Developing Lactic Acid Bacteria as an Oral Healthy Food
Abstract
1. Introduction
2. Materials and Methods
2.1. Anti-Carious and Anti-Periodontal Pathogens Functional Tests
2.1.1. Lactic Acid Bacteria
2.1.2. Bacteria of Dental Caries and Periodontal Disease
2.2. Screening of LAB Inhibition Oral Pathogens
2.2.1. Crude Bacteriocin Extraction
2.2.2. Anti-Oral Pathogenic Bacteria Test
2.3. Confirm Test of Anti-Cariogenic Bacteria and Anti-Periodontal Disease Bacteria
2.3.1. Testing of Coincubation of LAB and Oral Pathogens
2.3.2. Observing of Co-Aggregation
2.4. The Study of Optimal Culture Conditions of Target Strains
2.5. Preparation, Drying the Cultured Fluid of Target Strains, and Identification of the Strains
2.5.1. Preparation, Drying the Cultured Fluid Samples of the Target Strains
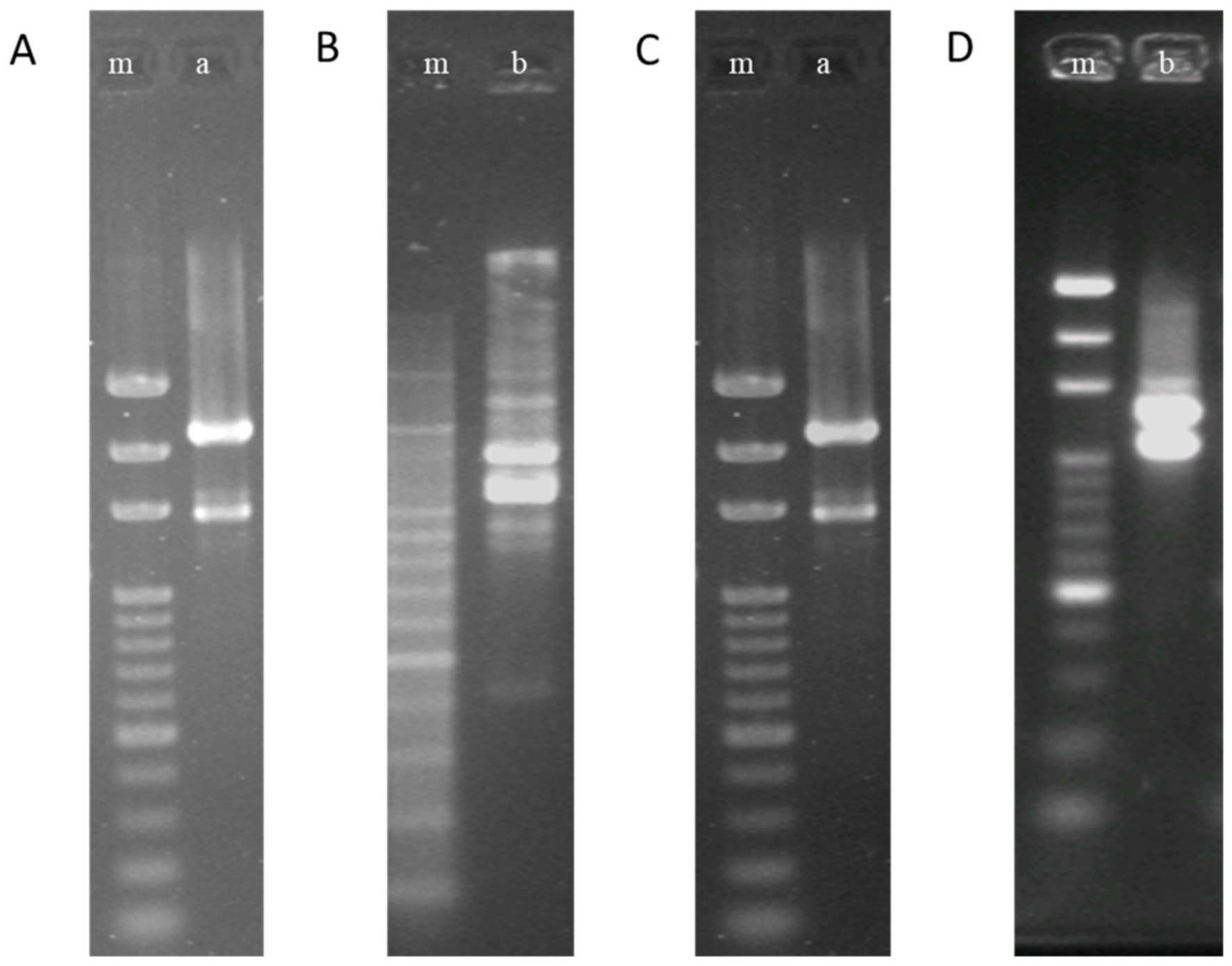
2.5.2. Identification of Strains
2.6. Healthy Food Product Design, Manufacturing, and Quality Evaluation
2.6.1. Shape, Size, and Prescription Design
2.6.2. Measurement of Heat-Inactivated LAB Biomass
2.7. Quality Evaluation and Improvement of Tablets
2.8. The Storability Test and Setting the Product Shelf Life
2.9. Clinical Trial of Periodontal Therapy
2.9.1. The Growth Inhibition of Periodontal Pathogens
2.9.2. Improvement of Periodontal Probing Depth (PPD)
2.9.3. Changes of Halitosis Following Treatment
2.10. Statistical Analysis
3. Results
3.1. Screening of LAB Inhibition Pathogens
3.2. Results of Confirm Tests of Antipathogens Activity
3.2.1. Testing of Coincubation of LAB with Oral Pathogens
3.2.2. Observing Co-Aggregation
3.3. The results of the Optimal Culture Conditions Research of Target Strains
3.4. Results of LAB Powder Preparation and Drying
3.5. Results of Tablet Preparation and Quality Evaluation
3.6. Results of Storability Test and Setting the Product Shelf Life
3.7. Clinical Trials of Tablet Product
3.7.1. Inhibiting the Growth of Periodontal Pathogens
3.7.2. Improvement of Probing Pocket Depth (PPD)
3.7.3. Changes of halitosis following treatment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zheng, J.; Wittouck, S.; Salvetti, E.; Franz, C.M.A.P.; Harris, H.M.B.; Mattarelli, P.; O’Toole, P.W.; Pot, B.; Vandamme, P.; Walter, J.; et al. A taxonomic note on the genus Lactobacillus: Description of 23 novel genera, emended description of the genus Lactobacillus Beijerinck 1901, and union of Lactobacillaceae and Leuconostocaceae. Int. J. Syst. Evol. Microbiol. 2020, 70, 2782–2858. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Cano, I.; Rocha-Mendoza, D.; Ortega-Anaya, J.; Wang, K.; Kosmerl, E.; Jimenez-Flores, R. Lactic acid bacteria isolated from dairy products as potential producers of lipolytic, proteolytic and antibacterial proteins. Appl. Microbiol. Biotechnol. 2019, 103, 5243–5257. [Google Scholar] [CrossRef] [PubMed]
- Helander, I.M.; von Wright, A. Mattila-Sandholm, T-M. Potential of lactic acid bacteria and novel antimicrobials against Gram-negative bacteria. Trends Food Sci. Technol. 1997, 8, 146–150. [Google Scholar] [CrossRef]
- Bintsis, T. Lactic acid bacteria as starter cultures: An update in their metabolism and genetics. AIMS Microbiol. 2018, 4, 665–684. [Google Scholar] [CrossRef]
- Zielinska, D.; Kolozyn-Krajewska, D. Food-origin lactic acid bacteria may exhibit probiotic properties. Review. Biomed. Res. Int. 2018, 5063185. [Google Scholar] [CrossRef]
- Corr, S.C.; Li, Y.; Riedel, C.U.; O’Toole, P.W.; Hill, C.; Gahan, C.G. Bacteriocin production as a mechanism for the antiinfective activity of Lactobacillus salivarius UCC118. Proc. Natl. Acad. Sci. USA 2007, 104, 7617–7621. [Google Scholar] [CrossRef]
- Ji, J.; Yang, H. Using probiotics as supplementation for Helicobacter pylori antibiotic therapy. Int. J. Mol. Sci. 2020, 21, 1136. [Google Scholar] [CrossRef]
- Karska-Wysocki, B.; Bazo, M.; Smoragiewicz, W. Antibacterial activity of Lactobacillus acidophilus and Lactobacillus casei against methicillin-resistant Staphylococcus aureus (MRSA). Microbiol. Res. 2010, 165, 674–686. [Google Scholar] [CrossRef]
- Abbasi, J. Are probiotics money down the toilet? Or Worse? JAMA 2019, 321, 633–635. [Google Scholar] [CrossRef]
- Zmora, N.; Zilberman-Schapira, G.; Suez, J.; Mor, U.; Dori-Bachash, M.; Bashiardes, S.; Kotler, E.; Zur, M.; Regev-Lehavi, D.; Ben-Zeev, R.B.; et al. Personalized gut mucosal colonization resistance to empiric probiotics is associated with unique host and microbiome features. Cell 2018, 174, 1388–1405. [Google Scholar] [CrossRef]
- Drider, D.; Bendali, F.; Naghmouchi, K.; Chikindas, M.L. Bacteriocins: Not only antibacterial agents. Probiotics Antimicro Prot. 2016. [Google Scholar] [CrossRef]
- Wang, J.; Jiang, Y.; Yu, P.; Lee, Y.K.; Liu, X.; Zhao, J.; Zhang, H.; Chen, W. Effect of carbon catabolite repression on lactose and galactose catabolism in Lacticaseibacillus paracasei. Food Biosci. 2021, 40. [Google Scholar] [CrossRef]
- Sookkhee, S.; Chulasiri, M.; Prachyabrued, W. Lactic acid bacteria from healthy oral cavity of Thai volunteers: Inhibition of oral pathogens. J. Appl. Microbiol. 2001, 90, 172–179. [Google Scholar] [CrossRef]
- Fang, F.; Xu, J.; Li, Q.; Xia, X.; Du, G. Characterization of a Lactobacillus brevis strain with potential oral probiotic properties. BMC Microbiol. 2018, 18, 221. [Google Scholar] [CrossRef]
- Do, K.H.; Park, H.E.; Kang, M.S.; Kim, J.T.; Yeu, J.E.; Lee, W.K. Effects of Weissella cibaria CMU on halitosis and calculus, plaque, and gingivitis indices in beagles. J. Vet. Dent. 2019, 36, 135–142. [Google Scholar] [CrossRef]
- Kacker, R.N.; Lagergren, E.S.; Filliben, J.J. Taguchi’s orthogonal arrays are classical designs of experiments. J. Res. Natl. Inst. Stand Technol. 1991, 96, 577–591. [Google Scholar] [CrossRef]
- Park, J.M.; Koh, J.H.; Kim, J.M. Predicting shelf-life of ice cream by accelerated conditions. Korean J. Food Sci. Anim. Resour. 2018, 38, 1216–1225. [Google Scholar] [CrossRef]
- Hyvärinen, K.; Laitinen, S.; Paju, S.; Hakala, A.; Suominen-Taipale, L.; Skurnik, M.; Könönen, E.; Pussinen, P.J. Detection and quantification of five major periodontal pathogens by single copy gene-based real-time PCR. Innate Immun. 2009, 15, 195–204. [Google Scholar] [CrossRef]
- Mummolo, S.; Tieri, M.; Nota, A.; Caruso, S.; Albani, F.; Gatto, R.; Marzo, G.; Marchetti, E.; Quinzi, V.; Tecco, S. Salivary concentrations of Streptococcus mutans and Lactobacilli during an orthodontic treatment. An observational study comparing fixed and removable orthodontic appliances. Clin. Exp. Dental Res. 2020, 6, 181–187. [Google Scholar] [CrossRef]
- Janković, T.; Frece, J.; Abram, M.; Gobin, I. Aggregation ability of potential probiotic Lactobacillus plantarum strains. International. J. Sanit. Eng. Res. 2012, 6, 19–24. [Google Scholar]
- Terai, T.; Okumura, T.; Imai, S. Screening of probiotic candidates in human oral bacteria for the prevention of dental disease. PLoS ONE 2015, 10, e0128657. [Google Scholar] [CrossRef] [PubMed]
- Parente, E.; Ricciardi, A. Production, recovery and purification of bacteriocins from lactic acid bacteria. Appl. Microbiol. Biotechnol. 1999, 52, 628–638. [Google Scholar] [CrossRef] [PubMed]
- NCCLS. Performance Standards for Antimicrobial Disc Suspectibility Tests; Approved Standard NCCLS Publication M2-A5: Villanova, PA, USA, 1993. [Google Scholar]
- Witt, J.; Ramji, N.; Gibb, R.; Dunavent, J.; Flood, J.; Barnes, J. Antibacterial and antiplaque effects of a novel, alcohol-free oral rinse with cetylpyridinium chloride. J. Contemp. Dent. Pract. 2005, 6, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Venkata, M.S.; Venkateswar, R.M. Optimization of critical factors to enhance polyhydroxyalkanoates (PHA) synthesis by mixed culture using Taguchi design of experimental methodology. Bioresour. Technol. 2013, 128, 409–416. [Google Scholar] [CrossRef]
- Fonseca, F.; Cenard, S.; Passot, S. Freeze-drying of lactic acid bacteria. Methods Mol. Biol. 2015, 1257, 477–488. [Google Scholar] [CrossRef]
- Gajardo, M.; Silva, N.; Gomez, L. Prevalence of periodontopathic bacteria in aggressive periodontitis patients in a Chilean population. J. Periodontol. 2005, 76, 289–294. [Google Scholar] [CrossRef]
- Moore, W.E.; Holdeman, L.V.; Smibert, R.M.; Hash, D.E.; Burmeister, J.A.; Ranney, R.R. Bacteriology of severe periodontitis in young adult humans. Infect. Immun. 1982, 38, 1137–1148. [Google Scholar] [CrossRef]
- Hefti, A.F. Periodontal probing. Crit. Rev. Oral. Biol. Med. 1997, 8, 336–356. [Google Scholar] [CrossRef]
- Soares, L.G.; Carvalho, E.B.; Tinoco, E.M.B. Clinical effect of Lactobacillus on the treatment of severe periodontitis and halitosis: A double-blinded, placebo-controlled, randomized clinical trial. Am. J. Dent. 2019, 32, 9–13. [Google Scholar] [CrossRef]
- Ishikawa, H.; Aiba, Y.; Nakanishi, M.; Oh-hashi, Y.; Koga, Y. Suppression of periodontal pathogenic bacteria in the saliva of humans by the administration of Lactobacillus salivarius TI 2711. J. Jpn. Soc. Periodontol. 2003, 45, 105–112. [Google Scholar] [CrossRef]
- Matsuoka, T.; Nakanishi, M.; Aiba, Y.; Koga, Y. Mechanism of Porphyromonas gingivalis killing by Lactobacillus salivarius TI 2711. J. Jpn. Soc. Periodontol. 2004, 46, 118–126. [Google Scholar] [CrossRef]
- Kang, M.S.; Na, H.S.; Oh, J.S. Coaggregation ability of Weissella cibaria isolates with Fusobacterium nucleatum and their adhesiveness to epithelial cells. FEMS Microbiol. Lett. 2005, 253, 323–329. [Google Scholar] [CrossRef]
- She, Y.; Luo, F.; Gao, W.; Li, X.; Liu, X. New progress in research on adhesion characteristics of lactic acid bacteria. Food Res. Development. 2018, 39, 218–224. [Google Scholar] [CrossRef]
- Gonzalez, A.B.; Camara, V.L.; Castellanos, A.G. Prevention of caries with Lactobacillus (final results of a clinical trial on dental caries with killed Lactobacillus [Sreptococcus and Lactobacillus] given orally). Pract. Odontol. 1990, 11, 37–39. [Google Scholar]
- Teughels, W.; Durukan, A.; Ucak, O.; Pauwels, M. Clinical and microbiological effects of Lactobacillus reuteri probiotics in the treatment of chronic periodontitis: A randomized placebo-controlled study. 2013; Volume 40, pp. 1025–1035. [Google Scholar] [CrossRef]
- Ahirwar, S.S.; Gupta, M.K.; Snehi, S.K. Dental caries and Latobacillus: Role and ecology in the oral cavity. IJPSR 2019, 10, 4818–4829. [Google Scholar]
| Strains of LAB a | Conc. of LAB (cells/mL) b | S. mutants | P. gingivalis | ||||
|---|---|---|---|---|---|---|---|
| 0 h c | 6 h | 24 h | 0 h | 6 h | 24 h | ||
| Lb. paracasei 111 | 1.0 × 107 | 10.0 ± 1.0 | 165.0 ± 39.7 | 172.3 ± 7.0 | 1050.0 ± 79.4 | 2356.7 ± 197.3 | 2693.3 ± 86.2 |
| 1.0 × 108 | 14.3 ± 3.1 | 13.3 ± 2.1 | 23.3 ± 1.5 | 833.3 ± 32.1 | 1990.0 ± 65.6 | 2240.0 ± 81.9 | |
| 1.0 × 109 | 6.7 ± 3.2 | 6.3 ± 2.5 | 2.0 ± 2.6 | 770.0 ± 55.7 | 1213.3 ± 110.2 | 1546.7 ± 107.9 | |
| Lb. paracasei 127 | 1.0 × 107 | 84.0 ± 8.2 | 766.7 ± 41.6 | 786.7 ± 40.4 | 86.7 ± 19.3 | 261.3 ± 28.0 | 783.3 ± 20.8 |
| 1.0 × 108 | 75.3 ± 17.7 | 133.0 ± 17.6 | 273.3 ± 20.4 | 78.0 ± 8.0 | 104.0 ± 25.1 | 250.7 ± 11.0 | |
| 1.0 × 109 | 58.0 ± 4.6 | 71.0 ± 7.0 | 44.0 ± 17.1 | 73.0 ± 6.1 | 70.0 ± 22.5 | 61.0 ± 3.5 | |
| Lb. paracasei 141 | 1.0 × 107 | 1023.3 ± 37.9 | 2540.0 ± 247.6 | 2706.7 ± 102.1 | 18.3 ± 8.6 | 780.0 ± 75.5 | 2090.0 ± 50.0 |
| 1.0 × 108 | 933.3 ± 73.7 | 2073.3 ± 58.6 | 2390.0 ± 148.0 | 13.3 ± 5.7 | 206.7 ± 25.0 | 341.0 ± 60.7 | |
| 1.0 × 109 | 793.3 ± 45.1 | 1073.3 ± 47.3 | 1360.0 ± 40.0 | 21.0 ± 2.6 | 17.7 ± 4.9 | 37.7 ± 2.1 | |
| Llb. salivarius 285 | 1.0 × 107 | 970.0 ± 50.0 | 2280.0 ± 141.8 | 2700.0 ± 78.1 | 25.0 ± 7.0 | 893.3 ± 56.9 | 2306.7 ± 70.2 |
| 1.0 × 108 | 863.3 ± 15.3 | 2063.3 ± 35.1 | 2413.3 ± 174.7 | 21.0 ± 2.6 | 177.3 ± 8.6 | 328.0 ± 44.7 | |
| 1.0 × 109 | 766.7 ± 32.1 | 950.0 ± 26.5 | 1310.0 ± 105.4 | 17.3 ± 1.5 | 65.7 ± 13.7 | 49.7 ± 13.4 | |
| Llb. salivarius 296 | 1.0 × 107 | 866.7 ± 25.2 | 1810.0 ± 127.7 | 2060.0 ± 81.9 | 863.3 ± 46.2 | 1456.7 ± 455.4 | 2116.7 ± 196.6 |
| 1.0 × 108 | 766.7 ± 25.2 | 1183.3 ± 129.0 | 1620.0 ± 95.4 | 786.7 ± 65.1 | 1230.0 ± 434.9 | 1886.7 ± 238.0 | |
| 1.0 × 109 | 713.3 ± 15.3 | 793.3 ± 45.1 | 870.0 ± 55.7 | 740.0 ± 10.0 | 773.3 ± 145.7 | 830.0 ± 70.0 | |
| Strains of Lactic Acid Bacteria a | Conc. of LAB (cells/mL) b | Counts of S. mutans | Counts of P. gingivalis |
|---|---|---|---|
| Lb. paracasei 111 | 1.0 × 107 | 11.7 ± 3.5 | 1083.3 ± 92.9 |
| 1.0 × 108 | 10.7 ± 2.5 | 880.0 ± 65.6 | |
| 1.0 × 109 | 5.7 ± 2.5 | 756.7 ± 35.1 | |
| Lb. paracasei 127 | 1.0 × 107 | 83.7 ± 12.5 | 80.7 ± 11.2 |
| 1.0 × 108 | 69.0 ± 9.2 | 68.0 ± 3.0 | |
| 1.0 × 109 | 60.3 ± 9.4 | 61.0 ± 5.0 | |
| Lb. paracasei 141 | 1.0 × 107 | 1023.3 ± 70.9 | 13.7 ± 9.8 |
| 1.0 × 108 | 886.7 ± 20.8 | 15.0 ± 3.0 | |
| 1.0 × 109 | 710.0 ± 81.8 | 9.3 ± 2.5 | |
| Llb. salivarius 285 | 1.0 × 107 | 896.7 ± 40.4 | 22.7 ± 2.5 |
| 1.0 × 108 | 826.7 ± 61.1 | 21.3 ± 6.5 | |
| 1.0 × 109 | 760.0 ± 26.4 | 15.0 ± 1.0 | |
| Llb. salivarius 296 | 1.0 × 107 | 840.0 ± 55.7 | 102.3 ± 5.1 |
| 1.0 × 108 | 766.7 ± 20.8 | 42.0 ± 7.0 | |
| 1.0 × 109 | 720.0 ± 17.3 | 18.0 ± 3.6 |
| Strains of Lactic Acid Bacteria a | S. mutans | P. gingivalis | Lb. Paracasei 141 |
|---|---|---|---|
| Lb. paracasei 111 | 62.25 ± 3.46 | 11.47 ± 0.15 | 7.63 ± 0.43 * |
| Lb. paracasei 127 | 34.50 ± 2.65 | 30.133 ± 2.16 | - |
| Lb. paracasei 141 | 17.33 ± 4.80 | 58.97 ± 1.70 | - |
| Llb. salivarius 285 | 15.93 ± 2.86 | 57.33 ± 0.80 | - |
| Llb. salivarius 296 | 18.10 ± 0.70 | 59.27 ± 0.91 | - |
| Strain | Medium (w/w) | Culture Temperature | Controlled pH | Amount of Starter(v/v) | Speed of Feed ((v/v)/h) | ||
|---|---|---|---|---|---|---|---|
| Skim Milk Powder | Glucose | Growth Factor | |||||
| Lb. paracasei 111 | 10% | 2.0% | 2.0% | 37 ℃ | 5.8 | 7.0% | 10% |
| Lb. paracasei 141 | 8% | 3.0% | 2.5% | 35 ℃ | 6.3 | 5.0% | 9% |
| Strain | Powder Weight (Gram) | Loss on Drying (%, w/w) | Bacterial Biomass (Cells/g) |
|---|---|---|---|
| Lb. paracasei 111 | 403 | 2.9 ± 0.3 | 1.47 × 1011 ± 0.31 |
| Lb. paracasei 141 | 421 | 3.1 ± 0.2 | 1.12 × 1011 ± 0.26 |
| Ingredients a | Lb. paracasei 111 | Lb. paracasei 141 | Maltodextrin | Sorbitol | Xylitol | Silicon Dioxide | Flavor |
|---|---|---|---|---|---|---|---|
| Ratio b | 10% | 10% | 36% | 15% | 15% | 13% | 1% |
| Item | Inhibitory Effect on S. mutans | Inhibitory Effect on P. gingivalis | Disintegration Time | Flavor Quality b | Hardness | Loss on Drying |
|---|---|---|---|---|---|---|
| Data | 5 ± 3 a | 11 ± 2 a | 500 ± 7 sec | 7.8 ± 0.2 | 22.1 ± 0.5 kg | 4.32 ± 0.11% |
| Periodontal Diseases | Time | Placebo, n = 20 | Product, n = 20 | p Value a |
|---|---|---|---|---|
| Positive | Baseline | 10 | 8 | 0.404 |
| Negative | 10 | 12 | ||
| Positive | 4 weeks | 9 | 1 | 0.003 ** |
| Negative | 11 | 19 | ||
| Positive | 8 weeks | 9 | 1 | 0.003 ** |
| Negative | 11 | 19 | ||
| p value b | 0.999 | 0.016 * | ||
| p value c | 1.000 | 0.016 * | ||
| Index | Score (mm) | Treating Time | Placebo, n = 20 | Product, n = 20 | p Value a |
|---|---|---|---|---|---|
| PPD | <5.0 | Baseline | 0 | 1 | 0.311 |
| ≥5.0 | 20 | 19 | |||
| <5.0 | 4 weeks | 5 | 6 | 0.723 | |
| ≥5.0 | 15 | 14 | |||
| <5.0 | 8 weeks | 10 | 16 | 0.047 * | |
| ≥5.0 | 10 | 4 |
| Halitosis | Time | Placebo, n = 20 | Product, n = 20 | p Value a |
|---|---|---|---|---|
| Yes | 4 weeks | 3 | 9 | 0.038 * |
| No | 17 | 11 | ||
| Yes | 8 weeks | 6 | 11 | 0.110 |
| No | 14 | 9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lai, W.-K.; Lu, Y.-C.; Hsieh, C.-R.; Wei, C.-K.; Tsai, Y.-H.; Chang, F.-R.; Chan, Y. Developing Lactic Acid Bacteria as an Oral Healthy Food. Life 2021, 11, 268. https://doi.org/10.3390/life11040268
Lai W-K, Lu Y-C, Hsieh C-R, Wei C-K, Tsai Y-H, Chang F-R, Chan Y. Developing Lactic Acid Bacteria as an Oral Healthy Food. Life. 2021; 11(4):268. https://doi.org/10.3390/life11040268
Chicago/Turabian StyleLai, Wei-Kuang, Ying-Chen Lu, Chun-Ren Hsieh, Chien-Kei Wei, Yi-Hong Tsai, Fang-Rong Chang, and You Chan. 2021. "Developing Lactic Acid Bacteria as an Oral Healthy Food" Life 11, no. 4: 268. https://doi.org/10.3390/life11040268
APA StyleLai, W.-K., Lu, Y.-C., Hsieh, C.-R., Wei, C.-K., Tsai, Y.-H., Chang, F.-R., & Chan, Y. (2021). Developing Lactic Acid Bacteria as an Oral Healthy Food. Life, 11(4), 268. https://doi.org/10.3390/life11040268







