The Relationship between the Concentration of Magnesium and the Presence of Depressive Symptoms and Selected Metabolic Disorders among Men over 50 Years of Age
Abstract
1. Introduction
2. Materials and Methods
2.1. Characteristics of the Study Sample
2.2. Questionnaire Survey
2.3. Determination of Magnesium by the Spectrophotometric Method
2.4. Determination of Lipids and Glucose by Spectrophotometric Method
2.5. Anthropometric and Blood Pressure Measurements
2.6. Statistical Analysis
3. Results
4. Discussion
4.1. Magnesium and Depressive Disorders
4.2. Magnesium and Metabolic Disorders
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Trivedi, M.H.; Greer, T.L. Cognitive dysfunction in unipolar depression: Implications for treatment. J. Affect. Disord. 2014, 152, 19–27. [Google Scholar] [CrossRef]
- Volkert, J.; Schulz, H.; Härter, M.; Wlodarczyk, O.; Andreas, S. The prevalence of mental disorders in older people in Western countries—A meta-analysis. Ageing Res. Rev. 2013, 12, 339–353. [Google Scholar] [CrossRef] [PubMed]
- Solhaug, H.I.; Romuld, E.B.; Romild, U.; Stordal, E. Increased prevalence of depression in cohorts of the elderly: An 11-year follow-up in the general population—the HUNT study. Int. Psychogeriatr. 2011, 24, 151–158. [Google Scholar] [CrossRef]
- Dobrzyńska, E.; Rymaszewska, J.; Kiejna, A. Depresje u osób w wieku podeszłym. Depressions in the elderly. Psychogeriatria Pol. 2007, 4, 51–60. [Google Scholar]
- Jarema, M.; Dudek, D.; Czernikiewicz, A. Dysfunkcje poznawcze w depresji—Niedoszacowany objaw czy nowy wymiar? Psychiatr. Pol. 2014, 48, 1105–1116. [Google Scholar] [CrossRef]
- Wang, C.; Liu, F.; Patterson, T.A.; Paule, M.G.; Slikker, W., Jr. Relationship between ketamine-induced developmental neurotoxicity and NMDA receptor-mediated calcium influx in neural stem cell-derived neurons. NeuroToxicology 2017, 60, 254–259. [Google Scholar] [CrossRef]
- Eby, G.A.; Eby, K.L. Magnesium for treatment-resistant depression: A review and hypothesis. Med. Hypotheses 2010, 74, 649–660. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, C.C.; Lobato, K.R.; Binfaré, R.W.; Ferreira, P.K.; Rosa, A.O.; Santos, A.R.S.; Rodrigues, A.L.S. Evidence for the involvement of the monoaminergic system in the antidepressant-like effect of magnesium. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2009, 33, 235–242. [Google Scholar] [CrossRef]
- You, H.J.; Cho, S.-E.; Kang, S.-G.; Cho, S.-J.; Na, K.-S. Decreased serum magnesium levels in depression: A systematic review and meta-analysis. Nord. J. Psychiatry 2018, 72, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Cheungpasitporn, W.; Thongprayoon, C.; Mao, M.A.; Srivali, N.; Ungprasert, P.; Varothai, N.; Sanguankeo, A.; Kittanamongkolchai, W.; Erickson, S.B. Hypomagnesaemia linked to depression: A systematic review and meta-analysis. Intern. Med. J. 2015, 45, 436–440. [Google Scholar] [CrossRef]
- Martínez-González, M.Á.; Sánchez-Villegas, A. Magnesium intake and depression: The SUN cohort. Magnes Res. 2016, 29, 102–111. [Google Scholar] [CrossRef]
- Popa, T.A.; Ladea, M. Nutrition and depression at the forefront of progress. J. Med. Life 2012, 5, 414–419. [Google Scholar] [PubMed]
- Quirk, S.E.; Williams, L.J.; O’Neil, A.; Pasco, J.A.; Jacka, F.N.; Housden, S.; Berk, M.; Brennan, S.L. The association between diet quality, dietary patterns and depression in adults: A systematic review. BMC Psychiatry 2013, 13, 175. [Google Scholar] [CrossRef]
- Houston, M. The Role of Magnesium in Hypertension and Cardiovascular Disease. J. Clin. Hypertens. 2011, 13, 843–847. [Google Scholar] [CrossRef] [PubMed]
- Kostov, K.; Halacheva, L. Role of Magnesium Deficiency in Promoting Atherosclerosis, Endothelial Dysfunction, and Arterial Stiffening as Risk Factors for Hypertension. Int. J. Mol. Sci. 2018, 19, 1724. [Google Scholar] [CrossRef]
- Harvey, A.; Montezano, A.C.; Lopes, R.A.; Rios, F.; Touyz, R.M. Vascular Fibrosis in Aging and Hypertension: Molecular Mechanisms and Clinical Implications. Can. J. Cardiol. 2016, 32, 659–668. [Google Scholar] [CrossRef]
- Wu, J.; Xun, P.; Tang, Q.; Cai, W.; He, K. Circulating magnesium levels and incidence of coronary heart diseases, hypertension, and type 2 diabetes mellitus: A meta-analysis of prospective cohort studies. Nutr. J. 2017, 16, 1–13. [Google Scholar] [CrossRef]
- Han, H.; Fang, X.; Wei, X.; Liu, Y.; Jin, Z.; Chen, Q.; Fan, Z.; Aaseth, J.; Hiyoshi, A.; He, J.; et al. Dose-response relationship between dietary magnesium intake, serum magnesium concentration and risk of hypertension: A systematic review and meta-analysis of prospective cohort studies. Nutr. J. 2017, 16, 26. [Google Scholar] [CrossRef] [PubMed]
- Suárez, A.; Pulido, N.; Casla, A.; Casanova, B.; Arrieta, F.J.; Rovira, A. Impaired tyrosine-kinase activity of muscle insulin receptors from hypomagnesaemic rats. Diabetologia 1995, 38, 1262–1270. [Google Scholar] [CrossRef]
- Veronese, N.; Watutantrige-Fernando, S.; Luchini, C.; Solmi, M.; Sartore, G.; Sergi, G.; Manzato, E.; Barbagallo, M.; Maggi, S.; Stubbs, B. Effect of magnesium supplementation on glucose metabolism in people with or at risk of diabetes: A systematic review and meta-analysis of double-blind randomized controlled trials. Eur. J. Clin. Nutr. 2016, 70, 1354–1359. [Google Scholar] [CrossRef]
- Xu, B.; Sun, J.; Deng, X.; Huang, X.; Sun, W.; Xu, Y.; Xu, M.; Lu, J.; Bi, Y. Low Serum Magnesium Level Is Associated with Microalbuminuria in Chinese Diabetic Patients. Int. J. Endocrinol. 2013, 2013, 1–6. [Google Scholar] [CrossRef]
- Rodríguez-Morán, M.; Guerrero-Romero, F. Oral Magnesium Supplementation Improves Insulin Sensitivity and Metabolic Control in Type 2 Diabetic Subjects: A randomized double-blind controlled trial. Diabetes Care 2003, 26, 1147–1152. [Google Scholar] [CrossRef]
- Belin, R.J.; He, K. Magnesium physiology and pathogenic mechanisms that contribute to the development of the metabolic syndrome. Magnes Res. 2007, 20, 107–129. [Google Scholar]
- Reckelhoff, J.F. Gender differences in hypertension. Curr. Opin. Nephrol. Hypertens. 2018, 27, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Salk, R.H.; Hyde, J.S.; Abramson, L.Y. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol. Bull. 2017, 143, 783–822. [Google Scholar] [CrossRef]
- Goodale, T.; Sadhu, A.; Petak, S.; Robbins, R. Testosterone and the Heart. Methodist DeBakey Cardiovasc. J. 2017, 13, 68–72. [Google Scholar] [CrossRef]
- Danysz, W.; Zajaczkowski, W.; Parsons, C.G. Modulation of learning processes by ionotropic glutamate receptor ligands. Behav. Pharmacol. 1995, 6, 455–474. [Google Scholar] [CrossRef] [PubMed]
- Castilho, R.F.; Ward, M.W.; Nicholls, D.G. Oxidative stress, mitochondrial function, and acute glutamate excitotoxicity in cultured cerebellar granule cells. J. Neurochem. 2001, 72, 1394–1401. [Google Scholar] [CrossRef]
- Eby, G.A.; Eby, K.L. Rapid recovery from major depression using magnesium treatment. Med. Hypotheses 2006, 67, 362–370. [Google Scholar] [CrossRef] [PubMed]
- Murck, H. Magnesium and Affective Disorders. Nutr. Neurosci. 2002, 5, 375–389. [Google Scholar] [CrossRef]
- Imada, Y.; Yoshioka, S.-I.; Ueda, T.; Katayama, S.; Kuno, Y.; Kawahara, R. Relationships between serum magnesium levels and clinical background factors in patients with mood disorders. Psychiatry Clin. Neurosci. 2002, 56, 509–514. [Google Scholar] [CrossRef]
- Eby, G.A.; Eby, K.L.; Murk, H. Magnesium and major depression. In Magnesium in the Central Nervous System; Vink, R., Nechifor, M., Eds.; University of Adelaide Press: Adelaide, Australia, 2011. Available online: https://www.ncbi.nlm.nih.gov/b (accessed on 1 January 2021).
- Paolisso, G.; Scheen, A.; D’Onofrio, F. Magnesium and glucose homeostasis. Diabetologia 1990, 33, 511–514. [Google Scholar] [CrossRef]
- Mather, H.; Nisbet, J.A.; Burton, G.; Poston, G.; Bland, J.; Bailey, P.A.; Pilkington, T. Hypomagnesaemia in diabetes. Clin. Chim. Acta 1979, 95, 235–242. [Google Scholar] [CrossRef]
- Vanroelen, W.F.; Gaal, L.F.; Rooy, P.E.; Leeuw, I.H. Serum and erythrocyte magnesium levels in type I and type II diabetics. Acta Diabetol. 1985, 22, 185–190. [Google Scholar] [CrossRef]
- Djurhuus, M.S.; Klitgaard, N.A.; Henriksen, J.E. Magnesium deficiency in patients with type 1 (insulin dependent) diabetes mellitus (abst). Diabetes 1994, 43, 259A. [Google Scholar]
- Schmidt, L.; Heins, J. Low magnesium intake among NIDDM patients: A call for concern (abst). Diabetes 1993, 42, 49A. [Google Scholar]
- Mooren, F.C.; Krüger, K.; Völker, K.; Golf, S.W.; Wadepuhl, M.; Kraus, A. Oral magnesium supplementation reduces insulin resistance in non-diabetic subjects—A double-blind, placebo-controlled, randomized trial. Diabetes Obes. Metab. 2011, 13, 281–284. [Google Scholar] [CrossRef]
- de Lourdes Lima de Souza e Silva, M.; Cruz, T.; Rodrigues, L.E.; Ladeia, A.M.; Bomfim, O.; Olivieri, L.; Melo, J.; Correia, R.; Porto, M.; Cedro, A. Magnesium Replacement Does Not Improve Insulin Resistance in Patients with Metabolic Syndrome: A 12-Week Randomized Double-Blind Study. J. Clin. Med. Res. 2014, 6, 456–462. [Google Scholar] [CrossRef]
- McCarron, D.A.; Morris, C.D.; Cole, C. Dietary calcium in human hypertension. Science 1982, 217, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Guerrero-Romero, F.; Simental-Mendía, L.E.; Hernández-Ronquillo, G.; Rodriguez-Morán, M. Oral magnesium supplementation improves glycaemic status in subjects with prediabetes and hypomagnesaemia: A double-blind placebo-controlled randomized trial. Diabetes Metab. 2015, 41, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Moran, M.; Guerrero-Romero, F. Oral Magnesium Supplementation Improves the Metabolic Profile of Metabolically Obese, Normal-weight Individuals: A Randomized Double-blind Placebo-controlled Trial. Arch. Med. Res. 2014, 45, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Villa-Bellosta, R. Impact of magnesium:calcium ratio on calcification of the aortic wall. PLoS ONE 2017, 12, e0178872. [Google Scholar] [CrossRef]
- Louvet, L.; Bazin, D.; Büchel, J.; Steppan, S.; Passlick-Deetjen, J.; Massy, Z.A. Characterisation of Calcium Phosphate Crystals on Calcified Human Aortic Vascular Smooth Muscle Cells and Potential Role of Magnesium. PLoS ONE 2015, 10, e0115342. [Google Scholar] [CrossRef] [PubMed]
- Hruby, A.; O’Donnell, C.J.; Jacques, P.F.; Meigs, J.B.; Hoffmann, U.; McKeown, N.M. Magnesium Intake Is Inversely Associated with Coronary Artery Calcification. JACC Cardiovasc. Imaging 2014, 7, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Ichihara, A.; Suzuki, H.; Saruta, T. Effects of magnesium on the renin-angiotensin-aldosterone system in human subjects. J. Lab. Clin. Med. 1993, 122, 432–440. [Google Scholar]
- Galan, P.; Preziosi, P.; Durlach, V.; Valeix, P.; Ribas, L.; Bouzid, D.; Favier, A.; Hercberg, S. Dietary magnesium intake in a French adult population. Magnes Res. 1997, 10, 321–328. [Google Scholar]
- Doyle, L.; Flynn, A.; Cashman, K. The effect of magnesium supplementation on biochemical markers of bone metabolism or blood pressure in healthy young adult females. Eur. J. Clin. Nutr. 1999, 53, 255–261. [Google Scholar] [CrossRef]
| Age (Years) Mean ± SD; Me | 61.66 ± 6.38; 62.00 | |
| Education (n, %) | Vocational | 59 (17.25%) |
| Primary | 19 (5.56%) | |
| Secondary | 140 (40.94%) | |
| Higher | 119 (34.80%) | |
| Smoking (n, %) | 55 (16.08%) | |
| Marital status (n, %) | Married | 72 (21.05%) |
| Unmarried | 267 (78.07%) | |
| BMI (n, %) | 18.5–24.9 | 66 (19.30%) |
| 25.0–29.9 | 177 (51.75%) | |
| 30.0–34.9 | 72 (21.05%) | |
| 35.0–39.9 | 17 (4.97%) | |
| ≥40.0 | 8 (2.34%) | |
| BMI (kg/m2); mean ± SD; Me | 28.41 ± 4.40; 27.77 | |
| Classification WHR (n, %) | ≤1.0 | 154 (64.98%) |
| >1.0 | 83 (35.02%) | |
| WHR mean ± SD; Me | 0.99 ± 0.07; 0.99 | |
| Hip circumference (cm) mean ± SD; Me | 103.10 ± 7.83; 103 | |
| Abdomen circumference (cm) mean ± SD; Me | 102.20 ± 12.08; 100 | |
| TAG (mg/dL); mean ± SD; Me | 145.26 ± 82.92; 121.82 | |
| Cholesterol (mg/dL); mean ± SD; Me | 216 ± 56.98; 211.69 | |
| HDL (mg/dL); mean ± SD; Me | 48.33 ± 12.32; 46.45 | |
| LDL (mg/dL); mean ± SD; Me | 140.69 ± 59.77; 133.48 | |
| Diabetes mellitus (n, %) | 56 (16.37%) | |
| Glucose (mg/dL); mean ± SD; Me | 106.73 ± 38.59; 103.06 | |
| Hypertension (n, %) | 190 (55.56%) | |
| RR systolic; mean ± SD; Me | 135.18 ± 19.71; 135 | |
| RR diastolic; mean ± SD; Me | 88.47 ± 56.17; 80 | |
| Insulin (µLU/mL); mean ± SD; Me | 14.84 ± 7.66; 13.45 | |
| HOMA; mean ± SD; Me | 3.94 ± 2.22; 3.44 | |
| Serum Mg (mg/L); mean ± SD; Me | 21.22 ± 2.52; 21.05 | |
| Without Depressiveness (n = 249) | With Depressiveness (n = 93) | p | |
|---|---|---|---|
| BMI (kg/m2); mean ± SD; Me | 28.17 ± 4.1; 27.73 | 29.02 ± 5.09; 28.58 | 0.169 |
| Abdomen (cm) mean ± SD; Me | 101.82 ± 11.25; 100 | 103.19 ± 14.01; 101 | 0.604 |
| TAG (mg/dL); mean ± SD; Me | 142.66 ± 80.98; 121.82 | 152.18 ± 87.95; 121.83 | 0.343 |
| Cholesterol (mg/dL); mean ± SD; Me | 215.11 ± 55.25; 213.96 | 218.48 ± 61.62; 209.04 | 0.837 |
| HDL (mg/dL); mean ± SD; Me | 48.37 ± 12.62; 46.53 | 48.24 ± 11.55; 46.18 | 0.94 |
| LDL (mg/dL); mean ± SD; Me | 141.02 ± 59.60; 133.98 | 139.81 ± 60.53; 132.79 | 0.888 |
| Diabetes mellitus (n, %) | 37 (14.98%) | 19 (20.43%) | 0.227 |
| Hypertension (n, %) | 133 (53.85%) | 57 (61.29%) | 0.219 |
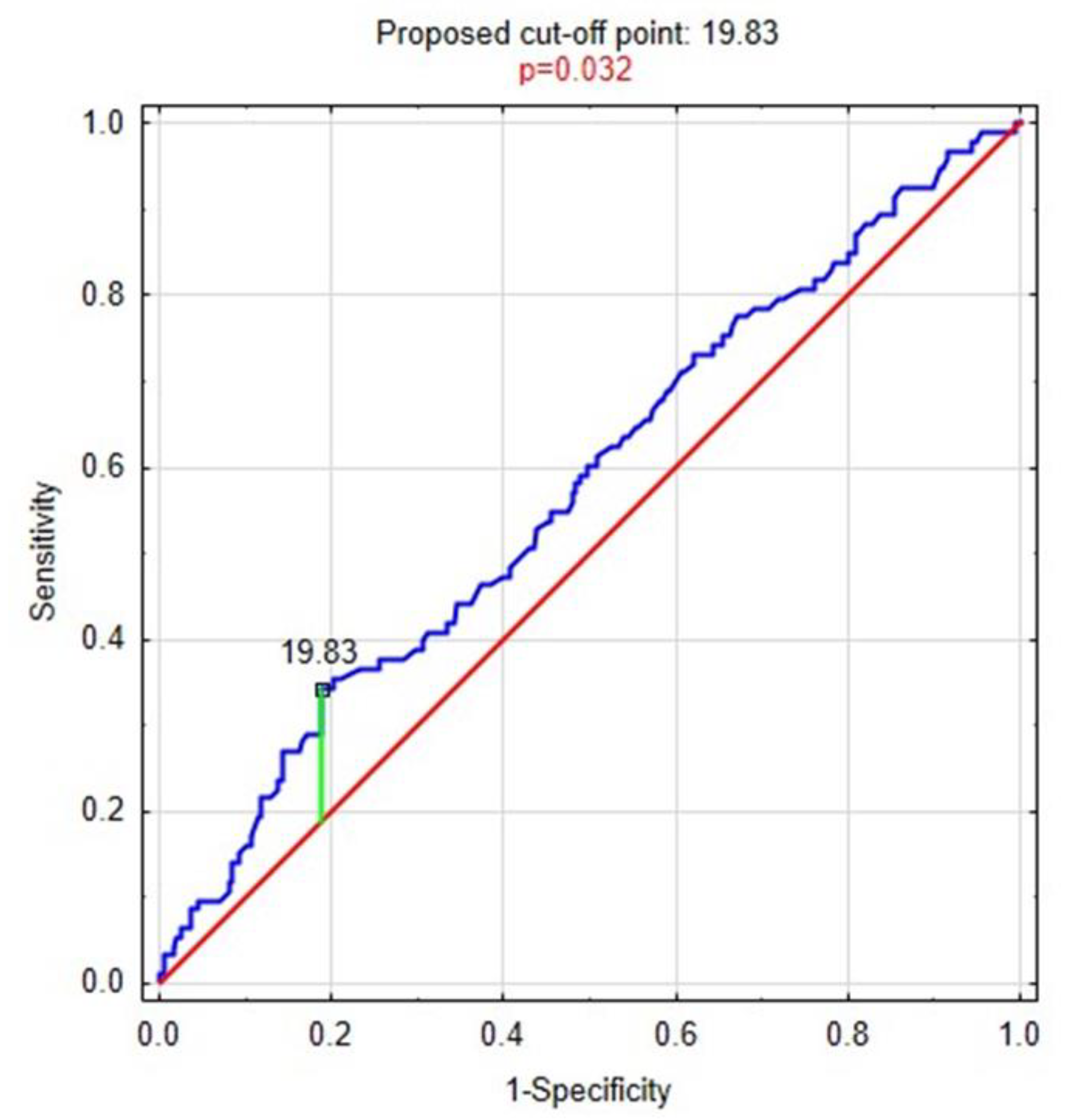
| Serum Mg (mg/L); mean ± SD; Me | 21.42 ± 2.49; 21.2 | 20.69 ± 2.56; 20.8 | 0.032 |
| Mg ≤ 19.83 (n = 78) | Mg > 19.83 (n = 263) | p | |
|---|---|---|---|
| BMI (kg/m2), mean ± SD; Me | 28.89 ± 4.36; 28.31 | 28.27 ± 4.42; 27.73 | 0.244 |
| Abdomen (cm), mean ± SD; Me | 104.51 ± 11.39; 101.50 | 101.51 ± 12.22; 100.00 | 0.056 |
| TAG (mg/dL), mean ± SD; Me | 148.97 ± 82.89; 120.67 | 144.14 ± 83.05; 121.82 | 0.716 |
| Cholesterol (mg/dL), mean ± SD; Me | 193.27 ± 50.49; 190.96 | 222.85 ± 57.13; 221.65 | <0.001 |
| HDL (mg/dL), mean ± SD; Me | 47.59 ± 12.20; 45.16 | 48.56 ± 12.37; 46.59 | 0.801 |
| LDL (mg/dL), mean ± SD; Me | 117.37 ± 49.51; 117.45 | 147.69 ± 60.88; 143.73 | <0.001 |
| Diabetes mellitus (n, %) | 28 (35.90%) | 28 (10.81%) | <0.001 |
| Hypertension (n, %) | 57 (73.08%) | 130 (50.19%) | <0.001 |
| Depressiveness (n, %) | 32 (41.03%) | 61 (23.37%) | 0.002 |
| Unadjusted | Adjusted by Age, BMI, WHR, Smoking, Education, Marital Status, Professional Activity | |||||||
|---|---|---|---|---|---|---|---|---|
| p | OR | −95% | 95% | p | OR | −95% | 95% | |
| BMI (kg/m2) | 0.288 | 1.031 | 0.975 | 1.090 | 0.101 | 1.052 | 0.990 | 1.117 |
| Abdomen (cm) | 0.058 | 1.020 | 0.999 | 1.041 | 0.021 | 1.026 | 1.004 | 1.049 |
| TAG (mg/dL) | 0.652 | 1.001 | 0.998 | 1.004 | 0.472 | 1.001 | 0.998 | 1.004 |
| Cholesterol (mg/dL) | <0.001 | 0.990 | 0.985 | 0.995 | <0.001 | 0.989 | 0.983 | 0.994 |
| HDL (mg/dL) | 0.545 | 0.994 | 0.973 | 1.015 | 0.290 | 0.988 | 0.966 | 1.010 |
| LDL (mg/dL) | <0.001 | 0.989 | 0.984 | 0.994 | <0.001 | 0.988 | 0.983 | 0.994 |
| Diabetes mellitus | <0.001 | 4.620 | 2.519 | 8.473 | <0.001 | 4.614 | 2.451 | 8.686 |
| Hypertension | <0.001 | 2.693 | 1.544 | 4.699 | <0.001 | 2.833 | 1.584 | 5.069 |
| Depressiveness | 0.003 | 2.281 | 1.336 | 3.893 | 0.009 | 2.135 | 1.210 | 3.769 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rotter, I.; Wiatrak, A.; Rył, A.; Kotfis, K.; Sipak-Szmigiel, O.; Ptak, M.; Tomska, N.; Szylińska, A. The Relationship between the Concentration of Magnesium and the Presence of Depressive Symptoms and Selected Metabolic Disorders among Men over 50 Years of Age. Life 2021, 11, 196. https://doi.org/10.3390/life11030196
Rotter I, Wiatrak A, Rył A, Kotfis K, Sipak-Szmigiel O, Ptak M, Tomska N, Szylińska A. The Relationship between the Concentration of Magnesium and the Presence of Depressive Symptoms and Selected Metabolic Disorders among Men over 50 Years of Age. Life. 2021; 11(3):196. https://doi.org/10.3390/life11030196
Chicago/Turabian StyleRotter, Iwona, Adrian Wiatrak, Aleksandra Rył, Katarzyna Kotfis, Olimpia Sipak-Szmigiel, Magdalena Ptak, Natalia Tomska, and Aleksandra Szylińska. 2021. "The Relationship between the Concentration of Magnesium and the Presence of Depressive Symptoms and Selected Metabolic Disorders among Men over 50 Years of Age" Life 11, no. 3: 196. https://doi.org/10.3390/life11030196
APA StyleRotter, I., Wiatrak, A., Rył, A., Kotfis, K., Sipak-Szmigiel, O., Ptak, M., Tomska, N., & Szylińska, A. (2021). The Relationship between the Concentration of Magnesium and the Presence of Depressive Symptoms and Selected Metabolic Disorders among Men over 50 Years of Age. Life, 11(3), 196. https://doi.org/10.3390/life11030196







