,90]. Raynaud’s phenomenon is usually the initial manifestation and is found in more than 90% of SSc patients. Capillary microscopy of the nailfold of the fingers is a good tool to observe abnormalities in microvasculature. In the active stage of the disease, moderate capillary loss and enlargement, as well as microhemorrhages, are observed. In longstanding SSc, luminal constriction and obstruction are observed as a result of intimal proliferation and marked fibrosis. Furthermore, besides microvascular disorders, SSc patients have higher peripheral vascular disease, the prevalence of coronary atherosclerosis, and cerebrovascular calcification [91].
A number of factors, such as autoantibodies and inflammation caused by immune abnormalities, induce various cytokine production, persistent EC activation, impairment of cell-cell adhesion, EC apoptosis, and the activation of complement and coagulant pathways, and cause the progression of vascular damage, defective angiogenesis and vasculogenesis, EndoMT, vascular tone alteration, and coagulation abnormalities [20,92]. Furthermore, EC damage induces platelet activation, and the activated platelets release profibrotic factors such as TGF-β and platelet-derived growth factor (PDGF). These factors induce fibroblast activation, ECM production, and reactive oxygen species (ROS) release [93]. The activated platelets also activate T cells and B cells through serotonin and CD40L release [93,94]. There is an imbalance between vasodilation and vasoconstriction in SSc. The decrease in endothelial nitric oxide synthase (eNOS) expression and nitric oxide (NO) release from ECs attenuates vasodilation. In the meantime, the increase in vasoconstrictors such as endothelin-1 (ET-1) accelerates abnormal vasoconstriction [63]. Although the expression of VEGF is elevated in the patient’s skin of SSc, defective angiogenesis is evident. Moreover, a decrease in the number of endothelial progenitor cells (EPC) has been reported in SSc patients, resulting in compromised vasculogenesis. Defective angiogenesis and vasculogenesis then cause capillary loss and fibrosis. In SSc, vascular dysfunction is also observed in the lung, kidney, and other organs as well as the skin, causing the development of pulmonary arterial hypertension (PAH) and kidney manifestation [21]. Thus, vascular dysfunction causes more immune abnormalities and ECM deposition in SSc.
α2AP induces the reduction of blood vessels and blood flow and causes vascular damage in mice [19]. In addition, α2AP is associated with vascular remodeling, EC apoptosis, VEGF production, and angiogenesis [10,15]. α2AP deficiency causes VEGF overproduction and an increase in angiogenesis in the cutaneous wound healing process [10], and α2AP attenuates the VEGF-induced pro-angiogenic effects such as EC proliferation and tube formation by inhibiting VEGFR2 through SHP2 activation [19]. The expression of VEGF is elevated in various types of different cells, such as immune cells, ECs, and fibroblasts; nevertheless, vascular insufficiency manifests in SSc [95,96]. The increase in α2AP may cause the impairment of VEGF responses in SSc. In addition, AngII, which regulates vascular constriction and increases blood pressure [97], has profibrotic activity, and serum AngII levels in patients with SSc are higher than those in healthy control [98]. α2AP deficiency attenuates the AngII-induced vascular remodeling and perivascular fibrosis [15]. The increase in α2AP may promote AngII signaling in SSc. Furthermore, α2AP positively regulates the AGEs-induced EndoMT progression through smad signaling activation [40]. The accumulation of AGEs has been observed in the skin of SSc patients [99,100], and the combination of AGEs and α2AP may affect EndoMT progression in SSc.
Plasmin damages EC integrity and endothelial barrier function and causes EC injury [101,102]. In addition, plasmin regulates fibrin-mediated EC spread and proliferation [103], platelet activation and platelet release reactions through PAR [49,104,105], MMP-regulated cell adhesion and cell migration [106], and TGF-β-mediated EC apoptosis [107]. Furthermore, plasmin regulates osteoprotegerin (OPG) production through the ERK1/2 and p38 MAPK pathways [43]. OPG is elevated in SSc and is associated with vascular calcification and atherosclerosis in SSc patients [108]. α2AP plays an important role in vascular homeostasis through its functions and plasmin inhibition and may affect the progression of vascular dysfunction in SSc.
8. α2AP and Fibrosis in SSc
Fibrosis is defined by tissue overgrowth, hardening, and/or scarring due to excessive production, deposition, and contraction of ECM. This process usually occurs over many months or years and causes organ damage or death. The progression of fibrosis is considered to result from maladaptive repair processes caused by profibrotic factors such as TGF-β, CTGF, AngII, PDGF, IFN-γ, and HMGB1, and the profibrotic factors induce myofibroblast differentiation from tissue-resident fibroblasts and bone marrow-derived mesenchymal stem cells (MSCs), epithelial-to-mesenchymal transition (EMT) and EndoMT [55,70,71,109,110,111]. In addition, PGF2α is elevated in SSc patients and is associated with fibrosis progression independently of TGF-β [112,113]. Activated myofibroblasts promote excessive ECM and various cytokine production. Furthermore, SSc myofibroblasts are less prone to undergoing apoptosis [109]. In SSc, the phosphoinositide 3-kinase (PI3K)/Akt pathway and c-Abl are increased, and these factors facilitate myofibroblast survival by inhibiting the activity of BAX [109]. On the other hand, PAP and TIMPs expression are elevated in SSc, and anti-MMP-1 and anti-MMP-3 autoantibodies have been identified in SSc patients [51,58,72,73,74,75,76]. The increase in TIMPs expression and the suppression of MMPs and plasmin activity attenuate ECM degradation and lead to ECM deposition. In addition, high oxidative stress biomarkers such as malondialdehyde (MDA), asymmetric dimethylarginine (ADMA), and 8-Isoprostane, in the circulating blood have been found in SSc patients to mediate the inflammatory response, EndoMT, and fibrosis progression [114,115,116].
α2AP deficiency attenuates fibrosis progression in the bleomycin-induced SSc model mice, and α2AP induces PGF2α and TGF-β production through ATGL and is associated with myofibroblast differentiation, EMT, EndoMT, and ECM production [5,11,34,35,40]. In addition, profibrotic factors including CTGF, HMGB1 and IFN-γ induce α2AP production in fibroblasts [11,38,66], and the increase in α2AP expression may affect fibrosis progression in SSc. Furthermore, it has been reported that α2AP deficiency attenuates oxidative stress [117] and promotes apoptosis [17], and α2AP may affect the induction of oxidative stress and resistance to apoptosis in SSc. On the other hand, plasmin can activate MMPs, such as MMP-1, MMP-3, and MMP-9, and degrade ECM [118,119,120]. In addition, plasmin has an anti-fibrotic function through the activation of HGF, which contributes to anti-fibrosis [47,121] and the induction of myofibroblast apoptosis [122].
9. α2AP and Coagulation/Fibrinolysis in SSc
The fibrinolytic system is known to play an important role in the maintenance of vascular integrity. The fibrinolytic activity is impaired in SSc, and the impaired fibrinolysis system causes fibrin deposition and hyper-coagulation [123,124]. In addition, platelet activation and aggregation in association with the elevated levels of fibrinogen, von Willebrand factor (vWF), lysophosphatidic acid, and sphingosine-1-phosphate (S1P) have been observed in SSc patients [93,125,126]. Fibrin is the most abundant ECM protein during the initial stage of tissue repair and provides a provisional matrix, promoting inward migration of tissue repair cells and preventing excessive blood loss [127]. Fibrin is also associated with angiogenesis, re-epithelialization, fibroblast migration and proliferation, and wound contraction. The fibrin deposition affects vascular injury, inflammation, immune cell activation, fibroblast growth and migration, and contributes to tissue remodeling, thrombosis, hyper-coagulation, pulmonary hypertension, and inflammatory response through multiple mechanisms [128,129,130,131,132]. Furthermore, fibrin regulates leukocyte migration and cell-to-cell adhesion between leukocytes and endothelium, immune cell activation, phagocytosis, and cytokine production [128,133,134,135]. Persistent fibrin enhances collagen accumulation and is associated with the development of dermal fibrosis [127]. Fibrin functions as a ligand for toll-like receptor-4 (TLR-4), vascular endothelial-cadherin (VE-cadherin), intercellular adhesion molecule (ICAM)-1, α5β1, αxβ2, αMβ2 integrin, and stimulates various cells, including leukocytes, ECs, platelets, and fibroblasts [128,136,137,138]. In addition, fibrin can anchor to the endothelial surface through the very-low-density lipoprotein receptor and promote leukocyte transmigration [139]. In vascular diseases, fibrin is present in normal arterial intima and atherosclerotic lesions [129]. In rheumatoid arthritis, fibrin becomes autoantigenic by the posttranslational modification, citrullination, and contributes to the inflammatory response through the TLR-4 pathway [129,140]. The crosslinking of fibrin by FXIII stabilizes fibrin clots, and the stable fibrin supports increased inflammatory cell adhesion, migration, and cytokine production [128,141]. FXIII is also known to induce angiogenesis and neovascularization through VEGFR-2 and αvβ3 integrin [142]. In addition, oxidative stress affects the cross-linking, branching, and height distribution of fibrin and significantly alters thrombus composition and architecture [143,144]. The impaired fibrinolysis system results in fibrin deposition in SSc [123,124]. Patients with SSc may be predisposed to thrombotic arterial complications and macrovascular impairment, which may also contribute to immune abnormalities, vascular damage, and fibrosis progression in SSc. Fibrin clearance may affect the onset of SSc.
α2AP is an important physiological substrate of FAP, including DPP4 [145]. The expression of DPP4 is elevated in the fibrotic skin of SSc patients [146]. The increase in DPP4 expression in SSc may induce the conversion of Met-α2AP to Asn-α2AP and promote cross-linking to fibrin, which then causes impaired fibrinolysis and fibrin deposition in SSc.
10. The Role of α2AP as a Therapeutic Target for SSc
The treatment of α2AP neutralizing antibody improves vascular function and fibrosis and attenuates autoantibody production in SSc model mice [18,19]. In addition, the α2AP neutralizing antibody enhances fibrinolysis and thrombus dissolution [23,25,147]. Furthermore, α2AP deficiency attenuates oxidative stress [117], and α2AP neutralization may attenuate oxidative stress in SSc.
The inactivation of α2AP by MMP-3 recovers the pro-fibrotic phenotype of SSc dermal fibroblasts [56]. The treatment of MMP-3 may promote the degradation of α2AP and recovery of immune abnormalities, vascular damage, and fibrosis progression in SSc.
The inhibition of APCE causes the arrest of Met-α2AP conversion and results in increased fibrinolysis [148]. In addition, the inhibition of DPP4 exerts potent anti-fibrotic effects [146]. On the other hand, Plg interacts with DPP4 and regulates DPP4 activity [81]. The inhibition of APCE and DPP4 may attenuate the cleavage of α2AP and cause an increase in fibrinolysis.
Small non-coding RNA sequences (miRNAs) are associated with vascular, immune response, and ECM homeostasis, and upregulation or downregulation of diverse miRNAs has been observed in blood and tissue from SSc patients [149]. MiR-29a represses α2AP and TIMP-1 expression and recovers the pro-fibrotic phenotype in SSc dermal fibroblasts [56,150]. The MMP-3 activation by the decrease in TIMP-1 expression may cause α2AP inactivation and affect the alleviation of SSc. In addition, an online database predicts that miR-30c can target α2AP mRNA, and the administration of miR-30c attenuates α2AP expression in the skin of SSc model mice [151]. MiR-30c also prevents pro-fibrotic changes such as myofibroblast differentiation, ECM overproduction, and vascular dysfunction, and exerts anti-fibrotic and anti-angiopathic effects in SSc model mice [151]. Furthermore, miR-133a-3p, miR-26a, and miR-30a attenuate fibrosis progression by inhibiting CTGF [152,153,154]. CTGF has been reported to induce α2AP expression [11]. This miRNA treatment may suppress α2AP expression.
The fusion protein of human serum albumin (HSA) to the α2AP N-terminal motif reduces fibrinolytic resistance by crosslinking to fibrinogen and fibrin [155]. In addition, synthetic peptide (AP26) corresponding to the carboxy-terminal region of α2AP enhances the conversion of plasminogen to plasmin induced by uPA and accelerates fibrinolysis [156]. The AP26 peptide also inhibits FXIIIa-catalyzed crosslinking of fibrin [156].
Microplasmin is a derivative of plasmin which lacks the five kringle domains [157], and microplasmin neutralize α2AP activity [158,159]. The neutralization of α2AP by microplasmin reduces ischemic stroke and improves neurological dysfunction [159,160].
The blockade and inactivation of α2AP by neutralizing antibodies, MMP-3, APCE inhibitor, miRNA, fusion proteins, and microplasmin may improve fibrosis progression, vascular dysfunction, and impaired fibrinolysis in SSc (Figure 5).
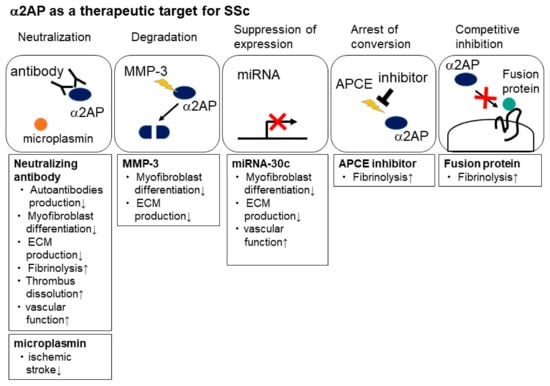
Figure 5.
α2AP as a therapeutic target for SSc. The blockade and inactivation of α2AP by neutralizing antibody, MMP-3, APCE inhibitor, miRNA, fusion proteins, and microplasmin suppress myofibroblast differentiation and ECM production and enhance fibrinolysis and thrombus dissolution and may improve fibrosis progression and vascular dysfunction in SSc.
11. Conclusions and Therapeutic Perspectives
In SSc, immune abnormalities, vascular damage, and fibrosis contribute to disease progression. The changes in α2AP expression and activity may result in immune system activation, disruption of endothelial homeostasis, and aberrant ECM metabolism, which consequently contribute to SSc progression (Figure 6). The blockade of α2AP functions may prevent the progression of SSc and may be a novel therapeutic approach to SSc.

Figure 6.
The mechanism of α2AP-associated SSc progression. The increase in these factors such as CTGF and HMGB1 induces α2AP expression, and the increase in anti-MMP-3 autoantibody and MMP-3 inhibitor, TIMP-1, inhibits α2AP degradation. α2AP deposition induces cytokine production, myofibroblast differentiation, ECM production, plasmin inhibition, and then may cause immune abnormalities, fibrosis progression, and vascular damage.
Author Contributions
Y.K. and E.S. writing—original draft preparation, Y.K. and E.S. writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gilbane, A.; Denton, C.; Holmes, A. Scleroderma Pathogenesis: A Pivotal Role for Fibroblasts as Effector Cells. Arthritis Res. 2013, 15, 215. [Google Scholar] [CrossRef] [PubMed]
- Collen, D. Identification and Some Properties of a New Fast-Reacting Plasmin Inhibitor in Human Plasma. Eur. J. Biochem. 1976, 69, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Kanno, Y.; Kaneiwa, A.; Minamida, M.; Kanno, M.; Tomogane, K.; Takeuchi, K.; Okada, K.; Ueshima, S.; Matsuo, O.; Matsuno, H. The Absence of uPAR Is Associated with the Progression of Dermal Fibrosis. J. Investig. Dermatol. 2008, 128, 2792–2797. [Google Scholar] [CrossRef] [PubMed]
- Manetti, M.; Romano, E.; Rosa, I.; Guiducci, S.; Bellando-Randone, S.; De Paulis, A.; Ibba-Manneschi, L.; Matucci-Cerinic, M. Endothelial-to-Mesenchymal Transition Contributes to Endothelial Dysfunction and Dermal Fibrosis in Systemic Sclerosis. Ann. Rheum. Dis. 2017, 76, 924–934. [Google Scholar] [CrossRef]
- Kanno, Y.; Kuroki, A.; Okada, K.; Tomogane, K.; Ueshima, S.; Matsuo, O.; Matsuno, H. Alpha2-Antiplasmin Is Involved in the Production of Transforming Growth Factor Beta1 and Fibrosis. J. Thromb. Haemost. 2007, 5, 2266–2273. [Google Scholar] [CrossRef]
- Kanno, Y. The Role of Fibrinolytic Regulators in Vascular Dysfunction of Systemic Sclerosis. Int. J. Mol. Sci. 2019, 20, 619. [Google Scholar] [CrossRef]
- Lemaire, R.; Burwell, T.; Sun, H.; Delaney, T.; Bakken, J.; Cheng, L.; Rebelatto, M.C.; Czapiga, M.; De-Mendez, I.; Coyle, A.J.; et al. Resolution of Skin Fibrosis by Neutralization of the Antifibrinolytic Function of Plasminogen Activator Inhibitor 1. Arthritis Rheumatol. 2015, 68, 473–483. [Google Scholar] [CrossRef]
- Lijnen, H.R.; De Cock, F.; Van Hoef, B.; Schlott, B.; Collen, D. Characterization of the Interaction between Plasminogen and Staphylokinase. JBIC J. Biol. Inorg. Chem. 1994, 224, 143–149. [Google Scholar] [CrossRef]
- Kanno, Y.; Ishisaki, A.; Kawashita, E.; Kuretake, H.; Ikeda, K.; Matsuo, O. uPA Attenuated LPS-Induced Inflammatory Osteoclastogenesis through the Plasmin/PAR-1/Ca2+/CaMKK/AMPK Axis. Int. J. Biol. Sci. 2016, 12, 63–71. [Google Scholar] [CrossRef]
- Kanno, Y.; Hirade, K.; Ishisaki, A.; Nakajima, K.; Suga, H.; Into, T.; Matsushita, K.; Okada, K.; Matsuo, O.; Matsuno, H. Lack of Alpha2-Antiplasmin Improves Cutaneous Wound Healing via Over-Released Vascular Endothelial Growth Factor-Induced Angiogenesis in Wound Lesions. J. Thromb. Haemost. 2006, 4, 1602–1610. [Google Scholar] [CrossRef]
- Kanno, Y.; Kawashita, E.; Minamida, M.; Kaneiwa, A.; Okada, K.; Ueshima, S.; Matsuo, O.; Matsuno, H. α2-Antiplasmin Is Associated with the Progression of Fibrosis. Am. J. Pathol. 2010, 176, 238–245. [Google Scholar] [CrossRef]
- Kanno, Y.; Ishisaki, A.; Kuretake, H.; Maruyama, C.; Matsuda, A.; Matsuo, O. α2-Antiplasmin Modulates Bone Formation by Negatively Regulating Osteoblast Differentiation and Function. Int. J. Mol. Med. 2017, 40, 854–858. [Google Scholar] [CrossRef]
- Kawashita, E.; Kanno, Y.; Asayama, H.; Okada, K.; Ueshima, S.; Matsuo, O.; Matsuno, H. Involvement of α2-Antiplasmin in Dendritic Growth of Hippocampal Neurons. J. Neurochem. 2013, 126, 58–69. [Google Scholar] [CrossRef]
- Kawashita, E.; Kanno, Y.; Ikeda, K.; Kuretake, H.; Matsuo, O.; Matsuno, H. Altered Behavior in Mice with Deletion of the Alpha2-Antiplasmin Gene. PLoS ONE 2014, 9, e97947. [Google Scholar] [CrossRef]
- Hou, Y.; Okada, K.; Okamoto, C.; Ueshima, S.; Matsuo, O. Alpha2-Antiplasmin Is a Critical Regulator of Angiotensin II–Mediated Vascular Remodeling. Arter. Thromb. Vasc. Biol. 2008, 28, 1257–1262. [Google Scholar] [CrossRef]
- Kager, L.M.; Weehuizen, T.A.; Wiersinga, W.J.; Roelofs, J.J.T.H.; Meijers, J.C.M.; Dondorp, A.M.; Veer, C.V.; Van Der Poll, T. Endogenous α2-Antiplasmin Is Protective during Severe Gram-Negative Sepsis (Melioidosis). Am. J. Respir. Crit. Care Med. 2013, 188, 967–975. [Google Scholar] [CrossRef]
- Kanno, Y.; Tsuchida, K.; Maruyama, C.; Hori, K.; Teramura, H.; Asahi, S.; Matsuo, O.; Ozaki, K.-I. Alpha2-Antiplasmin Deficiency Affects Depression and Anxiety-Like Behavior and Apoptosis Induced by Stress in Mice. J. Basic Clin. Physiol. Pharmacol. 2021. [Google Scholar] [CrossRef]
- Kanno, Y.; Shu, E.; Kanoh, H.; Seishima, M. The Antifibrotic Effect of α2AP Neutralization in Systemic Sclerosis Dermal Fibroblasts and Mouse Models of Systemic Sclerosis. J. Investig. Dermatol. 2015, 136, 762–769. [Google Scholar] [CrossRef]
- Kanno, Y.; Shu, E.; Kanoh, H.; Matsuda, A.; Seishima, M. α2AP Regulates Vascular Alteration by Inhibiting VEGF Signaling in Systemic Sclerosis: The Roles of α2AP in Vascular Dysfunction in Systemic Sclerosis. Arthritis Res. Ther. 2017, 19, 22. [Google Scholar] [CrossRef]
- Mostmans, Y.; Cutolo, M.; Giddelo, C.; Decuman, S.; Melsens, K.; Declercq, H.; Vandecasteele, E.; De Keyser, F.; Distler, O.; Gutermuth, J.; et al. The Role of Endothelial Cells in the Vasculopathy of Systemic Sclerosis: A Systematic Review. Autoimmun. Rev. 2017, 16, 774–786. [Google Scholar] [CrossRef]
- Kavian, N.; Batteux, F. Macro- and Microvascular Disease in Systemic Sclerosis. Vasc. Pharmacol. 2015, 71, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Menoud, P.A.; Sappino, N.; Boudal-Khoshbeen, M.; Vassalli, J.D.; Sappino, A.P. The Kidney Is a Major Site of α(2)-Antiplasmin Production. J. Clin. Investig. 1996, 97, 2478–2484. [Google Scholar] [CrossRef] [PubMed]
- Pechlivani, N.; Kearney, K.J.; Ajjan, R.A. Fibrinogen and Antifibrinolytic Proteins: Interactions and Future Therapeutics. Int. J. Mol. Sci. 2021, 22, 12537. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, S.; Mathew, P. α2-Antiplasmin and Its Deficiency: Fibrinolysis Out of Balance. Haemophilia 2008, 14, 1250–1254. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Houng, A.K.; Reed, G.L. Venous Stasis-Induced Fibrinolysis Prevents Thrombosis in Mice: Role of α2-Antiplasmin. Blood 2019, 134, 970–978. [Google Scholar] [CrossRef]
- Lee, K.N.; Jackson, K.W.; Christiansen, V.J.; Lee, C.S.; Chun, J.-G.; McKee, P.A. Antiplasmin-Cleaving Enzyme Is a Soluble Form of Fibroblast Activation Protein. Blood 2006, 107, 1397–1404. [Google Scholar] [CrossRef]
- Christiansen, V.J.; Jackson, K.W.; Lee, K.N.; McKee, P.A. Effect of Fibroblast Activation Protein and α2-Antiplasmin Cleaving Enzyme on Collagen Types I, III, and IV. Arch. Biochem. Biophys. 2007, 457, 177–186. [Google Scholar] [CrossRef]
- Lee, K.N.; Jackson, K.W.; Christiansen, V.J.; Chung, K.H.; McKee, P.A. A Novel Plasma Proteinase Potentiates α2-Antiplasmin Inhibition of Fibrin Digestion. Blood 2004, 103, 3783–3788. [Google Scholar] [CrossRef]
- Lijnen, H.; Van Hoef, B.; Collen, D. Inactivation of the Serpin α2-Antiplasmin by Stromelysin-1. Biochim. Biophys. Acta-Protein Struct. Mol. Enzym. 2001, 1547, 206–213. [Google Scholar] [CrossRef]
- Irving, J.; Pike, R.; Lesk, A.; Whisstock, J. Phylogeny of the Serpin Superfamily: Implications of Patterns of Amino Acid Conservation for Structure and Function. Genome Res. 2000, 10, 1845–1864. [Google Scholar] [CrossRef]
- Law, R.; Abu-Ssaydeh, D.; Whisstock, J. New Insights into the Structure and Function of the Plasminogen/Plasmin System. Curr. Opin. Struct. Biol. 2013, 23, 836–841. [Google Scholar] [CrossRef]
- Tombran-Tink, J.; Aparicio, S.; Xu, X.; Tink, A.R.; Lara, N.; Sawant, S.; Barnstable, C.J.; Zhang, S.S.-M. PEDF and the Serpins: Phylogeny, Sequence Conservation, and Functional Domains. J. Struct. Biol. 2005, 151, 130–150. [Google Scholar] [CrossRef]
- Notari, L.; Baladron, V.; Aroca-Aguilar, J.D.; Balko, N.; Heredia, R.; Meyer, C.; Notario, P.M.; Saravanamuthu, S.; Nueda, M.-L.; Sanchez-Sanchez, F.; et al. Identification of a Lipase-Linked Cell Membrane Receptor for Pigment Epithelium-Derived Factor. J. Biol. Chem. 2006, 281, 38022–38037. [Google Scholar] [CrossRef]
- Kanno, Y.; Kawashita, E.; Kokado, A.; Okada, K.; Ueshima, S.; Matsuo, O.; Matsuno, H. Alpha2-Antiplasmin Regulates the Development of Dermal Fibrosis in Mice by Prostaglandin F2α Synthesis through Adipose Triglyceride Lipase/Calcium-Independent Phospholipase A2. Arthritis Rheum. 2013, 65, 492–502. [Google Scholar] [CrossRef]
- Kanno, Y.; Kawashita, E.; Kokado, A.; Kuretake, H.; Ikeda, K.; Okada, K.; Seishima, M.; Ueshima, S.; Matsuo, O.; Matsuno, H. α2AP Mediated Myofibroblast Formation and the Development of Renal Fibrosis in Unilateral Ureteral Obstruction. Sci. Rep. 2014, 4, srep05967. [Google Scholar] [CrossRef]
- Ma, S.; Wang, S.; Li, M.; Zhang, Y.; Zhu, P. The Effects of Pigment Epithelium-Derived Factor on Atherosclerosis: Putative Mechanisms of the Process. Lipids Health Dis. 2018, 17, 240. [Google Scholar] [CrossRef]
- Abdul, S.; Leebeek, F.W.G.; Rijken, D.C.; De Willige, S.U. Natural Heterogeneity of α2-Antiplasmin: Functional and Clinical Consequences. Blood 2016, 127, 538–545. [Google Scholar] [CrossRef]
- Kanno, Y.; Miyashita, M.; Seishima, M.; Matsuo, O. α2AP Is Associated with the Development of Lupus Nephritis through the Regulation of Plasmin Inhibition and Inflammatory Responses. Immun. Inflamm. Dis. 2020, 8, 267–278. [Google Scholar] [CrossRef]
- Shiomi, A.; Kawao, N.; Yano, M.; Okada, K.; Tamura, Y.; Okumoto, K.; Matsuo, O.; Akagi, M.; Kaji, H. α2-Antiplasmin Is Involved in Bone Loss Induced by Ovariectomy in Mice. Bone 2015, 79, 233–241. [Google Scholar] [CrossRef]
- Kanno, Y.; Hirota, M.; Matsuo, O.; Ozaki, K.-I. α2-Antiplasmin Positively Regulates Endothelial-to-Mesenchymal Transition and Fibrosis Progression in Diabetic Nephropathy. Mol. Biol. Rep. 2021, 49, 205–215. [Google Scholar] [CrossRef]
- Thomas, L.; Moore, N.R.; Miller, S.; Booth, N.A. The C-Terminus of α2-Antiplasmin Interacts with Endothelial Cells. Br. J. Haematol. 2006, 136, 472–479. [Google Scholar] [CrossRef]
- Udvardy, M.; Schwartzott, D.; Jackson, K.; McKee, P. Hybrid Peptide Containing RGDF (Arg-Gly-Asp-Phe) Coupled with the Carboxy Terminal Part of Alpha 2-Antiplasmin Capable of Inhibiting Platelet Aggregation and Promoting Fibrinolysis. Blood Coagul. Fibrinolysis 1995, 6, 11–16. [Google Scholar] [CrossRef]
- Kanno, Y.; Ishisaki, A.; Kawashita, E.; Chosa, N.; Nakajima, K.; Nishihara, T.; Toyoshima, K.; Okada, K.; Ueshima, S.; Matsushita, K.; et al. Plasminogen/Plasmin Modulates Bone Metabolism by Regulating the Osteoblast and Osteoclast Function. J. Biol. Chem. 2011, 286, 8952–8960. [Google Scholar] [CrossRef]
- Syrovets, T.; Lunov, O.; Simmet, T. Plasmin as a Proinflammatory Cell Activator. J. Leukoc. Biol. 2012, 92, 509–519. [Google Scholar] [CrossRef]
- Li, X.; Syrovets, T.; Genze, F.; Pitterle, K.; Oberhuber, A.; Orend, K.-H.; Simmet, T. Plasmin Triggers Chemotaxis of Monocyte-Derived Dendritic Cells through an Akt2-Dependent Pathway and Promotes a T-Helper Type-1 Response. Arter. Thromb. Vasc. Biol. 2010, 30, 582–590. [Google Scholar] [CrossRef]
- Draxler, D.F.; Sashindranath, M.; Medcalf, R.L. Plasmin: A Modulator of Immune Function. Semin. Thromb. Hemost. 2017, 43, 143–153. [Google Scholar] [CrossRef]
- Hattori, N.; Mizuno, S.; Yoshida, Y.; Chin, K.; Mishima, M.; Sisson, T.H.; Simon, R.H.; Nakamura, T.; Miyake, M. The Plasminogen Activation System Reduces Fibrosis in the Lung by a Hepatocyte Growth Factor-Dependent Mechanism. Am. J. Pathol. 2004, 164, 1091–1098. [Google Scholar] [CrossRef]
- Kuliopulos, A.; Covic, L.; Seeley, S.K.; Sheridan, P.J.; Helin, J.; Costello, C.E. Plasmin Desensitization of the PAR1 Thrombin Receptor: Kinetics, Sites of Truncation, and Implications for Thrombolytic Therapy. Biochemistry 1999, 38, 4572–4585. [Google Scholar] [CrossRef]
- Quinton, T.M.; Kim, S.; Derian, C.K.; Jin, J.; Kunapuli, S.P.; Reynolds, L.F.; de Bettignies, C.; Norton, T.; Beeser, A.; Chernoff, J.; et al. Plasmin-Mediated Activation of Platelets Occurs by Cleavage of Protease-Activated Receptor 4. J. Biol. Chem. 2004, 279, 18434–18439. [Google Scholar] [CrossRef]
- Trejo, J.; Stover, T.; Kester, M. Protease-Activated Receptors: New Concepts in Regulation of G Protein-Coupled Receptor Signaling and Trafficking. J. Pharmacol. Exp. Ther. 2003, 307, 437–442. [Google Scholar] [CrossRef]
- Jinnin, M.; Ihn, H.; Yamane, K.; Asano, Y.; Yazawa, N.; Tamaki, K. Plasma Plasmin-Alpha2-Plasmin Inhibitor Complex Levels Are Increased in Systemic Sclerosis Patients with Pulmonary Hypertension. Rheumatology 2003, 42, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Bălănescu, P.; Lădaru, A.; Bălănescu, E.; Nicolau, A.; Băicuş, C.; Dan, G. IL-17, IL-6 and IFN-γ in Systemic Sclerosis Patients. Rom. J. Intern. Med. 2015, 53, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Yoshizaki, A.; Komura, K.; Iwata, Y.; Ogawa, F.; Hara, T.; Muroi, E.; Takenaka, M.; Shimizu, K.; Hasegawa, M.; Fujimoto, M.; et al. Clinical Significance of Serum HMGB-1 and sRAGE Levels in Systemic Sclerosis: Association with Disease Severity. J. Clin. Immunol. 2008, 29, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Makino, K.; Makino, T.; Stawski, L.; Lipson, K.E.; Leask, A.; Trojanowska, M. Anti-Connective Tissue Growth Factor (CTGF/CCN2) Monoclonal Antibody Attenuates Skin Fibrosis in Mice Models of Systemic Sclerosis. Arthritis Res. Ther. 2017, 19, 134. [Google Scholar] [CrossRef]
- Yamashita, T.; Asano, Y.; Taniguchi, T.; Nakamura, K.; Saigusa, R.; Miura, S.; Toyama, T.; Takahashi, T.; Ichimura, Y.; Yoshizaki, A.; et al. Glycyrrhizin Ameliorates Fibrosis, Vasculopathy, and Inflammation in Animal Models of Systemic Sclerosis. J. Investig. Dermatol. 2016, 137, 631–640. [Google Scholar] [CrossRef]
- Niwa, H.; Kanno, Y.; Shu, E.; Seishima, M. Decrease in Matrix Metalloproteinase-3 Activity in Systemic Sclerosis Fibroblasts Causes α2-Antiplasmin and Extracellular Matrix Deposition, and Contributes to Fibrosis Development. Mol. Med. Rep. 2020, 22, 3001–3007. [Google Scholar] [CrossRef]
- Young-Min, S.A.; Beeton, C.; Laughton, R.; Plumpton, T.; Bartram, S.; Murphy, G.; Black, C.; Cawston, T.E. Serum TIMP-1, TIMP-2, and MMP-1 in Patients with Systemic Sclerosis, Primary Raynaud’s Phenomenon, and in Normal Controls. Ann. Rheum. Dis. 2001, 60, 846–851. [Google Scholar]
- Nishijima, C.; Hayakawa, I.; Matsushita, T.; Komura, K.; Hasegawa, M.; Takehara, K.; Sato, S. Autoantibody against Matrix Metalloproteinase-3 in Patients with Systemic Sclerosis. Clin. Exp. Immunol. 2004, 138, 357–363. [Google Scholar] [CrossRef]
- Higashi-Kuwata, N.; Jinnin, M.; Makino, T.; Fukushima, S.; Inoue, Y.; Muchemwa, F.C.; Yonemura, Y.; Komohara, Y.; Takeya, M.; Mitsuya, H.; et al. Characterization of Monocyte/Macrophage Subsets in the Skin and Peripheral Blood Derived from Patients with Systemic Sclerosis. Arthritis Res. Ther. 2010, 12, R128. [Google Scholar] [CrossRef]
- O’Reilly, S.; Hügle, T.; Van Laar, J.M. T Cells in Systemic Sclerosis: A Reappraisal. Rheumatology 2012, 51, 1540–1549. [Google Scholar] [CrossRef]
- Sanges, S.; Guerrier, T.; Launay, D.; Lefèvre, G.; Labalette, M.; Forestier, A.; Sobanski, V.; Corli, J.; Hauspie, C.; Jendoubi, M.; et al. Role of B Cells in the Pathogenesis of Systemic Sclerosis. Rev. Médecine Interne 2016, 38, 113–124. [Google Scholar] [CrossRef]
- Fuschiotti, P. Current Perspectives on the Immunopathogenesis of Systemic Sclerosis. ImmunoTargets Ther. 2016, 5, 21–35. [Google Scholar] [CrossRef]
- Pattanaik, D.; Brown, M.; Postlethwaite, B.; Postlethwaite, A. Pathogenesis of Systemic Sclerosis. Front. Immunol. 2015, 6, 272. [Google Scholar] [CrossRef]
- Brown, M.; O’Reilly, S. The Immunopathogenesis of Fibrosis in Systemic Sclerosis. Clin. Exp. Immunol. 2018, 195, 310–321. [Google Scholar] [CrossRef]
- Yamamoto, T.; Nishioka, K. Animal Model of Sclerotic Skin. IV: Induction of Dermal Sclerosis by Bleomycin is T Cell Independent. J. Investig. Dermatol. 2001, 117, 999–1001. [Google Scholar] [CrossRef][Green Version]
- Kanno, Y.; Shu, E.; Niwa, H.; Kanoh, H.; Seishima, M. Alternatively Activated Macrophages Are Associated with the α2AP Production that Occurs with the Development of Dermal Fibrosis: The Role of Alternatively Activated Macrophages on the Development of Fibrosis. Arthritis Res. Ther. 2020, 22, 76. [Google Scholar] [CrossRef]
- Zhang, L.; Wang, Y.; Wu, G.; Xiong, W.; Gu, W.; Wang, C. Macrophages: Friend or Foe in Idiopathic Pulmonary Fibrosis? Respir. Res. 2018, 19, 170. [Google Scholar] [CrossRef]
- Nakayama, W.; Jinnin, M.; Makino, K.; Kajihara, I.; Makino, T.; Fukushima, S.; Inoue, Y.; Ihn, H. Serum Levels of Soluble CD163 in Patients with Systemic Sclerosis. Rheumatol. Int. 2010, 32, 403–407. [Google Scholar] [CrossRef]
- Mosser, D.M.; Edwards, J.P. Exploring the Full Spectrum of Macrophage Activation. Nat. Rev. Immunol. 2008, 8, 958–969. [Google Scholar] [CrossRef]
- LeBleu, V.S.; Taduri, G.; O’Connell, J.; Teng, Y.; Cooke, V.G.; Woda, C.; Sugimoto, H.; Kalluri, R. Origin and Function of Myofibroblasts in Kidney Fibrosis. Nat. Med. 2013, 19, 1047–1053. [Google Scholar] [CrossRef]
- Tsukui, T.; Shichino, S.; Shimaoka, T.; Ueha, S.; Matsushima, K. Cellular and Molecular Mechanisms of Chronic Inflammation-Associated Organ Fibrosis. In Chronic Inflammation; Springer: Tokyo, Japan, 2016; pp. 19–36. [Google Scholar] [CrossRef]
- Nunes, J.P.L.; Cunha, A.C.; Meirinhos, T.; Nunes, A.; Araújo, P.M.; Godinho, A.R.; Vilela, E.M.; Vaz, C. Prevalence of Auto-Antibodies Associated to Pulmonary Arterial Hypertension in Scleroderma—A Review. Autoimmun. Rev. 2018, 17, 1186–1201. [Google Scholar] [CrossRef] [PubMed]
- Ciechomska, M.; Huigens, C.A.; Hügle, T.; Stanly, T.; Gessner, A.; Griffiths, B.; Radstake, T.R.D.J.; Hambleton, S.; O’Reilly, S.; Van Laar, J.M. Toll-Like Receptor-Mediated, Enhanced Production of Profibrotic TIMP-1 in Monocytes from Patients with Systemic Sclerosis: Role of Serum Factors. Ann. Rheum. Dis. 2013, 72, 1382–1389. [Google Scholar] [CrossRef] [PubMed]
- Yazawa, N.; Kikuchi, K.; Ihn, H.; Fujimoto, M.; Kubo, M.; Tamaki, T.; Tamaki, K. Serum Levels of Tissue Inhibitor of MetalloProteinases 2 in Patients with Systemic Sclerosis. J. Am. Acad. Dermatol. 2000, 42, 70–75. [Google Scholar] [CrossRef]
- Elias, G.J.; Ioannis, M.; Theodora, P.; Dimitrios, P.P.; Despoina, P.; Kostantinos, V.; Charalampos, K.; Vassilios, V.; Petros, S.P. Circulating Tissue Inhibitor of Matrix Metalloproteinase-4 (TIMP-4) in Systemic Sclerosis Patients with Elevated Pulmonary Arterial Pressure. Mediat. Inflamm. 2008, 2008, 164134. [Google Scholar] [CrossRef] [PubMed]
- Tomimura, S.; Ogawa, F.; Iwata, Y.; Komura, K.; Hara, T.; Muroi, E.; Takenaka, M.; Shimizu, K.; Hasegawa, M.; Fujimoto, M.; et al. Autoantibodies against Matrix Metalloproteinase-1 in Patients with Localized Scleroderma. J. Dermatol. Sci. 2008, 52, 47–54. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Okada, K.; Ueshima, S.; Kawao, N.; Yano, M.; Tamura, Y.; Tanaka, M.; Sakamoto, A.; Hatano, M.; Arima, M.; Miyata, S.; et al. Lack of Both α2-Antiplasmin and Plasminogen Activator Inhibitor Type-1 Induces High IgE Production. Life Sci. 2013, 93, 89–95. [Google Scholar] [CrossRef]
- Eddy, J.L.; Schroeder, J.A.; Zimbler, D.L.; Bellows, L.E.; Lathem, W.W. Impact of the Pla Protease Substrate α2-Antiplasmin on the Progression of Primary Pneumonic Plague. Infect. Immun. 2015, 83, 4837–4847. [Google Scholar] [CrossRef]
- Zhabin, S.G.; Gorin, V.S. The Effects of Alpha 2-Antiplasmin Complex and Alpha 2-Antiplasmin on the Secretion of IgG and IgM by Cultured Human Mononuclear Cells. J. Clin. Lab. Immunol. 1997, 49, 77–82. [Google Scholar]
- Didiasova, M.; Wujak, L.; Wygrecka, M.; Zakrzewicz, D. From Plasminogen to Plasmin: Role of Plasminogen Receptors in Human Cancer. Int. J. Mol. Sci. 2014, 15, 21229–21252. [Google Scholar] [CrossRef]
- Kanno, Y.; Sakai, A.; Miyashita, M.; Tsuchida, K.; Matsuo, O. Plasminogen Deficiency Is Associated with Improved Glucose Tolerance, and Lower DPP-4 Activity. Diabetes Res. Clin. Pr. 2016, 120, 190–193. [Google Scholar] [CrossRef]
- Gomez-Salinero, J.M.; Rafii, S. Plasmin Regulation of Acute Cytokine Storm. Blood 2017, 130, 5–6. [Google Scholar] [CrossRef]
- Deryugina, E.I.; Quigley, J.P. Cell Surface Remodeling by Plasmin: A New Function for an Old Enzyme. J. Biomed. Biotechnol. 2012, 2012, 564259. [Google Scholar] [CrossRef]
- Das, R.; Ganapathy, S.; Settle, M.; Plow, E.F. Plasminogen Promotes Macrophage Phagocytosis in Mice. Blood 2014, 124, 679–688. [Google Scholar] [CrossRef]
- Lorenz, N.; Loef, E.J.; Kelch, I.D.; Verdon, D.J.; Black, M.M.; Middleditch, M.J.; Greenwood, D.R.; Graham, E.S.; Brooks, A.E.; Dunbar, P.R.; et al. Plasmin and Regulators of Plasmin Activity Control the Migratory Capacity and Adhesion of Human T Cells and Dendritic Cells by Regulating Cleavage of the Chemokine CCL21. Immunol. Cell Biol. 2016, 94, 955–963. [Google Scholar] [CrossRef]
- Shimazu, H.; Munakata, S.; Tashiro, Y.; Salama, Y.; Dhahri, D.; Eiamboonsert, S.; Ota, Y.; Onoda, H.; Tsuda, Y.; Okada, Y.; et al. Pharmacological Targeting of Plasmin Prevents Lethality in a Murine Model of Macrophage Activation Syndrome. Blood 2017, 130, 59–72. [Google Scholar] [CrossRef]
- Amara, U.; Flierl, M.A.; Rittirsch, D.; Klos, A.; Chen, H.; Acker, B.; Brückner, U.B.; Nilsson, B.; Gebhard, F.; Lambris, J.D.; et al. Molecular Intercommunication between the Complement and Coagulation Systems. J. Immunol. 2010, 185, 5628–5636. [Google Scholar] [CrossRef]
- Ward, J.R.; Dower, S.K.; Whyte, M.K.; Buttle, D.J.; Sabroe, I. Potentiation of TLR4 signalling by Plasmin Activity. Biochem. Biophys. Res. Commun. 2006, 341, 299–303. [Google Scholar] [CrossRef]
- Block, J.; Sequeira, W. Raynaud’s Phenomenon. Lancet 2001, 357, 2042–2048. [Google Scholar] [CrossRef]
- Walker, J.G.; Stirling, J.; Beroukas, D.; Dharmapatni, K.; Haynes, D.R.; Smith, M.D.; Ahern, M.J.; Roberts-Thomson, P.J. Histopathological and Ultrastructural Features of Dermal Telangiectasias in Systemic Sclerosis. Pathology 2005, 37, 220–225. [Google Scholar] [CrossRef]
- Au, K.; Singh, M.K.; Bodukam, V.K.; Bae, S.; Maranian, P.; Ogawa, R.; Spiegel, B.; McMahon, M.; Hahn, B.; Khanna, D. Atherosclerosis in Systemic Sclerosis: A Systematic Review and Meta-Analysis. Arthritis Care Res. 2011, 63, 2078–2090. [Google Scholar] [CrossRef]
- Manetti, M.; Guiducci, S.; Ibba-Manneschi, L.; Matucci-Cerinic, M. Mechanisms in the Loss of Capillaries in Systemic Sclerosis: Angiogenesis versus Vasculogenesis. J. Cell. Mol. Med. 2010, 14, 1241–1254. [Google Scholar] [CrossRef]
- Liu, X.; Gorzelanny, C.; Schneider, S.W. Platelets in Skin Autoimmune Diseases. Front. Immunol. 2019, 10, 1453. [Google Scholar] [CrossRef]
- Aloui, C.; Prigent, A.; Tariket, S.; Sut, C.; Fagan, J.; Cognasse, F.; Chakroun, T.; Garraud, O.; Laradi, S. Levels of Human Platelet-Derived Soluble CD40 Ligand Depend on Haplotypes of CD40LG-CD40-ITGA2. Sci. Rep. 2016, 6, 24715. [Google Scholar] [CrossRef]
- Liakouli, V.; Cipriani, P.; Marrelli, A.; Alvaro, S.; Ruscitti, P.; Giacomelli, R. Angiogenic Cytokines and Growth Factors in Systemic Sclerosis. Autoimmun. Rev. 2011, 10, 590–594. [Google Scholar] [CrossRef]
- Trojanowska, M. Cellular and Molecular Aspects of Vascular Dysfunction in Systemic Sclerosis. Nat. Rev. Rheumatol. 2010, 6, 453–460. [Google Scholar] [CrossRef]
- Zaman, M.; Oparil, S.; Calhoun, D. Drugs Targeting the Renin-Angiotensin-Aldosterone System. Nat. Rev. Drug Discov. 2002, 1, 621–636. [Google Scholar] [CrossRef]
- Kawaguchi, Y.; Takagi, K.; Hara, M.; Fukasawa, C.; Sugiura, T.; Nishimagi, E.; Harigai, M.; Kamatani, N. Angiotensin II in the lesional Skin of Systemic Sclerosis Patients Contributes to Tissue Fibrosis via Angiotensin II Type 1 Receptors. Arthritis Care Res. 2004, 50, 216–226. [Google Scholar] [CrossRef] [PubMed]
- Dadoniene, J.; Cypiene, A.; Ryliskyte, L.; Rugiene, R.; Ryliškiene, K.; Laucevičius, A. Skin Autofluorescence in Systemic Sclerosis Is Related to the Disease and Vascular Damage: A Cross-Sectional Analytic Study of Comparative Groups. Dis. Markers. 2015, 2015, 837470. [Google Scholar] [CrossRef] [PubMed]
- Davies, C.A.; Herrick, A.L.; Cordingley, L.; Freemont, A.J.; Jeziorska, M. Expression of Advanced Glycation end Products and Their Receptor in Skin from Patients with Systemic Sclerosis with and without Calcinosis. Rheumatology 2009, 48, 876–882. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Yao, Y.-C.; Gu, X.-Q.; Che, D.; Ma, C.-Q.; Dai, Z.; Li, C.; Zhou, T.; Cai, W.-B.; Yang, Z.-H.; et al. Plasminogen Kringle 5 Induces Endothelial Cell Apoptosis by Triggering a Voltage-dependent Anion Channel 1 (VDAC1) Positive Feedback Loop. J. Biol. Chem. 2014, 289, 32628–32638. [Google Scholar] [CrossRef] [PubMed]
- Okajima, K.; Abe, H.; Binder, B.R. Endothelial Cell Injury Induced by Plasmin in Vitro. J. Lab. Clin. Med. 1995, 126, 377–384. [Google Scholar]
- Mosesson, M.W. Fibrinogen and Fibrin Structure and Functions. J. Thromb. Haemost. 2005, 3, 1894–1904. [Google Scholar] [CrossRef]
- Watabe, A.; Ohta, M.; Matsuyama, N.; Mizuno, K.; El Borai, N.; Tanimoto, T.; Kawanishi, T.; Hayakawa, T. Characterization of Plasmin-Induced Platelet Aggregation. Res. Commun. Mol. Pathol. Pharmacol. 1997, 96, 341–352. [Google Scholar]
- Niewiarowski, S.; Senyi, A.F.; Gillies, P. Plasmin-Induced Platelet Aggregation and Platelet Release Reaction. Effects on Hemostasis. J. Clin. Investig. 1973, 52, 1647–1659. [Google Scholar] [CrossRef]
- Rundhaug, J.E. Matrix Metalloproteinases and Angiogenesis. J. Cell. Mol. Med. 2005, 9, 267–285. [Google Scholar] [CrossRef]
- Yan, Q.; Sage, E. Transforming Growth Factor-Beta1 Induces Apoptotic Cell Death in Cultured Retinal Endothelial Cells but not Pericytes: Association with Decreased Expression of p21waf1/cip1. J. Cell Biochem. 1998, 70, 70–83. [Google Scholar] [CrossRef]
- Gamal, R.M.; Gamal, W.M.; Abozaid, H.S.M.; Ghandour, A.M.; Mohamed, M.E.; Emad, Y.; Galeel, A.A. 201 Study of the Osteoprotegerin Receptor Activator of Nuclear Factor kB Ligand System Association with Inflammation and Atherosclerosis in Systemic Sclerosis. Rheumatology 2018, 57, key075-425. [Google Scholar] [CrossRef]
- Van Caam, A.; Vonk, M.; van den Hoogen, F.; van Lent, P.; van der Kraan, P. Unraveling SSc Pathophysiology; The Myofibroblast. Front. Immunol. 2018, 9, 2452. [Google Scholar] [CrossRef]
- Xing, X.; Li, A.; Tan, H.; Zhou, Y. IFN-γ+ IL-17+ Th17 Cells Regulate Fibrosis through Secreting IL-21 in Systemic Scleroderma. J. Cell Mol. Med. 2020, 24, 13600–13608. [Google Scholar] [CrossRef]
- Vernon, M.A.; Mylonas, K.J.; Hughes, J. Macrophages and Renal Fibrosis. Semin. Nephrol. 2010, 30, 302–317. [Google Scholar] [CrossRef]
- Cracowski, J.; Marpeau, C.; Carpentier, P.; Imbert, B.; Hunt, M.; Stanke-Labesque, F.; Bessard, G. Enhanced in Vivo Lipid Peroxidation in Scleroderma Spectrum Disorders. Arthritis Rheum. 2001, 44, 1143–1148. [Google Scholar] [CrossRef]
- Oga, T.; Matsuoka, T.; Yao, C.; Nonomura, K.; Kitaoka, S.; Sakata, D.; Kita, Y.; Tanizawa, K.; Taguchi, Y.; Chin, K.; et al. Prostaglandin F2alpha Receptor Signaling Facilitates Bleomycin-Induced Pulmonary Fibrosis Independently of Transforming Growth Factor-Beta. Nat. Med. 2009, 15, 1426–1430. [Google Scholar] [CrossRef]
- Vona, R.; Giovannetti, A.; Gambardella, L.; Malorni, W.; Pietraforte, D.; Straface, E. Oxidative Stress in the Pathogenesis of Systemic Scleroderma: An Overview. J. Cell. Mol. Med. 2018, 22, 3308–3314. [Google Scholar] [CrossRef]
- Mancini, O.K.; Acevedo, M.; Fazez, N.; Cuillerier, A.; Ruiz, A.F.; Huynh, D.N.; Burelle, Y.; Ferbeyre, G.; Baron, M.; Servant, M.J. Oxidative Stress-Induced Senescence Mediates Inflammatory and Fibrotic Phenotypes in Fibroblasts from Systemic Sclerosis Patients. Rheumatology 2022, 61, 1265–1275. [Google Scholar] [CrossRef] [PubMed]
- Thuan, D.T.B.; Zayed, H.; Eid, A.H.; Abou-Saleh, H.; Nasrallah, G.; Mangoni, A.A.; Pintus, G. A Potential Link between Oxidative Stress and Endothelial-to-Mesenchymal Transition in Systemic Sclerosis. Front. Immunol. 2018, 9, 1985. [Google Scholar] [CrossRef]
- Kawashita, E.; Ishihara, K.; Miyaji, H.; Tanishima, Y.; Kiriyama, A.; Matsuo, O.; Akiba, S. α2-Antiplasmin as a Potential Regulator of the Spatial Memory Process and Age-Related Cognitive Decline. Mol. Brain 2020, 13, 140. [Google Scholar] [CrossRef]
- Bobik, A.; Tkachuk, V. Metalloproteinases and Plasminogen Activators in Vessel Remodeling. Curr. Hypertens. Rep. 2003, 5, 466–472. [Google Scholar] [CrossRef]
- Waasdorp, M.; Duitman, J.; Spek, C.A. Plasmin Reduces Fibronectin Deposition by Mesangial Cells in a Protease-Activated Receptor-1 Independent Manner. Biochem. Biophys. Rep. 2017, 10, 152–156. [Google Scholar] [CrossRef]
- Horowitz, J.C.; Rogers, D.S.; Simon, R.H.; Sisson, T.H.; Thannickal, V.J. Plasminogen Activation–Induced Pericellular Fibronectin Proteolysis Promotes Fibroblast Apoptosis. Am. J. Respir. Cell Mol. Biol. 2008, 38, 78–87. [Google Scholar] [CrossRef]
- Bauman, K.A.; Wettlaufer, S.H.; Okunishi, K.; Vannella, K.M.; Stoolman, J.S.; Huang, S.K.; Courey, A.J.; White, E.S.; Hogaboam, C.M.; Simon, R.H.; et al. The Antifibrotic Effects of Plasminogen Activation Occur via Prostaglandin E2 Synthesis in Humans and Mice. J. Clin. Investig. 2010, 120, 1950–1960. [Google Scholar] [CrossRef]
- Kochtebane, N.; Choqueux, C.; Passefort, S.; Nataf, P.; Messika-Zeitoun, D.; Bartagi, A.; Michel, J.-B.; Anglés-Cano, E.; Jacob, M.-P. Plasmin Induces Apoptosis of Aortic Valvular Myofibroblasts. J. Pathol. 2009, 221, 37–48. [Google Scholar] [CrossRef]
- Asano, Y. Systemic Sclerosis. J. Dermatol. 2018, 45, 128–138. [Google Scholar] [CrossRef]
- Cerinic, M.M.; Valentini, G.; Sorano, G.; D’Angelo, S.; Cuomo, G.; Fenu, L.; Generini, S.; Cinotti, S.; Morfini, M.; Pignone, A.; et al. Blood Coagulation, Fibrinolysis, and Markers of Endothelial Dysfunction in Systemic Sclerosis. Semin. Arthritis Rheum. 2003, 32, 285–295. [Google Scholar] [CrossRef]
- Terrier, B.; Tamby, M.; Camoin, L.; Guilpain, P.; Bérezné, A.; Tamas, N.; Broussard, C.; Hotellier, F.; Humbert, M.; Simonneau, G.; et al. Antifibroblast Antibodies from Systemic Sclerosis Patients Bind to {Alpha}-Enolase and Are Associated with Interstitial Lung Disease. Ann. Rheum. Dis. 2010, 69, 428–433. [Google Scholar] [CrossRef]
- Ntelis, K.; Solomou, E.E.; Sakkas, L.; Liossis, S.-N.; Daoussis, D. The Role of Platelets in Autoimmunity, Vasculopathy, and Fibrosis: Implications for Systemic Sclerosis. Semin. Arthritis Rheum. 2017, 47, 409–417. [Google Scholar] [CrossRef]
- De Giorgio-Miller, A.; Bottoms, S.; Laurent, G.; Carmeliet, P.; Herrick, S. Fibrin-Induced Skin Fibrosis in Mice Deficient in Tissue Plasminogen Activator. Am. J. Pathol. 2005, 167, 721–732. [Google Scholar] [CrossRef]
- Luyendyk, J.P.; Schoenecker, J.G.; Flick, M.J. The Multifaceted Role of Fibrinogen in Tissue Injury and Inflammation. Blood 2019, 133, 511–520. [Google Scholar] [CrossRef]
- Schuliga, M. The Inflammatory Actions of Coagulant and Fibrinolytic Proteases in Disease. Mediat. Inflamm. 2015, 2015, 437695. [Google Scholar] [CrossRef]
- Schuliga, M.; Grainge, C.; Westall, G.; Knight, D. The Fibrogenic Actions of the Coagulant and Plasminogen Activation Systems in Pulmonary Fibrosis. Int. J. Biochem. Cell Biol. 2018, 97, 108–117. [Google Scholar] [CrossRef]
- Miniati, M.; Fiorillo, C.; Becatti, M.; Monti, S.; Bottai, M.; Marini, C.; Grifoni, E.; Formichi, B.; Bauleo, C.; Arcangeli, C.; et al. Fibrin Resistance to Lysis in Patients with Pulmonary Hypertension Other than Thromboembolic. Am. J. Respir. Crit. Care Med. 2010, 181, 992–996. [Google Scholar] [CrossRef]
- Davalos, D.; Akassoglou, K. Fibrinogen as a Key Regulator of Inflammation in Disease. Semin. Immunopathol. 2011, 34, 43–62. [Google Scholar] [CrossRef] [PubMed]
- Rubel, C.; Fernández, G.C.; Dran, G.; Bompadre, M.B.; Isturiz, M.A.; Palermo, M.S. Fibrinogen Promotes Neutrophil Activation and Delays Apoptosis. J. Immunol. 2001, 166, 2002–2010. [Google Scholar] [CrossRef] [PubMed]
- Sitrin, R.G.; Pan, P.M.; Srikanth, S.; Todd, R.F. Fibrinogen Activates NF-Kappa B Transcription Factors in Mononuclear Phagocytes. J. Immunol. 1998, 161, 1462–1470. [Google Scholar] [PubMed]
- Smiley, S.T.; King, J.A.; Hancock, W.W. Fibrinogen Stimulates Macrophage Chemokine Secretion Through Toll-Like Receptor 4. J. Immunol. 2001, 167, 2887–2894. [Google Scholar] [CrossRef]
- Suehiro, K.; Gailit, J.; Plow, E. Fibrinogen Is a Ligand for Integrin α5β1 on Endothelial Cells. J. Biol. Chem. 1997, 272, 5360–5366. [Google Scholar] [CrossRef]
- Yokoyama, K.; Zhang, X.; Medved, L.; Takada, Y. Specific Binding of Integrin α vs. β3 to the Fibrinogen γ and αE Chain C-Terminal Domains. Biochemistry 1999, 38, 5872–5877. [Google Scholar] [CrossRef]
- Millien, V.O.; Lu, W.; Shaw, J.; Yuan, X.; Mak, G.; Roberts, L.; Song, L.-Z.; Knight, J.M.; Creighton, C.J.; Luong, A.; et al. Cleavage of Fibrinogen by Proteinases Elicits Allergic Responses Through Toll-Like Receptor 4. Science 2013, 341, 792–796. [Google Scholar] [CrossRef]
- Yakovlev, S.; Mikhailenko, I.; Cao, C.; Zhang, L.; Strickland, D.K.; Medved, L. Identification of VLDLR as a Novel Endothelial Cell Receptor for Fibrin that Modulates Fibrin-Dependent Transendothelial Migration of Leukocytes. Blood 2012, 119, 637–644. [Google Scholar] [CrossRef]
- Sanchez-Pernaute, O.; Filkova, M.; Gabucio, A.; Klein, M.; Maciejewska-Rodrigues, H.; Ospelt, C.; Brentano, F.; Michel, B.A.; Gay, R.E.; Herrero-Beaumont, G.; et al. Citrullination Enhances the Pro-Inflammatory Response to Fibrin in Rheumatoid Arthritis Synovial Fibroblasts. Ann. Rheum. Dis. 2012, 72, 1400–1406. [Google Scholar] [CrossRef]
- Kattula, S.; Byrnes, J.R.; Wolberg, A.S. Fibrinogen and Fibrin in Hemostasis and Thrombosis. Arterioscler. Thromb. Vasc. Biol. 2017, 37, e13–e21. [Google Scholar] [CrossRef]
- Herwald, H.; Korte, W.; Allanore, Y.; Denton, C.P.; Cerinic, M.M.; Dickneite, G. Coagulation Factor XIII: A Multifunctional Transglutaminase with Clinical Potential in a Range of Conditions. Thromb. Haemost. 2015, 113, 686–697. [Google Scholar] [CrossRef]
- Wang, L.; Li, L.; Wang, H.; Liu, J. Study on the Influence of Oxidative Stress on the Fibrillization of Fibrinogen. Biochem. J. 2016, 473, 4373–4384. [Google Scholar] [CrossRef]
- Siudut, J.; Natorska, J.; Wypasek, E.; Wiewiórka, Ł.; Ostrowska-Kaim, E.; Wiśniowska-Śmiałek, S.; Plens, K.; Legutko, J.; Undas, A. Impaired Fibrinolysis in Patients with Isolated Aortic Stenosis is Associated with Enhanced Oxidative Stress. J. Clin. Med. 2020, 9, 2002. [Google Scholar] [CrossRef]
- Keane, F.; Nadvi, N.; Yao, T.; Gorrell, M. Neuropeptide Y, B-Type Natriuretic Peptide, Substance P and Peptide YY Are Novel Substrates of Fibroblast Activation Protein-α. FEBS J. 2011, 278, 1316–1332. [Google Scholar] [CrossRef]
- Soare, A.; Györfi, H.A.; Matei, A.E.; Dees, C.; Rauber, S.; Wohlfahrt, T.; Chen, C.W.; Ludolph, I.; Horch, R.E.; Bäuerle, T.; et al. Dipeptidyl-Peptidase-4 as a Marker of Activated Fibroblasts and a Potential Target for the Treatment of Fibrosis in Systemic Sclerosis. Arthritis Rheumatol. 2020, 72, 137–149. [Google Scholar] [CrossRef]
- Reed, G.; Houng, A.; Wang, D. Microvascular Thrombosis, Fibrinolysis, Ischemic Injury, and Death after Cerebral Thromboembolism Are Affected by Levels of Circulating α2-Antiplasmin. Arterioscler. Thromb. Vasc. Biol. 2014, 34, 2586–2593. [Google Scholar] [CrossRef]
- Lee, K.N.; Jackson, K.W.; Christiansen, V.J.; Dolence, E.K.; Mckee, P.A. Enhancement of Fibrinolysis by Inhibiting Enzymatic Cleavage of Precursor α2-Antiplasmin. J. Thromb. Haemost. 2011, 9, 987–996. [Google Scholar] [CrossRef]
- Szabo, I.; Muntean, L.; Crisan, T.; Rednic, V.; Sirbe, C.; Rednic, S. Novel Concepts in Systemic Sclerosis Pathogenesis: Role for miRNAs. Biomedicines 2021, 9, 1471. [Google Scholar] [CrossRef]
- Ciechomska, M.; O’Reilly, S.; Suwara, M.; Bogunia-Kubik, K.; van Laar, J. MiR-29a Reduces TIMP-1 Production by Dermal Fibroblasts via Targeting TGF-β Activated Kinase 1 Binding Protein 1, Implications for Systemic Sclerosis. PLoS ONE 2014, 30, e115596. [Google Scholar] [CrossRef]
- Kanno, Y.; Shu, E.; Niwa, H.; Seishima, M.; Ozaki, K.-I. MicroRNA-30c Attenuates Fibrosis Progression and Vascular Dysfunction in Systemic Sclerosis Model Mice. Mol. Biol. Rep. 2021, 48, 3431–3437. [Google Scholar] [CrossRef]
- Hirman, A.R.; Du, L.; Cheng, S.; Zheng, H.; Duo, L.; Zhai, Q.; Xu, J. MiR-133a-3p Inhibits Scar Formation in Scalded Mice and Suppresses the Proliferation and Migration of Scar Derived-Fibroblasts by Targeting Connective Tissue Growth Factor. Exp. Anim. 2021, 70, 322–332. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Wang, H.; Wang, B.; Yuan, Y.; Klein, J.D.; Wang, X.H. Exogenous miR-26a Suppresses Muscle Wasting and Renal Fibrosis in Obstructive Kidney Disease. FASEB J. 2019, 33, 13590–13601. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Ji, Q.; Zhu, H.; Ren, Y.; Fan, Z.; Tian, N. miR-30a Attenuates Cardiac Fibrosis in Rats with Myocardial Infarction by Inhibiting CTGF. Exp. Ther. Med. 2018, 15, 4318–4324. [Google Scholar] [CrossRef] [PubMed]
- Sheffield, W.P.; Eltringham-Smith, L.J.; Gataiance, S.; Bhakta, V. Addition of a Sequence from α2-Antiplasmin Transforms Human Serum Albumin into a Blood Clot Component that Speeds Clot Lysis. BMC Biotechnol. 2009, 9, 15. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.N.; Jackson, K.W.; McKee, P.A. Effect of a Synthetic Carboxy-Terminal Peptide of α2-Antiplasmin on Urokinase-Induced Fibrinolysis. Thromb. Res. 2002, 105, 263–270. [Google Scholar] [CrossRef]
- Shi, G.Y.; Wu, H.L. Isolation and Characterization of Microplasminogen. A Low Molecular Weight Form of Plasminogen. J. Biol. Chem. 1988, 263, 17071–17075. [Google Scholar] [CrossRef]
- Pakola, S.; Cahillane, G.; Stassen, J.; Lijnen, H.; Verhamme, P. Neutralization of α(2)-Antiplasmin by Microplasmin: A Randomized, Double-Blind, Placebo-Controlled, Ascending-Dose Study in Healthy Male Volunteers. Clin. Ther. 2009, 31, 1688–1706. [Google Scholar] [CrossRef]
- Nagai, N.; De Mol, M.; Van Hoef, B.; Verstreken, M.; Collen, D. Depletion of Circulating α(2)-Antiplasmin by Intravenous Plasmin or Immunoneutralization Reduces Focal Cerebral Ischemic Injury in the Absence of Arterial Recanalization. Blood 2001, 97, 3086–3092. [Google Scholar] [CrossRef]
- Suzuki, Y.; Chen, F.; Ni, Y.; Marchal, G.; Collen, D.; Nagai, N. Microplasmin Reduces Ischemic Brain Damage and Improves Neurological Function in a Rat Stroke Model Monitored with MRI. Stroke 2004, 35, 2402–2406. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).