Serum Adropin Levels in Patients on Hemodialysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Subject Inclusion Criteria
2.2. Hemodialysis Sessions
2.3. Laboratory Analysis
2.4. Anthropometric Measurements and Clinical Assessment
2.5. Nutrition and Inflammation Assessment Scores
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Study Population
3.2. Laboratory Parameters of the Study Population
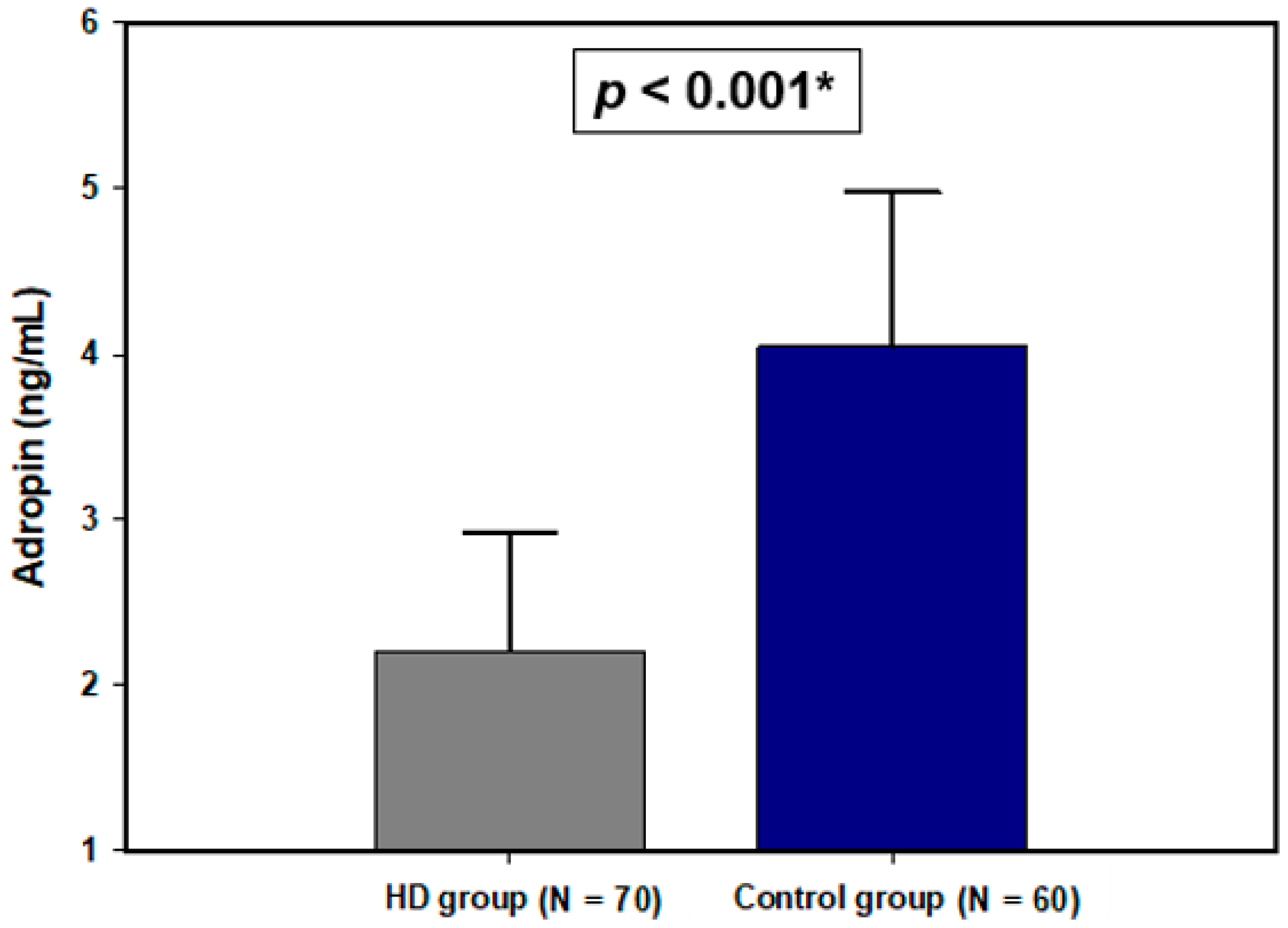
3.3. Serum Adropin Levels
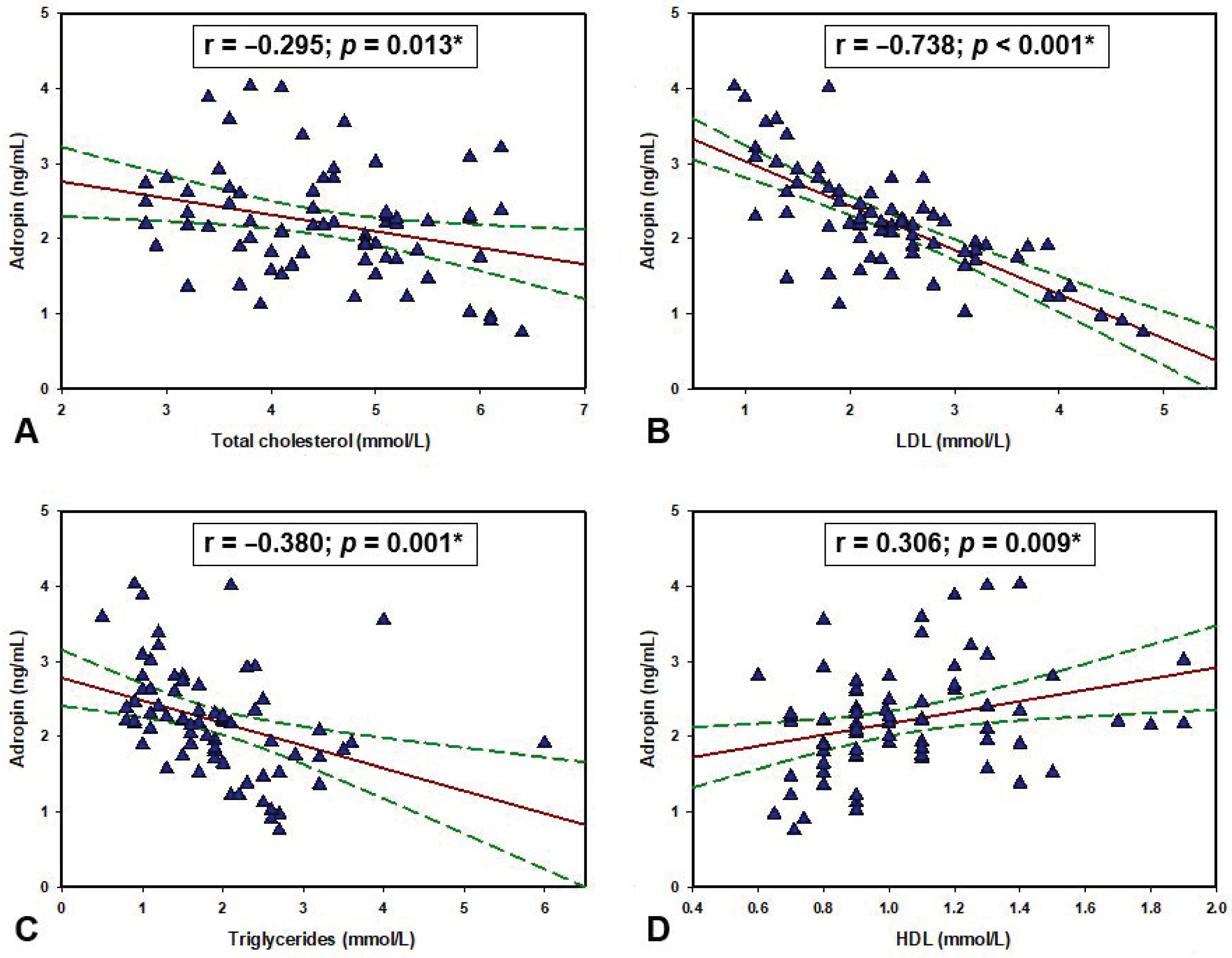
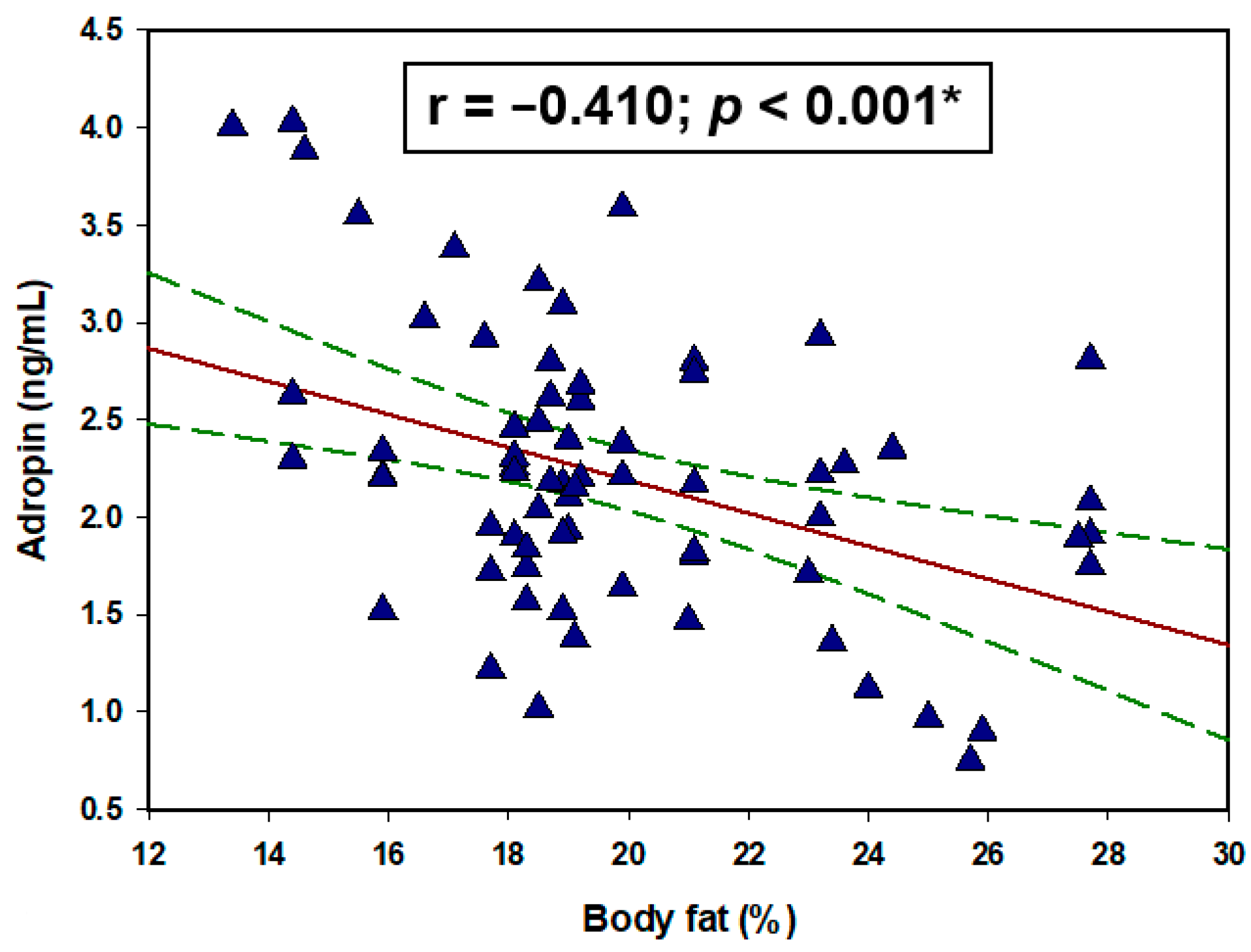
3.4. Adropin Correlations with Laboratory, Anthropometric and Clinical Parameters
3.5. Multiple Linear Regression Analysis for Serum Adropin Levels
4. Discussions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahmadmehrabi, S.; Tang, W.H.W. Hemodialysis-induced cardiovascular disease. Semin. Dial. 2018, 31, 258–267. [Google Scholar] [CrossRef] [PubMed]
- Rizikalo, A.; Coric, S.; Matetic, A.; Vasilj, M.; Tocilj, Z.; Bozic, J. Association of Glomerular Filtration Rate and Carotid Intima-Media Thickness in Non-Diabetic Chronic Kidney Disease Patients over a 4-Year Follow-Up. Life 2021, 11, 204. [Google Scholar] [CrossRef]
- Li, L.; Xie, W.; Zheng, X.L.; Yin, W.D.; Tang, C.K. A novel peptide adropin in cardiovascular diseases. Clin. Chim. Acta 2016, 453, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Aydin, S.; Kuloglu, T.; Eren, M.N.; Yilmaz, M.; Kalayci, M.; Sahin, I.; Kocaman, N.; Citil, C.; Kendir, Y. Expression of adropin in rat brain, cerebellum, kidneys, heart, liver, and pancreas in streptozotocin-induced diabetes. Mol. Cell Biochem. 2013, 380, 73–81. [Google Scholar] [CrossRef]
- Marczuk, N.; Cecerska-Heryć, E.; Jesionowska, A.; Dołęgowska, B. Adropin—Physiological and pathophysiological role. Postepy Hig. Med. Dosw. 2016, 70, 981–988. [Google Scholar] [CrossRef] [PubMed]
- Kumar, K.G.; Trevaskis, J.L.; Lam, D.D.; Sutton, G.M.; Koza, R.A.; Chouljenko, V.N.; Kousoulas, K.G.; Rogers, P.M.; Kesterson, R.A.; Thearle, M.; et al. Identification of adropin as a secreted factor linking dietary macronutrient intake with energy homeostasis and lipid metabolism. Cell Metab. 2008, 8, 468–481. [Google Scholar] [CrossRef] [PubMed]
- Ganesh Kumar, K.; Zhang, J.; Gao, S.; Rossi, J.; McGuinness, O.P.; Halem, H.H.; Culler, M.D.; Mynatt, R.L.; Butler, A.A. Adropin deficiency is associated with increased adiposity and insulin resistance. Obesity 2012, 20, 1394–1402. [Google Scholar] [CrossRef]
- Akcılar, R.; Emel Koçak, F.; Şimşek, H.; Akcılar, A.; Bayat, Z.; Ece, E.; Kökdaşgil, H. The effect of adropin on lipid and glucose metabolism in rats with hyperlipidemia. Iran J. Basic Med. Sci. 2016, 19, 245–251. [Google Scholar]
- Butler, A.A.; Tam, C.S.; Stanhope, K.L.; Wolfe, B.M.; Ali, M.R.; O’Keeffe, M.; St-Onge, M.P.; Ravussin, E.; Havel, P.J. Low circulating adropin concentrations with obesity and aging correlate with risk factors for metabolic disease and increase after gastric bypass surgery in humans. J. Clin. Endocrinol. Metab. 2012, 97, 3783–3791. [Google Scholar] [CrossRef]
- Thapa, D.; Xie, B.; Manning, J.R.; Zhang, M.; Stoner, M.W.; Huckestein, B.R.; Edmunds, L.R.; Zhang, X.; Dedousis, N.L.; O’Doherty, R.M.; et al. Adropin reduces blood glucose levels in mice by limiting hepatic glucose production. Physiol. Rep. 2019, 7, 14043. [Google Scholar] [CrossRef]
- Lovren, F.; Pan, Y.; Quan, A.; Singh, K.K.; Shukla, P.C.; Gupta, M.; Al-Omran, M.; Teoh, H.; Verma, S. Adropin is a novel regulator of endothelial function. Circulation 2010, 122, 931782. [Google Scholar] [CrossRef]
- Gulen, B.; Eken, C.; Kucukdagli, O.T.; Serinken, M.; Kocyigit, A.; Kılıc, E.; Uyarel, H. Adropin levels and target organ damage secondary to high blood pressure in the ED. Am. J. Emerg. Med. 2016, 34, 2061–2064. [Google Scholar] [CrossRef] [PubMed]
- Bolayır, H.A.; Kıvrak, T.; Gunes, H.; Bolayır, A.; Karaca, I. Adropin and circadian variation of blood pressure. Kardiol. Pol. 2018, 76, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.Y.; Zhao, P.; Wu, M.C.; Liu, J.; Yin, W. Serum adropin levels are decreased in patients with acute myocarDial. infarction. Regul. Pept. 2014, 191, 46–49. [Google Scholar] [CrossRef]
- Bozic, J.; Borovac, J.A.; Galic, T.; Kurir, T.T.; Supe-Domic, D.; Dogas, Z. Adropin and Inflammation Biomarker Levels in Male Patients With Obstructive Sleep Apnea: A Link With Glucose Metabolism and Sleep Parameters. J. Clin. Sleep Med. 2018, 14, 1109–1118. [Google Scholar] [CrossRef] [PubMed]
- Brnić, D.; Martinovic, D.; Zivkovic, P.M.; Tokic, D.; Tadin Hadjina, I.; Rusic, D.; Vilovic, M.; Supe-Domic, D.; Tonkic, A.; Bozic, J. Serum adropin levels are reduced in patients with inflammatory bowel diseases. Sci. Rep. 2020, 10, 9264. [Google Scholar] [CrossRef]
- Kuliczkowska-Płaksej, J.; Mierzwicka, A.; Jończyk, M.; Stachowska, B.; Urbanovych, A.; Bolanowski, M. Adropin in women with polycystic ovary syndrome. Endokrynol. Pol. 2019, 70, 151–156. [Google Scholar] [CrossRef]
- Tičinović Kurir, T.; Miličević, T.; Novak, A.; Vilović, M.; Božić, J. Adropin—Potential Link in Cardiovascular Protection for Obese Male Type 2 Diabetes Mellitus Patients Treated with Liraglutide. Acta Clin. Croat. 2020, 59, 344–350. [Google Scholar] [CrossRef]
- Roumeliotis, S.; Stamou, A.; Roumeliotis, A.; Theodoridis, M.; Leivaditis, K.; Panagoutsos, S.; Liakopoulos, V. Red Blood Cell Distribution Width Is Associated with Deterioration of Renal Function and Cardiovascular Morbidity and Mortality in Patients with Diabetic Kidney Disease. Life 2020, 10, 301. [Google Scholar] [CrossRef]
- Cerqueira, A.; Quelhas-Santos, J.; Sampaio, S.; Ferreira, I.; Relvas, M.; Marques, N.; Dias, C.C.; Pestana, M. Endothelial Dysfunction Is Associated with Cerebrovascular Events in Pre-Dialysis CKD Patients: A Prospective Study. Life 2021, 11, 128. [Google Scholar] [CrossRef]
- Mikolasevic, I.; Žutelija, M.; Mavrinac, V.; Orlic, L. Dyslipidemia in patients with chronic kidney disease: Etiology and management. Int. J. Nephrol. Renovasc. Dis. 2017, 10, 35–45. [Google Scholar] [CrossRef]
- Spoto, B.; Pisano, A.; Zoccali, C. Insulin resistance in chronic kidney disease: A systematic review. Am. J. Physiol. Renal Physiol. 2016, 311, F1087–F1108. [Google Scholar] [CrossRef]
- Mihai, S.; Codrici, E.; Popescu, I.D.; Enciu, A.M.; Albulescu, L.; Necula, L.G.; Mambet, C.; Anton, G.; Tanase, C. Inflammation-Related Mechanisms in Chronic Kidney Disease Prediction, Progression, and Outcome. J. Immunol. Res. 2018, 6. [Google Scholar] [CrossRef] [PubMed]
- Ikizler, T.A. Optimal nutrition in hemodialysis patients. Adv. Chronic Kidney Dis. 2013, 20, 181–189. [Google Scholar] [CrossRef]
- Grzegorzewska, A.E.; Niepolski, L.; Mostowska, A.; Warchoł, W.; Jagodziński, P.P. Involvement of adropin and adropin-associated genes in metabolic abnormalities of hemodialysis patients. Life Sci. 2016, 160, 41–46. [Google Scholar] [CrossRef]
- Kałużna, M.; Pawlaczyk, K.; Schwermer, K.; Hoppe, K.; Człapka-Matyasik, M.; Ibrahim, A.Y.; Sawicka-Gutaj, N.; Minczykowski, A.; Ziemnicka, K.; Oko, A.; et al. Adropin and irisin: New biomarkers of cardiac status in patients with end-stage renal disease? A preliminary study. Adv. Clin. Exp. Med. 2019, 28, 347–353. [Google Scholar] [CrossRef]
- Kałużna, M.; Hoppe, K.; Schwermer, K.; Ibrahim, A.Y.; Pawlaczyk, K.; Ziemnicka, K. Adropin and irisin levels in relation to nutrition, body composition, and insulin resistance in patients with end-stage renal disease on chronic hemodialysis and peritoneal dialysis. Pol. Arch. Med. Wewn. 2016, 126, 474–482. [Google Scholar] [CrossRef][Green Version]
- Jackson, A.S.; Ellis, K.J.; McFarlin, B.K.; Sailors, M.H.; Bray, M.S. Cross-validation of generalised body composition equations with diverse young men and women: The Training Intervention and Genetics of Exercise Response (TIGER) Study. Br. J. Nutr. 2009, 101, 871–878. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Kopple, J.D.; Block, G.; Humphreys, M.H. A malnutrition-inflammation score is correlated with morbidity and mortality in maintenance hemodialysis patients. Am. J. Kidney Dis. 2001, 38, 1251–1263. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K.; Kleiner, M.; Dunne, E.; Lee, G.H.; Luft, F.C. A modified quantitative subjective global assessment of nutrition for dialysis patients. Nephrol. Dial. Transpl. 1999, 14, 1732–1738. [Google Scholar] [CrossRef] [PubMed]
- Hu, W.; Chen, L. Association of Serum Adropin Concentrations with Diabetic Nephropathy. Mediat. Inflamm. 2016, 6038261, 28. [Google Scholar] [CrossRef]
- Kuloglu, T.; Aydin, S. Immunohistochemical expressions of adropin and ınducible nitric oxide synthase in renal tissues of rats with streptozotocin-ınduced experimental diabetes. Biotech. Histochem. 2014, 89, 104–110. [Google Scholar] [CrossRef]
- Gu, X.; Li, H.; Zhu, X.; Gu, H.; Chen, J.; Wang, L.; Harding, P.; Xu, W. Inverse Correlation Between Plasma Adropin and ET-1 Levels in Essential Hypertension: A Cross-Sectional Study. Medicine 2015, 94, e1712. [Google Scholar] [CrossRef]
- Topuz, M.; Celik, A.; Aslantas, T.; Demir, A.K.; Aydin, S. Plasma adropin levels predict endothelial dysfunction like flow-mediated dilatation in patients with type 2 diabetes mellitus. J. Investig. Med. 2013, 61, 1161–1164. [Google Scholar] [CrossRef]
- Yang, C.; DeMars, K.M.; Candelario-Jalil, E. Age-Dependent Decrease in Adropin is Associated with Reduced Levels of Endothelial Nitric Oxide Synthase and Increased Oxidative Stress in the Rat Brain. Aging Dis. 2018, 9, 322–330. [Google Scholar] [CrossRef]
- Chen, X.; Xue, H.; Fang, W.; Chen, K.; Chen, S.; Yang, W.; Shen, T.; Zhang, P.; Ling, W. Adropin protects against liver injury in nonalcoholic steatohepatitis via the Nrf2 mediated antioxidant capacity. Redox Biol. 2019, 21, 6. [Google Scholar] [CrossRef] [PubMed]
- Bellezza, I.; Giambanco, I.; Minelli, A.; Donato, R. Nrf2-Keap1 signaling in oxidative and reductive stress. Biochim. Biophys Acta Mol. Cell Res. 2018, 5, 721–733. [Google Scholar] [CrossRef] [PubMed]
- Liakopoulos, V.; Roumeliotis, S.; Zarogiannis, S.; Eleftheriadis, T.; Mertens, P.R. Oxidative stress in hemodialysis: Causative mechanisms, clinical implications, and possible therapeutic interventions. Semin. Dial. 2019, 32, 58–71. [Google Scholar] [CrossRef] [PubMed]
- Zang, H.; Jiang, F.; Cheng, X.; Xu, H.; Hu, X. Serum adropin levels are decreased in Chinese type 2 diabetic patients and negatively correlated with body mass index. Endocr. J. 2018, 65, 685–691. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.; Fang, J.; Chen, L.; Zhao, Z.; Luo, Y.; Lin, C.; Fan, L. Low serum adropin is associated with coronary atherosclerosis in type 2 diabetic and non-diabetic patients. Clin. Chem. Lab. Med. 2014, 52, 751–758. [Google Scholar] [CrossRef]
- Aydin, S. Three new players in energy regulation: Preptin, adropin and irisin. Peptides 2014, 56, 94–110. [Google Scholar] [CrossRef]
- Grzegorzewska, A.E.; Niepolski, L.; Świderska, M.K.; Mostowska, A.; Stolarek, I.; Warchoł, W.; Figlerowicz, M.; Jagodziński, P.P. ENHO, RXRA, and LXRA polymorphisms and dyslipidaemia, related comorbidities and survival in haemodialysis patients. BMC Med. Genet. 2018, 19, 194. [Google Scholar] [CrossRef]
- Ghoshal, S.; Stevens, J.R.; Billon, C.; Girardet, C.; Sitaula, S.; Leon, A.S.; Rao, D.C.; Skinner, J.S.; Rankinen, T.; Bouchard, C.; et al. Adropin: An endocrine link between the biological clock and cholesterol homeostasis. Mol. Metab. 2018, 8, 51–64. [Google Scholar] [CrossRef]
- Stevens, J.R.; Kearney, M.L.; St-Onge, M.P.; Stanhope, K.L.; Havel, P.J.; Kanaley, J.A.; Thyfault, J.P.; Weiss, E.P.; Butler, A.A. Inverse association between carbohydrate consumption and plasma adropin concentrations in humans. Obesity 2016, 24, 1731–1740. [Google Scholar] [CrossRef]
- Yosaee, S.; Khodadost, M.; Esteghamati, A.; Speakman, J.R.; Shidfar, F.; Nazari, M.N.; Bitarafan, V.; Djafarian, K. Metabolic Syndrome Patients Have Lower Levels of Adropin When Compared With Healthy Overweight/Obese and Lean Subjects. Am. J. Mens Health 2017, 11, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.B.; Chu, N.F.; Lin, F.H.; Hsu, J.T.; Chen, P.Y. Relationship between plasma adropin levels and body composition and lipid characteristics amongst young adolescents in Taiwan. Obes. Res. Clin. Pract. 2018, 12, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.N.; Yim, J.E. Plasma Adropin as a Potential Marker Predicting Obesity and Obesity-associated Cancer in Korean Patients With Type 2 Diabetes Mellitus. J. Cancer Prev. 2018, 23, 191–196. [Google Scholar] [CrossRef]
- Jasaszwili, M.; Wojciechowicz, T.; Billert, M.; Strowski, M.Z.; Nowak, K.W.; Skrzypski, M. Effects of adropin on proliferation and differentiation of 3T3-L1 cells and rat primary preadipocytes. Mol. Cell Endocrinol. 2019, 496, 110532. [Google Scholar] [CrossRef] [PubMed]
| Parameter | HD Group (N = 70) | Control Group (N = 60) | p * |
|---|---|---|---|
| Male gender (N, %) | 28 (40) | 24 (40) | 0.857 |
| Age (years) | 69.2 ± 13.0 | 66.8 ± 15.8 | 0.349 |
| Body weight (kg) | 74.5 ± 16.1 | 78.9 ± 14.7 | 0.111 |
| Body height (cm) | 173.6 ± 10.1 | 176.7 ± 9.7 | 0.084 |
| Body mass index (kg/m2) | 24.4 ± 5.1 | 25.2 ± 4.2 | 0.299 |
| Waist circumference (cm) | 98.2 ± 12.72 | 100.25 ± 12.1 | 0.354 |
| Hip circumference (cm) | 104.2 ± 10.5 | 107.2 ± 9.1 | 0.086 |
| Pre-dialysis systolic pressure (mmHg) | 136.2 ± 26.9 | - | - |
| Post-dialysis systolic pressure (mmHg) | 122.9 ± 26.6 | 119.5 ± 8.0 † | 0.502 |
| Pre-dialysis diastolic pressure (mmHg) | 71.0 ± 16.3 | - | - |
| Post-dialysis diastolic pressure (mmHg) | 69.2 ± 15.1 | 71.7 ± 8.5 † | 0.257 |
| Smoking (N, %) | 20 (28.6) | 13 (21.7) | 0.484 |
| Diabetes mellitus (N, %) | 18 (25.7) | - | - |
| HbA1C (%) | 6.89 ± 1.16 | 5.61 ± 0.34 | <0.001 |
| CKD duration (years) | 12 (7–31) | - | - |
| HD duration (years) | 4.5 (3–9) | - | - |
| Prior kidney transplantation (N, %) | 8 (11.4) | - | - |
| Prior PD (N, %) | 5 (7.1) | - | - |
| Urine output (mL) | 200 (0–1000) | - | - |
| DMS | 13 (10–16) | - | - |
| MIS | 6 (4–9) | - | - |
| Body fat percentage (%) | 22.8 ± 7.7 | 21.6 ± 6.6 | 0.359 |
| Dry body weight (kg) ‡ | 72.79 ± 15.64 | - | - |
| IDWG (kg) | 2.25 ± 0.84 | - | - |
| Parameter | HD Group (N = 70) | Control Group (N = 60) | p * |
|---|---|---|---|
| Hemoglobin (g/L) | 111.0 ± 9.9 | 127.6 ± 10.6 | <0.001 |
| Fasting glucose (mmol/L) | 5.4 (4.7–6.9) | 5.6 ± (5.0–6.2) | 0.503 |
| Pre-dialysis urea (mmol/L) | 23.1 ± 5.6 | - | - |
| Post-dialysis urea (mmol/L) | 7.6 ± 3.1 | 5.7 ± 2.6 † | <0.001 |
| Pre-dialysis creatinine (μmol/L) | 823.3 ± 191.8 | - | - |
| Post-dialysis creatinine (μmol/L) | 297.5 (245.0–376.0) | 76.0 (71.0–85.0) † | <0.001 |
| Total bilirubin (μmol/L) | 9.3 ± 3.0 | 10.8 ± 3.5 | 0.179 |
| Total proteins (g/L) | 65.8 ± 4.9 | 69.6 ± 4.2 | <0.001 |
| Albumins (g/L) | 38.8 ± 3.0 | 40.4 ± 4.2 | 0.017 |
| hsCRP (mg/L) | 5.2 ± 3.6 | 1.4 ± 0.7 | <0.001 |
| Triglycerides (mmol/L) | 1.9 ± 0.9 | 1.6 ± 0.8 | 0.108 |
| Total cholesterol (mmol/L) | 4.5 ± 0.9 | 4.42 ± 0.8 | 0.624 |
| HDL (mmol/L) | 1.0 ± 0.2 | 1.1 ± 0.2 | 0.005 |
| LDL (mmol/L) | 1.9 ± 0.9 | 1.6 ± 0.8 | 0.152 |
| Parameter | r * (p) | p |
|---|---|---|
| Total proteins (g/L) | −0.118 | 0.327 |
| Albumins (g/L) | −0.131 | 0.278 |
| Total bilirubin (μmol/L) | 0.158 | 0.190 |
| Fasting glucose (mmol/L) | −0.140 † | 0.247 |
| hsCRP (mg/L) | −0.646 | <0.001 |
| Pre-dialysis systolic pressure (mmHg) | −0.301 | 0.011 |
| Post-dialysis systolic pressure (mmHg) | −0.124 | 0.306 |
| Pre-dialysis diastolic pressure (mmHg) | −0.299 | 0.011 |
| Post-dialysis diastolic pressure (mmHg) | −0.184 | 0.127 |
| Age (years) | 0.109 | 0.366 |
| Body mass index (kg/m2) | −0.234 | 0.051 |
| Waist circumference (cm) | −0.141 | 0.242 |
| Hip circumference (cm) | −0.058 | 0.631 |
| CKD duration (years) | 0.194 † | 0.106 |
| DMS | −0.350 † | 0.003 |
| MIS | −0.476 † | <0.001 |
| HD duration (years) | −0.305 † | 0.010 |
| Variable | β * | SE † | t Value | p |
|---|---|---|---|---|
| Age | −0.0006532 | 0.005 | −0.123 | 0.902 |
| Gender | −0.021 | 0.041 | −0.517 | 0.607 |
| BMI | −0.027 | 0.013 | −2.006 | 0.049 |
| HD duration | −0.031 | 0.009 | −3.382 | 0.001 |
| hsCRP | −0.058 | 0.019 | −2.985 | 0.004 |
| MIS | −0.310 | 0.140 | −2.211 | 0.030 |
| DMS | 0.054 | 0.037 | 1.438 | 0.155 |
| Body fat | −0.053 | 0.020 | −2.631 | 0.010 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boric-Skaro, D.; Mizdrak, M.; Luketin, M.; Martinovic, D.; Tokic, D.; Vilovic, M.; Supe-Domic, D.; Kurir, T.T.; Bozic, J. Serum Adropin Levels in Patients on Hemodialysis. Life 2021, 11, 337. https://doi.org/10.3390/life11040337
Boric-Skaro D, Mizdrak M, Luketin M, Martinovic D, Tokic D, Vilovic M, Supe-Domic D, Kurir TT, Bozic J. Serum Adropin Levels in Patients on Hemodialysis. Life. 2021; 11(4):337. https://doi.org/10.3390/life11040337
Chicago/Turabian StyleBoric-Skaro, Dijana, Maja Mizdrak, Mirko Luketin, Dinko Martinovic, Daria Tokic, Marino Vilovic, Daniela Supe-Domic, Tina Ticinovic Kurir, and Josko Bozic. 2021. "Serum Adropin Levels in Patients on Hemodialysis" Life 11, no. 4: 337. https://doi.org/10.3390/life11040337
APA StyleBoric-Skaro, D., Mizdrak, M., Luketin, M., Martinovic, D., Tokic, D., Vilovic, M., Supe-Domic, D., Kurir, T. T., & Bozic, J. (2021). Serum Adropin Levels in Patients on Hemodialysis. Life, 11(4), 337. https://doi.org/10.3390/life11040337







