Tuberculosis in the Russian Federation: Dynamics of the Epidemic Indicators before and after COVID-19 Pandemic
Abstract
1. Introduction
- −
- The early diagnosis of tuberculosis;
- −
- The treatment and support of patients with TB;
- −
- The management of comorbidities of tuberculosis with Human Immunodeficiency Virus (HIV) infection;
- −
- The prevention of and vaccination against TB.
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Stojanovic, Z.; Gonçalves-Carvalho, F.; Marín, A.; Capa, J.A.; Domínguez, J.; Latorre, I.; Lacoma, A.; Prat-Aymerich, C. Advances in diagnostic tools for respiratory tract infections: From tuberculosis to COVID-19—Changing paradigms? ERJ Open Res. 2022, 8. [Google Scholar] [CrossRef] [PubMed]
- Goossens, H.; Derde, L.; Horby, P.; Bonten, M. The European clinical research response to optimise treatment of patients with COVID-19: Lessons learned, future perspective, and recommendations. Lancet Infect. Dis. 2022, 22, e153–e158. [Google Scholar] [CrossRef]
- World Health Organization. Global Tuberculosis Report; WHO: Geneva, Switzerland, 2015; 192p, Available online: http://www.who.int/tb/en/ (accessed on 1 August 2022).
- World Health Organization. Global Tuberculosis Report 2016 (End TB Strategy); WHO: Geneva, Switzerland, 2016; 18p. [Google Scholar]
- Reid, M.J.A.; Arinaminpathy, N.; Bloom, A.; Bloom, B.R.; Boehme, C.; Chaisson, R.; Chin, D.P.; Churchyard, G.; Cox, H.; Ditiu, L.; et al. Building a tuberculosis-free world: The Lancet Commission on tuberculosis. Lancet Comm. 2019, 393, 1331–1384. [Google Scholar] [CrossRef]
- Vasil’eva, I.A.; Belilovsky, E.M.; Borisov, S.E.; Sterlikov, S.A. World Health Organization Global Tuberculosis Reports: Formation and Interpretation. Tuberc. Lung Dis. 2017, 95, 7–16. (In Russia) [Google Scholar] [CrossRef]
- World Health Organization. Tuberculosis Surveillance and Monitoring in Europe 2017; WHO: Geneva, Switzerland, 2017; 162p, Available online: http://www.euro.who.int/tb/en/ISBN978-92-9498-037-3 (accessed on 1 August 2022).
- Matteelli, A.; Centis, R.; D’Ambrosio, L.; Sotgiu, G.; Tadolini, M.; Pontali, E.; Migliori, G.B. World Health Organization Strategies for the Programmatic Management of Drug-Resistant Tuberculosis. Expert Rev. Respir. Med. 2016, 10, 991–1002. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Hogan, A.B.; Jewell, B.L.; Sherrard-Smith, E.; Vesga, J.F.; Watson, O.J.; Whittaker, C.; Hamlet, A.; Smith, J.A.; Winskill, P.; Verity, R.; et al. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: A modelling study. Lancet Glob. Health 2020, 8, e1132–e1141. [Google Scholar] [CrossRef]
- Cilloni, L.; Fu, H.; Vesga, J.F.; Dowdy, D.; Pretorius, C.; Ahmedov, S.; Nair, S.A.; Mosneaga, A.; Masini, E.; Sahu, S.; et al. The potential impact of the COVID-19 pandemic on the tuberculosis epidemic a modelling analysis. EClinicalMedicine 2020, 28, 100603. [Google Scholar] [CrossRef]
- World Health Organization. Global Tuberculosis Report 2020; WHO: Geneva, Switzerland, 2021; Volume 4, p. 250. ISBN 978-92-4-003702-1. [Google Scholar]
- Migliori, G.B.; Thong, P.M.; Alffenaar, J.-W.; Denholm, J.; Tadolini, M.; Alyaquobi, F.; Blanc, F.-X.; Buonsenso, D.; Cho, J.-G.; Codecasa, L.R.; et al. Gauging the impact of the COVID-19 pandemic on tuberculosis services: A global study. Eur. Respir. J. 2021, 58, 2101786. [Google Scholar] [CrossRef]
- Nechaeva, O.B. The state and prospects of the anti-tuberculosis service in Russia during the period of COVID-19. Tuberc. Lung Dis. 2020, 98, 7–19. (In Russia) [Google Scholar] [CrossRef]
- Glaziou, P. Predicted impact of the COVID-19 pandemic on global tuberculosis deaths in 2020. medRxiv 2020, preprint. [Google Scholar] [CrossRef]
- McQuaid, C.F.; McCreesh, N.; Read, J.M.; Sumner, T.; Houben, R.M.G.J.; White, R.G.; Harris, R.C. The potential impact of COVID-19-related disruption on tuberculosis burden. Eur. Respir. J. 2020, 56, 2001718. [Google Scholar] [CrossRef] [PubMed]
- WHO Global Lists of High Burden Countries for TB, Multidrug/Rifampicin-Resistant TB (MDR/RR-TB) and TB/HIV, 2021–2025; World Health Organization: Geneva, Switzerland, 2021.
- Comella-del-Barrioa, P.; De Souza-Galvãob, M.L.; Prat-Aymericha, C.; Domínguez, J. Impact of COVID-19 on Tuberculosis Control. Arch. Bronconeumol. 2021, 57, S2. [Google Scholar] [CrossRef] [PubMed]
- WHO Consolidated Guidelines on Tuberculosis. Module 5: Management of Tuberculosis in Children and Adolescents; World Health Organization: Geneva, Switzerland, 2022.
- Official Statistic Data of the Russian Federation. Available online: https://www.fedstat.ru (accessed on 1 August 2022).
- Harvey, A.C. Forecasting, Structural Time Series Models, and the Kalman Filter; Cambridge University Press: Cambridge, UK, 1989; 268p. [Google Scholar]
- Hyndman, R.J.; Athanasopoulos, G. Forecasting: Principles and Practice, 2nd ed.; OTexts: Melbourne, Australia, 2018. [Google Scholar]
- Monedero-Recueroa, I.; Gegiac, M.; Waresd, D.F.; Chadhae, S.S.; Mirzayev, F. Situational analysis of 10 countries with a high burden of drug-resistant tuberculosis 2 years post-UNHLM declaration: Progress and setbacks in a changing landscape. Int. J. Infect. Dis. 2021, 108, 557–567. [Google Scholar] [CrossRef]
- Mokrousov, I.; Vyazovaya, A.; Narvskaya, O.; Zhuravlev, V.; Otten, T.; Vishnevsky, B.; Millet, J.; Rastogi, N.; Jiao, W.W.; Shen, A.D. Real-time pcr assay for rapid detection of epidemiologically and clinically significant mycobacterium tuberculosis beijing genotype isolates. J. Clin. Microbiol. 2014, 52, 1691–1693. [Google Scholar] [CrossRef]
- Borisov, S.E.; Belilovski, E.; Filippov, A.; Dheda, K.; Enwerem, M.; Leyet, R.R.; D’Ambrosio, L.; Centis, R.; Migliori, G.B.; Sotgiu, G.; et al. Effectiveness and safety of bedaquiline containing regimens in the treatment of MDR- and XDR-TB: A multicentre study. Eur. Respir. J. 2017, 49, 1700387. [Google Scholar] [CrossRef]
- Starshinova, A.A.; Nazarenko, M.M.; Belyaeva, E.N.; Kudlay, D.A.; Pavlova, M.V.; Yablonskiy, P.K. Efficacy of using bedaquiline in treatment of tuberculosis patients with multiple and extensive drug resistance. Tuberc. Lung Dis. 2022, 100, 56–63. [Google Scholar] [CrossRef]
- Yablonskiy, P.K.; Starshinova, A.A.; Nazarenko, M.M.; Beliaeva, E.N.; Chuzhov, A.L.; Alekseev, D.Y.; Pavlova, M.V. Efficacy of new treatment regimes of patients with extensive drug resistance of mycobacterium tuberculosis. Bull. Contemp. Clin. Med. 2022, 15, 67–75. [Google Scholar] [CrossRef]
- Starshinova, A.A.; Dovgalyk, I.; Malkova, A.M.; Zinchenko, Y.S.; Pavlova, M.V.; Belyaeva, E.; Basantsova, N.Y.; Nazarenko, M.; Kudlai, D.A.; Yablonskiy, P. Recombinant tuberculosis allergen (Diaskintest®) in tuberculosis diagnostic in Russia (meta-analysis). Int. J. Mycobacteriology 2020, 9, 335–346. [Google Scholar]
- Aksenova, V.A.; Baryshnikova, L.A.; Klevno, N.I.; Kudlay, D.A. Screening for tuberculosis infection in children and adolescents in Russia—past, present, future. Tuberc. Lung Dis. 2019, 97, 59–67. [Google Scholar] [CrossRef]
- Nechaeva, O.B. Socially important infectious diseases posing a biological threat to the population of Russia. Tuberc. Lung Dis. 2019, 97, 7–17. [Google Scholar] [CrossRef]
- Nechaeva, O.B.; Son, I.M.; Gordina, A.V.; Sterlikov, S.A.; Kucheryavaya, D.A.; Dergachev, A.V.; Ponomarev, S.B. Resources and Activities of TB Organizations in the Russian Federation in 2019–2020 (Statistical Materials); RIO TsNIIOIZ: Moscow, Russia, 2021; p. 112. (In Russia) [Google Scholar]
- Vasilyeva, I.A.; Testov, V.V.; Sterlikov, S.A. Tuberculosis Situation in the Years of the COVID-19 Pandemic—2020–2021. Tuberc. Lung Dis. 2022, 100, 6–12. [Google Scholar] [CrossRef]
- Tuberculosis in the Russian Federation 2011 Analytical Review of Statistical Indicators Used in the Russian Federation and in the World; Ministry of Health and Social Development of the Russian Federation: Moscow, Russia, 2015; 280p. (In Russia)
- Fronteira, I.; Sidat, M.; Magalhães, J.P.; de Barros, F.P.C.; Delgado, A.P.; Correia, T.; Daniel-Ribeiro, C.T.; Ferrinho, P. The SARS-CoV-2 pandemic: A syndemic perspective. One Health 2021, 12, 100228. [Google Scholar] [CrossRef] [PubMed]
- Trajman, A.; Felker, I.; Alves, L.C.; Coutinho, I.; Osman, M.; Meehan, S.-A.; Singh, U.B.; Schwartz, Y. The COVID-19 and TB syndemic: The way forward. Int. J. Tuberc. Lung Dis. 2022, 26, 710–719. [Google Scholar] [CrossRef]
- Best Practices in Child and Adolescent Tuberculosis Care; World Health Organization: Geneva, Switzerland, 2018; 124p, ISBN 9789241514651. Available online: https://apps.who.int/iris/handle/10665/274373 (accessed on 1 August 2022).
- Xia, Y.; Huang, F.; Chen, H.; Wang, N.; Du, X.; Chen, W.; Li, T.; Huan, S.; Sun, M.; Liu, J.; et al. The Impact of COVID-19 on Tuberculosis Patients’ Behavior of Seeking Medical Care—China, 2020. China CDC Wkly. 2021, 3, 553–556. [Google Scholar] [CrossRef]
- Mafalle, L.F.; Mikhnyakon, B.B.; Ogunrombi, M.O.; Adeleke, O.A. Treatment of childhood tuberculosis: A global problem or a Breakthrough? Children 2022, 9, 1120. [Google Scholar] [CrossRef]
- Ramesh, H.; Shoba, A.; Manjula, V.D. Results of treatment of pediatric tuberculosis from the point of view of Kottayam, Kerala. Indian J. Public Health 2012, 24, 280–284. [Google Scholar]
- Chatterjee, S.; Das, P.; Vassall, A. The impact of restrictive measures to combat COVID-19 on the income and use of medical services by tuberculosis patients in India. BMX Infect. Dis. 2022, 22, 711. [Google Scholar] [CrossRef]
- Liu, Q.; Lu, P.; Shen, Y.; Li, C.; Wang, J.; Zhu, L.; Lu, W.; Martinez, L. Concomitant impact of the 2019 coronavirus disease pandemic (COVID-19) on tuberculosis control in Jiangsu Province, China. Clean. Infect. Dis. 2021, 73, 542–544. [Google Scholar] [CrossRef]
- Jain, V.K.; Lyenger, K.D.; Sami, D.A.; Vaishya, R. tuberculosis in the era of COVID-19 in India. Diabetes Metab. Syndr. Clean. Res. Rev. 2020, 14, 1439–1443. [Google Scholar] [CrossRef]
- Sterlikov, S.A. Organizational aspects of increasing the effectiveness of preventive fluorographic examinations. Med. Alliance 2013, 4, 28–34. (In Russia) [Google Scholar]
| Years/Region | 2017 | 2018 | 2019 | 2020 | 2021 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Incidence among Population | Incidence among Children (0–17 Years) | Incidence among Population | Incidence among Children (0–17 Years) | Incidence among Population | Incidence among Children (0–17 Years) | Incidence among Population | Incidence among Children (0–17 Years) | Incidence among Population | Incidence among Children (0–17 Years) | |
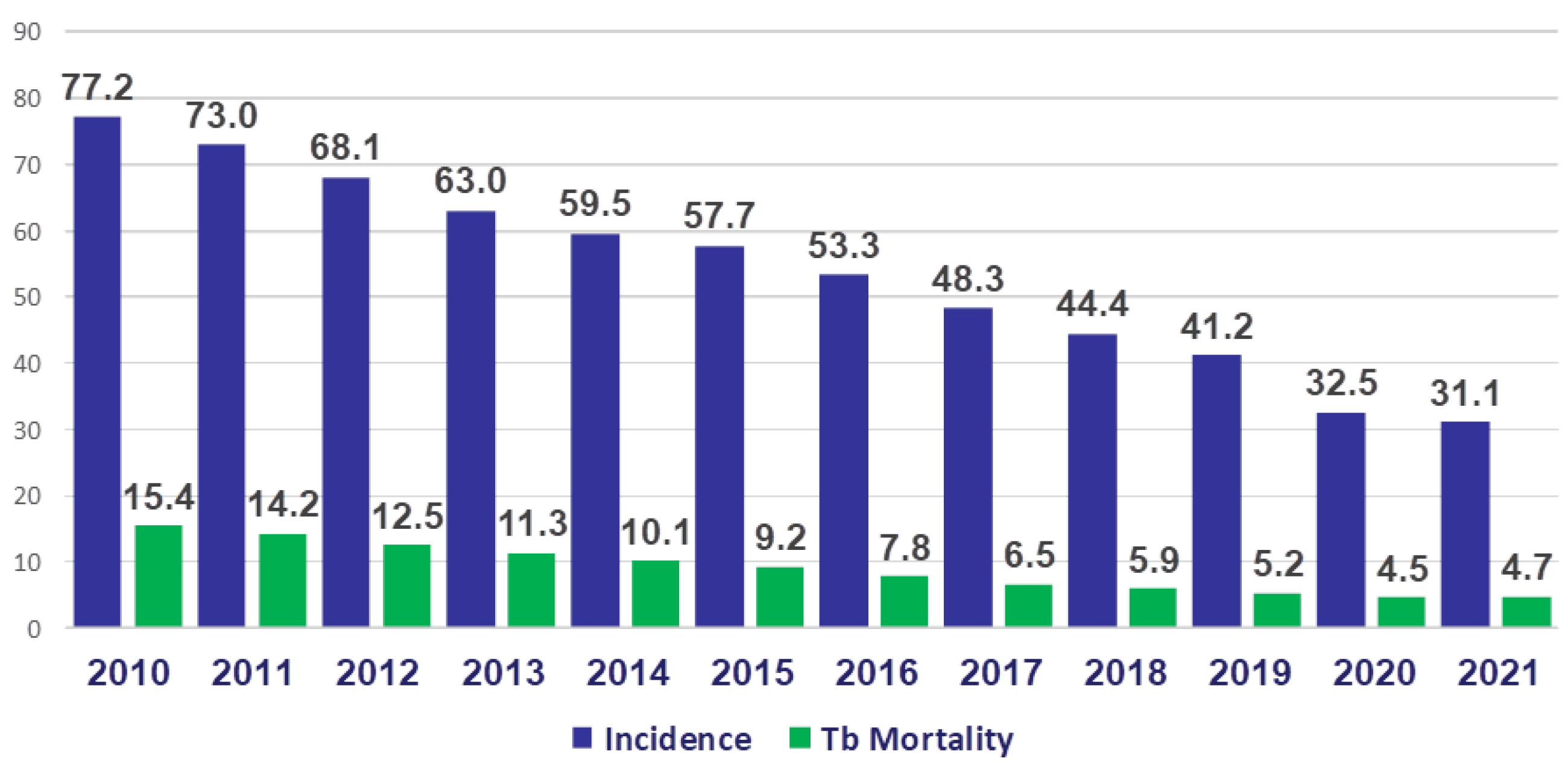
| Russian Federation | 48.3 | 11.2 | 44.4 | 9.7 | 41.2 | 9.0 | 32.5 | 7.2 | 31.1 | 7.5 |
| North-Western Federal District | 31.3 | 8.4 | 28.6 | 8.0 | 25.2 | 5.8 | 21.8 | 4.7 | 19.7 | 4.6 |
| Years/Region | 2017 | 2018 | 2019 | 2020 | 2021 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Incidence | Mortality | Incidence | Mortality | Incidence | Mortality | Incidence | Mortality | Incidence | Mortality | |
| Russian Federation | 48.3 | 6.5 | 44.4 | 5.9 | 41.2 | 5.2 | 32.5 | 4.5 | 31.1 | 4.7 |
| North-Western Federal District | 31.3 | 4.0 | 28.6 | 3.6 | 25.2 | 2.8 | 21.8 | 2.3 | 19.7 | 2.6 |
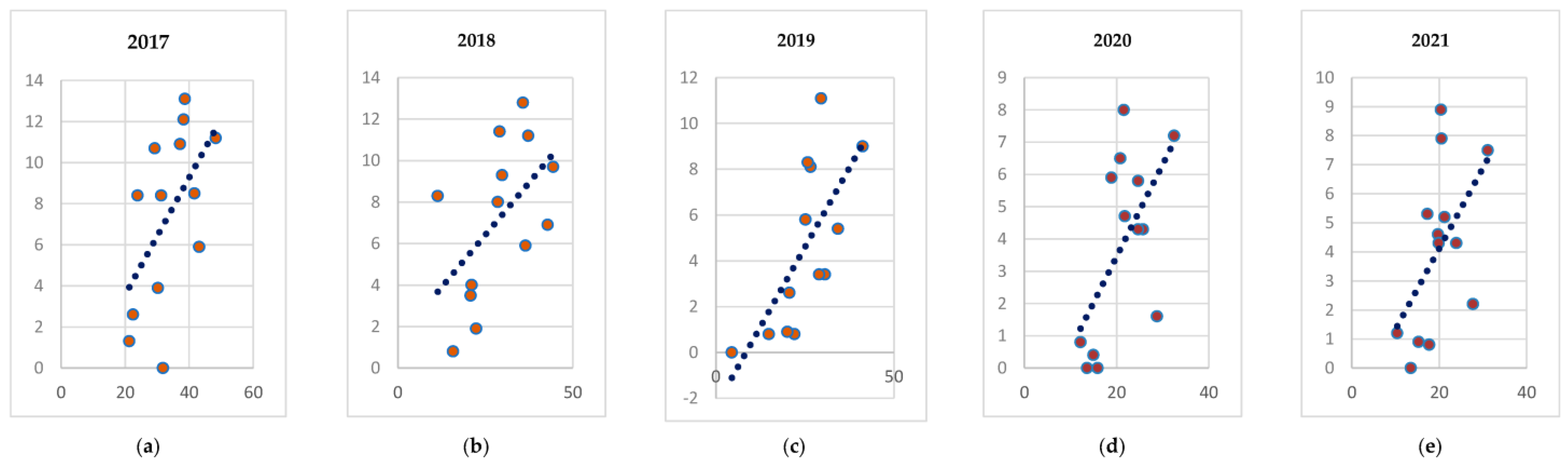
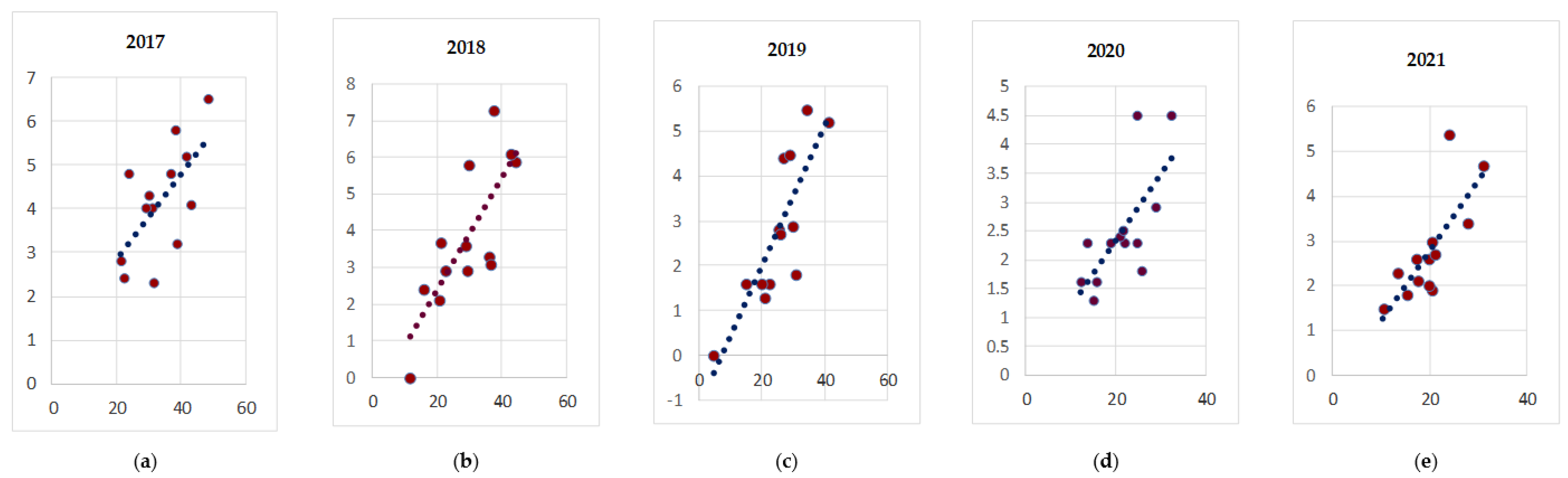
| Year | First Parameter | Incidence | Incidence | Incidence | Incidence among Children (0–17 Years) |
|---|---|---|---|---|---|
| Second Parameter | Coverage by Occupational Health Examination among Population | Incidence among Children (0–17 Years) | Tb Mortality | Tb Mortality | |
| 2017 | 0.72 | 0.55 | 0.64 | 0.67 | |
| 2018 | 0.41 | 0.54 | 0.78 | 0.37 | |
| 2019 | 0.09 | 0.69 | 0.84 | 0.64 | |
| 2020 | 0.32 | 0.60 | 0.70 | 0.47 | |
| 2021 | 0.40 | 0.53 | 0.76 | 0.32 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Starshinova, A.; Dovgalyk, I.; Beltukov, M.; Zinchenko, Y.; Glushkova, A.; Starshinova, A.Y.; Doktorova, N.; Kudlay, D. Tuberculosis in the Russian Federation: Dynamics of the Epidemic Indicators before and after COVID-19 Pandemic. Life 2022, 12, 1468. https://doi.org/10.3390/life12101468
Starshinova A, Dovgalyk I, Beltukov M, Zinchenko Y, Glushkova A, Starshinova AY, Doktorova N, Kudlay D. Tuberculosis in the Russian Federation: Dynamics of the Epidemic Indicators before and after COVID-19 Pandemic. Life. 2022; 12(10):1468. https://doi.org/10.3390/life12101468
Chicago/Turabian StyleStarshinova, Anna, Irina Dovgalyk, Mikhail Beltukov, Yulia Zinchenko, Anzhela Glushkova, Anastasia Y. Starshinova, Natalia Doktorova, and Dmitry Kudlay. 2022. "Tuberculosis in the Russian Federation: Dynamics of the Epidemic Indicators before and after COVID-19 Pandemic" Life 12, no. 10: 1468. https://doi.org/10.3390/life12101468
APA StyleStarshinova, A., Dovgalyk, I., Beltukov, M., Zinchenko, Y., Glushkova, A., Starshinova, A. Y., Doktorova, N., & Kudlay, D. (2022). Tuberculosis in the Russian Federation: Dynamics of the Epidemic Indicators before and after COVID-19 Pandemic. Life, 12(10), 1468. https://doi.org/10.3390/life12101468






