Impact of a Nutrition-Related Community Intervention on the Quantity and Quality of Children’s School almuerzo
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Study Population
2.2. Implementing the Intervention
2.2.1. Intervention Schools
2.2.2. Control Schools
2.3. Measurements
2.3.1. Sociodemographic Data
2.3.2. Anthropometric Measurements
2.3.3. Questionnaire Regarding Eating Habits and School almuerzo
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Obesity and Overweight. 2017. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 6 September 2019).
- Shamah-Levy, T.; Vielma-Orozco, E.; Heredia-Hernandez, O.; Romero-Martinez, M.; Mojica-Cuevas, J.; Cuevas-Nasu, L.; Santaella-Castell, J.A.; Rivera-Dommarco, J. Encuesta Nacional de Salud y Nutricion 2018-19: Resultados Nacionales; Instituto Nacional de Salud Publica: Cuernavaca, Mexico, 2020; Available online: https://ensanut.insp.mx/ (accessed on 15 January 2020).
- Hendrie, G.A.; Coveney, J.; Cox, D.N. Defining the complexity of childhood obesity and related behaviours within the family environment using structural equation modelling. Public Health Nutr. 2012, 15, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; van der Horst, K.; Jacquier, E.F.; Afeiche, M.C.; Eldridge, A.L. Snacking Patterns in Children: A Comparison between Australia, China, Mexico, and the US. Nutrients 2018, 10, 198. [Google Scholar] [CrossRef]
- Taillie, L.S.; Afeiche, M.C.; Eldridge, A.L.; Popkin, B.M. Increased Snacking and Eating Occasions Are Associated with Higher Energy Intake among Mexican Children Aged 2-13 Years. J. Nutr. 2015, 145, 2570–2577. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Salud Pública. Documento Técnico de Recomendaciones Para Guías de Alimentación en Escuelas Primarias Públicas. Caracterización del Ambiente Escolar en Escuelas Primarias de Estados de la República Mexicana y Recomendaciones Para un “Refrigerio Escolar Saludable”. 2010. Available online: https://www.insp.mx/images/stories/Centros/cinys/Docs/DOC_TECNICO_GUIAS_INSP_SSA_2010.pdf (accessed on 20 February 2020).
- Vargas, L.; Jimenez-Cruz, A.; Bacardí-Gascón, M. Unhealthy and Healthy Food Consumption Inside and Outside of the School by Pre-school and Elementary School Mexican Children in Tijuana, Mexico. J. Community Health 2013, 38, 1166–1174. [Google Scholar] [CrossRef] [PubMed]
- Vilchis-Gil, J.; Klünder-Klünder, M.; Duque, X.; Flores-Huerta, S. Decreased Body Mass Index in Schoolchildren After Yearlong Information Sessions With Parents Reinforced With Web and Mobile Phone Resources: Community Trial. J. Med. Internet Res. 2016, 18, e174. [Google Scholar] [CrossRef]
- Secretaría de Salud. Norma Oficial Mexicana NOM-043-SSA2-2012: Servicios Básicos De Salud. Promoción y Educación Para la Salud en Materia Alimentaria. Criterios Para Brindar Orientación. México. 2013. Available online: https://www.cndh.org.mx/DocTR/2016/JUR/A70/01/JUR-20170331-NOR37.pdf (accessed on 30 October 2020).
- WHO Expert Committee on Physical Status: The Use and Interpretation of Anthropometry; WHO Technical Report Series, No. 854; WHO: Geneva, Switzerland, 1995; pp. 4–33.
- World Health Organization. Growth Reference Data for School-Aged Children and Adolescents of 5–19 Years. 2007. Available online: http://www.who.int/growthref/en/ (accessed on 13 January 2020).
- Micha, R.; Karageorgou, D.; Bakogianni, I.; Trichia, E.; Whitsel, L.P.; Story, M.; Petalvo, J.L.; Mozaffarian, D. Effectiveness of school food environment policies on children’s dietary behaviors: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0194555. [Google Scholar] [CrossRef]
- Miyawaki, A.; Lee, J.S.; Kobayashi, Y. Impact of the school lunch program on overweight and obesity among junior high school students: A nationwide study in Japan. J. Public Health (Oxf.) 2019, 41, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Shamah, L.T.; Morales, R.C.; Benvecchio, A.A.; López, O.N. Evaluación de la Aplicación de la Tercera Etapa de los Lineamientos Para el Expendio de Alimentos y Bebidas en los Planteles de Educación Básica. Instituto Nacional de Salud Pública. 2014. Available online: https://www.insp.mx/epppo/blog/3180-lineamientos-alimentos-escuelas.html (accessed on 5 October 2020).
- World Bank. Taxes on Sugar-Sweetened Beverages: Summary of International Evidence and Experiences; World Bank: Washington, DC, USA, 2020; Available online: https://openknowledge.worldbank.org/handle/10986/33969 (accessed on 8 March 2021).
- Diario Oficial de la Federación. Excise Tax Law for Production and Services, DOF: 11/12/2013. 2013. Available online: http://www.dof.gob.mx/nota_detalle.php?codigo=5325371&fecha=11/12/2013 (accessed on 8 March 2021).
- Hernandez-F, M.; Batis, C.; Rivera, J.A.; Colchero, M.A. Reduction in purchases of energy-dense nutrient-poor foods in Mexico associated with the introduction of a tax in 2014. Prev. Med. 2019, 118, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, A.G.E.; Seira, E. The Effectiveness of without Food Taxes: Evidence from Mexico. Instituto Tecnológico Autónomo de México (ITAM) Working Paper. 2019. Available online: http://www.enriqueseira.com/uploads/3/1/5/9/31599787/obesidad_feb_13_2019_aejsub.pdf (accessed on 8 March 2021).
- Jiménez-Aguilar, A.; Muñoz-Espinosa, A.; Rodríguez-Ramírez, S.; Maya-Hernández, C.; Méndez Gómez-Humarán, I.; Uribe-Carvajal, R.; Salazar-Coronel, A.; Sachse-Aguilera, M.; Veliz, P.; Shamah-Levy, T. Plain water and sugar sweetened beverages intake and use of school drinking fountains in secondary schools of the National School Drinking Fountains Program in Mexico City. Salud Publica Mex. 2021, 63, 68–78. [Google Scholar] [CrossRef]
- Maersk, M.; Belza, A.; Staokilde-Jorgensen, H.; Ringgaard, S.; Chabanova, E.; Thomsen, H.; Pedersen, S.; Astrup, A.; Richelsen, B. Sucrose-sweetened beverages increase fat storage in the liver, muscle, and visceral fat depot: A 6-mo randomized intervention study. Am. J. Clin. Nutr. 2011, 95, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Ebbeling, C.B.; Feldman, H.A.; Chomitz, V.R.; Antonelli, T.A.; Gortmaker, S.L.; Osganian, S.K.; Ludwig, D.S. A randomized trial of sugar-sweetened beverages and adolescent body weight. N. Engl. J. Med. 2012, 367, 1407–1416. [Google Scholar] [CrossRef]
- Tani, Y.; Asakura, K.; Sasaki, S.; Hirota, N.; Notsu, A.; Todoriki, H.; Miura, A.; Fukui, M.; Date, C. The influence of season and air temperature on water intake by food groups in a sample of free-living Japanese adults. Eur. J. Clin. Nutr. 2015, 69, 907–913. [Google Scholar] [CrossRef] [PubMed]
- Meléndez, G. Factores Asociados con Sobrepeso y Obesidad en el Ambiente Escolar; Editorial Médica Panamericana: Ciudad de México, México, 2008. [Google Scholar]
- Diario Oficial de la Federación. Acuerdo Mediante el Cual se Establecen los Lineamientos Generales Para el Expendio y Distribución de Alimentos y Bebidas Preparados y Procesados en las Escuelas del Sistema Educativo Nacional. DOF: 16/05/2014; 2014. Available online: http://www.dof.gob.mx/nota_detalle.php?codigo=5344984&fecha=16/05/2014 (accessed on 9 March 2021).
- Flores-Huerta, S.; Klünder-Klünder, M.; Medina-Bravo, P. La escuela primaria como ámbito de oportunidad para prevenir el sobrepeso y la obesidad en los niños. Bol. Med. Hosp. Infant. Mex. 2008, 65, 626–638. Available online: http://www.scielo.org.mx/pdf/bmim/v65n6/v65n6a18.pdf (accessed on 10 October 2020).
- Vilchis-Gil, J.; Galvan-Portillo, M.; Klunder-Klunder, M.; Cruz, M.; Flores-Huerta, S. Food habits, physical activities and sedentary lifestyles of eutrophic and obese school children: A case and control study. BMC Public Health 2015, 15, 124. [Google Scholar] [CrossRef] [PubMed]
- Santillán, M.E.; Jiménez, C.A.; Bacardí, G.M. Programas para mejorar el contenido nutricional de las fiambreras (loncheras); revisión sistemática. Nutr. Hosp. 2013, 28, 1802–1805. [Google Scholar]
- Horne, P.J.; Hardman, C.A.; Lowe, C.F.; Tapper, K.; Le Noury, J.; Madden, P.; Patel, P.; Doody, M. Increasing parental provision and children’s consumption of lunchbox fruit and vegetables in Ireland: The Food Dudes intervention. Eur. J. Clin. Nutr. 2008, 63, 613–618. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.; Zask, A.; Dietrich, U. Tooty Fruity Vegie in Preschools: An obesity prevention intervention in preschools targeting children’s movement skills and eating behaviours. Health Promot. J. Austr. 2009, 20, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Zask, A.; Adams, J.K.; Brooks, L.O.; Hughes, D.F. Tooty Fruity Vegie: An obesity prevention intervention evaluation in Australian preschools. Health Promot. J. Austr. 2012, 23, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Roberts-Gray, C.; Briley, M.E.; Ranjit, N.; Byrd-Williams, C.E.; Sweitzer, S.J.; Sharma, S.V.; Palafox, M.R.; Hoelscher, D.M. Efficacy of the Lunch is in the Bag intervention to increase parents’ packing of healthy bag lunches for young children: A cluster-randomized trial in early care and education centers. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 3. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Intervention | Control | p ‡ |
|---|---|---|---|
| n = 225 | n = 177 | ||
| Mean ± SD | Mean ± SD | ||
| Age (y) | 7.9 ± 1.2 | 8.1 ± 1.2 | 0.152 |
| Sex (Female), n (%) | 101 (44.9) | 89 (50.3) | 0.282 |
| Anthropometric measures | |||
| Weight (kg) † | 29.3 ± 5.0 | 30.0 ± 5.1 | 0.154 |
| Height (cm) † | 126.3 ± 7.3 | 127.3 ± 7.4 | 0.171 |
| BMI z-score § | 0.85 ± 1.4 | 0.99 ± 1.3 | 0.290 |
| Classification of BMI §, n (%) | |||
| Normal (−2 < z-score < 1) | 129 (57.3) | 87 (49.2) | |
| Overweight (1 ≤ z-score < 2) | 52 (23.1) | 45 (25.4) | |
| Obesity (z-score ≥ 2) | 44 (19.6) | 45 (25.4) | 0.224 |
| Brought school almuerzo, n (%) | 203 (90.2) | 151 (85.3) | 0.132 |
| Brought money to buy food at school | 96 (42.7) | 76 (43.7) | 0.840 |
| Education level of the mother, n (%) | |||
| Secondary or less | 42 (20.9) | 24 (14.1) | |
| High school or technical school | 76 (37.8) | 77 (45.3) | |
| College career or postgraduate | 84 (41.3) | 69 (40.6) | 0.162 |
| Socioeconomic status (n = 356) n (%) | |||
| Lower | 63 (32.3) | 42 (26.1) | |
| Medium | 76 (39.0) | 53 (32.9) | |
| Higher | 56 (28.7) | 66 (40.1) | 0.052 |
| Macronutrients | All n = 354 Median (25p, 75p) | Intervention n = 203 Median (25p, 75p) | Control n = 151 Median (25p, 75p) |
|---|---|---|---|
| Energy (kcal) | 395 (281, 527) | 396 (269, 523) | 394 (289, 538) |
| Carbohydrates (g) | 57 (35, 79) | 55 (33, 76) | 60 (36, 83) |
| Carbohydrates (%) | 57 (46, 70) | 56 (44, 70) | 58 (49, 70) |
| Proteins (g) | 12 (8, 17) | 12 (7, 17) | 12 (8, 17) |
| Proteins (%) | 12 (9, 15) | 11 (9, 16) | 12 (8, 14) |
| Fat (g) | 13 (7, 20) | 13 (7, 20) | 13 (6, 20) |
| Fat (%) | 29 (18, 41) | 29 (18, 42) | 29 (17, 39) |
| Fiber (g) | 2.9 (1.1, 5.0) | 2.7 (1.1, 4.7) | 3.0 (1.1, 5.6) |
| Intervention (n = 193) | Control (n = 150) | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline n (%) | 6 Months n (%) | 12 Months n (%) | p‡ | Baseline n (%) | 6 Months n (%) | 12 Months n (%) | p‡ | |
| Categories According to Energy Value | ||||||||
| No school almuerzo | 21 (10.9) | 16 (8.3) | 32 (16.6) | 23 (15.3) | 17 (11.3) | 31 (20.7) | ||
| Low-calorie (<250 kcal) | 34 (17.6) | 31 (16.1) | 29 (15.0) | 20 (13.3) | 30 (20.0) | 25 (16.7) | ||
| Healthy (250 to 340 kcal) ¥ | 32 (16.6) | 38 (19.7) | 28 (14.5) | 24 (16.0) | 24 (16.0) | 11 (7.3) | ||
| High-calorie (>340 kcal) | 106 (54.9) | 108 (56.0) | 104 (53.9) | 0.012 | 83 (55.3) | 79 (52.7) | 83 (55.3) | 0.030 |
| Energy value (kcal) | Median (25p, 75p) | Median (25p, 75p) | Median (25p, 75p) | Median (25p, 75p) | Median (25p, 75p) | Median (25p, 75p) | ||
| <250 kcal | 171 (98, 224) | 176 (95, 217) | 137 (100, 186) | 194 (111, 231) | 152 (116, 216) | 183 (125, 229) | ||
| 250 to 340 kcal ¥ | 304 (272, 323) | 306 (284, 325) | 302 (273, 324) | 296 (276, 319) | 294 (261, 315) | 295 (284, 315) | ||
| ≥340 kcal | 480 (421, 582) | 473 (395, 562) | 477 (410, 595) | 508 (399, 626) | 494 (423, 595) | 486 (403, 601) | ||
| Children who only brought their own meal (kcal) | 426 (283, 542) | 394 (289, 500) | 401 (310, 547) | 415 (316, 547) | 391 (262, 498) | 420 (351, 551) | ||
| Children who brought their own meal + money (kcal) | 380 (269, 482) | 349 (292, 462) | 411 (267, 527) | 374 (290, 513) | 432 (142, 573) | 402 (236, 562) | ||
| Intervention | Control | |||||||
|---|---|---|---|---|---|---|---|---|
| Baseline Mean (95% CI) n = 203 | 6 Months Mean (95% CI) n = 195 | 12 Months Mean (95% CI) n = 162 | p * | Baseline Mean (95% CI) n = 151 | 6 Months Mean (95% CI) n = 144 | 12 Months Mean (95% CI) n = 119 | p * | |
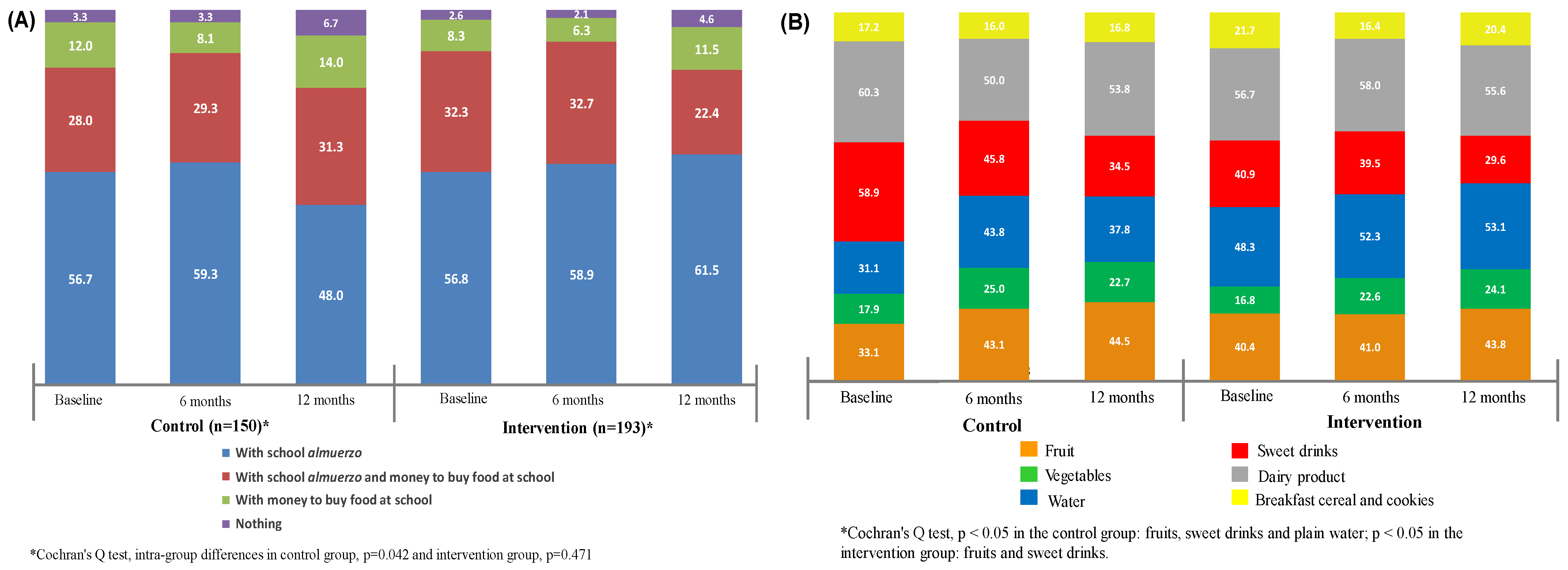
| Fruits, n (%) | 82 (40.4) | 80 (41.0) | 71 (43.8) | 0.787 | 50 (33.1) | 62 (43.1) | 53 (44.5) | 0.102 |
| Grams | 143 (119 to 167) | 180 (156 to 204) | 152 (125 to 178) | 0.112 | 146 (123 to 167) | 174 (156 to 193) | 140 (120 to 160) | 0.051 |
| % of kcal | 30.9 (25.7 to 36.1) | 24.6 (19.4 to 29.7) | 26.7 (21.0 to 32.4) | 0.269 | 21.0 (14.3 to 27.6) | 31.8 (26.1 to 37.6) | 19.8 (13.7 to 25.9) | 0.017 |
| Vegetables, n (%) | 34 (16.8) | 44 (22.6) | 39 (24.1) | 0.180 | 27 (17.9) | 36 (25.0) | 27 (22.7) | 0.319 |
| Grams | 91 (38 to 145) | 116 (74 to 156) | 103 (53 to 152) | 0.788 | 90 (33 to 146) | 118 (72 to 164) | 77 (16 to 138) | 0.572 |
| % of kcal | 9.7 (0 to 22.4) | 11.4 (1.8 to 21.1) | 18.9 (7.3 to 30.5) | 0.587 | 3.2 (0 to 12.7) | 25.8 (0 to 13.7) | 19.5 (9.2 to 29.8) | 0.106 |
| Water, n (%) | 98 (48.3) | 102 (52.3) | 86 (53.1) | 0.601 | 47 (31.1) | 63 (43.8) | 45 (37.8) | 0.081 |
| Milliliters | 454 (407 to 501) | 510 (464 to 555) | 546 (496 to 595) | 0.044 | 445 (366 to 525) | 547 (483 to 610) | 556 (477 to 634) | 0.132 |
| Sweet drinks, n (%) | 83 (40.9) | 77 (39.5) | 48 (29.6) | 0.061 | 89 (58.9) | 66 (45.8) | 41 (34.5) | <0.001 |
| Milliliters | 384 (334 to 433) | 399 (349 to 450) | 509 (441 to 576) | 0.019 | 407 (363 to 451) | 467 (415 to 518) | 571 (501 to 641) | 0.002 |
| % of kcal | 26.3 (23.5 to 29.1) | 27.7 (24.9 to 30.1) | 32.7 (28.8 to 36.5) | 0.047 | 27.7 (24.0 to 31.6) | 32.4 (27.9 to 36.9) | 28.1 (32.1 to 44.1) | 0.024 |
| Dairy products, n (%) | 117 (56.7) | 114 (58.0) | 90 (55.6) | 0.901 | 91 (60.3) | 72 (50.0) | 64 (53.8) | 0.201 |
| Grams | 79 (63 to 95) | 77 (61 to 93) | 92 (74 to 109) | 0.450 | 60 (42 to 77) | 85 (65 to 104) | 66 (45 to 86) | 0.198 |
| % of kcal | 27.1 (23.7 to 30.6) | 26.4 (22.9 to 29.7) | 30.1 (26.2 to 33.9) | 0.349 | 21.7 (17.3 to 26.1) | 24.0 (19.0 to 29.0) | 25.1 (19.8 to 30.4 | 0.642 |
| Cookies, n (%) | 44 (21.7) | 32 (16.4) | 33 (20.4) | 0.391 | 26 (17.2) | 23 (16.0) | 20 (16.8) | 0.958 |
| Grams | 55 (43 to 67) | 35 (21 to 48) | 38 (24 to 51) | 0.090 | 58 (42 to 75) | 63 (44 to 81) | 51 (32 to 68) | 0.662 |
| % of kcal | 40.9 (28.8 to 70.3) | 24.2 (12.8 to 39.7) | 27.5 (16.3 to 38.7) | <0.001 | 42.2 (26.4 to 52.7) | 48.3 (22.2 to 73.2) | 51.2 (22.5 to 71.2) | 0.664 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vilchis-Gil, J.; Klünder-Klünder, M.; Duque, X.; Martínez-Andrade, G.; Martínez-Almaráz, A.; Beristain-Lujano, B.; Flores-Huerta, S. Impact of a Nutrition-Related Community Intervention on the Quantity and Quality of Children’s School almuerzo. Life 2021, 11, 253. https://doi.org/10.3390/life11030253
Vilchis-Gil J, Klünder-Klünder M, Duque X, Martínez-Andrade G, Martínez-Almaráz A, Beristain-Lujano B, Flores-Huerta S. Impact of a Nutrition-Related Community Intervention on the Quantity and Quality of Children’s School almuerzo. Life. 2021; 11(3):253. https://doi.org/10.3390/life11030253
Chicago/Turabian StyleVilchis-Gil, Jenny, Miguel Klünder-Klünder, Ximena Duque, Gloria Martínez-Andrade, Andrea Martínez-Almaráz, Brenda Beristain-Lujano, and Samuel Flores-Huerta. 2021. "Impact of a Nutrition-Related Community Intervention on the Quantity and Quality of Children’s School almuerzo" Life 11, no. 3: 253. https://doi.org/10.3390/life11030253
APA StyleVilchis-Gil, J., Klünder-Klünder, M., Duque, X., Martínez-Andrade, G., Martínez-Almaráz, A., Beristain-Lujano, B., & Flores-Huerta, S. (2021). Impact of a Nutrition-Related Community Intervention on the Quantity and Quality of Children’s School almuerzo. Life, 11(3), 253. https://doi.org/10.3390/life11030253







