Anterior Dural Tear in Thoracic and Lumbar Spinal Fractures: Single-Center Experience with Coating Technique and Literature Review of the Available Strategies
Abstract
:1. Introduction
2. Materials and Methods
Literature Review
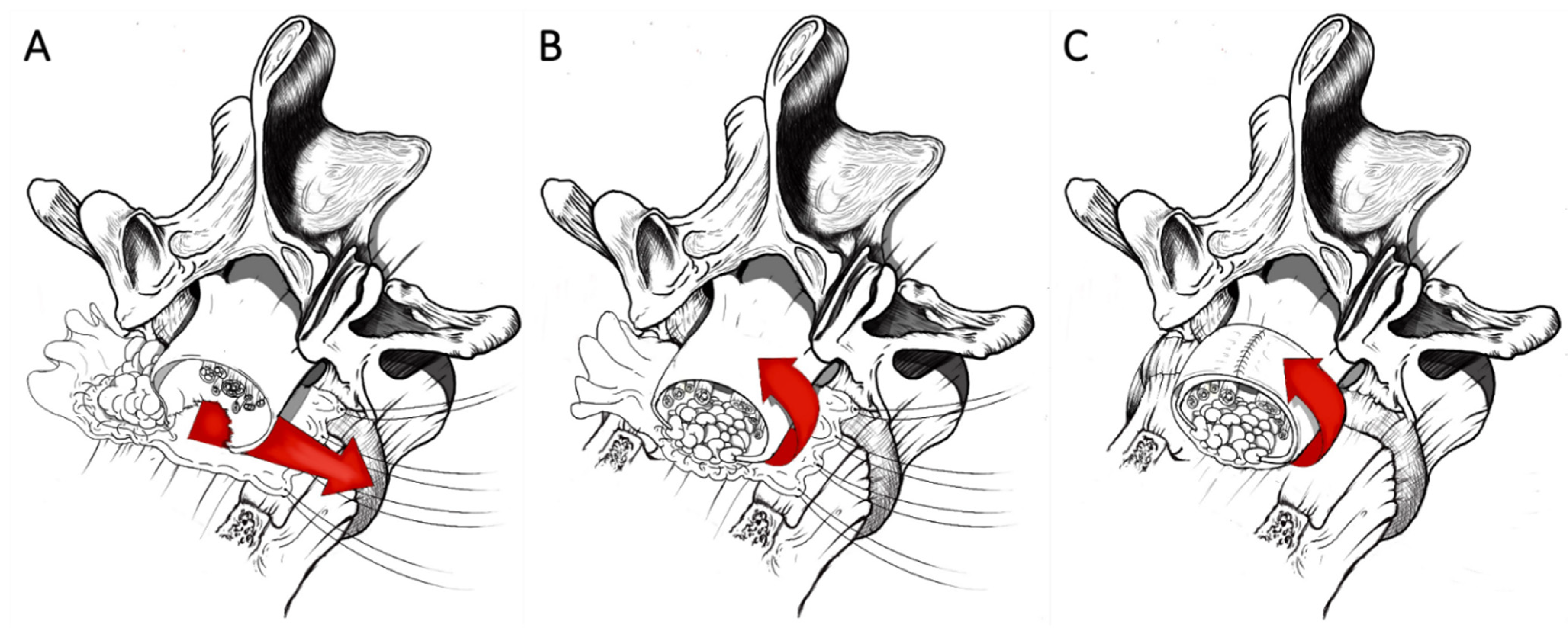
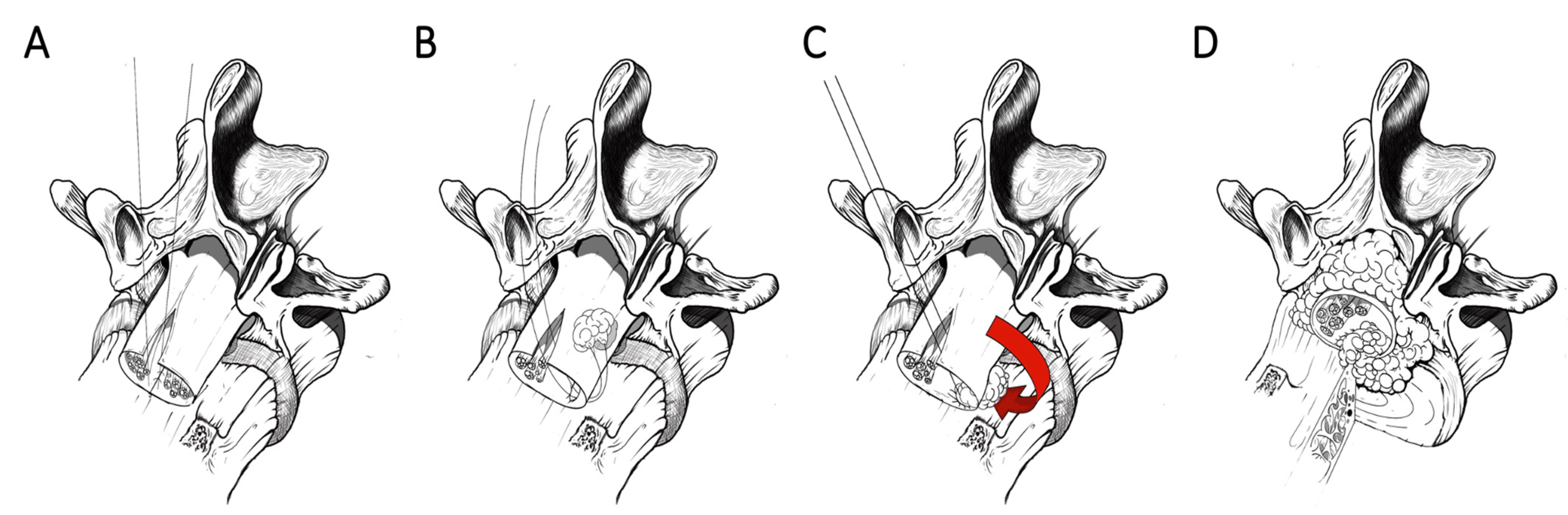
3. Coating Techniques
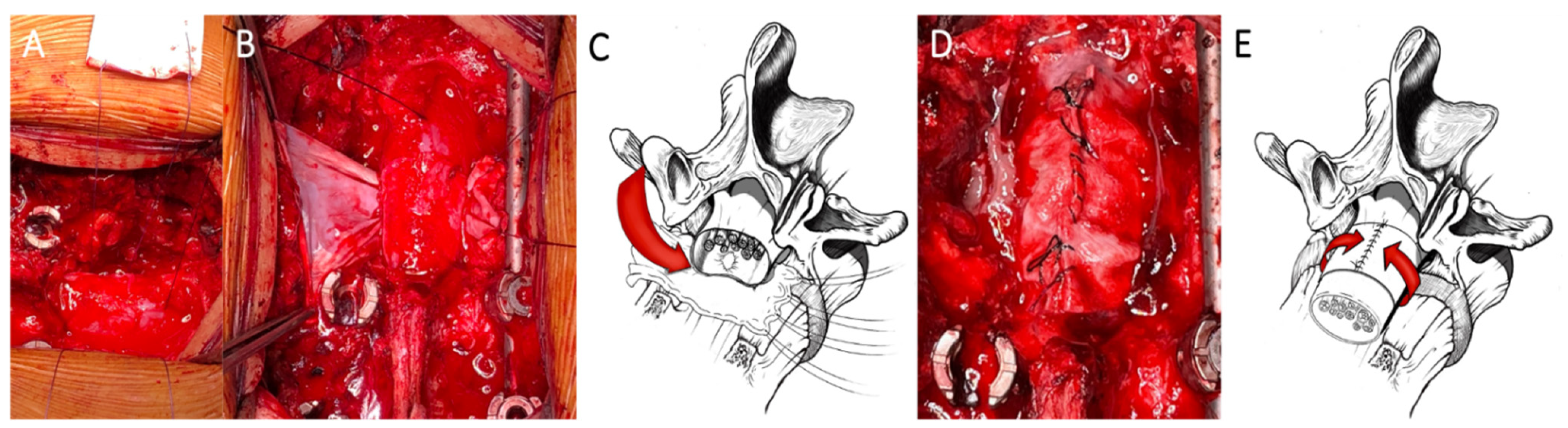
3.1. Dural Coating
3.2. Dural Coating Straddling Nerve Roots
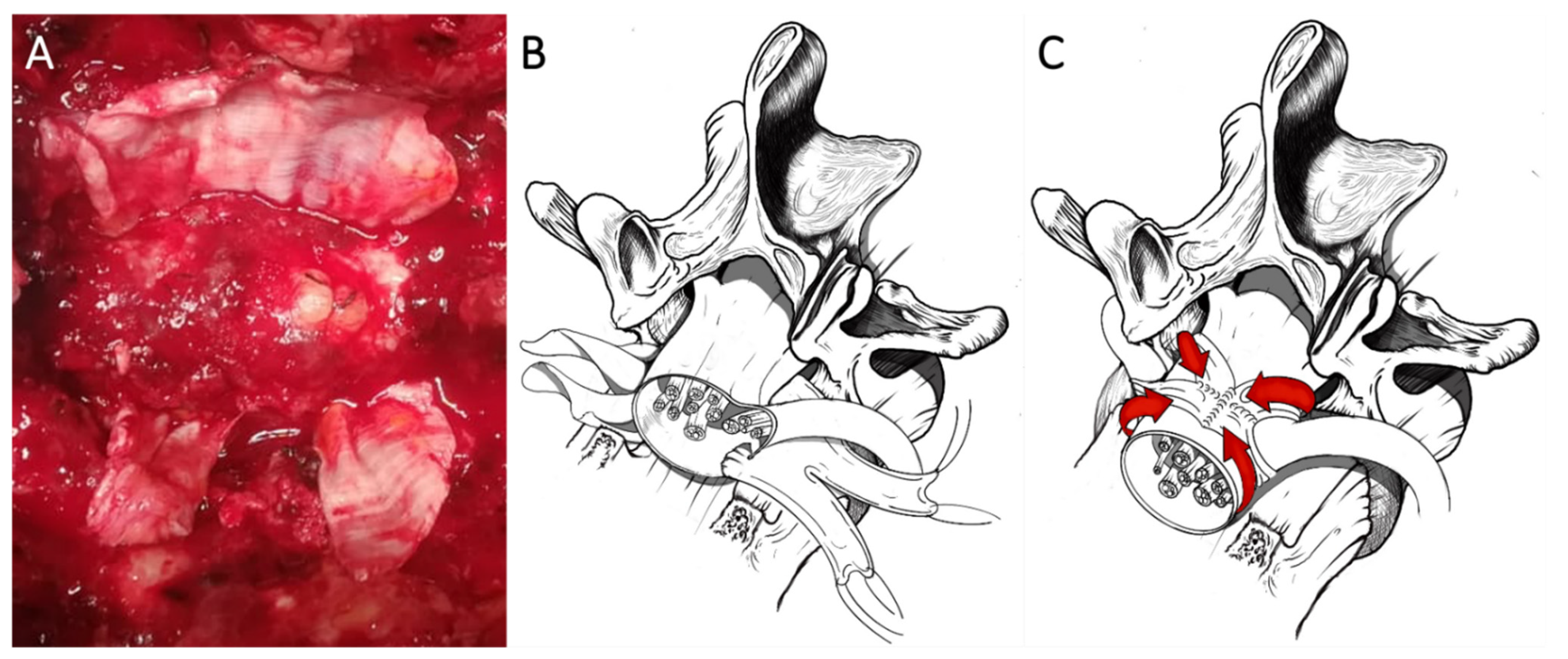
3.3. Dural Coating with Sutured Fat Graft
4. Results
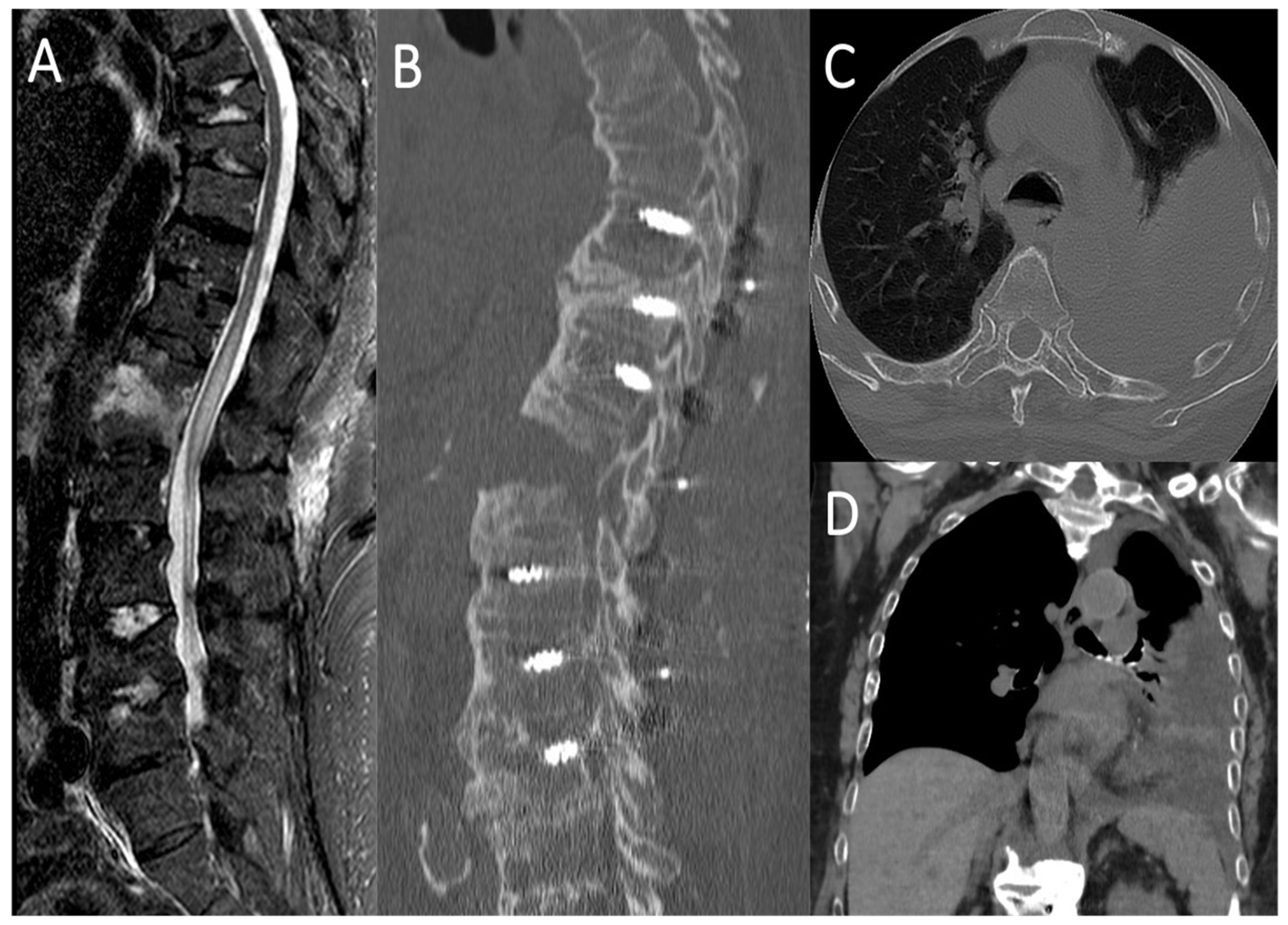
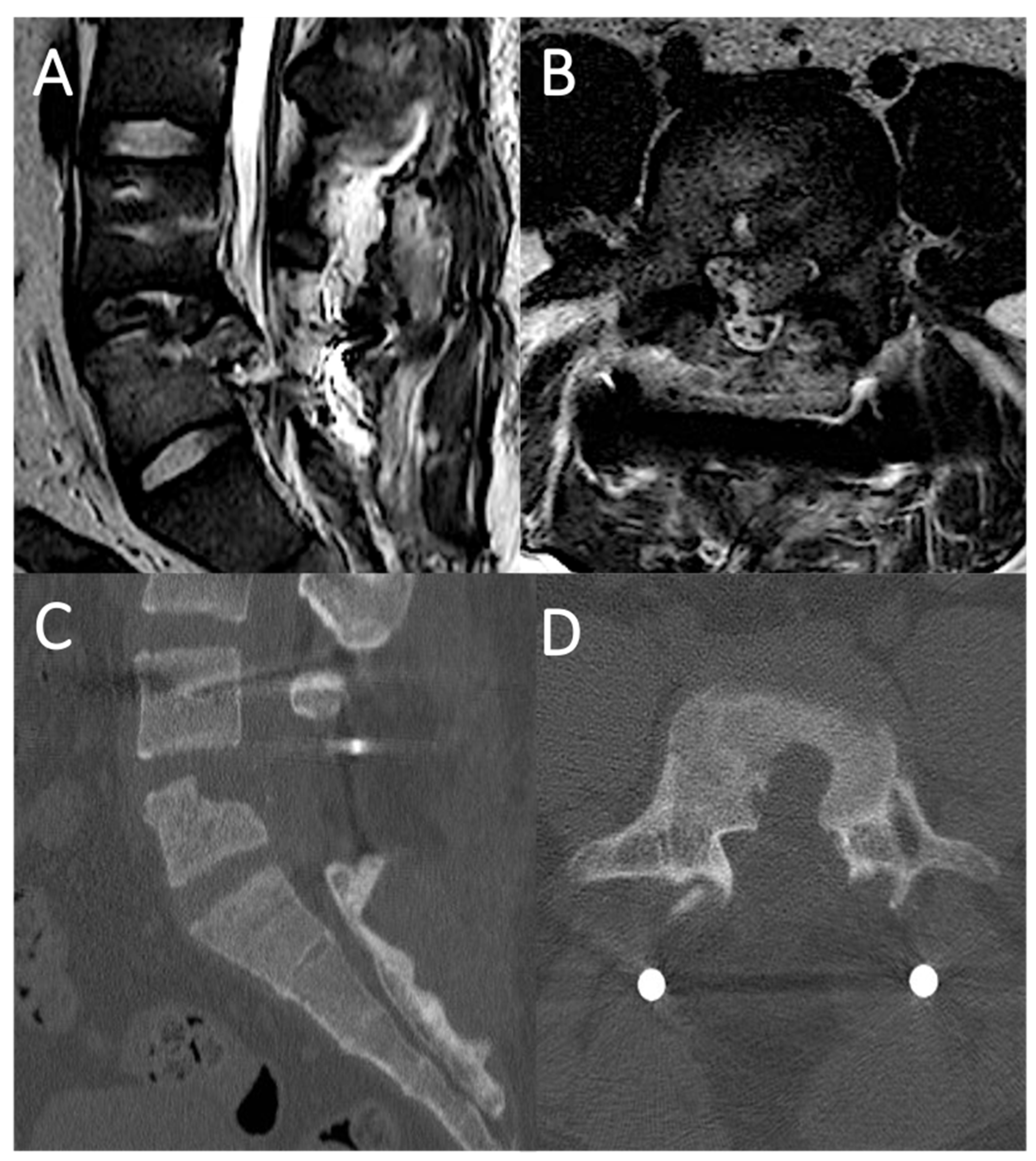
4.1. Case Report 1: Coating
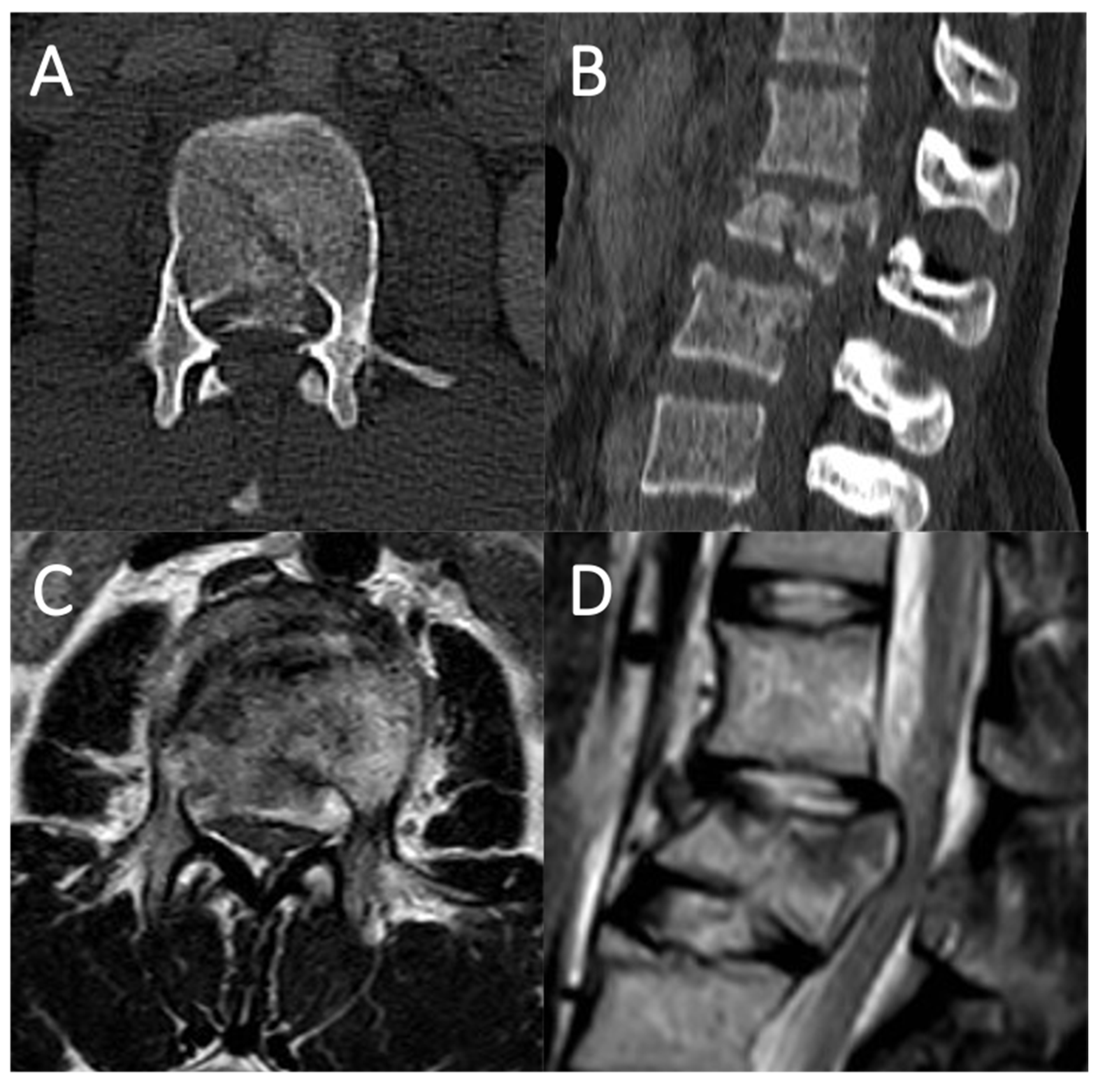
4.2. Case Report 2: Coating Straddling Nerve Roots
4.3. Case Report 3: Coating with Sutured Fat Graft
5. Literature Review
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Carl, A.L.; Matsumoto, M.; Whalen, J.T. Anterior dural laceration caused by thoracolumbar and lumbar burst fractures. J. Spinal Disord. 2000, 13, 399–403. [Google Scholar] [CrossRef]
- Vaccaro, A.R.; Oner, F.; Kepler, C.K.; Dvorak, M.; Schnake, K.; Bellabarba, C.; Reinhold, M.; Aarabi, B.; Kandziora, F.; Chapman, J.; et al. AOSpine thoracolumbar spine injury classification system: Fracture description, neurological status, and key modifiers. Spine 2013, 38, 2028–2037. [Google Scholar] [CrossRef]
- Choi, J.H.; Kim, J.-S.; Jang, J.-S.; Lee, D.Y. Transdural Nerve Rootlet Entrapment in the Intervertebral Disc Space through Minimal Dural Tear: Report of 4 Cases. J. Korean Neurosurg. Soc. 2013, 53, 52–56. [Google Scholar] [CrossRef]
- Huang, A.P.-H.; Chen, C.-M.; Lai, H.-S.; Chou, C.-C.; Lu, D.C.; Kuo, L.-T.; Chuang, H.-Y.; Tsai, J.-C. Posterior transthecal approach for repair of cauda equina fibers and ventral dural laceration in lumbar burst fracture: A novel surgical technique. Spine 2013, 38, E1156–E1161. [Google Scholar] [CrossRef] [PubMed]
- Nakhla, J.; Nasser, R.; Ramos, R.D.L.G.; Kobets, A.; Ammar, A.; Echt, M.; Gelfand, Y.; Kinon, M.; Yassari, R. Anterior Lumbar Dural Tear: A Transthecal Route for Primary Closure after Iatrogenic Durotomy. World Neurosurg. 2017, 107, 522–525. [Google Scholar] [CrossRef] [PubMed]
- Schievink, W.I.; Wasserstein, P.; Maya, M.M. Intraspinal hemorrhage in spontaneous intracranial hypotension: Link to superficial siderosis? Report of 2 cases. J. Neurosurg. Spine 2016, 24, 454–456. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pickett, J.; Blumenkopf, B. Dural lacerations and thoracolumbar fractures. J. Spinal Disord. 1989, 2, 99–103. [Google Scholar] [CrossRef]
- Black, P. Cerebrospinal fluid leaks following spinal surgery: Use of fat grafts for prevention and repair. Technical note. J. Neurosurg. 2002, 96 (Suppl. 2), 250–252. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.-H.; Kim, K.-T.; Park, J.-I.; Park, K.-S.; Cho, D.-C.; Sung, J.-K. Repair of Inaccessible Ventral Dural Defect in Thoracic Spine: Double Layered Duraplasty. Korean J. Spine 2016, 13, 87–90. [Google Scholar] [CrossRef]
- Mayfield, F.H.; Kurokawa, K. Watertight closure of spinal dura mater. Technical note. J. Neurosurg. 1975, 43, 639–640. [Google Scholar] [CrossRef]
- Takai, K.; Komori, T.; Niimura, M.; Taniguchi, M. Superficial siderosis of the central nervous system associated with intraspinal hemorrhage from ventral thoracic epidural veins and a ventral spinal CSF leak: Case report. J. Neurosurg. Spine 2017, 26, 751–753. [Google Scholar] [CrossRef] [Green Version]
- Moon, J.H.; Lee, S.; Chung, C.K.; Kim, C.H.; Heo, W. How to address cerebrospinal fluid leakage following ossification of the posterior longitudinal ligament surgery. J. Clin. Neurosci. 2017, 45, 172–179. [Google Scholar] [CrossRef]
- Lee, I.; Kim, H.; Lee, J.; Kim, S.-J.; Jeong, Y.; Kim, D.; Moon, T.-Y. Dural tears in spinal burst fractures: Predictable MR imaging findings. AJNR Am. J. Neuroradiol. 2009, 30, 142–146. [Google Scholar] [CrossRef] [Green Version]
- Cammisa, F.P., Jr.; Eismont, F.J.; Green, B.A. Dural laceration occurring with burst fractures and associated laminar fractures. J. Bone Joint Surg. Am. 1989, 71, 1044–1052. [Google Scholar] [CrossRef] [Green Version]
- De Iure, F.; Lofrese, G.; de Bonis, P.; Cultrera, F.; Cappuccio, M.; Battisti, S. Vertebral body spread in thoracolumbar burst fractures can predict posterior construct failure. Spine J. 2018, 18, 1005–1013. [Google Scholar] [CrossRef]
- Keenen, T.L.; Antony, J.; Benson, D.R. Dural tears associated with lumbar burst fractures. J. Orthop. Trauma 1990, 4, 243–245. [Google Scholar] [CrossRef]
- Miller, C.A.; Dewey, R.C.; Hunt, W.E. Impaction fracture of the lumbar vertebrae with dural tear. J. Neurosurg. 1980, 53, 765–771. [Google Scholar] [CrossRef]
- Shi, X.; Xiang, S.; Dai, B.; He, Z. Association of the presence and its types of lamina fractures with posterior dural tear and neurological deficits in traumatic thoracic and lumbar burst fractures. BMC Musculoskelet. Disord. 2021, 22, 300. [Google Scholar] [CrossRef]
- Yoshiiwa, T.; Miyazaki, M.; Kodera, R.; Kawano, M.; Tsumura, H. Predictable imaging signs of cauda equina entrapment in thoracolumbar and lumbar burst fractures with greenstick lamina fractures. Asian Spine J. 2014, 8, 339–345. [Google Scholar] [CrossRef] [Green Version]
- Lofrese, G.; Cultrera, F.; Visani, J.; Scerrati, A.; Mongardi, L.; Donati, R.; Tosatto, L.; De Bonis, P. Chylothorax in spine fractures: A rarely reported complication? Literature review with an example case. J. Trauma Acute Care Surg. 2020, 89, e140–e146. [Google Scholar] [CrossRef]
- Nairus, J.G.; Richman, J.D.; Douglas, R.A. Retroperitoneal pseudomeningocele complicated by meningitis following a lumbar burst fracture. A case report. Spine 1996, 21, 1090–1093. [Google Scholar] [CrossRef]
- Cornips, E.M.J. Multilayer Dura Reconstruction After Thoracoscopic Microdiscectomy: Technique and Results. World Neurosurg. 2018, 109, e691–e698. [Google Scholar] [CrossRef]
- Grannum, S.; Patel, M.S.; Attar, F.; Newey, M. Dural tears in primary decompressive lumbar surgery. Is primary repair necessary for a good outcome? Eur. Spine J. 2014, 23, 904–908. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oitment, C.; Aref, M.; Almenawar, S.; Reddy, K. Spinal Dural Repair: A Canadian Questionnaire. Glob. Spine J. 2018, 8, 359–364. [Google Scholar] [CrossRef] [PubMed]
| AOSpine Classification System of Thoracolumbar Spinal Fractures | ||
|---|---|---|
| Type | Subtype | Description |
| Type A Compression injuries | A0 | Minor, nonstructural fractures Fractures which do not compromise the structural integrity of the spinal column such as transverse process or spinous process fractures |
| A1 | Wedge-compression Fracture of a single endplate without involvement of the posterior wall of the vertebral body | |
| A2 | Split Fracture of both endplates without involvement of the posterior wall of the vertebral body | |
| A3 | Incomplete burst Fracture with any involvement of the posterior wall; only a single endplate fractured. Vertical fracture of the lamina is usually present and does not constitute a tension band failure | |
| A4 | Complete burst Fracture with any involvement of the posterior wall and both endplates. Vertical fracture of the lamina is usually present and does not constitute a tension band failure | |
| Type B Distraction injuries | B1 | Transosseous tension band disruption Monosegmental pure osseous failure of the posterior tension band. Fracture may extend through the pedicle and exit from the posterior aspect of the pars interarticularis or extend through the pedicle through the spinous process before exiting into the soft tissue posteriorly. |
| B2 | Posterior tension band disruption Bony and/or ligamentary failure of the posterior tension band of the spine together with a type A fracture. Type A fracture should be classified separately | |
| B3 | Hyperextension Injury through the disk or vertebral body leading to a hyperextended position of the spinal column. Commonly seen in ankylotic disorders. Disruption of the anterior longitudinal ligament (ALL) that serves as the anterior tension band of the spine, but there is a posterior hinge preventing further displacement | |
| Type C Displacement or dislocation | C | Displacement or dislocation There are no subtypes because various configurations are possible. Failure of all elements leading to displacement or dislocation in any direction of the fractured segments of the spine. |
| Authors | N° of Patients | Pathology | Canal Encroachment >50% (y/n) | Neurologic Impairment (y/n) | Treatment | Location of Dural Tear | Repair Technique | Subarachnoid Drainage (Days) | Complication | Follow-Up (Months) |
|---|---|---|---|---|---|---|---|---|---|---|
| Mayfield et al. 1975 | - | - | - | - | - | Anterior | Fat plug sutured in the defect | - | - | - |
| Pickett et al. 1989 | 3 | Thoracic and lumbar burst fracture | - | - | Posterior decompression and fusion | Antero-lateral | Direct suture | - | No | - |
| Carl et al. 2000 | 6 | L2 burst fracture | Y | Y | Anterior fusion | Anterior | Direct suture | - | - | - |
| L1 burst fracture | Y | Y | Anterior fusion | Anterior | Direct suture | - | - | - | ||
| L1 burst fracture | Y | Y | Anterior fusion | Anterior | Direct suture | - | - | - | ||
| L2 burst fracture | Y | Y | Anterior fusion | Anterior | Direct suture | - | - | - | ||
| L4 burst fracture | Y | Y | Anterior fusion | Anterior | Direct suture | - | - | - | ||
| T12 burst fracture | Y | Y | Anterior fusion | Anterior | Direct suture | 6 | CSF leakage in pleural space | 24 | ||
| Black 2002 | - | Degenerative spine diseases (thoracic and lumbar) | - | - | Laminectomy and discectomy | Anterior and antero-lateral | Fat pad covering defect and adjacent dura | No | No | - |
| Huang et al. 2013 | 5 | L2 burst fracture | Y | Y | Posterior decompression and fusion | Anterior | Transdural direct suture | - | No | 18 |
| L1 burst fracture | Y | Y | Posterior decompression and fusion | Anterior | Transdural direct suture | - | No | 16 | ||
| L2, L3 burst fractures | Y | Y | Posterior decompression and fusion | Anterior | Transdural direct suture | - | Pneumonia, bedsore, wound infection | 12 | ||
| L1 burst fracture | Y | Y | Posterior decompression and fusion | Anterior | Transdural direct suture | - | Bedsore | 9 | ||
| L2 burst fracture | Y | Y | Posterior decompression and fusion | Anterior | Transdural direct suture | - | No | 8 | ||
| Choi et al. 2013 | 4 | L4-L5 disc herniation | N | N | Laminectomy and discectomy | Anterior | Transdural direct suture | - | No | 6 |
| L2-L4 bulging and foraminal stenosis | N | N | Laminectomy, discectomy and interspinous device | Anterior | Transdural direct suture | - | No | 6 | ||
| L4-L5 disc herniation | N | N | Laminectomy, discectomy and interspinous device | Anterior | Transdural direct suture | - | No | 6 | ||
| L1-L2 disc herniation and OPLL | N | N | Anterior decompression and fusion | Anterior | Transdural direct suture | - | No | 6 | ||
| Schievink et al. 2016 | 1 | T9-T10 ventral dural defect in spontaneous intracranial hypotension | N | N | - | Anterior | Transdural direct suture | No | No | 12 |
| Lee et al. 2016 | 1 | Thoracic OPLL | - | Y | Posterior decompression and fusion | Anterior | Double layered (epidural and transdural) | 7 | No | 16 |
| Nakhla et al. 2017 | 1 | Grade II spondylolisthesis L4-L5 | N | N | Posterior lumbar interbody fusion | Anterior | Transdural direct suture | No | No | 6 |
| Takai et al. 2018 | 1 | T12-L1 osteophyte | N | N | Laminoplasty | Anterior | Transdural suture of fat graft | - | Subdural hematoma | 24 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lofrese, G.; Visani, J.; Cultrera, F.; De Bonis, P.; Tosatto, L.; Scerrati, A. Anterior Dural Tear in Thoracic and Lumbar Spinal Fractures: Single-Center Experience with Coating Technique and Literature Review of the Available Strategies. Life 2021, 11, 875. https://doi.org/10.3390/life11090875
Lofrese G, Visani J, Cultrera F, De Bonis P, Tosatto L, Scerrati A. Anterior Dural Tear in Thoracic and Lumbar Spinal Fractures: Single-Center Experience with Coating Technique and Literature Review of the Available Strategies. Life. 2021; 11(9):875. https://doi.org/10.3390/life11090875
Chicago/Turabian StyleLofrese, Giorgio, Jacopo Visani, Francesco Cultrera, Pasquale De Bonis, Luigino Tosatto, and Alba Scerrati. 2021. "Anterior Dural Tear in Thoracic and Lumbar Spinal Fractures: Single-Center Experience with Coating Technique and Literature Review of the Available Strategies" Life 11, no. 9: 875. https://doi.org/10.3390/life11090875
APA StyleLofrese, G., Visani, J., Cultrera, F., De Bonis, P., Tosatto, L., & Scerrati, A. (2021). Anterior Dural Tear in Thoracic and Lumbar Spinal Fractures: Single-Center Experience with Coating Technique and Literature Review of the Available Strategies. Life, 11(9), 875. https://doi.org/10.3390/life11090875








