1. Introduction
Blood lipids are an important predictive factor for atherosclerosis and an independent risk factor for coronary heart disease and ischemic stroke, which means that dyslipidemia might lead to many ongoing pathologies in people’s daily life, such as metabolic syndrome and cardiovascular disease [
1]. Moreover, a close association between serum lipid levels and the incidence of coronary heart disease has been well proven in middle-aged and elderly people with a probable degeneration of metabolic functions [
2]. Lipid profiles have been used to define dyslipidemia, and abnormal serum lipid profiles include changes in four indicators: high total cholesterol (TC), high triacylglyceride (TAG), low high-density lipoprotein cholesterol (HDL-C), and elevated low-density lipoprotein cholesterol (LDL-C) [
3]. Therefore, improving the blood lipid indicators of middle-aged and elderly people has become a hot topic that is receiving increased attention at present.
Medicine (e.g., statins, niacin drugs) is widely used in blood lipid improvement [
4]. However, with an increasing dose of statins, the occurrence of side effects, such as statin-associated myopathy and liver damage, may increase accordingly [
1]. Additionally, statins carry a risk of causing new-onset diabetes, and some experts have even suggested a risk of developing new tumors. This is making patients with elevated blood lipid levels seek complementary and alternative medicine as a lipid-lowering approach. According to the “Nutrition and Health Survey of Chinese Residents”, exercise can decrease the incidence of chronic lipid metabolic syndromes, such as HDL-C and high TAG [
5]. Related studies have demonstrated that exercise has the potential to alternate drug treatments, especially in the early phase of dyslipidemia [
4]. Thus, it can be seen that appropriate exercise can not only help middle-aged and elderly people to improve their blood lipid indicators but also play a role in physical fitness, which is an ideal treatment without any side effects. However, due to the physical characteristics of middle-aged and elderly people, the mode of exercise cannot be chosen blindly: high-intensity exercise is not suitable, and moderate to low-intensity exercise is the most appropriate option. The common characteristics of traditional Chinese exercises (TCEs) include that they are slow, relaxing, and systematic, and therefore suitable for physically weak patients. TCEs are easy to master in a short time and have few physical demands [
2] as they are considered to be a low-risk intervention. Yang Lina et al. (2009) [
6] concluded that long-term Taijiquan (TJQ) and Baduanjin (BDJ) exercise can improve the concentration of HDL in blood lipids, reduce the concentration of TAG, TC, and LDL, and reduce the incidence of cardiovascular diseases, such as high blood lipids, in which TCEs were recommended. Therefore, TCE is an exercise mode that can effectively improve blood lipids in middle-aged and elderly people.
TCE might improve the functions of the cardiopulmonary and nervous system as well as balance ability and psychological state [
6], which are especially important for middle-aged and older people [
7]. The National Fitness Guide issued by the State Sports General Administration of China in 2017 [
7] pointed out that TCEs, which include Taijiquan (TJQ), Wuqinxi (WQX), Baduanjin (BDJ), Yijinjing (YJJ), Liuzijue (LZJ), Dawu (DW), Mulan sword, and Martial arts routines, are gentle and safe with emphasis on the combination of meditation and physical activities. Previous studies suggest that TJQ [
8], BDJ [
9], WQX [
10], YJJ [
11], LZJ [
12], and DW [
2] have positive effects on blood lipid indicators. For example, TJQ can improve TAG and HDL levels [
8], YJJ can improve TAG, LDL, and HDL levels [
11], LZJ can increase HDL levels [
12], and DW has a significant effect on improving TC, TAG, and HDL indicators. However, there were differences in the sample sizes, interventions, and inaccurate measurement indicators among these studies, which led to different research results. Through an analysis of these previous studies, it was found that the effect of each TCE on blood lipid indicators was different; in different studies, the effect of the same TCE on blood lipid indicators was also different [
6], and comparisons among TCEs have rarely taken place. It is still unclear which TCE is most effective in improving blood lipids among middle-aged and elderly people. To the best of our knowledge, no comprehensive analysis has been undertaken to compare the effect of these TCEs on dyslipidemia treatment. Meta-analyses can generally compare differences in efficacy between two interventions. However, it is difficult to compare the effects among several exercise treatments because of the low number of available head-to-head comparisons. Network meta-analysis (NMA) can overcome this limitation by drawing together direct and indirect comparisons of all available treatment options. Therefore, this systematic review and network meta-analysis compares the effects of TJQ, BDJ, WQX, YJJ, LZJ, and DW on blood lipids, explores the effect of each TCE on the improvement of blood lipid indicators in middle-aged and elderly people, and determines which TCE is the optimal option for middle-aged and elderly individuals with dyslipidemia.
2. Materials and Methods
2.1. Registration
This study was performed following the PRISMA network statement. The protocol for this study was registered in the International Prospective Register of Systematic Reviews (PROSPERO). The registration number is CRD42020216190.
2.2. Data Sources and Search Strategy
The search strategy was created using a combination of medical subject heading (MeSH) terms, keywords, and phrases. The search terms “((Tai Chi) OR (Taijiquan) OR (Yijinjing) OR (Wuqinxi) OR (Five-animal exercise) OR (Liuzijue) OR (Six healing sounds) OR (Yijinjing) OR (Da wu)) AND ((blood lipid) OR (dyslipidemia) OR (dyslipidemias) OR (blood fats)) [Title]” were typed into the databases of PubMed, Web of Science, China National Knowledge Infrastructure (CNKI), and Chongqing VIP in turn, and all the results of these databases were exported to the software EndNote X9. Then, after excluding duplicates, the list of studies was screened using the search terms TC, TAG, HDL-C, and LDL-C in turn at the field of the abstract to screen out studies with eligible outcomes. At the same time, all the studies whose designs or protocols were randomized were included in full-text screenings with the search terms randomized. Studies before 1990 were not included in this study. The search strategy was constructed using the patient, intervention, comparison, outcome, study design (PICOS) framework.
Two researchers (Y.G. and L.Y.) searched the literature and reviewed the title and abstract of each article. The full text of the selected articles was evaluated according to the inclusion and exclusion criteria, and divergent articles were reviewed by a third reviewer (H.H.).
2.3. Inclusion and Exclusion Criteria
2.3.1. Inclusion Criteria
The inclusion criteria strategy was defined according to participants, interventions, comparisons, outcomes, and study design (PICOS): (1) Subjects of both sexes, aged 40 years old and over, and with a clinical diagnosis of healthy status, dyslipidemia, or chronic disease were included; (2) the type of study included was RCT comparing the effects of six TCEs on lipids. Experimental groups adopted BDJ, WQX, YJJ, LZJ, DW, or TJQ. The control group was a simple control group with non-exercise intervention (NEI), or routine aerobic exercise (AE), such as walking and jogging, or other specific TCEs; (3) the outcomes included at least one of the four lipid indicators (TC, TAG, HDL, CLDL-C); (4) ethically approved RCTs were included.
2.3.2. Exclusion Criteria
The exclusion criteria included: (1) literature not published in English or Chinese; (2) repetitions of previously published literature; (3) theoretical and review literature; (4) literature with only abstracts but no full text; (5) literature designed for non-randomized controlled studies—for example, before–after studies on the same patient; (6) joint-intervention trials; (7) studies where the experimental subjects were not middle-aged or elderly; (8) studies where the experimental data were not clear, and it was not possible to calculate the average and standard deviation of the outcome indicator; (9) studies with control groups that did not meet our requirements, such as drug control; (10) studies with data errors or missing literature.
2.4. Literature Screening and Data Extraction
According to the inclusion and exclusion criteria, a unified method and standardized search and selection were used, with the two authors (Y.G. and L.Y.) conducting searches in turn and independently. The figures and tables for information were produced after the two authors had verified their results. An independent arbitrator (H.H.) resolved any discrepancies in data extraction.
The following data were collected: (1) basic information extracted, including the name of the first author and the year of publication; (2) the demographic characteristics of the subjects, such as sex and age; (3) information regarding study design, such as sample size, interventions, measurement parameters, follow-up duration, and information related to bias risk assessment.
All the measurement parameters of blood lipids were converted to mean differences (MD) on blood lipids following exercise intervention under the international standard system of units. If an included study reported outcomes of different follow-up times or had more than one trial arm, each different follow-up time and trial arm were treated as a separate trial. The Cochrane Handbook for Systematic Review of Interventions provides detailed measures for dealing with such situations—one way to overcome this is to perform a fixed-effect meta-analysis across comparisons within a study, and a random-effects meta-analysis across studies; in practice, the difference between different analyses is likely to be trivial [
13].
Since the unit of a certain blood lipid parameter is uniform, the standardized mean difference was not chosen to illustrate the pooled effect. The software STATA® 16 (StataCorp LLC, College Station, TX, USA) was used to analyze the combined effect.
2.5. Quality Assessment
The Cochrane Collaboration tool was used to assess the risk of bias. The study quality was assessed and graded independently by two authors (Y.G. and L.Y.) according to the criteria described in The Cochrane Handbook. The risk of bias graph and the risk of bias summary graph were produced using RevMan5.3. If the evaluation results were inconsistent, the issue was resolved following discussion with the third researcher (A.W.).
2.6. Statistical Analysis
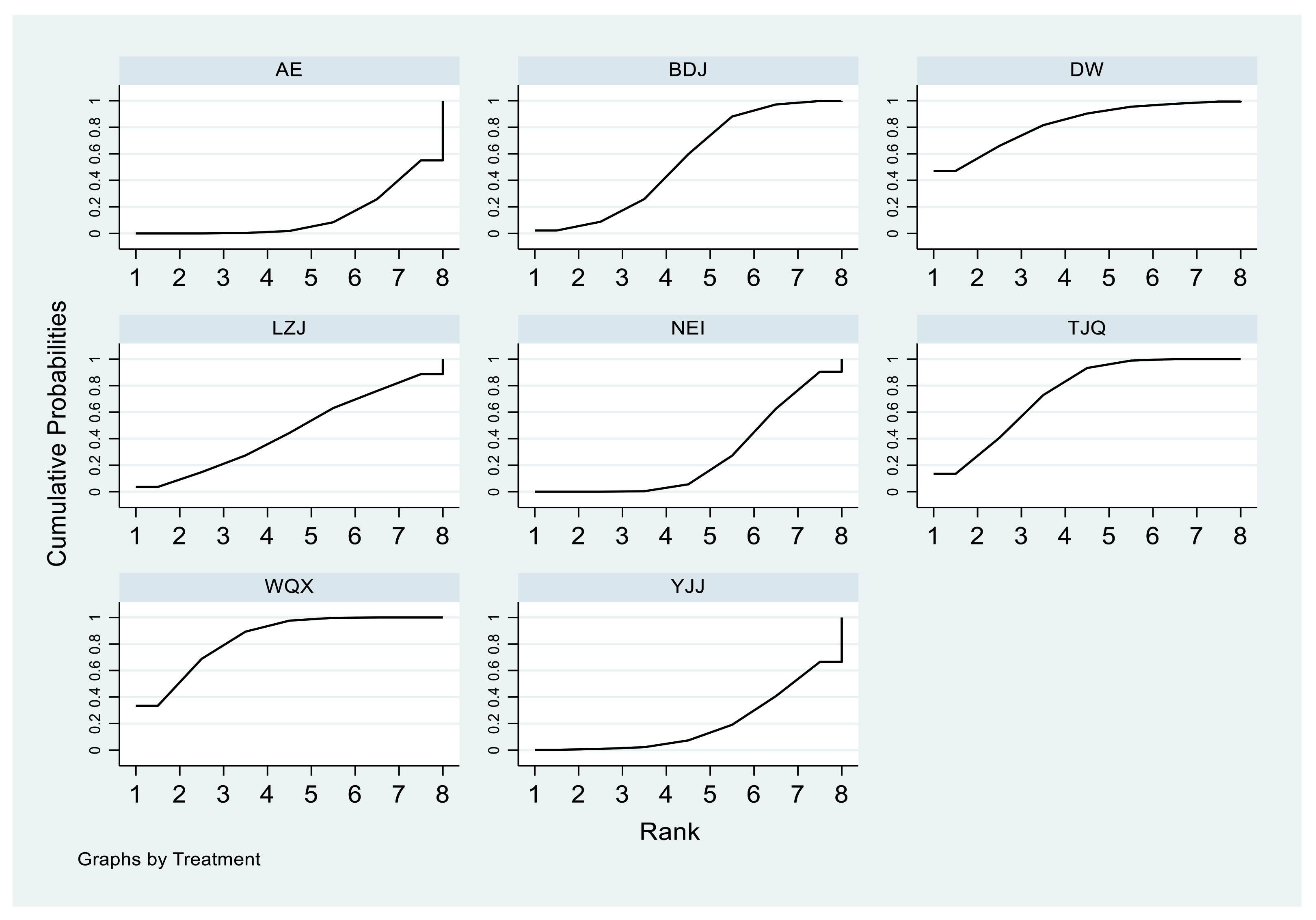
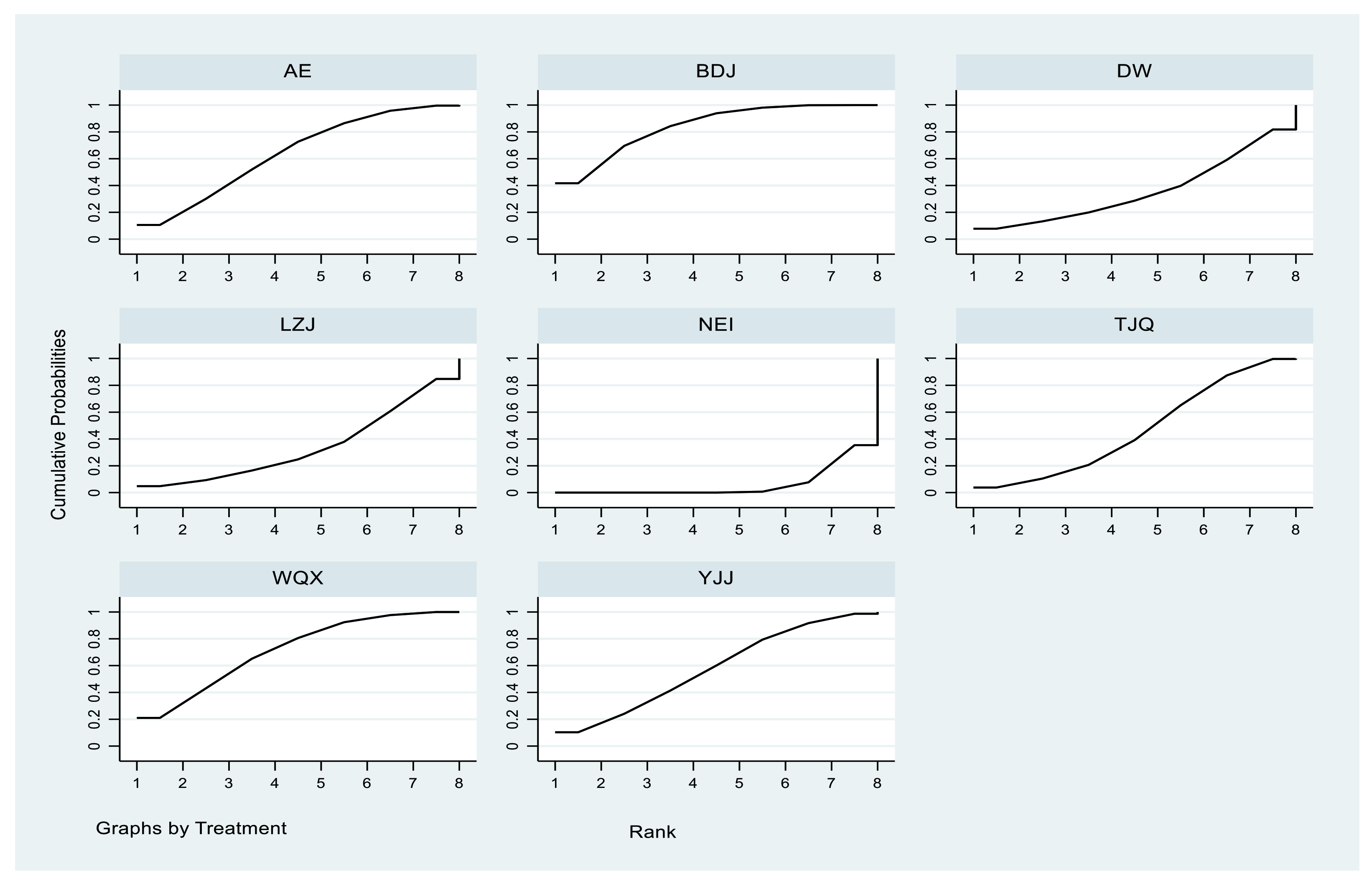
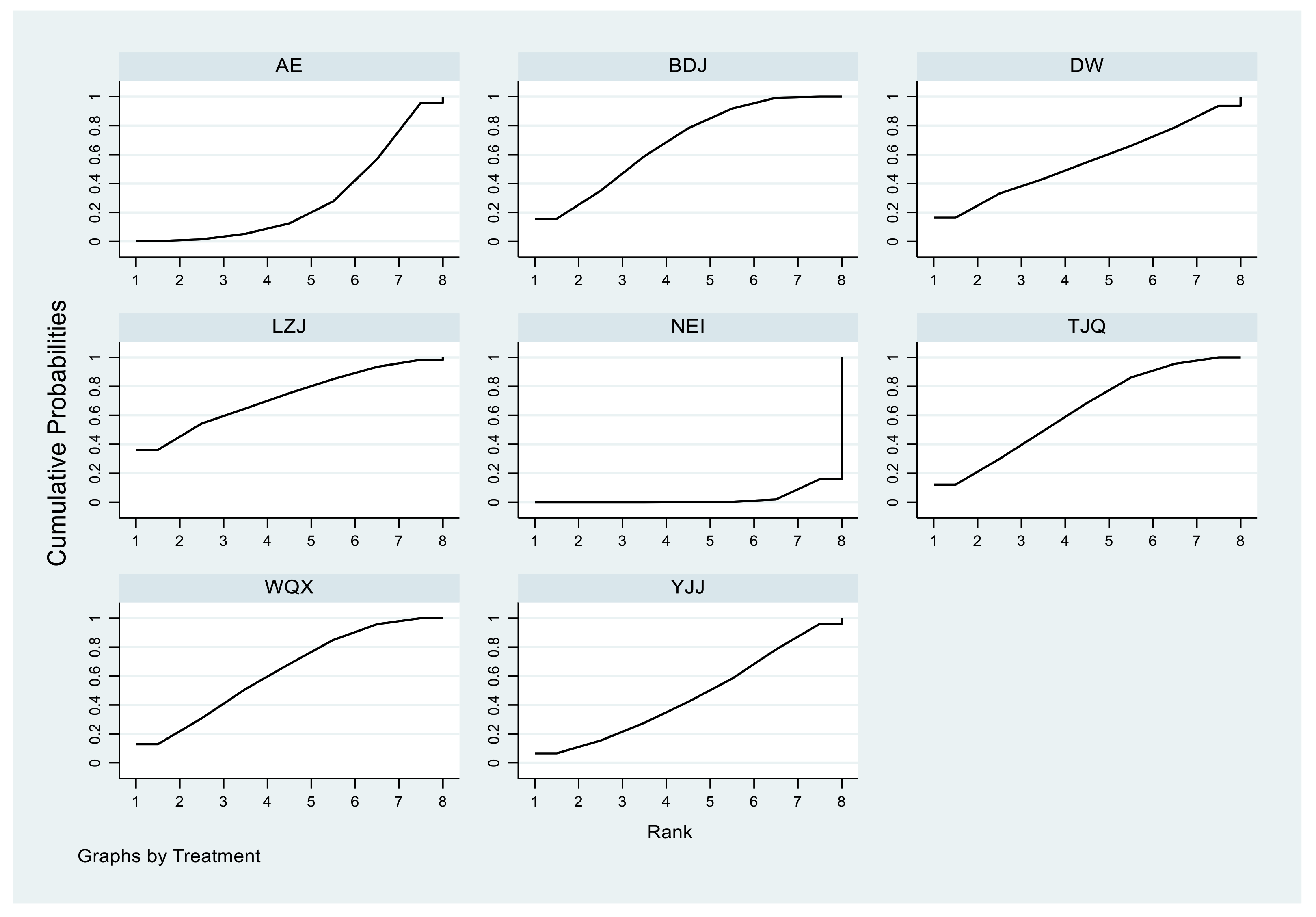
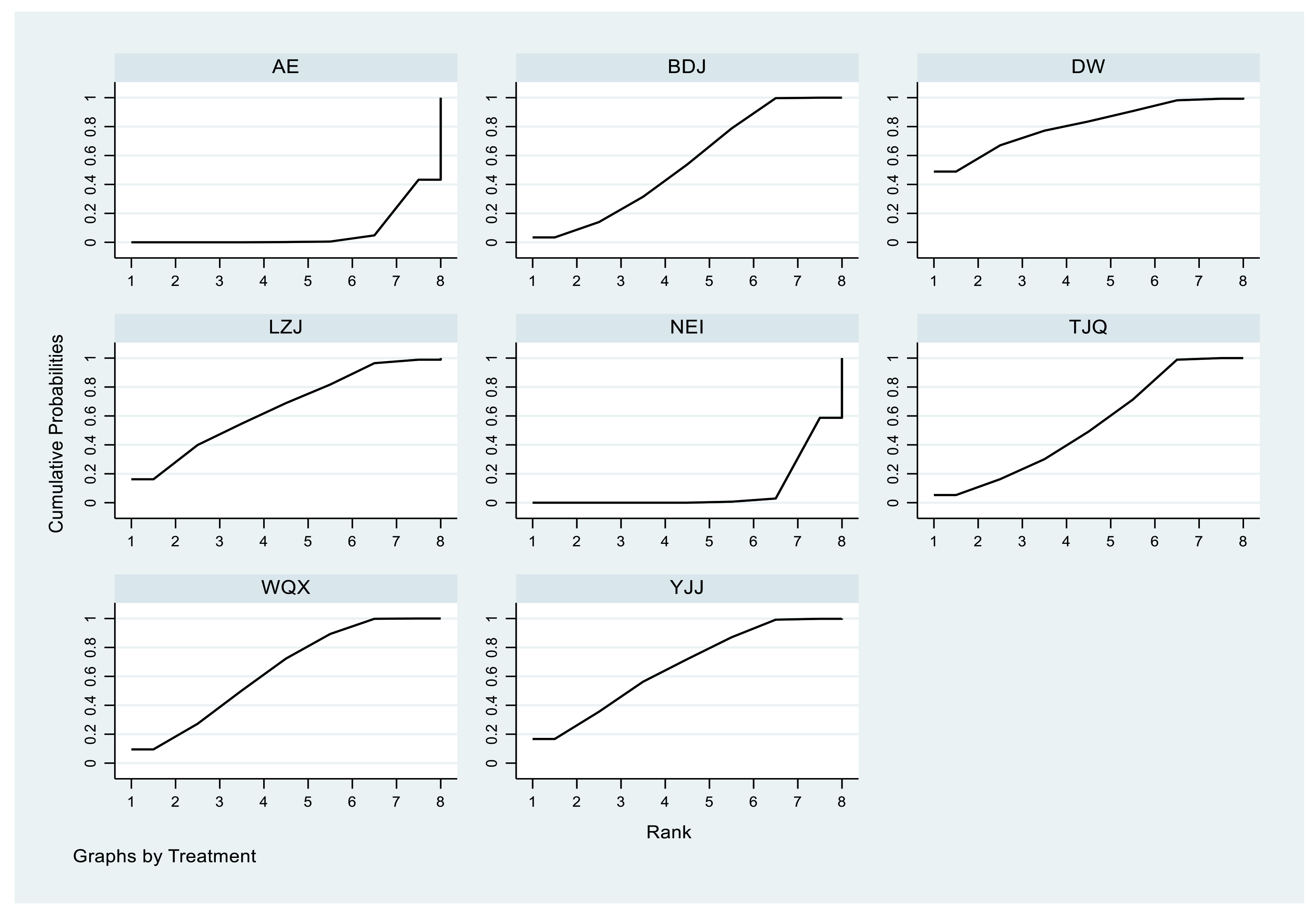
A set of multivariate meta-analysis programs in STATA® 16 (StataCorp LLC, College Station, TX, USA) software was used to deal with the statistical analysis, draw the net relation diagram of different interventions, and output the table of direct pairwise comparisons of different interventions as well as the forest plot to present the results of network meta-analysis visually. When there was a closed loop, the consistency between direct comparison and indirect comparison was judged by the node-splitting value, and inconsistency was considered to be significant when p < 0.05. When there was no closed-loop structure within the interventions, there was no need to make a consistency test. Continuous variables (TC, TAG, HDL-C, and LDL-C) were analyzed by mean differences (MDs) and 95% credible intervals (95%CI). The effectiveness of these six interventions can be ranked by the surface under the cumulative ranking curve (SUCRA). SUCRA values range from 0% to 100%. The higher the SUCRA value, and the closer to 100%, the higher the likelihood that therapy is in the top rank or one of the top ranks.
4. Discussion
As the General Administration of Sport of China recommends, more and more people are choosing TCEs to exercise at home. This manuscript has been written based on the hypothesis that TECs have a positive effect on the blood lipid parameters of middle-aged and older people. This systematic review included 42 RCTs, with 6 TCEs with 2977 subjects aged 55 to 60 years, providing high-quality evidence of the effect of six kinds of TCE on blood lipids. Maoxing Pan et al. (2019) [
58] studied the effect of Qigong on blood lipids in middle-aged and elderly people through a network meta-analysis, but TJQ was not included. Taijiquan is one of the main forms of TCEs, and it is also very popular in China. To the best of our knowledge, at present, this review is the first network meta-analysis comparing the effects of six TCEs.
People’s blood lipid parameters are becoming worse with the development of society. Around the world, over 4000 people die of cardiovascular diseases caused by dyslipidemia every day [
59]. Medicine treatments are underused in clinical practice because most doctors worry about their hepatotoxicity and nephrotoxicity [
58]. According to a survey of physical examiners in Beijing [
59], lifestyle changes play a great role in preventing and treating hypercholesterolemia. TCEs are mind–body exercises that focus on posture, coordination of breathing patterns, and meditation. Movements in TCE are smooth and slow, making this type of exercise safe for middle-aged and older people. In terms of metabolic types, oxidative metabolism, in which fat is oxidized by the body to provide energy, is dominant in TCEs. The positive effects of aerobic exercise on blood lipid parameters have already been verified in many trials enrolling subjects with dyslipidemia [
60]. Improvements in lipid levels include lowering the levels of TC, LDL-C, and TAG and increasing the level of HDL-C. Some studies have found that during aerobic exercise, total energy consumption and exercise intensity will affect the improvement of blood lipids and have a positive effect on the improvement of HDL-C and LDL-C [
61]. Moderate-intensity aerobic exercise can cause a significant increase in HDL-C, and improvement and reduction in LDL-C may require more intensive aerobic exercise. For middle-aged and elderly individuals, adhering to moderate physical activities can not only delay the senile degenerative changes of various system organs but also maintain relatively high physiological function [
62]. Therefore, TCEs can help to improve both physical and psychological conditions of middle-aged and older people [
63,
64,
65].
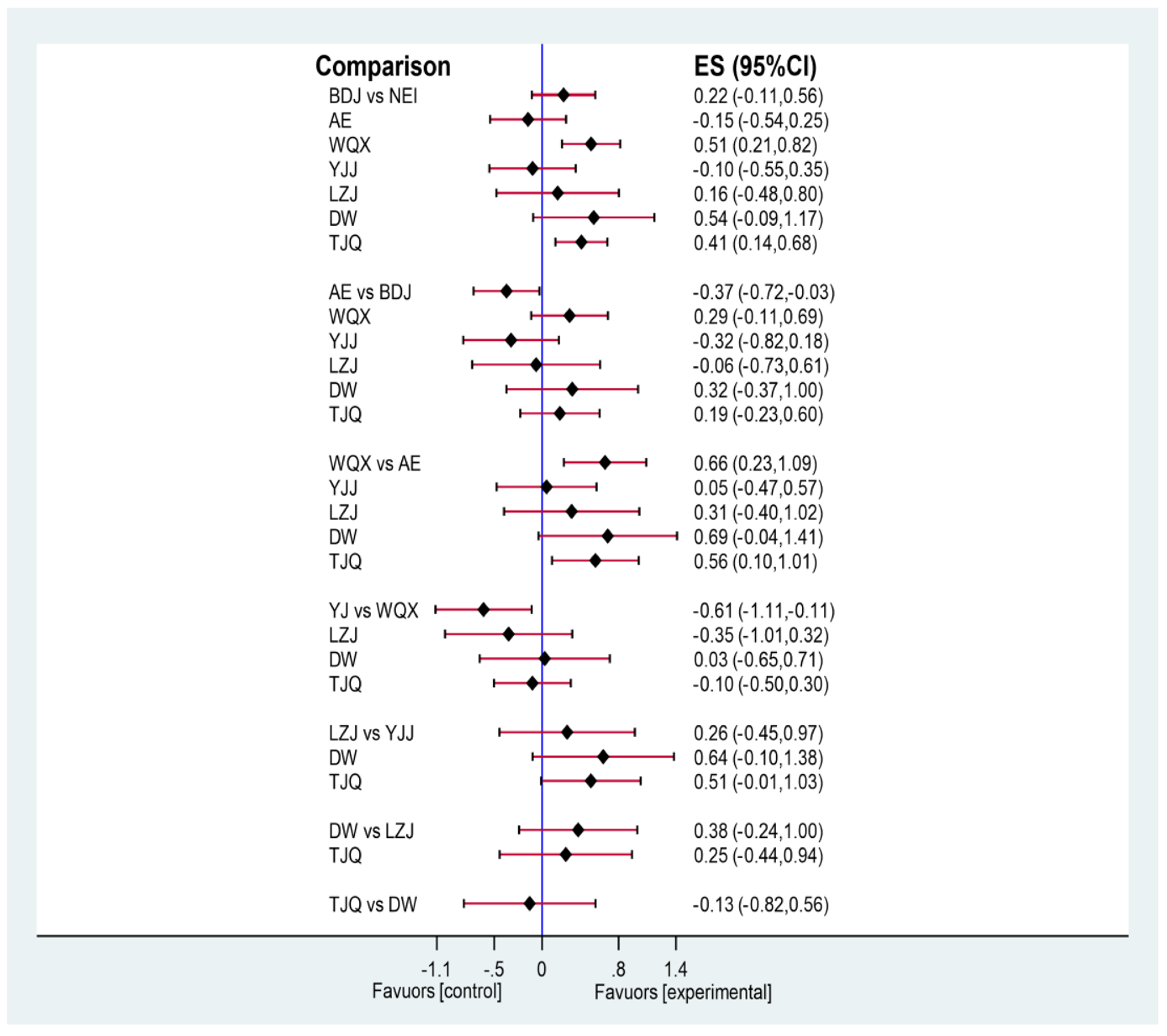
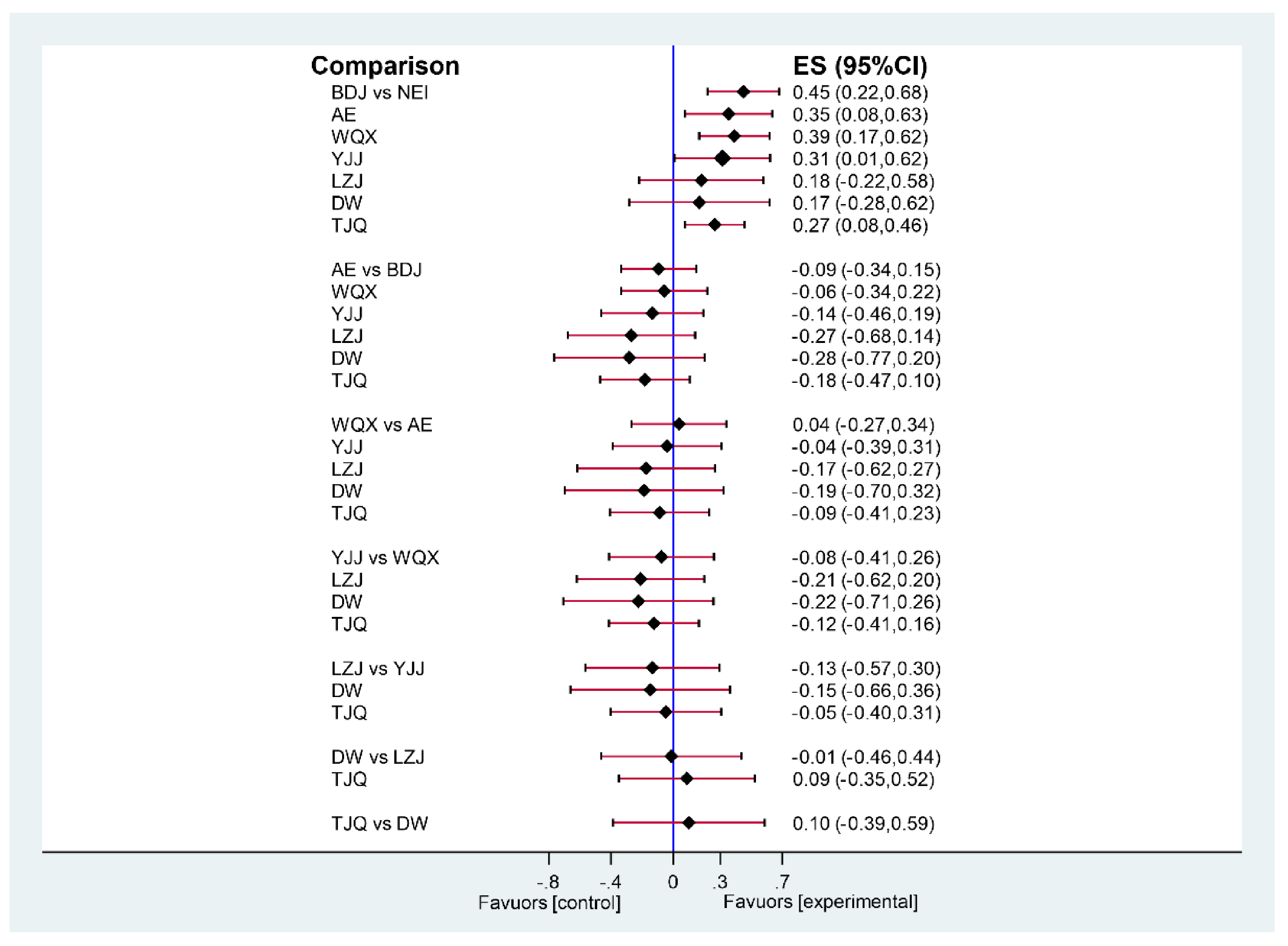
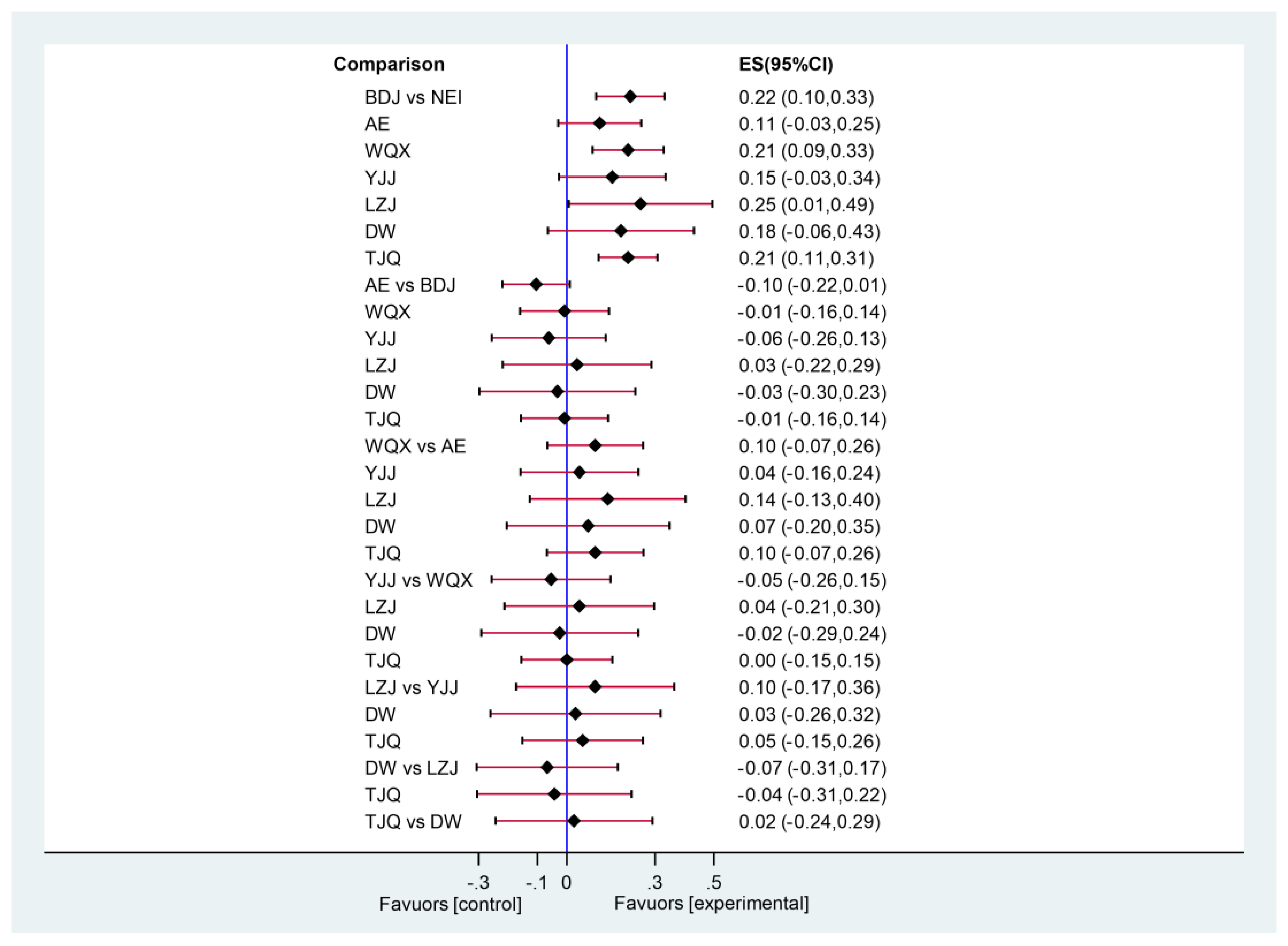
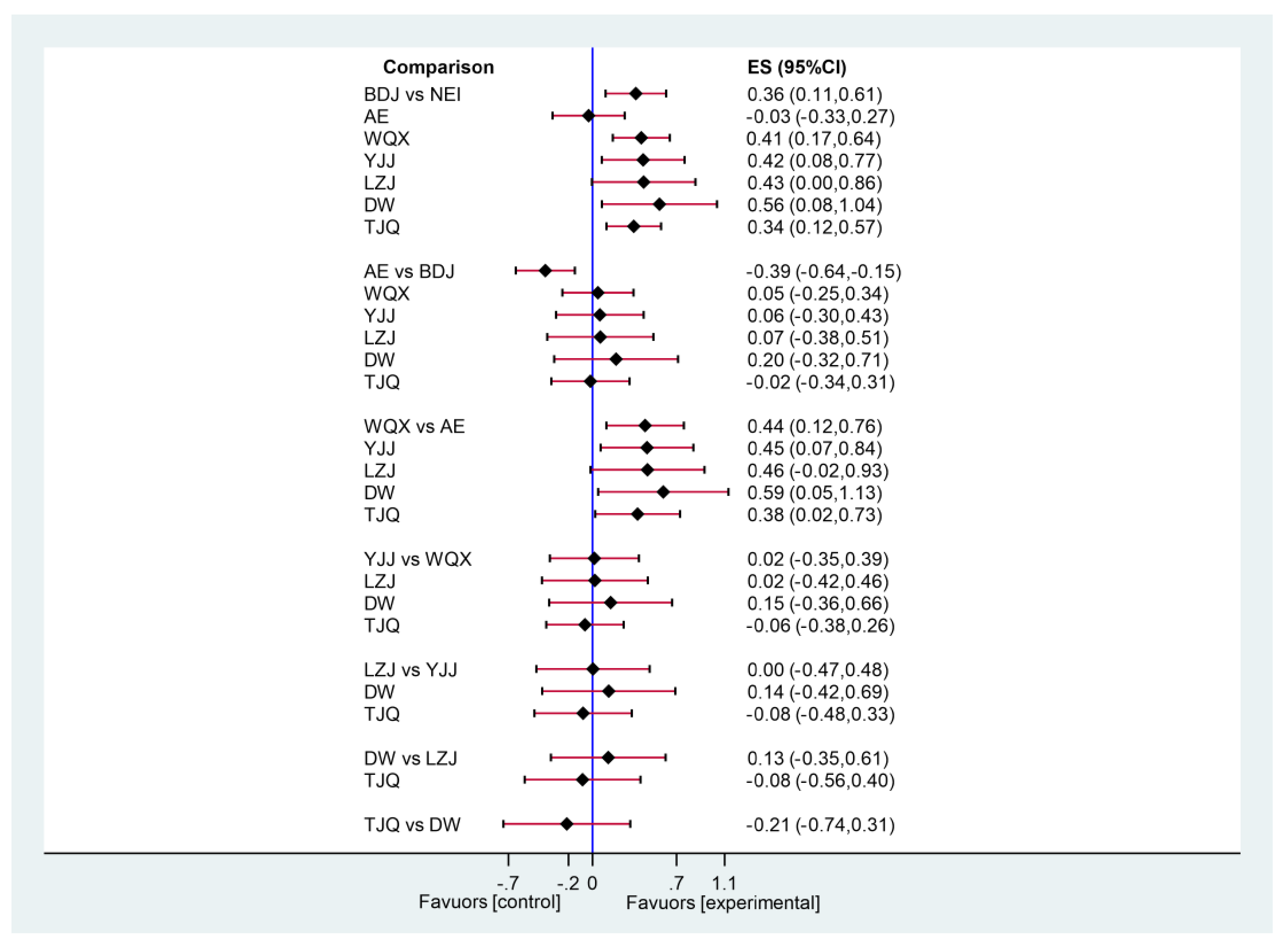
A total of 42 RCTs were included in this study, including six kinds of TCE and two general controls. Network meta-analysis of direct and indirect evidence showed that six kinds of TCE can effectively improve some blood lipid indicators in middle-aged and elderly individuals. Compared with the NEI group, WQX and TJQ had a significant effect on the decrease in TC, TAG, and LDL and an increase in HDL in middle-aged and elderly people. BDJ had a significant effect on the decrease in TAG and LDL and an increase in HDL in middle-aged and elderly people. YJJ had an obvious effect on the decrease in TAG and LDL in middle-aged and elderly people. LZJ had an obvious effect on the reduction in LDL and can increase the level of HDL in middle-aged and elderly people, while DW had an obvious effect on the reduction in blood LDL in middle-aged and elderly people. Compared with the YJJ group, the level of TC in the WQX group decreased more significantly. We can conclude that all six TCEs are effective in improving LDL-C and are partially effective for other lipid indicators. There are no significant differences in the consistency analysis, which reveals that the statistical model of indirect comparisons is reliable. This may be due to the similar exercise program and outcome indicators among the included studies. Therefore, it can be suggested that patients can choose an appropriate TCE according to their preferences and physical conditions to improve blood lipid parameters.
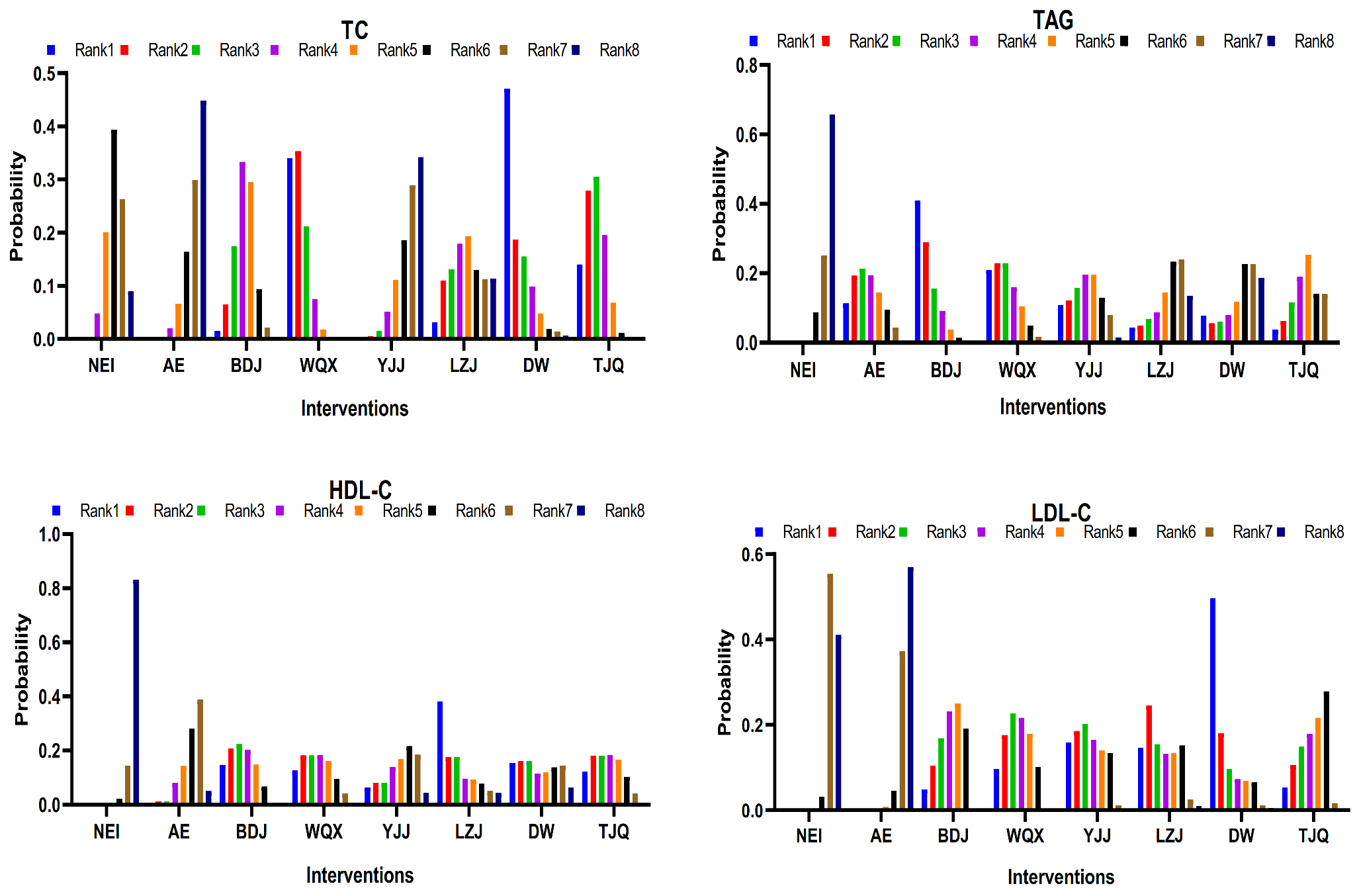
The ranking results for TC were as follows: WQX > DW > TJQ > BDJ > LZJ > NEI > YJJ > AE. Compared with the NEI group, WQX and TJQ had significant effectiveness, and WQX had the best effect in terms of improving TC. The ranking results for TAG were as follows: BDJ > WQX > AE > YJJ > TJQ > DW > LZJ > NEI. Compared with the NEI group, BDJ, WQX, YJJ, and TJQ had significant effectiveness, and BDJ had the best effect in terms of improving TAG. The ranking results for HDL were as follows: LZJ > BDJ > WQX > TJQ > DW > YJJ > AE > NEI. Compared with the NEI group, LZJ, BDJ, WQX, and TJQ had significant effectiveness, and LZJ had the best effect in terms of improving HDL. The ranking results for LDL were as follows: DW > YJJ > LZJ > WQX > BDJ > TJQ > NEI > AE. Compared with the NEI group, DW, YJJ, LZJ, WQX, BDJ, and TJQ had significant effectiveness, and DW had the best effect in terms of improving LDL. Additionally, statistical factors, such as study design, number of controls, and number of subjects, and many other factors, may have contributed to the difference in outcomes. Although the dominant metabolic patterns of different types of TCE are similar, their activity patterns and training principles are different.
To sum up, based on the comparison with NEI and AE groups, it was found that WQX, TJQ, and BDJ were more effective in improving blood lipids in middle-aged and elderly people. WQX and TJQ had a significant effect on all four indicators of blood lipid indicators. However, BDJ was effective on three indicators of blood lipids, but not TC. Therefore, WQX and TJQ are recommended as appropriate TCE methods for blood lipid control. The results of cumulative probability ranking showed that the SUCRA value of WQX was the highest, while the PrBest value, followed by BDJ and TJQ, indicated that WQX may be the most effective TCE to improve the blood lipid status of middle-aged and elderly people. Therefore, two methods (WQX and TJQ) are recommended as TCE methods for blood lipid control, of which WQX is recommended as the best choice.
The influential mechanism of WQX on blood lipids may be that it emphasizes the control of respiration and regulation of the mind during exercise [
66], which not only improves the function of the respiratory system but also accelerates blood circulation [
67]. By controlling breathing, the balance of the autonomic nerve can be regulated [
68], and the level of substance metabolism can be regulated, and thus, the disorder of lipid metabolism can be improved [
39]. The essence of mind regulation is to dominate and exercise the motor nervous system and autonomic nervous system, regulate hormone-sensitive lipase by increasing the activity of the sympathetic nervous system, and finally regulate lipid metabolism [
39]. The action mechanism of TJQ may be that its action plays a natural “massage” effect on vascular smooth muscle, promoting rhythmic contraction and relaxation of blood vessels [
21], gradually scouring and eliminating the deposition of cholesterol and cholesterol esters on the blood vessel wall; furthermore, TJQ exercise helps to eliminate the anxiety and tension of practitioners, reduce the tension of sympathetic vasoconstrictor nerves, reduce the release of norepinephrine in its terminals [
69], and improve the excitability of sympathetic vasoconstrictor nerves. However, the specific mechanism of these three kinds of TCE on improving blood lipids is not clear, with a noted lack of high-quality research at the cellular and molecular level, and thus, further research is needed.
There were some limitations in this network meta-analysis. Small sample sizes and large sex differences existed in some RCTs. There was a different number of RCTs included in different interventions, which may have had a certain impact on the evaluation of the intervention. Most of the RCTs were conducted in China and published in Chinese, which may affect the results. The differences between analyzed populations (middle-aged and elderly) were not reported. Most RCTs did not clearly report whether a random, double-blind method was used. The research did not discuss the adaptation time, size, and actual needs of each TCE.
In follow-up studies, after the emergence of more multicenter, standardized, and high-quality research using larger samples, we can make use of the advantages of network meta-analysis to further study the impact of TCEs on blood lipids among middle-aged and elderly people from all aspects. More research and attention should be paid to the time for adaptation, magnitude, and practical needs of each TCE, as well as the specific mechanism and the best training program for each TCE.