Total Facial Autologous Fat Grafting for Treating Skin Manifestations in Scleroderma
Abstract
1. Introduction
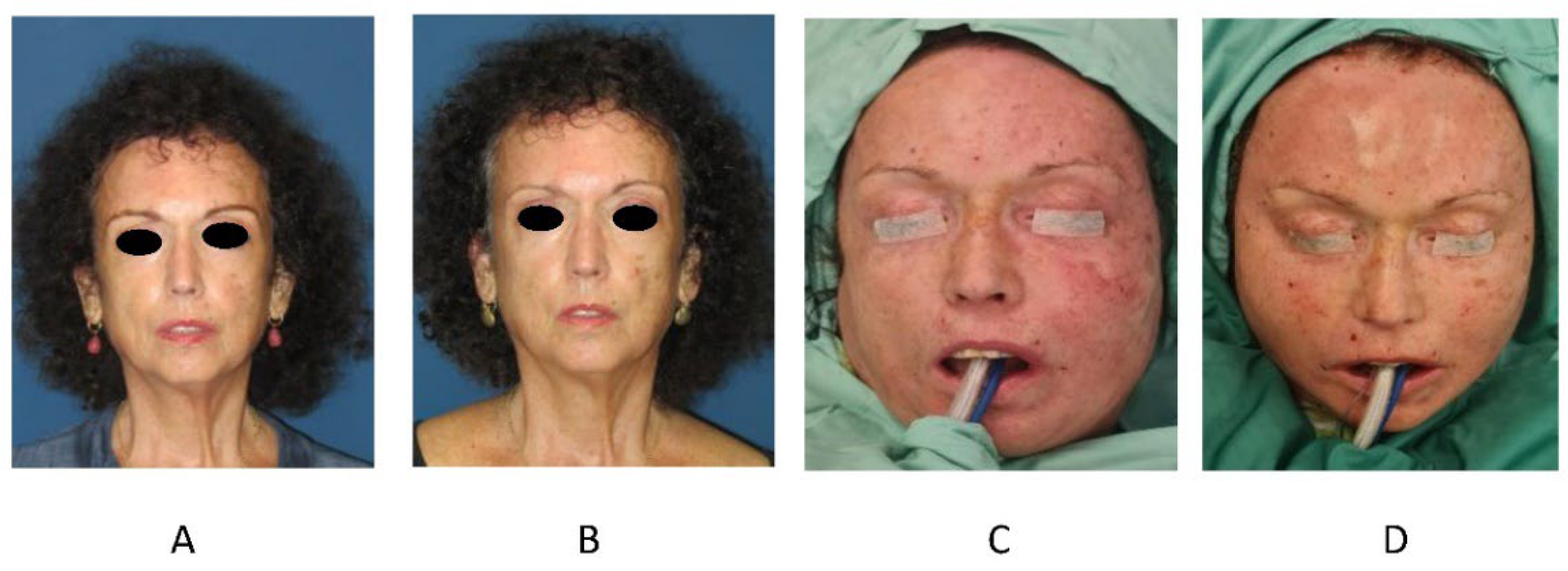
2. Materials and Methods
2.1. Ethics
2.2. Surgical Technique
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alhajeri, H.; Hudson, M.; Fritzler, M.; Pope, J.; Tatibouet, S.; Markland, J.; Robinson, D.; Jones, N.; Khalidi, N.; Docherty, P.; et al. 2013 American College of Rheumatology/European League against rheumatism classification criteria for systemic sclerosis outperform the 1980 criteria: Data from the Canadian Scleroderma Research Group. Arthritis Care Res. 2015, 67, 582–587. [Google Scholar] [CrossRef] [PubMed]
- Strong, A.; Rubin, J.; Kozlow, J.; Cederna, P. Fat Grafting for the Treatment of Scleroderma. Plast Reconstr. Surg. 2019, 144, 1498–1507. [Google Scholar] [CrossRef] [PubMed]
- Denton, C.; Khanna, D. Systemic sclerosis. Lancet 2017, 390, 1685–1699. [Google Scholar] [CrossRef] [PubMed]
- Peterson, L.; Nelson, A.; Su, W.; Mason, T.; O’Fallon, W.; Gabriel, S. The epidemiology of morphea (Localized scleroderma) in Olmsted County 1960. J. Rheumatol. 1997, 24, 73–80. [Google Scholar]
- Zhong, L.; Pope, M.; Shen, Y.; Hernandez, J.; Wu, L. Prevalence and incidence of systemic sclerosis: A systematic review and meta-analysis. Int. J. Rheum Dis. 2019, 22, 2096–2107. [Google Scholar] [CrossRef]
- Furst, D.; Fernandes, A.; Iorga, S.; Greth, W.; Bancroft, T. Epidemiology of systemic sclerosis in a large US managed care population. J. Rheumatol. 2012, 39, 784–786. [Google Scholar] [CrossRef]
- Knarborg, M.; Hyldgaard, C.; Bendstrup, E.; Davidsen, J.R.; Løkke, A.; Shaker, S.B.; Hilberg, O. Incidence, prevalence and regional distribution of systemic sclerosis and related interstitial lung disease: A nationwide retrospective cohort study. Chron. Respir. Dis. 2022, 19, 14799731221125559. [Google Scholar] [CrossRef]
- Knobler, R.; Moinzadeh, P.; Hunzelmann, N.; Kreuter, A.; Cozzio, A.; Mouthon, L.; Cutolo, M.; Rongioletti, F.; Denton, C.P.; Rudnicka, L.; et al. European Dermatology Forum S1-guideline on the diagnosis and treatment of sclerosing diseases of the skin, Part 1: Localized scleroderma, systemic sclerosis and overlap syndromes. J. Eur. Acad Dermatol. Venereol. 2017, 31, 1401–1424. [Google Scholar] [CrossRef]
- Panchbhai, A.; Pawar, S.; Barad, A.; Kazi, Z. Review of orofacial considerations of systemic sclerosis or scleroderma with report of analysis of 3 cases. Indian J. Dent. 2016, 7, 134–139. [Google Scholar] [CrossRef]
- Magalon, G.; Daumas, A.; Sautereau, N.; Magalon, J.; Sabatier, F.; Granel, B. Regenerative approach to scleroderma with fat grafting. Clin. Plast. Surg. 2015, 42, 353–364. [Google Scholar] [CrossRef]
- Crincoli, V.; Fatone, L.; Fanelli, M.; Rotolo, R.P.; Chialà, A.; Favia, G.; Lapadula, G. Orofacial manifestations and temporomandibular disorders of systemic scleroderma: An observational study. Int. J. Mol. Sci. 2016, 17, 1189. [Google Scholar] [CrossRef]
- Gheisari, M.; Ahmadzadeh, A.; Nobari, N.; Iranmanesh, B.; Mozafari, N. Autologous Fat Grafting in the Treatment of Facial Scleroderma. Dermatol. Res. Pract. 2018, 2018, 6568016. [Google Scholar] [CrossRef]
- Gonzalez, C.; Pamatmat, J.; Hutto, J.; Goff, H. Review of the current medical and surgical treatment options for microstomia in patients with scleroderma. Dermatol. Surg. 2021, 47, 780–784. [Google Scholar] [CrossRef]
- Tewari, A.; Garibaldinos, T.; Lai-Cheong, J.; Groves, R.; Sarkany, R.; Branislav Novakovic, L. Successful treatment of microstomia with UVA1 phototherapy in systemic sclerosis. Photodermatol. Photoimmunol. Photomed. 2011, 27, 113–114. [Google Scholar] [CrossRef]
- Rosholm Comstedt, L.; Svensson, Å.; Hesselstrand, R.; Lehti, L.; Troilius Rubin, A. Effects of intense pulsed light in microstomia in patients with systemic sclerosis: A pilot study. J. Cosmet. Laser Ther. 2017, 19, 143–148. [Google Scholar] [CrossRef]
- Kumar, M.; Kumar, M.; Kumar, S.; Kumar, K. A neoteric multidrug combination: Novel approach to limited cutaneous systemic scleroderma involving the face. BMJ Case Rep. 2016, 2016, bcr2015212. [Google Scholar] [CrossRef]
- Abbas, L.; Coias, J.; Jacobe, H.; Nijhawan, R. Hyaluronidase injections for treatment of symptomatic pansclerotic morphea-induced microstomia. JAAD Case Rep. 2019, 5, 871–873. [Google Scholar] [CrossRef]
- Melvin, O.; Hunt, K.; Jacobson, E. Hyaluronidase Treatment of Scleroderma-Induced Microstomia. JAMA Dermatol. 2019, 155, 857–859. [Google Scholar] [CrossRef]
- Barin, E.; Cinal, H.; Cakmak, M.; Tan, O. Treatment of Linear Scleroderma (en Coup de Sabre) With Dermal Fat Grafting. J. Cutan. Med. Surg. 2016, 20, 269–271. [Google Scholar] [CrossRef]
- Zanelato, T.; Marquesini, G.; Colpas, P.; Magalhães, R.; Moraes, A. Implantation of autologous fat globules in localized scleroderma and idiopathic lipoatrophy-report of five patients. An. Bras. Dermatol. 2013, 88, 120–123. [Google Scholar] [CrossRef]
- Skorochod, R.; Nesher, G.; Gronovich, Y. Management Options for Linear Scleroderma (“En Coup de Sabre”). Dermatol. Surg. 2022, 48, 1038–1045. [Google Scholar] [CrossRef] [PubMed]
- Zuk, P.; Zhu, M.; Ashjian, P.; De Ugarte, D.A.; Huang, J.I.; Mizuno, H.; Alfonso, Z.C.; Fraser, J.K.; Benhaim, P.; Hedrick, M.H. Human adipose tissue is a source of multipotent stem cells. Mol. Biol. Cell. 2002, 13, 4279–4295. [Google Scholar] [CrossRef] [PubMed]
- Roh, M.; Jung, J.; Chung, K. Autologous fat transplantation for depressed linear scleroderma-induced facial atrophic scars. Dermatol. Surg. 2008, 34, 1659–1665. [Google Scholar] [PubMed]
- Karaaltin, M.; Akpinar, A.; Baghaki, S.; Akpinar, F. Treatment of “en coup de sabre” deformity with adipose-derived regenerative cell-enriched fat graft. J. Craniofac. Surg. 2012, 23, e103–e105. [Google Scholar] [CrossRef]
- Djouad, F.; Bouffi, C.; Ghannam, S.; Noël, D.; Jorgensen, C. Mesenchymal stem cells: Innovative therapeutic tools for rheumatic diseases. Nat. Rev. Rheumatol. 2009, 5, 392–399. [Google Scholar] [CrossRef]
- Bellini, E.; Grieco, M.; Raposio, E. The science behind autologous fat grafting. Ann. Med. Surg. 2017, 24, 65–73. [Google Scholar] [CrossRef]
- Del Papa, N.; Caviggioli, F.; Sambataro, D.; Zaccara, E.; Vinci, V.; Di Luca, G.; Parafioriti, A.; Armiraglio, E.; Maglione, W.; Polosa, R.; et al. Autologous fat grafting in the treatment of fibrotic perioral changes in patients with systemic sclerosis. Cell Transplant. 2015, 24, 63–72. [Google Scholar] [CrossRef]
- Chen, W.; Xia, Z.K.; Zhang, M.H.; Ding, G.C.; Zhang, X.Y.; Wang, Z.X.; Yang, R.Y. Adipose tissue-derived stem cells ameliorates dermal fibrosis in a mouse model of scleroderma. Asian Pac. J. Trop. Med. 2017, 10, 52–56. [Google Scholar] [CrossRef]
- Wang, J.; Cai, J.; Zhang, Q.; Wen, J.; Liao, Y.; Lu, F. Fat transplantation induces dermal adipose regeneration and reverses skin fibrosis through dedifferentiation and redifferentiation of adipocytes. Stem Cell Res. Ther. 2022, 13, 499. [Google Scholar] [CrossRef]
- Merfeld-Clauss, S.; Gollahalli, N.; March, K.; Traktuev, D. Adipose tissue progenitor cells directly interact with endothelial cells to induce vascular network formation. Tissue Eng. Part A 2010, 16, 2953–2966. [Google Scholar] [CrossRef]
- Onesti, M.; Fioramonti, P.; Carella, S.; Fino, P.; Marchese, C.; Scuderi, N. Improvement of mouth functional disability in systemic sclerosis patients over one year in a trial of fat transplantation versus adipose-derived stromal cells. Stem Cells Int. 2016, 2016, 2416192. [Google Scholar] [CrossRef]
- Sautereau, N.; Daumas, A.; Truillet, R.; Jouve, E.; Magalon, J.; Veran, J.; Casanova, D.; Frances, Y.; Magalon, G.; Granel, B. Efficacy of Autologous Microfat Graft on Facial Handicap in Systemic Sclerosis Patients. Plast. Reconstr. Surg. Glob. Open. 2016, 4, e660. [Google Scholar] [CrossRef]
- Xue, E.; Narvaez, L.; Chu, C.; Hanson, S. Fat Processing Techniques. Semin. Plast. Surg. 2020, 34, 11–16. [Google Scholar] [CrossRef]
- Bootun, R. Effects of immunosuppressive therapy on wound healing. Int. Wound J. 2013, 10, 98–104. [Google Scholar] [CrossRef]
- Medellín-Luna, M.F.; Castañeda-Delgado, J.E.; Fernández-Ruiz, J.C.; Ochoa-González, F.L.; Troncoso-Vázquez, L.; García-Cruz, S.; Zapata-Zúñiga, M.; Serrano, C.J.; Portales-Pérez, D.; Enciso-Moreno, J.A.; et al. Methotrexate reduces keratinocyte proliferation, migration and induces apoptosis in HaCaT keratinocytes in vitro and reduces wound closure in Skh1 mice in vivo. J. Tissue Viability 2021, 30, 51–58. [Google Scholar] [CrossRef]
- Wang, A.S.; Armstrong, E.J.; Armstrong, A.W. Corticosteroids and wound healing: Clinical considerations in the perioperative period. Am. J. Surg. 2013, 206, 410–417. [Google Scholar] [CrossRef]
- Wang, H.C.; Yu, N.; Wang, X.; Dong, R.; Long, X.; Feng, X.; Li, J.; Wu, W.T.L. Cerebral embolism as a result of facial filler injections: A literature review. Aesthet. Surg. J. 2022, 42, NP162–NP175. [Google Scholar] [CrossRef]
- Miao, J.; Sun, W.; Zhu, Z.; Yang, Z.; Xu, Y. A massive right hemisphere infarction after autologous fat grafting for facial filling. J. Craniofac. Surg. 2021, 32, e215–e217. [Google Scholar] [CrossRef]

| Case | Sex | No. of Procedures | Age at First Procedure (Years) | SSc Subtype | Years since Diagnosis | BMI (kg/m2) |
|---|---|---|---|---|---|---|
| 1 | F | 4 | 48 | Diffuse | 13 | 21.8 |
| 2 | F | 2 | 64 | Diffuse | 19 | 25.2 |
| 3 | F | 4 | 60 | Diffuse | 18 | 22.1 |
| 4 | F | 2 | 53 | Diffuse | 22 | 25.3 |
| 5 | F | 3 | 65 | Diffuse | 13 | 22.6 |
| 6 | F | 1 | 47 | Limited | 10 | 20 |
| 7 | F | 1 | 32 | Diffuse | 8 | 18.2 |
| 8 | F | 2 | 41 | Systemic | 29 | 20.4 |
| 9 | F | 2 | 51 | Systemic | 19 | 23.1 |
| 10 | M | 1 | 72 | Systemic | 8 | 24.2 |
| 11 | F | 1 | 61 | Systemic | 15 | 21.5 |
| 12 | F | 1 | 27 | Diffuse | 10 | 27.9 |
| 13 | F | 2 | 43 | Systemic | 1.5 | 21 |
| 14 | M | 1 | 64 | Systemic | 22 | 23.4 |
| 15 | F | 3 | 65 | Systemic | 7 | 29 |
| 16 | F | 1 | 38 | Systemic | 15 | 23.9 |
| 17 | M | 1 | 35 | Diffuse | 2 | 27.5 |
| Case | Procedure | Facial Area Treated | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Forehead (n = 16) | Temporal Region (n = 17) | Zygoma/Cheek (n = 23) | Upper Lip (n = 29) | Lower Lip (n = 29) | Chin and Mandibular Areas (n = 16) | Nose (n = 12) | Total Volume/Procedure, mL (n = 32) | Donor Site | ||
| 1 | 1 | 10 | 10 | 20 | Abdomen | |||||
| 2 | 10 | 7 | 8 | 10 | 3 | 38 | Flank | |||
| 3 | 20 | 20 | 10 | 10 | 25 | 5 | 90 | Hips | ||
| 4 | 20 | 20 | 10 | 10 | 20 | 80 | Hips | |||
| 2 | 1 | 2 | 10 | 30 | 5 | 5 | 52 | Abdomen | ||
| 2 | 5 | 10 | 37 | 15 | 10 | 10 | 87 | Abdomen | ||
| 3 | 1 | 10 | 15 | 13 | 12 | 5 | 5 | 60 | Hips | |
| 2 | 12 | 15 | 3 | 30 | Abdomen, hips | |||||
| 3 | 10 | 15 | 15 | 15 | 55 | Flank, abdomen | ||||
| 4 | 15 | 20 | 20 | 20 | 10 | 5 | 95 | Flank, knees | ||
| 4 | 1 | 25 | 25 | 30 | 15 | 15 | 20 | 10 | 140 | Abdomen |
| 2 | 20 | 20 | 20 | 10 | 10 | 10 | 10 | 100 | Flank | |
| 5 | 1 | 10 | 13 | 14 | 37 | Flank | ||||
| 2 | 25 | 25 | Flank | |||||||
| 3 | 10 | 13 | 23 | Hips | ||||||
| 6 | 1 | 15 | 8 | 23 | Flank | |||||
| 7 | 1 | 24 | 6 | 15 | 40 | Abdomen | ||||
| 8 | 1 | 20 | 10 | 20 | 4 | 4 | 2 | 60 | Flank, abdomen | |
| 2 | 20 | 50 | 14 | 10 | 20 | 114 | Flank | |||
| 9 | 1 | 20 | 20 | 44 | 10 | 12 | 6 | 112 | Flank | |
| 2 | 20 | 10 | 42 | 18 | 15 | 6 | 16 | 127 | Abdomen | |
| 10 | 1 | 10 | 10 | 6 | 5 | 31 | Abdomen | |||
| 11 | 1 | 20 | 25 | 30 | 10 | 5 | 110 | Abdomen | ||
| 12 | 1 | 50 | Abdomen | |||||||
| 13 | 1 | 20 | 10 | 15 | 15 | 60 | Flank | |||
| 2 | 5 | 10 | 10 | 5 | 5 | 15 | 2 | 52 | Flank, abdomen | |
| 14 | 1 | 40 | 40 | 20 | 20 | 120 | Flank, abdomen | |||
| 15 | 1 | 20 | 20 | 30 | 110 | Flank, abdomen | ||||
| 2 | 10 | 46 | 54 | 10 | 10 | 22 | 152 | Flank, abdomen | ||
| 3 | 30 | 30 | 90 | 10 | 10 | 10 | 180 | Flank | ||
| 16 | 1 | 8 | 8 | 7 | 21 | Abdomen | ||||
| 17 | 1 | 10 | 10 | 20 | Abdomen | |||||
| Mean | 1.7 | 17 | 19 | 29.17 | 11.42 | 11.17 | 12.56 | 6.25 | 72.31 | -- |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berl, A.; Shir-az, O.; Perk, N.; Levy, A.; Levy, Y.; Shalom, A. Total Facial Autologous Fat Grafting for Treating Skin Manifestations in Scleroderma. Life 2022, 12, 1997. https://doi.org/10.3390/life12121997
Berl A, Shir-az O, Perk N, Levy A, Levy Y, Shalom A. Total Facial Autologous Fat Grafting for Treating Skin Manifestations in Scleroderma. Life. 2022; 12(12):1997. https://doi.org/10.3390/life12121997
Chicago/Turabian StyleBerl, Ariel, Ofir Shir-az, Noa Perk, Abraham Levy, Yair Levy, and Avshalom Shalom. 2022. "Total Facial Autologous Fat Grafting for Treating Skin Manifestations in Scleroderma" Life 12, no. 12: 1997. https://doi.org/10.3390/life12121997
APA StyleBerl, A., Shir-az, O., Perk, N., Levy, A., Levy, Y., & Shalom, A. (2022). Total Facial Autologous Fat Grafting for Treating Skin Manifestations in Scleroderma. Life, 12(12), 1997. https://doi.org/10.3390/life12121997








