Drug Repurposing for the Management of Depression: Where Do We Stand Currently?
Abstract
1. Introduction
2. Drug Repurposing
2.1. History
2.2. Different Types of Drug Repurposing
2.2.1. Drug Repositioning
2.2.2. Drug Reformulation
2.2.3. Drug Combination
2.3. Common Approaches
2.3.1. Computational Approaches
Signature Matching
- Transcriptomic: This technique compares gene expression in a healthy state, disease-associated state, and medication-using state. If a medication can reverse the expression pattern of the genes related to disease phenotype, it will probably also revert the disease phenotype itself [10,12,16,23,24,25].
- An example of this approach is that ketamine improves mood by modulating miRNAs like miR-598-5p and miR-451 [13]. Histone deacetylase (HDAC) inhibitors like vorinostat are promising drug repositioning targets for depression, anxiety and schizophrenia treatment due to their role in affecting gene expression [26]. Peroxisome proliferator-activator receptor (PPAR-γ) agonists, especially pioglitazone, have significant antidepressant outcomes in MDD and major depressive episodes of bipolar disorder due to their role in adjusting responsible gene expressions [13]. HMG-CoA reductase inhibitors (statins) are PPAR-α ligands that increase the expression of some neuronal growth factors. Randomized controlled trials have suggested that they possess beneficial effects in combination with selective serotonin reuptake inhibitors (SSRIs) [21].
- Metabolomics: Metabolomics is the study of all chemical procedures in the body [27]. A drug can be shared between two different disease treatments with similar pathophysiology [5]. This approach helps us to gain a comprehensive idea about the molecular processes involved in disease pathophysiology and finding how close our preclinical models to reality are [28]. Nuclear magnetic resonance and mass spectroscopy are two methods for analyzing the metabolome [29].
- Proteomics: Most medications apply their therapeutic effects by interacting with protein targets, and it is crucial to understand these interactions for drug development [12].
- Chemical Structure: In this method, networks are made based on the shared chemical features [10] as similarity in chemical structure may lead to the same biological activity [10,16]. As an example, chlorcyclizine belongs to the phenylpiperazine class. This class includes many antipsychotic and antidepressant medications and chemical structure similarities between these medications and chlorcyclizine make it likely to possess the same effects [26].
- Adverse Event Profiles: A hypothesis suggests that two different medications showing the same adverse effects might affect a shared target, protein, or pathway [10,16]. As well, a medication’s adverse effect resembling a disease phenotype can imply a shared pathway or physiology between the drug and the illness [10,15,16]. In addition, if two treatments for one disease with different mechanisms demonstrate the same uncommon adverse effect, there may be a shared underlying mechanism that links adverse events and therapeutic effects [30]. Side effects are more helpful in predicting drug indications than chemical structure or protein targets. It is possible to extract adverse events data from chemical structures if a drug has not reached the clinical trial level [31].
Computational Molecular Docking
Genome-Wide Associated Studies (GWAS)
Pathway or Network Mapping
2.3.2. Experimental Approaches
Retrospective Clinical Analysis
- EHRs: EHRs data are subdivided into structured (diagnosis and pathophysiology data, laboratory test results, and medication prescriptions) and unstructured (patients’ symptoms reports and imaging data) groups [10].
- Analyzing data gained from the national health insurance of Taiwan research database showed metformin is a promising target for drug repositioning for depression and anxiety [26]. The results of observational or case-control studies indicated a lower risk of MDD in patients using angiotensin-converting enzyme inhibitors (ACEIs) like telmisartan in comparison with other antihypertensive medications. Case reports also demonstrated that pramipexole, a relatively new dopamine receptor agonist, has potential effects in treating MDD. An observational study on 82,643 women revealed the relation between higher flavonoid intake and lower risk of MDD. Last but not least, a meta-analysis of 17 observational studies suggested the association between depression and zinc deficiency [21].
- Post-Marketing Surveillance and Clinical Data: Retrospective clinical data analysis showed that using anti-inflammatory medications, especially celecoxib, with antidepressants improves the responses to first-line antidepressants. Clinical data claims that valproic acid enhances the effects of antidepressants in resistant depression patients. Based on clinical data, quetiapine co-administered with antidepressants improves the outcomes in patients with MDD and cerebrovascular deterioration [13]. Reviewing prior literature has shown that phenothiazines have anti-depressive effects resembling tricyclic antidepressants. Atypical antipsychotics can also help treat depression as adjunctive or primary therapy based on a meta-analysis [28]. Taking antidepressants combined with zinc caused decreased depressive symptoms than antidepressants alone in randomized control trials [21].
Novel Sources
Binding Assays
Phenotypic Screening
| Explanation | Pros and/or Cons/Ref | |||||
|---|---|---|---|---|---|---|
| Common Approaches | Computational Approaches | Signature Matching | Transcriptomic, Metabolomics, and Proteomics | Transcriptomic | Comparison of Gene Expression in Healthy, Disease-Associated and Medication-Using State | Pros: finding new targets or off-target effects for existing medications [10], finding the new mechanism of action for drugs, involving more genetic level mechanisms in comparison to knowledge-based methods [25,32], low costs, public access to databases [23] Cons: medication-target genes not getting expressed in altered patterns and not being detectable [33] |
| Metabolomics | Recognizing potentially druggable targets in different diseases | Pros: involving more molecular level mechanisms in comparison to knowledge-based methods [25] | ||||
| Proteomics | Applying interaction between medication and proteome | Pros: gaining information about safety, probable medication toxicity, mode of action of small molecule medications [12], involving more genetic and/or molecular level mechanisms in comparison to knowledge-based methods, finding new mechanisms of action [25,32] | ||||
| Chemical structure | Developing networks based on shared chemical features | Cons: the difference between actual results and expectations, variety of physiological effects despite structure resemblance [10], possibility of happening alterations in structure due to biological activity [16] | ||||
| Adverse event profile | Finding shared targets, proteins, or pathways affected by different medications showing the same adverse effects | Pros: unlike animal models, both therapeutic and adverse effects are observable in humans [15] Cons: problems in extracting information on medication package inserts, lack of proper adverse event profile and causality assessment [10] | ||||
| Computational molecular | Testing different medications on a known target (conventional docking) or checking different targets | Pros: the ability to test all compounds with recognized structure [25] | ||||
| Docking | Match a particular medication (inverse docking) based on complementarity between ligand on target | Cons: difficulty in providing a 3D image of G-protein receptors, lack of eligible database providing appropriate information about targets’ structures, the difference between actual affinity between ligand and target and virtual results, different outcomes of different software packages [10], impossibility of identifying unknown mechanism beyond the known target in conventional docking [25] | ||||
| Genome-wide associated data (GWAS) | Finding genetic variants associated with common diseases and understanding the biology of disease | Pros: advances in technology, the accomplishment of the HGP, reduction in genotyping costs Cons: need for studies to assure in which direction gene variants affect disease, difficulty in identification responsible gene or gene variants due to linkage disequilibrium in gene-rich loci, not providing a comprehensive insight into disease pathophysiology, lack of definite knowledge of the human genome and the possibility of new human genes discovery [10], disease’s complicated genetic basis due to polygenic nature of illness [25] | ||||
| Pathway or network mapping | Building networks for disease or medication based on signature matching data, gene expression pattern, disease pathology, GWAS data, or protein interactions | Pros: narrowing the range of molecules from a large number to few targets [12] | ||||
| Experimental approaches | Retrospective clinical analysis | Electronic health records (EHRs) | Reviewing and extracting data from structured (diagnosis and pathophysiology data, laboratory test results, and medication prescriptions) and unstructured (of patients’ symptoms reports and imaging data) | Pros: easy access to different resources such as WHO or FAERS database and ability to analyze these data [10], discovering adverse events that were not noticed during drug development by applying Natural Language to EHRs [2] Cons: ethical and legal obstacles, challenges in extracting unstructured data [1] | ||
| Post-marketing surveillance and clinical data | Analyzing post-marketing surveillance and clinical data to extract information | Cons: restriction in accessing to these data due to commercial and ethical reasons [1] | ||||
| Novel sources | Using immortalized human CCLs for screening different compounds, linking EHR data to DNA bank to identify an association between patients’ genome and patients’ illness, using patients’ online self-reported data while taking medicine | Pros: development of sequencing technologies, which helps ones collect more thorough information on each patient’s genetics (2), acceleration in the drug discovery process, reduction in research costs, increase in patient involvement, ability to assess the effectiveness of the in-use medication (3) Cons: Happening alterations that make in vitro results better (1), challenges in using big data and technology for analysis (2), bias in collecting data, threat in patients’ safety in case of self-prescription (3) [10] | ||||
| Binding assays | Realizing interactions between target and ligand by using different methods as chromatography and mass spectroscopy | - | ||||
| Phenotypic screening | Identifying compounds showing disease consequences related effects in model systems, without any prior information about targets | Pros: testing many medications for a therapeutic effect over a complete range of concentration [34], high flexibility for administration to numerous drugs or diseases [32] Cons: not reaching a complete picture by in vitro assays [33] | ||||
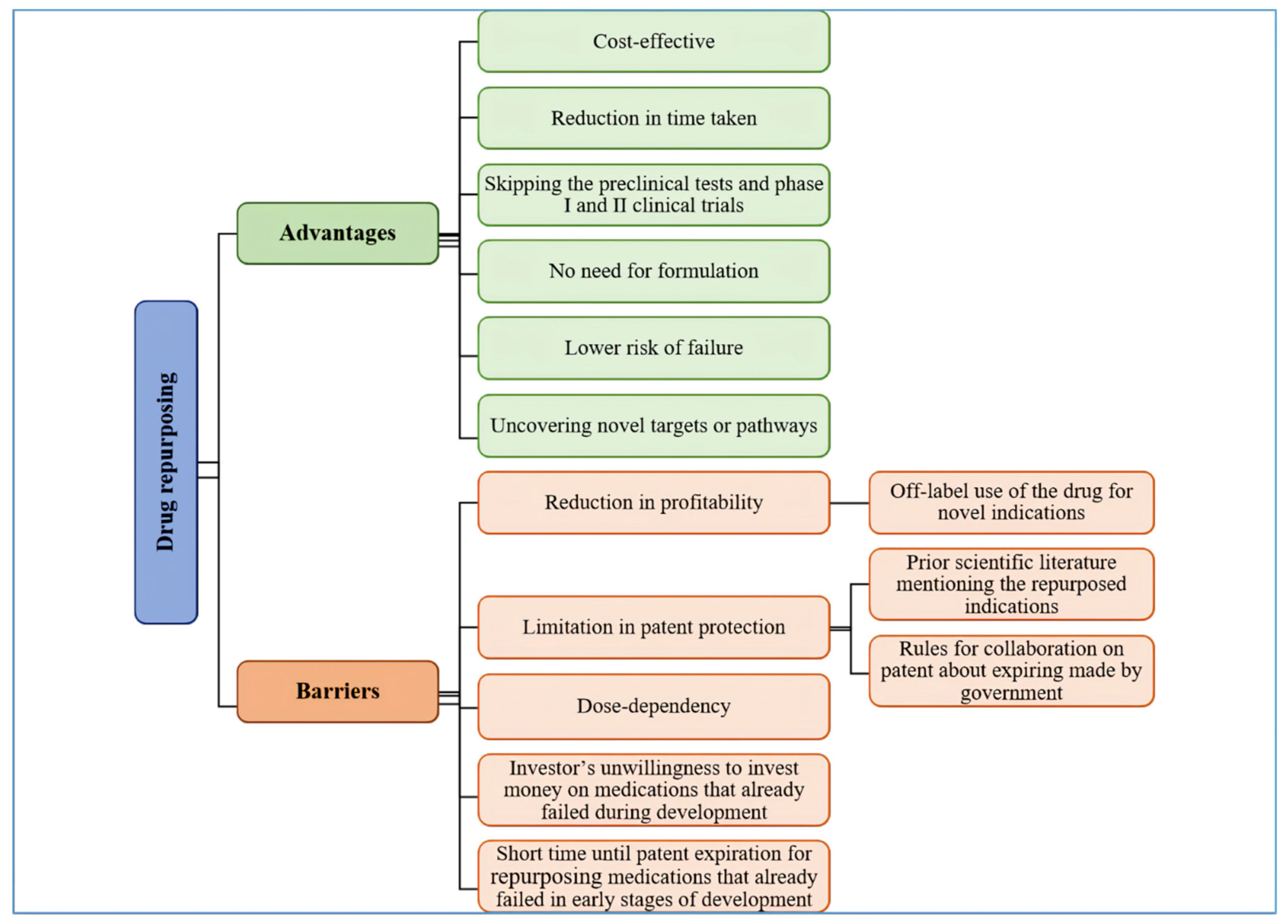
2.4. Advantages
2.5. Barriers
| Medication Name | Repurposing Approach/Ref | New Indication Suggested by Article, or Investigational/FDA Approved/Ref |
|---|---|---|
| Atypical antipsychotics Quetiapine Aripiprazole Brexpiprazole | Retrospective clinical analysis (PM surveillances and CD) [13] | MDD, BP1 depressive episodes (FA) [8] |
| NA | MDD (FA) [9] | |
| NA | MDD (FA) [35] | |
| Mecamylamine | Computational molecular docking [23] | Depression (SA) [23], MDD (INV) [17,19,20,36,37] |
| Cyproheptadine | Computational molecular docking [26] | NA |
| Dextromethorphan | Computational molecular docking [13] | MDD (INV) [38,39,40,41] |
| Pregabalin | GWAS [23] | MDD (SA) [23] |
| Gabapentin | GWAS [23] | MDD (SA) [23] |
| Cycloserine | GWAS [23] | BP depression (INV) [42], MDD (SA, INV) [23,36] |
| Risperidone | GWAS [23] | Extrapyramidal symptoms, suicidal ideation (INV) [43] |
| Cannabidiol | Pathway or network mapping [21] | MDD (SA) [21] |
| N-acetyl-l-cysteine | Pathway or network mapping [21] | MDD (SA) [21] |
| Sho-saiko-to | Pathway or network mapping [21] | NA |
| Spermine | Pathway or network mapping [21] | TRD (SA) [21] |
| Nimodipine | Pathway or network mapping [21] | Vascular depression in old patients (SA) [13] |
| Scopolamine | GWAS, Pathway or network mapping [13] | MDD (INV) [44,45] |
| Anti-inflammatory medications | Retrospective clinical analysis (PM surveillances and CD) [13] | NA |
| Valproic acid | Retrospective clinical analysis (PM surveillances and CD) [13] | Resistant depression (SA) [13] |
| Zinc | Retrospective clinical analysis (PM surveillances and CD) [21] | MDD (INV) [46] |
| Pramipexole | Retrospective clinical analysis (EHRs) [21] | MDD (SA, INV) [21,47] |
| Telmisartan | Retrospective clinical analysis (EHRs) [21] | MDD (SA) [21] |
| Metformin | Retrospective clinical analysis (EHRs) [26] | MDD (INV) [48] |
| Phenothiazines | Retrospective clinical analysis (PM surveillances and CD) [26] | NA |
| Cabergoline | Signature matching (adverse event profile) [15] | NA |
| Modafinil | Signature matching (adverse event profile) [15] | MDD (INV) [49], depressive episode in BP1 disorder (INV) [50], major depressive episode in BP1 disorder (INV) [51] |
| Pergolide | Signature matching (adverse event profile) [15] | NA |
| Phenytoin | Signature matching (adverse event profile) [15] | NA |
| Chlorcyclizine | Signature matching (chemical structure) [26] | NA |
| Vorinostat | Signature matching (transcriptomic) [26] | Depression, anxiety, schizophrenia (SA) [26] |
| Statins | Signature matching (transcriptomic) [21] | NA |
| Ketamine (esketamine) | Signature matching (transcriptomic) [13] | MDD and bipolar depression, Depressive symptoms in adults with MDD with acute suicidal ideation or behavior (FA) [52] |
| Pioglitazone | Signature matching (transcriptomic) [13] | MDD, a major depressive episode in bipolar disorder (SA) [13] |
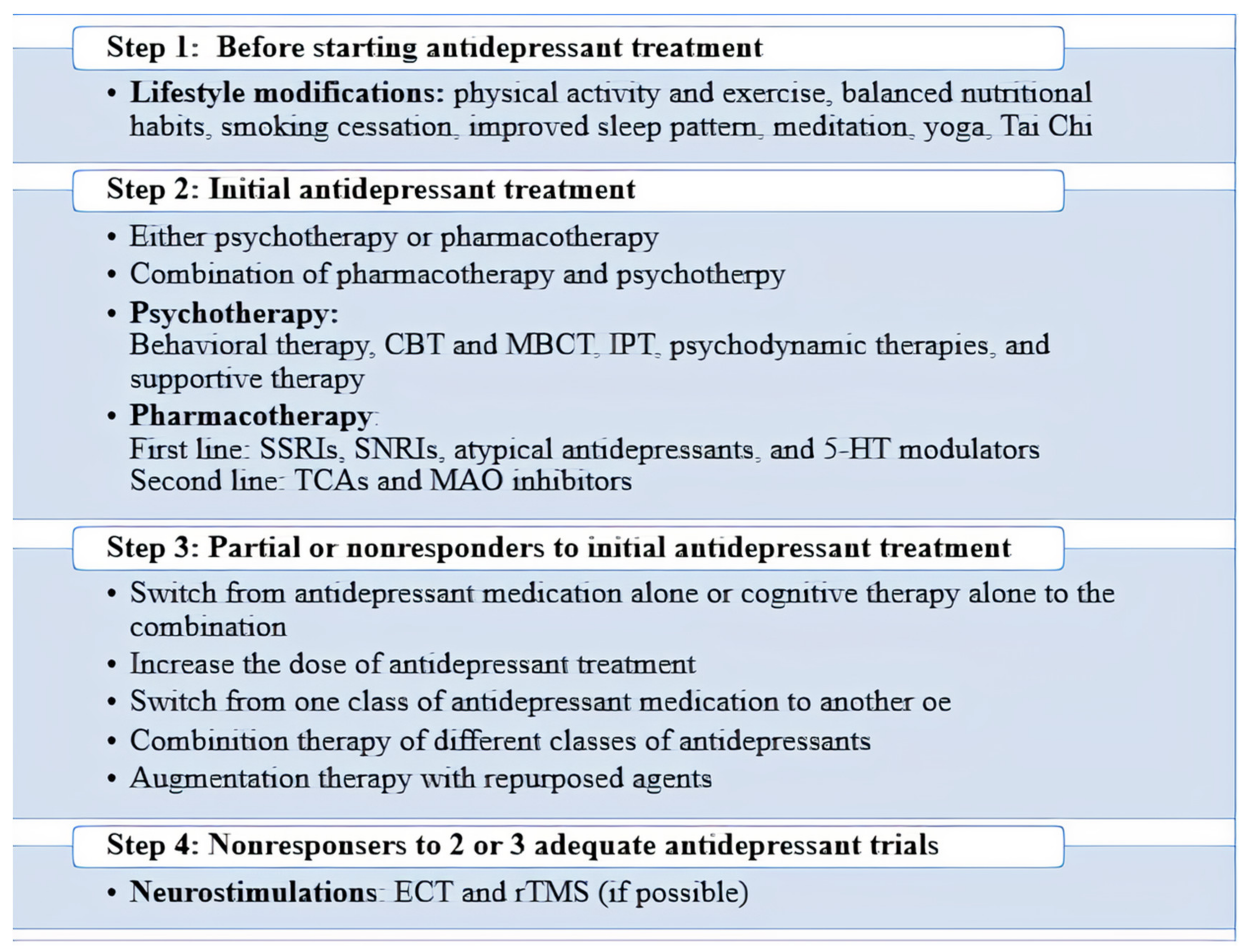
3. Management of Depression
3.1. Pharmacotherapy
3.1.1. Current Antidepressant Medications
3.1.2. Repurposed Drugs for MDD
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Novac, N. Challenges and opportunities of drug repositioning. Trends Pharmacol. Sci. 2013, 34, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Ashburn, T.T.; Thor, K.B. Drug repositioning: Identifying and developing new uses for existing drugs. Nat. Rev. Drug Discov. 2004, 3, 673–683. [Google Scholar] [CrossRef]
- Xue, H.; Li, J.; Xie, H.; Wang, Y. Review of Drug Repositioning Approaches and Resources. Int. J. Biol. Sci. 2018, 14, 1232–1244. [Google Scholar] [CrossRef]
- Pillaiyar, T.; Meenakshisundaram, S.; Manickam, M.; Sankaranarayanan, M. A medicinal chemistry perspective of drug repositioning: Recent advances and challenges in drug discovery. Eur. J. Med. Chem. 2020, 195, 112275. [Google Scholar] [CrossRef] [PubMed]
- Dudley, J.T.; Deshpande, T.; Butte, A.J. Exploiting drug-disease relationships for computational drug repositioning. Brief. Bioinform. 2011, 12, 303–311. [Google Scholar] [CrossRef]
- Depression. Available online: https://www.who.int/health-topics/depression#tab=tab_1 (accessed on 22 June 2021).
- Little, A. Treatment-resistant depression. Am. Fam. Physician 2009, 80, 167–172. [Google Scholar] [PubMed]
- Baune, B.T.; Smith, E.; Reppermund, S.; Air, T.; Samaras, K.; Lux, O.; Brodaty, H.; Sachdev, P.; Trollor, J.N. Inflammatory biomarkers predict depressive, but not anxiety symptoms during aging: The prospective Sydney Memory and Aging Study. Psychoneuroendocrinology 2012, 37, 1521–1530. [Google Scholar] [CrossRef]
- Taylor, C.; Fricker, A.D.; Devi, L.A.; Gomes, I. Mechanisms of action of antidepressants: From neurotransmitter systems to signaling pathways. Cell. Signal. 2005, 17, 549–557. [Google Scholar] [CrossRef]
- Pushpakom, S.; Iorio, F.; Eyers, P.A.; Escott, K.J.; Hopper, S.; Wells, A.; Doig, A.; Guilliams, T.; Latimer, J.; McNamee, C.; et al. Drug repurposing: Progress, challenges and recommendations. Nat. Rev. Drug Discov. 2019, 18, 41–58. [Google Scholar] [CrossRef]
- Henriksen, K.; Christiansen, C.; Karsdal, M.A. Serological biochemical markers of surrogate efficacy and safety as a novel approach to drug repositioning. Drug Discov. Today 2011, 16, 967–975. [Google Scholar] [CrossRef]
- Pulley, J.M.; Rhoads, J.P.; Jerome, R.N.; Challa, A.P.; Erreger, K.B.; Joly, M.M.; Lavieri, R.R.; Perry, K.E.; Zaleski, N.M.; Shirey-Rice, J.K.; et al. Using What We Already Have: Uncovering New Drug Repurposing Strategies in Existing Omics Data. Annu. Rev. Pharmacol. Toxicol. 2020, 60, 333–352. [Google Scholar] [CrossRef]
- Ebada, M.E. Drug repurposing may generate novel approaches to treating depression. J. Pharm. Pharmacol. 2017, 69, 1428–1436. [Google Scholar] [CrossRef]
- Caban, A.; Pisarczyk, K.; Kopacz, K.; Kapuśniak, A.; Toumi, M.; Rémuzat, C.; Kornfeld, A. Filling the gap in CNS drug development: Evaluation of the role of drug repurposing. J. Mark. Access Health Policy 2017, 5, 1299833. [Google Scholar] [CrossRef]
- Yang, L.; Agarwal, P. Systematic drug repositioning based on clinical side-effects. PLoS ONE 2011, 6, e28025. [Google Scholar] [CrossRef] [PubMed]
- Ko, Y. Computational Drug Repositioning: Current Progress and Challenges. Appl. Sci. 2020, 10, 5076. [Google Scholar] [CrossRef]
- Otte, C.; Gold, S.M.; Penninx, B.W.; Pariante, C.M.; Etkin, A.; Fava, M.; Mohr, D.C.; Schatzberg, A.F. Major depressive disorder. Nat. Rev. Dis. Primers 2016, 2, 1–20. [Google Scholar] [CrossRef]
- Koda-Kimble, M.A.; Young, L.Y. (Eds.) Applied Therapeutics: The Clinical Use of Drugs, 7th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2001. [Google Scholar]
- Block, S.G.; Nemeroff, C.B. Emerging antidepressants to treat major depressive disorder. Asian J. Psychiatry 2014, 12, 7–16. [Google Scholar] [CrossRef]
- Molero, P.; Ramos-Quiroga, J.; Martin-Santos, R.; Calvo-Sánchez, E.; Gutiérrez-Rojas, L.; Meana, J. Antidepressant efficacy and tolerability of ketamine and esketamine: A critical review. CNS Drugs 2018, 32, 411–420. [Google Scholar] [CrossRef]
- Fabbri, C.; Kasper, S.; Zohar, J.; Souery, D.; Montgomery, S.; Albani, D.; Forloni, G.; Ferentinos, P.; Rujescu, D.; Mendlewicz, J.; et al. Drug repositioning for treatment-resistant depression: Hypotheses from a pharmacogenomic study. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 104, 110050. [Google Scholar] [CrossRef]
- Kraus, C.; Wasserman, D.; Henter, I.D.; Acevedo-Diaz, E.; Kadriu, B.; Zarate, C.A., Jr. The influence of ketamine on drug discovery in depression. Drug Discov. Today 2019, 24, 2033–2043. [Google Scholar] [CrossRef] [PubMed]
- Shukla, R.; Henkel, N.D.; Alganem, K.; Hamoud, A.-r.; Reigle, J.; Alnafisah, R.S.; Eby, H.M.; Imami, A.S.; Creeden, J.F.; Miruzzi, S.A.; et al. Signature-based approaches for informed drug repurposing: Targeting CNS disorders. Neuropsychopharmacology 2021, 46, 116–130. [Google Scholar] [CrossRef]
- Arakelyan, A.; Nersisyan, L.; Nikoghosyan, M.; Hakobyan, S.; Simonyan, A.; Hopp, L.; Loeffler-Wirth, H.; Binder, H. Transcriptome-Guided Drug Repositioning. Pharmaceutics 2019, 11, 677. [Google Scholar] [CrossRef]
- Park, K. A review of computational drug repurposing. Transl. Clin. Pharm. 2019, 27, 59–63. [Google Scholar] [CrossRef]
- Zhao, K.; So, H.C. Drug Repositioning for Schizophrenia and Depression/Anxiety Disorders: A Machine Learning Approach Leveraging Expression Data. IEEE J. Biomed. Health Inform. 2019, 23, 1304–1315. [Google Scholar] [CrossRef]
- Troisi, J.; Cavallo, P.; Colucci, A.; Pierri, L.; Scala, G.; Symes, S.; Jones, C.; Richards, S. Chapter Three-Metabolomics in genetic testing. In Advances in Clinical Chemistry; Makowski, G.S., Ed.; Elsevier: Amsterdam, The Netherlands, 2020; Volume 94, pp. 85–153. [Google Scholar]
- Robertson, D.G.; Frevert, U. Metabolomics in drug discovery and development. Clin. Pharmacol. Ther. 2013, 94, 559–561. [Google Scholar] [CrossRef]
- Gligorijević, V.; Malod-Dognin, N.; Pržulj, N. Integrative methods for analyzing big data in precision medicine. Proteomics 2016, 16, 741–758. [Google Scholar] [CrossRef]
- Hurle, M.R.; Yang, L.; Xie, Q.; Rajpal, D.K.; Sanseau, P.; Agarwal, P. Computational drug repositioning: From data to therapeutics. Clin. Pharmacol. Ther. 2013, 93, 335–341. [Google Scholar] [CrossRef]
- Hodos, R.A.; Kidd, B.A.; Shameer, K.; Readhead, B.P.; Dudley, J.T. In silico methods for drug repurposing and pharmacology. Wiley Interdiscip. Rev. Syst. Biol. Med. 2016, 8, 186–210. [Google Scholar] [CrossRef]
- Jin, G.; Wong, S.T. Toward better drug repositioning: Prioritizing and integrating existing methods into efficient pipelines. Drug Discov. Today 2014, 19, 637–644. [Google Scholar] [CrossRef]
- Alaimo, S.; Pulvirenti, A. Network-Based Drug Repositioning: Approaches, Resources, and Research Directions. Methods Mol. Biol. 2019, 1903, 97–113. [Google Scholar] [CrossRef]
- Parvathaneni, V.; Kulkarni, N.S.; Muth, A.; Gupta, V. Drug repurposing: A promising tool to accelerate the drug discovery process. Drug Discov. Today 2019, 24, 2076–2085. [Google Scholar] [CrossRef]
- Otsuka Beijing Research Institute. The Safety and Efficacy of Brexpiprazole as Adjunctive Therapy in the Treatment of Major Depressive Disorder. Available online: https://ClinicalTrials.gov/show/NCT03487198 (accessed on 3 June 2021).
- Salvadore, G.; Singh, J.B. Ketamine as a fast-acting antidepressant: Current knowledge and open questions. CNS Neurosci. Ther. 2013, 19, 428–436. [Google Scholar] [CrossRef]
- A Study to Assess the Efficacy and Safety of TC-5214 as an Adjunct Therapy in Patients With Major Depressive Disorder (MDD). Available online: https://ClinicalTrials.gov/show/NCT01157078 (accessed on 22 June 2021).
- Medical University of South Carolina. A Trial of Dextromethorphan for Treatment of Major Depressive Disorder. Available online: https://ClinicalTrials.gov/show/NCT02860962 (accessed on 3 June 2021).
- Axsome Therapeutics, Inc. Assessing Symptomatic Clinical Episodes in Depression. Available online: https://ClinicalTrials.gov/show/NCT03595579 (accessed on 3 June 2021).
- Axsome Therapeutics, Inc. A Trial of AXS-05 in Patients With Major Depressive Disorder. Available online: https://ClinicalTrials.gov/show/NCT04019704 (accessed on 3 June 2021).
- Axsome Therapeutics, Inc. Open-Label Safety Study of AXS-05 in Subjects With Depression. Available online: https://ClinicalTrials.gov/show/NCT04039022 (accessed on 3 June 2021).
- Drevets, W.C.; Zarate, C.A., Jr.; Furey, M.L. Antidepressant effects of the muscarinic cholinergic receptor antagonist scopolamine: A review. Biol. Psychiatry 2013, 73, 1156–1163. [Google Scholar] [CrossRef]
- O’Connor, R.M.; Grenham, S.; Dinan, T.G.; Cryan, J.F. microRNAs as novel antidepressant targets: Converging effects of ketamine and electroconvulsive shock therapy in the rat hippocampus. Int. J. Neuropsychopharmacol. 2013, 16, 1885–1892. [Google Scholar] [CrossRef]
- The Taub Group. The Safety and Efficacy of Naltrexone and Scopolamine Utilized in the Treatment of Major Depression. Available online: https://ClinicalTrials.gov/show/NCT03386448 (accessed on 3 June 2021).
- Capital Medical University. Effectiveness Study of Scopolamine Combined with Escitalopram in Patients With MDD. Available online: https://ClinicalTrials.gov/show/NCT03131050 (accessed on 3 June 2021).
- Unipolar Major Depression in Adults: Choosing Initial Treatment. Available online: https://www.uptodate.com/contents/unipolar-major-depression-in-adults-choosing-initial-treatment#H51 (accessed on 20 June 2021).
- New York State Psychiatric Institute; Columbia University; Research Foundation for Mental Hygiene, Inc.; Mclean Hospital; Icahn School of Medicine at Mount Sinai; National Institute of Mental Health (NIMH). Imaging Dopamine Release in Depression. Available online: https://ClinicalTrials.gov/show/NCT02033369 (accessed on 3 June 2021).
- Sadat City University. The Antidiabetic Metformin as a Novel Adjunct to Antidepressants in Major Depressive Disorder Patients. Available online: https://ClinicalTrials.gov/show/NCT04088448 (accessed on 3 June 2021).
- De Assis Lima, I.V.; Almeida-Santos, A.F.; Ferreira-Vieira, T.H.; Aguiar, D.C.; Ribeiro, F.M.; Campos, A.C.; de Oliveira, A.C.P. Antidepressant-like effect of valproic acid—Possible involvement of PI3K/Akt/mTOR pathway. Behav. Brain Res. 2017, 329, 166–171. [Google Scholar] [CrossRef]
- Guo, M.; Mi, J.; Jiang, Q.M.; Xu, J.M.; Tang, Y.Y.; Tian, G.; Wang, B. Metformin may produce antidepressant effects through improvement of cognitive function among depressed patients with diabetes mellitus. Clin. Exp. Pharmacol. Physiol. 2014, 41, 650–656. [Google Scholar] [CrossRef]
- Study to Evaluate the Efficacy and Safety of Armodafinil Treatment as Adjunctive Therapy in Adults With Major Depression Associated With Bipolar I Disorder. Available online: https://ClinicalTrials.gov/show/NCT01072630 (accessed on 22 June 2021).
- US Food and Drug Administration. Esketamine Nasal Spray. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/211243lbl.pdf (accessed on 5 June 2021).
- Zeind, C.S.; Carvalho, M.G. Applied Therapeutics: The Clinical Use of Drugs; Wolters Kluwer Health: Philadelphia, PA, USA, 2017. [Google Scholar]
- Katzung, B.G. Basic and Clinical Pharmacology, 14th ed.; McGraw-Hill Education: New York, NY, USA, 2017. [Google Scholar]
- Kole, M.H.; Swan, L.; Fuchs, E. The antidepressant tianeptine persistently modulates glutamate receptor currents of the hippocampal CA3 commissural associational synapse in chronically stressed rats. Eur. J. Neurosci. 2002, 16, 807–816. [Google Scholar] [CrossRef]
- Bortolato, B.; Miskowiak, K.W.; Köhler, C.A.; Maes, M.; Fernandes, B.S.; Berk, M.; Carvalho, A.F. Cognitive remission: A novel objective for the treatment of major depression? BMC Med. 2016, 14, 9. [Google Scholar] [CrossRef]
- Camargo, A.; Rodrigues, A.L.S. Novel targets for fast antidepressant responses: Possible role of endogenous neuromodulators. Chronic Stress 2019, 3, 2470547019858083. [Google Scholar] [CrossRef]
- Aripiprazole (Short-Acting Oral and Injectable and Long-Acting Injectable [Abilify Maintena]): Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=aripiprazole-short-acting-oral-and-injectable-and-long-acting-injectable-abilify-maintena-drug-information (accessed on 4 June 2021).
- US Food and Drug Administration. Brexanolone. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/211371lbl.pdf (accessed on 5 June 2021).
- Brexpiprazole: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=brexpiprazole-drug-information (accessed on 4 June 2021).
- Cabergoline: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=cabergoline-drug-information (accessed on 10 June 2021).
- US Food and Drug Administration. Epidiolex. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/210365lbl.pdf (accessed on 5 June 2021).
- Celecoxib: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=celecoxib-drug-information (accessed on 4 June 2021).
- Cycloserine: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=cycloserine-drug-information#F155547 (accessed on 22 June 2021).
- Cyproheptadine: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=cyproheptadine-drug-information (accessed on 4 June 2021).
- Dextromethorphan: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=dextromethorphan-drug-information (accessed on 4 June 2021).
- Etanercept (Including Biosimilars of Etanercept): Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=etanercept-drug-information (accessed on 4 June 2021).
- Gabapentin: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=gabapentin-drug-information (accessed on 22 June 2021).
- Infliximab (Including Biosimilars of Infliximab): Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=infliximab-including-biosimilars-of-infliximab-drug-information (accessed on 4 June 2021).
- Ketamine: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=ketamine-drug-information (accessed on 4 June 2021).
- Liothyronine: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=liothyronine-drug-information (accessed on 4 June 2021).
- Lisdexamfetamine: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=lisdexamfetamine-drug-information (accessed on 4 June 2021).
- Lithium: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=lithium-drug-information (accessed on 4 June 2021).
- Metformin: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=metformin-drug-information (accessed on 4 June 2021).
- Mecamylamine: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=mecamylamine-drug-information (accessed on 22 June 2021).
- Minocycline: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=minocycline-drug-information (accessed on 4 June 2021).
- Modafinil: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=modafinil-drug-information (accessed on 10 June 2021).
- US Food and Drug Administration. PROVIGIL® (Modafinil). Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2007/020717s020s013s018lbl.pdf (accessed on 10 June 2021).
- Acetylcysteine: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=acetylcysteine-drug-information (accessed on 4 June 2021).
- Nimodipine: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=nimodipine-drug-information (accessed on 4 June 2021).
- Olanzapine: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=olanzapine-drug-information (accessed on 4 June 2021).
- US Food and Drug Administration. Permax® Pergolide Mesylate. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2003/19385slr030,031,035_permax_lbl.pdf (accessed on 10 June 2021).
- Pioglitazone: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=pioglitazone-drug-information (accessed on 4 June 2021).
- Phenytoin: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=phenytoin-drug-information (accessed on 10 June 2021).
- Pramipexole: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=pramipexole-drug-information (accessed on 4 June 2021).
- Pregabalin: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=pregabalin-drug-information (accessed on 22 June 2021).
- Quetiapine: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=quetiapine-drug-information (accessed on 4 June 2021).
- Risperidone: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=risperidone-drug-information (accessed on 4 June 2021).
- Rosiglitazone: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=rosiglitazone-drug-information (accessed on 4 June 2021).
- Scopolamine (Hyoscine) (Systemic): Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=scopolamine-hyoscine-systemic-drug-information (accessed on 4 June 2021).
- Lovastatin: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=lovastatin-drug-information (accessed on 4 June 2021).
- Telmisartan: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=telmisartan-drug-information (accessed on 4 June 2021).
- Valproate: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=valproate-drug-information (accessed on 4 June 2021).
- Vorinostat: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=vorinostat-drug-information (accessed on 4 June 2021).
- US Food and Drug Administration. Zolinza (Vorinostat) Capsules Label. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/021991s002lbl.pdf (accessed on 8 June 2021).
- Zinc Acetate: Drug Information. Available online: https://uptodatefree.ir/topic.htm?path=zinc-acetate-drug-information (accessed on 4 June 2021).
- VA Puget Sound Health Care System. Ketamine Anesthesia for Improvement of Depression in ECT. Available online: https://ClinicalTrials.gov/show/NCT02752724 (accessed on 3 June 2021).
- Sunnybrook Health Sciences Centre. Effect of Ketamine vs. Active Placebo on Suicidal Ideation in Depressed Inpatients with Major Depressive Disorder or Bipolar Depression. Available online: https://ClinicalTrials.gov/show/NCT02593643 (accessed on 3 June 2021).
- St Patrick’s Hospital. Ketamine as an Adjunctive Therapy for Major Depression. Available online: https://ClinicalTrials.gov/show/NCT03256162 (accessed on 3 June 2021).
- Shalvata Mental Health Center. Intra-Nasal vs. Intra-Venous Ketamine Administration. Available online: https://ClinicalTrials.gov/show/NCT02644629 (accessed on 3 June 2021).
- Massachusetts General Hospital; Brain & Behavior Research Foundation; National Institutes of Health. Ketamine for Depression: An MRI Study. Available online: https://ClinicalTrials.gov/show/NCT02544607 (accessed on 3 June 2021).
- Sheba Medical Center. Ketamine IV Classic Protocol: Five Years Follow Up. Available online: https://ClinicalTrials.gov/show/NCT04824157 (accessed on 3 June 2021).
- Yale University. Cognitive Therapy to Sustain the Antidepressant Effects of Intravenous Ketamine in Treatment-Resistant Depression. Available online: https://ClinicalTrials.gov/show/NCT03027362 (accessed on 3 June 2021).
- Novartis Pharmaceuticals; Novartis. Proof of Concept Study Evaluating the Efficacy and Safety of MIJ821 in Patients with Treatment-Resistant Depression. Available online: https://ClinicalTrials.gov/show/NCT03756129 (accessed on 3 June 2021).
- NeuroRx, Inc.; Massachusetts General Hospital; Target Health Inc. Sequential Therapy for the Treatment of Severe Bipolar Depression. Available online: https://ClinicalTrials.gov/show/NCT02974010 (accessed on 3 June 2021).
- Intra-Cellular Therapies, Inc. Clinical Trial Evaluating ITI-007 as an Adjunctive Therapy to Lithium or Valproate for the Treatment of Bipolar Depression. Available online: https://ClinicalTrials.gov/show/NCT02600507 (accessed on 3 June 2021).
- Heintjes, E.M.; Overbeek, J.A.; Penning-van Beest, F.J.; Brobert, G.; Herings, R.M. Post authorization safety study comparing quetiapine to risperidone and olanzapine. Hum. Psychopharmacol. 2016, 31, 304–312. [Google Scholar] [CrossRef]
- Otsuka Pharmaceutical Development & Commercialization, Inc. Exploratory Trial to Assess the Functionality of an Integrated Call Center for the Digital Medicine System. Available online: https://ClinicalTrials.gov/show/NCT02722967 (accessed on 3 June 2021).
- Duke University; Forest Laboratories; Institute for Advanced Medical Research. Levomilnacipran ER vs. Adjunctive Quetiapine for Adults with Inadequate Relief with SSRIs in MDD. Available online: https://ClinicalTrials.gov/show/NCT02720198 (accessed on 3 June 2021).
- Janssen Research & Development, LLC. A Study to Compare the Efficacy, Safety, and Tolerability of JNJ-42847922 Versus Quetiapine Extended-Release as Adjunctive Therapy to Antidepressants in Adult Participants With Major Depressive Disorder Who Have Responded Inadequately to Antidepressant Therapy. Available online: https://ClinicalTrials.gov/show/NCT03321526 (accessed on 3 June 2021).
- Whitton, A.E.; Reinen, J.M.; Slifstein, M.; Ang, Y.S.; McGrath, P.J.; Iosifescu, D.V.; Abi-Dargham, A.; Pizzagalli, D.A.; Schneier, F.R. Baseline reward processing and ventrostriatal dopamine function are associated with pramipexole response in depression. Brain J. Neurol. 2020, 143, 701–710. [Google Scholar] [CrossRef]
- Frye, M.A.; Amchin, J.; Bauer, M.; Adler, C.; Yang, R.; Ketter, T.A. Randomized, placebo-controlled, adjunctive study of armodafinil for bipolar I depression: Implications of novel drug design and heterogeneity of concurrent bipolar maintenance treatments. Int. J. Bipolar Disord. 2015, 3, 34. [Google Scholar] [CrossRef][Green Version]
- Ketter, T.A.; Yang, R.; Frye, M.A. Adjunctive armodafinil for major depressive episodes associated with bipolar I disorder. J. Affect. Disord. 2015, 181, 87–91. [Google Scholar] [CrossRef]
- Calabrese, J.R.; Frye, M.A.; Yang, R.; Ketter, T.A. Efficacy and safety of adjunctive armodafinil in adults with major depressive episodes associated with bipolar I disorder: A randomized, double-blind, placebo-controlled, multicenter trial. J. Clin. Psychiatry 2014, 75, 1054–1061. [Google Scholar] [CrossRef]
- Allama Iqbal Open University Islamabad; King Edward Medical University. Role of Omega-3 Polyunsaturated Fatty Acid in the Management of Major Depressive Disorder. Available online: https://ClinicalTrials.gov/show/NCT03732378 (accessed on 3 June 2021).
- China Medical University Hospital; National Science Council of Taiwan. Omega-3 Polyunsaturated Fatty Acids on Major Depressive Disorder in Patients With Cardiovascular Diseases. Available online: https://ClinicalTrials.gov/show/NCT03072823 (accessed on 3 June 2021).
- Janssen Research & Development, LLC. 54135419SUI3001: A Study to Evaluate the Efficacy and Safety of Intranasal Esketamine in Addition to Comprehensive Standard of Care for the Rapid Reduction of the Symptoms of Major Depressive Disorder, Including Suicidal Ideation, in Adult Participants Assessed to be at Imminent Risk for Suicide. Available online: https://clinicaltrials.gov/ct2/show/NCT03039192 (accessed on 3 June 2021).
- Fu, D.J.; Ionescu, D.F.; Li, X.; Lane, R.; Lim, P.; Sanacora, G.; Hough, D.; Manji, H.; Drevets, W.C.; Canuso, C.M. Esketamine Nasal Spray for Rapid Reduction of Major Depressive Disorder Symptoms in Patients Who Have Active Suicidal Ideation With Intent: Double-Blind, Randomized Study (ASPIRE I). J. Clin. Psychiatry 2020, 81. [Google Scholar] [CrossRef]
- Janssen Research & Development, LLC. 54135419SUI3002: A Study to Evaluate the Efficacy and Safety of Intranasal Esketamine in Addition to Comprehensive Standard of Care for the Rapid Reduction of the Symptoms of Major Depressive Disorder, Including Suicidal Ideation, in Adult Participants Assessed to be at Imminent Risk for Suicide. Available online: https://ClinicalTrials.gov/show/NCT03097133 (accessed on 3 June 2021).
- Ionescu, D.F.; Fu, D.J.; Qiu, X.; Lane, R.; Lim, P.; Kasper, S.; Hough, D.; Drevets, W.C.; Manji, H.; Canuso, C.M. Esketamine Nasal Spray for Rapid Reduction of Depressive Symptoms in Patients With Major Depressive Disorder Who Have Active Suicide Ideation With Intent: Results of a Phase 3, Double-Blind, Randomized Study (ASPIRE II). Int. J. Neuropsychopharmacol. 2021, 24, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Celon Pharma SA; National Center for Research and Development. Efficacy, Safety and Pharmacokinetic Study of Inhaled Esketamine in Treatment-resistant Depression. Available online: https://ClinicalTrials.gov/show/NCT03965858 (accessed on 3 June 2021).
- A Study to Evaluate the Effects of a Single-Dose and Repeat-Administration of Intranasal Esketamine on On-Road Driving in Participants With Major Depressive Disorder. Available online: https://ClinicalTrials.gov/show/NCT02919579 (accessed on 3 June 2021).
- JNJ-54135419 (Esketamine). Available online: https://s3.amazonaws.com/ctr-jnj-7051/CR108228/d2a59202-2675-439e-a1f3-fe2d4c870cd2/f0a86e38-1c8c-495d-8394-7a6a46291e9c/CR108228_CSR_Synopsis-v1.pdf (accessed on 3 June 2021).
- Efficacy and Safety of AXS-05, an Oral NMDA Receptor Antagonist with Multimodal Activity, in Major Depressive Disorder: Results from the GEMINI Trial. Available online: https://d3dyybxyjb4kyh.cloudfront.net/pdfs/APA+2021+GEMINI+poster+3_31_21+FINAL.pdf (accessed on 3 June 2021).
- Efficacy and Safety of AXS-05, an Oral NMDA Receptor Antagonist with Multimodal Activity, in Major Depressive Disorder: Results from the ASCEND Trial. Available online: https://d3dyybxyjb4kyh.cloudfront.net/pdfs/APA+2021+ASCEND+poster+3_31_21+FINAL.pdf (accessed on 3 June 2021).
- Sustained Efficacy and Long-Term Safety of AXS-05, an Oral NMDA Receptor Antagonist, in Major Depressive Disorder: COMET Study Results. Available online: https://d3dyybxyjb4kyh.cloudfront.net/pdfs/APA+2021+COMET+poster+3_31_21+FINAL.pdf (accessed on 3 June 2021).
- Meyer, J.; Centre for Addiction and Mental Health. New Treatment Approach for Major Depressive Disorder Based Upon Targeting Monoamine Oxidase A (MAO-A). Available online: https://ClinicalTrials.gov/show/NCT02269540 (accessed on 3 June 2021).
- Meyer, J.; Centre for Addiction and Mental Health. Biomarkers of Neuroinflammation and Anti-Inflammatory Treatments in Major Depressive Disorder. Available online: https://ClinicalTrials.gov/show/NCT02362529 (accessed on 3 June 2021).
- Charite University. Adjunct Minocycline in Treatment-Resistant Depression. Available online: https://ClinicalTrials.gov/show/NCT02456948 (accessed on 3 June 2021).
- Mineralocorticoid Receptor, NMDA Receptor and Cognitive Function in Depression. Available online: https://ClinicalTrials.gov/show/NCT03062150 (accessed on 22 June 2021).
- Nowacki, J.; Wingenfeld, K.; Kaczmarczyk, M.; Chae, W.R.; Abu-Tir, I.; Deuter, C.E.; Piber, D.; Hellmann-Regen, J.; Otte, C. Cognitive and emotional empathy after stimulation of brain mineralocorticoid and NMDA receptors in patients with major depression and healthy controls. Neuropsychopharmacology 2020, 45, 2155–2161. [Google Scholar] [CrossRef]
- A Study to Assess the Efficacy and Safety of TC-5214 as an Adjunct Therapy in Patients With Major Depressive Disorder. Available online: https://ClinicalTrials.gov/show/NCT01197508 (accessed on 22 June 2021).
- Möller, H.J.; Demyttenaere, K.; Olausson, B.; Szamosi, J.; Wilson, E.; Hosford, D.; Dunbar, G.; Tummala, R.; Eriksson, H. Two Phase III randomised double-blind studies of fixed-dose TC-5214 (dexmecamylamine) adjunct to ongoing antidepressant therapy in patients with major depressive disorder and an inadequate response to prior antidepressant therapy. World. J. Biol. Psychiatry 2015, 16, 483–501. [Google Scholar] [CrossRef]
- Vieta, E.; Thase, M.E.; Naber, D.; D’Souza, B.; Rancans, E.; Lepola, U.; Olausson, B.; Szamosi, J.; Wilson, E.; Hosford, D.; et al. Efficacy and tolerability of flexibly-dosed adjunct TC-5214 (dexmecamylamine) in patients with major depressive disorder and inadequate response to prior antidepressant. Eur. Neuropsychopharmacol. 2014, 24, 564–574. [Google Scholar] [CrossRef]
- A Study to Assess the Long-Term Safety of TC-5214 as an Adjunct Therapy in Patients With Major Depressive Disorder. Available online: https://ClinicalTrials.gov/show/NCT01152554 (accessed on 22 June 2021).
- Tummala, R.; Desai, D.; Szamosi, J.; Wilson, E.; Hosford, D.; Dunbar, G.; Eriksson, H. Safety and tolerability of dexmecamylamine (TC-5214) adjunct to ongoing antidepressant therapy in patients with major depressive disorder and an inadequate response to antidepressant therapy: Results of a long-term study. J. Clin. Psychopharmacol. 2015, 35, 77–81. [Google Scholar] [CrossRef]
| Medication/Bioactive Compound Brand Name/ Ref | US-FDA Approval | Pharmacological Category/Mechanism of Action | Dosage | Significant Adverse Effects | Contraindications |
|---|---|---|---|---|---|
| Aripiprazole Abilify® [58] | Bipolar disorder, irritability associated with autistic disorder, MDD, TRD, schizophrenia, Tourette disorder | Partial agonist at the D2 and 5-HT1A receptors, an antagonist at the 5-HT2A/Second-generation (atypical) antipsychotic | MDD and TRD as an adjunctive treatment. Oral: 2 to 5 mg/day | >10%: decreased HDL-C, increased LDL-C, increased serum cholesterol, increased serum TG, weight gain, akathisia, headache, increased serum glucose, constipation, nausea, and vomiting | Hypersensitivity to aripiprazole or any component of the formulation |
| Increase dose based on response in 5 mg increments up to a maximum of 15–20 mg/day | |||||
| Brexanolone Zulresso® [59] | Postpartum depression (PPD) in adults | The mechanism of action is not fully understood, but is thought to be related to its positive allosteric modulation of GABAA receptors/GABAA receptor-positive modulator | Postpartum depression. IV: 0 to 4 h: 30 mcg/kg/h 4 to 24 h: 60 mcg/kg/h 24 to 52 h: 90 (or 60) mcg/kg/h 52 to 56 h: 60 mcg/kg/h 56 to 60 h: 30 mcg/kg/hour | >5%: sedation/somnolence, dry mouth, loss of consciousness, and flushing/hot flush | No contraindications were listed in the US-FDA monograph |
| Brexpiprazole Rexulti® [60] | MDD, schizophrenia | Partial agonist activity for 5-HT1A and D2 receptors and antagonist activity for 5-HT2A receptors/Second-generation (atypical) antipsychotic | MDD as an adjunct therapy to antidepressants. Oral: 0.5 mg or 1 mg once daily; titrate to 1 mg once daily, followed by 2 mg once daily; maximum daily dose: 3 mg | >10%: increased serum TG, weight gain, akathisia | Hypersensitivity (e.g., anaphylaxis, facial swelling, rash, urticarial) to brexpiprazole or any component of the formulation |
| Cabergoline Dostinex® [61] | Hyperprolactinemic disorders | Long-acting dopamine receptor agonist with a high affinity for D2 receptors, a potent 5-HT2B-receptor agonist/Ergot derivative | NA | Headache, dizziness, nausea | Known hypersensitivity to cabergoline, ergot derivatives, or any component of the formulation, uncontrolled hypertension; history of cardiac valvular disorders, history of pulmonary, pericardial, or retroperitoneal fibrotic disorders |
| Cannabidiol Epidiolex® [62] | Treatment of seizures associated with Lennox-Gastaut syndrome or Dravet syndrome in patients with 2 years of age and older | The precise mechanisms of its anticonvulsant effect in humans are unknown; however, it does not appear to exert its effects through interaction with cannabinoid receptors/Anticonvulsant, cannabinoid | NA | >10%: somnolence, decreased appetite, diarrhea, transaminase elevations, fatigue, malaise and asthenia, rash, insomnia, sleep disorder and poor quality sleep, infections | Hypersensitivity to cannabidiol or any of the ingredients in Epidiolex® |
| Celecoxib CeleBREX® [63] | Acute pain, ankylosing spondylitis, juvenile idiopathic arthritis, osteoarthritis, primary dysmenorrhea, rheumatoid arthritis | Inhibits prostaglandin synthesis by decreasing COX-2 enzyme/Analgesic, nonopioid, NSAID, COX-2 selective | NA | Serious cardiovascular thrombotic events, myocardial infarction, and stroke increased the risk of serious gastrointestinal adverse events, including bleeding, ulceration, and perforation of the stomach or intestines | Hypersensitivity to celecoxib, sulfonamides, aspirin, other NSAIDs, or any component of the formulation |
| Cycloserine Seromycin® [64] | Tuberculosis, UTI | Inhibits bacterial cell wall synthesis by competing with amino acid (D-alanine) for incorporation into the bacterial cell wall/Antibiotic, antitubercular agent | NA | Cardiac arrhythmia, cardiac failure, coma, confusion, dizziness, drowsiness, dysarthria, headache, hyperreflexia, paresis, paresthesia, psychosis, restlessness, seizure, vertigo, skin rash, cyanocobalamin deficiency, folate deficiency, increased liver enzymes, hypersensitivity reaction, tremor | Hypersensitivity to cycloserine or any component of the formulation, epilepsy, depression, severe anxiety, or psychosis, severe renal insufficiency, excessive concurrent use of alcohol |
| Cyproheptadine Euro-Cyproheptadine®, PMS-Cyproheptadine® [65] | Allergic conditions | Potent antihistamine and serotonin antagonist with anticholinergic effects competes with histamine H1 receptors/First, generation histamine H1 antagonist, a piperidine derivative | NA | Extrasystole, hypotension, palpitations, tachycardia, ataxia, chills, confusion, dizziness, drowsiness, euphoria, excitement, fatigue, hallucination, headache, hysteria, insomnia, irritability, nervousness, neuritis, paresthesia, restlessness, sedation, seizure, vertigo, etc. | MAO inhibitor therapy, close angle glaucoma, stenosing peptic ulcer, symptomatic prostatic hypertrophy, bladder neck obstruction, pyloroduodenal obstruction, elderly, debilitated patients |
| Dextromethorphan Buckleys cough®, Creomulsion adult®, Cough DM®, Delsym®, etc. [66] | Cough suppressant | Decreases the sensitivity of cough receptors and interrupts cough impulse transmission by depressing the medullary cough center through sigma receptor stimulation/Antitussive, NMDA receptor antagonist | NA | Dizziness, drowsiness, nervousness, restlessness, gastrointestinal distress, nausea, stomach pain, vomiting | Concurrent administration with or within two weeks of discontinuing MAO inhibitor |
| Esketamine Spravato® [52] | TRD, MDD with suicidality | Nonselective, noncompetitive NMDA receptor antagonist/NMDA receptor antagonist | TRD. Intranasal: induction: 56 mg (may increase to 84 mg) twice weekly for 4 weeks Maintenance: on week 5, the previously established dose (56 or 84 mg) once weekly—on week 9 and onward continue effective dose (56 to 84 mg) once weekly or every 2 weeks MDD with suicidality. Intranasal: 84 mg twice weekly for 4 weeks; may reduce dosage to 56 mg twice weekly | >5%: dissociation, dizziness, nausea and vomiting, sedation, vertigo, hypoesthesia, anxiety, lethargy, increased blood pressure, feeling drunk | Hypersensitivity to esketamine, ketamine, or any of the excipients, Aneurysmal vascular disease or arteriovenous malformation, intracerebral hemorrhage |
| Etanercept Enbrel®, Erelzi®, Brenzys® [67] | Ankylosing spondylitis, plaque psoriasis, polyarticular juvenile idiopathic arthritis, psoriatic arthritis, rheumatoid arthritis | Binds TNF-α and blocks its interaction with cell surface receptors/Antirheumatic, disease-modifying, TNF-α blocking agent | NA | >10%: skin rash, diarrhea, positive ANA titer, antibody development, infection, injection site reaction, respiratory tract infections | Sepsis, hypersensitivity to etanercept, or any component of the formulation |
| Gabapentin Fanatrex FusePaq®, Gralise®, Gralise Starter®, Neuraptine®, Neurontin® [68] | Postherpetic neuralgia, seizures | Modulates the release of excitatory neurotransmitters which participate in epileptogenesis and nociception/Anticonvulsant, GABA analog | NA | >10%: dizziness, drowsiness, ataxia, fatigue, viral infections | Hypersensitivity to gabapentin or any component of the formulation |
| Infliximab Avsola®, Inflectra®, Remicade®, Renflexis® [69] | Ankylosing spondylitis, Crohn disease, plaque psoriasis, psoriatic arthritis, rheumatoid arthritis, ulcerative colitis | Binds to human TNF-α and interfere with endogenous TNF-α activity/Antirheumatic, disease-modifying, gastrointestinal agent, immunosuppressant agent, monoclonal antibody, TNF-α blocking agent | NA | >10%: abdominal pain, nausea, anemia, increased ALT, antibody development, increased ANA titer, abscess, infection, headache, cough, pharyngitis, sinusitis | Hypersensitivity to infliximab, murine proteins, or any component of the formulation |
| Ketamine Ketalar® [70] | Induction and maintenance of general anesthesia | Noncompetitive NMDA receptor antagonist (blocks glutamate)/General anesthetic | Depressive episodes and MDD. IV: 0.5 mg/kg administered over 40 min; 1 to 3 times weekly; may increase dose to 0.75 to 1 mg/kg. Treatment up to 6 weeks (optimal duration of therapy is unknown) | >10%: prolonged emergence from anesthesia (includes confusion, delirium, dreamlike state, excitement, hallucinations, irrational behavior, vivid imagery) | Hypersensitivity to ketamine or any component of the formulation, conditions in which an increase in blood pressure would be hazardous |
| Liothyronine Cytomel®, Triostat® [71] | Thyroid disorders, a myxedema coma | Manufactured form of the thyroid hormone triiodothyronine (T3) and exerts its many metabolic effects through control of DNA transcription and protein synthesis/Thyroid product | Antidepressant augmentation. Oral: 25 mcg/day; may be increased to 50 mcg/day after ~1 week. Dose ranges of 20 to 62.5 mcg/day have been studied in clinical trials. | 1% to 10%: cardiac arrhythmia, tachycardia, hypotension, myocardial infraction | Hypersensitivity to liothyronine sodium or any component of the formulation, uncorrected adrenal insufficiency, untreated thyrotoxicosis, concurrent use with artificial rewarming of the patient |
| Lisdexamfetamine Vyvanse® [72] | ADHD, binge eating disorder | Converts to the active component dextroamphetamine, a noncatecholamine, sympathomimetic amines that cause a release of dopamine and NE from their storage sites/Central nervous system stimulant | NA | >10%: insomnia, decreased appetite, xerostomia, upper abdominal pain | Hypersensitivity to amphetamine products or any component of the formulation, concurrent use of MAO inhibitor, or within 14 days of the last MAO inhibitor dose |
| Lithium Lithobid® [73] | Bipolar disorder | Influence the reuptake of serotonin and/or NE and inhibit 2nd messenger systems involving phosphatidylinositol cycle, increasing glutamate clearance, enhancing the expression of neurotrophic factors (BDNF)/Antimanic agent | MDD and TRD as an adjunctive treatment. Oral: 300 to 600 mg/day in 1 to 2 divided doses; may increase every 1 to 5 days to a target dose of 600 mg to 1.2 g/day in divided doses. Clinical improvement may take up to 6 weeks. | The most significant adverse reaction is lithium toxicity; signs: diarrhea, vomiting, drowsiness, muscular weakness, and lack of coordination | Hypersensitivity to lithium or any component of the formulation |
| Metformin D-Care DM2®, Fortamet®, Glucophage®, Glumetza®, Riomet® [74] | Type 2 diabetes mellitus | Decreases hepatic glucose production, reduces intestinal absorption of glucose and improve insulin sensitivity, increases peripheral glucose uptake and utilization/Antidiabetic agent, biguanide | NA | >10%: diarrhea, flatulence, nausea and vomiting, dyspepsia, abdominal pain, lactic acidosis, vitamin B12 deficiency | Hypersensitivity to metformin or any component of the formulation, severe renal dysfunction, metabolic acidosis |
| Mecamylamine Vecamyl® [75] | Hypertension | Inhibits acetylcholine at the autonomic ganglia/Ganglionic blocking agent | NA | Orthostatic hypotension, syncope altered mental status, convulsions, fatigue, paresthesia, sedation decreased libido, anorexia, constipation, glossitis, intestinal obstruction, nausea, vomiting, xerostomia, urinary retention, tremor, weakness, blurred vision, mydriasis, pulmonary edema, pulmonary fibrosis | Hypersensitivity to mecamylamine or any component of the formulation; mild, moderate, labile hypertension, coronary insufficiency or recent myocardial infarction, uremia, glaucoma, organic pyloric stenosis, coadministration with antibiotics or sulfonamides |
| Minocycline CoreMino®, Minocin®, Minolira®, Solodyn®, Ximino® [76] | Different types of infections, acne, etc. | Inhibits bacterial protein synthesis by binding with the 30S and possibly the 50S ribosomal subunit/Antibiotic, tetracycline derivative | NA | 1% to 10%: pruritus, urticaria, dizziness, fatigue, malaise, drowsiness, arthralgia, tinnitus | Hypersensitivity to minocycline, other tetracyclines, or any component of the formulation |
| Modafinil Provigil®, Alertec® [77,78] | Narcolepsy, obstructive sleep apnea, shift work sleep disorder | Increase dopamine in the brain by blocking dopamine transporters/Central nervous system stimulant | Antidepressant augmentation for MDD. Oral: 100 mg/day for 3 to 7 days, then increase to 200 mg/day; further, adjust dose based on response and tolerability up to 400 mg/day. | Headache, nausea, nervousness, rhinitis, diarrhea, back pain, anxiety, insomnia, dizziness, dyspepsia | Contraindicated in patients with known hypersensitivity to modafinil, armodafinil or its inactive ingredients |
| N-acetyl cysteine Acetadote®, Cetylev®, Parvolex® [79] | Acetaminophen overdose, mucolytic | Restoring hepatic glutathione, serving as a glutathione substitute, exerts mucolytic effects through its free sulfhydryl group, which opens up the disulfide bonds in the mucoproteins/Antidote, mucolytic agent | NA | >10%: autoimmune disease, anaphylactoid reaction | Hypersensitivity to acetylcysteine or any component of the formulation |
| Nimodipine Nymalize®, Nimotop® [80] | Subarachnoid hemorrhage | Inhibits calcium ion from entering the slow channels/Calcium channel blocker, dihydropyridine | NA | 1% to 10%: decrease blood pressure, bradycardia, headache, nausea | Concomitant use with potent CYP3A4 inhibitors |
| Olanzapine ZyPREXA® [81] | Acute agitation/aggression associated with psychiatric disorders, bipolar disorder, unipolar MDD, TRD, schizophrenia | Combination of dopamine and serotonin type 2 receptor antagonism/Antimanic agent, second-generation (atypical) antipsychotic | MDD and psychotic depression as an adjunctive therapy. Oral: 5 mg once daily; may increase the dose in increments of 5 mg up to 20 mg/day. TRD as an adjunctive therapy. Oral: 5 mg once daily; may increase dose up to 20 mg/day. | Postural hypotension, constipation, weight gain, dizziness, personality disorder, akathisia, sedation, headache, increased appetite, abdominal pain, pain in extremity, fatigue, dry mouth, asthenia, drowsiness, tremor | No contraindication with ZyPREXA® monotherapy, caution in combination therapy with fluoxetine, lithium or valproate |
| A fixed-dose of olanzapine/fluoxetine combination may be used instead of separate components. | |||||
| Pergolide Permax®, Prascend® [82] | Adjunctive treatment to levodopa/carbidopa in the management of the signs and symptoms of Parkinson’s disease | Potent dopamine receptor agonist/Ergot derivative | NA | Dyskinesia, hallucinations, somnolence, insomnia, nausea, constipation, diarrhea, dyspepsia, rhinitis | Hypersensitive to pergolide mesylate or other ergot derivatives |
| Pioglitazone Actos® [83] | Type 2 diabetes mellitus | Improving target cell response to insulin, a potent and selective agonist for PPARγ/Antidiabetic agent, thiazolidinedione | NA | >10%: edema, hypoglycemia, upper respiratory tract infection | Hypersensitivity to pioglitazone or any component of the formulation, NYHA class III/IV heart failure |
| Phenytoin Dilantin®, Phenytek® [84] | Seizures (non-emergent use), status epilepticus | Stabilizes neuronal membranes and decreases seizure activity by modulating efflux or influx of sodium, shortens action potential in the heart/Anticonvulsant, hydantoin | NA | Nystagmus, ataxia, slurred speech, decreased coordination, somnolence, mental confusion | Hypersensitivity to phenytoin, other hydantoins, or any component of the formulation, concurrent use of delavirdine, history of prior acute hepatotoxicity attributable to phenytoin |
| Pramipexole Mirapex® [85] | Parkinson disease, restless legs syndrome | Nonergot dopamine agonist with specificity for the D2 subfamily dopamine receptor. Additionally, it binds to D3 and D4 receptors/Anti-parkinson agent, dopamine agonist | NA | >10%: orthostatic hypotension, drowsiness, extrapyramidal reaction, insomnia, dizziness, hallucination, headache, restless leg syndrome, abnormal dreams, nausea, constipation, dyskinesia, asthenia, accidental injury | Parkinson disease, restless legs syndrome |
| Pregabalin Lyrica®, Lyrica CR® [86] | Fibromyalgia, neuropathic pain associated with diabetic peripheral neuropathy or spinal cord injury, partial-onset seizures, postherpetic neuralgia | modulates calcium influx at the nerve terminals, thereby inhibits excitatory neurotransmitter release, may also affect descending noradrenergic and serotonergic pain transmission pathways from the brainstem to the spinal cord/Anticonvulsant, GABA analog | NA | Peripheral edema, Dizziness, drowsiness, headache, fatigue, weight gain, xerostomia, visual field loss, blurred vision | Hypersensitivity (e.g., angioedema) to pregabalin or any component of the formulation |
| Quetiapine SEROquel® [87] | Bipolar disorder, unipolar MDD schizophrenia | Antipsychotic activity through a combination of dopamine type 2 (D2) and serotonin type 2 (5-HT2) antagonism/Second-generation (atypical) antipsychotic | MDD or nonpsychotic depression as an adjunctive therapy. Oral: 50 mg/day on days 1 and 2; increase to 150 mg/day on day 3. Usual dosage range: 150 to 300 mg/day. | >10%: increased blood pressure, orthostatic hypotension, tachycardia, decreased HDL-C, increased serum cholesterol, increased serum TG, weight gain | Hypersensitivity to quetiapine or any component of the formulation |
| Doses up to 600 mg/day may be needed in psychotic depression. Nonpsychotic depression, monotherapy. Oral: 20 mg once daily; may be gradually increased up to 300 mg/day. | |||||
| Risperidone Perseris®, RisperDAL®, RisperiDONE® [88] | Bipolar disorder, schizophrenia, bipolar mania, irritability associated with autistic disorder | High 5-HT2 and dopamine-D2 receptor antagonist activity/Antimanic agent, second-generation (atypical) antipsychotic | MDD and TRD, as an adjunctive therapy. Oral: 0.25 to 0.5 mg/day; may increase dose in increments of 0.25 to 1 mg/day every 3 to 7 days up to 3 mg/day. Usual effective dose: 1 to 1.5 mg/day. | Activating/sedating effects, angioedema, dyslipidemia, extrapyramidal symptoms, hematologic abnormalities, hyperglycemia, weight gain, hyperprolactinemia, neuroleptic malignant syndrome, orthostatic hypotension, QT prolongation, sexual dysfunction, temperature dysregulation | Hypersensitivity to risperidone, paliperidone, or any component of the formulation |
| Rosiglitazone Avandia® [89] | Type 2 diabetes mellitus | Improving target cell response to insulin, a potent and selective agonist for PPARγ/Antidiabetic agent, thiazolidinedione | NA | >10%: increased HDL-C, increased LDL-C, increased total serum cholesterol, weight gain | Hypersensitivity to rosiglitazone or any component of the formulation; NYHA class III/IV heart failure |
| Scopolamine (hyoscine) Transderm Scop®, Buscopan® [90] | Prevention of nausea and vomiting associated with motion sickness, recovery from anesthesia, and surgery | Blocks the action of acetylcholine; increases cardiac output, dries secretions, antagonizes histamine and serotonin/anticholinergic agent | NA | >10%: drowsiness, dizziness, xerostomia | Hypersensitivity to scopolamine, other belladonna alkaloids, or any component of the formulation, narrow-angle glaucoma |
| Statins, for example,Lovastatin Altoprev®, Mevacor® [91] | Adjunctive therapy to diet to reduce elevated total cholesterol, LDL cholesterol, Apo B and TG and to increase HDL-C in patients with primary hypercholesterolemia | competitively blocking the active site of HMG-CoA reductase/Antilipemic agent, HMG-CoA reductase inhibitor | NA | >10%: Increased creatine phosphokinase | Hypersensitivity to lovastatin or any component of the formulation, active liver disease or unexplained persistent elevations of serum transaminases, concomitant use of potent CYP3A4 inhibitors |
| Telmisartan Micardis® [92] | Cardiovascular risk reduction, hypertension | Nonpeptide AT1 angiotensin II receptor antagonist/Angiotensin II receptor blocker, antihypertensive | NA | 1% to 10%: intermittent claudication, chest pain, hypertension, peripheral edema, dizziness, fatigue, headache, pain, dermal ulcer, diarrhea, abdominal pain, dyspepsia, nausea, UTI, back pain, myalgia, upper respiratory tract infection, sinusitis, cough, flu-like symptoms, pharyngitis | Known hypersensitivity (e.g., anaphylaxis, angioedema) to telmisartan or any component of the formulation, concurrent use of aliskiren in patients with diabetes |
| Valproic acid [93] | Bipolar disorder, focal (partial) onset and generalized onset seizures, migraine prophylaxis | Increased availability and enhance the action of GABA, blocks voltage-dependent Na channels/Anticonvulsant, antimanic agent, histone deacetylase inhibitor | NA | >10: headache, drowsiness, dizziness, insomnia, pain, nervousness, alopecia, nausea and vomiting, abdominal pain, diarrhea, dyspepsia, anorexia, thrombocytopenia, infections, tremor, weakness, diplopia, visual disturbance, flu-like symptoms, accidental injury | Hypersensitivity to valproic acid, divalproex, derivatives, or any component of the formulation, hepatic disease, urea cycle disorders, mitochondrial disorders caused by mutations in mitochondrial DNA |
| Vorinostat Zolinza® [94,95] | Cutaneous T-cell lymphoma | Inhibits HDAC enzymes, HCAC1, HDAC2, HDAC3, and HDAC6, which catalyze acetyl group removal from protein lysine residues/Antineoplastic agent, histone deacetylase inhibitor | NA | >10%: peripheral edema, fatigue, chills, dizziness, headache, alopecia, pruritus, hyperglycemia, weight loss, dehydration, diarrhea, nausea, dysgeusia, anorexia, xerostomia, constipation, vomiting, decreased appetite, proteinuria, thrombocytopenia, anemia, muscle spasm, increased serum creatinine, cough, fever, upper respiratory tract infection | Severe hepatic impairment |
| Zinc Galzin®, Wilzin® [96] | Wilson disease | Induces production of the copper-binding protein metallothionein in enterocytes/Chelating agent | NA | Gastric irritation increased serum amylase, increased serum lipase, increased serum ALP | Hypersensitivity to zinc acetate or any component of the formulation |
| Treatment (Tₓ) Phase/Year First, Posted Ref | Dosage (Duration of Therapy) | Subjects/F/M Condition Groups | Study Design | Results | Non-Serious AEs (Treatment-Related) | Serious AEs (Treatment-Related) |
|---|---|---|---|---|---|---|
| General anesthetics | ||||||
| Ketamine NA/2016 [97] | Experimental: 1 mg/kg IV ketamine for the duration of their ECT index course over 2–3 weeks Active comparator: 1 mg/kg of IV methohexital for the duration of their ECT index course over 2–3 weeks | 52/NA/NA MDD | R, PG, DB | NA | NA | NA |
| Ketamine Early phase I/2015 [98] | Experimental: ketamine + TAU Active comparator: midazolam + TAU | 9/NA/NA MDD, BP1 disorder, BP2 disorder, BP depression, suicidal ideation | R, PG, DB | NA | NA | NA |
| Ketamine Phase I/2017 [99] | Experimental: 4 ketamine infusions at 0.05 mg/kg—once weekly Active comparator: 4 infusions at 0.045 mg/kg—once weekly | 25/NA/NA A major depressive episode, unipolar depression, BP depression | R, PG, QB | NA | NA | NA |
| Ketamine Phase IV/2016 [100] | Placebo: saline 0.9%, IV administration of 0.2 mg/kg or 50 mg Medication: ketamine (1st phase) IV administration of 0.2 mg/kg or 50 mg Medication: ketamine (2nd phase) additional 4 sessions (twice a week, 2 weeks) of 0.5 mg/kg over 40 min | 45/NA/NA MDD | R, PG, QB | NA | NA | NA |
| Ketamine Phase IV/2015 [101] | Medication: ketamine 0.5 mg/kg over 40 min IV Other: MRI technology will be used before and after ketamine for patients with depression | 16/8/8 MDD, anxious depression, depression | SG, OL | NA | None | Not reported |
| Ketamine NA/2021 [102] | Received IV ketamine in 2014–15 and will be evaluated in 5 years | 11/NA/NA/ MDD, medication abuse, medications, relapse | Retrospective | NA | NA | NA |
| Ketamine NA/2017 [103] | Experimental: ketamine and 16 CBT sessions over 14 weeks Active comparator: ketamine and psychoeducation all sessions over 14 weeks | 28/NA/NA MDD | R, PG, SB | NA | NA | NA |
| Ketamine Phase II/2018 [104] | Experimental: different dosages and regimens for MIJ821 Active comparator: ketamine infusion 0.5 mg/kg weekly Placebo Comparator: placebo infusion | 70/35/35 TRD | R, PG, DB | NA | None | Hyperacusis, photophobia, vision blurred, dry mouth, nausea, fatigue, feeling of relaxation, gait disturbance, increased systolic blood pressure, decreased platelet count, dizziness, dysgeusia, headache, paresthesia, sciatica, somnolence, anxiety, depersonalization/derealization disorder, disinhibition, irritability, alopecia, pruritus |
| Ketamine Phase II/2016 [105] | Experimental: NRX-101 oral capsule + ketamine IV infusion + saline solution IV infusion Active comparator: lurasidone oral capsule + ketamine IV infusion + saline solution IV infusion | 22/16/6 BP depression, suicidal ideation, suicide attempts | R, SG, QB | NA | None | Angina pectoris, tinnitus, vision blurred, diarrhea, dry mouth, coordination abnormal, dizziness, dysmetropsia, hypoesthesia, sedation, restlessness, depression, suicidal ideation, acute kidney injury, dry skin, hypertension |
| Antimanic agents | ||||||
| Lithium Phase III/2015 [106] | Experimental: 40 mg ITI-007 administered orally as capsules once daily for 6 weeks Experimental: 60 mg ITI-007 administered orally as capsules once daily for 6 weeks Placebo Comparator: placebo administered orally as visually-matched capsules once daily for 6 weeks | 529/NA/NA BD | R, PG, QB | NA | NA | NA |
| Risperidone 2011 [68,107] | Groups: olanzapine users, quetiapine users, risperidone users, all other antipsychotic users | 17743/9692/8051 SCH = 475 MDD = 798 BP disorder = 270 Generalized anxiety disorder = 17 Other mental health disorders = 637 Unknown indication = 15546 Quetiapine = 4658 Olanzapine = 5856 Risperidone = 7229 | Observational, cohort, retrospective | Comparison between quetiapine and olanzapine: quetiapine is associated with lower extrapyramidal symptoms and diabetes mellitus Comparison between quetiapine and risperidone: quetiapine is associated with lower extrapyramidal symptoms, but higher failed suicide attempt rates | NA | NA |
| Atypical antipsychotics | ||||||
| Aripiprazole Phase II/2016 [108] | Oral tablet (2,5,10,15,20, or 30 mg) with an IEM QD (8 weeks) | 49/31/18 BP1 (n = 22) SCH (n = 15) MDD (n = 12) Tx = 49 | SG, OL, multi-center | NA | Rash, erythema, pruritus skin irritation, upper respiratory tract infection, sinusitis, headache, syncope, meniscus injury, sunburn, peripheral swelling, pain in extremity | Not reported |
| Quetiapine Phase III/2016 [109] | Active comparator: levomilnacipran ER 20–120 mg/d starting at 20 mg/d on days 1–2, 40 mg/d on days 3–7 in week 1, then between 40–120 mg/d during weeks 2–8 Active comparator: 1uetiapine XR 50 mg/d on day 1–2, 150 mg/d on days 3–7 in week 1, then between 150–300 mg/d during weeks 1–8 along with their current antidepressant | 60/NA/NA MDD | R, PG, TB | NA | NA | NA |
| Quetiapine Phase II/2017 [110] | Experimental: 1 capsule of 20 mg JNJ-42847922 and 1 capsule of placebo once daily for 14 days. Then, JNJ-42847922 dose can be increased to 40 mg (2 capsules) until day 167 Active comparator: 1 capsule of quetiapine XR 50 mg along with 1 capsule of placebo once daily for 2 days, followed by 1 capsule of 150 mg along with 1 capsule of placebo once daily from day 3–14. Then, the dose can be increased to 300 mg (2 capsules) until day 167. | 107/NA/NA MDD | R, PG, DB | NA | NA | NA |
| Patients should continue to take their baseline SSRI/SNRI. | ||||||
| Brexpiprazole Phase III/2018 [35] | Experimental: brexpiprazole, 2–3 mg/day, once daily for 6 weeks, oral administration Placebo Comparator: placebo, 2–3 mg/day, once daily for 6 weeks, oral administration | 65/NA/NA MDD | R, PG, TB | NA | NA | NA |
| Dopamine agonists | ||||||
| Pramipexole Phase IV/2014 [47,111] | Started at 0.125 mg BD PO and increased by 0.25 mg/day every 3–4 days to a target range of 1.0–2.5 mg/day (6 weeks) | 51/25/26 MDD (n = 26) Healthy (n = 25) Healthy control patients did not receive study medication and only have baseline measures | Non-randomized, PG, OL | Symptom’s improvement | Nausea, heartburn, vomiting, ↑appetite, ↓appetite, diarrhea, constipation, somnolence, restlessness, insomnia, forgetfulness, sleep attacks, compulsive behaviors, impaired concentration, headache, lightheadedness, dizziness, dry mouth, fatigue, ↓ libido, sexual dysfunction, skin problems, sweating, impaired coordination, tremor, blurry vision, bruising | Not reported |
| Armodafinil Phase III/2011 [50,112] | Tablet, PO, QD in the morning, started at 50 mg/day; the dosage was increased by 50 mg/day on days 2 and 4, up to 150 mg/day. (8 weeks) | 399/241/158 depressive episode despite maintenance therapy for BP1 disorder P = 199 Tx = 200 | R, PG, DB, PC, multi-center | ↓Severity of depression, ↓depressive symptoms, Improved functioning | Headache, nausea | Anxiety, BP1 disorder, depression, insomnia, suicide attempt, cholecystitis chronic, social stay hospitalization |
| Armodafinil Phase III/2010 [51,113] | Tablet, PO, QD in the morning, started at 50 mg/kg and titrated up in the first week to 150 or 200 mg/kg. Treatment with 200 mg/kg dose was discontinued via a protocol amendment. (8 weeks) | 492/273/219 major depressive episode despite BP1 disorder maintenance therapy P = 230 Tx (150 mg/kg) = 232 Tx (200 mg/kg) = 30 | R, PG, DB, PC, multi-center | ↓ Depressive symptoms | Nausea, diarrhea, dry mouth, toothache, dyspepsia, headache, dizziness, insomnia, anxiety, suicidal ideation, nasopharyngitis, cough | Mania, psychotic disorder, suicidal ideation, pulmonary embolism, abortion spontaneous, accidental overdose, non-cardiac chest pain, coronary artery disease |
| Armodafinil Phase III/2010 [49,114] | Tablet, PO, QD in the morning, started at 50 mg/kg and titrated up in the first week to 150 or 200 mg/kg. Treatment with 200 mg/kg dose was discontinued via a protocol amendment. (8 weeks) | 433/288/145 major depressive episode while taking at least 4 weeks of conventional maintenance medication P = 199 Tx (150 mg/kg) =201 Tx (200 mg/kg) =33 | R, PG, DB, PC, multi-center | Improvement in depressive symptoms | Diarrhea, nausea, headache, migraine, insomnia, feeling jittery | Psychotic disorder, suicidal ideation, depressive symptom, aggression, acute hepatic failure, hepatitis acute |
| Modafinil with D-cycloserine (DCS) Phase III/2015 [7] | 250 mg DCS before two weekly sessions, 100 mg modafinil before two weekly sessions | 36/20/14/2 (transgender) MDD P = 11 Tx (modafinil) = 12 Tx (DCS) = 13 | R, PG, DB, PC | NA | ↑Energy/concentration, fatigue/low motivation | Not reported |
| Supplementation | ||||||
| Omega-3 PUFA Not applicable/2018 [115] | One capsule (EPA 300 mg and 200 mg DHA) QD were given antidepressant (citalopram, escitalopram, paroxetine 1 tablet at night time). (12 weeks) | 70/NA/NA Taking antidepressants P = NA Tx = NA | R, PG, SB, PC | NA | NA | NA |
| n-3 Polyunsaturated fatty acid Not applicable/2017 [116] | 2 g of EPA and 1 g of DHA (12 weeks) | 60/NA/NA MDD and cardiovascular disease P = NA Tx = NA | R, PG, DB, PC | NA | NA | NA |
| Zinc Not applicable/2020 [46] | Oral 30 mg zinc sulfate QD with SSRIs (8 weeks) | 100/NA/NA MDD P = 50 Tx = 50 | R, PG, DB, PC | NA | NA | NA |
| NMDA receptor antagonist | ||||||
| Dextromethorphan hydrobromide Phase I/2016 [38] | Two 75 mg capsules PO, separated by 4 h | 4/NA/NA MDD P = NA Tx = NA | R, PG, DB, PC | NA | NA | NA |
| Esketamine Phase III/2017 [117,118] | 84 mg intranasal, twice a week (on days 1,4,8,11,15,18,22 and 25) along with the standard of care antidepressant treatment initiated on day 1 (4 weeks) | 225/139/86 MDD and have suicidal ideation with intent but without psychotic features P = 112 Tx = 113 | R, PG, DB, PC, multi-center | ↓ MADRS total score (improved), improvement in the severity of suicidality measured by CGI-SS-r | Dizziness, headache, somnolence, dysgeusia, hypoesthesia, sedation, dizziness postural, nausea, constipation, vomiting, dissociation, insomnia, anxiety, ↑ blood pressure, blurred vision, vertigo | Suicidal depression, depression, suicide attempt, diabetic ketoacidosis |
| Esketamine Phase III/2017 [119,120] | 84 mg intranasal, twice a week (on days 1,4,8,11,15,18,22 and 25) along with the standard of care antidepressant treatment initiated on day 1 (4 weeks) | 227/136/91 MDD and having suicidal ideation with intent, but without psychotic features P = 113 Tx = 114 | R, PG, DB, PC, multi-center | ↓MADRS total score (improved), ↓ in the severity of suicidality measured by CGI-SS-r | Dizziness, dysgeusia, somnolence, headache, paresthesia, sedation, hypoesthesia, dizziness postural, nausea, vomiting, paresthesia oral, dry mouth, constipation, hypoesthesia oral, dissociation, anxiety, euphoric mood, depersonalization/derealization disorder, insomnia, vision blurred, diplopia, nasal discomfort, oropharyngeal pain, throat irritation, vertigo, ↑ blood pressure, hyperhidrosis, feeling drunk | Suicide attempt, suicidal ideation, depersonalization/derealization disorder |
| Esketamine Phase II/2019 [121] | Four low, medium, or high doses (three different groups) on days 1,4,8 and 11 via dry powder inhaler (2 weeks) | 88/NA/NA TRD in the course of MDD P = NA Tx = NA | R, PG, DB, PC, multi-center | NA | NA | NA |
| Esketamine Phase I/2016 [122,123] | Treatment A: intranasal placebo on day 1 and oral placebo on day 2 Treatment B: intranasal placebo on day 1 and oral alcohol on day 2 Treatment C: 84 mg of intranasal esketamine on day 1 and oral placebo on day 2 Participants will receive one of the ABC, BCA, CAB, CBA, ACB, or BAC treatments in part A and intranasal placebo on day 1 and 84 mg of intranasal esketamine on days 4,8,11,15,18,22 and 25 in part B | 23/16/7 MDD P = 20 Tx = 23 | Part A: R, cross-over assignment, SB, PC, active-controlled, double-dummy, 3-period Part B: OL, PC, fixed sequence, single period | Improvement in overall depression scores in MADRS | Dissociation, dizziness, dysgeusia, paresthesia, fatigue, paresthesia oral, nausea, headache, feeling abnormal, nasal discomfort, vision blurred, somnolence, euphoric mood, tinnitus, diplopia, ↑ blood pressure, feeling drunk, dysarthria, feeling of relaxation, illusion, hypoesthesia, altered time perception | Not reported |
| Combined medications | ||||||
| AXS-05 Phase III/2019 [40,124] | Oral tablets of 45 mg dextromethorphan and 105 mg bupropion, BID (6 weeks) | 327/215/112 Moderate or severe MDD P = 164 Tx = 163 | R, PG, DB, PC, multi-center | ↓ MADRS total score, improvement in daily functioning, improvement in quality of life | Dizziness, nausea, headache, diarrhea, somnolence, dry mouth | Not reported |
| AXS-05 Phase II/2018 [39,125] | 45 mg dextromethorphan and 105 mg bupropion BID and Bupropion as AC (6 weeks) | 80/51/29 Moderate or severe MDD AC = 37 Tx = 43 | R, PG, DB, active-controlled, multi-center | ↓ MADRS total score, improvement in core symptoms of depression | Nausea, dizziness, dry mouth, ↓ appetite, anxiety | Not reported |
| AXS-05 Phase III/2019 [41,126] | Oral tablets of 45 mg dextromethorphan and 105 mg bupropion, BID (12 months) | 876/380/496 MDD including TRD Tx = 876 | SG, OL, multi-center | ↓ Depression symptoms, improvement in functioning | Dizziness, nausea, headache, dry mouth, ↓ appetite | Not reported |
| Anticholinergic agents | ||||||
| Scopolamine Phase IV/2017 [45] | Experimental: scopolamine (0.3 mg/1 mL, IM) BID; escitalopram (10 mg/d PO) QD Experimental: scopolamine (0.3 mg/1 mL, IM) QD; placebo (1 mL saline, IM) QD; escitalopram (10 mg/d PO) QD Placebo comparator: placebo (1 mL saline, IM) BID; escitalopram (10 mg/d PO) QD | 66/NA/NA MDD | R, PG, QB | NA | NA | NA |
| Scopolamine Phase IV/2017 [44] | Experimental: participants will receive active medications scopolamine and naltrexone Placebo comparator: participants will receive placebo medication | 14/NA/NA Depression | R, PG, DB | NA | NA | NA |
| Mucolytic agents | ||||||
| N-acetyl cysteine Early phase I/2014 [127] | Experimental: sertraline and N-acetyl cysteine for 7 weeks Experimental: citalopram and N-acetyl cysteine for 7 weeks Experimental: existing depression medication treatment and N-acetyl cysteine for 7 weeks | 10/NA/NA MDD | Non-randomized, SG, OL | NA | NA | NA |
| Antibiotics | ||||||
| Minocycline Early phase I/2015 [128] | Experimental: minocycline 50 mg/day on week 1, 50 mg/BID on week 2, and 100 mg/BID weeks 3–8. For tapering, the dose will be reduced to 50 mg BID for a week and then stopped Placebo comparator: the number and appearance of the pills would be identical to those in the minocycline arm | 115/NA/NA MDD | R, SG, QB | NA | NA | NA |
| Minocycline Phase II/2015 [129] | Experimental: minocycline and standard antidepressant treatment Placebo comparator: placebo and standard antidepressant treatment | 168/NA/NA MDD | R, PG, TB | NA | NA | NA |
| Cycloserine Not applicable/2017 [130,131] | Group A: placebo + placebo: placebo 8 mm pill, single dose Group B: fludrocortisone + placebo: fludrocortisone Astonin H 0, 1 gm, single-dose + placebo 8 mm pill, single dose Group C: D-cycloserine + placebo: cycloserine 250 mg capsule, single-dose + placebo 8 mm pill, single dose Group D: fludrocortisone + D-Cycloserine: fludrocortisone Astonin H 0, 1 gm, single-dose + cycloserine 250 mg capsule, single dose | 232/182/50 MDD = 116 Healthy = 116 P = 58 Group B = 58 Group C = 58 Group D = 58 | R, PG, DB, PC | ↑ Cognitive empathy in the group with stimulated mineralocorticoid receptor, ↓ cognitive empathy only for positive emotions in MDD patients with NMDA-R stimulation, | NA | NA |
| D-cycloserine Phase IIb/III/2016 [42,105] | Experimental: NRX-101 (D-cycloserine + lurasidone) oral capsule with fixed-dose (administered to subjects who respond to an intravenous infusion of ketamine—0.5 mg/kg administered over 40 min; on Day 0)ketamine intravenous infusion (Randomized administration of Ketamine or Placebo in a 3 to 1 ratio), saline solution intravenous infusion (Randomized administration of Ketamine or Placebo in a 3 to 1 ratio) Active comparator: Lusaridone in the same dosage as lurasidone in NRX-101 ketamine intravenous infusion (Randomized administration of Ketamine or Placebo in a 3 to 1 ratio), saline solution intravenous infusion (Randomized administration of Ketamine or Placebo in a 3 to 1 ratio) (6 weeks) | 22/16/6 BP depression, suicidal ideas, suicidal ideation, attempted suicide Ketamine Followed by NRX-101 = 12 Ketamine Followed by Lurasidone = 5 Saline Followed by NRX-101 = 4 Saline Followed by Lurasidone = 1 | R, SA, QB, multicenter | NA | Angina pectoris, palpitation, tinnitus, diplopia, vision blurred, diarrhea, vomiting, dyspepsia, abdominal distention, dry mouth, nausea, gastroesophageal reflux disease, fatigue, vulvovaginal candidiasis, thermal burn, wound, ↑weight, muscle spasm, coordination abnormal, dizziness, dysmetropsia, headache, hypoesthesia, akathisia, hypersomnia, lethargy, somnolence, sedation, dissociation, restlessness, euphoric mood, anorgasmia, depressed mood, depression, suicidal ideation, acute kidney injury, ejaculation delayed, dry skin, rash, hypertension | Not reported |
| Antidiabetic agents | ||||||
| Metformin Phase I and II/2019 [132] | Experimental: fluoxetine 20 mg capsule once daily for 12 weeks + metformin 1000 mg XR tablet once daily for 12 weeks Placebo comparator: fluoxetine 20 mg capsule once daily for 12 weeks + placebo tablet once daily for 12 weeks | 80/NA/NA MDD | R, PG, DB | NA | NA | NA |
| Ganglionic blocking agents | ||||||
| Mecamylamine (TC-5214) Phase III/2012 [132,133] | Experimental: SSRI/SNRI + TC-5214, 0.1 mg BID SSRI/SNRI + TC-5214, 1 mg BID SSRI/SNRI + TC-5214, 4 mg BID Placebo comparator: SSRI/SNRI + placebo BID (8 weeks) | 696/498/198 MDD with inadequate response to no more than one antidepressant P = 174 0.1 mg = 174 1 mg = 174 4 mg = 174 | R, PG, DB, PC, multi-center | No significant difference between the two groups | Headache, dizziness, somnolence, dysgeusia, constipation, dry mouth, nausea, abdominal pain upper, diarrhea, vomiting, insomnia, agitation, nightmare, nervousness, fatigue, hyperhidrosis, influenza, UTI, ↑ alanine aminotransferase, nasopharyngitis, orthostatic hypotension, hypertension, hypotension, vertigo, ↑ appetite | Suicide attempt, suicidal ideation, depression, pneumonia, UTI, toxicity to various agents, food poisoning |
| Mecamylamine (TC-5214) Phase III/2010 [37,134] | Experimental: SSRI/SNRI + oral tablet TC-5214, 1–4 mg BID Placebo comparator: SSRI/SNRI + oral tablet placebo BID (8 weeks) | 319/200/119 MDD or depression with inadequate response to no more than one antidepressant P = 160 Tx = 159 | R, PG, DB, PC, multi-center | No significant difference between the two groups | Constipation, diarrhea, nausea, dry mouth, vomiting, headache, dizziness, somnolence, dizziness postural, abnormal dreams, insomnia, anxiety, agitation, nightmare, upper respiratory tract infection, nasopharyngitis, fatigue, ↑ weight, orthostatic hypotension, hyperhidrosis, musculoskeletal stiffness | headache |
| Mecamylamine (TC-5214) Phase III/2010 [132,134] | Experimental: SSRI/SNRI + oral tablet TC-5214, 1–4 mg BID Placebo comparator: SSRI/SNRI + oral tablet placebo BID (8 weeks) | 295/189/106 MDD or depression with inadequate response to no more than one antidepressant P = 148 Tx = 147 | R, PG, DB, PC, multi-center | No significant difference between the two groups | Constipation, nausea, dry mouth, diarrhea, abdominal distention, abdominal pain upper, headache, dizziness, somnolence, dizziness postural, sedation, tremor, orthostatic hypotension, hypertension, nasopharyngitis, sinusitis, influenza, fatigue, asthenia, insomnia, anxiety, back pain, vertigo, hyperhidrosis, vision blurred, ↑ appetite, ↑ aspartate aminotransferase | Uterine cancer |
| Mecamylamine (TC-5214) Phase III/2010 [132,133] | Experimental: SSRI/SNRI + TC-5214, 0.5 mg BID SSRI/SNRI + TC-5214, 2 mg BID SSRI/SNRI + TC-5214, 4 mg BID Placebo comparator: SSRI/SNRI + placebo BID (8 weeks) | 641/355/276 MDD or depression with inadequate response to no more than one antidepressant P = 161 0.5 mg = 160 2 mg = 160 4 mg = 160 | R, PG, DB, PC, multi-center | No significant difference between the two groups | Blurred vision, constipation, nausea, dry mouth, diarrhea, abdominal distention, vomiting, dyspepsia, flatulence, fatigue, pyrexia, asthenia, pain, nasopharyngitis, bronchitis, upper respiratory tract infection, sinusitis, ↑ aspartate aminotransferase, ↑ appetite, back pain, muscle spasms, muscle tightness, myalgia, headache, dizziness, somnolence, dizziness postural, akathisia, insomnia, nightmare, agitation, abnormal dreams, pollakiuria, orthostatic hypotension, hypertension | Major depression, suicidal ideation, clavicle fracture, rib fracture, scapula fracture, obstructive uropathy, renal failure acute, upper respiratory tract infection, benign prostatic hyperplasia, pulmonary fibrosis, convulsion |
| Mecamylamine (TC-5214) Phase III/2010 [135,136] | Experimental: SSRI/SNRI + oral tablet TC-5214, 1–4 mg BID Placebo comparator: SSRI/SNRI + oral tablet placebo BID (52 weeks) | 813/566/247 MDD or depression with inadequate response to no more than one antidepressant P = 203 Tx = 610 | R, PG, DB, PC, multi-center | No significant difference between the two groups | Constipation, nausea, dry mouth, diarrhea, abdominal pain, vomiting, abdominal pain upper, flatulence, abdominal distension, fatigue, seasonal allergy, nasopharyngitis, bronchitis, upper respiratory tract infection, sinusitis, influenza, UTI, gastroenteritis, gastroenteritis viral, contusion, muscle strain, ↑ weight, ↑ blood pressure, ↑ appetite, arthralgia, back pain, muscle spasms, musculoskeletal pain, neck pain, pain in extremities, myalgia, headache, dizziness, somnolence, dizziness postural, sedation, memory impairment, migraine, paresthesia, tremor, insomnia, abnormal dreams, agitation, anxiety, bruxism, cough, nasal congestion, oropharyngeal pain, wheezing, hyperhidrosis, rash, hypertension, orthostatic hypotension | Bradycardia, abdominal hernia, diverticulum, hemorrhoids, small intestinal obstruction, cellulitis, oral infection, pneumonia, brain contusion, cerebral vertebral fracture, contusion, facial bones fracture, fibula fracture, tibia fracture, toxicity to various agents, musculoskeletal chest pain, abortion spontaneous, alcohol withdrawal syndrome, psychotic disorder, suicidal ideation, suicide attempt, ovarian torsion, hypertensive crisis |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohammad Sadeghi, H.; Adeli, I.; Mousavi, T.; Daniali, M.; Nikfar, S.; Abdollahi, M. Drug Repurposing for the Management of Depression: Where Do We Stand Currently? Life 2021, 11, 774. https://doi.org/10.3390/life11080774
Mohammad Sadeghi H, Adeli I, Mousavi T, Daniali M, Nikfar S, Abdollahi M. Drug Repurposing for the Management of Depression: Where Do We Stand Currently? Life. 2021; 11(8):774. https://doi.org/10.3390/life11080774
Chicago/Turabian StyleMohammad Sadeghi, Hosna, Ida Adeli, Taraneh Mousavi, Marzieh Daniali, Shekoufeh Nikfar, and Mohammad Abdollahi. 2021. "Drug Repurposing for the Management of Depression: Where Do We Stand Currently?" Life 11, no. 8: 774. https://doi.org/10.3390/life11080774
APA StyleMohammad Sadeghi, H., Adeli, I., Mousavi, T., Daniali, M., Nikfar, S., & Abdollahi, M. (2021). Drug Repurposing for the Management of Depression: Where Do We Stand Currently? Life, 11(8), 774. https://doi.org/10.3390/life11080774






