Cutoff Point of Mini-Balance Evaluation Systems Test Scores for Elderly Estimated by Center of Pressure Measurements by Linear Regression and Decision Tree Classification
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects Information and Survey Distributions
2.2. CoP Recording and CoP Feature Extraction
2.3. Linear Regression
2.4. Binary Classification Performance Evaluation by Regression and Decision Tree
2.5. Statistics
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BESTest | Balance Evaluation Systems Test |
| Mini-BESTest | Mini-Balance Evaluation Systems Test |
| CoP | center of pressure |
| DT | decision tree |
| BMI | body mass index |
| IPAQ | The International Physical Activity Questionnaire |
| F12M | fall within 12 months |
| Short FES-I | Short Falls Efficacy Scale International |
| RMSD | root–mean–square deviation |
| ApEn | approximate entropy |
| SampEn | sample entropy |
| PSD | power of spectral density |
| MF | median frequency |
| STD | standard deviation |
| TP | true positive |
| FP | false positive |
| TN | true negative |
| FN | false negative |
| ROC | receiver operating characteristic |
| AUC | area under the curve |
References
- BESTtest. Available online: http://www.bestest.us/ (accessed on 15 October 2020).
- Horak, F.B.; Wrisley, D.M.; Frank, J. The balance evaluation systems test (BESTest) to differentiate balance deficits. Phys. Ther. 2009, 89, 484–498. [Google Scholar] [CrossRef] [PubMed]
- Ruhe, A.; Fejer, R.; Walker, B. Center of pressure excursion as a measure of balance performance in patients with non-specific low back pain compared to healthy controls: A systematic review of the literature. Eur. Spine J. 2011, 20, 358–368. [Google Scholar] [CrossRef] [PubMed]
- Quijoux, F.; Vienne-Jumeau, A.; Bertin-Hugault, F.; Zawieja, P.; Lefevre, M.; Vidal, P.-P.; Ricard, D. Center of pressure displacement characteristics differentiate fall risk in older people: A systematic review with meta-analysis. Ageing Res. Rev. 2020, 62, 101117. [Google Scholar] [CrossRef] [PubMed]
- da Conceição, N.R.; de Sousa, P.N.; Pereira, M.P.; Gobbi, L.T.B.; Vitório, R. Utility of center of pressure measures during obstacle crossing in prediction of fall risk in people with Parkinson’s disease. Hum. Mov. Sci. 2019, 66, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Estévez-Pedraza, Á.G.; Parra-Rodríguez, L.; Martínez-Méndez, R.; Portillo-Rodríguez, O.; Ronzón-Hernández, Z. A novel model to quantify balance alterations in older adults based on the center of pressure (CoP) measurements with a cross-sectional study. PLoS ONE 2021, 16, e0256129. [Google Scholar] [CrossRef]
- Romaniszyn, P.; Kawa, J.; Stępien, P.; Nawrat-Szołtysik, A. Video-based time assessment in 360 degrees turn Berg balance test. Comput. Med. Imaging Graph. 2020, 80, 101689. [Google Scholar] [CrossRef]
- Aldenhoven, C.M.; Reimer, L.M.; Jonas, S. mBalance: Detect Postural Imbalance with Mobile Devices. In dHealth 2022; IOS Press: Amsterdam, The Netherlands, 2022; pp. 30–38. [Google Scholar]
- Ren, P.; Huang, S.; Feng, Y.; Chen, J.; Wang, Q.; Guo, Y.; Yuan, Q.; Yao, D.; Ma, D. Assessment of balance control subsystems by artificial intelligence. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 658–668. [Google Scholar] [CrossRef]
- Sauerbrei, W.; Meier-Hirmer, C.; Benner, A.; Royston, P. Multivariable regression model building by using fractional polynomials: Description of SAS, STATA and R programs. Comput. Stat. Data Anal. 2006, 50, 3464–3485. [Google Scholar] [CrossRef]
- Montgomery, D.C.; Peck, E.A.; Vining, G.G. Introduction to Linear Regression Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2021. [Google Scholar]
- Ayodele, T.O. Types of machine learning algorithms. New Adv. Mach. Learn. 2010, 3, 19–48. [Google Scholar]
- Ramalingam, V.; Dandapath, A.; Raja, M.K. Heart disease prediction using machine learning techniques: A survey. Int. J. Eng. Technol. 2018, 7, 684–687. [Google Scholar] [CrossRef]
- Liao, F.-Y.; Wu, C.-C.; Wei, Y.-C.; Chou, L.-W.; Chang, K.-M. Analysis of center of pressure signals by using decision tree and empirical mode decomposition to predict falls among older adults. J. Healthc. Eng. 2021, 6252445. [Google Scholar] [CrossRef]
- Steffen, T.; Seney, M. Test-retest reliability and minimal detectable change on balance and ambulation tests, the 36-item short-form health survey, and the unified Parkinson disease rating scale in people with parkinsonism. Phys. Ther. 2008, 88, 733–746. [Google Scholar] [CrossRef]
- Santos, D.A.; Duarte, M. A public data set of human balance evaluations. PeerJ 2016, 4, e2648. [Google Scholar] [CrossRef]
- Anson, E.; Thompson, E.; Ma, L.; Jeka, J. Reliability and fall risk detection for the BESTest and Mini-BESTest in older adults. J. Geriatr. Phys. Ther. 2019, 42, 81. [Google Scholar] [CrossRef]
- Duchesne, E.; Hébert, L.J.; Mathieu, J.; Côté, I.; Roussel, M.P.; Gagnon, C. Validity of the Mini-BESTest in adults with myotonic dystrophy type 1. Muscle Nerve 2020, 62, 95–102. [Google Scholar] [CrossRef]
- Lopes, L.K.R.; Scianni, A.A.; Lima, L.O.; de Carvalho Lana, R.; Rodrigues-De-Paula, F. The Mini-BESTest is an independent predictor of falls in Parkinson Disease. Braz. J. Phys. Ther. 2020, 24, 433–440. [Google Scholar] [CrossRef]
- Beauchamp, M.K.; Niebuhr, R.; Roche, P.; Kirkwood, R.; Sibley, K.M. A prospective study to establish the minimal clinically important difference of the Mini-BESTest in individuals with stroke. Clin. Rehabil. 2021, 35, 1207–1215. [Google Scholar] [CrossRef]
- Magnani, P.E.; Genovez, M.B.; Porto, J.M.; Zanellato, N.F.G.; Alvarenga, I.C.; Freire, R.C., Jr.; de Abreu, D.C.C. Use of the BESTest and the Mini-BESTest for fall risk prediction in community-dwelling older adults between 60 and 102 years of age. J. Geriatr. Phys. Ther. 2020, 43, 179–184. [Google Scholar] [CrossRef]
- Glowinski, S.; Krzyzynski, T.; Bryndal, A.; Maciejewski, I. A Kinematic Model of a Humanoid Lower Limb Exoskeleton with Hydraulic Actuators. Sensors 2020, 20, 6116. [Google Scholar] [CrossRef]
- Abou, L.; Peters, J.; Wong, E.; Akers, R.; Dossou, M.S.; Sosnoff, J.J.; Rice, L.A. Gait and Balance Assessments Using Smartphone Applications in Parkinson’s Disease: A Systematic Review. J. Med. Syst. 2021, 45, 87. [Google Scholar] [CrossRef]
- Ferreira, R.N.; Ribeiro, N.F.; Santos, C.P. Fall Risk Assessment Using Wearable Sensors: A Narrative Review. Sensors 2022, 22, 984. [Google Scholar] [CrossRef] [PubMed]


| Subject Numbers | Male 15/Female 60 |
|---|---|
| Age (year) | 71.3 (6.5) [max = 85.8, min = 60.5] |
| Height (cm) | 157.3 (8.2) [max = 178.5, min = 140] |
| Weight (kg) | 63.3 (8.3) [max = 75.9, min = 44.2] |
| Mini-BESTest scores | 18.2 (4.0) [max = 26, min = 4] |
| Symbol | Corresponding Meaning |
|---|---|
| Y | Original Mini-BESTest scores |
| X1 | RMSD. CoPx |
| X2 | RMSD. CoPy |
| X3 | ApEn. CoPx |
| X4 | ApEn. CoPy |
| X5 | SampEn. CoPx |
| X6 | SampEn. CoPy |
| X7 | PSD. CoPx |
| X8 | PSD. CoPy |
| X9 | MF. CoPx |
| X10 | MF. CoPy |
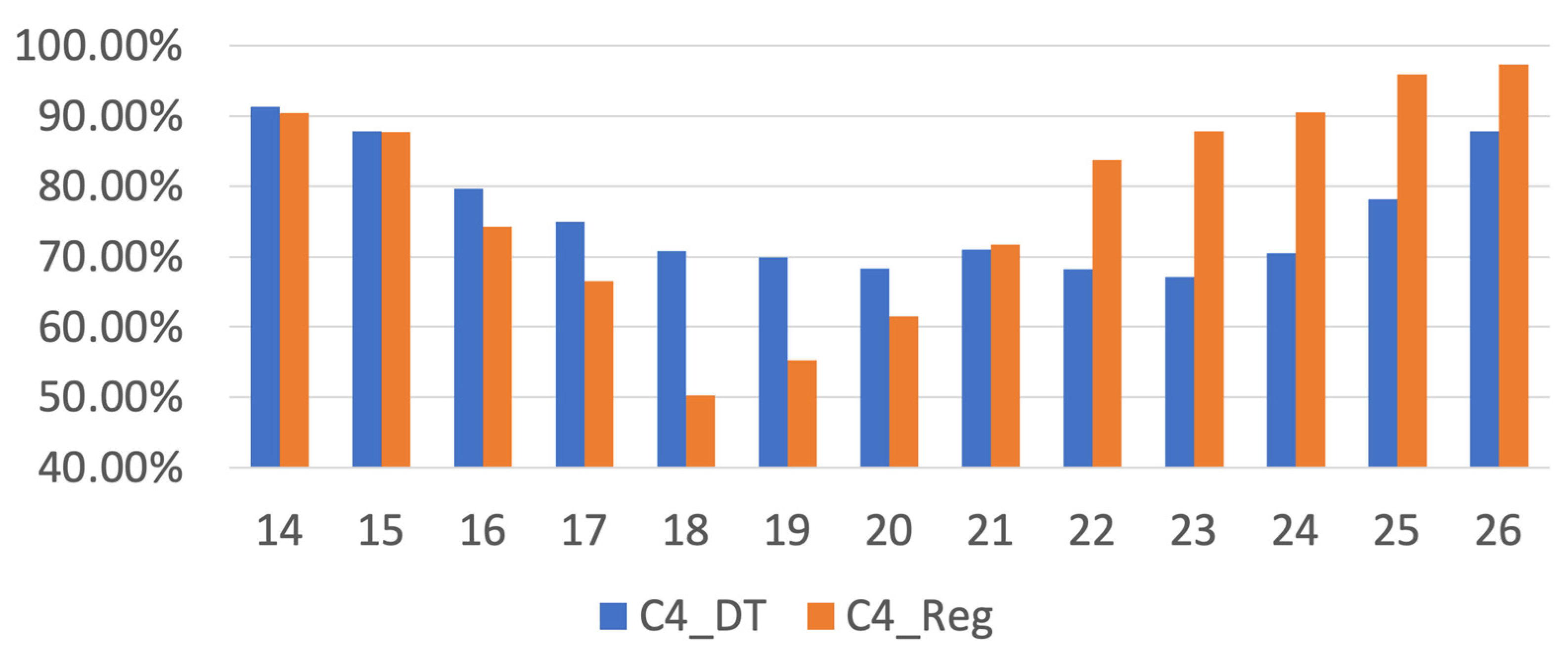
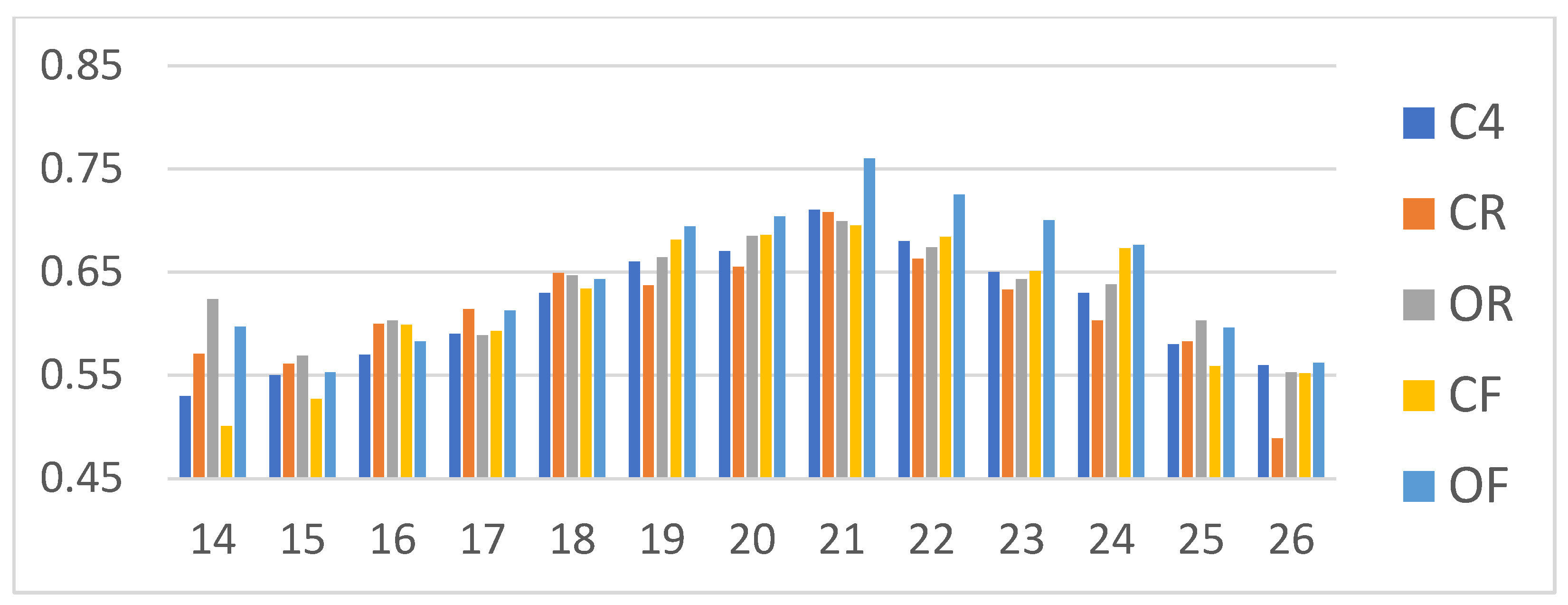
| Mini-BESTest Cutoff Scores | CR_DT | OR_DT | CF_DT | OF_DT | CR_Reg | OR_Reg | CF_Reg | OF_Reg |
|---|---|---|---|---|---|---|---|---|
| 14 | 89.74% | 91.84% | 93.26% | 93.80% | 88.94% | 88.16% | 90.94% | 91.78% |
| 15 | 87.24% | 86.12% | 90.53% | 88.13% | 86.28% | 85.53% | 88.22% | 89.04% |
| 16 | 80.66% | 81.07% | 81.37% | 79.95% | 75.22% | 71.93% | 74.62% | 75.34% |
| 17 | 75.46% | 74.08% | 77.95% | 76.77% | 64.60% | 65.79% | 66.47% | 67.12% |
| 18 | 72.50% | 71.89% | 72.47% | 71.98% | 51.77% | 49.12% | 51.06% | 51.60% |
| 19 | 67.91% | 71.12% | 72.84% | 73.28% | 56.64% | 52.19% | 54.38% | 55.25% |
| 20 | 66.84% | 70.26% | 70.74% | 72.08% | 61.06% | 63.16% | 61.63% | 62.10% |
| 21 | 70.82% | 69.90% | 69.79% | 76.15% | 72.12% | 72.37% | 71.60% | 71.23% |
| 22 | 66.38% | 67.70% | 68.63% | 72.50% | 84.07% | 84.21% | 83.69% | 83.56% |
| 23 | 66.33% | 66.63% | 66.68% | 71.61% | 88.05% | 88.16% | 87.76% | 87.67% |
| 24 | 69.64% | 71.17% | 73.21% | 74.17% | 90.71% | 90.79% | 90.48% | 90.41% |
| 25 | 76.84% | 78.37% | 75.95% | 78.80% | 96.02% | 96.05% | 95.92% | 95.89% |
| 26 | 86.33% | 87.81% | 87.16% | 88.49% | 97.35% | 97.37% | 97.28% | 97.26% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liao, W.-Y.; Chu, Y.-H.; Liu, F.-Y.; Chang, K.-M.; Chou, L.-W. Cutoff Point of Mini-Balance Evaluation Systems Test Scores for Elderly Estimated by Center of Pressure Measurements by Linear Regression and Decision Tree Classification. Life 2022, 12, 2133. https://doi.org/10.3390/life12122133
Liao W-Y, Chu Y-H, Liu F-Y, Chang K-M, Chou L-W. Cutoff Point of Mini-Balance Evaluation Systems Test Scores for Elderly Estimated by Center of Pressure Measurements by Linear Regression and Decision Tree Classification. Life. 2022; 12(12):2133. https://doi.org/10.3390/life12122133
Chicago/Turabian StyleLiao, Wen-Yen, Yu-Hsiu Chu, Fan-Yu Liu, Kang-Ming Chang, and Li-Wei Chou. 2022. "Cutoff Point of Mini-Balance Evaluation Systems Test Scores for Elderly Estimated by Center of Pressure Measurements by Linear Regression and Decision Tree Classification" Life 12, no. 12: 2133. https://doi.org/10.3390/life12122133
APA StyleLiao, W.-Y., Chu, Y.-H., Liu, F.-Y., Chang, K.-M., & Chou, L.-W. (2022). Cutoff Point of Mini-Balance Evaluation Systems Test Scores for Elderly Estimated by Center of Pressure Measurements by Linear Regression and Decision Tree Classification. Life, 12(12), 2133. https://doi.org/10.3390/life12122133







